Abstract
Background and aims
COVID-19 is an ongoing global pandemic, affecting nearly 35 million people from 214 countries as at September 30, 2020 and emerging evidence suggests that obesity is a potential risk factor for communicable diseases, including viral infections. Therefore, we investigated the relationship between obesity prevalence of the total adult population and COVID-19 infection and mortality rates, in different countries.
Methods
A total of 54 countries from six continents were selected. Country-specific obesity prevalence data were retrieved from the latest non-communicable diseases profiles released by the Non-communicable Diseases and Mental Health Cluster of World Health Organization, while the real time statistics from the Worldometer website were used to extract data on COVID-19 infections and mortality per million of the total population as of September 30, 2020.
Results
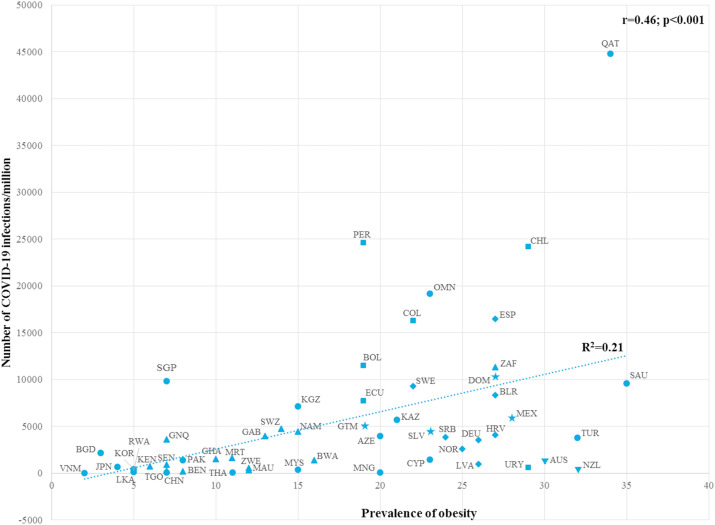
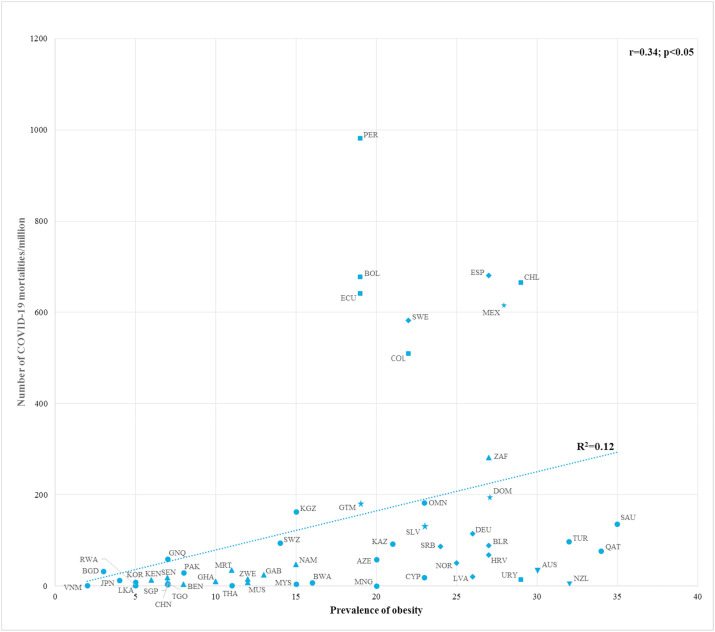
Obesity prevalence data ranged from 2.0% (Vietnam) to 35.0% (Saudi Arabia). Among the selected countries, the highest number of COVID-19 cases per million was documented in Qatar (n = 44,789) while the lowest was reported from Vietnam (n = 11). Highest mortality per million population due to COVID-19 infections occurred in Peru (n = 981), in contrast with the smallest number reported in Mongolia (n = 0). A significant positive correlation (r = 0.46; p < 0.001) was observed between the total number of COVID-19 infections and the prevalence of obesity. COVID-19 mortality was also significantly correlated (r = 0.34; p < 0.05) with the prevalence of obesity.
Conclusions
Obesity prevalence in each country was significantly associated with both infection and mortality rate of COVID-19.
Keywords: Obesity, COVID-19, Prevalence, Mortality
Highlights
-
•
Obesity is associated with increased risk of viral infections including COVID-19.
