Abstract
The present study aimed to identify pathways to suicidal behavior in late life that can guide identification of those most at risk and improve treatment. In a longitudinal study of late-life depression, we prospectively assessed risk factors specifically associated with fatal and near-fatal as compared to less lethal suicidal behavior. We enrolled 401 participants (age 66 ± 9.9): 311 with unipolar non-psychotic depression and 90 non-psychiatric controls. The median follow-up was 5.4 years. Results indicated that history of suicide attempt predicted a two-fold increase in the risk of dying from natural causes. In univariate models, male gender, higher income, current depression and current and worst lifetime suicidal ideation severity, cognitive control deficits, and low levels of non-planning impulsivity predicted fatal and near-fatal suicidal behavior. In contrast, incident less lethal suicidal behavior was mostly associated with maladaptive personality traits, impulsivity, and severity of psychiatric illness in univariate models. In multipredictor models, male gender, worst lifetime suicidal ideation, and deficits in cognitive control independently predicted fatal/near-fatal suicidal behavior, while introversion, history of suicide attempt, and earlier age of onset of depression predicted less lethal suicidal behavior. While clinicians may be familiar with suicide risk factors identified in younger samples such as dysfunctional personality, impulsivity, and co-morbid substance use, in late life these characteristics only pertain to lower-lethality suicidal behavior. Cognitive control deficits, which likely play a greater role in old age, predict serious suicidal behavior.
Keywords: Incident suicidal behavior, Late-life depression, Cognition, Personality, Cognitive control
1. Introduction
Suicidal behavior is heterogeneous, ranging in its medical seriousness from fatal and near-fatal cases to those that do not require medical attention. This variation does not appear to merely reflect different stages in the progression of the suicidal process or external circumstances. Rather, it may reflect psychologically distinct pathways to suicidal behavior, at least in older adults (Dombrovski et al., 2012, 2011; Richard-Devantoy et al., 2015; Szanto et al., 2018, 2014; Vanyukov et al., 2017, 2016). These pathways, however, have yet to be prospectively validated. Thus, our longitudinal study of high-suicide-risk older adults examined unique risk factors associated with fatal or near-fatal suicidal behavior. We examined a broad range of potential risk factors, including cognition and personality/interpersonal functioning.
Globally, suicide rates increase after sixty years of age, particularly in males. While the reasons for this elevated suicide risk are complex, suicide attempts in late life appear more akin to “failed” suicides (Conwell et al., 1998; De Leo et al., 2001; Dombrovski et al., 2008; Friedmann and Kohn, 2008), characterized by high lethality and intent that does not subside after the initial attempt. A study by Murphy and colleagues found that elderly individuals who were admitted to a hospital following a suicide attempt were three times more likely to die by suicide than younger attempters, and the risk of suicide was 67 times that of older adults in the general population (Murphy et al., 2012). Thus, attempted suicide in late life gives us a unique window into processes that result in death by suicide (Pearson and Brown, 2000).
Traditionally recognized risk factors (including hopelessness, comorbidity with psychiatric and substance use disorders, impulsivity) provide more information about suicide contemplation than suicidal behavior (Franklin et al., 2017; Klonsky et al., 2017; May and Klonsky, 2016). While contemplation is a necessary antecedent of suicide, its predictors often differ from those of the transition from ideation to attempt (May and Klonsky, 2016; Franklin et al., 2017; Klonsky et al., 2017; Oquendo et al., 2004). Machine learning approaches identified history of attempt, psychiatric diagnoses and substance abuse, as well as hospitalization for any physical health problems, diagnoses related to injuries, and chronic infections as predictors for suicidal behavior using medical records (Kessler et al., 2017, 2015). However, medical records generally lack the detailed cognitive and clinical characterization necessary to parse out the heterogeneity, and medical record data have not yet been used to stratify attempters based on the severity of the attempt.
The heterogeneity of suicidal behavior indicates that no single deficit may be shared by all suicidal people. Heterogeneity implies the existence of multivariate patterns of risk factors including psychopathology, personality traits, impulsivity, somatic illness burden, sociodemographic factors, and cognition. Evidence suggests that risk factors may be different for low and high lethality attempt. While the interpersonal theory of suicide posits that perceived burdensomeness is a predictor of suicide ideation and suicide attempt (Joiner et al., 2002), some evidence suggests this may predict only low-lethality attempts in late life (Vanyukov et al., 2017). Similarly, impulsivity has been proposed as an endophenotype for suicidal behavior, yet many older suicide attempters do not exhibit high levels of impulsivity (McGirr et al., 2008). It may be the case that the contribution of specific suicide vulnerability factors changes across the life-cycle. Neurocognitive and decision-related factors, for example, may play a particularly salient role in late-life suicide due to age-related cognitive decline (Erlangsen et al., 2008; Tu et al., 2016). The study of older adults provides a unique opportunity to examine the cognitive diathesis and its role in late-life suicide.
Therefore, we performed a longitudinal study of late-life depression to elucidate the psychological and cognitive mechanisms leading to various types of suicidal behavior. Previous studies mostly linked cognitive deficits with near-fatal (high medical lethality) attempts (Keilp et al., 2001; McGirr et al., 2012; Richard-Devantoy et al., 2015), while maladaptive personality was predominantly associated with low medical lethality suicide attempts (Oquendo et al., 2007). Thus, we predicted that incident fatal and near-fatal suicidal behavior (encompassing high medical lethality attempts and death by suicide), will be predicted by cognitive deficits. In contrast, interpersonal difficulties and impulsivity will predict lower-lethality suicide-related behavior (referred to as less lethal suicide events), including attempts that were low-medical lethality or aborted, as well as emergency referrals to psychiatric hospitals to prevent suicide, which are commonly included as broadly-defined suicide events in other studies (Brent et al., 2009; Melhem et al., 2019).
To address the heterogeneity of late-life suicide attempts, we used detailed clinical and cognitive characterization in addition to traditionally measured suicide risk factors. Given the low base rate of suicidal behavior even among those who suffer from depression, our recruitment strategy was to oversample those at-risk for suicidal behavior, such as those with a history of suicide attempt and suicidal ideation. We broke down suicidal outcomes by medical lethality in order to examine whether cognitive and personality characteristics map onto distinct putative pathways of suicidal behavior. Thus, our prospectively observed events of interest included: (1) fatal and near-fatal suicidal behavior and (2) less lethal suicide events. In an additional analysis, we explored the associations of suicide risk with other adverse outcomes, namely, whether mortality from natural causes was increased in those who had a history of suicide attempt. Since some studies reported higher treatment-resistance in suicidal depressed patients (Jick et al., 1995; Melhem et al., 2019; Szanto et al., 2003, 2001), while others found a history of inadequate treatment (Isacsson et al., 1992), we also examined whether greater intensity of past antidepressant treatment predicted incident suicidal behavior.
2. Experimental procedures
2.1. Sample
The total sample included 401 older adults who participated in a longitudinal study of late-life depression and decision-making (Szanto et al., 2015). We tested the effect of baseline clinical and cognitive/decision-making factors on prospectively assessed suicidal behavior (median follow-up: 5.4 years). Subjects’ timeframe for the study spanned from 30 days to 5307 days (14.5 years for our first recruited pilot study participants) in 311 non-demented depressed older-adults: 153 with prior attempts at enrollment, 71 with suicidal ideation only, and 87 without any history of suicide attempt or ideation. Ninety non-psychiatric controls served as a benchmark. Participants provided written informed consent as required by the University of Pittsburgh Institutional Review Board. They were recruited from psychogeriatric inpatient units, a late-life depression clinic, primary care, and community advertisements.
2.1.1. Baseline group status
Suicide attempters had (1) a self-injurious act with the intent to die within one month of completing the study assessments, or (2) a previous suicide attempt and current suicidal ideation with a plan at the time of study enrollment. We followed the O’Caroll definition for suicide attempt (O’Carroll et al., 1996) (self-injurious act undertaken with intent to die) to establish baseline attempter status as well as incident suicide attempts during follow up. Prospective and retrospective assessments of suicidal behavior were verified by a psychiatrist, using all available information, including participant’s report, medical records, and collateral information from family or friends. Suicide ideators had suicidal ideation with a specific plan at the time of recruitment. They may have had history of preparatory acts for suicide or aborted attempts, but no lifetime history of suicide attempt. Non-suicidal depressed older adults had no lifetime history of self-injurious behavior, suicidal ideation, or suicide attempts, based on clinical interviews, review of medical records, SCID/DSM-IV, and a score of 0 on the suicide item of the 17-item Hamilton Rating Scale for Depression (HRSD-17)(Hamilton, 1960). All participants in the attempter, ideator, and non-suicidal groups had a SCID/DSM-IV diagnosis of unipolar, non-psychotic major depression and a score of 14 or higher on the HRSD-17 at study entry. Healthy controls additionally had no lifetime history of psychiatric disorders, as determined by the SCID/DSM-IV and no history of suicidal ideation or behavior. We excluded individuals with clinical dementia (clinical diagnosis or score <23 on the Mini-Mental State Examination (Folstein et al., 1975), neurological disorder, delirium, or sensory disorder that would preclude completion of the cognitive tasks.
