Abstract
Background and Objectives
Children and youth in immigrant families (CIF)—children and youth with at least one foreign-born parent—face unique psychosocial stressors. Yet little is known about access to mental/behavioral health (MBH) services for CIF. Among US CIF and non-CIF with MBH problems, we assessed access to MBH treatment.
Methods
We used the National Survey of Children’s Health-2016, a nationally-representative survey of predominantly English- or Spanish-speaking US parents. The sample included 2–17 year-aids whose parent reported at least one MBH problem. The primary outcome was prior-year receipt of MBH treatment (counseling, medication, or both).
Results
Of 50,212 survey respondents, 7,164 reported a current MBH problem (809 CIF and 6,355 non-CIF). The majority of CIF were Hispanic/Latinx (56% CIF vs 13% non-CIF, p<0.001). CIF were less likely than non-CIF to have an ADHD diagnosis (35% vs 59%, p<0.001) and less likely to have received MBH medication and/or counseling (61% vs 71%, p = 0.02). This difference was pronounced for receiving medication (32% vs 50%, p<0.001). When controlling for multiple covariates, differences in any MBH treatment were no longer statistically significant (AOR 0.76, 95% CI 0.52–1.11), while the odds of receipt of medication remained significantly lower for CIF (AOR 0.61, 95% CI 0.42 – 0.88).
Conclusions
Among children and youth with at least one parent-reported MBH problem, CIF, compared with non-CIF, were less likely to receive MBH treatment, specifically medication. This may be explained, in part, by differences in the proportion of CIF and non-CIF diagnosed with ADHD.
Keywords: Mental and Behavioral Health, Treatment Access, Children and Youth in Immigrant Families, National Survey of Children’s Health
Introduction
One in six US children and youth aged 6–17 years have at least one mental and behavioral health (MBH) diagnosis.1 While the majority of MBH conditions present in youth under 25 years of age,2 childhood MBH problems have both short-term and long-term sequelae that can persist into adulthood. Nine MBH conditions are responsible for 50% of disability-adjusted-life-years, a measure of years lost to death or disability.3 Thus, to reduce severity and to prevent known sequelae, pediatric providers should implement evidence-based, effective treatments, such as combined pharmacotherapy and psychotherapy for depression.2 Yet, depending on geographic location, approximately 30–70% of children and youth with MBH diagnoses do not receive treatment.1
Access to treatment may be particularly problematic for children and youth in immigrant families (CIF), US- or foreign-born children and youth with at least one foreign-born parent, who comprise 25% of the US child population. Notable barriers to MBH care for CIF include lack of accommodation for language barriers (56% of CIF have at least one parent with limited English proficiency), lower rates of diagnostic screening, a paucity of culturally or linguistic-concordant providers, stigma, provider racial/ethnic biases, and distrust of providers.4–12 Recent studies of children with Autism Spectrum Disorder (ASD) exemplify these barriers. In qualitative interviews, Hispanic/Latinx immigrant parents report lack of empowerment, language barriers, stigma, and a delayed process of diagnosis as reasons for delays In ASD care.7
Concurrently, many CIF are at higher risk for multiple stressors associated with suboptimal mental health. For example, immigration-related policy has had measurable effects on CIF mental health; when it was enacted, the Deferred Action for Childhood Arrival (DACA) program was associated with improvement in reported psychological distress for CIF who were DACA-eligible compared with those who were ineligible,13 although self-reported health of DACA-eligible CIF worsened amid later political uncertainties.14 Hispanic/Latinx adolescents whose family members were detained and/or deported were found to have higher a prevalence of suicidal ideation, alcohol use, externalizing behaviors, PTSD symptoms, and psychologic distress.15,16 Other risks for suboptimal mental health that CIF face include lack of health insurance or underinsurance,17 adverse childhood experiences including racism and exposure to violence18 acculturative stress, low income or socioeconomic status.13 unaccompanied status or family separation, and stress associated with migration status.19,20 With the known sequelae of MBH problems and demonstrated benefits of treatment, quantitative data on relative access to MBH services for CIF compared with non-CIF are necessary to inform health system prioritization and MBH resource allocation. Previous studies of Hispanic/Latinx children referred to child welfare have found that children of undocumented parents are less likely to have access needed MBH care,21 but there is a paucity of data assessing CIF compared with non-CIF more broadly. To address this gap, we use a nationally-representative sample to examine receipt of MBH treatment for CIF and non-CIF with parent-reported MBH problems.
Methods
Data Source
This study used the National Survey of Children’s Health 2016 (NSCH-16), a cross-sectional, nationally-representative survey of caretakers of noninstitutionalized US children and youth ≤ 17 years old. The NSCH is funded by the Health Resources and Services Administration’s Maternal Child Health Bureau and is conducted by the US Census Bureau. It assesses multiple domains of emotional and physical health and well-being of children and youth 0–17 years old in the United States.18
Prior iterations of the survey were administered via random-digit dialing, but the NSCH-16 was administered via web and/or mail from June 2016 through February 2017. Outreach was conducted in English and Spanish. An initial screening questionnaire was administered, followed by a detailed survey focusing on one randomly-selected child per household. The survey was translated into English and Spanish, and telephonic interpretation was offered to parents requesting other language support. The survey oversampled children ≤5 years of age and children with special healthcare needs. Sampling weights were adjusted for non-response, and survey data were weighted to allow for generalizability to the entire non-institutionalized, ≤17 year-old population. The NSCH-16 sample size was 50,212 (representing 73.35 million children and youth nationally), with an overall weighted response rate of 40.7%. Additional information regarding survey methodology is available elsewhere.22
The NSCH-16 is a publicly-available, de-identified dataset. Its use is not considered Human Subjects Research and did not require IRB approval.
Analytic Sample
The analytic sample wa s restricted to 2–17 year-aids with non-missing data on household generation (an NSCH variable combining parental and child nativity) and at least one of the five parent-reported current MBH problems, consistent with MBH problems included in prior NSCH studies of children.23 The five MBH problems assessed were: “Behavioral or Conduct Problems,” “Attention Deficit Disorder or Attention Deficient/Hyperactivity Disorder,” “Autism or Autism Spectrum Disorder,” “Depression,” and “Anxiety Problems” They required affirmative responses to the survey questions of, “Has a doctor or other health care provider [or educator, for behavior or conduct problems] EVER told you that the child has…” and, “If Yes, does the child CURRENTLY have the condition.” A total of 725 respondents were excluded from the analytic sample because of missing data: 17 had missing data on all five MBH problems, and of those with identified MBH problems, 689 had missing data on household generation and 21 were 0 to ≤1 years of age (2 had missing data in both age and household generation categories).
