Abstract
Purpose
The present study was conducted to evaluate the epidemiological characteristics of the Acetabular fractures treated in a level one trauma centre of India. This study is one of the largest to provide first-hand information regarding the demography, fracture patterns, other associated injuries, and the hospital stay of acetabular fractures in India.
Method
Patients admitted with the diagnosis of acetabular fractures between January 2013 and November 2019 were retrospectively analyzed in terms of demographic data such as age and sex, mechanism of injury, other associated injuries, and the duration of hospital stay.
Results
A total of 305 patients with 313 fractures of the acetabulum were included in the study. Among the 305 patients, 268 (87.8%) were male and 37 (12.1%) were female, with a declining male to female ratio over the years. The mean age was 37.1 ± 13.2 years (range 14–84 years). During the seven years, the mean age of presentation progressively increased. Linear regression showed an increase from 33 to 40 years from 2013 to 2019 (R2 = 0.027). Road traffic injuries were the most common mechanism of injury, contributing to about 77.4% of all cases. Associated injuries were seen in 62% of total cases with multiple system involvement in 26.6% of patients. The most frequent pattern in this epidemiological study was an isolated posterior wall fracture (21.4%) while the isolated anterior wall was the least frequent (0.95%).
Conclusion
Acetabular fractures are increasing in numbers and with increasing knowledge so is their surgical management in our country. It shall be prudent to establish an integrated electronic national trauma registry to maintain complete documentation in all institutions dealing with trauma management to ascertain the changing trends of acetabular fracture patterns in the country over time.
Keywords: Epidemiology, Acetabular fractures, Classification, Demography, India
1. Introduction
The literature on the epidemiology of acetabulum fractures is limited1 mainly due to its low incidence when compared to other skeletal fractures. Very few studies with large sample sizes are available and most of them are from western literature.1, 2, 3, 4, 5
The majority of the data regarding the epidemiological characteristics of acetabular fractures are part of the outcome analysis of fracture management.6, 7, 8, 9 They indicate the changing trends in the presentation and demographic variations of the acetabular fractures.1,4,10 The classical series of Letournel and Matta gives extensive data on the incidence of types of acetabular fractures and in both series Associated Both Column fracture (ABC) was the commonest.2,3 However, in the last two decades, the majority of epidemiological studies and meta-analysis have found the incidence of isolated posterior wall (PW) fracture to be the commonest, superseding ABC fracture.9, 10, 11, 12, 13, 14, 15, 16 Also, other epidemiological characteristics of acetabular fractures like age, sex, mechanism of injury, and associated injuries are scant and heterogeneous due to geographical, cultural, and lifestyle variation.11, 12, 13
The majority of acetabular fractures are attributed to road traffic injuries followed by fall from height.6,14 However, the incidence of acetabular fractures varies from country to country1,4,10,11,15, 16, 17, 18 as it depends on local and global demographic characteristics, cultural differences, and occupational preferences also, which can alter exposure to higher energy trauma and trauma mechanisms. Therefore, it seems prudent to assume international differences in specific fractures epidemiology and acetabulum fractures are not the exception.19 Whether these differences are clinically (beyond statistically) significant or not, needs to be identified and evaluated to be useful in the country-specific management of these injuries. It is necessary to recognize regional differences worldwide to be able to understand the globally published information in the proper context and use it for the benefit of our regional patients. India has overtaken the world in the number of road traffic accident deaths, disproportionate to the rate of increase in the population of the country.20 Hence, there is an urgent need to recognize the magnitude of the situation in our country to take appropriate action.
The present study was conducted to evaluate the epidemiological characteristics of the acetabular fractures in a level one trauma centre of India and also to get first-hand information regarding the demography, fracture patterns, other associated injuries, and the hospital stay of these patients.
2. Patients and methods
This was a retrospective study conducted in a tertiary care, level one trauma centre of north India. Ethical clearance was taken from the Institute Ethical Committee for this study. Data of patients admitted with the diagnosis of acetabular fractures between January 2013 and November 2019 was retrieved from the hospital record using a computerized patient record system (CPRS).
All admitted patients with acetabular fractures of age more than 14 years were included in this study, while patients with pelvic injuries without acetabular fractures, patients with incomplete preoperative radiological images i.e. Anteroposterior (AP) and Judet radiographic views, and whole pelvis computer tomography (CT) scan were excluded from the study. Our surgical indications for fracture fixation were – fracture displacement >2 mm, Matta’s roof angle <45° or unstable/non-concentric joint reduction, unstable posterior wall fracture dislocation, presence of acetabulum cartilage marginal impaction with significant fracture displacement. Surgical approach and sequence of fixation was decided based on the degree of displacement of the affected column, direction of femur head dislocation, quadrilateral plate involvement, and surgeon discretion.
