Abstract
The management of both-column fractures of the acetabulum is challenging for the orthopaedic surgeon. Operative treatment is usually recommended in this particular fracture pattern, as residual joint surface displacement has been shown to increase local contact stress, drastically leading to rapid cartilage destruction. In this review, we present an overview of operative steps and surgical technique for both-column acetabular fracture reconstruction. Therefore, we demonstrate how correct understanding of fracture morphology and displacement, preoperative preparation, including choice of approach and patient positioning, reduction strategies, and programmed sequential fixation, starting from superior fracture lines on the anterior acetabular column and ending on the posterior components of this fracture type, may provide satisfactory outcomes in this difficult acetabular fracture pattern.
Keywords: Both-column acetabular fracture, Acetabular fracture, Hip fracture, Approach to the acetabulum
1. Introduction
The management of displaced fractures of the acetabulum is challenging for the orthopaedic surgeon potentially leading to devastating complications, such as posttraumatic osteoarthritis and avascular necrosis of the femoral head, among others. Resultant osteoarthritis occurs in up to 20% of the patients and is the most common long-term complication.1,2 The type of fracture, damage to the femoral head, associated injuries, and multiple comorbidities have been shown to have negative effects on the longevity of the affected joint and the quality of life of the patient.1 In addition, the timing of the operative management, choice of surgical approach, and the quality of reduction are among the most surgeon-related controllable factors influencing the functional outcome.1
According to Letournel, acetabular fractures were divided into elementary and associated fracture patterns.3 The both-column associated fracture type is a relatively common injury, observed in approximately 22.3% of the cases.2 It is characterized by the complete discontinuity of the acetabular articular surface from the rest of the axial skeleton. It has been shown that both-column fractures of the acetabulum result from high-energy trauma in 87.4%, with 61.5% of patients injured in road traffic accidents.4 It is assumed to result from lateral compressive forces transmitted though the femoral head to the joint cavity, producing medialization of the articular joint fragments and rotation of both acetabular columns.5 Associated skeletal and non-skeletal lesions are frequent, with an increased incidence of injury to the bladder, kidney, liver, spleen, and pelvic vessels.6
Operative treatment is usually recommended in this particular fracture pattern, as residual joint surface displacement has been shown to increase local contact stress, drastically leading to rapid cartilage destruction.7 Historically the concept of secondary congruence, characterized by an extra-anatomical orientation of all articular fragments around the femoral head, has been used for selected cases of both-column acetabular fractures.8 However, in a biomechanical study it was found that even a perfect secondary congruence positioning is less than ideal, creating a larger acetabulum with increased pressures in the dome region.7 In a retrospective cohort study with 115 patients, anatomic articular reconstruction (considered as less than 1.0-mm step-off) was significantly associated with better clinical outcome.9 Conversely, initial displacement of more than 10.0-mm and initial intra-articular fragments were associated with worse outcome.9
Herein, we present an overview of operative steps and surgical technique for both-column acetabular fracture reconstruction. We demonstrate how correct understanding of fracture morphology and displacement, preoperative preparation, including choice of approach and patient positioning, reduction strategies, and programmed sequential fixation may provide satisfactory outcomes in this difficult acetabular fracture pattern.
2. Understanding the fracture morphology and displacements
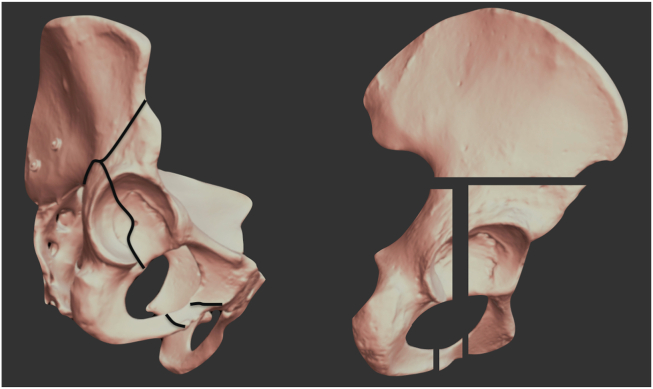
A full understanding of the fracture morphology is essential in decision making.10 Regardless of the degree of displacement and the severity of the injury, both-column fractures normally present two main converging fracture lines, determining a T- or Y-shaped fracture morphology (Fig. 1).5,10 Secondary fracture lines are common and can be observed in association, including a fracture line that separates the posterior wall of the acetabulum from the posterior column and another that separates a small medial fragment of the acetabular roof from the anterior column. Using 3-dimensional reconstruction images from 71 both-column fractures, Yang et al. found that 39% of the fractures involved the posterior column traversing the posterior wall.10 Moreover, these authors observed a high anterior column fracture in 62% cases, a low anterior column fracture in 66% cases, and a posterior column fracture without posterior wall involvement in 59% cases.10
Fig. 1.
Pelvic plastic model. A, T-shaped pattern. In this fracture pattern, the proximal vertical fracture line generally exits between the ASIS∗ and the AIIS∗∗; B, Y-shaped pattern. In this fracture pattern, the proximal vertical fracture line can exit either between the ASIS and the iliac tuberosity (low anterior column fracture) or up in the iliac crest (high anterior column fracture). ∗ASIS (anterior superior iliac spine); ∗∗AIIS (anterior inferior iliac spine).
