Abstract
Introduction
The management of acetabulum fractures in osteoporotic elderly, as well as comminuted fractures in younger patients is likely to be difficult. These fractures need specific fixation techniques especially when the quadrilateral plate is involved. Standard implants may not be able to adequately support the fixation, so newer pre-shaped fixation plates have been proposed with some of these already in use. The concept of anatomic plates has come up for many fracture locations for providing a better buttress effect to the comminuted fragments. There has been a need to look for an anatomic buttress plates being developed for acetabulum fractures involving the quadrilateral surface.
Materials and methods
The literature has been reviewed to find the various newer designs that have been used for buttressing the quadrilateral surface in comminuted acetabular fractures. An attempt has been made to study their design characteristics and clinical outcomes. The review also includes the analysis of Anatomic Quadrilateral plate (AQP) used in fixation of acetabulum fracture involving quadrilateral surface in a series of 33 patients.
Results
There has been few anatomical plates developed for the stabilization of acetabular quadrilateral surface fractures. Some of these plates have been successfully used in management of acetabular fractures primarily in young patients. Issues however remain in their application and outcomes in osteoporotic fractures of the acetabulum, as these plates support the pelvic brim fragments either from superior or medial surface. The newer development i.e. ‘Anatomical Quadrilateral Plate’ is optimized to counter the displacement forces due to its positioning on the pelvic brim rather than its superior or medial surface. Other special features include the possibility of longer screws across bone due to oblique position of holes, the typical location of a locking hole on the plate beam which permits dual cortical compression fixation either by using a bigger screw or a specially designed screw in screw construct across the supra-acetabular corridor. The option of using hybrid fixation of both locking and unlocked screws in AQP allows proper stress distribution on the underlying bone, aiding both primary as well as secondary stability. The minimum of one year post surgery outcome of patients having acetabular fixation using this Anatomic quadrilateral plate has been analyzed in 33 patients. Twenty three of these were aged more than 50 years and 28 out of total 33 were males. Associated injuries included Ipsilateral lower limb injury in 2 patients and distal radius fracture in 5 patients. The fracture pattern included ‘Anterior column posterior hemi-transverse’ in 10 patients,’ Associated Both Column’ injury in 9 and ‘T type’ acetabular fractures in 8 patients. Isolated ‘Anterior column’ was fractured in 6 patients. The surgical approach was ‘Anterior Intra-pelvic’ (AIP) in 23 patients and ‘Modified Ileo-femoral’ in other 10 patients. One patient had additional K L approach. Among the implants, the AQP plate was used without its pubic arm in 6 patients. The post-operative x rays showed anatomical reduction in 28 patients, while other 5 had gaps and/or steps up to 2 mm size. In subsequent car, one of these patients needed hip arthroplasty for problem arising due to collapse in fixation within six months. EQ 5D 5L telephonic score was used to know the outcome at minimum of one year follow up in 33 patients. As per this score, only 3 patients had an issue with mobility, with only one having problem in self-care activity. Six patients complained of minor limitations in carrying out their usual activities and only one patient had anxiety affecting him. In their self-assessment of overall health status, 22 patients marked it 100, 7 made it 90, 3 as 80 and 1 had marked it as 70 in a score range of 0–100. Considering the predominant elderly profile in this series of patients, the acetabular reconstruction using ‘Anatomic quadrilateral plate’ has shown encouraging results.
Conclusion
For stabilization of acetabular fractures involving quadrilateral surface area and pelvic brim, various new implants have been used. The Anatomic quadrilateral plate due to its anatomical shape, the various options in fracture fixation is best optimized for management of comminuted acetabulum fractures especially in poor quality bones. It has been successful in achieving good outcome in elderly group of patients having these complex injuries.
