Abstract
Background:
Angioplasty using a carotid stent is a treatment modality for carotid stenosis, with results similar to those obtained with endarterectomy, as demonstrated by important studies. The increasing use of this procedure has also led to a larger number of reports of complications, stent fractures among those. Stent fracture is a rare manifestation and hence needs further studying so that its actual prevalence can be determined, as well as its associated risk factors and proper clinical management. The current study reports the case of a patient who had previously undergone angioplasty with a carotid stent and, after an automobile accident, presented with a stent fracture and distal embolization of fragments thereof with neurological manifestation.
Case Description:
A male patient, 40 years old, presented with a history of previously stent carotid angioplasty. He had been involved in an automobile accident and suffered a stent fracture with distal fragment migration. As he was an asymptomatic patient (NIHSS 0, Rankin zero), we opted for a conservative treatment with oral anticoagulant.
Conclusion:
Angioplasty is an effective treatment for extracranial atherosclerosis and, albeit rare, stent fractures can result in the migration of fragments thereof. This occurrence should be suspected in patients who have sustained severe neck injuries due to sudden deceleration and may be associated with thromboembolism.
Keywords: Carotid artery injuries, Carotid stenosis, Cerebrovascular trauma, Intracranial embolism, Prostheses and implants, Stents

INTRODUCTION
Angioplasty coupled to carotid stent placement is a therapeutic option for the treatment of carotid stenosis having long- and medium-term results similar to those yielded by endarterectomy.[2,3] The increasing use of this treatment modality has led to a greater number of reports of complications related thereto.
Endovascular stent fractures are one of the possible complications and have been described in multiple topographies.[1,4,8] However, consistent information on the risks relating to this complication and how to manage these cases is still scarce.[8] The purpose of this paper is to describe the case of a carotid stent fracture associated with distal embolization of its fragments after a “whiplash” cervical trauma.
CASE DESCRIPTION
Male patient, 40 years old, dyslipidemic, presented with a right carotid territory transient ischemic attack 7 months prior. At the time, he underwent diagnostic investigation during which there was found evidence of moderate stenosis (about 60%) in the right carotid bulb associated with an ulcerated plaque. Double antiplatelet aggregation therapy was then prescribed with aspirin and clopidogrel and the use of statins, in addition to angioplasty with a 7 × 40 mm carotid wall stent. He progressed without complications and was discharged after 3 days without sequelae.
The patient had been involved in an automobile accident (a collision between a car and a pole) and was referred to the emergency room, with no neurological deficit at the time of admission. Tomography and angiotomography scans of both the neck and skull were performed and revealed signs of thrombosis/occlusion of the bifurcation of the right internal carotid artery, close to the origin of the middle cerebral artery.
Subsequently, he underwent cerebral angiography that showed multiple fractures in the stent and a small metallic image in the topography of a branch of the right lingual artery, which is suggestive of a fragment thereof [Figure 1]. The study of intracranial vessels showed the presence of a negative image in the bifurcation of the right internal carotid artery, which was compatible with a thrombus and thus determined a subocclusive stenosis (about 95%) at the site. That observation was also associated with an increasing slowing down in the opacification process of the right middle cerebral artery [Figure 2]. This artery was rechanneled from pial anastomoses originating from the right anterior and posterior cerebral arteries. Two small metallic images were evident in the topography of branches of the right middle cerebral artery as well, which was also suggestive of stent fragments [Figure 2].
Figure 1:
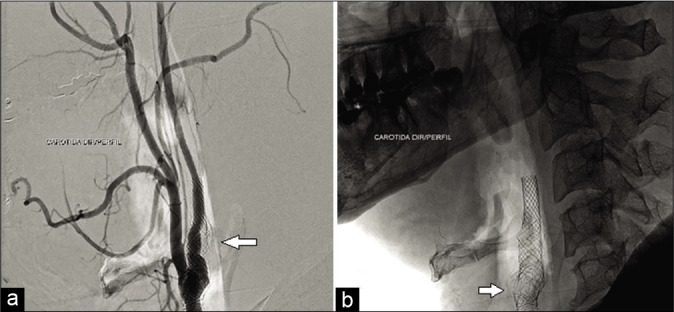
The right carotid angiography (lateral view) showing stent positioned in the right carotid bulb, irregularities, and in-stent stenosis (a). Image of the right carotid stent (arrow) (lateral view) showing the points of traumatic fracture in the stent (arrow) (b).