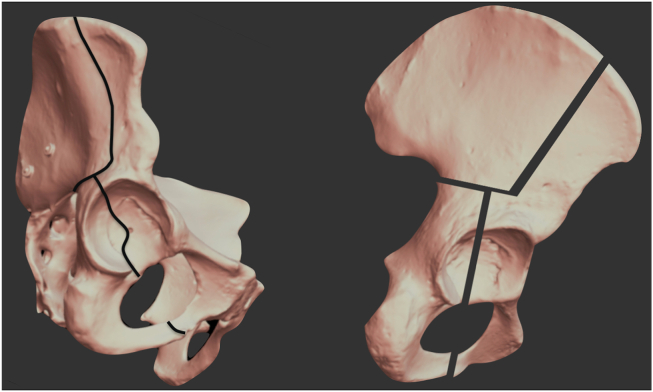
The first main fracture line divides the acetabulum vertically into anterior and posterior column fragments. Despite some variations, the obturator foramen is broken in one or two parts and the fracture line ascends to some part of the iliac wing. In the T-shaped pattern, the proximal vertical fracture line generally exits between the anterior superior iliac spine (ASIS) and the anterior inferior iliac spine (AIIS). Some other secondary fracture lines can be observed in the iliac bone, as well in the medial acetabular roof, which can be divided in two or more fragments. In the Y-shaped pattern, the proximal vertical fracture line can exit either between the ASIS and the iliac tuberosity (low anterior column fracture) or up in the iliac crest (high anterior column fracture). Yang et al. observed that most of major fracture lines entered in three directions resembling the Y-shaped pattern (Fig. 2).10 Sacroiliac (SI) joint involvement although uncommon can be observed in certain cases.
Fig. 2.
Y-shaped fracture types. A, Low anterior column fracture – the vertical fracture line exits between the ASIS and the iliac tuberosity; B, High anterior column fracture – the vertical fracture line exits up in the iliac crest. Note that there is also a secondary fracture line exiting between the ASIS and the iliac tuberosity. This pattern is also called H-shaped type; C, High anterior column fracture – the vertical fracture line exits up in the iliac crest. Observe that a secondary fracture line extends into the SI joint. We call this pattern X-shaped type.
The second main fracture line is either horizontally- or slightly oblique-oriented and reaches the vertical fracture line in the anterior column. The fracture line descends to the posterior column and separates the greater sciatic notch in two parts, superior and inferior.5,10 The majority of the posterior column fractures exits the upper part of the sciatic notch, with posterior wall involvement in nearly two fifths of cases (Fig. 3).10
Fig. 3.
3-D pelvic image demonstrating the posterior aspect of pelvis. Associated posterior wall (white arrowheads) is often a large, noncomminuted, nondisplaced or minimally anteriorly displaced fragment. It occurs in nearly two fifths of cases and is generally created by a pull-type mechanism. (courtesy Adrién Roa-Zoppi, MD)
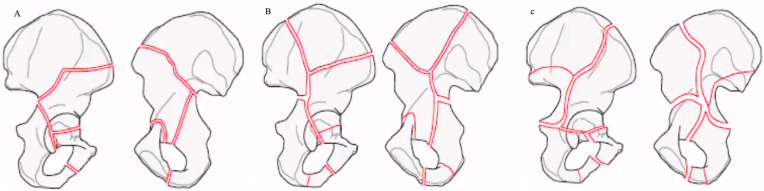
Fracture displacement is mainly determined both by the magnitude of the lateral compressive force applied to the greater trochanter and the position of the hip.5,11 With the hip in abduction and external rotation, the femoral head is medially displaced, directly striking on the anterior medial wall of the acetabulum and quadrilateral plate (Fig. 4). The anterior column is pushed medially and externally rotated, while the posterior column is also pushed medially, but internally rotated.5,11,12 The most superior triangular extension of the sciatic notch remains attached to the axial skeleton, projecting inferiorly and laterally from the sacroiliac joint. This spur is exposed when the fractured columns are medially displaced and is better observed in the obturator oblique radiographic view and the CT scan – so-called spur sign (Fig. 5).13 When present, the posterior wall fragment component is generally created by a pull-type mechanism and is often a large, noncomminuted, nondisplaced or minimally anteriorly displaced fragment.11,12,14
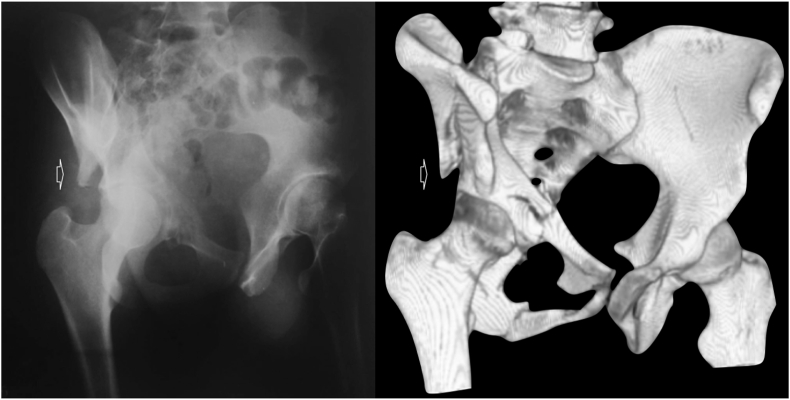
Fig. 4.