Keywords: Acetabulum fracture, Quadrilateral plate fractures, Osteoporosis, Anatomical plate, Anterior column fractures, Comminution, Dual cortical fixation
1. Introduction
Management of a patient having acetabular fracture is usually a challenge to the orthopaedic surgeons, due to the inherent difficulties in getting the fragments reduced anatomically and fixed. It is well-established that acetabular fractures in elderly patients tend to be more difficult to handle due to additional co-morbidities associated with the age as well as poor bone quality due to osteoporosis which affects both the injury pattern and its comminution. Incidentally the group of patients 65 years and older, has been observed to be the fastest growing segment in acetabular fractures.1 Furthermore, these individuals are becoming increasingly active, better informed and also have high expectations for their health outcomes. In contrast to younger patients, where high velocity trauma in MVA is the usual cause, elderly patients get these fractures mostly by fall within their homes i.e. a low velocity injury. During the fall, the primary impact occurs on greater trochanteric area and the femur head is pushed medially and strikes on the quadrilateral plate.2 This way the acetabular fractures tend to involve primarily the anterior column or both columns and invariably accompanied by comminution around the pelvic brim and quadrilateral plate area.3 In elderly patients, this pattern is often accompanied by impaction of the anteromedial weight bearing dome, seen as separate cortical density giving appearance of so called “gull sign”. The comminution at impact site creates high chances of failures in achieving anatomical reduction fracture fragments even with the surgical intervention. Matta4 achieved anatomic reduction in 74% of patients younger than 60 years; but only 44% in patients over 60 years. Worse clinical results were associated with increased patient age as Miller et al.5 also found that anatomic reduction of the acetabular dome was compromised in elderly patients. In their study of 45 patients with a mean age of 67 years, anatomic reduction was 58% when evaluated by plain radiographs; however, this number decreased to 11% when evaluated by postoperative CT. They concluded that even in experienced hands, anatomic reduction of acetabular fractures in geriatric patients was possible in less than half, secondary to poor bone quality and extensive comminution. The rate of conversion to THR is also much higher i.e. 23.1% in the elderly population when compared to 8.5% in all age groups.6
In the treatment of such injury patterns due to osteoporosis with comminution, there is expected difficulty in reduction and stabilization of each displaced fragment. Any impacted articular pose further difficulty in achieving congruent articular surface. Further the low-quality cancellous or cortical osteoporotic bones in elderly lack enough mechanical strength for stable anchorage of plates or screws affecting the primary stability.7 Secondary stability is also affected as with gradual loading, in poor quality bone, the purchase of the fixation screws can fail prematurely and lead to subsidence of reduced fracture fragments, cut out by metal hardware & ultimately failure of overall fracture construct.8 To minimize the complications of immobilization, there is a need for more stable construct stability in acetabular fracture fixation in elderly patients so as to allow rapid rehabilitation as these patients may not adhere to the post-operative partial weight bearing protocols. It has been established that there is decrease in holding power of plate-and-screw fixation in osteoporotic bone fractures leading to high fixation failure rate, (10–25%).9 This inability to obtain adequate stability in such patients has led to increase in the use of primary arthroplasty as a treatment option. Though the technical quality of arthroplasty may also be compromised due to weaker bone in such elderly acetabulum fractures.
While early improvement in the bone quality is not possible in such scenario, the alternative option is to use such pelvic implants which can help in getting more stable osteosynthesis even in such osteoporotic bones.10 One of the option described has been the application of long screws passing across the supra pectineal plate going down on medial surface of quadrilateral area, and buttressing it.11 But till date, no specific evaluation has been made for the available implants supporting the quadrilateral surface anatomically. So the aim of this review is to find various anatomic plates designed for this purpose.
1.1. Development till date on intra-pelvic plates
Primary access for all anteromedial acetabular injuries have been the ilio-inguinal approach in last 60 years, so the conventional plates have been used with their positioning on the superior surface of pelvic brim and any medial support wherever required was with use of either longer screws across the quadrilateral plate or by buttressing it using an extra plate from supra-pectineal area downwards. For this buttressing effect, either the standard pelvic plates have been used as spring plates or one of the plates like T-plate, H plate, 1/3rd semi-tubular plate have been the option.6 The issues with these buttressing plates are the difficulties in contouring these plates to the surface of quadrilateral area and their ability to adequately buttress it. Fixation failures with continued hip loading has been the frequent outcome in many of these cases which eventually ends up with secondary arthroplasties.
Lately many newer designs have come up with pre-bent plates with inferior extensions supposed to buttress the quadrilateral area.12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23With the increasing use of Anterior Intra pelvic approach, there has been options of using primarily the medial support, and the extra fixations going up to the superior surface. Few of these designs have been clinically used with variable results. This has also been observed that with regard to the periacetabular surface of the inner pelvis, the pelvis can be considered sufficiently symmetric for using the mirrored contralateral hemipelvis as a template for patient-specific implants in acetabular fracture fixation.11
A, Zhang et al.12 in 2019 had reported an anatomical Quadrilateral Surface plate, which has been used in a total of 26 young patients having displaced fractures involving quadrilateral surface. Anatomical and good reductions were obtained in 23 patients and the mean Merle d’Aubigne score at final followup was reported to be 16.38 ± 1.33 points. It was concluded that such satisfactory fixation can be obtained by using an ‘anatomic quadrilateral plate system.’
B, Zha et al.13 reported in 2020, a retrospective analysis of 24 patients with acute displaced quadrilateral plate fractures of the acetabulum treated by a new implant named acetabular fracture reduction internal fixator (AFRIF) in patients with mean age of 61.5 ± 9.2 years (range, 31–82 years). In a followup analysis of more than 45 months duration, no re-protrusion of the femoral head was observed. Twenty of the 24 patients had good or excellent radiological outcomes, emphasizing the buttress role of such a quadrilateral plate.
C, The acetabulum wing plate is primarily infra-pectineal with superior extensions for screw holes. In a study by Schafler et al.14 observed this plate to be promising as it helped in getting satisfactory results in their patients. The osteosynthesis is performed with the AIP approach, in combination with the first window of the ilio-inguinal approach. In most patients, the plate was applied without complications, and in some patients, it even supported repositioning of fracture fragments. However its clinical usage has not been reported subsequently.