Demographic, clinical, cognitive, and impulsivity/personality measures across groups and mean differences therein are reported in Supplementary Tables 1a and 1b.
Table 1.
Univariate Models for Suicidal Behavior.
| 95% Confidence Interval | |||||
|---|---|---|---|---|---|
| B | Hazard Ratio | Lower Bound | Upper Bound | P Value | |
| 1a. Fatal and Near-fatal suicidal behavior | |||||
| Socio-Demographic | |||||
| Sex (Male) | 1.53 | 4.61 | 1.33 | 16.06 | 0.016 |
| Income (Per Capita) | 0.28 | 1.32 | 1.10 | 1.59 | 0.003 |
| Physical Illness Burden | |||||
| Overalli | 0.18 | 1.20 | 0.80 | 1.79 | 0.380 |
| Highii | 0.09 | 1.09 | 0.94 | 1.26 | 0.250 |
| Severity of Psychiatric illness | |||||
| Depression severityiii | 0.47 | 1.60 | 1.14 | 2.25 | 0.006 |
| Age of depression onset | 0.01 | 1.01 | 0.98 | 1.04 | 0.520 |
| Prior attemptiv | 0.44 | 1.56 | 0.55 | 4.40 | 0.400 |
| Ideation | |||||
| Currentv | 0.48 | 1.62 | 1.17 | 2.22 | 0.003 |
| Worst Lifetimevi | 0.65 | 1.92 | 1.38 | 2.66 | 0.000 |
| Substance use disorder | |||||
| Currentvii | 0.61 | 1.84 | 0.54 | 6.21 | 0.330 |
| Lifetimevii | −0.49 | 0.61 | 0.20 | 1.90 | 0.400 |
| Cognition | |||||
| Verbal IQviii | 0.05 | 1.05 | 0.64 | 1.71 | 0.850 |
| Executive Functionix | 0.42 | 1.52 | 1.19 | 1.94 | 0.001 |
| Global Cognitive Functioningx | 0.09 | 1.10 | 0.82 | 1.47 | 0.540 |
| Personality/ Interpersonal Functioning | |||||
| Perceived Burdensomenessxi | −0.04 | 0.96 | 0.78 | 1.18 | 0.690 |
| ISEL- Belongingnessxii | −0.27 | 0.76 | 0.55 | 1.07 | 0.110 |
| Self-Esteemxiii | −0.08 | 0.92 | 0.71 | 1.20 | 0.550 |
| Appraisalxiv | −0.04 | 0.96 | 0.80 | 1.14 | 0.630 |
| Tangible Supportxv | −0.08 | 0.93 | 0.72 | 1.19 | 0.540 |
| NEO- Neuroticismxvi | 0.25 | 1.29 | 0.44 | 3.76 | 0.640 |
| Extroversionxvii | 0.30 | 1.35 | 0.24 | 7.66 | 0.740 |
| Conscientiousnessxviii | 0.33 | 1.39 | 0.53 | 3.64 | 0.500 |
| Impulsivity | |||||
| BIS- Non-planningxix | −0.44 | 0.64 | 0.43 | 0.96 | 0.030 |
| UPPS- Negative Urgencyxx | −0.13 | 0.87 | 0.41 | 1.86 | 0.730 |
| Positive Urgencyxxi | −0.25 | 0.78 | 0.44 | 1.38 | 0.400 |
| Lack of Premeditationxxii | 0.11 | 1.11 | 0.84 | 1.47 | 0.460 |
| 1b. Less lethal suicide events | |||||
| Socio-Demographic | |||||
| Sex (Male) | −0.55 | 0.58 | 0.31 | 1.09 | 0.088 |
| Income (Per Capita) | −0.16 | 0.85 | 0.66 | 1.11 | 0.240 |
| Physical Illness Burden | |||||
| Overalli | 0.08 | 1.09 | 0.81 | 1.45 | 0.580 |
| Highii | 0.12 | 1.13 | 0.99 | 1.30 | 0.077 |
| Severity of Psychiatric Illness | |||||
| Depression severityiii | 0.48 | 1.62 | 1.16 | 2.28 | 0.005 |
| Age of depression onset | −0.03 | 0.97 | 0.96 | 0.99 | 0.000 |
| Prior attemptiv | 2.44 | 11.45 | 4.12 | 31.81 | 0.000 |
| Ideation | |||||
| Currentv | 0.55 | 1.74 | 1.38 | 2.18 | 0.000 |
| Worst Lifetimevi | 1.06 | 2.90 | 1.99 | 4.21 | 0.000 |
| Substance use disorder- | |||||
| Currentvii | 1.08 | 2.93 | 1.46 | 5.87 | 0.002 |
| Lifetimevii | 0.67 | 1.96 | 1.07 | 3.57 | 0.029 |
| Cognition | |||||
| Verbal IQviii | 0.19 | 1.21 | 0.95 | 1.55 | 0.120 |
| Executive Functionix | −0.01 | 0.99 | 0.82 | 1.20 | 0.910 |
| Global Cognitive Functioningx | −0.02 | 0.98 | 0.82 | 1.17 | 0.820 |
| Personality/ Interpersonal Functioning | |||||
| Perceived Burdensomenessxi | 0.10 | 1.11 | 1.05 | 1.17 | 0.000 |
| ISEL- Belongingnessxii | 0.22 | 1.25 | 1.06 | 1.46 | 0.007 |
| Self-Esteemxiii | 0.21 | 1.23 | 1.02 | 1.48 | 0.030 |
| Appraisalxiv | 0.20 | 1.22 | 1.05 | 1.42 | 0.008 |
| Tangible Supportxv | 0.24 | 1.28 | 1.09 | 1.49 | 0.002 |
| NEO- Neuroticismxvi | 0.27 | 1.32 | 1.09 | 1.59 | 0.005 |
| Extraversionxvii | 0.64 | 1.90 | 1.24 | 2.92 | 0.003 |
| Conscientiousnessxviii | 0.21 | 1.23 | 1.00 | 1.52 | 0.052 |
| Impulsivity | |||||
| BIS- Non-planningxix | 0.24 | 1.27 | 1.01 | 1.60 | 0.043 |
| UPPS- Negative Urgencyxx | 0.39 | 1.48 | 1.23 | 1.78 | 0.000 |
| Positive Urgencyxxi | 0.17 | 1.18 | 1.03 | 1.36 | 0.017 |
| Lack of Premeditationxxii | 0.25 | 1.28 | 1.05 | 1.57 | 0.014 |
Cumulative Illness Rating Scale for Geriatrics-Overall illness burden
Cumulative Illness Rating Scale for Geriatrics-High physical illness burden [defined as scoring a “3” (severe/constant significant disability/“uncontrollable” chronic problems) or “4” (extremely severe/immediate treatment required/end organ failure/severe impairment in function) in at least one organ system]
Hamilton Rating Scale for depression
Suicide attempt at or before the time of study entry
Beck’s Scale for Suicidal Ideation Baseline
Beck’s Scale for Suicidal Ideation Worst point in life
Structured Clinical Interview for DSM-IV (SCID-IV)
Wechsler Test of Adult Reading-raw scores (lower scores indicative of more pathology)
Executive Interview
Mattis Dementia Rating Scale
Perceived Burdensomeness Questionnaire
Interpersonal Support Evaluation List (ISEL) Belongingness Subscale
Interpersonal Support Evaluation List (ISEL) Self Esteem Subscale
Interpersonal Support Evaluation List (ISEL) Appraisal Subscale
Interpersonal Support Evaluation List (ISEL) Tangible Support Subscale
NEO Five Factor Inventory Neuroticism subscale
NEO Five Factor Inventory Extraversion subscale (inverted)
xviii: NEO Five Factor Inventory Conscientiousness subscale (inverted)
Barratt Impulsivity Scale (BIS)-Non-planning subscale
Urgency, Premeditation, Perseverance, Sensation Seeking Impulsive Behavior Scale (UPPS) Negative Urgency Subscale
Urgency, Premeditation, Perseverance, Sensation Seeking Impulsive Behavior Scale (UPPS) Positive Urgency Subscale
Urgency, Premeditation, Perseverance, Sensation Seeking Impulsive Behavior Scale (UPPS) Lack of Premeditation Subscale
2.2. Assessment of longitudinal outcomes
There were 76 total deaths, including 9 by suicide. Cause of death was verified from death certificates, and categories appeared as suicide vs. natural/accidental death. The suicide category (N = 9) included cases which were highly suspected to be suicide deaths but categorized otherwise (N = 4: e.g., death certificate lists accidental overdose, however the same medications were used in a previous suicide attempt and family shared with us a suicide note that was not disclosed to the coroner). Time to death or to last confirmed alive date (for non-deceased participant), in months, was counted from baseline. Incident suicide attempts were ascertained during the 3-month and yearly in-person interviews and were also verified from medical records and by reaching out to treatment providers. Aborted attempts, defined as preparatory acts without actual behavior (e.g., gun taken out but trigger not pulled), and psychiatric hospitalizations to prevent suicide were also recorded.