AP right hip radiograph. A lateral compressive force applied to the greater trochanter with the hip in slight abduction and external rotation displaces the acetabulum columns medially. The femoral head acts as a hammer, directly striking on the anterior medial wall of the acetabulum and quadrilateral plate.
Fig. 5.
The spur sign is considered pathognomonic of both-column fracture. It is better observed in the obturator oblique radiographic view and the CT scan.
Both the spur sign and the detachment of the entire acetabular articular surface from the axial skeleton are considered pathognomonic of both-column fracture.
3. Operative planning– patient positioning and choice of approach
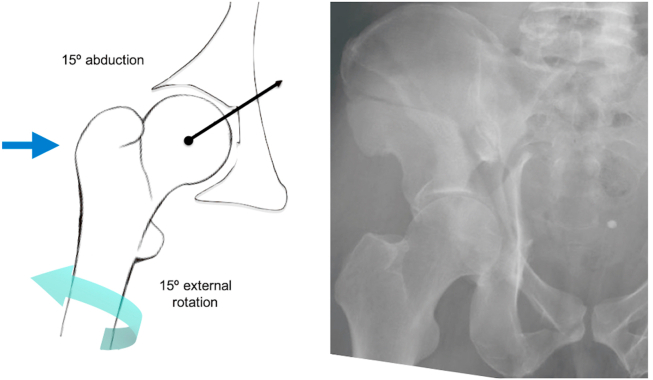
It is strongly advised to perform Judet radiographic views and computed tomography reconstructions of the pelvis on all patients before surgery. While planning the surgical approach, it is essential to perfectly understand orientation of major fracture lines and degree of displacement (Fig. 6). Preoperative 3D printed anatomical models may be a helpful resource to save time in acetabular fracture fixation, especially if a mirrored model based on the intact opposite hemi-pelvis is used for accurate plate contouring and positioning.15
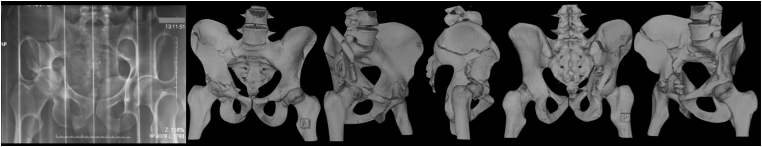
Fig. 6.
AP pelvis radiograph and 3D-CT reconstruction of the pelvis of a 35-year-old male who fell from approximately 8 m height. Images show a high anterior column pattern extending into the SI joint (X-type) associated with a displaced posterior wall acetabular fracture. Observe that posterior column component is minimally displaced.
Generally, the more dislocated column dictates both the choice of approach and patient positioning. The typical pattern of both-column fracture presents a comminuted anterior column fracture extending up to the iliac crest (high anterior column fracture) with a simple posterior column fracture.4 Therefore, we suggest start approaching the majority of both-column fractures through the anterior ilioinguinal approach.3 Advocates of this approach consider its advantages to be the wide access to the acetabulum, the muscle-sparing nature, the extensibility, and the historical familiarity of the pelvic surgeon with a highly stablished surgical technique.16,17 This approach allows exposure of the entire anterior column, the SI joint, the lateral ala of the ipsilateral sacrum, and the inner part of the posterior column.16,17 Patient is positioned supine on a radiolucent table and the fracture is checked with image intensifier in AP, obturator oblique, and iliac oblique views prior to surgical preparation and draping. We use routinely the OSI table in our practice which with the insertion of a distal femoral pin on the affected extremity, allows the application of intraoperatively skeletal traction facilitating closed fracture reduction. The C-arm must be positioned opposite the side of injury. A urinary catheter is inserted to guarantee emptying of the bladder. Normal preoperative procedures, such as antibiotic prophylaxis and trichotomy, should follow the guidelines of the infection control committee from the institution.
Alternative options are the modified Stoppa (anterior intrapelvic – AIP) approach and the pararectus approach.18,19 Both approaches present the advantage to facilitate the management of severely medial displaced fracture patterns involving the quadrilateral plate. In the case of both-column fractures, the AIP approach must be combined with lateral window of the ilioinguinal approach (so-called Olerud approach) to expose all fractures lines extending superiorly to the iliac crest, while the pararectus approach is a single-incision combining the advantages of the 2nd and 3rd windows of the ilioinguinal approach with the medial view of the AIP approach.18, 19, 20 Patient positioning and normal preoperative procedures are the same as for the ilioinguinal approach. Differently, the C-arm must be positioned on the same side as the injury. The iliofemoral approach with iliac crest osteotomy alone or in combination with the AIP can also give good direct exposure of the anterior column.
A complementary posterior Kocher-Langenbeck approach has been suggested when the posterior column component is hugely displaced and/or the surgeon cannot satisfactorily reduce it through an anterior approach.5,21 Although a combined anterior and posterior approach can be performed with the patient in a floppy lateral position, we prefer to begin supine with the ilioinguinal approach and whether necessary to reposition the patient prone for the posterior approach.22 The C-arm must be positioned opposite the side of injury. Normal preoperative procedures should follow the guidelines of the infection control committee from the institution.