During the above period, a total of 605 patients with pelvic and acetabular fractures were admitted and of these 508 patients had complete preoperative radiological images and clinical records. 203 patients with isolated pelvic fractures were excluded. Radiographs and CT scans of all these patients were reviewed using a Picture Archiving and Communication System (PACS) for the classification of acetabular fractures. All cases were initially classified based on a series of radiographic views according to the Judet and Letournel classification21 and later confirmed on CT scans. All radiological images were reviewed by two trained pelvic acetabulum fellows independently. When any disagreement in the classification of fractures occurred, the discretion was left to the senior author for a final agreement on the fracture classification. The cases not fitting into the classical description as per the Judet and Letournel Classification system were classified as atypical fracture patterns. Based on these radiological reviews, 305 patients with 313 fractures of the acetabulum were identified and included in this study.
Demographic data such as age, sex, mechanism of injury, other associated injuries, and days of stay in the hospital was reviewed. Associated injuries were determined by Abbreviated Injury Scale (AIS) and Injury Severity Score (ISS). Data storage and processing were performed using Microsoft-Excel® software.
3. Results
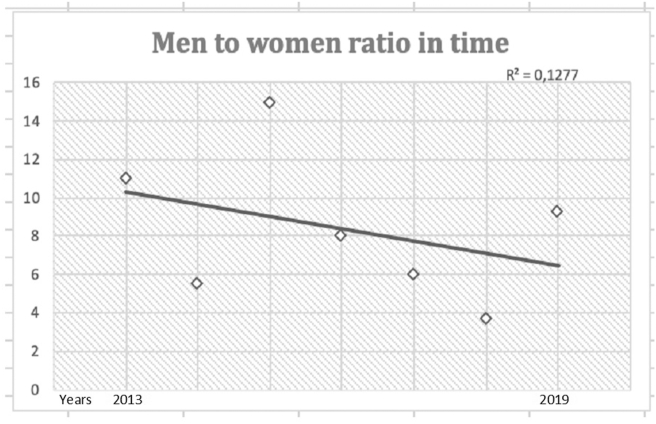
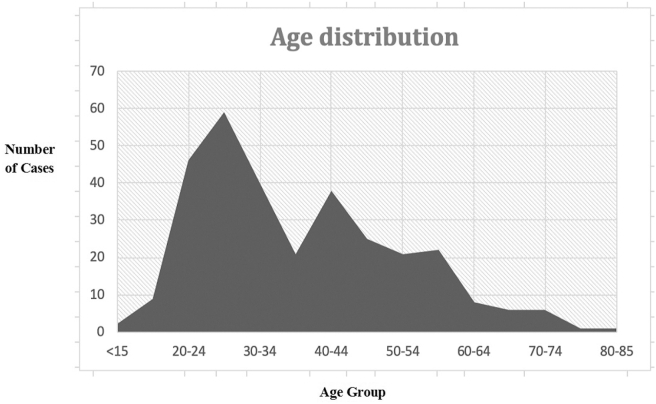
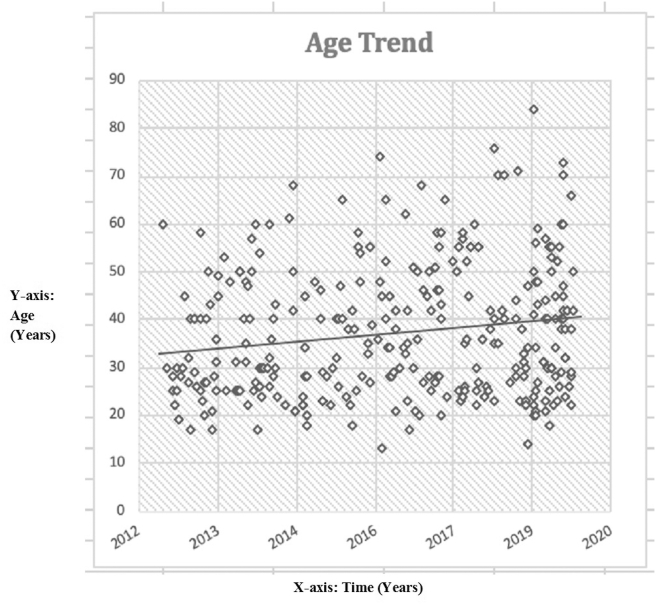
Among the 305 patients, 268 (87.8%) were male and 37 (12.1%) were female, with a declining male to female ratio over the study period from 2013–2019. (Fig. 1). The mean age was 37.1 ± 13.2 years (range 14–84 years). Women had a mean age of 36 years while in men it was 37.2 years. There were two peaks in the age of presentation: first between 25 and 30 years and second between 40 and 45 years (Fig. 2). During the seven years, the mean age of presentation progressively increased. Linear regression showed an increase from 33 to 40 years from 2013 to 2019 (R2 = 0.027) (Fig. 3).