The final analytic sample, after exclusions, included 7,183 children and youth (representing 8.87 million nationally). Among these, 813 were CIF and 6,370 were non-CIF. The survey-weighted prevalence of ≥1 parent-reported current MBH problem was significantly lower for CIF than non-CIF (9.5% vs 17.0%, p<0.001), and, with the exception of ASD, the survey-weighted prevalence of each MBH problem was also statistically significantly lower for CIF than non-CIF (Appendix Figure 1).
Study Variable Construction and Selection
Children and Youth in Immigrant Families
Consistent with prior studies,24,25 CIF were defined as US- or foreign-born children and youth with at least one parent born outside of the United States. Using the NSCH “household generation” variable, CIF were defined as children and youth in 1st and 2nd generation households, and non-CIF were defined as those in 3rd generation households.
Outcome Variables
The primary outcome was receipt, in the 12 months prior to the survey, of “any MBH treatment,” defined as an affirmative response to any of the six survey questions about MBH treatment. Secondary outcomes were non-mutually exclusive receipt of the individual treatment types: (1) counseling (+/− medication) and (2) medication (+/− counseling) (Appendix Figure 2).
Covariate Selection
Based on prior studies of access to MBH services and of CIF, covariates included: gender, age (continuous measurement in years), race/ethnicity (compiled by NSCH into Hispanic, Non-Hispanic Black, Non-Hispanic Asian, Non-Hispanic Other/Multi-Racial, and Non-Hispanic white, and subsequently reported in this study as Hispanic/Latinx, African-American/Black, Asian, other, and white), household structure (single mother, two parent, or other), insurance (public, uninsured, private, or unknown), household income (reported as percent of federal poverty level), parental education, and primary household language (English or other).26 The NSCH’s medical home composite measure was also included, given its association with access to care,27 which included an affirmative to at least one of the five criteria: has a personal doctor or nurse; has a usual source of care; received family-centered care; obtained specialty care referrals if needed; and obtained health care coordination if needed.22
Statistical Analyses
Statistical analyses were conducted using Stata Version 15 (StataCorp College Station, Texas). All analyses accounted for survey weights using the svy(subpop) command. Simple descriptive statistics and Pearson χ2 tests were used to compare the social and demographic characteristics of CIF and non-CIF as well as the primary and secondary outcomes. Using bivariate logistic regression, the principle variable (CIF/non-CIF) and all covariates were examined for association with the primary outcome (MBH treatment). Multivariable logistic regression was used to calculate adjusted odds ratios for receipt of the primary outcome (any MBH treatment) and secondary outcomes (medication +/− counseling, counseling +/− medication) by CIF compared with non-CIF after adjusting for covariates found to be significant at the P<0.2 level in bivariate models, which excluded the medical home and parental education variables from the analysis. Additionally, primary-household language was found to be collinear with non-CIF status (99.0% of non-CIF reported English as their primary household language) and was thus excluded. Multivariable logistic regression was also performed to assess primary and secondary outcomes by each MBH problem.
To ensure that our results were not overly sensitive to the way in which “MBH problems” was operationalized, sensitivity analyses were conducted in which the analytic samples were adjusted to include: (1) children and youth who had ever had a MBH problem, (2) children and youth with “other mental health condition” as a sixth current MBH problem, (3) children and youth with ADHD, ASD, anxiety, or depression (but not “behavioral or conduct problems”), (4) children and youth with ADHD, anxiety, behavioral or conduct problems, or depression (but not “ASD”), and (5) a restricted age range of 6–17. Results were comparable to those documented below. See Appendix for details.
We also assessed whether the relationship between receipt of treatment and CIF was modified by family income, insurance status, age, geographic region, or family structure and did not find statistically significant differences among these interaction terms (p>0.05 for all).
Results
Sociodemographic characteristics
Among children and youth with MBH problems, sociodemographic characteristics that varied significantly (all p<0.001) between CIF and non-CIF included: report of English as the primary language spoken at home (60.1% CIF vs 99.0% non-CIF), white race (24.8% CIF vs 66.3% non-CIF), Hispanic/Latinx ethnicity (55.6% CIF vs 12.8% non-CIF), and parental post-high school education (59.9% CIF vs 83.7% non-CIF). Fewer CIF (29.1% vs 43.1% non-CIF) met the criteria of having a medical home. Gender, age distribution, insurance type, and household income were not significantly different (Table 1).
Table 1.
Children 2–17 years old with ≥1 Parent-Reported Mental/Behavioral Health Problem: Sociodemographic Characteristics, National Survey of Children’s Health-2016
| Children and Youth in Immigrant Families | Children and Youth in NonImmigrant Families | |
|---|---|---|
| Gender - Female | 41.04 (33.07 – 49.51) | 38.45 (36.12 – 40.84) |
| Age in Years | ||
| 2 to 5 | 9.07 (5.94 – 13.60) | 7.76 (6.39 – 9.39) |
| 6 to 11 | 39.97 (31.76 – 48.79) | 39.28 (36.88 – 41.73) |
| 12 to 17 | 50.96 (42.70 – 59.16) | 52.96 (50.51 – 55.39) |
| Race/Ethnicity*** | ||
| Hispanic/Latinx | 55.58 (47.69 – 63.19) | 12.8 (10.89 – 15.07) |
| African-American/Black, Non-Hispanic | 6.05 (3.76 – 9.59) | 13.5 (11.67 – 15.52) |
| Asian, Non-Hispanic/Latinx | 6.03 (4.06 – 8.88) | 0.69 (0.43 – 1.12) |
| Other, Non-Hispanic/Latinx | 7.59 (5.19 – 10.96) | 6.71 (5.44 – 8.26) |
| White, Non-Hispanic/Latinx | 24.75 (19.07 – 31.47) | 66.28 (63.66 – 68.80) |
| Insurance | ||
| Public | 44.54 (36.18 – 53.22) | 35.60 (33.11 – 38.16) |
| Private | 50.07 (41.88 – 58.26) | 59.40 (56.85 – 61.90) |
| Uninsured | 3.42 (1.72 – 6.67) | 3.49 (2.60 – 4.73) |
| Unknown | 1.97 (0.70 – 5.39) | 1.51 (1.05 – 2.19) |
| Household Income | ||
| 0–99% Federal Poverty Level | 28.24 (20.98 – 36.84) | 22.63 (20.49 – 24.92) |
| 100–199% Federal Poverty Level | 26.38 (18778 – 35.72) | 21.18 (19.18 – 23.33) |
| 200–399% Federal Poverty Level | 21.24 (15.82 – 27.90) | 26.51 (24.39 – 28.74) |
| >400% Federal Poverty Level | 24.15 (19.31 – 29.74) | 29.69 (27.73 – 31.72) |
| Household Structure*** | ||
| Single Mother | 11.99 (8.10 – 17.41) | 28.20 (26.01 – 30.50) |
| Two Parent | 85.79 (80.20 – 90.00) | 66.45 (64.04 – 68.77) |
| Other | 2.22 (1.06 – 4.59) | 5.35 (4.23 – 6.75) |
| Primary Household Language*** | ||
| English | 60.18 (51.56 – 68.22) | 98.95 (98.12 – 99.42) |
| Other | 39.82 (31.78 – 48.44) | 1.05 (0.58 – 1.88) |
| Has Medical Home*** | 29.06 (23.30 – 35.58) | 43.11 (40.77 – 45.49) |
| Highest Parental Education*** | ||
| < High School | 19.02 (12.52 – 27.82) | 5.97 (4.6 – 7.8) |
| High School or GED | 21.09 (14.23 – 30.08) | 20.33 (18.3 – 22.6) |
| > High School or GED | 59.89 (50.86 – 68.29) | 73.70 (71.2 – 76.0) |
Children and Youth in Immigrant Families – US or foreign-born children with at least one parent/guardian born outside of the United States. Percentages and 95% Confidence Intervals (CI) are survey-weighted. Reported n’s are non-weighted. Pearson χ2:
p <0.05;
p <0.01;
p <0.001.