The existence of associated both-column fracture with posterior wall involvement is not a prerequisite for a posterior approach (Fig. 7). Wang et al. demonstrated excellent to good clinical results after lag-screw fixation of posterior wall fractures through single ilioinguinal approach in cases of associated both-column fractures of the acetabulum.12 More recent data suggested that posterior wall fractures associated with both-column fractures can be successfully ignored if the posterior wall fragment is adequately attached to the acetabulum through the capsulolabral complex, the hip joint is congruent, and there is < 2.0-mm step-off and <3.0-mm gap.23
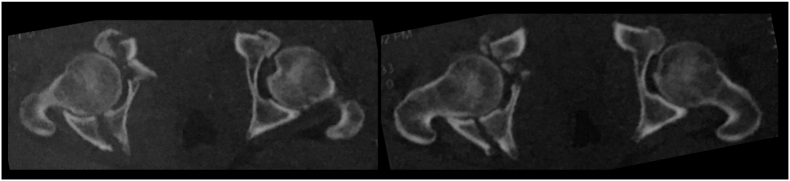
Fig. 7.
Axial tomographic cuts from the same patient revealing a complex fracture of the anterior component and an associated unique displaced posterior wall acetabular fracture. Note the low-anterior column acetabular fracture on the contralateral side.
The use of extensile approaches, such as the extended iliofemoral approach suggested by Pierannunzii et al., has been associated with more complications.5,24 In our hands, the extended iliofemoral approach is reserved for selected cases of delayed or malunited acetabular fracture reconstruction. In this situation, it may be helpful to debride the soft tissue scarring and remove fracture callus. Nevertheless, Giannoudis et al. concluded that only 17% of patients will require an extensile or combined approach.1
Although the majority of both-column acetabular fracture patterns can be treated successfully through a single approach, it is strongly recommended that the surgeon dealing with these fracture types be familiar with the different approaches to the acetabulum and be prepared to perform them during the same operative procedure.24 Of extreme importance, patient and/or relatives should be informed about the possibility of more than one surgical incision and the potential operative risks, such as iatrogenic nerve or vessel injury, nonanatomic fracture reduction, and articular hardware penetration.16,25
4. Sequence of reduction and fixation
As mentioned before, we prefer to use a radiolucent table, which allows better visualization of the posterior ring and permits free mobility of the entire lower limb, which facilitates intraoperative reduction maneuvers. In particular, it increases the exposure of both the lateral and medial windows of the ilioinguinal approach. The major disadvantage of using a radiolucent table is the need for manual traction, thus requiring a minimum of two or three assistants.16 The entire lower limb is then prepared and draped extending proximally to the subcostal region.
Before starting the operation, it is necessary to check if all pelvic set instruments and implants are available. Reduction should begin proximally in the iliac wing through the lateral window of the ilioinguinal approach. After careful elevation of the iliac muscle from the inner table, exposure of the entire iliac wing and SI joint allows identification of the upper part of the main vertical fracture line. Secondary fracture lines and small pieces of loose cortical bone from the inner table are usually present. Exposure is increased by placing a curved sharp Hohmann retractor on the lateral ala of the sacrum, taking care to not damage L5 nerve root, and a curved blunt Hohmann retractor medially to the pelvic brim into the greater sciatic notch, avoiding any neurovascular injury. This will allow direct visualization of the SI joint which can be disrupted with associated both column fractures. A constant triangular or quadrangular bone piece is always present in the iliac fossa close to the inferior part of the SI joint. Reduction of the superior part of the fracture should start with this key fragment as this restores the upper medial portion of the pelvic brim (Fig. 8). A 1.6-mm K-wire is used to temporarily hold the key fragment. Definitive fixation is performed with a 3.5-mm cortical lag-screw with or without a washer if the piece is large enough to do so. Then, the iliac crest is reduced using a pointed reduction clamp and temporarily stabilized with multiple 1.6-mm K-wires. A 3.5-mm drill bit is used to make several sliding holes in the crest of the ilium, and multiple 3.5-mm long cortical lag-screws are placed between the inner and outer tables of the ilium (Fig. 9). Final reduction of the iliac wing is checked both by direct vision and fluoroscopy before starting reduction of the anterior column component (Fig. 10).
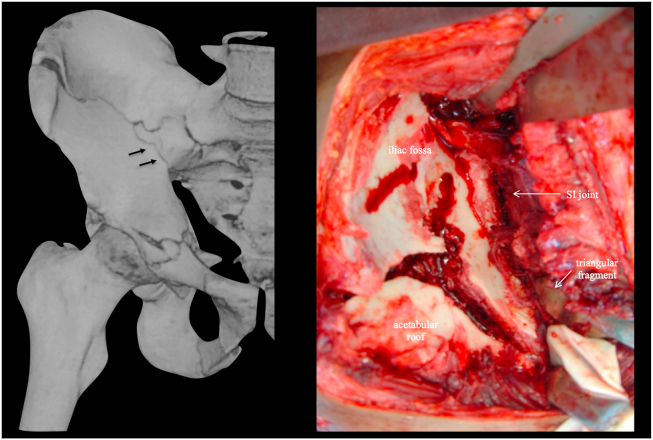
Fig. 8.
