Abstract
Panic disorder (PD) is ~2 times more frequent in women. An excessive ventilatory response to CO2 inhalation is more likely during the premenstrual phase. While ovarian hormones appear important in the pathophysiology of PD, their role remains poorly understood as female animals are rarely used in pre-clinical studies. Using neonatal maternal separation (NMS) to induce a “PD-like” respiratory phenotype, we tested the hypothesis that NMS disrupts hormonal regulation of the ventilatory response to CO2 in female rats. We then determined whether NMS attenuates the inhibitory actions of 17-β estradiol (E2) on orexin neurons (ORX). Pups were exposed to NMS (3 h/day; postnatal day 3–12). The ventilatory response to CO2-inhalation was tested before puberty, across the estrus cycle, and following ovariectomy. Plasma E2 and hypothalamic ORXA were measured. The effect of an ORX1 antagonist (SB334867; 15 mg/kg) on the CO2 response was tested. Excitatory postsynaptic currents (EPSCs) were recorded from ORX neurons using whole-cell patch-clamp. NMS-related increase in the CO2 response was observed only when ovaries were functional; the largest ventilation was observed during proestrus. SB334867 blocked this effect. NMS augmented levels of ORXA in hypothalamus extracts. EPSC frequency varied according to basal plasma E2 levels across the estrus cycle in controls but not NMS. NMS reproduces developmental and cyclic changes of respiratory manifestations of PD. NMS disrupts the inhibitory actions of E2 on the respiratory network. Impaired E2-related inhibition of ORX neurons during proestrus is a novel mechanism in respiratory manifestations of PD in females.
Subject terms: Physiology, Neuroscience
Introduction
Many panic disorder (PD) patients experience respiratory symptoms, including hyperventilation, sleep apnea, chest pain, and dyspnea1–3. According to Klein’s “False suffocation alarm hypothesis”, excessive sensitivity to respiratory stimuli is at the core of PD4. CO2 inhalation can trigger intense fear, autonomic, and ventilatory responses5 and the probability of experiencing the panicogenic effects of CO2 is greater in PD patients than healthy subjects6,7. Located in a hypothalamic region initially known as the “panic area”, orexin-producing neurons (ORX) regulate arousal and the intensity of respiratory reflexes8–10. ORX concentration in the cerebrospinal fluid of PD patients is higher than in healthy subjects11 and activation of ORX neurons and ORX-1 receptors are both necessary to observe a panic-prone state in rats and in humans11–13.
Early life adversities are an important risk factor for PD; clinical and pre-clinical data show that unstable parental conditions or experimental disruption of maternal care augment respiratory and behavioral responses to CO214–16. Much like chronic stress, neonatal maternal separation (NMS) augments ORX function17–19. Together, these data strongly argue that NMS-related dysregulation of ORX function is an important mechanism in excessive ventilatory response to CO2 inhalation in PD patients. The mechanisms responsible for abnormal ORX-modulation of the ventilatory control system are not fully understood, but to make significant progress that will ultimately influence clinical practice, pre-clinical research requires animal models that are close to the clinical reality20,21.
The prevalence of PD is 2–3 fold greater in women than in men, yet most of our basic knowledge arises from experiments performed on males despite strong evidence indicating that endocrine regulation of ORX neurons is sex-specific22,23. This is an important issue because clinical observations point to an important role of ovarian hormones in the pathophysiology of PD. The incidence of PD rises at puberty and in adult women, the responsiveness to CO2 inhalation is highest during the pre-menstrual phase. Together, these observations suggest that PD patients are more sensitive to hormonal fluctuation than healthy subjects24–26. To address this issue, we first tested the hypothesis that early life adversities (in the form of NMS) disrupts hormonal regulation of the ventilatory response to CO2. Specifically, we determined whether NMS-related increase in the responsiveness to CO2 inhalation evolves with reproductive status of females. Non-invasive respiratory measurements were performed prior to puberty, across each phase of the estrus cycle, and following ovariectomy. We then used a pharmacological approach to determine whether activation of ORX1-receptors is necessary to NMS-induced enhancement of the CO2 response. The evidence indicating that 17β-estradiol (E2) inhibits ORX neurons being indirect27,28, we then used whole-cell patch-clamp recordings to assess E2’s effects on green fluorescent protein (GFP)-labeled ORX neurons in females. Finally, we tested the hypothesis that NMS disrupts E2’s inhibitory actions on the ORX system and its influence on CO2-induced respiratory manifestation of PD in females.
Methods
Animals and ethical approval
Experiments were performed on sexually mature female Sprague–Dawley rats and pre-pubertal rat pups (14–15 days old) of both sexes. Rats were preferred to mice because, unlike mice, enhancement of the CO2 response due to early life adversities is sex-specific in this species15,29. Details about age, body weight, and animal distribution amongst the experimental groups are reported in Supplemental Table 1 and in the figures. All animals were born and raised in our animal care facilities. Rats were supplied with food and water ad libitum and maintained in standard conditions (21 °C, 12:12-h dark–light cycle: lights on at 06:00 and off at 18:00). Animal Care Committee of Université Laval approved all the experimental procedures and protocols, which were in accordance with the guidelines of the Canadian Council on Animal Care.
Neonatal maternal separation (NMS)
The NMS protocol was identical to the one used in our previous studies29,30. Briefly, virgin females were mated and 3 days after delivery, each litter was separated daily from their mother 3 h/day (09:00–12:00) from postnatal day 3–12. Control animals were undisturbed during the same period; see the Supplement for details. Rats were weaned and raised under standard animal care conditions until experiments were performed. For each group, rats originated from multiple litters to avoid litter-specific effects.
Whole-body plethysmography and tissue sampling
Ventilatory variables were measured in unrestrained, unanesthetized rats using whole-body plethysmography according to standard procedures30. 45 to 60 min prior to the recording, females were injected either with vehicle or with the selective ORX1 receptor antagonist (SB334867; 15 mg/kg). Ventilation was recorded at rest (room air) followed by hypercapnic exposure (5% CO2, balance air; 10 min). CO2 levels used to assess ventilatory and behavioral responsiveness varies between 5 and 35% in animals and humans31,32. The level chosen here ensured a robust ventilatory response with minimal change in behavior to avoid movement artefacts that interfere with respiratory measurements. At the end of the experiment, rats were deeply anesthetised; as NMS increases vaginal sensitivity33, determination of the estrus cycle by vaginal smear was performed only at this time to avoid influencing results. Blood and brains were then harvested to obtain post-CO2 samples immunohistochemistry and quantification of plasma E2 levels. Experiments were performed between 13:00 and 15:00. Note that blood and brains were also obtained from a distinct group exposed to room air to obtain baseline data for E2 and quantification of ORXA in hypothalamus extracts. For setup, protocol, and data collection details, see the Supplement.