Receipt of Any MBH Treatment among CIF and Non-CIF with MBH Diagnoses
Fewer CIF than non-CIF received any MBH treatment in the prior year (61.1% vs 71.3%, p = 0.02; Figure 1). In the bivariate (unadjusted) logistic regression model, the odds of receipt of any MBH treatment were lower for CIF than non-CIF with current parent-reported MBH problems (OR 0. 63, 95% CI 0.44–0.92; Table 2). In the multivariable logistic regression model,CIF status was no longer statistically significantly associated with MBH treatment after adjustment for covariates (AOR 0.76 95% CI 0.52–1.11; Table 2).
Figure 1.
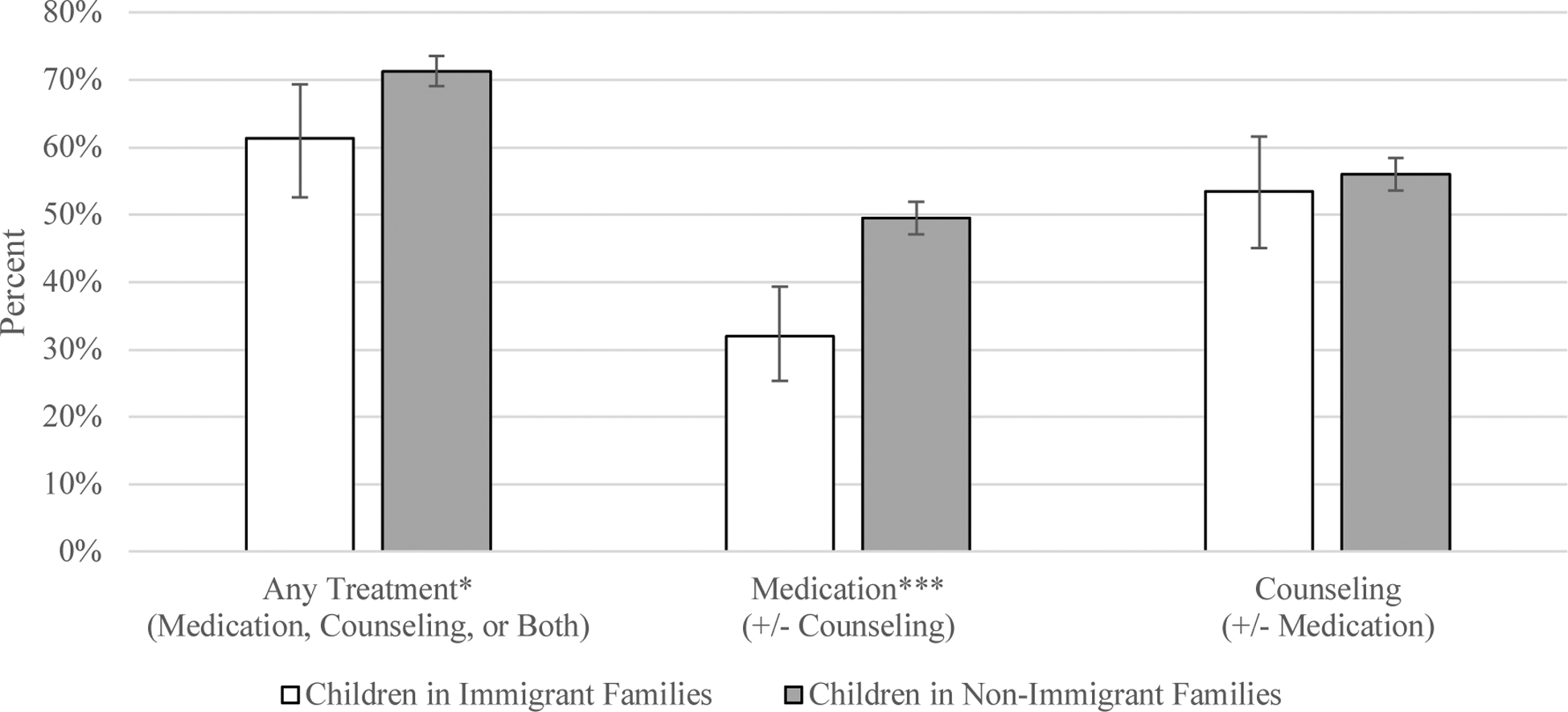
Children 2–17 years old with ≥1 Parent-Reported Mental/Behavioral Health Problem: Receipt of Mental/Behavioral Health Treatment by Type, National Survey of Children’s Health-2016
Children and Youth in Immigrant Families: US or foreign-born children with at least one parent/guardian born outside of the United States. Percentages and 95% Confidence Intervals (95 % CI), shown by bars, are survey-weighted.
Pearson χ2: *p <0.05; **p <0.01; ***p <0.001.
Table 2.