Non-fatal suicide attempts with high medical severity were combined with the fatal suicide attempts into a single category of serious suicidal behavior. Medical seriousness of suicide attempts was assessed using the Beck Lethality Scale (BLS)(Beck et al., 1975). Similarly to other studies (Mann and Malone, 1997), attempts were classified as high lethality (BLS ≥4), if they could have resulted in death without medical intervention, while attempts with BLS <4 were classified as low-lethality. All the other attempts and psychiatric hospitalizations to prevent suicide were combined to the less lethal suicidal behavior category.
2.3. Assessment of predictors
Given our hypothesis that cognitive and dispositional characteristics map onto distinct putative pathways of suicidal behavior, we assessed five broad domains of risk factors: 1) sociodemographic variables, 2) history and severity of psychiatric illness (age of onset and severity of depression, comorbidity, history of suicidal ideation and behavior), 3) cognition, 4) impulsivity, 5) personality/interpersonal functioning. We considered separately, and added to the final model, the baseline treatment intensity score as measured by the Antidepressant Treatment History Form (Sackeim, 2001). Given the potential importance of somatic illness in late-life suicidal behavior (Fässberg et al., 2016), we also separately tested the predictive power of somatic illness for our two outcomes.
Sociodemographic characteristics included age, gender, race, marital status, and per capita household income.
Physical illness burden was assessed with the Cumulative Illness Rating Scale for Geriatrics (CIRS-G)(Linn et al., 1968). This scale provides a total score for overall physical illness, taking into account all physical conditions (e.g. hypertension well-controlled with first-line treatment) as well as their severity. We also separately evaluated the effects of severity; individuals were considered to have high physical illness burden if they scored a “3” (severe/constant significant disability/ “uncontrollable” chronic problems) or “4” (extremely severe/immediate treatment required/ end organ failure/severe impairment in function) in at least one organ system.
2.4. History and severity of psychiatric illness
We assessed severity of depressive illness and onset of first lifetime depressive episode using the SCID/DSM-IV and HRSD-17. We assessed comorbidity using current and lifetime SCID/DSM-IV diagnoses of anxiety and substance use disorders. We assessed lifetime history of suicide attempt. Suicidal ideation was assessed with the Beck’s Scale for Suicidal Ideation (SSI)(Beck et al., 1979) at two timepoints: baseline and at worst point in life.
2.5. Cognitive characterization
Premorbid IQ was assessed with the Wechsler Test of Adult Reading (WTAR)(Wechsler, 2001). Global cognitive ability was assessed with the Mattis Dementia Rating Scale (DRS)(Schmidt et al., 1994) total score. The DRS assesses Initiation/Perseveration, Attention, Construction, Conceptualization, and Memory. Cognitive control was assessed using the Executive Interview (EXIT)(Royall et al., 1992) where items include modifications of well-known “frontal lobe” tests (number/letter sequencing, Stroop, fluency tests, go/no-go tests, and Luria’s hand sequences). Eleven of the 25 EXIT items assess the ability to inhibit an automatic behavior or capture error detection or conflict monitoring.
2.6. Impulsivity
Different facets of impulsivity were measured with the Barratt Impulsiveness Scale (BIS)(Patton et al., 1995) and the UPPS Impulse Behavior Scale (Whiteside et al., 2005). High values on the BIS non-planning subscale indicate a tendency to act without regard for consequences and focus on more immediate outcomes. Mood-related impulsivity was assessed with the negative urgency (tendency to act when experiencing negative emotion) and positive urgency (excitability) subscales of the UPPS (Whiteside et al., 2005).
2.7. Personality/Interpersonal functioning
The NEO Five Factor Inventory (NEO-FFI) was used to assess the five personality dimensions: neuroticism, extraversion, openness to experience, conscientiousness and agreeableness (Costa and McCrae, 1992). Interpersonal problems were assessed with the Interpersonal Support Evaluation List (ISEL)(Cohen, 1985). The ISEL includes four measures of perceived availability of social resources, including Belonging, Appraisal, Self-Esteem, and Tangible Support (the availability of practical support; e.g., if needed, do you have somebody to take you to the hospital). We assessed feelings of burdensomeness with the Perceived Burdensomeness Questionnaire (Van Orden et al., 2010; Vanyukov et al., 2017).
2.8. Treatment resistance
We measured the intensity of pharmacotherapy for the baseline depressive episode (6-month period) with the Antidepressant Treatment History Form (ATHF). The ATHF score is based on antidepressant dose and trial duration, and also reflects the use of augmenting agents (Sackeim, 2001).
2.9. Statistical analysis
Statistical analysis was performed using R version 3.1.2.
Participants’ demographic and clinical characteristics were compared between depressed groups (attempters, ideators, non-suicidal depressed), using F statistics for continuous measures, Kruskal-Wallis tests for extremely skewed measures (such as income), and chi-square tests of independence or Fisher’s exact test, as appropriate, for categorical measures. Post-hoc pairwise group comparisons were performed, and significance levels adjusted for multiple comparisons using Tukey’s HSD for quantitative measures and Holm’s adjustment for categorical characteristics. A separate sample of healthy controls served as a reference group for summary statistics and the mortality outcome, and for standardizing of hazard ratios as described below, but this sample was not included in the group comparisons.
Missing data in the outcome measures were exclusively in the form of censored times to suicidal behavior or death and were analyzed using competing risk models. Competing risk models are survival analysis models that adjust the risk of the event of interest for the risk of secondary events, in this case death by other causes. These models are applied when the assumption of random censoring for the survival analysis models may be violated, as the same underlying factors may affect the risk of both kinds of events.
Missing data in the predictor variables was mostly due to the late introduction of certain scales during the study. For the first screening step, single predictor models were fit on the observed data separately for the two outcomes. For the second phase of the model, selection using multipredictor models, the predictors were imputed using multiple imputation as implemented in the mice library (Multiple Imputation by Chained Equations), based on the default method of predictive mean matching for quantitative data and logistic regression for binary data (van Buuren and Groothuis-Oudshoorn, 2011) to ensure that models were fit across domains using the same number of subjects. This commonly used method is based on Fully Conditional Specification, where each incomplete variable is imputed by a separate model, appropriate for its distribution, using all other variables in the input data. For predictors that have missing data themselves, the most recently generated imputations are used to complete the predictors prior to imputation of the target column. The default method for binary data (such as the anxiety or the substance use disorder diagnosis) is logistic regression, while the default method for continuous measures, such as the NEO personality factors, is predictive mean matching, a method that can impute even skewed data through sampling from the values of other subjects with similar values on other input measures. Only one imputed version was used for the multipredictor models presented. Three types of competing risk events were considered, out of which two were of primary interest: (1) fatal and near-fatal suicidal behavior and (2) less lethal suicide events. The third competing risk event was (3) natural death, which was of secondary interest, accounting for participants removed from the risk-pool before any type of suicidal behavior could be observed. When the study ended before suicidal behavior was observed, the subject’s time to suicidal behavior was considered to be censored, also called random censoring. The time to the first of the events for any subject was calculated and used as the time at risk. In case of those subjects who had both one or more less lethal event and a near-fatal or fatal attempt, the more lethal attempt’s timing was considered.
The following models were fit:
Comparison of the cumulative incidence of near-fatal and fatal suicidal behavior, less lethal suicide events, and natural death, among the recruitment groups (three depressed groups for attempt outcomes, all four groups for the natural death outcome) using competing risk survival analysis (Gray, 1988). This method calculates the so-called subdistribution estimates in a non-parametric way. For the risk for natural death, we also fit a competing risk model adjusted for age and baseline physical illness burden, using the proportional subdistribution hazards model of (Gray, 1988).
Screening Models in depressed patients were developed using single predictor competing risk regressions, using the proportional subdistribution hazards model, with cognitive, psychopathological, sociodemographic, and suicide history characteristics as independent variables. No imputed data was used for this step. For outcomes (1) and (2) hazard ratios with 95% CIs and significance levels were estimated.