Figure 2:
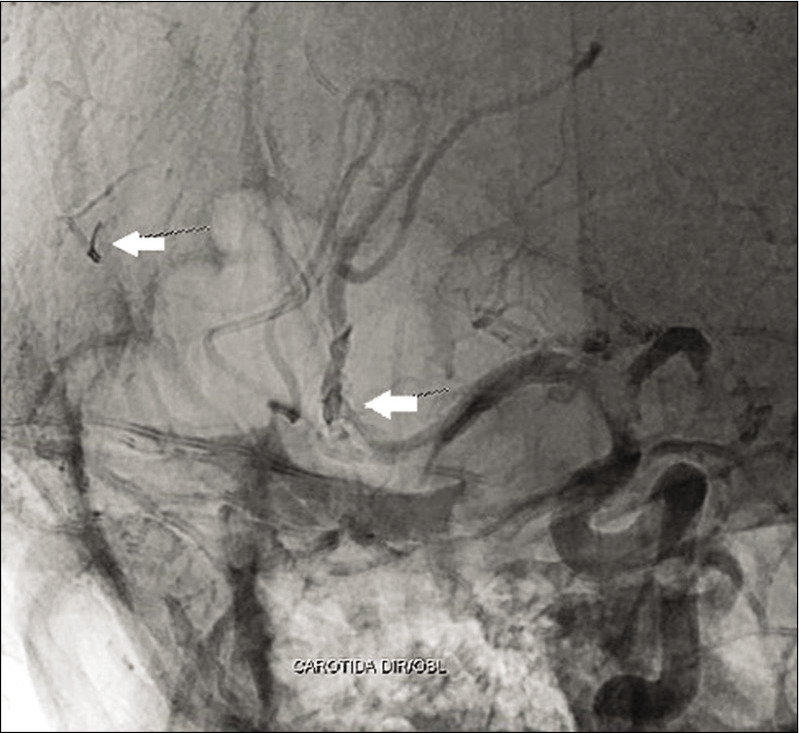
The right carotid angiography (oblique view) showing stent fragments (arrows) that migrated in the right middle cerebral artery.
As he was an asymptomatic patient (NIHSS 0, Rankin zero), we opted for a conservative treatment with oral anticoagulant and a target international normalized ratio (INR) between 2.0 and 3.0.
DISCUSSION
Endovascular stent fractures can occur in different topographies, but they usually occur in areas having arteries with great flexibility and exposed to repetitive movements.[1,4,8,9] The cervical region has great mobility, which predisposes the carotid to external mechanical forces.[1,5,6]
According to Vos et al.,[10] the presence of a carotid stent reduces arterial flexibility in head movements such as flexion, extension, and rotation.[10] Stent placement reduces the physiological curvature of the vessel, making it less compliant, more rigid as it creates points of articulation and parietal tension. These aspects make the stent more prone to fractures in certain regions.[8] The overlapping of stents and the implantation of long devices also increase the risk of fractures.[8]
Stent fractures are still a poorly studied event. The occurrence rate ranges from 0% to 29%,[4,11] but systematic studies are still required to assess the actual incidence of this complication.[11] Sfyroeras et al.,[8] in their review, found that stent fractures can occur from the time of implantation to 37 months thereafter.[8]
The asymptomatic carotid trial (ACT-1) carried out by Weinberg et al.[11] showed a stent fracture incidence of 5.4%.[11] In the group of patients with stent fractures, the lesions were found in or adjacent to the carotid bulb. In this group, the presence of calcification was one of the main risk factors.[11] There was no statistical difference regarding primary outcomes (death, stroke, and acute myocardial infarction) between groups with and without stent fractures.