Children 2–17 years old with ≥1 Parent-Reported Mental/Behavioral Health Problem: Unadjusted and Adjusted Odds Ratios of Receipt of Any Mental/Behavioral Health Treatment in Prior Year, National Survey of Children’s Health −2016
| Receipt of Any MBH Treatment UOR (95% CI) | Receipt of Treatment AOR (95% CI) | |||
|---|---|---|---|---|
| Immigrant Family | ||||
| CIF | 0.63 (0.44 – 0.92) | 0.76 (0.52 – 1.11) | 0.61 (0.42 – 0.88) | 0.92 (0.64 – 1.33) |
| Non-CIF | 1.00 | 1.00 | 1.00 | 1.00 |
| Gender | ||||
| Male | 1.32 (1.04 – 1.67) | 1.37 (1.09 – 1.74) | 1.75 (1.43 – 2.12) | 0.99 (0.81 – 1.22) |
| Female | 1.00 | 1.00 | 1.00 | 1.00 |
| Age in Years | 1.06 (1.03 – 1.09) | 1.06 (1.03 – 1.09) | 1.13 (1.10 – 1.16) | 1.01 (0.99 – 1.04) |
| Race/Ethnicity | ||||
| Hispanic/Latinx | 0.62 (0.43 – 0.89) | 0.75 (0.43 – 1.06) | 0.59 (0.42 – 0.82) | 1.01 (0.72 – 1.40) |
| African-American/Black, Non-Hispanic/Latinx | 1.03 (0.73 – 1.46) | 0.99 (0.69 – 1.44) | 0.88 (0.63 – 1.24) | 1.18 (0.84 −1.65) |
| Asian, Non-Hispanic/Latinx | 0.82 (0.44 – 1.53) | 1.04 (0.54 – 2.00) | 0.62 (0.35 – 1.11) | 1.62 (0.86 – 3.05) |
| Other, Non-Hispanic/Latinx | 0.59 (0.37 – 0.94) | 0.61 (0.39 – 0.96) | 0.68 (0.48 – 0.96) | 0.72 (0.48 – 1.08) |
| White, Non-Hispanic/Latinx | 1.00 | 1.00 | 1.00 | 1.00 |
| Insurance | ||||
| Public | 1.08 (0.82 – 1.42) | 1.41 (1.02 – 1.95) | 1.32 (0.99 – 1.75) | 1.47 (1.10 – 1.96) |
| Uninsured | 0.43 (0.25 – 0.76) | 0.54 (0.32 – 0.91) | 0.81 (0.48 – 1.36) | 0.61 (0.36 – 1.03) |
| Unknown | 0.57 (0.26 – 1.27) | 0.74 (0.35 – 1.57) | 1.10 (0.48 – 2.50) | 0.67 (0.29 – 1.13) |
| Private | 1.00 | 1.00 | 1.00 | 1.00 |
| Household Income | ||||
| 0–99% Federal Poverty Level | 0.70 (0.51 – 0.96) | 0.59 (0.31 – 0.85) | 0.73 (0.53 – 1.01) | 0.61 (0.44 – 0.85) |
| 100–199% Federal Poverty Level | 0.69 (0.50 – 0.95) | 0.61 (0.43 – 0.87) | 0.74 (0.53 – 1.03) | 0.69 (0.50 – 0.94) |
| 200–399% Federal Poverty Level | 0.68 (0.52 – 0.88) | 0.67 (0.52 – 0.87) | 0.66 (0.53 – 0.83) | 0.72 (0.58 – 0.91) |
| >400% Federal Poverty Level | 1.00 | 1.00 | 1.00 | 1.00 |
| Household Structure | ||||
| Single Mother | 1.71 (0.97 – 3.02) | 1.39 (1.04 – 1.85) | 1.14 (0.89 – 1.47) | 1.34 (1.04 – 1.72) |
| Other | 1.22 (0.71 – 2.10) | 0.87 (0.53 – 1.40) | 0.81 (0.51 – 1.28) | 0.92 (0.59 – 1.42) |
| Two Parent | 1.00 | 1.00 | 1.00 | 1.00 |
Children and Youth in Immigrant Families – US or foreign-born children with at least one parent/guardian born outside of the United States. Unadjusted and adjusted odds ratios (UOR and AOR) and 95% Confidence Intervals (CI) are survey-weighted.
Receipt of MBH Medication among CIF and Non-CIF with MBH Diagnoses
Fewer CIF with current parent-reported MBH problems received medication than non-CIF (32.0% vs 49.5%, p < 0.001; Figure 1). In both the bivariate (unadjusted) and multivariable (adjusted) logistic regression models, the odds of receipt of medication (with or without counseling) were lower for CIF compared with non-CIF (OR 0.61, 95% CI 0.42–0.88; AOR 0.61, 95% CI 0.42–0.88; Table 2).
Receipt of MBH Counseling among CIF and Non-CIF with MBH Diagnoses:
There was no significant difference in the proportion of CIF compared with non-CIF who received counseling (53.4% vs 56.0%, p = 0.56; Figure 1). CIF status was not associated with receipt of counseling in either the unadjusted or adjusted model (Table 2).
Analysis of the Relationship Between MBH Problems and MBH Treatment
Because of the association between certain MBH problems and MBH treatment, access to treatment for each MBH problem was explored. In the analytic sample (comprised only of children and youth with at least one parent-reported, current MBH problem), CIF had a significantly lower prevalence of ADHD compared with non-CIF (34.5% vs 58.6%, p<0.001) as well as significantly lower prevalence of polymorbid (≥2) conditions (40.9% vs 51.4%; Figure 2). However, the receipt of MBH treatment, especially medication, was similar for CIF and non-CIF with ADHD, with markedly higher odds of receipt of medication for all who were reported to have ADHD (AOR 10.27, 95% CI 8.33 – 12.65; Table 3 and Figure 3).
Figure 2.
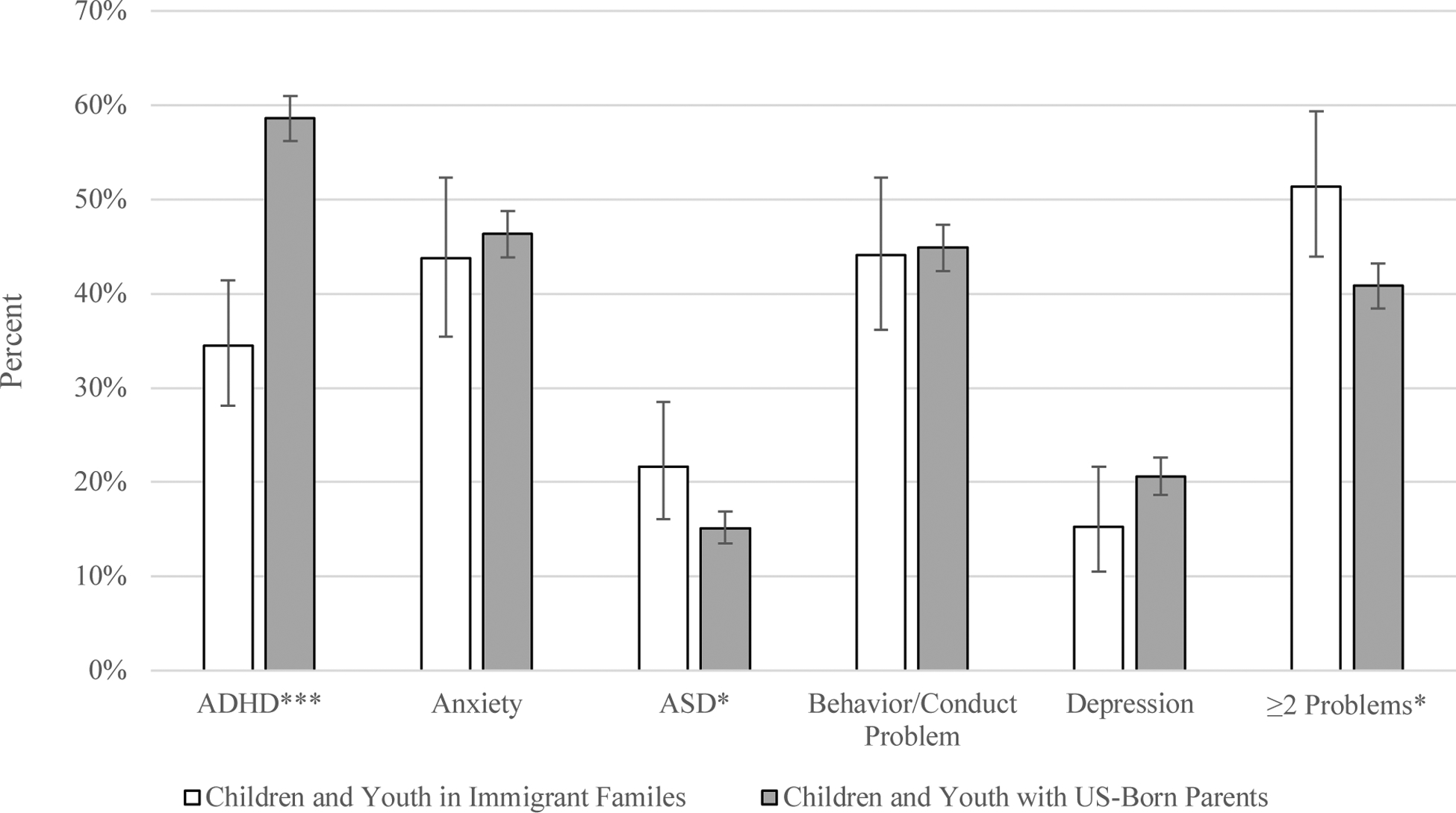
Children 2–17 years with ≥1 Parent-Reported Mental/Behavioral Health Problem: Prevalence of Specific Problems and of More than One Reported Problem, National Survey of Children’s Health-2016
Children and Youth in Immigrant Families: US or foreign-born children with at least one parent/guardian born outside of the United States. Percentages and 95% Confidence Intervals (95 % CI), shown by bars, are survey-weighted.
Pearson χ2: *p <0.05; **p <0.01; ***p <0.001
Table 3.
Odds Ratios for Receipt of Treatment in Prior Year by Mental/Behavioral Health Problem for Children 2–17 years old with ≥1 Parent-Reported Mental/Behavioral Health Problem, National Survey of Children’s Health-2016
| ° | Receipt of Any MBH Treatment UOR (95% CI) | Receipt of Treatment AOR (95% CI) | ||
|---|---|---|---|---|
| ADHD | ||||
| ADHD | 3.93 (3.12 – 4.96) | 3.72 (2.98 – 4.65) | 10.27 (8.33 – 12.65) | 1.42 (1.17 – 1.73) |
| CIF° | 0.92 (0.63 – 1.43) | 0.79 (0.54 – 1.14) | 0.93 (0.66 – 1.30) | |
| Anxiety | ||||
| Anxiety | 1.06 (0.83 – 1.34) | 1.03 (0.81 – 1.32) | 0.97 (0.78 – 1.20) | 1.90 (1.51 – 2.39) |
| CIF° | 0.77 (0.53 – 1.13) | 0.62 (0.42 – 0.91) | 0.95 (0.65 – 1.38) | |
| ASD | ||||
| ASD | 2.05 (1.48 – 2.84) | 2.35 (1.66 – 3.31) | 0.85 (0.66 – 1.10) | 3.11 (2.32 – 4.18) |
| CIF° | 0.72 (0.49 – 1.05) | 0.61 (0.42 – 0.89) | 0.86 (0.59 – 1.25) | |
| Behavior/Conduct Problem | ||||
| Behavior/Conduct Problem | 2.00 (1.58 – 2.45) | 2.33 (1.79 – 3.02) | 2.33 (1.88 – 2.89) | 2.57 (2.04 – 3.24) |
| CIF° | 0.77 (0.53 – 1.10) | 0.58 (0.40 – 0.84) | 0.93 (0.65 – 1.33) | |
| Depression | ||||
| Depression | 3.87 (2.83 – 5.27) | 3.95 (2.81 – 5.56) | 1.94 (1.49 – 2.52) | 5.01 (3.72 – 6.74) |
| CIF° | 0.79 (0.54 – 1.15) | 0.60 (0.41 – 0.89) | 0.97 (0.66 – 1.43) | |
Adjusted for individual MBH Problem (reference: no reported individual MBH problem) (data shown); Children or Youth in Immigrant Family (CIF) status (reference: non-CIF) (data shown); and adjusted for gender, age in years, insurance status, household income, and household structure (data not shown). MBH problems are not mutually exclusive. Unadjusted and adjusted odds ratios (UOR and AOR) and 95% Confidence Intervals (CI) are s urvey-weighted.
Figure 3.