Domain-specific multipredictor competing risk regressions were run as described above, for each outcome, and each of five domains separately (cognition, personality/interpersonal functioning, impulsivity, sociodemographic variables, and history and severity of psychiatric illness, selected based on literature (Galfalvy et al., 2006; Hawton et al., 2013), using predictors from Step 2’s screening models that were significant. These models were fit on the imputed dataset. To avoid confounding the effects, from predictors within a domain that were highly correlated (r >0.5, see correlation table in Supplement), only the most significant in the single-predictor model was included in the multipredictor model. Keeping in mind the limited number of subjects with negative event outcomes (15 for fatal and near-fatal, and 42 for the less lethal events), no more than 5 predictors were used in any model, and most had considerably fewer. Our rationale for variable selection by domains was that variables in the same domain often explain overlapping parts of the variability in the outcomes, and thus reduce the number of dimensions.
The across-domain prediction model for each outcome was fit using the significant variables from the domain-specific multipredictor models, with the above restriction as to the number of predictors included. If there were no significant variables in a domain-specific model, that domain was not represented in the final model for that outcome.
To the final model, we added the treatment intensity score, to test the adjusted effects of the treatment the subject received at the baseline time point, over and above that of the significant risk factors.
All tests were two-sided, and for hazard ratios, 95% CIs were calculated. For ease of comparison of hazard ratios, continuous predictors for depressed participants were scaled based on the mean/SD of the healthy controls. The exceptions to this were depression severity, where depressed participants’ scores were used as the benchmark; income, which was scaled for increments of $10,000; and predictors expressed as age (baseline age, age of onset of depression), which were not scaled. Prior to calculating hazard ratios when applicable, scales were recoded so higher hazard ratios indicated higher psychopathology (e.g., inverted extraversion indicated higher levels of introversion).
3. Results
Of the 401 older adult participants, 76 died during the study follow-up period (see Fig. 1. CONSORT diagram). All attempts and psychiatric hospitalizations occurred among the 311 depressed participants. Among the depressed participants, 50 died before any suicide attempt or event had been observed. For fatal and near-fatal attempts, there were 16 high-medical lethality attempts by 15 participants, including 9 suicides. A total of six baseline ideators and nine baseline attempters had high-lethality attempts or deaths by suicide during the study. Breaking this down, five of the baseline ideators and four of the baseline attempters died by suicide, with the remaining six events being near-fatal attempts. There were 42 additional participants with less lethal suicide events (22 had low-lethality attempts, and additionally 20 subjects had suicide-related hospitalizations or aborted attempts).
Fig. 1.

CONSORT diagram.
3.1. Differences in non-suicide mortality by baseline suicide history
The natural causes of death (N = 66) included cardiovascular/respiratory disease related (n = 47), cancer (n = 11), dementia (n = 9), other (including sepsis, multiorgan failure, diabetes mellitus; n = 12). Of note, for many individuals more than one cause of death was recorded. A single death by car accident was merged with natural death for analysis. First, we examined whether those who had a prior history of suicide attempt were more likely to die from natural causes. In a competing risk model across all four groups, there were significant differences in the risk of natural death (p = 0.029) between those with and without a history of suicide attempt at baseline. Post-hoc tests were not significant after adjustment for multiple testing (all adjusted p>0.05). However, among the depressed participants, in a competing risk regression model, with suicide as the competing risk, attempter status was a significant predictor of natural death (HR=1.91, 95%CI: 1.11–3.29, p = 0.019) after adjusting for age and high physical illness burden.
3.2. Model-building by predictor domain
Single predictor proportional subdistribution hazards (competing risk) models with sociodemographic, psychopathological, cognitive, and dispositional (impulsivity and personality/interpersonal functioning) characteristics as independent variables indicated a distinctive pattern of significant predictors (see Fig. 2) for near-lethal attempt and death by suicide, that were dominated by psychiatric illness severity and cognitive factors. By contrast, for less lethal suicide events, a range of dispositional predictors (personality/interpersonal dysfunction and impulsivity) influenced risk in addition to illness severity.
Fig. 2.
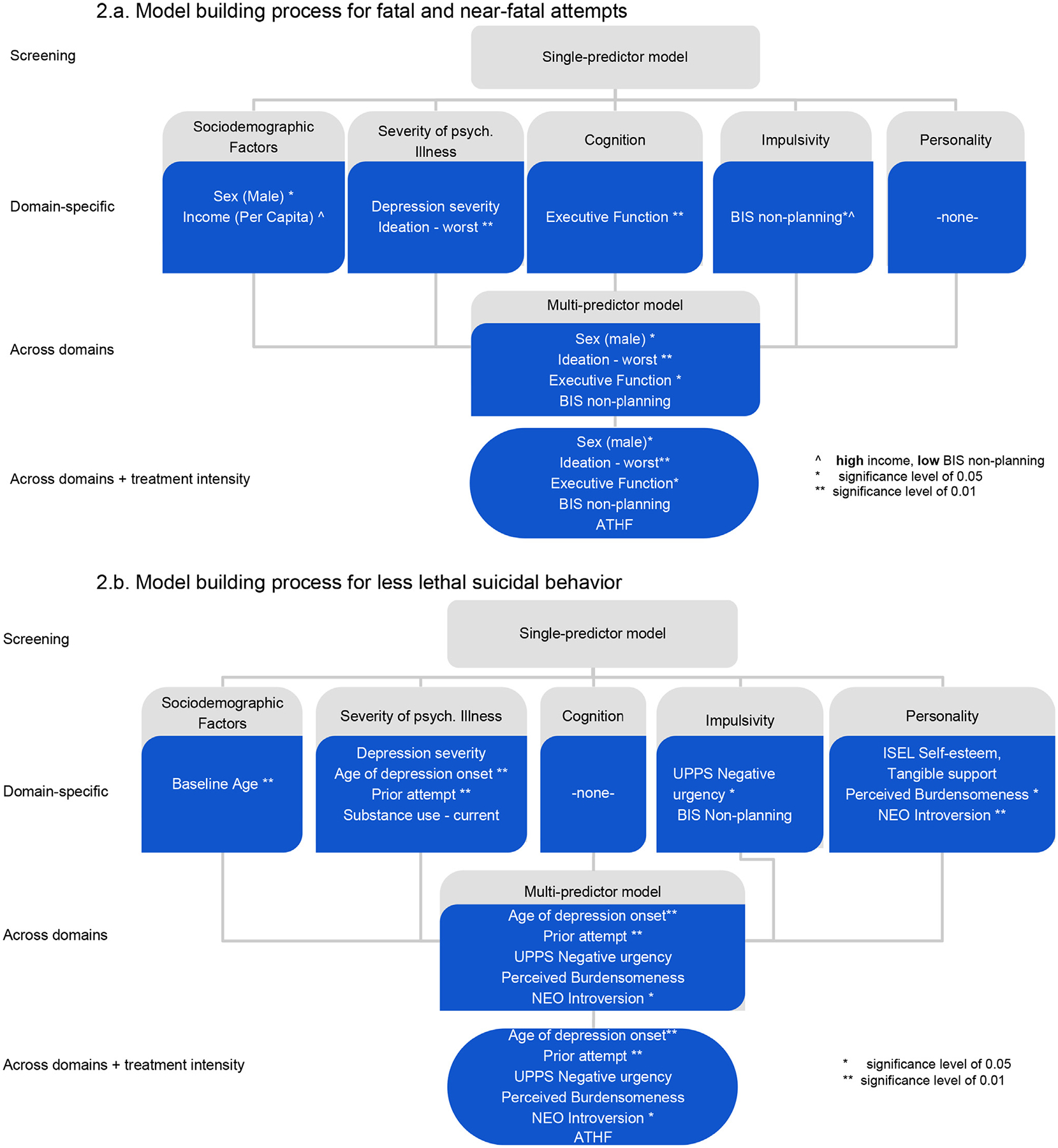
Model building process.
See model building steps in Fig. 2.
3.3. Predictors of fatal and near-fatal suicidal behavior
Male gender, higher income, current depression severity, current and worst lifetime suicidal ideation severity, cognitive control deficits, and low levels of non-planning impulsivity were identified as single predictors for fatal and near-fatal suicidal behavior (Table 1a). Multipredictor models identified male gender, severity of worst lifetime suicidal ideation and cognitive control deficits as independent predictors (Table 2a). Higher treatment intensity was not a significant predictor of fatal and near-fatal suicidal behavior in either the single-predictor model (HR=0..98, 95%CI: 0.67–1.45, p = 0.930) or the across-domain model (HR=0.99, 95%CI: 0.67–1.46, p = 0.950).