-
•
Country-specific obesity prevalence was significantly associated with both infection and mortality rate of COVID-19.
-
•
Countries with high prevalence of obesity should take measures to reduce COVID-19 infections to prevent unwanted deaths.
1. Introduction
COVID-19 has emerged as a global pandemic, affecting almost 35 million people as of September 30, 2020. While the USA, India and Brazil reported the highest number of confirmed cases, there are significant variations in the prevalence, severity and mortality associated with COVID-19 among different countries [1]. Variations are possibly attributable to differences in health care facilities and potential risk factors such as gender, age, chronic diseases, and other underlying health conditions [2]. For example, in a survival analysis conducted soon after the outbreak of COVID-19 in Wuhan Province, China, a high severity rate was observed among male patients over 65 years with underlying comorbidities such as diabetes, hypertension, coronary heart disease, and respiratory diseases [3]. Moreover, a recent study exploring multiple potential mechanisms responsible for the severity of COVID-19 infections, suggested that obesity could be a risk factor which mediates progression to a critical stage [4].
Obesity has long been linked with higher risk of non-communicable diseases (NCDs) [5], however previous research has established it is also associated with an increased risk of viral infections [6]. According to World Health Organization (WHO) estimates, more than 1.9 billion adults (≥18 years), were overweight and over 650 million were obese in 2016. This number has tripled within the last two decades [7]. A retrospective review of adult patients admitted with COVID-19 showed that 33% of obese patients had a higher rate of ICU admission and intubation, compared to normal-weight patients (21%, p = 0.001) and 78% of this number were more likely to suffer from fever and shortness of breath [8]. Similarly, COVID-19 patients with a body mass index (BMI) of 30–34 kg m−2 and >35 kg m−2 had 1.8 times and 3.6 times greater probability of being admitted to acute and critical care, respectively, than patients with a BMI <30 kg m−2 [9]. Simonnet et al. also observed that the proportion of COVID-19 patients who required IMV (Invasive Mechanical Ventilation) in critical care increased with BMI values, where 85.7% of patients with a BMI >35 kg m−2 needed IMV upon admission [10]. Furthermore, Huang and co-workers reported that the BMI values >28 kg m−2 were independently associated with the severity of COVID-19 disease (OR: 5.872; p = 0.008) [11].
Therefore, it will be valuable to explore the impact of country-specific obesity prevalence on both infection rate and severity of COVID-19. It is critically important to plan and implement sound preventive and therapeutic strategies to reduce the risk of severity and mortality of COVID-19, and to tackle the resultant economic crisis. Hence, we aimed to investigate the relationship of country-specific obesity prevalence with respect to infection and mortality rates from COVID-19 across different countries.
2. Methods
2.1. Data sources and inclusion/exclusion criteria
The real time statistics of total numbers of COVID-19 cases and deaths per million of the total population of selected countries as of September 30, 2020, were retrieved from the Worldometer website [1]. This source includes data from individual countries derived directly from official government reports or indirectly, through local media sources which are deemed reliable. Recent country profiles released by the Non-communicable Diseases and Mental Health Cluster (NMH) of World Health Organization presenting key facts on NCDs, were examined for obesity prevalence data [12], where obesity has been defined as BMI <30 kg m−2. Countries were selected based on the following inclusion/exclusion criteria: a) total population of the country >1 million; b) attenuated the first wave of COVID-19; c) scale flattened following a clear first peak; d) > 10,000 PCR tests done per million of the total population and e) not facing a second wave at the time of reporting.
2.2. Data extraction and analysis
Data were extracted from the NCD country profiles and the Worldometer website by one reviewer (DTJ) using a standardized form and checked for accuracy by a second reviewer (PR). The data extracted were: country name, continent, total population, number of COVID-19 infections per million population, COVID-19 mortality per million population, PCR tests done per million population, year of the NCD reports and obesity prevalence of adults. Discrepancies in the extracted data were resolved by discussion, with involvement of a third reviewer when necessary (RJ). The relationship between the prevalence of obesity and other dependent variables – total number of COVID-19 infections per million population and total number of COVID-19 mortalities per million population, were explored with correlation coefficients. Scatter plots were utilized to gain a visual representation of the correlation and the outcomes were analyzed by drawing a regression line. All countries were represented by a 3-letter country code based on the ISO (International Organization for Standardization) 3166, retrieved from the Terminology Bulletin Country Names and the Country and Region Codes for Statistical Use maintained by the United Nations Statistics Divisions [13].