Fig. 1.
Male/Female ratio over the study period of 2013–2019.
Fig. 2.
Age distribution of the patients with Acetabular fractures.
Fig. 3.
Age trend of Acetabular Fractures over the seven years period.
166/305 cases (54.4%) were on the right side and 131/305 (42.9%) were on the left side. Eight patients (2.6%) were having bilateral involvement. Road traffic injuries were the most common mechanism of injury, contributing to about 77.4%, whereas fall from height caused 19% of the fractures (Table 1).
Table 1.
Mechanism Of Injury of Acetabular Facture in the study cohort.
| Mechanism of Injury | Total | Male | Female | |
|---|---|---|---|---|
| Crush Injury | 8 | 2.6% | 6 | 2 |
| Fall From Height | 58 | 19.0% | 37 | 21 |
| 1st Floor | 19 | 6.2% | 11 | 8 |
| 2nd Floor | 5 | 1.6% | 2 | 3 |
| 3rd Floor | 4 | 1.3% | 2 | 2 |
| 4th Floor | 2 | 0.7% | 2 | 0 |
| Bed | 1 | 0.3% | 1 | 0 |
| Stairs | 4 | 1.3% | 1 | 3 |
| Tree | 2 | 0.7% | 2 | 0 |
| Unspecified | 21 | 6.9% | 16 | 5 |
| Hit by train | 3 | 1.0% | 3 | 0 |
| Road Traffic Accident | 236 | 77.4% | 222 | 14 |
Associated injuries were seen in 62% of the total cases. The median ISS was 22 (interquartile range 9–32). Multiple system involvement was seen in 26.6% of the total cases (Table 2). The most frequent involvement was seen in the abdomen (9.8%) and Pelvic region (14.1%). Posterior dislocation of the hip was seen in 49 (16.1%) patients with 10 cases having sciatic nerve palsy at presentation. The most common long bone to be fractured in the lower limb was the ipsilateral femur in 36 (11.8%) patients, with the proximal femur being the most commonly involved site (41.6%) of these 36 patients. Tibial fractures were next common with 11.5% involvement with these fractures.
Table 2.
Distribution of associated injuries with acetabular fractures.
| Associated injuries | Total | |
| Any | 189 | 62.0% |
| Isolated asociated injury | 108 | 35.4% |
| Multiple injuries | 81 | 26.6% |
| Specific Injuries | ||
| Cranio-facial | 24 | 7.9% |
| Head | 14 | 4.6% |
| Face fracture | 11 | 3.6% |
| Spine | 15 | 4.9% |
| Cervical | 1 | 0.3% |
| Thoracic | 3 | 1.0% |
| Lumbar | 6 | 2.0% |
| Sacrum | 5 | 1.6% |
| Chest | 19 | 6.2% |
| Hemothorax | 12 | 3.9% |
| OtherThoracic | 6 | 2.0% |
| Diaphragm | 2 | 0.7% |
| Ribs | 11 | 3.6% |
| Abdomen | 30 | 9.8% |
| Enteric | 4 | 1.3% |
| Spleen | 3 | 1.0% |
| Liver | 8 | 2.6% |
| OtherAbdominal | 19 | 6.2% |
| Pelvis | 43 | 14.1% |
| Pelvic fracture | 41 | 13.4% |
| Testes | 2 | 0.7% |
| Bladder | 6 | 2.0% |
| Morel Lavalle | 5 | 1.6% |
| Around the hip | 53 | 17.4% |
| Bilateral acetabulum | 8 | 2.6% |
| Posterior hip dislocation | 49 | 16.1% |
| Sciatic nerve palsy | 10 | 3.3% |
| Proximal Femur | 15 | 4.9% |
| Femur shaft | 14 | 4.6% |
| Around the knee | 24 | 7.9% |
| Distal femur | 7 | 2.3% |
| Patella | 9 | 3.0% |
| Tibial plateau | 10 | 3.3% |
| Common peroneal nerve palsy | 1 | 0.3% |
| Below the knee | 26 | 8.5% |
| Tibia shaft | 16 | 5.2% |
| Ankle | 9 | 3.0% |
| Foot | 6 | 2.0% |
| Around the shoulder | 17 | 5.6% |
| Clavicle | 5 | 1.6% |
| Scapula | 5 | 1.6% |
| Humerus | 10 | 3.3% |
| Elbow and below | 27 | 8.9% |
| Around the elbow | 3 | 1.0% |
| Forearm | 12 | 3.9% |
| Hand | 13 | 4.3% |
The frequency of fractures according to the Judet-Letournel classification, the age, and the gender distribution are as shown in Table 3. The most frequent pattern in this epidemiological study was an isolated posterior wall fracture (21.4%) while the isolated anterior wall was the least frequent (0.95%). 23% (72/313) of the fractures were non-classifiable according to the 10 classic Judet-Letournel patterns. However, 73.6% (53/72) of these 72 cases were classifiable when combining isolated patterns with an associated posterior wall.
