Abstract
Acetabular impaction fractures when not adequately addressed leads to early arthritis. Dome impaction injuries and marginal impaction injuries have to be properly planned pre-operatively with respect to surgical approach, disimpaction techniques and fixation strategies. CT scan is the best modality to analyse the site, extent of impaction and plan strategies to reduce. Emphasis of early mobilisation should not drive the surgeon towards the motive of rigid fixation of columns alone, as the inadequate reduction of acetabular impaction leads to loss of mechanical support on weight bearing and thereby cause loss of reduction. Bone grafting either by auto or allograft or graft substitutes in the void after disimpaction helps in reducing anatomically and provide mechanical support adequately. In cases of severe comminution, reconstruction of the wall defect with autologous graft is a better treatment option. In this article we reviewed the characteristics of impaction injuries of acetabulum exploring surgical procedures, approaches and techniques for achieving open reduction and internal fixation.
Keywords: Dome impaction fracture, Marginal impaction fracture, Cranial marginal impaction fracture, Bone grafting in acetabular impaction fracture, Sea-gull sign
1. Introduction
Acetabular impaction fractures could be either ‘dome impaction’ fractures or ‘Posterior wall marginal impaction’ fractures of acetabulum. Both the patterns, when unreduced properly lead to early arthritis and hip joint instability particularly with unreduced posterior wall impaction injuries. These incarcerated fracture fragments are often termed as harbinger for failure following internal fixation.1 Fracture forces in such injuries leads to compaction of underlying cancellous bone, when disimpacted they often require grafting or bone substitutes to fill the void. ‘Sea gull’ sign [Fig. 1] is pathognomonic sign seen in acetabular roof compression fractures, where a typical double arc shadow resembling sea gull wings in flight is observed.2 These articular dome impaction fractures are commonly observed in elderly patients particularly with osteoporosis as a result of low velocity injury.3,4 Letournel and Judet described the term ‘Marginal impaction’ fracture, which is defined as a rotated and impacted, with depression of osteo-cartilaginous fragment of the posterior part of acetabulum that occurs in conjunction with a posterior fracture dislocation of the hip.5,6 The incidence of marginal impaction in acetabular fractures involving the posterior wall is about 30%.7
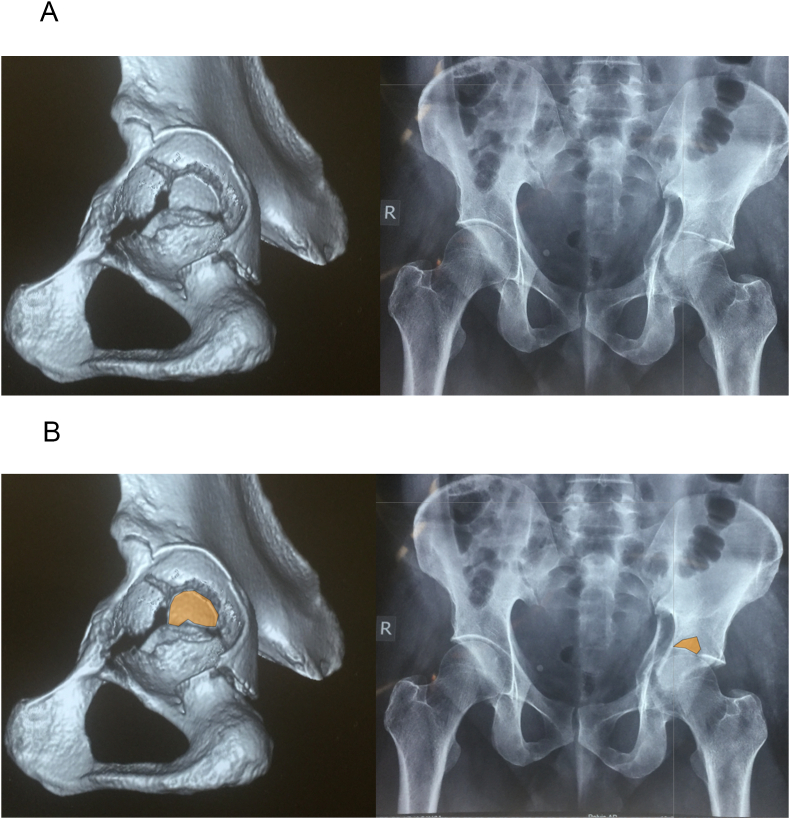
Fig. 1.
