Abstract
Background
On March 16, 2020, the federal government of Austria declared a nationwide lockdown due to the COVID-19 pandemic. Since the lockdown, screening examinations and routine checkups have been restricted to prevent the spread of the virus and to increase the hospitals’ bed capacity across the country. This resulted in a severe decline of patient referrals to the hospitals.
Objective
To assess the impact of the COVID-19 pandemic on the rate of newly diagnosed gynecological and breast cancers in Austria.
Methods
Data of 2077 patients from 18 centers in Austria with newly diagnosed gynecological or breast cancer between January and May 2019 and January and May 2020 were collected. Clinical parameters, including symptoms, performance status, co-morbidities, and referral status, were compared between the time before and after the COVID-19 outbreak.
Results
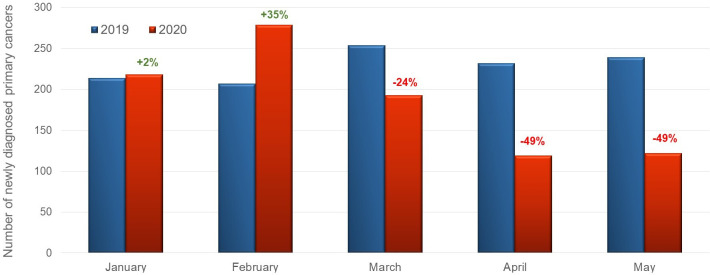
Our results showed a slight increase of newly diagnosed cancers in January and February 2020 as compared with 2019 (+2 and +35%, respectively) and a strong decline in newly diagnosed tumors since the lockdown: −24% in March 2020 versus March 2019, −49% in April 2020 versus April 2019, −49% in May 2020 versus May 2019. Two-thirds of patients diagnosed during the pandemic presented with tumor-specific symptoms compared with less than 50% before the pandemic (p<0.001). Moreover, almost 50% of patients in 2020 had no co-morbidities compared with 35% in 2019 (p<0.001). Patients, who already had a malignant disease, were rarely diagnosed with a new cancer in 2020 as compared with 2019 (11% vs 6%; p<0.001).
Conclusions
The lockdown led to a decreased number of newly diagnosed gynecological and breast cancers. The decreased accessibility of the medical services and postponed diagnosis of potentially curable cancers during the COVID-19 pandemic may be a step backwards in our healthcare system and might impair cancer treatment outcomes. Therefore, new strategies to manage early cancer detection are needed to optimize cancer care in a time of pandemic in the future.
Keywords: neoplasms
HIGHLIGHTS.
A strong decline in newly diagnosed gynecological tumors since the COVID-19 pandemic lockdown was observed in Austria.
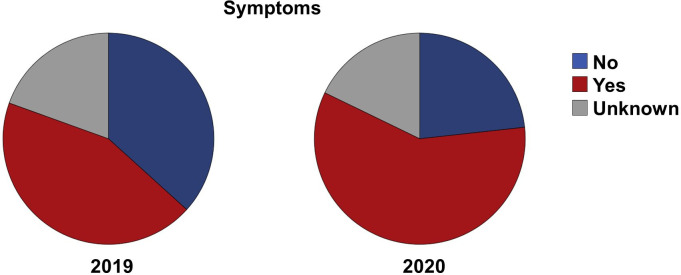
Two-thirds of patients diagnosed during the COVID-19 pandemic presented with tumor-specific symptoms.
50% of patients diagnosed during the pandemic had no co-morbidities compared with 35% before the pandemic.
INTRODUCTION
The ongoing coronavirus disease 2019 (COVID-19) pandemic is still challenging healthcare systems around the world. As of September 7, 2020, almost 27 million infections were reported worldwide with a death toll of more than 880 000.1 In Austria, more than 29 000 cases and 746 deaths were confirmed by September 7, 2020, leading to a death rate (2.5%) comparable to that of other European countries such as Germany (3%) but lower than in Italy (13%).1
The first COVID-19 cases in Austria were detected on February 25, 2020 at the University Hospital of Innsbruck. In the following days, several new cases were reported from Vienna. At the beginning of March, all outdoor events with more than 500 people and all indoor events with more than 100 people were canceled, universities switched to distance learning, and travel restrictions were established. On March 16, 2020, the federal government of Austria declared a nationwide lockdown, requiring citizens to remain in their homes except for necessary reasons.