Table 3.
Distribution of Acetabular Fracture pattern as per classical Judet- Letournel classification.
| Fracture Type (Judet-Letournel) | Mean age (years) | Frequency |
||
|---|---|---|---|---|
| Total (313) | Male | Female | ||
| Elementary patterns | ||||
| Posterior wall (PW) | 36.8 | 67 (21.4%) | 64 | 3 |
| Posterior column (PC) | 40.9 | 10 (3.2%) | 10 | 0 |
| Anterior wall (AW) | 39.6 | 3 (0.95%) | 3 | 0 |
| Anterior column (AC) | 39.5 | 21 (6.7%) | 18 | 3 |
| Transverse (Tr) | 33.6 | 16 (5.1%) | 13 | 3 |
| Associated patterns | ||||
| Associated Both column (ABC) | 31 | 20 (6.38%) | 15 | 5 |
| Transverse + PW (Tr + PW) | 31.9 | 40 (12.7%) | 39 | 1 |
| T-shape | 37.6 | 15 (4.8%) | 14 | 1 |
| Posterior column + PW (PC+ PW) | 33 | 16 (5.1%) | 16 | 0 |
| Anterior Column Posterior Hemitransverse (ACPHT) | 46.7 | 33 (10.5%) | 25 | 8 |
| Non classifiable | ||||
| Anterior Column + PW (AC+ PW) | 50.5 | 6 (1.9%) | 6 | 0 |
| Associated Both column + PW (ABC+ PW) | 42 | 23 (7.3%) | 16 | 7 |
| ACPHT + PW | 47.2 | 6 (1.9%) | 6 | 0 |
| T shape + PW ( T shape + PW) | 31.7 | 18 (5.7%) | 17 | 1 |
| Others | 33 | 19 (6.07%) | 12 | 7 |
Fractures patterns in the younger age groups <40 years were Posterior Wall (PW) fractures and Transverse with posterior wall (TPW) fractures. These patterns were associated with higher energy trauma and a posteromedial vector, which is consistent with this age group (Table 4). In the age group of 40–60 years also, the PW fractures along with TPW fractures predominated. However, the Anterior Column Posterior Hemitransverse (ACPHT) fracture pattern also had substantial numbers.
Table 4.
Age-wise distribution of acetabular fracture pattern as per Judet-Letournel Classification. PW-Posterior Wall; AC-Anterior Column; AW-Anterior Wall; Tr-Transverse; PC-Posterior Column; ACPHT-Anterior Column Posterior HemiTransverse; ABC-Associated Both Column; T-T Shape Fractures
| Elementary |
Associated |
Non classifiable | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Age group (Yrs) | PW | AC | AW | TR | PC | ACPHT | ABC | PC + PW | TR + PW | T | |
| <20 | 3 | 0 | 0 | 0 | 0 | 1 | 2 | 1 | 0 | 2 | 0 |
| 20–29 | 18 | 9 | 0 | 2 | 5 | 9 | 7 | 6 | 18 | 3 | 15 |
| 30–39 | 18 | 3 | 2 | 5 | 0 | 3 | 5 | 3 | 12 | 3 | 13 |
| 40–49 | 13 | 3 | 1 | 3 | 0 | 2 | 0 | 5 | 6 | 3 | 14 |
| 50–59 | 13 | 3 | 0 | 6 | 3 | 8 | 2 | 1 | 4 | 3 | 10 |
| 60–70 | 2 | 1 | 0 | 0 | 2 | 7 | 4 | 0 | 0 | 1 | 20 |
| >70 | 0 | 2 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 0 | 0 |
Fracture patterns occurring more frequently in older patients (above 60 years) were ACPHT fractures along with atypical patterns of anterior column + posterior wall, ACPHT with or without a posterior wall, and ABC with a PW fracture. These patterns have in common the compromise of both anterior and posterior acetabulum (Table 4).
Analysis of the timing of surgery and discharge revealed the meantime from the injury to surgery to be 7.8 days and time to discharge after surgery of 5.1 days, with a mean time of total hospitalization of 12.9 days.
4. Discussion
Despite the great interest in acetabular fractures worldwide, there have been very limited epidemiological studies available. An epidemiological study with large sample size is essential to draw significant conclusions and to do subsequent analysis. Countries, where the patient’s referral system is followed critically and complex fractures are referred to regional level apex trauma centers for better patient care, can contribute to such epidemiological studies in a better way projecting the national demographic variation in the presentation of these fractures.
Previous available epidemiological studies of acetabular fractures have been of small sample size6, 7, 8, 9,11,12,22, 23, 24 and have been multicentric in origin25. Due to the paucity of data, very often studies with small sample sizes have included epidemiological characteristics of patients as their secondary objective.6, 7, 8, 9 To the best of our knowledge, this is the largest study from India and one of the largest epidemiological series of surgically treated acetabular fractures from a single institution over a period of seven years.