A constant triangular bone piece is always present in the iliac fossa close to the inferior part of the SI joint (left image, black arrows). Reduction of the superior part of the fracture should start with this key fragment as this restores the upper medial portion of the pelvic brim (right image).
Fig. 9.
Pelvic plastic model for demonstration purposes. Reduction should begin proximally in the iliac wing through the 1st window of the ilioinguinal approach. The key fragment is reduced first and temporarily secured with a 1.6-mm K-wire, then the iliac crest is reduced and fixed with multiple 3.5-mm long cortical lag-screws placed between the inner and outer tables of the ilium.
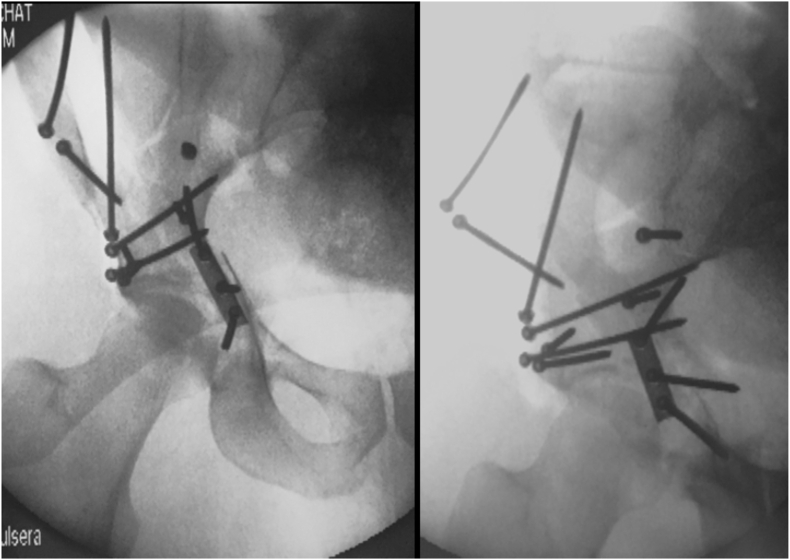
Fig. 10.
Intraoperative fluoroscopic images from the same patient presented in Fig. 6, Fig. 7. Reduction and fixation of the iliac wing using multiple 3.5-mm cortical screws. Additionally, a suprapectineal plate was used to fix the medial roof fragment.
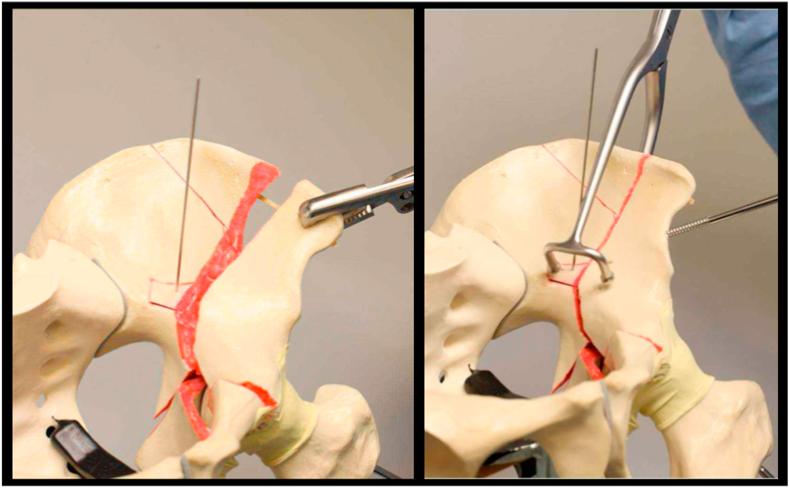
The anterior column is usually externally rotated and medialized, and keeping this fragment in an acceptable alignment can be challenging.5,11,12 Therefore, the surgeon must be aware of different reduction aids. The first step is to bring the femoral head to its normal position below the acetabular roof. A 5.0-mm Schanz pin is placed through a separate stab incision on the lateral aspect of the ipsilateral thigh into the femoral neck. Lateral traction is applied with a T-handle and femoral head lateralization is monitored using fluoroscopy. With femoral head reduced, malreduction can be corrected. In good quality bone application of a Farabeuf clamp helps manipulate and handling the anterior column through the lateral and middle windows of the ilioinguinal approach.26 A second reduction instrument, such as a 5.0-mm Schanz pin in a T-handle or a tong clamp, aids in the correction of the external rotation of the anterior column (Fig. 11).5,17 In addition, a pusher can be used to caudally displace the medial edge of the anterior column.17 Alternatively, if the AIP is being used a pusher is applied to laterally reduce the quadrilateral plate.18 Provisional fixation is achieved with multiple 1.6-mm K-wires and reduction is re-checked. A 3.5-mm drill bit is used to make several sliding holes from the anterior column to the iliac crest, and multiple 3.5-mm long cortical lag-screws are placed between the inner and outer tables of the ilium. A contoured 3.5-mm long reconstruction plate is positioned over the pelvic brim buttressing the most central part of anterior column component. At this time, no screw from the anterior column plate should invade the posterior column.17
Fig. 11.
Pelvic plastic model for demonstration purposes. Anterior column is usually externally rotated and medialized. A Farabeuf clamp helps manipulate and handling the anterior column through the 1st and 2nd windows of the ilioinguinal approach. Final reduction can be accomplished using a tong clamp and a Schanz pin. It is imperative that the femoral head is reduced under the acetabular roof.