A: 3D CT scan showing dome impaction fracture of acetabulum which resembles a Sea Gull wings in flight on a X ray AP view – ‘See Gull Sign’. Fig. 1B: Marking of the osteochondral fragment in dome impaction in 3D CT and correspondingly on X ray.
It is evident that type of impaction acetabular fractures in elderly age group involves anterior acetabular elements and in younger age group posterior wall impaction injuries are observed. Among elderly, landing on greater trochanter while falling from a height creates a medially directed force that drives the femoral head through anterior column and the quadrilateral surface resulting in anterior and medial displacement followed by impaction of the acetabular dome with a predominant fracture patterns involving anterior column and the anterior column/posterior hemi-transverse areas. The anteromedial dome fragment is either free floating or hinged on the lateral articular surface creating a characteristic gull wing appearance.1 They are difficult to manage with respect the challenges posed in achieving reduction of the fragment. Most authors earlier recommended that the chances of failure of internal fixation were high in acetabular roof fractures.1,8 Laflamme and Hebert-Davies achieved good results by direct reduction of superior medial dome impaction in the well-selected geriatric patient.9
The marginal impaction fractures involving posterior acetabular wall [Fig. 2] represent severe form of injury as a result of high velocity trauma leading to impaction of posterior wall, which when unreduced properly would lead to early arthritis and instability of joint due to loss of secondary reduction. The treatment of posterior marginal impaction fractures is ORIF with disimpaction followed by filling of the void to provide good mechanical stability without any loss of secondary reduction upon weight bearing.
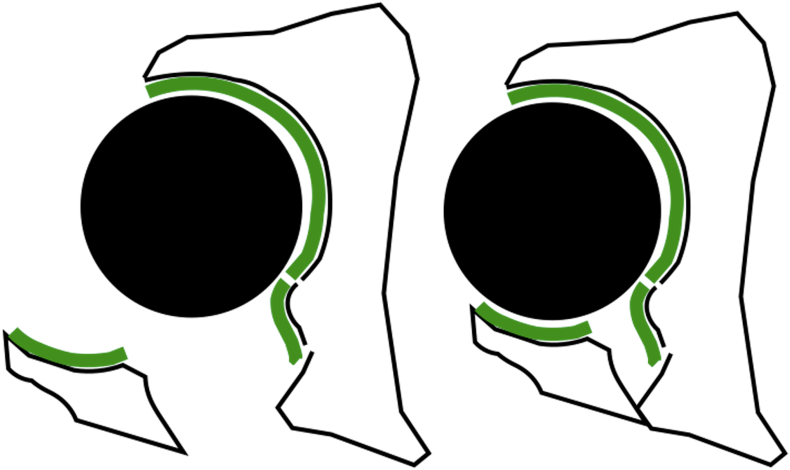
Fig. 2.
Marginal impaction seen in posterior acetabular wall fractures. Impacted fragment, noted prominently after initial reduction of posterior wall is usually rotated with osteo-cartilaginous component with or without soft tissue attachments to it.
We reviewed here the characteristics of acetabular impaction fractures of dome and posterior wall, exploring surgical procedures, approaches and techniques for achieving open reduction and internal fixation.
1.1. Acetabular dome impaction injuries
Anatomic reduction and stable fixation of acetabular dome aid in early mobilisation with good functional outcome as in any articular injuries. Among elderly group, to facilitate early mobilisation, stable fixation of columns are preferred by most surgeons than anatomic reduction as any arthritic changes can be contemplated to total hip arthroplasty. But, the value of early mobilisation cannot be overemphasized by stable fixation of the column alone, as an inadequate reduction of dome impaction leads to loss of mechanical support, thereby causing secondary loss of reduction.9,10 While attempting reduction and fixation of dome impaction injuries, careful pre-operative planning is needed with respect to approach, reduction tools based the location and configuration of fracture.