Ovariectomy and 17β-estradiol (E2) replacement
Ovariectomy (OVX) was used to reduce circulating ovarian hormones chronically; surgery was performed according to standard procedures34. Two weeks after surgery, the CO2 response was measured and compared between NMS and controls. A distinct group of OVX females received either vehicle (peanut oil; 100 µl) or one E2 injection (3 or 10 µg) every 4 days to restore E2 level within physiological range and mimic cyclic fluctuations. The effects of higher E2 supplementation was tested in another group of OVX females by injecting with 25 µg. The last injections were performed on the day of the experiments. Based on the evidence suggesting that E2 inhibits ORX neurons27,28, only E2 was used in the replacement.
c-Fos/orexin-A immunohistochemistry
We first used c-Fos protein expression to determine whether NMS augments neuronal activation of ORX neurons in females. Based on ventilatory measurements, this initial evaluation was performed during the proestrus phase only. 40 μm coronal brain sections were double-labeled with primary antibodies against c-Fos and ORXA to confirm cell phenotype. Since the physiological function of ORX neurons differs between hypothalamic sub regions35–37, single (ORXA only) and double-labeled cells were counted in the dorsomedial and lateral hypothalamus (DMH and LH, respectively) and the perifornical area (PeF). See Supplement for details.
Whole-cell patch-clamp recording of orexin neurons
Identification of orexin neurons with an adeno-associated virus (AAV)
Four weeks-old females were injected with an AAV construct that expresses a green fluorescent protein (GFP) under the control of an ORX promoter. During surgery, rats received unilateral injections (1 µl/side) of the ORX:GFP virus in the following stereotaxic coordinates (from Bregma: RC: −2.6 mm; ML: 1.2 mm; DV: −9.0 mm). A 4-week recovery period ensured consistent GFP labeling; the intensity of GFP labeling observed in the PeF area was more apparent than in adjacent areas.
Slice electrophysiology
Hypothalamic slices (300 µm) containing GFP-labeled ORX neurons were used for whole-cell patch-clamp recording of basic electrophysiological properties, excitatory postsynaptic currents converging onto ORX neurons, and responses to E2 application (100 nM; 10 min). E2 concentration was based on the literature38. Slice preparation and recording procedures were performed as described previously39,40. Since ORX neurons of the LH do not contribute to cardiorespiratory regulation37, recordings were performed in the PeF/DMH. The estrus cycle was determined after the brain was harvested; data were compared between NMS and controls. See the Supplement for details.
Statistics
Multifactorial analysis of variance (ANOVA) assessed the effects of NMS and estrous cycle on respiratory variables, 17β-estradiol (E2), immunohistochemical, and electrophysiological data. CO2 exposure was also considered for analyses of respiratory data and E2; a repeated measures design was used when appropriate; equality of variance was tested. The relationship between E2 and the ventilatory response to CO2 was assessed using analysis of co-variance (ANCOVA) and a correlation z-test. Since patch-clamp data often originate from multiple cells from the same animal, a mixed ANOVA model (mixed-effect model) was used to ensure that between-group differences were not attributable to a specific subject41. ANOVA results are reported in the figures for clarity and conciseness. All data are presented as means ± SEM. A significant ANOVA results (P ≤ 0.05) was followed by a post hoc test (Fisher’s least significant difference) to identify specific differences; a Bonferroni correction was applied when multiple comparisons were performed. Analyses were performed using Statview 5.0 (SAS Institute, Cary, NC, USA) and JASP (version 0.13; University of the Netherlands).
Results
The ventilatory response to CO2 and 17β-estradiol (E2) levels across the female’s reproductive status
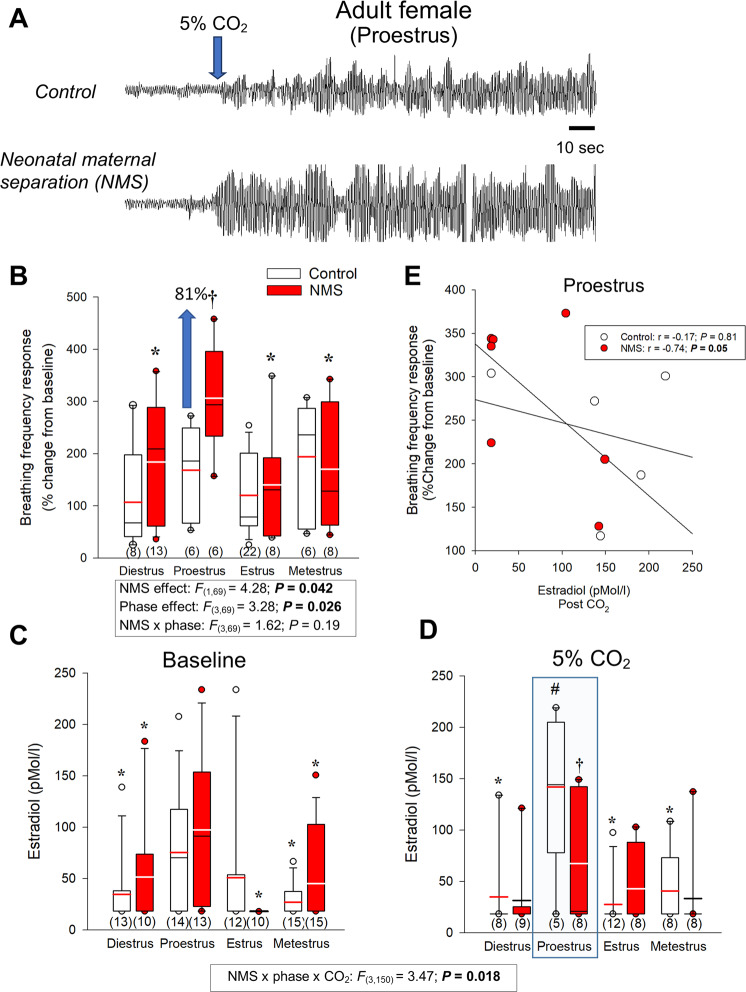
CO2 inhalation induced a rapid and robust hyperpnoea, which was greater in NMS females than controls (Fig. 1A, B). The intensity of the respiratory frequency and minute ventilation responses varied across the different phases of the estrus cycle and the largest difference between NMS and controls were observed during proestrus (Fig. 1A, B and Supplementary Fig. 1B). Baseline E2 levels fluctuated across the estrus cycle and peaked during proestrus; NMS did not affect those values (Fig. 1C). During proestrus, CO2 exposure augmented E2 levels in control, but not NMS females (Fig. 1D). The E2 levels measured following CO2 exposure during proestrus were inversely correlated with the intensity of the breathing frequency response in NMS but not controls (Fig. 1E).
Fig. 1. Comparison of the hyperventilatory response to CO2 inhalation (5% CO2; 10 min) between adult females raised under standard conditions or subjected to neonatal maternal separation (NMS) across the different phase of the estrus cycle.
A Original plethysmographic recording comparing ventilatory activity at rest and at the onset of CO2 inhalation (blue arrow) in a female raised under control conditions (top trace) versus a female subjected to neonatal maternal separation (bottom trace; NMS: 3 h/day; postnatal days 3–12). B The breathing frequency response expressed as a percentage change from baseline (room air). 17β-estradiol (E2) levels across the estrus cycles measured C while breathing room air (baseline) and D 30 min following CO2 inhalation test (5% CO2; 10 min). E Regression analysis comparing the relationship between E2 levels during proestrus (post-CO2; blue box) and the intensity of the breathing frequency response to CO2 between NMS (red circles) and control females (white circles). Box plots: the top and bottom boundaries of the box indicate the 25th and 75th percentile, respectively. Within the box, the black bar indicates the median; the other bar (red or white) indicate the mean. The error bars indicate the 10th and 90th percentiles. The numbers in brackets below the boxes indicate the number of replicates in each group. Post hoc pairwise comparisons were performed only when warranted by ANOVA. *Indicates a value different from corresponding proestrus value at P < 0.05. †Indicates a value different from corresponding control value at P < 0.05.