D, Two anatomical pre-shaped plates primarily a Suprapectineal plate as well as its infrapectineal variant have been in use for some years.15 Egli et al.16 has evaluated this suprapectineal plate, allowing a standard fixation along the iliopectineal line and additionally buttressing the quadrilateral surface, as well as stabilization of posterior column fracture components over the 90° bent triangular plate component from the inner side (true pelvis). It was observed that this supra-pectineal plate facilitates anatomic or at least imperfect fracture reduction quality in respectively 40%, and 23% of all cases.17 At the one year follow-up, their radiological results according to the Matta grading were worse compared to the data of Chesser et al.18 (excellent: 50% versus 84%; good: 25% versus 9%; fair: 11% versus 4%; poor: 14% versus 2%), but comparable to the data by Ma et al.19 (excellent: 43%; good: 37%; fair: 10%; poor: 10%). The reason proposed for these differences in results was easier contouring of conventional plates compared to these 3D-pre-contoured supra-pectineal plates, which have been harder to bend and theoretically allowed some loss of reduction by their imperfect fitting. It has further been commented that it is difficult to distinguish if these results are attributed to the use of the AIP, the new Pelvic 305 PRO System or both. Analyzing these plates, Gras et al.20 have observed that though the guidelines are available for safe screw fixation for the anterior and posterior columns, there might be a concern for intra-articular placement of screws placed through the infra-pectineal part of this quadrilateral buttress plate.
E, ‘Acetabular compression plate with dual cortical fixation’21 is a new implant for buttressing quadrilateral surface area fractures. Keeping up with the expected principles of acetabular fracture fixation in osteoporotic bones, this innovative plate named as Anatomic Quadrilateral plate (AQP) and has been developed to match with the exact anatomical shape of the brim from supero-medial surface. It has a central long curved beam which primarily supports the ilo-pectineal line rather than the superior or medial surface. Though primarily developed with all the options for stabilization of osteoporotic acetabular fractures, it can very well facilitate reduction and stabilization of highly comminuted fractures in younger individuals also.
1.2. It has following structural features
-
-
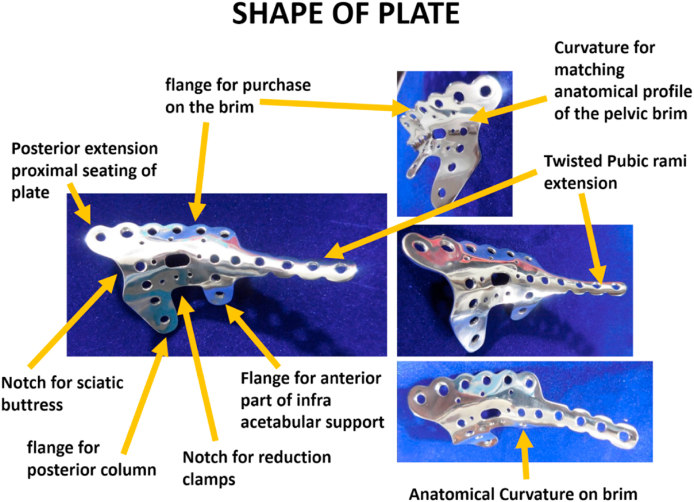
A central beam plate which is curved and contoured to match with the semicircular shape of pelvic brim and supporting it both on the edge of superior and medial aspect of ileo-pectineal line. Posteriorly the beam has a notched shape which is designed to fit anatomically in that part of pelvic brim, and anteriorly it extends to reach over to the pubic symphysis(Fig. 1, Fig. 2).