The presence of thick and irregular calcification plaques makes it difficult to place the stent, as these prevent the device from fully expanding. The irregularity of the calcified plaque causes tension points on the stent’s external wall, and this tension can be exacerbated by neck movements.[8] Accordingly, the presence of calcification has been described as one of the main risk factors of stent fractures and deformities.[4]
In their review article published in 2010, Sfyroeras et al.[8] showed that calcified injuries can increase the risk of fractures by up to 7.7-fold.[8] In the group with stent fractures from ACT-1, 34.5% of participants had rather severe calcifications.[11] Chang et al.[4] in their case series showed a prevalence of fractures and deformities of 4% and 23%, respectively. The presence of calcified plaques increased the risk of fractures or deformities 6-fold. It was found that closed-cell stents are more prone to fractures when compared to open-cell stents, even though the latter showed a higher rate of deformities overtime.[4]
We present herein the case of a patient who had a stent fracture that was detected following severe trauma (i.e ., after being a victim in an automobile x pole collision). The sudden deceleration (“whiplash”) may have triggered the fracture accompanied by migration of small fragments thereof. To date, there is little information in the literature about the management of patients with carotid stent fractures. Despite having no reports of stent fractures associated to degenerative cervical spine disease, degenerative deformities of cervical spine, like spondylosis, might contribute to increase external forces against carotid wall and then could enhance chances of stent fractures after a trauma. Further studies are needed to evaluate cervical spine degenerative disorders and its association with carotid stent fractures.
Carotid Doppler ultrasonography is the test used for the clinical follow-up of patients who have undergone stent angioplasty. When in-stent restenosis is suspected, it is important to request imaging tests that visualize the stent’s structure, given that restenosis may be associated with fractures.[8] As in the reported case, patients who have sustained cervical trauma and also have a previous history of carotid stent should undergo tests that can assess the stent’s integrity.
The limited information regarding management of carotid stent fractures[8] leads it with variable ways to conduct. Treatment for carotid stent fractures may vary according to the type of fractures, others conditions associated such as instent restenosis and also according to clinical manifestations. The majority of the stent fractures are not associated with in-stent restenosis or neurological symptoms and may be followed up with imaging tests and no interventions are required.[1,4,11]
In cases of fractures associated with in-stent restenosis in asymptomatic patients, it is likely that the clinical follow-up alone will suffice.[8] Although restenting may stiffen the carotid segment and increase the susceptibility to further fractures,[8] stent in stent application might be an option for the treatment of in-stent restenosis associated with clinical symptoms.[1] Severe deformities within the stent may forbid a restenting treatment, and surgery for excision of the deformed carotid artery stent and reconstruction with interposition graft is an option.[4] In the presence of impedance to blood flow, stent penetrating the artery wall, or dissection of the carotid artery, open surgery with stent removal is an alternative treatment.[7,8]
In situations where the fracture is associated with thrombus formation, the placement of a new stent should be avoided due to the risk of distal embolization.[8]
In the case herein presented, the placement of another stent and mechanical thrombectomy was not indicated due to the risk that new fragments could migrate. Anticoagulant treatment was chosen because the patient was asymptomatic, and thrombi were distally present.
CONCLUSION
Most studies on angioplasty accompanied by the placement of a carotid stent do not aim to assess the structural behavior of stents overtime. Angioplasty is an effective treatment for extracranial atherosclerosis and, albeit rare, stent fractures can result in the migration of fragments thereof. This occurrence should be suspected in patients who have sustained severe neck injuries due to sudden deceleration and may be associated with thromboembolism.
Footnotes
How to cite this article: Silva DA, de Aguiar GB, Jory M, Conti ML, Veiga JC. “Whiplash” cervical trauma with fracture and migration of carotid stent fragments. Surg Neurol Int 2020;11:329.