In Austria, general practitioners and specialists function as gatekeepers of the healthcare system. They provide preventive and primary care and refer patients to hospitals if necessary. No organized screening program has been implemented in Austria for gynecological and breast cancers but an annual Pap smear and gynecological examination from the age of 20 and biennial mammography from the age of 40 is recommended. Since the lockdown, screening examinations and routine checkups have been restricted to prevent the spread of the virus and to increase the hospitals’ bed capacity across the country. This resulted in a severe decline of patient referrals to hospitals. At the gynecological departments, significantly fewer cancer diagnoses were noticed after the lockdown. The aim of this study was to validate the observation by data collection in large gynecologic and breast oncology centers across Austria.
METHODS
Patients
All patients diagnosed with gynecological or breast cancer in the period from January to May 2019 and from January to May 2020 at participating gynecological departments (n=18) in Austria were included in the present study. Clinical parameters, including tumor-specific symptoms, performance status, co-morbidities, tumor type, tumor stage, referral status, and COVID-19 infection status were evaluated. Referral status was defined as follows: referral by a specialist with or without tumor-specific symptoms, or presentation at an emergency or gynecological department with or without tumor-specific symptoms. Pre-defined sub-group analyses were performed in patients who were newly diagnosed with cancer in the period of the lockdown in 2020 (March 16, 2020 to May 31, 2020) and in the same period in 2019 (March 16, 2019 to May 31, 2019). The following symptoms have been regarded as tumor-associated: abdominal swelling/pain, vaginal bleeding, and palpable mass of the breast.
Statistical Analyses
Descriptive statistics, such as median, mean, frequencies, and percentages were used to describe the data. Clinical characteristics were analyzed using chi-square and Mann-Whitney U test. For all statistical analyses SPSS software version 26.0 was used. Two-sided p values <0.05 were regarded as significant. Bonferroni correction was applied for correction in multiple comparisons.
RESULTS
Data of 2077 patients from 18 gynecological and breast cancer departments around Austria with either newly diagnosed gynecological or breast cancer between January and May 2019 (n=1146) and 2020 (n=931) were retrospectively collected. Of these 2077 patients, 852 presented with a newly diagnosed gynecological cancer and 1225 with a newly diagnosed breast cancer.
Our results showed a slight increase of newly diagnosed cancers in January and February 2020 as compared with 2019 (+2% and+35%) and a strong decline in newly diagnosed cancers since the lockdown: −24% in March 2020 versus March 2019, −49% in April 2020 versus April 2019, −49% in May 2020 versus May 2019 (Figure 1).
Figure 1.
Newly diagnosed cancers. Cases of newly diagnosed gynecological and breast cancer in Austria 2019 (blue) and 2020 (red).
Due to low COVID-19 prevalence in Austria, no COVID-19 testing was performed for patients without symptoms. However, screening of symptoms by questionnaires, travel history, and temperature measurements were performed for all patients admitted to the hospitals. Of 150 patients who underwent a pre-operative COVID-19 test, one patient presented with COVID-19 specific symptoms and tested positive. This was a 96-year-old patient with endometrial cancer, who received neoadjuvant endocrine treatment due to her COVID-19 infection.