With the ilioinguinal approach the anteriomedial ‘dome impaction’ can be visualized either through an independent iliac cortical window or via the pre-existing fracture of the internal iliac fossa.10 Zhuang et al.2 recommended using ilioinguinal approach to address the dome injuries via the pre-existing iliac bone fracture line. Modified Stoppa’s approach is gaining popularity in management of such injuries as it gives access to anterior column and quadrilateral plate.11 Collinge and Lebus12 have described a detailed technique of reduction and fixation of the acetabular dome fractures by modified Stoppa’s approach. They disimpacted the incarcerated fragment through the quadrilateral plate fragment after the femoral head is reduced under the lateral acetabular dome. Casstevens et al.13 describe the reduction of the dome fragment via the anterior column fracture or an osteotomy along the pelvic brim using Modified Stoppa’s technique. Anterior column fracture extending into the quadrilateral plate is used to pass reduction tools to elevate the incarcerated fragments. In cases where fracture line extends more laterally, and oblique fractures of anterior column dome impaction cannot be accessed through fracture planes, osteotomy of anterior column/ilium (iliopectineal line) is advocated. Laflamme and Hebert-Davies9 describe the direct reduction of the impacted fragments by Modified Stoppas approach after accentuating the displacement of the medialised quadrilateral plate fragment below the pelvic brim, i.e. though major fracture lines. Keel et al.14 described an intrapelvic approach - the Pararectus approach, which provides sufficient intrapelvic access to acetabular fractures involving the anterior column and the quadrilateral plate and gives exposure of neurovascular structures at risk from iatrogenic injury. They describe it as advantageous over ilio-inguinal approach as it avoids inguinal hernia and traction injuries to lateral cutaneous femoral nerve. But like any other intrapelvic approaches, there is a high risk of entering the peritoneum and might be unsuitable for obese and patients with bowel obstruction/ileus.
We address the dome injuries by the afore mentioned techniques. Most of them are addressed with modified Stoppa’s approach combined with extended iliac window when required. Acetabular dome fractures extending towards laterally and neglected presentations are preferred with ilio-inguinal or ilio-femoral approach. The impacted fragment is manipulated using a combination of blunt periosteal elevator or by a ball spike or by both tools. Lateral traction of femoral head by schanz pin yields fragments in impaction which can be elevated and reduced and is an important surgical step to disimpact the incarcerated fragment. Once elevated, the traction is released and the fragments are pushed using a ball spike, to achieve anatomic reduction as the femoral head acts as a template of reduction. The residual void is filled with graft or graft substitutes to prevent secondary loss of reduction. Maintaining the reduction is difficult as most of the times the fragment is found free floating after disimpaction and hence provisionally fixed with k wires. K-wire reduction is stabilized using cortical raft screws from medial to lateral, followed by quadrilateral buttress and columnar plating where required [Fig. 3].
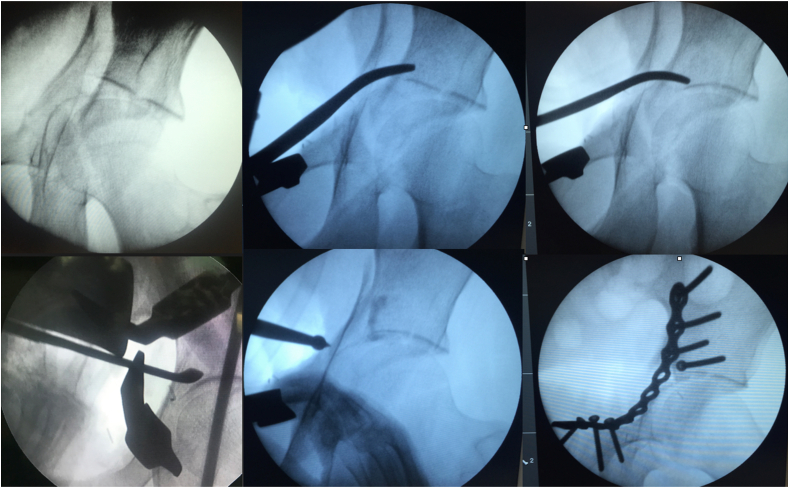
Fig. 3.