-
-
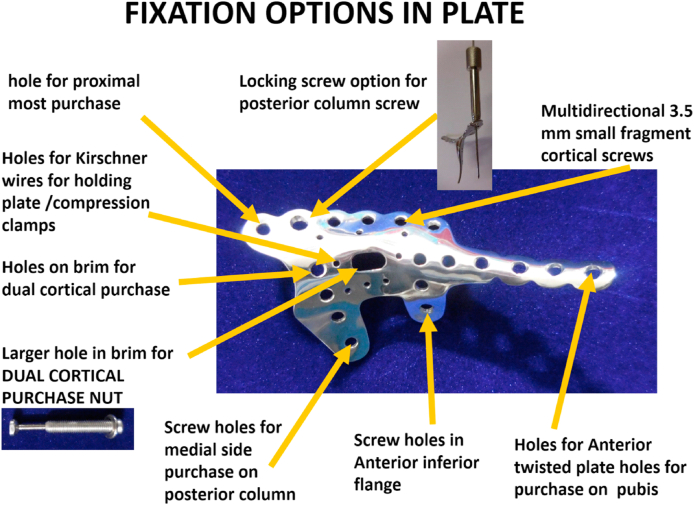
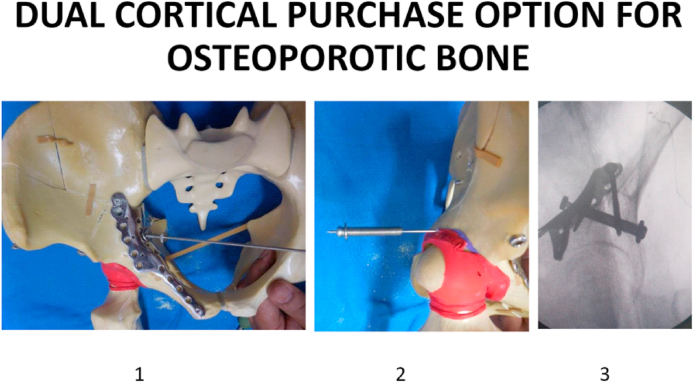
The beam has multiple sized holes for 4 mm screws, 2 mm holes for ball spike application or temporary Kirschner wire fixations. There is one oblong hole with locking mechanism for putting a drill sleeve which is used to hold the plate for intraoperative positioning as well as for directing the drill from pelvic brim to outer cortex of pelvis to reach a point postero-superior to the acetabulum, a safe and thick area. Through this locking sleeve directed drill hole a screw of larger diameter can be passed for good purchase. In osteoporotic acetabulum, the sleeve hole can be used to pass a guide wire over which the specifically designed nuts can glide over, one from inside through the plate, and other from outer cortex percutaneously to get screwed into each other (Fig. 3). This nut construct provides significant compression to the anatomical plate with purchase onto the outer cortex. This fixation is at the outer supra acetabular level and prevents both primary and secondary fixation failures even in the poor quality osteoporotic bones.
-
-
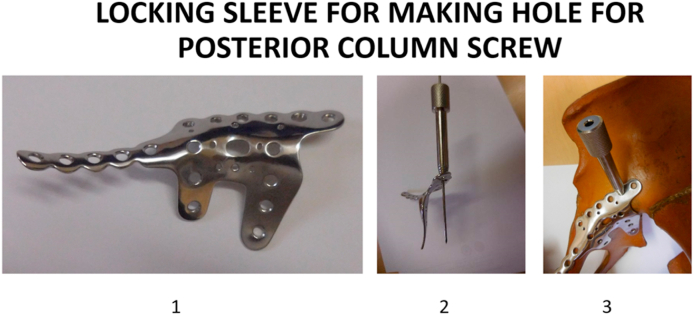
The central beam of plate has about 1.5 cm extension superiorly for its fit on superior surface of pelvic brim from the point of ileo-pectineal eminence. The posterior reach of this extension is little beyond the beam, and has a hole which allows a screw, and is expected to be used as first hold of the plate during its application. Just anterior is a bigger locking hole (5 mm) to engage a sleeve which guides the drill anatomically into the posterior column (Fig. 4). Further anteriorly there are plate holes for allowing 4 mm screw insertions pointing downwards, as well as smaller holes for facilitating Kirschner wires for temporary fixation or for ball spike use.
-
-
The inferior medial side of plate beam has two extensions not joining each other and contoured well to buttress the inner surface of the quadrilateral area, one positioned posteriorly along the posterior column and other buttressing the quadrilateral plate in its anterior margin. Both extensions being separate, allows easier insert of the plate even with clamps holding the reduction in the central part of the quadrilateral plate. These inferior extensions also have screw holes for fixation of fracture fragments along the column.
-
-
These plates have been designed anatomically of three sizes for either side of the pelvis as small, medium and large. The distribution of the holes have accordingly been adjusted with this size variation. If surgery is restricted to lateral buttress only then anterior part of the plate can be cut with plate cutting tools thus a new option for need based limited utilization.
-
-
There are some specifically sized screws, especially the compression nut for the supra-acetabular placement, in which the two parts can screw into each other to achieve and maintain the compression across.
-
-
The plate is not primarily for reduction of fragments as this needs to be obtained before AQP application (Fig. 5). But it can buttress anatomically aligned slightly displaced fragments to their position.
Fig. 1.
Shape of Anatomical Quadrilateral Plate.
Fig. 2.
Fixation options in AQP.
Fig. 3.
Supra-acetabular dual cortical fixation in AQP, 1,AIP approach for insertion of inner screw over guide wire, 2. outer nut over guide wire to compress onto inner screw, 3. Dual cortical fixation.
Fig. 4.
Locking hole in AQP for posterior column screw,1.plate in full profile, 2.locking hole for posterior column 3. sleeve for locking hole.
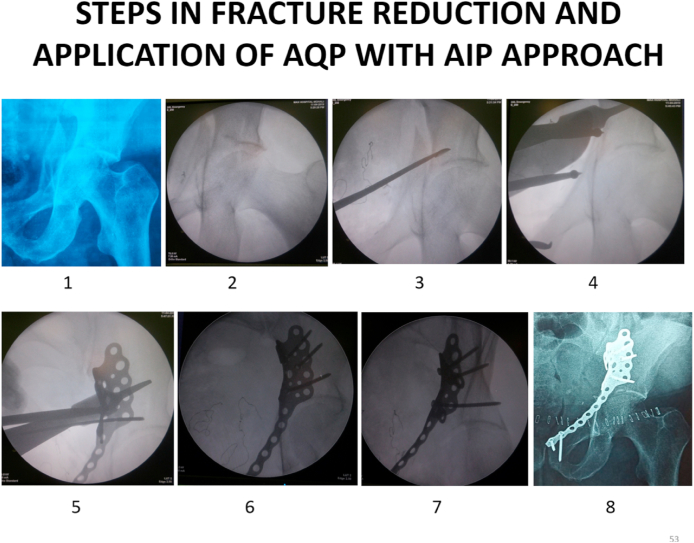
Fig. 5.