The mean age at which acetabular fractures occurred is 37.1 years in our cohort, similar to the other Indian studies6, 7, 8, 9 (Table 5), but much lower than the western population1,14 (Table 6). The age distribution curve of the patients in this study followed a bimodal curve, similar to the age distribution curve of Denver, Colorado population19 and that in Finland study,10 but with an earlier onset of the second peak. These age distribution differences signify that the major concentration of patients in our country with acetabular fractures is below 60 years of age and the elderly and osteoporotic type of fracture patterns have still not assumed major proportions in our country, unlike the major western world.26, 27, 28
Table 5.
Comparison of the present study with the other studies published from India. PW-Posterior Wall; AC-Anterior Column; AW-Anterior Wall; Tr-Transverse; PC-Posterior Column; ACPHT-Anterior Column Posterior HemiTransverse; ABC-Associated Both Column; T-T shape Fractures
| Classification (Judet - Letournel)21 | Present study (2020) n = 313 | Jindal et al.7 (2019) n = 116 | Meena et al.6 (2013) n = 118 | Gupta et al.8 (2007) n = 63 | Kumar et al.9 (2005) n = 73 |
|---|---|---|---|---|---|
| PW | 21.4% | 28.3% | 24.5% | 7.9% | 32.8% |
| AW | 0.95% | 7.5% | NR (included in AC) | 1.5% | 0 |
| PC | 3.2% | 4.1% | 5.0% | 6.3% | 2.7% |
| AC | 6.7% | 10.8% | 5.0% | 4.7% | 4.1% |
| Tr | 5.1% | 13.3% | 11.0% | 3.1% | 6.8% |
| T shape | 4.8% | 11.6% | 10.1% | 9.5% | NR |
| ACPHT | 10.5% | 1.6% | 5.9% | 4.7% | 0 |
| ABC | 6.38% | 12.5% | 14.4% | 34.9% | 36.9% |
| PC + PW | 5.1% | 5.1% | 14.4% | 4.7% | 5.4% |
| Tr + PW | 12.7% | 5.0% | 9.3% | 22.2% | 9.5% |
| Non-Classifiable | 23.0% | NR | NR | NR | NR |
| Mechanism Of Injury | |||||
| RTA | 77.4% | 72.4% | 83.9% | – | 65.0% |
| Fall from height | 19.0% | 21.6% | 12.7% | – | 25.0% |
| Others | 3.6% | 6.0% | 3.4% | – | 10.0% |
| Associated Injuries | |||||
| Dislocation | 16.1% | 17.5% | NR | – | 33.0% |
| Hip | 4.9% | 3.3% | 2.5% | – | – |
| Pelvis | 13.4% | 25.8% | 27.2% | – | 5.5% |
| Other Limb Injury | 38.7% | 43.3% | 9.3% | – | 25.0% |
| Head Injury | 4.6% | 15.0% | 5.1% | – | 1.3% |
| Abdomen | 9.8% | 12.5% | NR | – | 5.5% |
| Chest | 6.2% | 6.7% | NR | – | 16.6% |
| Other Injuries | 12.8% | 3.3% | NR | – | NR |
| Mean Age (Years) | 37.02 ± 13.82 | 40.0 | 38.8 | 38.4 | 39.5 |
| Men to Women Ratio | 7.2 | 4.2 | 5.2 | NR | 10.1 |
Table 6.