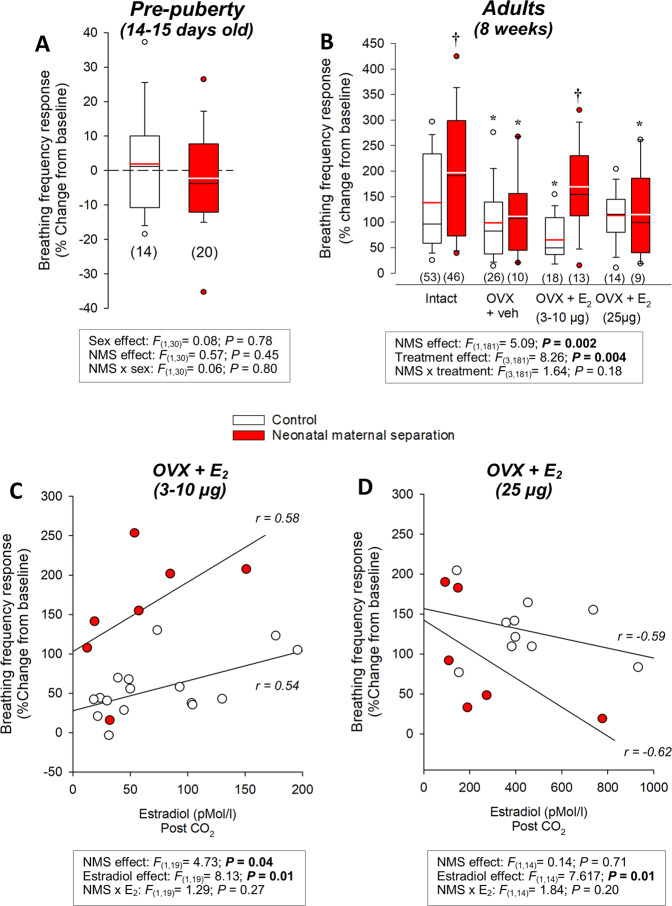
Prior to puberty, the hypercapnic ventilatory response was modest42; the response did not differ between sexes and was unaffected by NMS (Fig. 2A and see Supplementary Fig. 1C, D for effects on other respiratory variables). In adults, OVX reduced E2 levels (Supplementary Fig. 2) and the CO2 response such that the intensity of the hyperpnoea was now similar between groups (Fig. 2B). In OVX females, the first E2 supplementation protocol restored plasma E2 to physiological levels (Fig. 3C) and increased the respiratory frequency response in NMS but not controls. In both groups, the response was directly proportional to E2 levels (Fig. 2B, C and Supplementary Fig. 1). While the E2 levels achieved with the second supplementation protocol exceed normal values (Fig. 2D), this treatment demonstrated that at that elevated E2 inhibits the ventilatory response to CO2 (Fig. 2D and Supplementary Fig. 1E, F).
Fig. 2. Importance of ovarian function on the breathing frequency response to CO2 inhalation (5% CO2; 10 min).
Breathing frequency response to CO2 inhalation (5% CO2; 10 min) in A pre-pubertal rat pups (14–15 days old) and B adult females with intact ovaries or following (OVX) with and without 17-β estradiol (E2) replacement. Data from intact adult females include females without surgical procedure (from Fig. 1) and females that subjected to sham surgery that received vehicle injections (peanut oil; 100 µl). Ovariectomy or sham surgeries were performed 2 weeks prior to ventilatory measurements. E2 replacement reproduced cyclic fluctuations by performing a daily injection every 4 days over 12 days prior to the experiments (4 injections in total). Each injection contained either vehicle (peanut oil, 100 µl) or E2 (3 or 10 µg; normal levels or 25 µg; high levels). The histograms represent the frequency responses expressed as a percentage change from baseline (room air). Data are compared between rats raised under standard conditions (white bars) or subjected to neonatal maternal separation (NMS; red bars). Box plots: the top and bottom boundaries of the box indicate the 25th and 75th percentile, respectively. Within the box, the black bar indicates the median; the other bar (red or white) indicate the mean. The error bars indicate the 10th and 90th percentiles. The numbers in brackets below the boxes indicate the number of replicates in each group. Post hoc pairwise comparisons were performed only when warranted by ANOVA. *Indicates a value different from the corresponding intact value at P < 0.05. †Indicates a value different from the corresponding control value at P < 0.05. The relationship between plasma E2 levels and the intensity of the hyperventilatory response in OVX females supplemented with C normal E2 (3–10 µg) or D high E2 (25 µg).
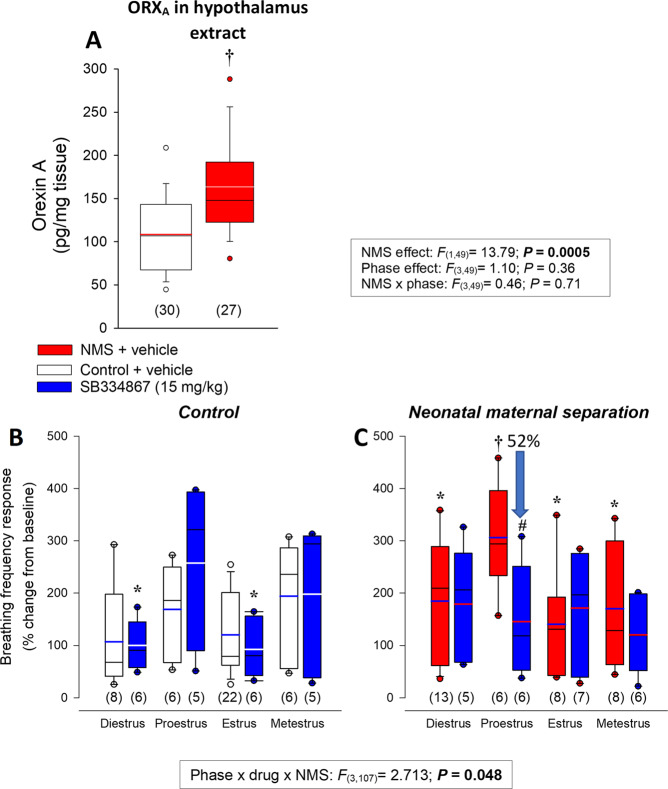
Fig. 3. Effects of neonatal stress on ORXA in the hypothalamus and effectiveness to the selective orexin-1 receptor antagonist SB334867 on the hyperventilatory response to CO2.
A Comparison of basal ORXA levels in hypothalamus extracts from females subjected to neonatal maternal separation (NMS; red bars) or raised under control conditions (white bars). Data were obtained from different each phase of the estrus cycle; however, data are pooled since the effect of ovarian status was not significant. B Effect of pre-treatment with SB334867 on the breathing frequency response of control females and C females subjected to NMS. Data were obtained during each phase of the estrus cycle; breathing was measured at the end of the CO2 inhalation test (5% CO2; 10 min) and expressed as a percentage change from baseline (room air). Data from SB334867-treated rats (15 mg/kg; I.P.; blue bars) are compared with those that received an injection of vehicle (50 mM HP-β-CD—10% + DMSO—2%) 45–60 min before start the plethysmography recordings. Box plots: the top and bottom boundaries of the box indicate the 25th and 75th percentile, respectively. Within the box, the black bar indicates the median; the other bar (red, white, or blue) indicate the mean. The error bars indicate the 10th and 90th percentiles. The numbers in brackets below the boxes indicate the number of replicates in each group. Post hoc pairwise comparisons were performed only when warranted by ANOVA. *Indicates a value statistically different from corresponding proestrus value at P < 0.05. †Indicates a value different from corresponding control value at P < 0.05. #Indicates a value different from corresponding vehicle value at P < 0.05.