AIP approach for fracture reduction and AQP application,1.Preoperative radiograph, 2–7. Reduction images on IITV, 8, Postoperative AP radiograph hip.
In last three years, this Anatomical Quadrilateral plate has been used in 45 patients having quadrilateral surface involvement in acetabular fractures. To know the outcome of these patients, telephonic calls were made to 39 patients who had completed minimum of 12 months after index surgery. The contact telephone numbers were picked up only by 33 patients, who were reviewed for their current status using EQ 5D 5L score.22 This score uses five questions to know the current abilities of patient in: 1, mobility 2, self-care 3, performing usual activities 4, pain or discomfort and 5, anxiety or depression, with 1–5 grading. Then the patient is asked to rate his quality of life from 0 to 100 with 100 meaning as best health he can imagine. Enquiry is also made for any other issues in the affected hip or limb. The profile of patients, their injuries and management details have been given in Table 1.
Out of these 33 patients, 23 were aged more than 50 years,(mean age 65.8 years) and among these, 18 patients had low velocity injury. Ten patients who were less than 50 years of age had significant comminution in quadrilateral surface area of the acetabulum and were the result of motor vehicle accidents. Twenty eight patients were males and right side acetabulum was affected in 20 patients. Two patients had ipsilateral lower limb injuries, while five patients had distal radius fracture out of six having associated upper limb injuries. One case was an acetabular non-union with failed fixation. Among these 33 patients, 16 patients had Anterior column fractures with ten having associated posterior hemi-transverse pattern. Nine had Associated Both Column injury and 8 patients had T type fractures. The surgeries were performed using anterior intra-pelvic (AIP) approach in 23 patients and Modified Ileo-femoral approach was used in other 10 patients. One patient had additional K L approach. Among the implants, the AQP plate was used without its pubic arm in 6 patients. Ante grade posterior column screw was used in 4 patients. Supra acetabular nut was required in three patients where the bones were quite osteoporotic. The fracture reduction of the acetabular dome was perfect in 28 patients, with other 5 showing gaps and or steps of 1–2 mm size. Some patients reported some issues in affected hip i.e. pain off and on in 3 patients and stick support needed in other 3 patients. One patient had undergone THR within 6 months of the index surgery. A total of 30 patients had no issue with mobility, only one had some problem in self-care activity, six patients reported some difficulty in carrying out usual activities, and only one patient complained of anxiety. When asked about their overall health status, 22/33 had marked 100, 7 had marked 90, 3 as 80 and 1 had marked it as 70. Overall the outcome was reasonably good in most patients, in spite of the predominant elderly profile of patients. (Fig. 6, Fig. 7, Fig. 8, Fig. 9).
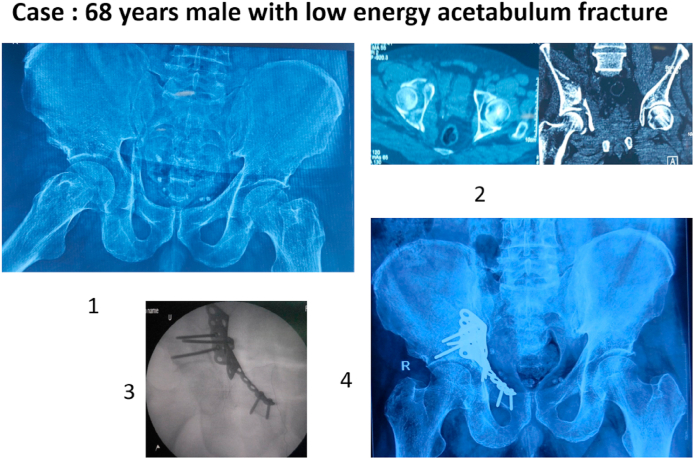
Fig. 6.
Elderly patient with acetabulum fracture, 1–2. preoperative radiograph and CT scan, 3. intraoperative IITV image, 4. post operative radiograph.