Comparison of the present study data with international epidemiological Studies. PW-Posterior Wall; AC-Anterior Column; AW-Anterior Wall; Tr-Transverse; PC-Posterior Column; ACPHT-Anterior Column Posterior HemiTransverse; ABC-Associated Both Column; T-T shape Fractures
| Classification (Judet - Letournel)21 | Present study (2020) n = 313 INDIA | Letournel et al.2 (1993) n = 567 | Matta et al.3 (1986) n = 255 | Giannoudis et al.14 (2005) n = 3670 META-ANALYSIS | Dias et al.23 (2010) n = 73 BRAZIL | Briffa et al.24 (2011) n = 161 UK | Laird et al.1 (2005) n = 351 UK | Mesbahi et al.22 (2018) n = 79 IRAN |
|---|---|---|---|---|---|---|---|---|
| PW |
21.4% | 22.4% | 8.6% | 23.6% | – | 15.9% | 23.3% | 43% |
| AW | 0.95% | 1.6% | 1.2% | 1.7% | – | 0.8% | 1.8% | 1.8% |
| PC | 3.2% | 2.3% | 3.1% | 3.5% | – | 3.5% | 6.7% | 7.6% |
| AC | 6.7% | 3.9% | 4.7% | 3.9% | – | 7.0% | 14.7% | 3.8% |
| TR | 5.1% | 3.7% | 3.5% | 8.3% | – | 12.8% | 8.6% | 1.3% |
| T type | 4.8% | 5.3% | 12.2% | 9.3% | – | 11.3% | 11.0% | 6.3% |
| ACPHT | 10.5% | 8.8% | 5.9% | 5% | – | 5.4% | 6.7% | 2.5% |
| ABC | 6.38% | 27.9% | 33.3% | 21.7% | – | 26.1% | 13.5% | 21.5% |
| PC + PW | 5.1% | 3.5% | 3.9% | 5.7% | – | 5.1% | 4.3% | 8.9% |
| TR + PW | 12.7% | 20.6% | 23.5% | 17.4% | – | 12.1% | 9.2% | 3.8% |
| Non-Classifiable | 23.0% | NR | NR | NR | – | NR | NR | NR |
| Mechanism Of Injury | ||||||||
| RTA | 77.4% | – | – | 61.0% | 78.0% | 82% | 46.5% | 82.3% |
| Fall from height | 19.0% | – | – | 24.0% | 12.4% | 13% | 40.2% | 15.2% |
| Others | 3.6% | – | – | 15.0% | 9.6% | 5% | 11.1% | 2.5% |
| Associated Injuries | ||||||||
| Dislocation | 16.1% | – | – | – | 30.0% | 33% | – | – |
| Hip | 4.9% | – | – | – | – | – | – | – |
| Pelvis | 13.4% | – | – | 6.2% | 8.0% | – | – | – |
| Other Limb Injury | 38.7% | – | – | 40.3% | 16.0% | – | – | – |
| Head Injury | 4.6% | – | – | 22.0% | 21.7% | – | – | – |
| Abdomen | 9.8% | – | – | 7.9% | 17.4% | – | – | – |
| Chest | 6.2% | – | – | 12.0% | 39.1% | – | – | – |
| Other Injuries | 12.8% | – | – | 5.6% | NR | – | – | – |
| Mean Age (Years) | 37.02 ± 13.82 | – | 37.0 | 38.6 | 39.6 | 36 | 50 | 36.8 |
| Men to Women Ratio | 7.2 | 1.9 | 2.5 | 2.2 | 3.3 | 3 | 1.9 | 4.6 |
The male to female ratio in our study is 7.2, which is similar to other Indian studies.6,7 Still, this ratio was about double than the studies from the developed world1,14,23,24 probably due to cultural differences resulting in lesser exposure of women to outdoor activities and 2 wheeler motorbike riding. However, the mechanism of injury most commonly implicated was road traffic injuries and fall from a height, in congruence with other studies.1,17,23,24
Associated injuries were seen in 62% of patients which is almost 1.5 to 2 times more frequently than other studies,9,14,23 with abdominal-pelvic injuries being the most frequent associated injury in comparison to the chest and head injury. This finding is significant and in contrast to the study by Giannoudis et al.14 which may be attributed to the lack of safety protocols in vehicular traffic in our country causing severe injuries including acetabular fractures. Limb fractures were more common than Pelvic fractures as an associated injury to acetabular fractures which is similar to the results of the study by Giannoudis et al. but is, in contrast, to study by Dias et al.14,23
In this study, Judet–Letournel classification was used as it is the most widely accepted classification system for acetabular fractures.29 The PW fractures were the most frequent elementary fracture pattern (21.4%) in line with the majority of national and international studies.1,4,6, 7, 8, 9,14, 23 The TPW fractures were the most frequent associated fracture pattern (12.7%) in this study, unlike in most studies1, 4, 8, 9, 14, 23, 24 where ABC fracture was the most common (Table 5, Table 6) pattern. This again may be attributed to the increased incidence of acetabular fractures in India in the younger population, unlike other countries.
A large number of fractures (23%) however could not be classified as per the classical Judet and Letournel classification system as these fractures had associated posterior wall fractures with the complex fracture patterns of Letournel classification (Table 3). We believe this big difference might be because of the previous trend to classify any atypical or unclassifiable fracture into the most subjectively similar classification type and may also be due to extensive use of CT scans, which reveals more information and patterns not well addressed on radiographic analysis of these fractures. We strongly feel that this discrepancy in the classification system needs to be addressed by the addition of a qualifier of associated additional fracture patterns for the classical 10 patterns of the Judet and Letournel classification system. This shall help in keeping the fracture patterns system intact while encompassing the additional outliers which at present are not classifiable despite having a major fracture pattern.
The gradual increase in the number of acetabular fractures in India over the last decade may be attributed to an increase in the number of cases of road traffic accidents due to the rising density of population and motor vehicles or better pre-hospital care which improves the number of patients arriving alive to the hospital or it could also be due to the fact that more of these complex injuries are now being referred to the specific major trauma centers where proper record keeping and documentation is possible.