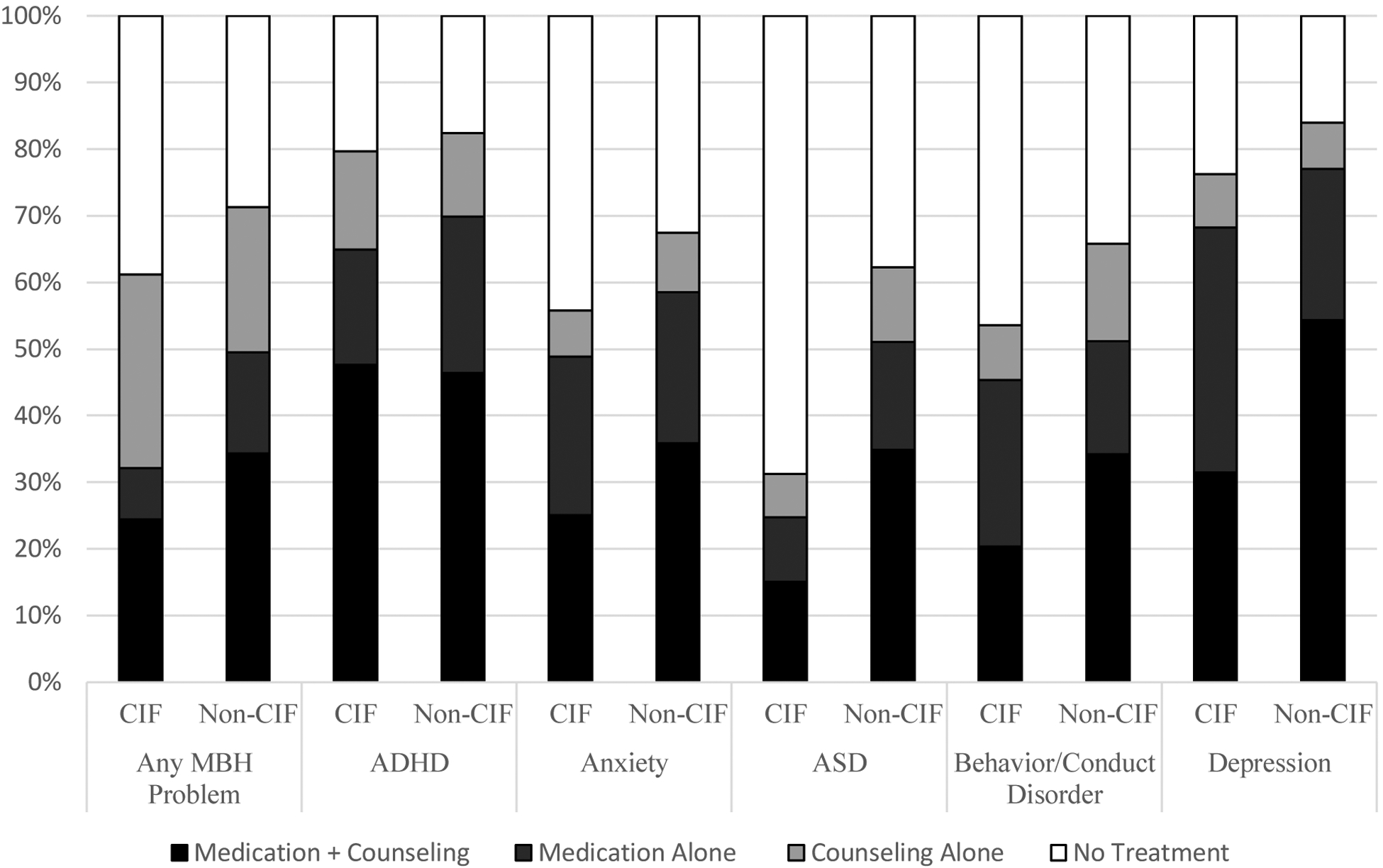
Receipt of Treatment by MBH Problem, Stratified by Treatment Type, in Children 2–17 years old with ≥1 Parent-Reported Mental/Behavioral Health Problem, National Survey of Children’s Health-2016
Need for Treatment for MBH Problems: Parent-Reported Severity
To assess the need for treatment among those with MBH problems, parent-reported MBH severity was assessed post-hoc. Parent-reported MBH severity was comparable for CIF and non-CIF (“moderate/severe” reported in 53.6% of CIF vs 59.3% of non-CIF, p = 0.184) and, in an adjustment for parent-reported severity of MBH problem alone, CIF again had lower odds of receipt of any MBH treatment (AOR 0.65, 95% CI 0.44 – 0.95).
Discussion
In this study using the nationally representative NSCH-16 dataset, we demonstrate that, among children and youth with parent-reported MBH problems, CIF, compared with non-CIF, are less likely to receive treatment, particularly medication. This difference in receipt of any treatment is not statistically significant after adjusting for multiple covariates, although receipt of medication remains statistically significantly different in the adjusted model. Children and youth with parent-reported ADHD—regardless of their immigrant s tatus—are far more likely to receive MBH treatment than children and youth with other parent-reported MBH concerns. However, among those with parent-reported MBH problems, fewer CIF than non-CIF have reported ADHD.
Differences in parent-reported ADHD diagnosis between CIF and non-CIF may be explained by prior research identifying racial/ethnic disparities in “access to diagnosis.” In the United States, multiple prior studies have identified fewer ADHD diagnoses among Hispanic/Latinx and African-American/Black children compared with white children.28–30 By contrast, research that has directly evaluated children for ADHD symptoms has found that Hispanic/Latinx and African-American/Black children have similar rates of ADHD symptoms compared with white children.28 This body of work suggests that ADHD may be underdiagnosed for African-American/Black and/or Hispanic/Latinx children, who together comprise 32.7% of the CIF in our analytic sample. For those who report a known ADHD diagnosis, however, receipt of treatment was similar for both CIF and non-CIF. This may reflect accessibility to treatment without subspecialty care; ADHD medications are most often prescribed by general pediatricians who treat ADHD more frequently than any other MBH diagnosis.31–33
This study adds to the established literature describing inequities in health care for CIF. Prior studies have demonstrated that CIF are less likely to have access to health insurance, a usual source of care, a patient-centered medical home, or access to a physician within one day when sick.34 In the fully adjusted model, those without health insurance or in lower income brackets were less likely to receive MBH treatment. Additionally, parents of CIF report fewer patient-centered interactions with healthcare providers. Specifically, they are less likely to report that providers spend enough time, listen carefully, provide detailed information, are culturally sensitive, or partner in care.35
We also found that CIF with MBH problems are less likely to be treated with medication, including in the fully adjusted model, while the receipt of counseling is comparable for CIF and non-CIF. This finding is consistent with prior reports on treatment preferences among African-American/Black, Hispanic/Latinx, and Asian parents and youth.36 Additionally, it may reflect a threshold effect for access to psychosocial treatment and counseling, given the United States’ well-documented shortage of pediatric MBH specialists,37 with fewer than 11% of respondents to the 2015 American Psychological Association Survey of Psychology Health Service Providers reporting an ability to provide care in a language other than English and fewer than 6% reporting an ability to provide Spanish-language care.38 ln other words, access to MBH counseling may be suboptimal for both CIF and non-CIF for reasons that are both population-specific and broadly systemic.
There were several limitations to this study. These data are based on parent report, and prior studies show that white parents are more likely to report that their children have ADHD and other MBH concerns compared with African-American/Black and Hispanic/Latinx parents.29 Of children and youth with ≥1 reported MBH problem, 689 had missing data on household generational status, and this group had different sociodemographic characteristics than the included sample population. Further, the dataset does not allow for nuanced analyses among immigrant subgroups—e.g., refugees or asylum-seekers—and was underpowered for this analysis to compare treatment for CIF born outside compared to inside the US. Additionally, while a sensitivity analysis that restricted the sample to 6–17 years of age found similar results to those reported, the dataset was underpowered to compare treatment by further age category restrictions (eg assessing 12–17 compared with 6–11 years). Individual items on the NSCH may also perform differently for CIF compared with non-CIF, as has been described prior in its under-identification of CIF with Special Healthcare Needs.39
Furthermore, because NSCH recruitment was conducted only in English and Spanish, other-language households were likely under-sampled, meaning families with limited English proficiency are likely to be both underrepresented in this sample and not representative of those other-language families with limited English proficiency who may have the greatest difficulty finding bilingual providers and other accommodation for language barriers.4 Additionally, the NSCH-16 relied on written materials for outreach, so findings from the NSCH-16 sample may not be representative of the experiences of children whose parents have low literacy skills. Finally, this survey was fielded during a politically contentious and fearful time for immigrants,40 and thus non-response and/or missing data may reflect under-sampling of more vulnerable immigrant families, such as those who have undocumented family members. Thus, this sample may not be representative of families with the greatest access barriers, and the findings likely overestimate access to care for CIF.