None of the ventilatory variables and other indicators of metabolism measured at rest differed between groups. Breathing frequency of “resting” OVX females was slightly higher than intact females but this was not sufficient to augment minute ventilation (Supplementary Table 1).
Excessive ORX modulation contributes to NMS-related increase in CO2 response
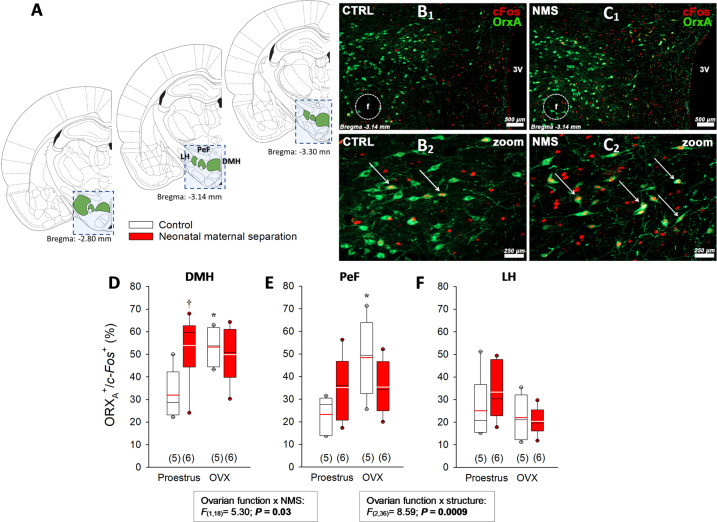
Anomalies in ORX neurotransmission contributes to the pathophysiology of a panic-prone state in rats and in humans11–13. To determine whether enhanced ORX contributes to NMS-related increase in CO2 responsiveness in females, we first quantified ORXA levels in hypothalamus extracts; values obtained in NMS females were 51% higher than controls (Fig. 3A). We then inactivated ORX1 receptors by pre-treatment with SB334867. The treatment did not affect breathing at rest (Supplementary Table 1) and generally had limited effects on the CO2 response; however, SB334867 prevented the excessive ventilatory response of NMS rats during proestrus (Fig. 3C and Supplementary Fig. 3). As physiological data indicate that NMS-related anomalies in respiratory control are more important during proestrus (Fig. 1), we used c-Fos immunolabeling to determine if ORX neurons of NMS females were more active than control during that phase (Fig. 4). By comparing data with OVX females, we evaluated the sensitivity to E2 withdrawal between groups. In the DMH, the percentage of ORX neurons expressing c-Fos was greater in NMS than control during proestrus. Since OVX increased this ratio only in controls, the level achieved was now similar between groups (Fig. 4D). While a similar trend was observed in the PeF, neither NMS nor OVX affected the number of double-labeled cells in the LH (Fig. 4E and F, respectively).
Fig. 4. Neonatal maternal separation (NMS) augments hypothalamic levels of orexin A (ORXA) and augments c-Fos immunolabelling in ORXA neurons in adult female rats.
A Schematic representation of frontal brain sections illustrating the hypothalamic region (blue square) that was isolated and homogenised to measure basal ORXA levels by ELISA assay. The schematic also illustrates the regions containing ORX neurons that were delineated to quantify c-Fos immunolabelling (adapted with permission from ref. 72). Photomicrographs comparing c-Fos (Texas red) and ORXA (FITC) immunolabelling between tissue sections from females in proestrus B1 raised under control conditions (CTRL) or C2 previously subjected to NMS (3 h/day, postnatal days 3–12). The third ventricle (3 V) and fornix (f) are identified as landmarks. Panels B2 and C2 were obtained at higher magnification for CTRL and NMS, respectively and white arrows identify double-labeled neurons. D Comparison of the proportion of ORXA positive neurons expressing c-Fos in the dorsomedial hypothalamus (DMH) between NMS and controls during proestrus and two weeks following ovariectomy (OVX). Similar analyses were performed in E the perifornical area (PeF) and F the lateral hypothalamus. Box plots: the top and bottom boundaries of the box indicate the 25th and 75th percentile, respectively. Within the box, the black bar indicates the median; the other bar (red or white) indicate the mean. The error bars indicate the 10th and 90th percentiles. The numbers in brackets below the boxes indicate the number of replicates in each group. Post hoc pairwise comparisons were performed only when warranted by ANOVA. †Significantly different from corresponding control value at P ≤ 0.05. *Indicates a value statistically different from corresponding proestrus value at P < 0.05.
Neonatal maternal separation disrupts E2 regulation of orexin neurons of the PeF/DMH
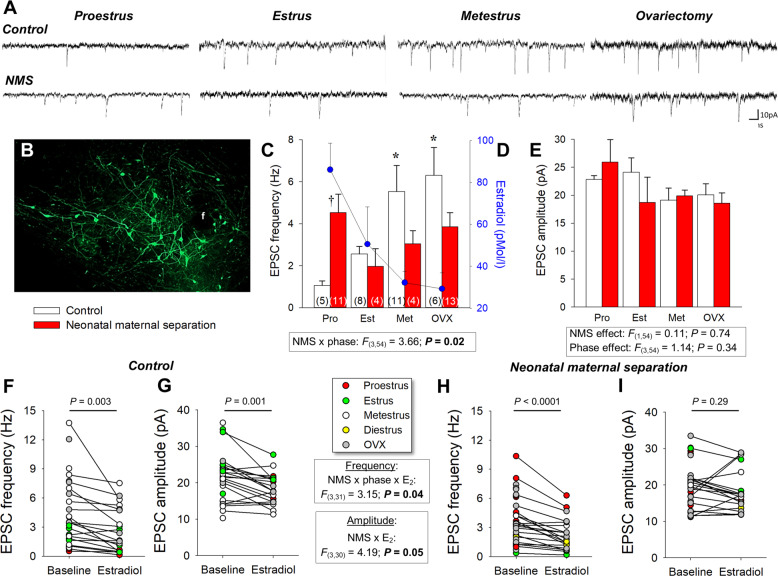
As our data indicate that NMS-related potentiation of ORX action on respiratory control is the greatest during proestrus, we then used whole-cell patch-clamp recording to assess the impacts of NMS and E2 on ORX neurons. In naturally cycling females, membrane potential (Vm) did not change across the estrus cycle and values recorded in NMS females were slightly lower than controls. However, OVX augmented cell capacitance and the resting Vm of ORX neurons in NMS but not controls (Supplementary Table 2). None of the other basic cell properties was influenced by NMS or ovarian function (Supplementary Table 2). Ovarian status influenced the excitatory postsynaptic currents (EPSC) frequency, especially in controls (Fig. 5A, C). In those females, EPSC frequency was inversely proportional to the basal level of E2 associated with each phase of the estrus cycle (Fig. 5C). In contrast with controls, ORX neurons from NMS females had the highest EPSC frequency during proestrus, when E2 levels peaked (Fig. 5A, C). EPSC amplitude was not affected by NMS or the estrus cycle (Fig. 5A, E). Bath application of E2 reduced EPSCs frequency in both control and NMS; however, the largest drop was observed during proestrus in NMS females (−0.63 versus −4.09 Hz for control and NMS, respectively). E2 reduced EPSC amplitude in ORX cells from control but not NMS (Fig. 5F, G–I).