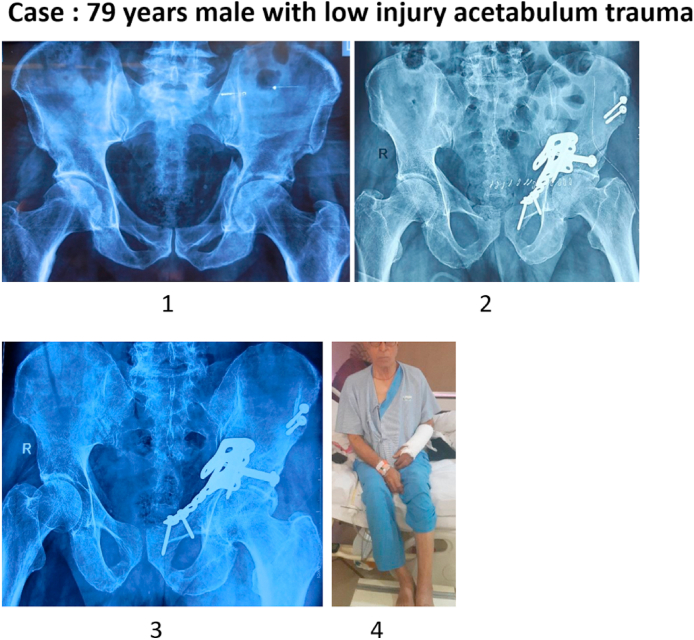
Fig. 7.
Acetabulum fracture in osteoporotic bones,1. preoperative radiograph, 2. AQP with supra acetabular dual cortical compression screw. 3.followup radiograph 4. clinical image.
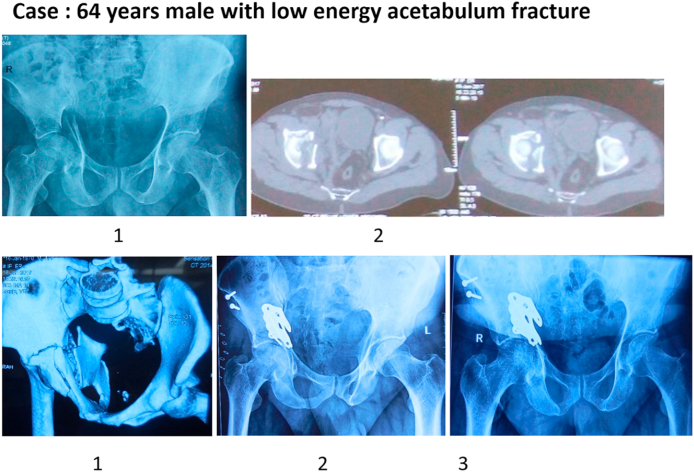
Fig. 8.
Acetabulum fracture reduction using part of AQP. 1–3. preoperative radiograph and CT scans. 4–5 post operative and 6 months FU radiographs.
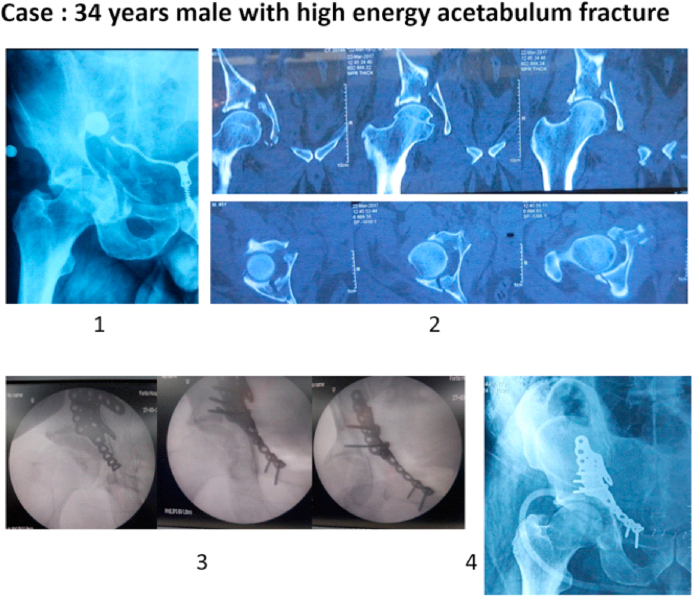
Fig. 9.
Young patient with high energy acetabulum fracture,1–2 preoperative radiograph and CT scans, 3. intraoperative images with oblique views.4. post-operative radiograph. Patent of plate.
2. Discussion
Many new concepts and strategies have emerged in last decades for the fixation of implants and screws in acetabulum fractures15,18,. There is need to define how the proposed plate is able to meet the challenges of fracture fixation in osteoporotic bones as compared to existing available implants.