Clinical characteristics of the patients, who were diagnosed with cancer after the lockdown in 2020 (March 16th 2020 to May 31st 2020; n=342) and those, who were diagnosed with cancer in the same period in 2019 (March 16, 2019 to May 31, 2019; n=594) were included in the sub-group analysis (Table 1). In this sub-group analysis, diagnosis of different tumor types and performance status did not differ between the observed time points. During the COVID-19 pandemic, the median age of patients was significantly lower than for patients diagnosed with cancer in 2019 (59.4 vs 61.3 years, p=0.038). In 2019, almost 70% of the patients were 55 years old or older, versus only 60% in 2020. In gynecological tumors, there were no differences in tumor stage, while in patients with breast cancer, there was a decline in stage T1 as well as in stage T2–T4 tumors (−11% and −10%, respectively, NS). However, in 2020 significantly more patients with a newly diagnosed breast cancer were primary treated with neoadjuvant chemotherapy (+18%, p<0.001), therefore the pre-therapeutic pathological TNM stage was missing in a large amount of patients (n=71, 36%) (Table 2). No differences were observed in gynecological cancer treatment (neoadjuvant therapy or primary surgery) before or after the lockdown (data not shown). Since the lockdown, more patients presented at hospital without a referral compared with the same period in 2019 (30% vs 23%, p=0.009) (Table 3). Moreover, significantly more patients with a newly diagnosed cancer presented to gynecological departments due to tumor-specific symptoms since the lockdown in 2020 compared with the same period in 2019 (59% vs 44%, p<0.001) (Figure 2). Further evaluation of clinical data showed that nearly 50% of the patients in 2020 had no co-morbidities versus 35% in 2019 (p<0.001) (Table 3).
Table 1.
Patients‘ characteristics
| Characteristics | Patients with cancer diagnosed: | Difference (%) | P value | |
| Before lockdown (March 16, 2019 to May 31, 2019) |
During lockdown (March 16, 2020 to May 31, 2020) |
|||
| Number of patients | 594 | 342 | −42% | |
| Age, median (range) | 61.3 (21–93) | 59.4 (26–95) | 0.038* | |
| Patients with distant metastases (FIGO IV or M1) | 117 (20%) | 55 (16%) | −4% | NS† |
| Patients with early-stage disease (FIGO I or Tis/T1 and N0) | 284 (48%) | 133 (39%) | −9% | NS† |
| Breast cancer | 351 | 201 | −43% | |
| Tis | 34 (10%) | 17 (8.5%) | −1.5% | <0.001† |
| T1 | 149 (43%) | 64 (32%) | −11% | |
| T2–4 | 118 (34%) | 48 (24%) | −10% | |
| Tx (due to neoadjuvant chemotherapy) | 48 (14%) | 71 (35%) | ||
| N0 | 190 (54%) | 87 (43%) | −11% | <0.001† |
| N1-3 | 102 (29%) | 33 (16%) | −13% | |
| Nx (due to neoadjuvant chemotherapy) | 59 (17%) | 81 (40%) | ||
| Ovarian cancer | 70 | 36 | −49% | |
| FIGO I/II | 19 (27%) | 9 (25%) | −2% | NS† |
| FIGO III/IV | 51 (73%) | 27 (75%) | +2% | |
| Endometrial cancer | 77 | 51 | −34% | |
| FIGO I/II | 62 (80%) | 39 (76%) | −3% | NS† |
| FIGO III/IV | 15 (19%) | 11 (22%) | +3% | |
| Cervical cancer | 64 | 33 | −48% | |
| FIGO I/II | 44 (69%) | 28 (85%) | +17% | NS† |
| FIGO III/IV | 20 (31%) | 5 (15%) | −17% | |
| Vulvar cancer | 19 | 9 | −53% | |
| FIGO I/II | 15 (83%) | 5 (56%) | −27% | NS† |
| FIGO III/IV | 3 (17%) | 4 (44%) | +27% | |
| Uterine sarcoma | 5 | 4 | −20% | |
| Others | 8 | 8 | 0% | |
Characteristics before and after lockdown of all patients and dependent on cancer type.
*Mann-Whitney U-test.
†χ2 test.
NS, non-significant.
Table 2.