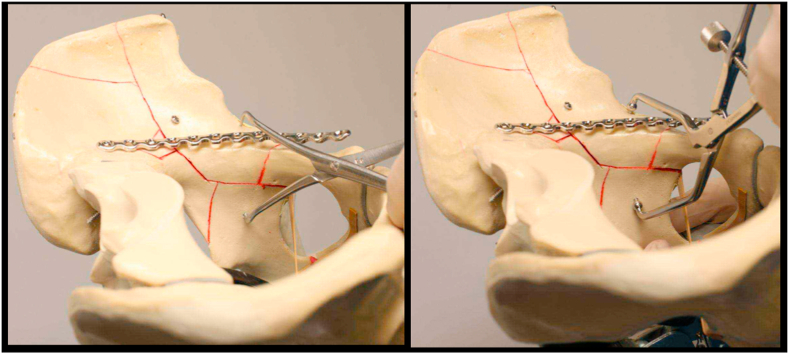
The next step is to reduce and fix the posterior column component, which includes great part of the quadrilateral plate. Normally, posterior column is medialized and internally rotated. Reduction maneuvers are slightly facilitated when surgeon works through both the lateral and middle windows of the ilioinguinal approach. Asymmetrical Matta clamps, Weber pointed clamps, colinear clamp, and bone hooks are of special value to aid reduction, particularly when using the medial window (Fig. 12). Care must be taken to prevent bone hook disengagement during reduction maneuvers, especially when being used via the middle window. The femoral head must be reduced under the acetabular roof, thus lateral traction must be continued. Provisional fixation is achieved with multiple 1.6-mm K-wires and reduction is re-checked. At least two 3.5-mm long cortical lag-screws are placed through or outside the pelvic brim buttress plate to hold the posterior column to the anterior column.17
Fig. 12.
Pelvic plastic model for demonstration purposes. Posterior column and quadrilateral plate are reduced through both the 1st and 2nd windows of the ilioinguinal approach Weber pointed clamps and asymmetrical Matta clamps are of special value to aid reduction. Fixation is accomplished using long cortical lag-screws placed through or outside the pelvic brim buttress plate.
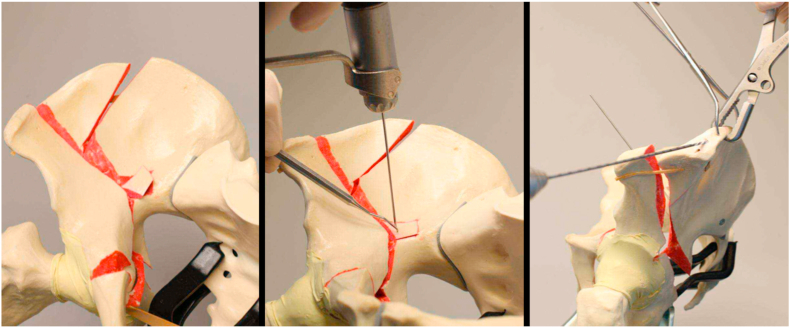
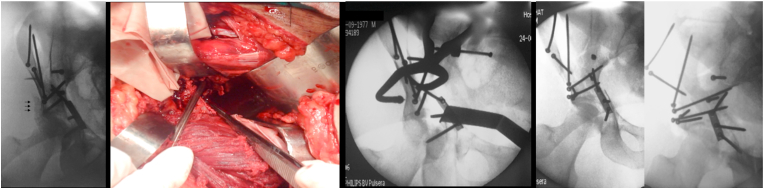
When present, a concomitant posterior wall fracture should be fixed if there is > 2.0-mm step-off and/or >3.0-mm gap.23 Inlet-obturator oblique view (Leeds view) is a useful imaging for fracture reduction and fixation.13 Reduction is achieved through additional dissection on the outer table of the ilium and the use of asymmetric long-arm pelvic clamps.27 Posterior wall fragment is provisionally stabilized with 1.6-mm K-wires. Definitive fixation is performed with 3.5-mm long cortical lag-screws placed from the internal iliac fossa to the posterior wall (Fig. 13).12,13,17 Alternatively, lag screws can be placed from the outer surface heading towards the quadrilateral surface.
Fig. 13.
Reduction of the posterior wall fragment is achieved through additional dissection on the outer table of the ilium. Intraoperative images from the same patient presented in Fig. 6, Fig. 7, Fig. 10. Note the posterior wall fragment completely displaced (black arrows). The use of an asymmetric long-arm pelvic clamp through the 2nd window of the ilioinguinal approach allows anatomic reduction of the posterior wall fragment. Fixation is done with 3.5-mm long cortical lag-screws placed from the inner iliac fossa to the posterior wall.