Fig. 5. Neonatal maternal separation (NMS) reduces the excitatory postsynaptic currents (EPSC) recorded in GFP-labeled orexin neurons in response to natural and ovariectomy-induced changes in 17β-estradiol (E2) level.
A Comparison of EPSC recordings from orexin neurons between cells obtained from females during different phase of the estrus cycle and 2 weeks following ovariectomy (OVX); tissue slices originated from females raised under control conditions (top traces) or subjected to neonatal maternal separation (NMS, bottom traces; 3 h/day, postnatal days 3–12). B Photomicrograph illustrating GFP-labeled orexin neurons; the fornix (f) is shown as a landmark. C Population data of EPSC frequencies recorded during three distinct phases of the estrus cycle and following OVX. D Baseline E2 values from Fig. 2A measured in each stage are reported for comparison; values from NMS and controls were pooled since they are not statistically different. E Reports EPSC amplitudes. Note that since recordings in diestrus were performed only in controls (see F, G), data for this stage could not be compared between groups. Effect of E2 application (10 min; 100 nM) on EPSC F frequency and G amplitude in slices from control females. EPSC frequency and amplitude data from NMS females are reported in (H, I), respectively. Within histogram bars, the numbers in brackets indicate the number of replicates in each group. Data are expressed as the mean ± SEM. Post hoc pairwise comparisons were performed only when warranted by ANOVA. †Significantly different from corresponding control value at P ≤ 0.05. *Indicates a value statistically different from corresponding proestrus value at P < 0.05.
Discussion
Puberty and cyclic fluctuations in ovarian hormones are normal physiological processes but in a subpopulation of women, these events contribute to the onset and cyclic exacerbation of PD43–45. Thus, elucidating how ovarian function affects respiratory manifestations of PD is of utmost importance to our understanding of the pathophysiology of this disorder. Early life adversities are a significant risk factor for PD and the sex-specific enhancement of the ventilatory response to CO2 inhalation in rats is an attractive model to address this question29. Here, we show that in NMS females endogenous release of E2 during CO2 inhalation is insufficient to maintain the ventilatory response within a normal range. These data support our main hypothesis and indicate that mature (functional) ovaries are necessary to observe an excessive ventilatory response to CO2 inhalation in NMS females. This, and the involvement of the ORX system in this process strengthens the model and our demonstration that NMS disrupts E2 regulation of ORX neurons point to a novel mechanism in the pathophysiology of PD in females.
Neonatal maternal separation affects E2 signaling regulating the response to CO2 inhalation
Progesterone and E2 both fluctuate across the estrus cycle. However, the largest NMS-related increase in CO2 response coincided with the peak in E2 (proestrus) and following OVX, restoring normal E2 levels alone was sufficient to reinstate an excessive ventilatory response in NMS rats. We, therefore, conclude that E2 plays a primary role in the enhanced response to CO2. NMS does not affect the cyclic changes in E2 or progesterone under basal conditions (Fig. 1C;46) but attenuates E2 release following CO2 exposure, especially during proestrus. The sympathetic system regulates ovarian E2 secretion47, and ovarian aromatase expression peaks during proestrus48. Since plasma E2 closely reflects brain levels49, such impairment in E2 signalling within the brain of NMS females is likely. The inability of NMS females to augment E2 in response to CO2 during proestrus suggests that NMS reduced E2 synthesis capacity and thus compromise the response to an acute challenge. The relationships between E2 levels and the intensity of the ventilatory response suggest that impairment of E2 signalling contributes to the abnormal respiratory phenotype of NMS females. Experiments performed on OVX females show that E2 can attenuate the excessive CO2 response of NMS females; however, higher levels are necessary.
Neonatal maternal separation augments ORX activation under basal conditions
Having previously shown that NMS does not affect the carotid body’s response to CO2 in male and female rats50, our investigation focused on central mechanisms regulating the ventilatory response to CO2. Orexin neurons project to key medullary areas regulating breathing, including those that generate respiratory rhythm and contribute to CO2 chemosensitivity9. The clinical evidence implicating ORX in PD is important11,51 and our results showing that NMS augments ORXA levels in the hypothalamus are consistent with clinical and preclinical data. A similar increase has been reported in males18 but since regulation of ORX neurons likely differs between sexes19,22, testing this effect in females was necessary. ORX synthesis is activity-dependent and highly plastic52. In light of the close relationship between the hypothalamo-pituitary adrenal (HPA) axis and the ORX system19,53 the enhancement of basal HPA activity commonly reported in animals and humans who experienced early life adversities could explain the higher ORXA level in hypothalamic extracts54–56. In adult rats, however, disruption of HPA axis function by NMS is significant only in males57,58. Thus, another mechanism should be considered to explain this result.
In control females, comparison of c-Fos expression between females experiencing high (proestrus) and low (OVX) E2 clearly supports an inhibitory action of estrogens on ORX neurons. Conversely, the high c-Fos/ORXA ratio observed in NMS females, regardless of the ovarian function, suggests a generally higher degree of basal activity and a reduced sensitivity to E2 and/or insufficient levels. This result therefore provides a plausible explanation for greater level of ORXA in hypothalamic extracts and the larger ventilatory response to CO2 inhalation. The latter interpretation is supported by fact that NMS augmented the c-Fos/ORXA ratio in PeF/DMH areas that, unlike the LH, regulate cardiorespiratory homeostasis37. Moreover, pre-treatment with SB334867 prevented NMS-related increase in the ventilatory response to CO2.
Neonatal maternal separation disrupts E2 regulation of ORX neurons
ORX neurons are essential to several homeostatic functions. To the best of our knowledge, this is the first study documenting the impact of natural fluctuations in ovarian hormones (and OVX) on basic properties and excitatory synaptic inputs in females. While natural fluctuations in ovarian hormones have no impact on basic properties, the Vm and capacitance values obtained during the natural E2 nadir (metestrus) differs from those recorded following OVX. While OVX is the gold standard in preclinical research for evaluating gonadal hormone effects in females59, these results remind us that the changes induced by OVX may be more complex than a simple reduction of circulating hormones. Keeping that limitation in mind, the opposing effects of OVX on Vm between NMS and controls nonetheless indicate that NMS affects the way ovarian hormones influence this important property of ORX neurons.
Orexin neurons are the target of multiple afferent signals form diverse origins10,60,61. The frequency and amplitude of spontaneous EPSC’s reflect the number and the strength of excitatory synaptic inputs acting on ORX neurons, respectively. E2 acts via both membrane and nuclear receptors and the results reported here provide valuable insights into the mechanisms by which endogenous E2 contributes to inhibition of ORX neurons. EPSC frequencies measured in controls were inversely related to basal plasma E2 levels associated with natural cyclic fluctuations or OVX; exogenous E2 elicited a similar decrease in frequency in the minutes that followed its application onto slices. This implies that both E2 receptor types could regulate the number of synapses converging onto ORX neurons. Conversely, the fact that only acute E2 reduced EPSCs amplitude suggests that regulation of synaptic strength by E2 signalling is rapid but transient.