However, this study has a few limitations, which need to be considered. Firstly, the population catered by our centre is referral in nature, and therefore, our findings may not be the true representation of the entire population. Secondly, this study did not involve patients who have been treated nonoperatively for acetabular fractures. This population had been omitted due to the lack of complete documentation of such cases in our hospital electronic record system. Lastly, the surgical management, fracture complications, and functional outcomes have not been included as it was outside the scope of this epidemiological study.
Based on this study, we can project that the typical Indian acetabular fracture patient would be a man in his 4th decade of life-sustaining a road traffic injury. He has most likely a right-sided posterior wall fracture with nearly 66% of them having an associated injury to one or more other organ systems. He is likely to be treated surgically within 8 days of his injury and discharged from our hospital in approximately 2 weeks from the date of injury.
5. Conclusion
Acetabular fractures are increasing in numbers and with increasing knowledge so is their surgical management in our country. It shall be prudent to establish an integrated electronic national trauma registry to maintain complete documentation in all institutions dealing with trauma management to ascertain the changing trends of acetabular fracture patterns in the country over time.
Funding
No funding or grants were received or will be received from any commercial party relating to the subject of this article.
Ethical approval
Ethical approval was taken from institute review board. All procedures performed in this study involving human participants were in accordance with the ethical standard of the institutional and/international research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standard.
Declaration of competing interest
On behalf of all authors, the corresponding author states that there is no conflict of interest to disclose.
Acknowledgements
None.
References
- 1.Laird A., Keating J.F. Acetabular fractures: a 16-year prospective epidemiological study. J Bone Joint Surg British Vol. 2005;87(7):969–973. doi: 10.1302/0301-620X.87B7.16017. [DOI] [PubMed] [Google Scholar]
- 2.Letournel E., Judet R., Elson R.A. Fractures of the Acetabulum. Springer; Berlin, Heidelberg: 1993. Operative treatment between three weeks and four months after injury; pp. 591–633. [Google Scholar]
- 3.Matta J.M., Mehne D.K., Roffi R. Fractures of the acetabulum. Early results of a prospective study. Clin Orthop Relat Res. 1986;(205):241–250. [PubMed] [Google Scholar]
- 4.Zhang R., Yin Y., Li A. Three-column classification for acetabular fractures: introduction and reproducibility assessment. The Journal of bone and joint surgery. Am Vol. 2019;101(22):2015–2025. doi: 10.2106/JBJS.19.00284. [DOI] [PubMed] [Google Scholar]
- 5.Herman A., Tenenbaum S., Ougortsin V., Shazar N. There is No column: a new classification for acetabular fractures. J Bone Jt Surg Am Vol. 2018;100(2):e8. doi: 10.2106/JBJS.17.006006. [DOI] [PubMed] [Google Scholar]
- 6.Meena U.K., Tripathy S.K., Sen R.K., Aggarwal S., Behera P. Predictors of postoperative outcome for acetabular fractures. Orthop Traumatol Surg Res. 2013;99(8):929–935. doi: 10.1016/j.otsr.2013.09.004. [DOI] [PubMed] [Google Scholar]
- 7.Jindal K., Aggarwal S., Kumar P., Kumar V. Complications in patients of acetabular fractures and the factors affecting the quality of reduction in surgically treated cases. J Clin Orthopaed Trauma. 2019;10(5):884–889. doi: 10.1016/j.jcot.2019.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gupta R.K., Singh H., Dev B., Kansay R., Gupta P., Garg S. Results of operative treatment of acetabular fractures from the Third World--how local factors affect the outcome. Int Orthop. 2009;33(2):347–352. doi: 10.1007/s00264-007-0461-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kumar A., Shah N.A., Kershaw S.A., Clayson A.D. Operative management of acetabular fractures: a review of 73 fractures. Injury. 2005;36(5):605–612. doi: 10.1016/j.injury.2004.11.022. [DOI] [PubMed] [Google Scholar]
- 10.Rinne P.P., Laitinen M.K., Huttunen T., Kannus P., Mattila V.M. The incidence and trauma mechanisms of acetabular fractures: a nationwide study in Finland between 1997 and 2014. Injury. 2017;48(10):2157–2161. doi: 10.1016/j.injury.2017.08.003. [DOI] [PubMed] [Google Scholar]