Conclusion
These data add to previous studies of CIF by demonstrating that, for children and youth with MBH problems, after adjustment for multiple covariates, the odds of receipt of any treatment (medication and/or counseling) was not statistically significantly different, but the odds of receipt of medication was significantly lower for CIF. This may be explained, in part, by differences in the proportion of CIF and non-CIF diagnosed with ADHD. It is important to note that survey limitations resulting from language and structural barriers may have resulted in under-sampling of selected CIF, especially CIF in families whose preferred language is neither English nor Spanish.
Programmatic and health policy interventions, as well as changes to future surveys to ensure full participation of CIF subgroups with the greatest access challenges, are needed to address unique barriers. We call for expanding access to health insurance; ensuring pediatric MBH systems offer interpretation, translation, and qualified bilingual/bicultural providers; and implementing quality improvement to address “access to diagnosis” disparities.
Supplementary Material
What’s New:
Compared with other children and youth with parent-reported mental and behavioral health problems, children and youth in immigrant families (CIF) are less likely to receive medication. A lower prevalence of reported ADHD diagnosis for CIF may contribute to this difference.
Acknowledgements:
Dr. Rosenberg’s postdoctoral fellowship and Drs. Rosenthal, Sharifi, and Cramer are supported by the Vale National Clinician Scholars Program and by CTSA Grant Number TL1TR001864 from the National Center for Advancing Translational Science (NCATS), a component of the National Institutes of Health (NIH). Dr. Sharifi is supported by grant number K08HS024332 from the Agency for Healthcare Research and Quality (AHRQ). Dr. Lebowitz is supported by National Institute of Mental Health (NIMH) Grant Number R61MH115113. Dr. Yun is supported by NICHD Grant Number K23HD082312. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or AHRQ.
Research Project Support: Dr. Rosenberg’s postdoctoral fellowship and Drs. Rosenthal, Sharifi, and Cramer are supported by the Yale National Clinician Scholars Program and by CTSA Grant Number TL1 TR001864 from the National Center for Advancing Translational Science (NCATS), a component of the National Institutes of Health (NIH). Dr. Sharifi is supported by grant number K08HS024332 from the Agency for Healthcare Research and Quality (AHRQ). Dr. Lebowitz is supported by National Institute of Mental Health (NIMH) Grant Number R61MH115113. Dr. Yun is supported by NICHD Grant Number K23HD082312. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or AHRQ.
Uncommon Abbreviations:
- NSCH-16
National Survey of Children’s Health 2016
- CIF
Children and Youth in Immigrant Families
- Non-CIF
Children and Youth in non-Immigrant Families
- MBH
Mental/Behavioral Health
- DACA
Deferred Action for Childhood Arrival
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest/Financial Disclosure: The authors have indicated they have no potential conflicts of interest nor relevant financial relationships relevant to this article to disclose.
References
- 1.Whitney DG, Peterson MD. US National and State-Level Prevalence of Mental Health Disorders and Disparities of Mental Health Care Use in Children. JAMA Pediatr. 2019;173(4):389–391. doi: 10.1001/jamapediatrics.2018.5399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patel V, Flisher AJ, Hetrick S, McGarry P. Mental health of young people: a global public-health challenge. Lancet. 2007;369(9569):1302–1313. doi: 10.1016/S0140-6736(07)60368-7 [DOI] [PubMed] [Google Scholar]
- 3.Costello EJ, He J, Sampson NA, Kessler RC, Merikangas KR. Services for Adolescents With Psychiatric Disorders: 12-Month Data From the National Comorbidity Survey-Adolescent. PS. 2014;65(3):359–366. doi: 10.1176/appi.ps.201100518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Children of Immigrants Data Tool. Accessed June 7, 2019 https://datatool.urban.org/charts/datatool/pages.cfm#
- 5.Thomson MS, Chaze F, George U, Guruge S. Improving Immigrant Populations’ Access to Mental Health Services in Canada: A Review of Barriers and Recommendations. J Immigr Minor Health. 2015;17(6):1895–1905. doi: 10.1007/s10903-015-0175-3 [DOI] [PubMed] [Google Scholar]
- 6.Phelps R, Coker TR. First, Do No Harm: Improving Access in Autism Diagnostic Assessments for Children Without Exacerbating Inequities in Care. Journal of Developmental & Behavioral Pediatrics. 2019;40(3):217–218. doi: 10.1097/DBP.0000000000000663 [DOI] [PubMed] [Google Scholar]
- 7.Zuckerman KE, Sinche B, Mejia A, Cobian M, Becker T, Nicolaidis C. Latino Parents’ Perspectives of Barriers to Autism Diagnosis. Acad Pediatr. 2014;14(3):301–308. doi: 10.1016/j.acap.2013.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yun K,Jenicek G, Gerdes M. Overcoming Language Barriers in Mental and Behavioral Health Care for Children and Adolescents-Policies and Priorities. JAMA Pediatr. Published online April 1, 2019. doi: 10.1001/jamapediatrics.2019.0400 [DOI] [PubMed] [Google Scholar]
- 9.Abe-Kim J,Takeuchi DT, Hong S, et al. Use of Mental Health–Related Services Among Immigrant and US-Born Asian Americans: Results From the National Latino and Asian American Study. Am J Public Health. 2007;97(1):91–98. doi: 10.2105/AJPH.2006.098541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hall WJ, Chapman MV, Lee KM, et al. Implicit Racial/Ethnic Bias Among Health Care Professionals and Its Influence on Health Care Outcomes: A Systematic Review. Am J Public Health. 2015;105(12):e60–76. doi: 10.2105/AJPH.2015.302903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Trent M, Dooley DG, Dougé J, Health Son A, Pediatrics C on C, Adolescence CO. The Impact of Racism on Child and Adolescent Health. Pediatrics. Published online July 29, 2019:e20191765. doi: 10.1542/peds.2019-1765 [DOI] [PubMed] [Google Scholar]
- 12.Flores G, Olson L, Tomany-Korman SC. Racial and ethnic disparities in early childhood health and health care. Pediatrics. 2005;115(2):e183–193. doi: 10.1542/peds.2004-1474 [DOI] [PubMed] [Google Scholar]