2.1. The anatomic design of pelvic brim plate
As it is understood, the pelvic brim defined by a line formed by the upper margin of the pubic symphysis anteriorly, on to the pectineal line of the pubis, the arcuate line of the ilium, and reaching to the sacral promontory (the anterior margin of the superior sacrum) posteriorly. The cortical bone has thickness between 0.1 mm and 0.5 mm at the ischium, acetabulum, pubic tubercle, iliac fossa, and posterior superior iliac spine depending upon the stress concentrations at various sites.23 The stress and displacement distributions across these areas change when the fracture occurs. The fracture fixation systems are expected to increase the stiffness of the entire pelvis. In fractures of the quadrilateral plate24 it is expected to counter the substantial medializing forces of the hip joint. It has been conventional to opt for an 8 to 12 holes long plate for intra-pelvic fixation.10 As contouring on table is time consuming, so these plates have been pre-bent in a concave fashion to buttress the superior & medial wall of the acetabulum to support the fracture reduction and its maintenance. It becomes important to define how anatomical the plate should be contoured. Harith et al.25 observed that placing the plate to about 2 mm from the surface maintains its periosteal blood supply to the bone beneath and allows a mechanically stable support at the fracture region. A larger gap between plate and bone immensely increases the stresses in the fracture region, and therefore inhibits the healing process. On the other hand, less than 1 mm gap between plate and bone not only increases the stress at the fracture site but also leads to bone re-fracture occurring due to the insufficient blood supply during the fracture healing.26 So, it is essential to reach an optimal fit between plate and the underlying bone, which has been achieved in some of the plate designs available14,15 as well as in the present “anatomic quadrilateral plate” (AQP). Regarding the optimum size of the anatomical plate, it has also suggested26 that the plates should have big contact area to spread the stress over a larger area of bone in osteoporosis. With increased anatomical support to bone underneath, It has been expected that a well-fitted ‘optimum sized’ plate can also facilitate the process of reduction in terms of axial and rotational alignment of the main fragments.27 Thus the ‘plate fixation should be optimized by securing stable bone contact across the fracture site. It has been observed by Cornell9 that load-sharing fixation devices fair better for osteoporotic metaphyseal locations. In view of these perceptions the spread of the AQP is adequate enough to take care of most common fracture patterns, thus reducing the need for bigger inventory.
The conventional position of the plate through the standard ilioinguinal or AIP approach has been on upper surface of the pelvic brim with fixation screws going downwards into cancellous bone.27 This purchase of screws is reduced in patients with osteoporosis as the underlying cancellous bone is of poor quality. Second plate has been applied on medial surface through AIP approach with screws pointing towards the outer cortex to counter the medially directed forces of injury.28 It is expected that application of these two plates i.e. one on superior surface and the other on medial surface will support the fractures of the brim and quadrilateral area. Due to femur head pushing supero-medially, the primary vector of force causing fracture is usually at pelvic brim which is often maximally displaced with transmitted forces displacing its superior and medial aspect. The design from Stryker uses a combined frame of two plates with a junctional support from superior to medial buttress plate or vice versa to counter both the vectors of injury15. As the apex of injury is at the brim2, the ideal stability should be obtained by direct buttress support to the pelvic brim itself rather than superior or medial aspect. None of the quadrilateral plates primarily support the pelvic brim at ileo-pectineal line. With AQP, the beam primarily buttressing the pelvic brim at the ilio-pectineal line can counter the main vector of displacement effectively and can also support superior and medial surface by its surface extensions. An advantage of such a brim based support is to have holes through this beam, which will allow the screws into the pelvic bone in oblique direction allowing longer screws purchase exactly opposing the deforming forces. It is established that the oosteoporotic bone has limited fatigue strength and can have brittle failure, creep or trabecular crushing with localized strain concentrations.29 Ruden & Augat27 postulated that screws in osteoporotic pelvis fixation should be thinner which generate smaller local strain in cortical as well as trabecular bone compared to thicker screws. Long thin screws provide more flexibility and thus the ability to distribute the load within a large volume of bone. In AQP using the AIP approach, the additional holes in superior and inferior extensions allow further multiple screws if needed for widespread purchase in poor quality bone as similar perceptions have been observed by Kistler et al.30 in usage of quadrilateral buttress plate. Plate fixation by positioning of periarticular long screws as well as the multidirectional positioning has been observed to be the most sufficient fracture stabilization.31
Boguniovic et al.10 have observed that the holding power of screw is reduced due to decreased bone mass, due to comminution leading to screw & implant cut out. The cancellous screws have better bone purchase in osteoporotic bone but if BMD falls below 0.4 g/cm, screw geometry no longer improves fixation strength.32 It is with this perception as well as with additional consideration of the soft tissue constraints and the possibility of joint penetration, locking screws have been suggested to have a role in the management of acetabular fractures.33 It has also been seen that locking screws improve the stability of acetabular fractures by eliminating the need for placement of an interfragmentary lag screw. Though Marintschev et al.34 did not find the increased stability of the construct using low profile “Synthes plate” or “Matta acetabular plate” with locking screws. Further it was also observed that the high stiffness of the locking plate construct, relative to the low stiffness of osteoporotic bone, generates a stress-riser effect, predisposing the construct to periprosthetic fracture, especially under bending loads.9 One of the options they suggested include the replacement of some of the screws to be with locking hole making it a Hybrid fixation, which improves the bending strength by 40% without affecting the ability of the plate to withstand torsional or compressive loads. Thus the acetabular fractures in elderly should be stabilized with the use of a plate which has some traditional and some locking screws, making it a hybrid fixation. This has been achieved in AQP, where posterior column screw has locking option in addition to guiding the drill in anatomical corridor of posterior column. Another option for locking also is also available in AQP at the beam of plate in an oval hole both for directional guidance sleeve as well as locking screw in to supra acetabular area.