Direct reduction - Sequential steps to disimpact the incarcerated fragment and elevate using blunt periosteal elevator, bone grafting, pushing with ball spike and raft screw fixation followed by columnar plating.
When the impacted fragment has been identified on pre- or intra-operative imaging but is not accessible during surgery, alternative means for indirect reduction by independent iliac cortical window as described by Scolaro and Rout can be used.15 According to them, an independent iliac window allows to insert reduction tools to reduce the cranial dome impaction as in proximal tibia fractures. This is a useful technique for a displaced impacted acetabular superior dome fragment that is not connected to the primary fracture fragments [Fig. 4].
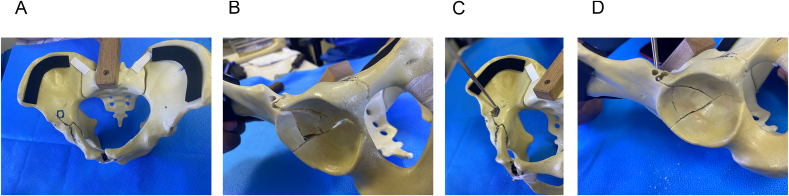
Fig. 4.
Indirect reduction technique: (Fig. 4A) Pelvic saw bone model with fracture line imenacable to direct reduction. Marked square to create a bone window for indirect reduction. (Fig. 4B) Corresponding image showing Acetabulum fracture lines with dome impaction. (Fig. 4C) A Punch used to elevate the impacted osteocartilagenous fragment through Iliac bone window by indirect method. (Fig. 4D) Reduced fracture with elevated dome impaction.
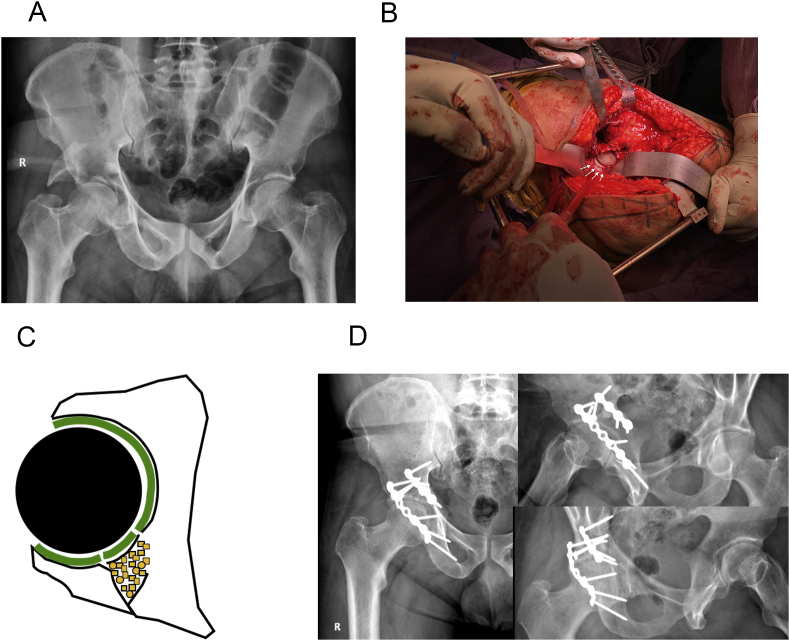
1.2. Posterior wall marginal impaction injuries [Fig. 5]:
Fig. 5.
(Fig. 5A) Posterior wall Marginal Impaction fracture. (Fig. 5B) Intra operative pictures showing the osteocartilagenous fragment (Fig. 5C) Reduction of the osteocartilagenous fragment and filling up the void with bone graft (Fig. 5D) 3 years follow up X ray.