3. Results
A total of 54 countries, satisfying the inclusion/exclusion criteria, were selected among six geographic regions (Asia-19; Africa-15; Europe-8; South America-6; North America-4; Oceania-2). With regards to obesity prevalence data, Saudi Arabia showed the highest obesity prevalence of 35.0% while Vietnam showed the lowest value of 2.0%. As of September 30, 2020, the number of COVID-19 infections ranged from 11 to 44,789 per million of the total country population, where the lowest and highest number of cases per million were reported in Vietnam and Qatar, respectively. The highest number of mortalities, 981 deaths per million, occurred in Peru, while zero deaths were reported in Mongolia.
The total population affected by COVID-19 showed a significant positive correlation (r = 0.46; p < 0.001) with the prevalence of obesity (Fig. 1 ). Moreover, our comparison suggested that 21% of the variation in the total infections can be attributed to the high prevalence of obesity among susceptible individuals (R2 = 0.21). The regression line generated from the correlation analysis showed an upward trend, and as expected, most countries were scattered around the line, with a few countries, including Singapore, Qatar, Peru and Chile, as outliers. The correlation effect was not significantly changed after removing the outliers from the analysis.
Fig. 1.
Correlation between the number of COVID-19 infections per million population and the prevalence of obesity among the selected countries, as of September 30, 2020.
AUS-Australia; AZE-Azerbaijan; BEN-Benin; BGD-Bangladesh; BLR-Belarus; BOL-Bolivia; BWA- Botswana; CHL- Chile; CHN-China; COL-Colombia; CYP-Cyprus;DEU-Germany; DOM-Dominican Republic; ECU-Ecuador; ESP-Spain; GAB-Gabon; GHA-Ghana; GNQ- Equatorial Guinea; GTM-Guatemala; HRV-Croatia; JPN-Japan; KAZ- Kazakhstan; KEN-Kenya; KGZ-Kyrgyzstan; KOR-South Korea; LKA-Sri Lanka; LVA-Latvia; MEX-Mexico; MNG-Mongolia; MRT-Mauritania; MUS-Mauritius; MYS-Malaysia; NAM-Namibia; NOR-Norway; NZL-New Zealand; OMN-Oman; PAK-Pakistan; PER-Peru; QAT-Qatar; RWA-Rwanda; SAU-Saudi Arabia; SEN-Senegal; SLV-El Salvador; SGP-Singapore; SRB-Serbia; SWE-Sweden; SWZ-Eswatini; TGO-Togo; TUR-Turkey; URY-Uruguay; VNM-Vietnam; ZAF-South Africa; ZWE-Zimbabwe;  - Africa;
- Africa;  - Asia;
- Asia;  - Europe;
- Europe;  - North America;
- North America;  - South America;
- South America;  - Oceania.
- Oceania.
The lower end of the line was densely populated by most of the Asian and African countries, indicating a low prevalence of obesity and a low infection rate. However, Asian countries showed greater variation in obesity prevalence and number of COVID-19 infections. Among the African countries, South Africa showed the highest obesity prevalence and number of infections. All European countries, except Spain and Sweden, were clustered below the upper middle of the regression line with moderate obesity prevalence and infection rate. In contrast, all South American countries except Uruguay were clustered above the upper middle of the regression line, with moderate obesity prevalence and high infection rate. Despite the high prevalence of obesity, Oceanic countries had a lower number of infections. Countries in the Middle East such as Saudi Arabia and Qatar were located around the top end of the regression line with higher values for both obesity prevalence and number of infections.
COVID-19 mortalities per million population was also significantly positively correlated with obesity prevalence (r = 0.34; p < 0.05) (Fig. 2 ). Most countries were scattered around the regression line, indicating 12% variability among the mortalities being due to high prevalence of obesity (R2 = 0.12). The bottom end of the regression line was populated by Asian and African countries with low levels of obesity prevalence and COVID-19 fatalities. Even though a wide range of obesity prevalence (2.0%–35.0%) was observed among Asian countries, none had higher levels of mortality, including Middle Eastern countries such as Qatar, Turkey and Saudi Arabia. All European countries (excluding Spain and Sweden), had moderate levels of obesity prevalence as well as mortalities. However, most Latin American countries as was the case for Spain and Sweden, had higher mortality numbers, despite moderate levels of obesity. Countries in Oceania showed a lower mortality rate and high prevalence of obesity.