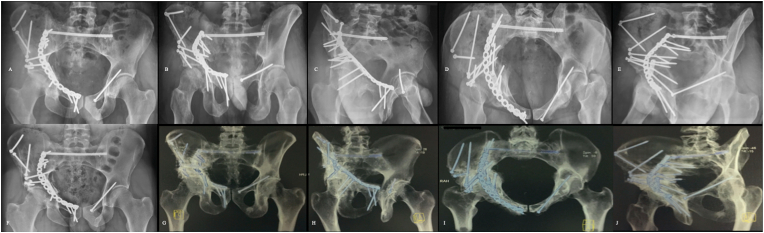
Finally, SI joint involvement is rare, but when present should be managed accordingly. As both-column fractures result from lateral compressive forces, SI joint injury is generally a stable Young and Burgess LC-I type not needing fixation.28 However, sometimes a horizontally unstable Young and Burgess LC-II type is observed.28 Rarely there is a significant widening of the SI joint indicative of an APC-type injury. In this case, we prefer to percutaneously stabilize S1 or S2 with a long SI screw or a transacral screw (Fig. 14). Plating across the SI joint is also an option through the already exposed lateral window. A significant SI joint injury must be appreciated ideally in the pre-operative or intraoperative period and reduced and stabilized.
Fig. 14.
Radiographic and tomographic images from the same patient presented in Fig. 6, Fig. 7, Fig. 10, Fig. 13. A to E: Immediate post-operative AP pelvis, outlet view, obturator oblique, inlet view, and iliac oblique radiographs. Observe the anatomic reduction of the right hemipelvis and the acetabulum. SI joint was fixed with a 7.0-mm cannulated screw in S1. The left acetabulum fracture (infra-tectal simple transverse fracture) was fixed with a percutaneous retrograde 3.5-mm long cortical screw; F to J: AP pelvis and 3D reconstruction tomographic outlet, obturator oblique, inlet, and iliac oblique views after 3-year follow-up. No signs of osteoarthritis, heterotopic ossification, or vascular damage to the femoral heads.
5. Closure
After checking final reduction and implant positioning, the wound is irrigated with saline solution and hemostasis is reviewed. One or two drains can be inserted, one in the space of Retzius (medial window) and one in the iliac fossa (lateral window) of the ilioinguinal approach. The inguinal canal, external abdominal fascia, and inguinal ligament are closed with nonabsorbable sutures. Then the wound is closed in layers with absorbable sutures. The skin is closed with nonabsorbable sutures using a modified Donatti suture.
Although not discussed in this overview of operative steps and surgical technique for both-column acetabular fracture reconstruction, vigorous rehabilitation is an integral part of patient recovery.
6. Conclusion
The management of both-column fractures of the acetabulum is challenging for the orthopaedic surgeon. Correct understanding of fracture morphology and displacements, preoperative preparation, including choice of approach and patient positioning, reduction strategies, and programmed sequential fixation may provide satisfactory outcomes in this difficult acetabular fracture pattern.
Funding
Nil.
Declaration of competing interest
None.
Acknowledgements
Nil.
References
- 1.Giannoudis P.V., Grotz M.R.W., Papakostidis C., Dinopoulos H. Operative treatment of displaced fractures of the acetabulum. A meta-analysis. J Bone Joint Surg Br. 2005;87(1):2–9. [PubMed] [Google Scholar]
- 2.Kelly J., Ladurner A., Rickman M. Surgical management of acetabular fractures – a contemporary literature review. Injury. 2020;S0020–1383(20):30525–30528. doi: 10.1016/j.injury.2020.06.016. [DOI] [PubMed] [Google Scholar]
- 3.Letournel E. Acetabulum fractures: classification and management. Clin Orthop Relat Res. 1980;(151):81–106. [PubMed] [Google Scholar]
- 4.Gänsslen A., Frink M., Hildebrand F., Krettek C. Both column fractures of the acetabulum: epidemiology, operative management and long-term-results. Acta Chir Orthop Traumatol Cech. 2012;79(2):107–113. [PubMed] [Google Scholar]
- 5.Pierannunzii L., Fischer F., Tagliabue L., Calori G.M., D’Imporzano M. Acetabular both-column fractures: essential of operative management. Injury. 2010;41(11):1145–1149. doi: 10.1016/j.injury.2010.08.011. [DOI] [PubMed] [Google Scholar]
- 6.Porter S.E., Schroeder A.C., Dzugan S.S., Graves M.L., Zhang L., Russell G.V. Acetabular fracture patterns and their associated injuries. J Orthop Trauma. 2008;22(3):165–170. doi: 10.1097/BOT.0b013e318165918b. [DOI] [PubMed] [Google Scholar]
- 7.Levine R.G., Renard R., Behrens F.F., Tornetta P., 3rd Biomechanical consequences of secondary congruence after both-column acetabular fracture. J Orthop Trauma. 2002;16(2):87–91. doi: 10.1097/00005131-200202000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Gänsslen A., Hildebrand F., Krettek C. Conservative treatment of acetabular both column fractures: does the concept of secondary congruence work? Acta Chir Orthop Traumatol Cech. 2012;79(5):411–415. [PubMed] [Google Scholar]