E2 is generally known to promote dendritic spine formation, potentiate excitatory synaptic transmission, and reduce the efficacy of GABAergic inhibition62–65. In the cortex and the hippocampus, however, application of LY 3201 (a selective agonist of the nuclear receptor ERβ) can elicit an opposite response by reducing dendritic spines and increasing expression of glutamic acid decarboxylase (GAD)66. This increase in GAD expression, combined with a reduction in the expression of NMDA receptors shifts the balance between excitatory and inhibitory neurotransmission in favor of inhibition66. Together, these effects explain the anxiogenic and anxiolytic actions of ERα and ERβ, respectively67. Since E2 inhibits expression of ERs68, region-specific changes in the relative expression of ERα and ERβ likely contribute to the phase-dependent effects reported here. While NMS affects ERβ expression in the hippocampus of males69, its impact in females is yet to be tested.
At the system level, the CO2 responses measured in controls indicate that as E2 declines across the cycle, the increased activation of ORX cells is dampened to prevent excessive hyperpnoea. Obviously, this mechanism is not fully functional in NMS females. Regulation of ORX neurons is a complex process that involves an important local network of neurons and astrocytes60 but obviously, NMS reduces E2’s actions on these cells. In fact, the CO2 response following E2 replacement in OVX NMS females suggests that depending on the concentration administered, E2 may have excitatory or inhibitory effects. Interestingly, PD is rare following menopause but E2 replacement therapy has been linked with the development of panic attacks in some patients70.
Limitations and conclusion
Inadequate modeling of human disease hinders translation of basic knowledge into effective treatment for human21. While our study shows that NMS closely reproduces developmental and cyclic changes in the respiratory manifestations of PD and enhancement of ORX modulation, we must keep in mind that animal research cannot reproduce the complex psychosocial reality often associated with PD. Furthermore, the estrus cycle in rodents is not equivalent to the menstrual cycle in humans59. That being said, NMS nonetheless meets key criteria expected from an animal model, including time-dependent and sex-specific effects on respiration20,71. The results reported here, therefore, offer valuable insights into the basic mechanism in this neurological disorder affecting female rats. Our demonstration that NMS disrupts the inhibitory actions of E2 on respiratory control are significant as they offers new avenues to alleviate PD.
Supplementary information
Acknowledgements
L.T.L. was supported by National Council for Scientific and Technological Development CNPq–Brazil (206239/2014-9-PDE) and an operating grant from the Canadian Institutes of Health Research (MOP 133686 to R.K. and F.B.) and the Fondation de l’Institut Universitaire en Cardiologie et Pneumologie de Québec (R.K.). The authors acknowledge the technical support of Dr. R. Gulemetova, Dr. Olivier Pothier-Piccinin, Agathe Bernet, and Anabel Buteau-Poulin in this research. We also acknowledge the generous intellectual contributions and guidance offered by Dr. G. Drolet.
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Luana Tenorio-Lopes, Stéphanie Fournier
Supplementary information
Supplementary Information accompanies this paper at (10.1038/s41398-020-01076-x).
References
- 1.Grassi M, et al. Are respiratory abnormalities specific for panic disorder? A meta-analysis. Neuropsychobiology. 2014;70:52–60. doi: 10.1159/000364830. [DOI] [PubMed] [Google Scholar]
- 2.Su VY-F, et al. Sleep apnea and risk of panic disorder. Ann. Fam. Med. 2015;13:325–330. doi: 10.1370/afm.1815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Freire RC, et al. Clinical features of respiratory and nocturnal panic disorder subtypes. Psychiatry Res. 2007;152:287–291. doi: 10.1016/j.psychres.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 4.Klein DF. False suffocation alarms, spontaneous panics, and related conditions. An integrative hypothesis. Arch. Gen. Psychiatry. 1993;50:306–317. doi: 10.1001/archpsyc.1993.01820160076009. [DOI] [PubMed] [Google Scholar]
- 5.Vollmer LL, Strawn JR, Sah R. Acid-base dysregulation and chemosensory mechanisms in panic disorder: a translational update. Transl. Psychiatry. 2015;5:e572. doi: 10.1038/tp.2015.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coryell W, Pine D, Fyer A, Klein D. Anxiety responses to CO2 inhalation in subjects at high-risk for panic disorder. J. Affect Disord. 2006;92:63–70. doi: 10.1016/j.jad.2005.12.045. [DOI] [PubMed] [Google Scholar]
- 7.Gorman JM, et al. Anxiogenic effects of CO2 and hyperventilation in patients with panic disorder. Am. J. Psychiatry. 1994;151:547–553. doi: 10.1176/ajp.151.4.547. [DOI] [PubMed] [Google Scholar]
- 8.Carrive, P. & Kuwaki, T. in Current Topics in Behavioral Neurosciences (eds Lawrence, A. J., & de Lecea, L.), vol. 33, 157–196 (Springer, 2017). [DOI] [PubMed]
- 9.Gestreau C, Bevengut M, Dutschmann M. The dual role of the orexin/hypocretin system in modulating wakefulness and respiratory drive. Curr. Opin. Pulm. Med. 2008;14:512–518. doi: 10.1097/MCP.0b013e32831311d3. [DOI] [PubMed] [Google Scholar]
- 10.Li A, Nattie EE. Orexin, cardio-respiratory function and hypertension. Front. Neurosci. 2014;8:22. doi: 10.3389/fnins.2014.00022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Johnson PL, et al. A key role for orexin in panic anxiety. Nat. Med. 2010;16:111–115. doi: 10.1038/nm.2075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Johnson PL, et al. Orexin 1 and 2 receptor involvement in CO2‐induced panic‐associated behavior and autonomic responses. Depress Anxiety. 2015;32:671–683. doi: 10.1002/da.22403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Johnson PL, et al. Activation of the orexin 1 receptor is a critical component of CO2-mediated anxiety and hypertension but not bradycardia. Neuropsychopharmacology. 2012;37:1911–1922. doi: 10.1038/npp.2012.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Asselmann E, et al. Assessing the interplay of childhood adversities with more recent stressful life events and conditions in predicting panic pathology among adults from the general population. J. Affect Disord. 2018;225:715–722. doi: 10.1016/j.jad.2017.08.050. [DOI] [PubMed] [Google Scholar]
- 15.Battaglia M, Ogliari A, D’Amato F, Kinkead R. Early-life risk factors for panic and separation anxiety disorder: insights and outstanding questions arising from human and animal studies of CO2 sensitivity. Neurosci. Biobehav. Rev. 2014;46:455–464. doi: 10.1016/j.neubiorev.2014.04.005. [DOI] [PubMed] [Google Scholar]