Precise reduction of the posterior wall fracture is very important, as the posterior wall constitutes a large portion of the articular surface, which is particularly loaded in flexion. Marginal impaction fractures represent a severe injury pattern. CT scan is the choice of investigation to mark the site and extent of impaction, than a MRI or X ray pelvis.16 Poor outcomes of posterior wall fractures are thought to be due to posterior wall comminution or cartilage injury, but failure to identify posterior wall marginal impaction injuries add up to the poorly reported outcomes.17 For typical posterior wall fractures, a standard Kocher-Langenbach approach with patient in lateral position is recommended. Posterior wall fragments are identified and are rotated and elevated from fracture bed along with the subchondral bone using a blunt periosteal elevator or a broad osteotome, without further damaging their capsular attachments. Due to compaction of cancellous bone, void left underneath the subchondral bone is filled with bone graft or substitutes to prevent secondary displacement and avoid hip instability.6 In a study by Giannoudis et al. it was noted that 25.8% of patients who had good reduction initially had secondary displacement at follow up attributed to collapse of disimpacted fragment due to lack of underneath subchondral support.7 Hence it is highly recommended even from our experience to graft the void, particularly in marginal impaction injuries. The provisional reduction is converted to stable reduction using a separate cortical screw, if the impacted fragment is large. If the fragments are either peripheral or comminuted, an over contoured spring plate or a cut 1/3 semitubular plate is applied to allow reconstruction plate to be applied over it, so that the captured fragments are held firmly [Fig. 6].
Fig. 6.
Spring plate or a Cut 1/3rd semitubular plate used to hook peripheral fragments for reduction of communited or small peripheral fragments.
Cranial dome marginal impaction injuries are not uncommon and disimpaction of incarcerated fragment in such injuries is difficult to access. Osteotomy of Greater trochanter which easily reflects the abductors, give good access to this area to disimpact the incarcerated bone to achieve anatomical reduction.18 This is followed by other necessary standard columnar and wall fixations followed by greater trochanter fixation with screws.
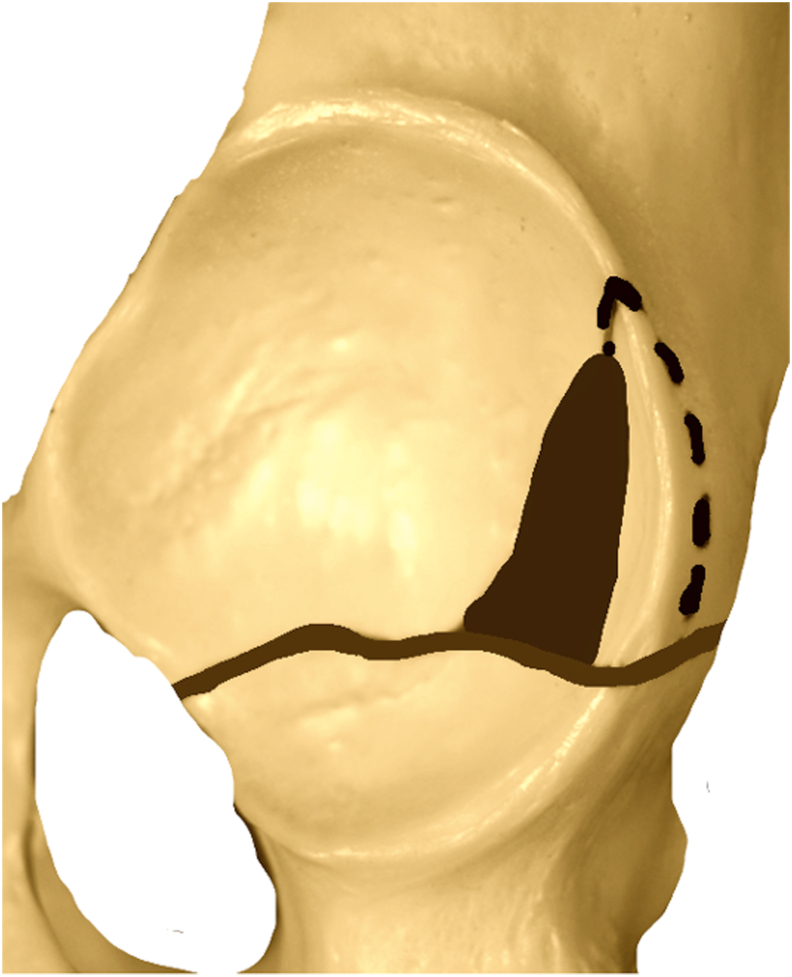
Usually, posterior marginal impaction injuries are accessible through fracture planes. Schroeder et al.19 and Putnis et al.20 reported few cases where in the marginal impaction injuries are not accessible through fracture lines and recommended posterior wall osteotomy to address the same[Fig. 7]. The osteotomy should avoid penetration of the posterior column cortex along the quadrilateral surface. A trapezoidal shape osteotomy created with hip joint capsule as hinge, and the osteotome is utilized to “crack” the remaining intact wall adjacent to the femoral head to expose the impacted fragments. Size and site of osteotomy is templated pre-operatively basing on pattern of marginal impaction.