Frontline therapy in breast cancer before and during lockdown
| Front-line therapy in breast cancer (n=552) | ||||
| Parameter | Before lockdown (March 16, 2019 to May 31, 2019) |
During lockdown (March 16, 2020 to May 31, 2020) |
Difference (%) | P value |
| Primary surgery | 238 (68%) | 102 (51%) | −17% | <0.001* |
| Neoadjuvant chemotherapy | 77 (22%) | 81 (40%) | +18% | |
| Neoadjuvant endocrine therapy | 27 (8%) | 16 (8%) | 0% | |
| No therapy | 9 (2%) | 2 (1%) | −1% | |
| Total | 351 | 201 | ||
*χ2 test.
Table 3.
Patients’ characteristics
| Parameter | Patients with cancer diagnosed: | Difference (%) | P value | |
| Before lockdown (March 16, 2019 to May 31, 2019) |
During lockdown (March 16, 2020 to May 31, 2020) |
|||
| Number of patients | 594 | 342 | −42% | |
| Reported tumor-associated symptoms at diagnosis | ||||
| No | 207 (37%) | 77 (23%) | −14% | <0.001* |
| Yes | 247 (44%) | 195 (59%) | +15% | |
| Unknown | 140 | 70 | ||
| Referral of patients | ||||
| Patients without symptoms | 109 (18%) | 53 (16%) | −2% | 0.009* |
| Patients with symptoms | 30 (5%) | 41 (12%) | +7% | |
| Specialist | 378 (64%) | 209 (61%) | −3% | |
| General practitioner | 35 (6%) | 18 (5%) | −1% | |
| Emergency | 13 (2%) | 7 (2%) | 0% | |
| Unknown | 29 | 14 | ||
| Leading co-morbidities | ||||
| None | 206 (35%) | 163 (49%) | +14% | <0.001* |
| Cardiovascular disease | 124 (21%) | 81 (24%) | +3% | |
| Malignant disease | 67 (11%) | 22 (6%) | −5% | |
| Respiratory disease | 17 (3%) | 6 (2%) | −1% | |
| Infectious disease | 3 (0.5%) | 0 | −0.5% | |
| Rheumatic disease | 5 (1%) | 2 (1%) | 0% | |
| Endocrine & metabolic | 28 (5%) | 26 (8%) | +3% | |
| Psychiatric disorders | 20 (3%) | 8 (2%) | −1% | |
| Others | 23 (4%) | 5 (2%) | −2% | |
| Unknown | 101 | 20 | ||
Symptoms, referral of patients and co-morbidities before and after lockdown.
*χ2 test.
Figure 2.
Tumor-associated symptoms. Patients with and without symptoms at time of diagnosis in the years 2019 (March 16, 2019 to May 31,12019) and 2020 (March 16, 2020 to May 31 2020).
DISCUSSION
The lockdown due to the COVID-19 pandemic was implemented in Austria on March 16, 2020, resulting in social distancing and reduction of commercial activity, and also in severe restrictions in the healthcare system. Regular medical services and outpatient care were nearly shut down in an effort to prevent the spread of the virus and to increase the total capacity of hospitals. Thus, patients faced barriers to attending preventive checkups, to having mammography or screening for cervical cancer, or to consulting their general practitioner. As a result, significantly fewer cancer diagnoses were reported during the COVID-19 pandemic in different countries.2 3
Our results from 18 gynecological departments in Austria showed a strong decline in newly diagnosed cancers since March 2020. Moreover, significantly more patients with a newly diagnosed cancer presented to gynecological departments due to tumor-specific symptoms in 2020 as compared with 2019. We suppose that tumor-specific symptoms forced patients to consult a hospital, while patients with non-symptomatic cancer remained undetected. Of note, the number of patients presenting at the emergency unit of gynecological departments did not increase during the lockdown. Patients seemed to have concerns about coming into contact with other patients. Moreover, patients presenting at gynecological departments after the lockdown were significantly younger. This may display the attempt of older patients to minimize the risk of acquiring COVID-19 by avoiding hospitals and leaving their home, as more than 75% of patients who died due to COVID-19 infection were older than 75 years, although the majority of COVID-19 positive patients were younger than 55 years. While analyzing co-morbidities, we noticed, that patients who already had malignant disease, were more rarely diagnosed with a new cancer in 2020 as compared with 2019. Probably, the reason why these immunocompromised patients did not consult a specialist, was the anxiety about acquiring COVID-19 in a healthcare setting. Moreover, choice of primary treatment changed after lockdown in favor of neoadjuvant therapy. This implies medical doctors’ attempt to reduce intensive care bed occupancy.