Fig. 2.
Correlation between the number of COVID-19 mortalities per million population and the prevalence of obesity among the selected countries, as of September 30, 2020.
AUS-Australia; AZE-Azerbaijan; BEN-Benin; BGD-Bangladesh; BLR-Belarus; BOL-Bolivia; BWA- Botswana; CHL- Chile; CHN-China; COL-Colombia; CYP-Cyprus; DEU-Germany; DOM-Dominican Republic; ECU-Ecuador; ESP-Spain; GAB-Gabon; GHA-Ghana; GNQ- Equatorial Guinea; GTM-Guatemala; HRV-Croatia; JPN-Japan; KAZ- Kazakhstan; KEN-Kenya; KGZ-Kyrgyzstan; KOR-South Korea; LKA-Sri Lanka; LVA-Latvia; MEX-Mexico; MNG-Mongolia; MRT-Mauritania; MUS-Mauritius; MYS-Malaysia; NAM-Namibia; NOR-Norway; NZL-New Zealand; OMN-Oman; PAK-Pakistan; PER-Peru; QAT-Qatar; RWA-Rwanda; SAU-Saudi Arabia; SEN-Senegal; SLV-El Salvador; SGP-Singapore; SRB-Serbia; SWE-Sweden; SWZ-Eswatini; TGO-Togo; TUR-Turkey; URY-Uruguay; VNM-Vietnam; ZAF-South Africa; ZWE-Zimbabwe;  - Africa;
- Africa;  - Asia;
- Asia;  - Europe;
- Europe;  - North America;
- North America;  - South America;
- South America;  - Oceania.
- Oceania.
4. Discussion
The results of our analysis demonstrate that obesity prevalence is a potential risk factor for both COVID-19 infection rate and mortality. This is in accordance with findings of previous studies [9,10,14]. To the best of our knowledge, this is the first research to report on the potential the impact of country-specific obesity prevalence on infection and mortality rate associated with the COVID-19 epidemic.
Only 54 of 214 affected countries globally, surpassed the first wave of COVID-19 infections and satisfied other inclusion criteria. Nearly one third of the countries were selected from the Asian continent. However, this is consistent with previous epidemiological findings, highlighting that the very first outbreak of the SARS CoV-2 virus occurred in China and subsequently spread to other continents [15]. Consequently, these countries were able to flatten the number of COVID-19 infections earlier compared to others that have emerged as new epicenters [16]. For example, Mongolia, which shares a border with China, has successfully contained the virus with a reported 300 cases and zero deaths [1]. This result may have been possible due to early and strict border closures or being one of the least densely populated countries in the world [17].
Our results revealed that obesity prevalence is a significant risk factor among the susceptible individuals to be infected by SARS-CoV-2 virus, but the largest proportion of COVID-19 mortalities were reported among countries with moderate obesity prevalence. Generally, countries with higher obesity prevalence rates are also economically developed and citizens provided with well-established and highly equipped health care facilities. Therefore, we presume that the lower number of COVID-19 fatalities in these countries, despite a higher infection rate, can be attributed to their advanced medical care. Remarkably, the wealthiest country included in our study [18], Qatar, reported the maximum number of COVID-19 infections (n = 44,789) with only 76 mortalities, despite a high obesity prevalence rate (34%). The same pattern was observed in other affluent countries such as Saudi Arabia, Germany, Australia and New Zealand with a significantly lower number of fatalities despite more than 25% of the total adult population with obesity. This paradox can be attributed to several factors, advanced preventive and curative health policies, political leadership and mean age of the population. In contrast, South American countries like Peru, Chile and Ecuador have a higher number of mortalities, despite a moderate level of obesity, due to limited health care facilities [19]. We observed that Spain and Sweden had a higher rate of COVID-19 mortalities compared to other European countries, as they were affected in the initial months soon after the breakout and during that time, knowledge regarding the treatment of COVID-19 was limited.