Fig. 7.
Posterior wall osteotomy (dotted line) to address impacted fractures which are not accesible through fracture plane.
Owing to high energy trauma, acetabular fractures can always be associated with femoral head fractures. Papachristos et al. suggested treatment of such incarcerated impaction of acetabular fractures with concomitant osteochondral femoral head fractures by the use of a posterior wall osteotomy and surgical hip dislocation.21 Maintaining reduction of the communited fracture fragments of posterior acetabulum until solid union takes place is a challenge. Giannoudis et al. described the “two level reconstruction” of the communited posterior wall of acetabulum fractures. They used subchondral mini screws for the stabilisation of comminuted posterior-wall marginal acetabular fragments before applying lag screws and a buttress plate to the main overlying posterior fragment. This two level reconstruction technique reinforced posterior wall fragments mechanically, allowing for early mobilisation and yet maintaining reduction to achieve good clinical outcome.22
We strongly recommend grafting either by auto/allo or graft substitutes while addressing the impaction injuries of acetabulum to prevent secondary loss of reduction, which could be main reason for catastrophic failure. Recent studies have shown a superiority of tricalcium phosphate over autograft particularly in dome impaction injuries.23 While inserting tricalcium phosphate paste in anterior elements, it is advised to use it in slight thick form than in liquid form to avoid spillage which is difficult to remove. Tricalcium phosphate paste form is advantageous over pellet form which need contained defects.24 Excision of multifragmentary posterior wall fragments followed by reconstruction with tricortical iliac crest autograft has also showed good outcomes in the series reported by Sen et al..25 Wedge shaped autografts can also be considered to fill up the void in neglected presentations to fill in the defect after excision or osteotomy of the malunited fragment[Fig. 7]. Morselised allografts have also shown to provide good mechanical strength without any loss of secondary reduction in posterior wall injuries, without any donor site morbidity and complications related to artificial substitutes.26
2. Summary
Acetabular impaction fractures are earlier considered to be one of the main criteria for failure following their internal fixation.1,2,27 Most of these presented series have short study groups and no data regarding the elevation of impacted fragment and any graft used. When direct visualisation techniques with appropriate approach is used, reduction of the impacted fragment yielded good outcomes.9 Severely community and impacted fragments with multifragmentation have fair outcomes compared to large impacted fragments reduced anatomically and fixed using a raft buttress screw.13 Cases with severe comminution of posterior wall can be considered for reconstruction using a tricortical autograft for better outcome. No indirect reduction technique can do justice to achieve anatomical reduction which is possible only through direct access for direct reduction. Proper pre-operative planning and knowledge of strategic alternatives to have direct access to the incarcerated fragment helps in achieving proper reduction which is required for good outcome.
Declaration of competing interest
The authors declare no conflicts of interest.