Interestingly, we observed an increase of newly diagnosed gynecological and breast cancers in February 2020 as compared with February 2019 (+35%). We suppose that the pandemic situation and lockdown measures in Italy—Austria’s neighbour country—might have increased the awareness of patients of the need to attend screening examinations before the pandemic reached Austria.
Although Austria is a country with a maximum intensive care bed occupancy of 26% during the COVID-19 pandemic4 the accessibility of healthcare services was severely impaired, preventive care and early cancer detection programs were restricted, leading to an increase of undetected or postponed tumor diagnoses.
The aim of our work is to raise awareness of this issue. Several studies have shown that postponed cancer diagnoses affect tumor stage and delayed treatment start affects clinical prognosis in patients with cancer.5 6 However, it is still controversial whether delayed cancer diagnoses will lead to potential months of life lost. In our study, we did not notice a change in tumor stage at time of diagnosis before and after lockdown. However, the observation period in this study might be too short to observe a stage change, as of September 7 patients are still cautious and tend to postpone routine checkups. Nonetheless, the decreased accessibility of medical services and postponed diagnosis of potentially curable cancers during the COVID-19 pandemic, shown in this study of a large and representative cohort of patients, is clearly a step backwards in our healthcare system and might impair cancer treatment outcomes. Therefore, new strategies to maintain early cancer detection are needed to optimize cancer care during pandemics in the future, such as self-collection of HPV tests, optimization of patients’ waiting time to avoid unnecessary contacts, compulsory masks in healthcare settings, etc.
Footnotes
IT and ER contributed equally.
Contributors: IT, ER: Methodology, data curation, Writing-original draft preparation. GB, EP, JH-T, AR, CW, TW, SB, BP, MH, DH, KH, ET, SC, JP, SA, DG, GG, CE, KK, KL, AS, MS, VS, CS, TA, BH: Data curation, investigation, writing-reviewing and editing. CM: Supervision, conceptualization, methodology, data curation, writing-reviewing and editing.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: The ethics committee of the Medical University of Innsbruck, Austria approved the present study (IRB-Number 1163/2020).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request. The data that support the findings of this study are available on request from the corresponding author (C.M.)
References
- 1. John Hopkins University and Medicine COVID-19 Map - Johns Hopkins Coronavirus Resource Center, 2020. Available: https://coronavirus.jhu.edu/map.html [Accessed 7 Sep 2020].
- 2. Dinmohamed AG, Visser O, Verhoeven RHA, et al. Fewer cancer diagnoses during the COVID-19 epidemic in the Netherlands. Lancet Oncol 2020;21:750–1. 10.1016/S1470-2045(20)30265-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rosenbaum L. The untold toll — the pandemic’s effects on patients without Covid-19. N Engl J Med Overseas Ed 2020;382:2368–71. 10.1056/NEJMms2009984 [DOI] [PubMed] [Google Scholar]
- 4. Federal Ministry of Social Affairs, H., Care and Consumer Protection, Republic of Austria "Official COVID19 Dashboard (Public Information): Hospitalisation.", 2020. Available: https://info.gesundheitsministerium.at/dashboard_Hosp.html?l=de
- 5. Neal RD, Tharmanathan P, France B, et al. Is increased time to diagnosis and treatment in symptomatic cancer associated with poorer outcomes? Systematic review. Br J Cancer 2015;112 Suppl 1:S92–107. 10.1038/bjc.2015.48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hofstetter G, Concin N, Braicu I, et al. The time interval from surgery to start of chemotherapy significantly impacts prognosis in patients with advanced serous ovarian carcinoma - analysis of patient data in the prospective OVCAD study. Gynecol Oncol 2013;131:15–20. 10.1016/j.ygyno.2013.07.086 [DOI] [PubMed] [Google Scholar]