Table 2.
Multipredictor Models for Suicidal Behavior.
| 95% Confidence Interval | |||||
|---|---|---|---|---|---|
| B | Hazard Ratio | Lower Bound | Upper Bound | P Value | |
| 2a. Fatal and near-fatal attempts | |||||
| Sex (Male) | 1.52 | 4.59 | 1.36 | 15.51 | 0.0140 |
| Ideation - Worst Lifetimei | 0.70 | 2.02 | 1.30 | 3.15 | 0.0018 |
| Executive Functionii | 0.36 | 1.43 | 1.05 | 1.95 | 0.0230 |
| BIS- Non-planningiii | −0.21 | 0.81 | 0.60 | 1.08 | 0.1600 |
| 2b. Less lethal suicide-re ated events | |||||
| Age of depression onset | −0.02 | 0.98 | 0.97 | 0.99 | 0.0053 |
| Prior attemptiv | 2.25 | 9.45 | 3.27 | 27.36 | 0.0000 |
| Perceived Burdensomenessv | 0.03 | 1.03 | 0.98 | 1.09 | 0.2700 |
| UPPS- Negative Urgencyvi | 0.00 | 1.00 | 0.83 | 1.20 | 0.9800 |
| Extraversionvii | 0.34 | 1.41 | 1.07 | 1.85 | 0.0150 |
Beck’s Scale for Suicidal Ideation Worst point in life
Executive Interview
Barratt Impulsivity Scale (BIS)-Non-planning subscale
Suicide attempt at or before the time of study entry
Perceived Burdensomeness Questionnaire
Urgency, Premeditation, Perseverance, Sensation Seeking Impulsive Behavior Scale (UPPS) Negative Urgency Subscale
NEO Five Factor Inventory Extraversion subscale (inverted)
3.4. Predictors of lower lethality suicide-related events
Significant predictors of less lethal suicide events included maladaptive personality traits (introversion, neuroticism, low levels of self-esteem, perceived belonging, appraisal and tangible support, perceived burdensomeness), and impulsivity (UPPS negative and positive urgency, and BIS total and non-planning subscale scores). In addition, earlier age of depression onset, greater depression severity, current and worst lifetime ideation severity, younger baseline age, history of suicide attempt, and current and lifetime substance abuse were significant predictors in univariate models (Table 1b). In the multipredictor model, history of suicide attempt, introversion, and earlier age of onset of depression were significant risk factors (Table 2b). Higher treatment intensity did not reach the significance threshold of less lethal suicide events in the single-predictor model (HR=1.18, 95%CI: 0.97–1.43, p = 0.092), and when added to the across-domain model, it was no longer close to significant (HR=1.07, 95%CI: 0.84–1.35, p = 0.580).
Given the potential importance of somatic illness in late-life suicidal behavior, we separately tested the predictive power of somatic illness using two variables: overall somatic illness burden and number of severe somatic conditions, and found that it had no significant predictive power for fatal or near fatal suicide attempts (overall burden: HR=1.2, 95%CI: 0.80–1.79, p = 0.380, severe: HR=1.09, 95%CI: 0.94–1.26; p = 0.250). For less lethal suicide events, the risk associated with severe conditions was at a trend level (overall: HR=1.09, 95%CI: 0.81–1.45, p = 0.580, severe: HR=1.13, 95%CI: 0.99–1.30; p = 0.077).
4. Discussion
Confirming our hypothesis, we found that incident less lethal suicide events were predicted by interpersonal difficulties and impulsivity, while male gender, cognitive control deficits, and worst lifetime ideation predicted incident fatal and near-fatal suicidal behavior. Predictors of less lethal suicide events included earlier age of onset of depression and introversion, suggesting a lifelong predisposition.
Even though our study excluded participants diagnosed with dementia, we found that cognitive control deficits (previously called executive function), increased the risk of fatal and near-fatal suicide attempts. How do cognitive control deficits contribute to suicidal behavior? Cognitive control is the active maintenance of patterns of cortical activity that represent goals and the means to achieve them by way of bias signals that promote task-appropriate responding (Miller and Cohen, 2001). It is the ability to organize information in a way that helps achieve the best outcome (Burgess and Stuss, 2017). These abilities are critical for decision-making under uncertainty, which appears to be impaired in older suicide attempters (Dombrovski et al., 2019; Richard-Devantoy et al., 2013). This view agrees with early accounts of the suicidal crisis, emphasizing problem solving deficits (Pollock and Williams, 1998). This relationship is multi-faceted, as problem-solving deficits may influence one’s ability to avoid potentially controllable stressful life events, solve conflicts, and find alternative solutions to suicide (Williams et al., 2005). Executive dysfunction may increase the frequency of suicidal ideation and interfere with treatment progress, as it is associated with greater levels of disability (Alexopoulos et al., 2004) and poorer illness outcomes in late-life depression (Alexopoulos et al., 2005, 2004, 2000). However, showing promise, one study indicated that problem-solving therapy reduces suicidal ideation in depressed older adults with executive dysfunction (Gustavson et al., 2016).
These findings fit prior indications of a link between cognitive deficits and suicidal behavior (Gujral et al., 2016; McGirr et al., 2012; Richard-Devantoy et al., 2013). The present study indicates that preexisting (often latent), cognitive deficits and/or age-related cognitive decline, particularly in cognitive control (Cabeza et al., 2016; MacPherson et al., 2002; Raz et al., 2005) may contribute to medically serious suicidal behavior. We reported previously that among depressed older adults, there is a high suicide risk subgroup characterized by late-onset depression and a cognitive profile that corresponds most closely to that of incipient dementia (Szanto et al., 2018). Similarly, supporting the dementia prodrome theory, a nationwide Taiwanese study reported that attempted suicide in late-life predicted subsequent dementia (Tu et al., 2016).
Despite the accumulating evidence implicating cognitive deficits in late-life suicidal behavior, this profile still does not seem to fit all older suicidal individuals. Some appear to follow a distinct pathway defined by dispositional risk factors. Univariate predictors of less lethal suicide events included indicators of interpersonal difficulty/personality dysfunction (for example, lack of feelings of belongingness, low-self-esteem, perceived burdensomeness, introversion, neuroticism), as well as certain facets of impulsivity (urgency, non-planning). However, in the multipredictor models, only prior history of suicide attempt, earlier age of onset of depression, and higher introversion remained as independent risk factors. Previous studies suggested lower levels of extraversion in older suicide victims (Tsoh et al., 2005) and in older male attempters (Duberstein et al., 2000) as well as younger attempters (Seidlitz et al., 2001; Useda et al., 2004; for a review, see Szücs et al., 2020). This is not unexpected, as high extraversion is linked with the ability to build/maintain relationships and potentially to mobilize social support in a crisis. Individuals with dispositional risk factors naturally resemble younger suicide attempters, many of whom display early-onset, repeated attempts, often with chronically high levels of suicidal ideation. Future studies will need to test whether a personality profile characterized by limited or conflictual social interactions may interact with common life events, such as physical illness, contributing to suicide risk in older age.
In contrast, there may be different dispositional factors that contribute to fatal and near-fatal suicidal behavior. In the present study, attempters at risk for fatal and near-fatal suicidal behavior were also found to have low levels of non-planning impulsivity. A somewhat unexpected finding in the present study is that higher income predicted fatal and near-fatal suicidal behavior. While indicators of poverty are more typically associated with suicide risk, this may not be the case for all older adults. Studies from Kjølseth et al. (2009), and our own findings (Szücs et al., 2020), suggest that older adults who die by suicide or have late-onset (mostly high-medical lethality) suicide attempts are often high-functioning throughout most of their life, and characterized as controlling, rigid, high-achievers, also high on orderliness (a conscientiousness subcomponent). It may be the case that traits that are generally adaptive and facilitate higher socioeconomic status earlier in life may be maladaptive and convey suicide risk in old age.
While it is well-known that life expectancy is reduced in those with mental illness (Chesney et al., 2014), less is known about the relationship between suicidal behavior and risk of death from natural causes (Wiktorsson et al., 2011). A study by Wiktorsson and colleagues followed 100 suicide attempters (aged 70+) over a year. While the attrition rate was too high to prospectively assess risk factors for repeated suicidal behavior, authors did observe increased mortality due to natural causes in older suicide attempters compared to community living controls (Wiktorsson et al., 2011). Similarly, the present study prospectively corroborated that suicide attempters are at risk of an earlier death than healthy controls, be it by suicide or natural causes. It may be the case that neurocognitive deficits and personality factors linked to suicidal behavior influence health behaviors and problem-solving abilities, in turn leading to premature mortality by causes other than suicide as well. Multiple physical diseases have been associated with increased risk for suicide in older adults (Fassberg et al., 2012; Juurlink et al., 2004). Our more nuanced analyses found that severe physical conditions were risk factors for less lethal suicide events at a trend level. Overall physical illness burden, including conditions well-controlled by first-line treatment, may not be a major contributor to suicidal behavior. This is in line with the report that chronic conditions alone were not predictive of death by suicide when functional limitations were not considered (Kaplan et al., 2007).