- 16.Ogliari A, et al. The relationships between adverse events, early antecedents, and carbon dioxide reactivity as an intermediate phenotype of panic disorder: a general population study. Psychother. Psychosom. 2010;79:48–55. doi: 10.1159/000259417. [DOI] [PubMed] [Google Scholar]
- 17.Sargin D. The role of the orexin system in stress response. Neuropharmacology. 2019;154:68–78. doi: 10.1016/j.neuropharm.2018.09.034. [DOI] [PubMed] [Google Scholar]
- 18.Feng P, Vurbic D, Wu Z, Strohl KP. Brain orexins and wake regulation in rats exposed to maternal deprivation. Brain Res. 2007;1154:163–172. doi: 10.1016/j.brainres.2007.03.077. [DOI] [PubMed] [Google Scholar]
- 19.Grafe LA, Bhatnagar S. Orexins and stress. Front. Neuroendocrinol. 2018;51:132–145. doi: 10.1016/j.yfrne.2018.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schenberg LC. Towards a translational model of panic attack. Psychol. Neurosci. 2010;3:9–37. doi: 10.3922/j.psns.2010.1.003. [DOI] [Google Scholar]
- 21.Perry CJ, Lawrence AJ. Hurdles in Basic Science Translation. Front Pharm. 2017;8:478–478. doi: 10.3389/fphar.2017.00478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grafe LA, Bhatnagar S. The contribution of orexins to sex differences in the stress response. Brain Res. 2018;1731:145893. doi: 10.1016/j.brainres.2018.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Beery AK, Zucker I. Sex bias in neuroscience and biomedical research. Neurosci. Biobehav Rev. 2011;35:565–572. doi: 10.1016/j.neubiorev.2010.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nillni YI, Pineles SL, Rohan KJ, Zvolensky MJ, Rasmusson AM. The influence of the menstrual cycle on reactivity to a CO2 challenge among women with and without premenstrual symptoms. Cogn. Behav. Ther. 2017;46:239–249. doi: 10.1080/16506073.2016.1236286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Reardon LE, Leen-Feldner EW, Hayward C. A critical review of the empirical literature on the relation between anxiety and puberty. Clin. Psychol. Rev. 2009;29:1–23. doi: 10.1016/j.cpr.2008.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nillni YI, Toufexis DJ, Rohan KJ. Anxiety sensitivity, the menstrual cycle, and panic disorder: a putative neuroendocrine and psychological interaction. Clin. Psychol. Rev. 2011;31:1183–1191. doi: 10.1016/j.cpr.2011.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Russell SH, et al. Orexin A interactions in the hypothalamo-pituitary gonadal axis. Endocrinology. 2001;142:5294–5302. doi: 10.1210/endo.142.12.8558. [DOI] [PubMed] [Google Scholar]
- 28.El‐Sedeek M, Korish AA, Deef MM. Plasma orexin‐A levels in postmenopausal women: possible interaction with estrogen and correlation with cardiovascular risk status. BJOG. 2010;117:488–492. doi: 10.1111/j.1471-0528.2009.02474.x. [DOI] [PubMed] [Google Scholar]
- 29.Genest SE, Gulemetova R, Laforest S, Drolet G, Kinkead R. Neonatal maternal separation induces sex-specific augmentation of the hypercapnic ventilatory response in awake rat. J. Appl Physiol. 2007;102:1416–1421. doi: 10.1152/japplphysiol.00454.2006. [DOI] [PubMed] [Google Scholar]
- 30.Tenorio-Lopes L, et al. Neonatal maternal separation opposes the facilitatory effect of castration on the respiratory response to hypercapnia of the adult male rat: Evidence for the involvement of the medial amygdala. J. Neuroendocrinol. 2017;29:e12550–e12550. doi: 10.1111/jne.12550. [DOI] [PubMed] [Google Scholar]
- 31.Leibold NK, et al. Carbon dioxide inhalation as a human experimental model of panic: the relationship between emotions and cardiovascular physiology. Biol. Psychol. 2013;94:331–340. doi: 10.1016/j.biopsycho.2013.06.004. [DOI] [PubMed] [Google Scholar]
- 32.Leibold NK, et al. CO2 exposure as translational cross-species experimental model for panic. Transl. Psychiatry. 2016;6:e885–e885. doi: 10.1038/tp.2016.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pierce AN, Ryals JM, Wang R, Christianson JA. Vaginal hypersensitivity and hypothalamic–pituitary–adrenal axis dysfunction as a result of neonatal maternal separation in female mice. Neuroscience. 2014;263:216–230. doi: 10.1016/j.neuroscience.2014.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fournier S, Gulemetova R, Baldy C, Joseph V, Kinkead R. Neonatal stress affects the aging trajectory of female rats on the endocrine, temperature, and ventilatory responses to hypoxia. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2015;308:R659–R667. doi: 10.1152/ajpregu.00418.2014. [DOI] [PubMed] [Google Scholar]
- 35.Zhang W, Zhang N, Sakurai T, Kuwaki T. Orexin neurons in the hypothalamus mediate cardiorespiratory responses induced by disinhibition of the amygdala and bed nucleus of the stria terminalis. Brain Res. 2009;1262:25–37. doi: 10.1016/j.brainres.2009.01.022. [DOI] [PubMed] [Google Scholar]
- 36.Harris GC, Wimmer M, Aston-Jones G. A role for lateral hypothalamic orexin neurons in reward seeking. Nature. 2005;437:556–559. doi: 10.1038/nature04071. [DOI] [PubMed] [Google Scholar]
- 37.Sunanaga J, Deng B-S, Zhang W, Kanmura Y, Kuwaki T. CO2 activates orexin-containing neurons in mice. Respiratory Physiol. Neurobiol. 2009;166:184–186. doi: 10.1016/j.resp.2009.03.006. [DOI] [PubMed] [Google Scholar]
- 38.Oberlander JG, Woolley CS. 17β-Estradiol acutely potentiates glutamatergic synaptic transmission in the hippocampus through distinct mechanisms in males and females. J. Neurosci. 2017;37:12314–12327. doi: 10.1523/JNEUROSCI.3011-17.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fournier S, et al. Distinct dampening effects of progesterone on the activity of nucleus tractus solitarus neurons in rat pups. Exp. Physiol. 2019;104:463–468. doi: 10.1113/EP087461. [DOI] [PubMed] [Google Scholar]
- 40.Baldy C, Chamberland S, Fournier S, Kinkead R. Sex-specific consequences of neonatal stress on cardio-respiratory inhibition following laryngeal stimulation in rat pups. eNeuro. 2017;4:ENEURO.0393-17.2017. doi: 10.1523/ENEURO.0393-17.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fournier S, et al. Gestational stress promotes pathological apneas and sex-specific disruption of respiratory control development in newborn rat. J. Neurosci. 2013;33:563–573. doi: 10.1523/JNEUROSCI.1214-12.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Putnam, R. W., Conrad, S. C., Gdovin, M. J., Erlichman, J. S. & Leiter, J. C. Neonatal maturation of the hypercapnic ventilatory response and central neural CO2 chemosensitivity. Respir. Physiol. Neurobiol. 149, 165–179 (2005). [DOI] [PMC free article] [PubMed]
- 43.Reed V, Wittchen HU. DSM-IV panic attacks and panic disorder in a community sample of adolescents and young adults: how specific are panic attacks? J. Psychiatr. Res. 1998;32:335–345. doi: 10.1016/S0022-3956(98)00014-4. [DOI] [PubMed] [Google Scholar]
- 44.Lovick TA. Sex determinants of experimental panic attacks. Neurosci. Biobehav Rev. 2014;46P3:465–471. doi: 10.1016/j.neubiorev.2014.03.006. [DOI] [PubMed] [Google Scholar]