- 9.Lichte P., Sellei R.M., Kobbe P., Dombroski D.G., Gänsslen A., Pape H.C. Predictors of poor outcome after both column acetabular fractures: a 30-year retrospective cohort study. Patient Saf Surg. 2013;7(1):9. doi: 10.1186/1754-9493-7-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang Y., Zou C., Fang Y. Mapping of both column acetabular fractures with three-dimensional computed tomography and implications on surgical management. BMC Muscoskel Disord. 2019;20(1):255. doi: 10.1186/s12891-019-2622-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tian S., Chen Y., Yin Y., Zhang R., Hou Z., Zhang Y. Morphological characteristics of posterior wall fragments associated with acetabular both-column fracture. Sci Rep. 2019;9(1):20164. doi: 10.1038/s41598-019-56838-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang H., Utku K., Zhuang Y. Post wall fixation by lag screw only in associated both column fractures with posterior wall involvement. Injury. 2017;48(7):1510–1517. doi: 10.1016/j.injury.2017.05.035. [DOI] [PubMed] [Google Scholar]
- 13.Tosonounidis T., Giannoudis P. Use of inlet-obturator view (Leeds view) for placement of posterior wall screws in acetabular fracture surgery. J Orthop Trauma. 2017;31(4):e133–e136. doi: 10.1097/BOT.0000000000000724. [DOI] [PubMed] [Google Scholar]
- 14.Bodanapally U.K., Dattwyler M. Acetabular fractures: a stepwise approach to identification and classification on 2D computed tomography. Appl Radiol. 2019;8(4):17–23. [Google Scholar]
- 15.Upex P., Jouffroy G., Riouallon G. Application of 3D printing for treating fractures of both column of the acetabulum: benefit of pre-contouring plates on the mirrored healthy pelvis. Orthop Traumatol Surg Res. 2017;103(3):331–334. doi: 10.1016/j.otsr.2016.11.021. [DOI] [PubMed] [Google Scholar]
- 16.Rommens P.M. Ilioinguinal approach for acetabular fractures. Orthop Traumatol. 2002;10:179–189. doi: 10.1007/s00065-002-1047-7. [DOI] [Google Scholar]
- 17.Tosounidis T.H., Giannoudis V.P., Kanakaris N.K., Giannoudis P.V. The ilioinguinal approach: state of the art. JBJS Essent Surg Tech. 2018;8(2) doi: 10.2106/JBJS.ST.16.00101. e19(1–7) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tannast M., Keel M.J.B., Siebenrock K.A., Bastian J.D. Open reduction and internal fixation of acetabular fractures using the modified Stoppa approach. JBJS Essent Surg Tech. 2019;9(1) doi: 10.2106/JBJS.ST.18.00034. e3(1–12) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Keel M.J., Ecker T.M., Cullmann J.L. The pararectus approach for anterior intrapelvic management of acetabular fractures: an anatomical and clinical evaluation. J Bone Joint Surg Br. 2012;94(3):405–411. doi: 10.1302/0301-620X.94B3.27801. [DOI] [PubMed] [Google Scholar]
- 20.Ashwani S., Ravi G., Ramesh S. Modified Stoppa approach for acetabulum fracture: a review. Rev Bras Ortop. 2019;54(2):109–117. doi: 10.1016/j/rboe.2017.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gänsslen A., Grechenig S., Nerlich M., Müller M. Standard approaches to the acetabulum part 1: Kocher-Langenbeck approach. Acta Chir Orthop Traumatol Cech. 2016;83(3):141–146. [PubMed] [Google Scholar]
- 22.Harris A.M., Althausen P., Kellam J.F., Bosse M.J. Simultaneous anterior and posterior approaches for complex acetabular fractures. J Orthop Trauma. 2008;22(7):494–497. doi: 10.1097/BOT.0b013e3181830d2a. [DOI] [PubMed] [Google Scholar]
- 23.Shin K.H., Choi J.H., Han S.B. Posterior wall fractures associated with both-column acetabular fractures can be skilfully ignored. Orthop Traumatol Surg Res. 2020;S1877–0568(20) doi: 10.1016/j/otsr.2020.02.019. 30168-7. [DOI] [PubMed] [Google Scholar]
- 24.Gusic N., Sabalic S., Pavic A., Ivkovic A., Sotosek-Tokmadzic V., Cicvaric T. Rationale for more consistent choice of surgical approaches for acetabular fractures. Injury. 2015;46(Suppl 6):S78–S86. doi: 10.1016/j.injury.2015.10.045. [DOI] [PubMed] [Google Scholar]
- 25.Elnahal W.A., Ward A.J., Acharya M.R., Chesser T.J.S. Does routine postoperative computerized tomography after acetabular fracture fixation affect management? J Orthop Trauma. 2019;33(Suppl 2):S43–S48. doi: 10.1097/BOT.0000000000001405. [DOI] [PubMed] [Google Scholar]
- 26.Gänsslen A., Krettek C. Osteosynthese von Zwei-Pfeiler-Frakturen des Azetabulums über den ilioinguinalen Zugang. Operat Orthop Traumatol. 2009;21(3):270–282. doi: 10.1007/s00064-009-1804-6. [DOI] [PubMed] [Google Scholar]
- 27.Gorczyca J.T., Powell J.N., Tile M. Lateral extension of the ilioinguinal incision in the operative treatment of acetabulum fractures. Injury. 1995;26(3):207–212. doi: 10.1016/0020-1383(95)93505-c. [DOI] [PubMed] [Google Scholar]
- 28.Young J.W., Burgess A.R., Brumback R.J., Poka A. Pelvic fractures: value of plain radiography in early assessment and management. Radiology. 1986;160(2):445–451. doi: 10.1148/radiology/160.2.3726125. [DOI] [PubMed] [Google Scholar]