- 13.Mclaughlin KA, Costello EJ, Leblanc W, Sampson NA, Kessler RC. Socioeconomic Status and Adolescent Mental Disorders. Am J Public Health. 2012;102(9):1742–1750. doi: 10.2105/AJPH.2011.300477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Patler C, Hamilton E, Meagher K, Savinar R. Uncertainty About DACA May Undermine Its Positive Impact On Health For Recipients And Their Children. Health Affairs. 2019;38(5):738–745. doi: 10.1377/hlthaff.2018.05495 [DOI] [PubMed] [Google Scholar]
- 15.Roche KM, White RMB, Lambert SF, et al. Association of Family Member Detention or Deportation With Latino or Latina Adolescents’ Later Risks of Suicidal Ideation, Alcohol Use, and Externalizing Problems. JAMA Pediatr. Published online March 16, 2020. doi: 10.1001/jamapediatrics.2020.0014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rojas-Flores L, Clements ML, Hwang Koo J, London J. Trauma and psychological distress in Latino citizen children following parental detention and deportation. Psychol Trauma. 2017;9(3):352–361. doi: 10.1037/tra0000177 [DOI] [PubMed] [Google Scholar]
- 17.Lin SC, Yu SM, Harwood RL. Autism spectrum disorders and developmental disabilities in children from immigrant families in the United States. Pediatrics. 2012;130 Suppl 2:S191–197. doi: 10.1542/peds.2012-0900R [DOI] [PubMed] [Google Scholar]
- 18.Fazel M, Reed RV, Panter-Brick C, Stein A. Mental health of displaced and refugee children resettled in high-income countries: risk and protective factors. The Lancet. 2012;379(9812):266–282. doi: 10.1016/S0140-6736(11)60051-2 [DOI] [PubMed] [Google Scholar]
- 19.Hainmueller J, Lawrence D, Martén L, et al. Protecting unauthorized immigrant mothers improves their children’s mental health. Science. 2017;357(63 55):1041–1044. doi: 10.1126/science.aan5893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Venkataramani AS, Shah SJ, O’Brien R, Kawachi I, Tsai AC. Health consequences of the US Deferred Action for Childhood Arrivals (DACA) immigration programme: a quasi-experimental study. The Lancet Public Health. 2017;2(4):e175–e181. doi: 10.1016/S2468-2667(17)30047-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Finno-Velasquez M, Cardoso JB, Dettlaff AJ, Hurlburt MS. Effects of Parent Immigration Status on Mental Health Service Use Among Latino Children Referred to Child Welfare. PS. 2015;67(2):192–198. doi: 10.1176/appi.ps.201400444 [DOI] [PubMed] [Google Scholar]
- 22.US Census Bureau. 2016 National Survey of Children’s Health Methodology Report; 2018. Accessed May 5, 2019 https://www.census.gov/content/dam/Census/programs-surveys/nsch/tech-documentation/methodology/2016-NSCH-Methodology-Report.pdf
- 23.Tan TX. Emotional and Behavioral Disorders in 1.5th Generation, 2nd Generation Immigrant Children, and Foreign Adoptees. J Immigr Minor Health. 2016;18(5) :957–965. doi: 10.1007/s10903-016-0388-0 [DOI] [PubMed] [Google Scholar]
- 24.Mendoza FS. Health disparities and children in immigrant families: a research agenda. Pediatrics. 2009;124 Suppl 3:S187–195. doi: 10.1542/peds.2009-1100F [DOI] [PubMed] [Google Scholar]
- 25.Caballero TM, Johnson SB, Buchanan CRM, DeCamp LR. Adverse Childhood Experiences Among Hispanic Children in Immigrant Families Versus US-Native Families. Pediatrics. 2017;140(5). doi: 10.1542/peds.2017-0297 [DOI] [PubMed] [Google Scholar]
- 26.Novak P, Williams-Parry KF, Chen J. Racial and Ethnic Disparities Among the Remaining Uninsured Young Adults with Behavioral Health Disorders After the ACA Expansion of Dependent Coverage. J Racial Ethn Health Disparities. 2017;4(4):607–614. doi: 10.1007/s40615-016-0264-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fleary SA. Association Between the Medical Home Model of Care and Demographic Characteristics in US Children. Clin Pediatr (Phila). 2019;58(3):270–281. doi: 10.1177/0009922818813568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Coker TR, Elliott MN, Toomey SL, et al. Racial and Ethnic Disparities in ADHD Diagnosis and Treatment. Pediatrics. 2016;138(3). doi: 10.1542/peds.2016-0407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Morgan PL, Staff J, Hillemeier MM, Farkas G, Maczuga S. Racial and ethnic disparities in ADHD diagnosis from kindergarten to eighth grade. Pediatrics. 2013;132(1):85–93. doi: 10.1542/peds.2012-2390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schneider H, Eisenberg D. Who receives a diagnosis of attention-deficit/ hyperactivity disorder in the United States elementary school population? Pediatrics. 2006;117(4):e601–609. doi: 10.1542/peds.2005-1308 [DOI] [PubMed] [Google Scholar]
- 31.Chirdkiatgumchai V, Xiao H, Fredstrom BK, et al. National Trends in Psychotropic Medication Use in Young Children: 1994–2009. Pediatrics. 2013;132(4):615–623. doi: 10.1542/peds.2013-1546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Olfson M, Blanco C, Wang S, Laje G, Correll CU. National Trends in the Mental Health Care of Children, Adolescents, and Adults by Office-Based Physicians. JAMA Psychiatr y. 2014;71(1):81–90. doi: 10.1001/jamapsychiatry.2013.3074 [DOI] [PubMed] [Google Scholar]
- 33.Williams J, Klinepeter K, Palmes G, Pulley A, Fay JM. Diagnosis and treatment of behavioral health disorders in pediatric practice. Pediatrics. 2004;114(3):601–606. doi: 10.1542/peds.2004-0090 [DOI] [PubMed] [Google Scholar]
- 34.Kan K,Choi H, Davis M. Immigrant Families, Children With Special Health Care Needs, and the Medical Home. Pediatrics. 2016;137(1):e20153221. doi: 10.1542/peds.2015-3221 [DOI] [PubMed] [Google Scholar]
- 35.Calvo R, Hawkins SS. Disparities in Quality of Healthcare of Children from Immigrant Families in the US. Matern Child Health J. 2015;19(10):2223–2232. doi: 10.1007/s10995-015-1740-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cummings JR, Ji X, Allen L, Lally C, Druss BG. Racial and Ethnic Differences in ADHD Treatment Quality Among Medicaid-Enrolled Youth. Pediatrics. 2017;139(6):e20162444. doi: 10.1542/peds.2016-2444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Thomas KC, Ellis AR, Konrad TR, Holzer CE, Morrissey JP. County-Level Estimates of Mental Health Professional Shortage in the United States. PS. 2009;60(10):1323–1328. doi: 10.1176/ps.2009.60.10.1323 [DOI] [PubMed] [Google Scholar]
- 38.2015 APA Survey of Psychology Health Service Providers. https://www.apa.org. Accessed June 9, 2020.
- 39.Warden C, Yun K, Semere W. Using the Children with Special Health Care Needs Screener with Immigrant Families: An Analysis of the National Survey of Children’s Health. J Immigr Minor Health. Published online March 30, 2018. doi: 10.1007/s10903-018-0719-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