References
- 1.Anglen J.O., Burd T.A., Hendricks K.J., Harrison P. The “Gull Sign”: a harbinger of failure for internal fixation of geriatric acetabular fractures. J Orthop Trauma. 2003;17:625–634. doi: 10.1097/00005131-200310000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Zhuang Y., Lei J.L., Wei X., Lu D.G., Zhang K. Surgical treatment of acetabulum top compression fracture with sea gull sign. Orthop Surg. 2015;7(2):146–154. doi: 10.1111/os.12175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ferguson T.A., Patel R., Bhandari M., Matta J.M. Fractures of the acetabulum in patients aged 60 years and older: an epidemiological and radiological study. J Bone Joint Surg Br. 2010;92:250–257. doi: 10.1302/0301-620X.92B2.22488. [DOI] [PubMed] [Google Scholar]
- 4.Gary J.L., Paryavi E., Gibbons S.D. Effect of surgical treatment on mortality after acetabular fracture in the elderly: a multicenter study of 454 patients. J Orthop Trauma. 2015;29:202–208. doi: 10.1097/BOT.0000000000000223. [DOI] [PubMed] [Google Scholar]
- 5.Letournel E., Judet R. second ed. Springer; New York: 1993. Fractures of the Acetabulum. [Google Scholar]
- 6.Brumback R.J., Holt E.S., McBride M.S., Poka A., Bathon G.H., Burgess A.R. Acetabular depression fracture accompanying posterior fracture dislocation of the hip. J Orthop Trauma. 1990;4(1):42–48. doi: 10.1097/00005131-199003000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Giannoudis P.V., Kanakaris N.K., Delli Sante E., Morell D.J., Stengel D., Prevezas N. Acetabular fractures with marginal impaction: mid-term results. Bone Joint Lett J. 2013;95-B(2):230–238. doi: 10.1302/0301-620X.95B2.30548. [DOI] [PubMed] [Google Scholar]
- 8.Mears D.C., Velyvis J.H. Acute total hip arthroplasty for selected displaced acetabular fractures: two to twelve- year results. J Bone Joint Surg Am. 2002;84:1–9. doi: 10.2106/00004623-200201000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Laflamme G.Y., Hebert-Davies J. Direct reduction technique for superomedial dome impaction in geriatric acetabular fractures. J Orthop Trauma. 2014;28:e39–e43. doi: 10.1097/BOT.0b013e318298ef0a. [DOI] [PubMed] [Google Scholar]
- 10.Tosounidis T.H., Stengel D., Giannoudis P.V. Anteromedial dome impaction in acetabular fractures: issues and controversies. Injury. 2016 Aug;47(8):1605–1607. doi: 10.1016/j.injury.2016.07.020. [DOI] [PubMed] [Google Scholar]
- 11.Yao S., Chen K., Ji Y. Supra-ilioinguinal versus modified Stoppa approach in the treatment of acetabular fractures: reduction quality and early clinical results of a retrospective study. J Orthop Surg Res. 2019;14:364. doi: 10.1186/s13018-019-1428-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Collinge C.A., Lebus G.F. Techniques for reduction of the quadrilateral surface and dome impaction when using the anterior intrapelvic (modified Stoppa) approach. J Orthop Trauma. 2015;29(Suppl. 2):S20–S24. doi: 10.1097/BOT.0000000000000271. [DOI] [PubMed] [Google Scholar]
- 13.Casstevens C., Archdeacon M.T., d’Heurle A., Finnan R. Intrapelvic reduction and buttress screw stabilization of dome impaction of the acetabulum: a technical trick. J Orthop Trauma. 2014;28:e133–e137. doi: 10.1097/BOT.0000000000000005. [DOI] [PubMed] [Google Scholar]
- 14.Keel M.J., Ecker T.M., Cullmann J.L. The Pararectus approach for anterior intrapelvic management of acetabular fractures: an anatomical study and clinical evaluation. J Bone Joint Surg Br. 2012;94(3):405–411. doi: 10.1302/0301-620X.94B3.27801. [DOI] [PubMed] [Google Scholar]