We failed to find a significant association between incident suicidal behavior and intensity of antidepressant treatment. Higher treatment intensity, which includes the use of augmenting agents (e.g., antipsychotics and lithium) showed a trend towards being a risk factor for less lethal suicide events in the single-predictor model.
During the course of the present study (average follow-up 5.4 years), among the 311 depressed participants, about 12% had suicide attempts. While this rate may appear lower than previously reported (De Leo et al., 2001), it only includes suicide attempts or death by suicide. We also assessed broadly defined suicide events, which additionally included aborted attempts and suicide-related emergency hospitalizations. Over the course of the study, there were 96 emergency psychiatric hospitalizations by 53 participants (17% total), 77 of which were suicide-related (prompted by suicidal ideation or behavior). Twenty participants (6%) with a total of 31 suicide-related emergency hospitalizations ultimately did not have follow-up suicidal behavior. Thus, study involvement itself may have prevented suicidal behavior on occasions when participants were deemed to be at high risk, and study clinicians facilitated referral.
4.1. Limitations
Despite including over 300 high suicide risk older adults, the total number of participants with suicide events (n = 57) in the dataset limits the statistical power of our analyses. Given the limited number of events, our final multipredictor models were able to test no more than five predictors simultaneously. Although we assessed a wide range of potential predictors, we did not include indicators of Cluster B personality disorders, often associated with suicide attempts in younger age groups. As this study aimed to investigate the association of baseline predictors with incident suicidal behavior, omitting the trajectories/ change of predictors; for example, we cannot draw conclusions about changes in treatment during the course of the study. Further, as depression was an inclusion criterion, the study results can only generalize to older adults with depression. Additionally, in our analyses we adjusted for death by natural causes, which may have mitigated age effects.
4.2. Strengths
The present study adds to the literature by longitudinally ascertaining suicidal behavior in a sample enriched for suicide risk. A review of 19 studies of suicide risk factors in depressed individuals of all ages (Hawton et al., 2013) concluded that relatively few risk factors for suicide have been identified (also see Troya et al., 2019). This study provides detailed characterization of both cognitive and personality factors that were not measured in existing prospective studies. Further, both the in-depth characterization of the suicidal behavior itself, and its resultant subdivision constitute strengths of the study.
4.3. Implications for practice and future research
Our study investigated cognitive impairment (which is highly prevalent in late-life depression) as a component of the suicidal diathesis, and demonstrated the predictive utility of cognitive factors in identifying the risk of future near-fatal attempt and death by suicide. Given the rarity of medically serious suicidal behavior, and suicide attempts in general, many studies use broadly-defined suicide events as outcomes. While this approach helps to identify risk factors for ideation and behavior, it fails to isolate features exclusively related to fatal- and near-fatal suicidal behavior.
Understanding the risk factors that define distinct pathways to suicide, particularly the interactions between cognitive deficits and other risk factors, may help to identify those most at-risk for suicide and develop individualized treatment strategies. Models indicated a distinctive pattern of significant predictors for near-lethal attempt and death by suicide, dominated by cognitive and sociodemographic factors. These risk factors differed from those for less lethal suicide events, which were dominated by a range of dispositional predictors in addition to the well-established indicators (presence and severity of psychiatric illness). The present findings support the notion that clinicians cannot simply think of risk factors as simply additive and should consider the existence of distinct pathways to late-life suicidal behavior.
Supplementary Material
Acknowledgements
The authors would like to acknowledge Morgan Buerke BS, Michelle Perry BA, and Kexin Chen MS for their assistance in data collection and preparation of the manuscript.
Role of funding source
Funding for this study was provided by NIMH R01 MH085651-05, NIMH R01 MH085651-11, and NIMH R01 MH100095-01A1. The NIMH had no further role in study design, in the collection, analysis and interpretation of data, in the writing of the report, or in the decision to submit the paper for publication.
Footnotes
Declaration of Competing Interest
None.
Supplementary materials
Supplementary material associated with this article can be found, in the online version, at doi: 10.1016/j.euroneuro.2020.06.005.
References
- Alexopoulos G, Kiosses DN, Heo M, Murphy CF, Shanmugham B, Gunning-Dixon F, 2005. Executive dysfunction and course of geriatric depression. Biol. Psychiatry 58, 204–210. [DOI] [PubMed] [Google Scholar]
- Alexopoulos G, Kiosses DN, Murphy C, Heo M, 2004. Executive dysfunction, heart disease burden, and remission of geriatric depression. Neuropsycholopharmacology 29, 2278–2284. [DOI] [PubMed] [Google Scholar]
- Alexopoulos GS, Meyers BS, Young RC, Balu K, Kakuma T, Sirey JA, Hull J, 2000. Executive dysfunction and long-term outcomes of geriatric depression. Arch. Gen. Psychiatry 57, 285–290. 10.1001/archpsyc.57.3.285. [DOI] [PubMed] [Google Scholar]
- Beck AT, Beck R, Kovacs M, 1975. Classification of suicidal behaviors: I. Quantifying intent and medical lethality. Am. J. Psychiatry 132, 285–287. [DOI] [PubMed] [Google Scholar]
- Beck AT, Kovacs M, Weissman A, 1979. Assessment of suicidal intention: the scale for suicide ideation. J. Consult. Clin. Psychol 47, 343–352. [DOI] [PubMed] [Google Scholar]
- Brent DA, Emslie GJ, Clarke GN, Asarnow J, Spirito A, Ritz L, Vitiello B, Iyengar S, Birmaher B, Ryan ND, 2009. Predictors of spontaneous and systematically assessed suicidal adverse events in the treatment of SSRI-resistant depression in adolescents (TORDIA) study. Am. J. Psychiatry 166, 418–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgess PW, Stuss DT, 2017. Fifty years of prefrontal cortex research: impact on assessment. J. Int. Neuropsychol. Soc 23, 755–767. [DOI] [PubMed] [Google Scholar]
- Cabeza R, Nyberg L, Park DC, 2016. Cognitive Neuroscience of Aging: Linking Cognitive and Cerebral Aging Oxford University Press. [Google Scholar]
- Chesney E, Goodwin GM, Fazel S, 2014. Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry 13, 153–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Mermelstein R, et al. , 1985. Measuring the functional components of social support In: Sarason IG, Sarason B (Eds.), Social support: Theory, Research and Applications The Hague, Martinus, Nijhoff, pp. 73–94. [Google Scholar]
- Conwell Y, Duberstein PR, Cox C, Herrmann J, Forbes N, Caine ED, 1998. Age differences in behaviors leading to completed suicide. Am. J. Geriatr. Psychiatry 6, 122–126. [PubMed] [Google Scholar]
- Costa PT, McCrae RR, 1992. Revised NEO personality inventory (NEO PI-R) and NEO five-factor inventory (NEO-FFI). Psychol. Assess. Resour [Google Scholar]
- De Leo D, Padoani W, Scocco P, Billebrahe U, Arensman E, Hjelmeland H, Crepet P, Haring P, Hawton K, Lonnqvist J, Michel K, Pommereau X, Querejeta I, Phillipe J, Salander-Renberg E, Schmidtke A, Fricke S, Weinacker B, Tamesvary B, Wasserman D, Faria S, 2001. Attempted and completed suicide in older subjects: results form the WHO/EURO multicentre study of suicidal behavior. Int. J. Geriatr. Psychiatry 16, 300–310. [DOI] [PubMed] [Google Scholar]