- 45.Gorman JM, et al. Physiological changes during carbon dioxide inhalation in patients with panic disorder, major depression, and premenstrual dysphoric disorder: evidence for a central fear mechanism. Arch. Gen. Psychiatry. 2001;58:125–131. doi: 10.1001/archpsyc.58.2.125. [DOI] [PubMed] [Google Scholar]
- 46.Dumont FS, Biancardi V, Kinkead R. Hypercapnic ventilatory response of anesthetized female rats subjected to neonatal maternal separation: Insight into the origins of panic attacks? Respiratory Physiol. Neurobiol. 2011;175:288–295. doi: 10.1016/j.resp.2010.12.004. [DOI] [PubMed] [Google Scholar]
- 47.Uchida S, Kagitani F. Neural mechanisms involved in the noxious physical stress-induced inhibition of ovarian estradiol secretion. Anat. Rec. 2019;302:904–911. doi: 10.1002/ar.24078. [DOI] [PubMed] [Google Scholar]
- 48.Kobayashi H, Yoshida S, Sun Y-J, Shirasawa N, Naito A. Changes of gastric aromatase and portal venous 17β-estradiol during the postnatal development and estrus cycle in female rats. Endocrine. 2014;46:605–614. doi: 10.1007/s12020-013-0096-7. [DOI] [PubMed] [Google Scholar]
- 49.Sze Y, Gill AC, Brunton PJ. Sex-dependent changes in neuroactive steroid concentrations in the rat brain following acute swim stress. J. Neuroendocrinol. 2018;30:e12644. doi: 10.1111/jne.12644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Soliz, J., Tam, R. & Kinkead, R. Neonatal maternal separation augments carotid body response to hypoxia in adult males but not female rats. Front Physiol.7, 432 (2016). [DOI] [PMC free article] [PubMed]
- 51.Flores Á, Saravia R, Maldonado R, Berrendero F. Orexins and fear: implications for the treatment of anxiety disorders. Trends Neurosci. 2015;38:550–559. doi: 10.1016/j.tins.2015.06.005. [DOI] [PubMed] [Google Scholar]
- 52.Gao X-B, Wang AH. Experience-dependent plasticity in hypocretin/orexin neurones: re-setting arousal threshold. Acta Physiologica. 2010;198:251–262. doi: 10.1111/j.1748-1716.2009.02047.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Winsky-Sommerer R, et al. Interaction between the corticotropin-releasing factor system and hypocretins (orexins): a novel circuit mediating stress response. J. Neurosci. 2004;24:11439–11448. doi: 10.1523/JNEUROSCI.3459-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chintamaneni K, Bruder ED, Raff H. Programming of the hypothalamic-pituitary-adrenal axis by neonatal intermittent hypoxia: effects on adult male ACTH and corticosterone responses are stress specific. Endocrinology. 2014;155:1763–1770. doi: 10.1210/en.2013-1736. [DOI] [PubMed] [Google Scholar]
- 55.Weaver IC, et al. Epigenetic programming by maternal behavior. Nat. Neurosci. 2004;7:847–854. doi: 10.1038/nn1276. [DOI] [PubMed] [Google Scholar]
- 56.de Kloet ER, Sibug RM, Helmerhorst FM, Schmidt M. Stress, genes and the mechanism of programming the brain for later life. Neurosci. Biobehav Rev. 2005;29:271–281. doi: 10.1016/j.neubiorev.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 57.Wigger A, Neumann ID. Periodic maternal deprivation induces gender-dependent alterations in behavioral and neuroendocrine responses to emotional stress in adult rats. Physiol. Behav. 1999;66:293–302. doi: 10.1016/S0031-9384(98)00300-X. [DOI] [PubMed] [Google Scholar]
- 58.Genest SE, Gulemetova R, Laforest S, Drolet G, Kinkead R. Neonatal maternal separation and sex-specific plasticity of the hypoxic ventilatory response in awake rat. J. Physiol. 2004;554:543–557. doi: 10.1113/jphysiol.2003.052894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Koebele SV, Bimonte-Nelson HA. Modeling menopause: The utility of rodents in translational behavioral endocrinology research. Maturitas. 2016;87:5–17. doi: 10.1016/j.maturitas.2016.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Burt J, Alberto CO, Parsons MP, Hirasawa M. Local network regulation of orexin neurons in the lateral hypothalamus. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2011;301:R572–R580. doi: 10.1152/ajpregu.00674.2010. [DOI] [PubMed] [Google Scholar]
- 61.Sakurai T. The role of orexin in motivated behaviours. Nat. Rev. Neurosci. 2014;15:719–731. doi: 10.1038/nrn3837. [DOI] [PubMed] [Google Scholar]
- 62.Woolley CS. Acute effects of estrogen on neuronal physiology. Annu. Rev. Pharmacol. Toxicol. 2007;47:657–680. doi: 10.1146/annurev.pharmtox.47.120505.105219. [DOI] [PubMed] [Google Scholar]
- 63.Woolley C, McEwen B. Estradiol mediates fluctuation in hippocampal synapse density during the estrous cycle in the adult rat. J. Neurosci. 1992;12:2549–2554. doi: 10.1523/JNEUROSCI.12-07-02549.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Smejkalova T, Woolley CS. Estradiol acutely potentiates hippocampal excitatory synaptic transmission through a presynaptic mechanism. J. Neurosci. 2010;30:16137–16148. doi: 10.1523/JNEUROSCI.4161-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mukherjee J, et al. Estradiol modulates the efficacy of synaptic inhibition by decreasing the dwell time of GABAA receptors at inhibitory synapses. Proc. Natl Acad. Sci. USA. 2017;114:11763–11768. doi: 10.1073/pnas.1705075114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tan X-j, et al. Reduction of dendritic spines and elevation of GABAergic signaling in the brains of mice treated with an estrogen receptor β ligand. Proc. Natl Acad. Sci. USA. 2012;109:1708–1712. doi: 10.1073/pnas.1121162109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Walf AA, Frye CA. A review and update of mechanisms of estrogen in the hippocampus and amygdala for anxiety and depression behavior. Neuropsychopharmacology. 2006;31:1097–1111. doi: 10.1038/sj.npp.1301067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Murata T, Narita K, Ichimaru T. Rat Uterine Oxytocin Receptor and Estrogen Receptor α and β mRNA Levels are Regulated by Estrogen Through Multiple Estrogen Receptors. J. Reprod. Dev. 2014;60:55–61. doi: 10.1262/jrd.2012-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wang H, Meyer K, Korz V. Stress induced hippocampal mineralocorticoid and estrogen receptor β gene expression and long-term potentiation in male adult rats is sensitive to early-life stress experience. Psychoneuroendocrinology. 2013;38:250–262. doi: 10.1016/j.psyneuen.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 70.Kunte H, Harms L, Plag J, Hellweg R, Kronenberg G. Acute onset of panic attacks after transdermal estrogen replacement. Gen. Hospital Psychiatry. 2014;36:e7. doi: 10.1016/j.genhosppsych.2014.05.009. [DOI] [PubMed] [Google Scholar]
- 71.Moreira F, et al. Modeling panic disorder in rodents. Cell Tissue Res. 2013;354:1–7. doi: 10.1007/s00441-013-1610-1. [DOI] [PubMed] [Google Scholar]
- 72.Paxinos, G. & Watson, C. The rat brain in stereotaxic coordinates. 4th Edition edn. (Academic Press, San Diego, 1998).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.