- 15.Scolaro J.A., Routt M.L., Jr. Reduction of osteoarticular acetabular dome impaction through an independent iliac cortical window. Injury. 2013;44(12):1959–1964. doi: 10.1016/j.injury.2013.07.012. [DOI] [PubMed] [Google Scholar]
- 16.Martins e Souza P., Giordano V., Goldsztajn F., Siciliano A.A., Grizendi J.A., Dias M.V. Marginal impaction in posterior wall fractures of the acetabulum. AJR Am J Roentgenol. 2015;204(4):W470–W474. doi: 10.2214/AJR.14.12451. [DOI] [PubMed] [Google Scholar]
- 17.Uchida K., Kokubo Y., Yayama T. Fracture of the acetabulum: a retrospective review of ninety-one patients treated at a single institution. Eur J Orthop Surg Traumatol. 2013;23(2):155–163. doi: 10.1007/s00590-012-0938-7. [DOI] [PubMed] [Google Scholar]
- 18.Siebenrock K.A., Gautier E., Ziran B.H., Ganz R. Trochanteric flip osteotomy for cranial extension and muscle protection in acetabular fracture fixation using a Kocher-Langenbeck approach. J Orthop Trauma. 1998;12(6):387–391. doi: 10.1097/00005131-199808000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Schroeder A.J., Avilucea F.R., Archdeacon M.T. Posterior wall osteotomy of the acetabulum to access incarcerated marginal impaction. J Orthop Trauma. 2017;31(5):e163–e166. doi: 10.1097/BOT.0000000000000759. [DOI] [PubMed] [Google Scholar]
- 20.Putnis S.E., Dala-ali B.M., Bircher M. Posterior wall osteotomy to facilitate reduction of complex acetabular fractures. Injury. 2007;38(10):1214–1217. doi: 10.1016/j.injury.2006.09.022. [DOI] [PubMed] [Google Scholar]
- 21.Papachristos I.V., Johnson J.P., Giannoudis P.V. Treatment of incarcerated impaction of acetabular fractures with concomitant osteochondral femoral head fractures by the use of a posterior wall osteotomy and surgical hip dislocation: a novel technique. J Am Acad Orthop Surg. 2019;27(24):e1086–e1092. doi: 10.5435/JAAOS-D-18-00789. [DOI] [PubMed] [Google Scholar]
- 22.Giannoudis P.V., Tzioupis C., Moed B.R. Two-level reconstruction of comminuted posterior-wall fractures of the acetabulum. J Bone Joint Surg Br. 2007;89(4):503–509. doi: 10.1302/0301-620X.89B4.18380. [DOI] [PubMed] [Google Scholar]
- 23.Leucht P., Castillo A.B., Bellino M.J. Comparison of tricalcium phosphate cement and cancellous autograft as bone void filler in acetabular fractures with marginal impaction. Injury. 2013;44(7):969–974. doi: 10.1016/j.injury.2013.04.017. [DOI] [PubMed] [Google Scholar]
- 24.Moed B.R., Willson Carr S.E., Craig J.G., Watson J.T. Calcium sulfate used as bone graft substitute in acetabular fracture fixation. Clin Orthop Relat Res. 2003;410:303–309. doi: 10.1097/01.blo.0000063788.32430.8f. [DOI] [PubMed] [Google Scholar]
- 25.Sen R.K., Tripathy S.K., Aggarwal S., Tamuk T. Posterior wall reconstruction using iliac crest strut graft in severely comminuted posterior acetabular wall fracture. Int Orthop. 2011;35(8):1223–1228. doi: 10.1007/s00264-010-1177-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Perumal R., Valleri D.P., Gessesse M.T., Jayaramaraju D., Rajasekaran S. Marginal impaction in complex posterior wall acetabular fractures: role of allograft and mid-term results. Eur J Orthop Surg Traumatol. 2020;30(3):435–440. doi: 10.1007/s00590-019-02584-3. [DOI] [PubMed] [Google Scholar]
- 27.Zha G.C., Sun J.Y., Dong S.J. Predictors of clinical outcomes after surgical treatment of displaced acetabular fractures in the elderly. J Orthop Res. 2013;31(4):588–595. doi: 10.1002/jor.22279. [DOI] [PubMed] [Google Scholar]