Contributor Information
Danilo Almeida Silva, Email: danilo.med87@gmail.com.
Guilherme Brasileiro de Aguiar, Email: guilhermebraguiar@yahoo.com.br.
Maurício Jory, Email: jory@uol.com.br.
Mario Luiz Marques Conti, Email: mlconti@uol.com.br.
José Carlos Esteves Veiga, Email: jcemveiga@uol.com.br.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Boehm G, Gschwendtner M, Schillinger M. Carotid stent fracture: Diagnosis and management. Catheter Cardiovasc Interv. 2009;74:273–7. doi: 10.1002/ccd.22051. [DOI] [PubMed] [Google Scholar]
- 2.Brott TG, Hobson RW, 2nd, Howard G, Roubin GS, Clark WM, Brooks W, et al. Stenting versus endarterectomy for treatment of carotid-artery stenosis. N Engl J Med. 2010;363:11–23. doi: 10.1056/NEJMoa0912321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brott TG, Howard G, Roubin GS, Meschia JF, Mackey A, Brooks W, et al. Long-term results of stenting versus endarterectomy for carotid-artery stenosis. N Engl J Med. 2016;374:1021–31. doi: 10.1056/NEJMoa1505215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chang CK, Huded CP, Nolan BW, Powel RJ. Prevalence and clinical significance of stent fracture and deformation following carotid artery stenting. J Vasc Surg. 2011;54:685–90. doi: 10.1016/j.jvs.2011.03.257. [DOI] [PubMed] [Google Scholar]
- 5.Garcia-Toca M, Rodriguez HE, Naughton PA, Keeling A, Phade SV, Morasch MD, et al. Are carotid stent fractures clinically significant? Cardiovasc Intervent Radiol. 2012;35:263–7. doi: 10.1007/s00270-011-0149-3. [DOI] [PubMed] [Google Scholar]
- 6.Ling AJ, Mwipatayi P, Gandhi T, Sieunarine K. Stenting for carotid artery stenosis: Fractures, proposed etiology and the need for surveillance. J Vasc Surg. 2008;47:1220–6. doi: 10.1016/j.jvs.2008.01.043. [DOI] [PubMed] [Google Scholar]
- 7.Nazzal M, Abbas J, Nazzal M, Afridi S, Ritter M. Fractured internal carotid artery stent. Vascular. 2008;16:179–82. doi: 10.2310/6670.2008.00009. [DOI] [PubMed] [Google Scholar]
- 8.Sfyroeras GS, Koutsiaris A, Karathanos C, Giannakopoulos A, Giannoukas AD. Clinical relevance and treatment of carotid stent fractures. J Vasc Surg. 2010;51:1280–5. doi: 10.1016/j.jvs.2010.01.050. [DOI] [PubMed] [Google Scholar]
- 9.Valibhoy AR, Mwipatayi BP, Sieunarine K. Fracture of a carotid stent: An unexpected complication. J Vasc Surg. 2007;45:603–6. doi: 10.1016/j.jvs.2006.08.086. [DOI] [PubMed] [Google Scholar]
- 10.Vos JA, Vos AW, Linsen MA, Marcus JT, Overtoom TT, van den Berg JC, et al. Impact of head movements on morphology and flow in the internal carotid artery after carotid angioplasty and stenting versus endarterectomy. J Vasc Surg. 2005;41:469–75. doi: 10.1016/j.jvs.2004.12.033. [DOI] [PubMed] [Google Scholar]
- 11.Weinberg I, Beckman JA, Matsumura JS, Rosenfield K, Ansel GM, Chaturvedi S, et al. Carotid stent fractures are not associated with adverse events: Results from the ACT-1 multicenter randomized trial (carotid angioplasty and stenting versus endarterectomy in asymptomatic subjects who are at standard risk for carotid endarterectomy with significant extracranial carotid stenotic disease) Circulation. 2018;137:49–56. doi: 10.1161/CIRCULATIONAHA.117.030030. [DOI] [PubMed] [Google Scholar]