- Dombrovski AY, Hallquist MN, Brown VM, Wilson J, Szanto K, 2019. Value-based choice, contingency learning, and suicidal behavior in mid- and late-life depression. biological psychiatry. Revisit. Neural Circ. Depress 85, 506–516. 10.1016/j.biopsych.2018.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dombrovski AY, Siegle GJ, Szanto K, Clark L, Reynolds CF, Aizenstein H, 2012. The temptation of suicide: striatal gray matter, discounting of delayed rewards, and suicide attempts in late-life depression. Psychol. Med 42, 1203–1215. 10.1017/S0033291711002133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dombrovski AY, Szanto K, Duberstein P, Conner KR, Houck PR, Conwell Y, 2008. Sex differences in correlates of suicide attempt lethality in late life. Am. J. Geriatr. Psychiatry 16, 905–913. 10.1097/JGP.0b013e3181860034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dombrovski AY, Szanto K, Siegle GJ, Wallace ML, Forman SD, Sahakian B, Reynolds CF 3rd, Clark L, 2011. Lethal forethought: delayed reward discounting differentiates high- and low-lethality suicide attempts in old age. Biol. Psychiatry 70, 138–144. 10.1016/j.biopsych.2010.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duberstein PR, Conwell Y, Seidlitz L, Denning DG, Cox C, Caine ED, 2000. Personality traits and suicidal behavior and ideation in depressed inpatients 50 years of age and older. J. Gerontol. Ser. B 55, P18–P26. [DOI] [PubMed] [Google Scholar]
- Erlangsen A, Zarit SH, Conwell Y, 2008. Hospital-diagnosed dementia and suicide: a longitudinal study using prospective, nationwide register data. Am. J. Geriatr. Psychiatry 16, 220–228. 10.1097/JGP.0b013e3181602a12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fässberg MM, Cheung G, Canetto SS, Erlangsen A, Lapierre S, Lindner R, Draper B, Gallo JJ, Wong C, Wu J, 2016. A systematic review of physical illness, functional disability, and suicidal behaviour among older adults. Aging Ment. Health 20, 166–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fassberg MM, Van Orden K, Duberstein P, Erlangsen A, Lapierre S, E B, Canetto SS, De Leo D, Szanto K, Waern M, 2012. A systematic review of social factors and suicidal behavior in older adulthood. J. Environ. Res. Public Health 9, 722–745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR, 1975. Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr Res 12, 189–198. [DOI] [PubMed] [Google Scholar]
- Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Huang X, Musacchio KM, Jaroszewski AC, Chang BP, Nock MK, 2017. Risk factors for suicidal thoughts and behaviors: a meta-analysis of 50 years of research. Psychol. Bull 143, 187. [DOI] [PubMed] [Google Scholar]
- Friedmann H, Kohn R, 2008. Mortality, or probability of death, from a suicidal act in the United States. Suicide Life Threat. Behav 38, 287–301. 10.1521/suli.2008.38.3.287. [DOI] [PubMed] [Google Scholar]
- Galfalvy H, Oquendo MA, Carballo JJ, Sher L, Grunebaum MF, Burke A, Mann JJ, 2006. Clinical predictors of suicidal acts after major depression in bipolar disorder: a prospective study. Bipolar Disord 8, 586–595. 10.1111/j.1399-5618.2006.00340.x. [DOI] [PubMed] [Google Scholar]
- Gray RJ, 1988. A class of K-sample tests for comparing the cumulative incidence of a competing risk. Ann. Stat 1141–1154. [Google Scholar]
- Gujral S, Ogbagaber S, Dombrovski AY, Butters MA, Karp JF, Szanto K, 2016. Course of cognitive impairment following attempted suicide in older adults. Int. J. Geriatr. Psychi- atry 31, 592–600. 10.1002/gps.4365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustavson KA, Alexopoulos GS, Niu GC, McCulloch C, Meade T, Areán PA, 2016. Problem-solving therapy reduces suicidal ideation in depressed older adults with executive dysfunction. Am. J. Geriatr. Psychiatry 24, 11–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton M, 1960. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry 23, 56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawton K, i Comabella CC, Haw C, Saunders K, 2013. Risk factors for suicide in individuals with depression: a systematic review. J. Affect. Disord 147, 17–28. [DOI] [PubMed] [Google Scholar]
- Isacsson G, Boëthius G, Bergman U, 1992. Low level of antidepressant prescription for people who later commit suicide: 15 years of experience from a population-based drug database in Sweden. Acta Psychiatr. Scand 85, 444–448. 10.1111/j.1600-0447.1992.tb03209.x. [DOI] [PubMed] [Google Scholar]
- Jick SS, Dean AD, Jick H, 1995. Antidepressants and suicide. BMJ 310, 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joiner TE, Pettit JW, Walker RL, Voelz ZR, Cruz J, Rudd DM, Lester D, 2002. Perceived burdensomeness and suicidality: two studies on the suicide notes of those attempting and those completing suicide. J. Soc. Clin. Psychol 21, 531–545. [Google Scholar]
- Juurlink DN, Herrmann N, Szalai JP, Kopp A, Redelmeier DA, 2004. Medical illness and the risk of suicide in the elderly. Arch. Intern. Med 164, 1179–1184. [DOI] [PubMed] [Google Scholar]
- Kaplan MS, McFarland B, Huguet N, Newsom JT, 2007. Physical illness, functional limitations, and suicide risk: a population-based study. Am. J. Orthopsychiatry 77, 56–60. 10.1037/0002-9432.77.1.56. [DOI] [PubMed] [Google Scholar]
- Keilp JG, Sackeim HA, Brodsky BS, Oquendo MA, Malone KM, Mann JJ, 2001. Neuropsychological dysfunction in depressed suicide attempters. Am. J. Psychiatry 158, 735–741. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Stein MB, Petukhova MV, Bliese P, Bossarte RM, Bromet EJ, Fullerton CS, Gilman SE, Ivany C, Lewandowski-Romps L, Bell AM, Naifeh JA, Nock MK, Reis BY, Rosellini AJ, Sampson NA, Zaslavsky AM, Ursano RJ, Collaborators AS, Ursano RJ, Stein MB, Heeringa S, Kessler RC, Colpe LJ, Schoen-baum M, Cersovsky S, Cox K, Aliaga PA, Benedek DM, Borja S, Brown GG, Sills LC, Dempsey CL, Frank R, Fullerton CS, Gebler N, Gifford RK, Gilman SE, Holloway MG, Hurwitz PE, Jain S, Kao T-C, Koenen KC, Romps LL, Mash HH, McCarroll JE, McLaughlin KA, Naifeh JA, Nock MK, Raman R, Rose S, Rosellini AJ, Sampson NA, Santiago LP, Scanlon M, Smoller J, Thomas ML, Vegella PL, Wassel C, Zaslavsky AM, Mann J, Oquendo M, Stanley B, Posner K, Keilp J, 2017. Predicting suicides after outpatient mental health visits in the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). Mol. Psychiatry 22, 544–551. 10.1038/mp.2016.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Warner CH, Ivany C, Petukhova MV, Rose S, Bromet EJ, Brown M, Cai T, Colpe LJ, Cox KL, 2015. Predicting suicides after psychiatric hospitalization in US Army soldiers: the Army Study to assess risk and resilience in service-members (Army STARRS). JAMA Psychiatry 72, 49–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kjølseth I, Ekeberg Ø, Steihaug S, 2009. “Why do they become vulnerable when faced with the challenges of old age?” Elderly people who committed suicide, described by those who knew them. Int. Psychogeriatr 21, 903–912. [DOI] [PubMed] [Google Scholar]
- Klonsky ED, Qiu T, Saffer BY, 2017. Recent advances in differentiating suicide attempters from suicide ideators. Curr. Opin. Psychiatry 30, 15–20. [DOI] [PubMed] [Google Scholar]
- Linn BS, Linn MW, Gurel L, 1968. Cumulative illness rating scale. J. Am. Geriatr. Soc 16, 622–626. [DOI] [PubMed] [Google Scholar]
- MacPherson SE, Phillips LH, Della Sala S, 2002. Age, executive function and social decision making: a dorsolateral prefrontal theory of cognitive aging. Psychol. Aging 17, 598–609. 10.1037/0882-7974.17.4.598. [DOI] [PubMed] [Google Scholar]
- Mann JJ, Malone KM, 1997. Cerebrospinal fluid amines and higher-lethality suicide attempts in depressed inpatients. Biol. Psychiatry 41, 162–171. [DOI] [PubMed] [Google Scholar]
- May AM, Klonsky ED, 2016. What distinguishes suicide attempters from suicide ideators? A meta-analysis of potential factors. Clin. Psychol. Sci. Pract 23, 5–20. 10.1111/cpsp.12136. [DOI] [Google Scholar]