4.1. Limitations
Our study has several limitations. The BMI value of 30 kg m−2 was considered as the cut-off point for defining obesity among the sample population. Even though this is in accordance with other observational studies [20], different cut-off points can be employed to define obesity among different ethnic groups. For instance, among Asian countries, a BMI value of 27 kg m−2, i.e. lower than WHO criteria, is used as the cut-off value for obesity [21]. In contrast, for Pacific Islanders, a BMI value of 32 kg m−2, higher than WHO criteria, is used as the cut-off value for obesity [22]. Furthermore, obesity data were obtained from a secondary source – WHO, therefore updated and most recent prevalence data may have been missed. Although recently published regional data on the prevalence of obesity are available for countries like Singapore, we used WHO country reports with the intention of possibly reducing substantial discrepancies between countries.
In addition, we excluded countries such as the USA, India and Brazil as they failed to satisfy one of our inclusion criteria of successfully flattening the curve of COVID-19 infections. Infection curves in these countries are still on exponential phase with nearly one-third of total global COVID-19 [1]. However, the countries which satisfy our inclusion criteria will likely change in coming days/weeks, and we expect to incorporate the changes in future analyses.
4.2. Future perspectives
Indeed, people worldwide should be encouraged to improve their life style with low calorie balance diets [23] comprised of vitamins (A and D), trace elements (Zinc and Selenium), nutraceuticals, and probiotics [24] and moderate to high physical activity levels [25]. The goal should be to reduce obesity prevalence in each country, which could be challenging despite the quarantine measures, and work from home behaviours during this pandemic. Governments should implement active measures to make populations more aware of the risk of obesity and the risk of greater adverse reactions of the COVID-19 infections in subsequent waves of the viral pandemic. Furthermore, countries with a higher prevalence of obesity should take extra precautions to minimize COVID-19 infections to prevent unwanted mortalities.
5. Conclusions
Significant positive correlations were observed between the total number of COVID-19 infections per million population (r = 0.46; p < 0.001) and mortality per million population (r = 0.34; p < 0.05) with respect to country-specific obesity prevalence in 54 countries. Most of the economically developed countries showed lower COVID-19 mortalities per million population despite a higher infection rate and higher obesity prevalence, likely due to superior hospital care facilities. Most South American countries had a higher number of COVID-19 mortalities per million population despite moderate levels of infection and obesity prevalence.
Declaration of competing interest
All authors declare that there are no conflicts of interest regarding the publication of this paper.
Abbreviations
- BMI
Body Mass Index
- COVID-19
Coronavirus disease 2019
- ICU
Intensive Care Unit
- IMV
Invasive Medical Care
- ISO
International Organization for Standardization
- NCD
Non-communicable disease
- PCR
Polymerase Chain Reaction
- SARS-CoV-2
Severe Acute Respiratory Syndrome Coronavirus
- USA
United States of America
- WHO
World Health Organization
References
- 1.Worldometer. COVID-19 coronovirus pandemic. Available online: https://www.worldometers.info/coronavirus/(Accessed on 01 October 2020).
- 2.Clark A., Jit M., Warren-Gash C., Guthrie B., Wang H.H., Mercer S.W. Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: a modelling study. Lancet Glob Health. 2020;8:E1003–E1017. doi: 10.1016/S2214-109X(20)30264-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li X., Xu S., Yu M., Wang K., Tao Y., Zhou Y. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J Allergy Clin Immunol. 2020;146:110–118. doi: 10.1016/j.jaci.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sattar N., McInnes I.B., McMurray J.J. Obesity a risk factor for severe COVID-19 infection: multiple potential mechanisms. Circulation. 2020;142:4–6. doi: 10.1161/CIRCULATIONAHA.120.047659. [DOI] [PubMed] [Google Scholar]
- 5.Field A.E., Coakley E.H., Must A., Spadano J.L., Laird N., Dietz W.H. Impact of overweight on the risk of developing common chronic diseases during a 10-year period. Arch Intern Med. 2001;161:1581–1586. doi: 10.1001/archinte.161.13.1581. [DOI] [PubMed] [Google Scholar]
- 6.Huttunen R., Syrjänen J. Obesity and the outcome of infection. Lancet Infect Dis. 2010;10:442–443. doi: 10.1016/S1473-3099(10)70103-1. [DOI] [PubMed] [Google Scholar]
- 7.Obesity and overweight. World health organization: Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (Accessed on 08 August 2020).