- 11.Ahmed M., Abuodeh Y., Alhammoud A., Salameh M., Hasan K., Ahmed G. Epidemiology of acetabular fractures in Qatar. Int Orthop. 2018;42(9):2211–2217. doi: 10.1007/s00264-018-3824-z. [DOI] [PubMed] [Google Scholar]
- 12.Boudissa M., Francony F., Kerschbaumer G. Epidemiology and treatment of acetabular fractures in a level-1 trauma centre: retrospective study of 414 patients over 10 years. J Orthop Traumatol: Surg Res. 2017;103(3):335–339. doi: 10.1016/j.otsr.2017.01.004. [DOI] [PubMed] [Google Scholar]
- 13.Cavalcante M.C., Arruda F., Boni G., Sanchez G.T., Balbachevsky D., Reis F.B.D. Demographic analysis of acetabular fractures treated in a quaternary care hospital from 2005 to 2016. Acta Ortopédica Bras. 2019;27(6):317–320. doi: 10.1590/1413-785220192706207042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Giannoudis P.V., Grotz M.R.W., Papakostidis C., Dinopoulos H. Operative treatment of displaced fractures of the acetabulum: a meta-analysis. J Bone Joint Surg British Vol. 2005;87(1):2–9. [PubMed] [Google Scholar]
- 15.Best M.J., Buller L.T., Quinnan S.M. Analysis of incidence and outcome predictors for patients admitted to US hospitals with acetabular fractures from 1990 to 2010. Am J Orthoped. 2018;47(9) doi: 10.12788/ajo.2018.0083. [DOI] [PubMed] [Google Scholar]
- 16.Amin S., Achenbach S.J., Atkinson E.J., Khosla S., Melton L.J., 3rd Trends in fracture incidence: a population-based study over 20 years. J Bone Miner Res : Off J Am Soc Bone Min Res. 2014;29(3):581–589. doi: 10.1002/jbmr.2072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Löfman O., Berglund K., Larsson L., Toss G. Changes in hip fracture epidemiology: redistribution between ages, genders and fracture types. Osteoporos Int. 2002;13(1):18–25. doi: 10.1007/s198-002-8333-x. [DOI] [PubMed] [Google Scholar]
- 18.Dhanwal D.K., Dennison E.M., Harvey N.C., Cooper C. Epidemiology of hip fracture: worldwide geographic variation. Indian J Orthop. 2011;45:15–22. doi: 10.4103/0019-5413.73656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mauffrey C., Hao J., Cuellar D.O. The epidemiology and injury patterns of acetabular fractures: are the USA and China comparable? Clin Orthop Relat Res. 2014;472(11):3332–3337. doi: 10.1007/s11999-014-3462-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Singh S.K. Road traffic accidents in India: issues and challenges. Transport Res Procedia. 2017;25:4708–4719. [Google Scholar]
- 21.Judet R., Judet J., Letournel E. Fractures of the acetabulum: classification and surgical approaches for open reduction: preliminary report. JBJS. 1964;46(8):1615–1675. [PubMed] [Google Scholar]
- 22.Mesbahi S.A.R., Ghaemmaghami A., Ghaemmaghami S., Farhadi P. Outcome after surgical management of acetabular fractures: a 7-year experience. Bull Emergency Trauma. 2018;6(1):37. doi: 10.29252/beat-060106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dias M.V.F., Goldsztajn F., Guimarães J.M., Grizendi J.A., Correia M., Rocha T.H. Epidemiology of acetabulum fractures treated at the instituto nacional de traumatologia e ortopedia (Into) Revista Brasileira de Ortopedia. 2010;45(5):474–477. doi: 10.1016/S2255-4971(15)30438-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Briffa N., Pearce R., Hill A.M., Bircher M. Outcomes of acetabular fracture fixation with ten years’ follow-up. J Bone Joint Surg British Vol. 2011;93(2):229–236. doi: 10.1302/0301-620X.93B2.24056. [DOI] [PubMed] [Google Scholar]
- 25.Ochs B.G., Marintschev I., Hoyer H. Changes in the treatment of acetabular fractures over 15 years: analysis of 1266 cases treated by the German Pelvic Multicentre Study Group (DAO/DGU) Injury. 2010;41(8):839–851. doi: 10.1016/j.injury.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 26.Malhotra N., Mithal A. Osteoporosis in Indians. Indian J Med Res. 2008;127(3) [PubMed] [Google Scholar]
- 27.Harinarayan C.V., Akhila H. Modern India and the tale of twin nutrient deficiency–calcium and vitamin D–nutrition trend data 50 Years-retrospect, introspect, and prospect. Front Endocrinol. 2019;10 doi: 10.3389/fendo.2019.00493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Babu U.S., Calvo M.S. Modern India and the vitamin D dilemma: evidence for the need of a national food fortification program. Mol Nutr Food Res. 2010;54(8):1134–1147. doi: 10.1002/mnfr.200900480. [DOI] [PubMed] [Google Scholar]
- 29.Polesello G.C., Nunes M.A.A., Azuaga T.L., Queiroz M.C.D., Honda E.K., Ono N.K. Comprehension and reproducibility of the Judet and Letournel classification. Acta Ortopédica Bras. 2012;20(2):70–74. doi: 10.1590/S1413-78522012000200002. [DOI] [PMC free article] [PubMed] [Google Scholar]