- McGirr A, Dombrovski AY, Butters M, Clark L, Szanto K, 2012. Deterministic learning and attempted suicide among older depressed individuals: cognitive assessment using the Wisconsin Card Sorting Task. J. Psychiatr Res 46, 226–232. 10.1016/j.jpsychires.2011.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGirr A, Renaud J, Bureau A, Seguin M, Lesage A, Turecki G, 2008. Impulsive-aggressive behaviours and completed suicide across the life cycle: a predisposition for younger age of suicide. Psychol. Med 38, 407–417. 10.1017/S0033291707001419. [DOI] [PubMed] [Google Scholar]
- Melhem NM, Porta G, Oquendo MA, Zelazny J, Keilp JG, Iyengar S, Burke A, Birmaher B, Stanley B, Mann JJ, 2019. Severity and variability of depression symptoms predicting suicide attempt in high-risk individuals. JAMA Psychiatry [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller EK, Cohen JD, 2001. An integrative theory of prefrontal cortex function. Annu. Rev. Neurosci 24, 167–202. 10.1146/annurev.neuro.24.1.167. [DOI] [PubMed] [Google Scholar]
- Murphy E, Kapur N, Webb R, Purandare N, Hawton K, Bergen H, Waters K, Cooper J, 2012. Risk factors for repetition and suicide following self-harm in older adults: multicentre cohort study. Br. J. Psychiatry 200, 399–404. [DOI] [PubMed] [Google Scholar]
- O’Carroll PW, Berman AL, Maris RW, Moscicki EK, Tanney BL, Silverman MM, 1996. Beyond the tower of Babel: a nomenclature for suicidology. Suicide Life Threat. Behav 26, 237–252. [PubMed] [Google Scholar]
- Oquendo MA, Bongiovi-Garcia ME, Galfalvy H, Goldberg PH, Grunebaum MF, Burke AK, Mann JJ, 2007. Sex differences in clinical predictors of suicidal acts after major depression: a prospective study. Am. J. Psychiatry 164, 134–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oquendo MA, Galfalvy H, Russo S, Ellis SP, Grunebaum MF, Burke A, Mann JJ, 2004. Prospective study of clinical predictors of suicidal acts after a major depressive episode in patients with major depressive disorder or bipolar disorder. Am. J. Psychiatry 161, 1433–1441. [DOI] [PubMed] [Google Scholar]
- Patton JH, Stanford MS, Barratt ES, 1995. Factor structure of the Barratt impulsiveness scale. J. Clin. Psychol 51, 768–774. [DOI] [PubMed] [Google Scholar]
- Pearson JL, Brown GK, 2000. Suicide prevention in late life: directions for science and practice. Clin. Psychol. Rev 20, 685–705. [DOI] [PubMed] [Google Scholar]
- Pollock LR, Williams JM, 1998. Problem solving and suicidal behavior. Suicide Life Threat. Behav 28, 375–387. [PubMed] [Google Scholar]
- Raz N, Lindenberger U, Rodrigue KM, Kennedy KM, Head D, Williamson A, Dahle C, Gerstorf D, Acker JD, 2005. Regional brain changes in aging healthy adults: general trends, individual differences and modifiers. Cereb. Cortex 15, 1676–1689. 10.1093/cercor/bhi044. [DOI] [PubMed] [Google Scholar]
- Richard-Devantoy S, Berlim M, Jollant F, 2013. A meta-analysis of neuropsychological markers of vulnerability to suicidal behavior in mood disorders. Psychol. Med 1–11. [DOI] [PubMed] [Google Scholar]
- Richard-Devantoy S, Szanto K, Butters MA, Kalkus J, Dom- brovski AY, 2015. Cognitive inhibition in older high-lethality suicide attempters. Int. J. Geriatr. Psychiatry 30, 274–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Royall DR, Mahurin RK, Gray KF, 1992. Bedside assessment of executive cognitive impairment: the executive interview. J . Am. Geriatr. Soc 40, 1221–1226. [DOI] [PubMed] [Google Scholar]
- Sackeim HA, 2001. The definition and meaning of treatment-resistant depression. J. Clin. Psychiatry 16 (62 Supplement), 10–17. [PubMed] [Google Scholar]
- Schmidt R, Freidl W, Fazekas F, Reinhart B, Grieshofer P, Koch M, Eber B, Schumacher M, Polmin K, Lechner H, 1994. The Mattis Dementia Rating Scale: normative data from 1 001 healthy volunteers. Neurology 44, 964–966. [DOI] [PubMed] [Google Scholar]
- Seidlitz L, Conwell Y, Duberstein P, Cox C, Denning D, 2001. Emotion traits in older suicide attempters and non-attempters. J. Affect. Disord 66, 123–131. [DOI] [PubMed] [Google Scholar]
- Szanto K, Clark L, Hallquist M, Vanyukov P, Crockett M, Dombrovski AY, 2014. The cost of social punishment and high-lethality suicide attempts in the second half of life. Psychol. Aging 29, 84–94. 10.1037/a0035339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szanto K, de Bruin WB, Parker AM, Hallquist MN, Vanyukov PM, Dombrovski AY, 2015. Decision-making competence and attempted suicide. J. Clin. Psychiatry 76, 1590–1597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szanto K, Galfalvy H, Vanyukov PM, Keilp JG, Dombrovski AY, 2018. Pathways to late-life suicidal behavior: c luster analysis and predictive validation of suicidal behavior in a sample of older adults with major depression. J. Clin. Psychiatry 79 10.4088/JCP.17m11611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szanto K, Mulsant BH, Houck P, Dew MA, Reynolds CF, 2003. Occurrence and course of suicidality during short-term treatment of late-life depression. Arch. Gen. Psychiatry 60, 610–617. [DOI] [PubMed] [Google Scholar]
- Szanto K, Mulsant BH, Houck PR, Miller MD, Mazumdar S, Reynolds CF, 2001. Treatment outcome in suicidal vs. non-suicidal elderly patients. Am. J. Geriatr. Psychiatry 9, 261–268. [PubMed] [Google Scholar]
- Szücs A, Szanto K, Wright AG, Dombrovski AY, 2020. Personality of late-and early-onset elderly suicide attempters. Int. J. Geriatr. Psychiatry 35, 384–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szücs A, Szanto K, Wright AG, Dombrovski AY, 2020. Personality of late-and early-onset elderly suicide attempters. Int. J. Geriatr. Psychiatry 35, 384–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troya MI, Babatunde O, Polidano K, Bartlam B, Mc-Closkey E, Dikomitis L, Chew-Graham CA, 2019. Self-harm in older adults: systematic review. Br. J. Psychiatry 214, 186–200. [DOI] [PubMed] [Google Scholar]
- Tsoh J, Chiu HF, Duberstein PR, Chan SS, Chi I, Yip PS, Conwell Y, 2005. Attempted suicide in elderly Chinese persons: a multi-group, controlled study. Am. J. Geriatr. Psychiatry 13, 562–571. 10.1176/appi.ajgp.13.7.562. [DOI] [PubMed] [Google Scholar]
- Tu Y-A, Chen M-H, Tsai C-F, Su T-P, Bai Y-M, Li C-T, Lin W-C, Liu M-E, Pan T-L, Chen T-J, 2016. Geriatric suicide attempt and risk of subsequent dementia: a nationwide longitudinal follow-up study in Taiwan. Am. J. Geriatr. Psychiatry 24, 1211–1218. [DOI] [PubMed] [Google Scholar]
- Useda JD, Duberstein PR, Conner KR, Conwell Y, 2004. Personality and attempted suicide in depressed adults 50 years of age and older: a facet level analysis. Compr. Psychiatry 45, 353–361. [DOI] [PubMed] [Google Scholar]
- van Buuren S, Groothuis-Oudshoorn K, 2011. mice: multivariate imputation by chained equations in R. J. Stat. Softw 45, 1–67. [Google Scholar]
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE Jr., 2010. The interpersonal theory of suicide. Psychol. Rev 117, 575–600. 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanyukov PM, Szanto K, Hallquist M, Moitra M, Dombrovski AY, 2017. Perceived burdensomeness is associated with low-lethality suicide attempts, dysfunctional interpersonal style, and younger rather than older age. Int. J. Geriatr. Psychiatry 32, 788–797. 10.1002/gps.4526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanyukov PM, Szanto K, Hallquist MN, Siegle GJ, Reynolds CF, Forman SD, Aizenstein HJ, Dombrovski AY, 2016. Paralimbic and lateral prefrontal encoding of reward value during intertemporal choice in attempted suicide. Psychol. Med 46, 381–391. 10.1017/S0033291715001890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D, 2001. Wechsler Test of Adult Reading The Psychological Corporation; San Antonio, Texas. [Google Scholar]
- Whiteside SP, Lynam DR, Miller JD, Reynolds SK, 2005. Validation of the UPPS impulsive behaviour scale: a four-factor model of impulsivity. Eur. J. Pers 19, 559–574. [Google Scholar]
- Wiktorsson S, Marlow T, Runeson B, Skoog I, Waern M, 2011. Prospective cohort study of suicide attempters aged 70 and above: one-year outcomes. J. Affect. Disord 134, 333–340. [DOI] [PubMed] [Google Scholar]
- Williams JM, Barnhofer T, Crane C, Beck AT, 2005. Problem solving deteriorates following mood challenge in formerly depressed patients with a history of suicidal ideation. J. Abnorm. Psychol 114, 421–431. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