- 8.Hajifathalian K., Kumar S., Newberry C., Shah S., Fortune B., Krisko T. 2020. Obesity is associated with worse outcomes in COVID-19: analysis of early data from New York city. Obesity. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lighter J., Phillips M., Hochman S., Sterling S., Johnson D., Francois F. Obesity in patients younger than 60 years is a risk factor for Covid-19 hospital admission. Clin Infect Dis. 2020;71:896–897. doi: 10.1093/cid/ciaa415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Simonnet A., Chetboun M., Poissy J., Raverdy V., Noulette J., Duhamel A. High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation. Obesity. 2020;28:1195–1199. doi: 10.1002/oby.22831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huang R., Zhu L., Xue L., Liu L., Yan X., Wang J. Clinical findings of patients with coronavirus disease 2019 in Jiangsu province, China: a retrospective, multi-center study. PLoS Neglected Trop Dis. 2020;14 doi: 10.1371/journal.pntd.0008280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Noncommunicable diseases country profiles world health organization. 2018. https://www.who.int/nmh/countries/en/ Available online: Accessed on. [Google Scholar]
- 13.ISO 3166 Country Codes. In the International Standard for country codes and codes for their subdivisions, International organization for standardization: Available online: https://www.iso.org/obp/ui/#search (Accessed on 08 August 2020).
- 14.Grasselli G., Zangrillo A., Zanella A., Antonelli M., Cabrini L., Castelli A. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. J Am Med Assoc. 2020;323:1574–1581. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dawood F.S., Ricks P., Njie G.J., Daugherty M., Davis W., Fuller J.A. Observations of the global epidemiology of COVID-19 from the prepandemic period using web-based surveillance: a cross-sectional analysis. Lancet Infect Dis. 2020;20:1255–1262. doi: 10.1016/S1473-3099(20)30581-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Coronavirus: Africa could be next epicentre, WHO warns. Coronovirus pandemic. BBC news service: Available online: https://www.bbc.com/news/world-africa-52323375 (Accessed on 08 August 2020).
- 17.Daniel A., Anand T., Amelia K. Business insider. 2020. Mongolia beat the coronavirus with zero deaths — but its economy is in free fall and thousands of citizens remain stranded abroad.https://www.businessinsider.com/mongolia-coronavirus-border-closure-citizens-abroad-2020-10 Available online: Accessed on. [Google Scholar]
- 18.Richest countries in the world 2020. Global finance 2020. https://www.gfmag.com/global-data/economic-data/richest-countries-in-the-world Available online: Accessed on.
- 19.Quevedo-Ramirez A., Al-kassab-Córdova A., Mendez-Guerra C., Cornejo-Venegas G., Alva-Chavez K.P. Altitude and excess mortality during COVID-19 pandemic in Peru. Respir Physiol Neurobiol. 2020;281 doi: 10.1016/j.resp.2020.103512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Secondary Obesity: preventing and managing the global epidemic. World Health Organization; 2000. Obesity: preventing and managing the global epidemic.who.int/nutrition/publications/obesity/WHO_TRS_894/e Available online: Accessed on. [PubMed] [Google Scholar]
- 21.The asia-pacific perspective: redefining obesity and its treatment. World Health Organization; February 2000. https://apps.who.int/iris/bitstream/handle/10665/206936/0957708211_eng.pdf?sequence=1&isAllowed=y Available online: Accessed on. [Google Scholar]
- 22.Swinburn B., Ley S., Carmichael H., Plank L. Body size and composition in Polynesians. Int J Obes. 1999;23:1178–1183. doi: 10.1038/sj.ijo.0801053. [DOI] [PubMed] [Google Scholar]
- 23.Jayawardena R., Misra A. Balanced diet is a major casualty in COVID-19. Diabetes Metab Syndr. 2020;14:1085–1086. doi: 10.1016/j.dsx.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jayawardena R., Sooriyaarachchi P., Chourdakis M., Jeewandara C., Ranasinghe P. Diabetes & metabolic syndrome. Clinical Research & Reviews; 2020. Enhancing immunity in viral infections, with special emphasis on COVID-19: a review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ranasinghe C., Jayawardena R., Palihawadana V. Kick start training during the COVID-19 pandemic-Challenges of the sporting community. Sri Lankan J Sports Exerc Med. 2020;2 [Google Scholar]