One of the option for more secure plate fixation in osteoporotic bone is to have more of cortical purchase of screws in contrast to the cancellous bone as it is usually compromised.35 Maximising this cortical purchase is only possible within the limits of the given anatomical situation and the allowable surgical technique. The plate application on the quadrilateral area is challenging due to its anatomical relationship to the acetabulum, restricting the options of bi-cortical purchase to the screws. While the screws from superior surface downwards can be longer screws, from medial to lateral direction, the length available is restricted both in numbers which can be applied as well as length. The plate can be made more secure if screws are passed obliquely downwards and outward, which is possible with holes on the plate beam over the ileo-pectinal line. This site of plate also permits a screw just superior to acetabulum and this is actually the area which is under maximal stress during weight bearing.16
A concept that is building up in fixation of fractures include ‘Far cortical locking’ where the threads at the tip achieve purchase only in the far cortex. Smooth shaft of screw decreases the stiffness of the plating construct by acting as an elastic cantilever beam. Flexible fixation by FCL reduces stiffness by 80%–88% to actively promote callus proliferation.36 The load is evenly distributed between FCL screws to mitigate stress risers at the end screw. They have shown the increase in callus volume as 36% higher, and bone mineral content as 44% higher. It has been further observed that mechanically, specimens with FCL implant construct becomes 54% stronger in torsion & will have 156% greater energy to failure in torsion. Progressive stiffening occurs by near cortex support of FCL screws and provides additional support under elevated loading.36,37 This concept has been further taken by the use of slotted in place of standard holes in the plate. This way the screw crosses the plate with its head compressing on proximal cortex by its holds the opposite cortex only by use of a nut over the screw. This concept is labelled as ‘Screw locking element’ (SLE) and function is similar to the far cortical locking technique as construct stiffness is reduced while the overall fixation stability is maintained.38 This locking of screw over the far cortex only allows micro-movement at the plate-screw interface as well as within the proximal cortex envelope of the screw. Fixation strength of the construct is better maintained, since the engagement of the screw in SLE is independent of the bone quality. Thus even a single screw with SLE in a construct of fixation avoids any disengagement of the plate where the remaining screws (without SLE) maintain the fixation of the construct. The use of SLE avoided loosening of the system and stimulated stronger osteotomy consolidation.
In the best interest of the patient, any implant in pelvic fracture construct should be load sharing, should be of sufficient strength, and contains least amount of metal ware. It is a very well perceived concept that a curved plate resists a higher bending load when it is directed towards the center of the arc.39 As compared to flat plates across the pelvic brim on ileopectineal line, same material contoured to its curvature anatomically will be much stronger. This curvature and the plate thickness proportionately influence plate resistance to load. A plate contoured on the pelvic brim with curvature will have better strength than a flat plate on superior side or on medial side with same amount of metal ware.
Surgical approach for any fixation should provide wide exposure to the injury area. In elderly patients due to comorbidities, there remains an advice to restrict surgical approach to minimum. Guerado et al.40 have described that for the common injury of anterior column or anterior column posterior hemitransverse, best is to use AIP approach as it has limited morbidity and gives direct access to the pelvic brim. Modified Stoppa approach for ORIF with an infra-pectineal buttress plating of the quadrilateral surface has been advocated to obtain anatomic reduction in more than half of the patients.41 Modified Ileofemoral approach has also been used for stabilization of these fractures involving quadrilateral surface area.42 Good perspective with AQP is that it can be used with any approach, though AIP is best suited for its application in osteoporotic fractures.
A series of 33 patients, where Anatomic quadrilateral plate have been used were analyzed for the efficacy of concepts used in the design. Among these 33 patients, majority were higher than 50 years of age and 18 had low velocity trauma indicative of osteoporosis. The satisfactory outcome in most of these patients highlights the importance of both primary and secondary stability achieved by using this AQP even in osteoporotic bones. This outcome is much better than the reported literature for this age group patients having acetabulum fractures involving quadrilateral surface. The successful outcome in younger patients also highlights the role of this plate for highly comminuted fractures of the pelvic brim and quadrilateral surface. Thus the efficacy of anatomic quadrilateral plate in acetabulum fractures is well substantiated in this preliminary report of its clinical usage.
3. Conclusions
Anatomical quadrilateral plate has a design which can help in the reduction and fixation of acetabulum fractures especially in osteoporotic bones. The anatomically curved and contoured AQP beam has superior and inferior extensions which can adequately buttress the acetabulum fracture area. It has all the options for temporary hold using Kirschner wires or ball spike, for the definitive purchase with multiple multidirectional screws, for locking screws into posterior column as well as supra acetabular bi-cortical purchase needed in osteoporotic bones by using specially designed screw into screw nut to give SLE effect. Its inferior extensions support both the anterior and posterior part of quadrilateral surface. This AQP can be fixed in its position without taking off the reduction clamps. This plate can be applied through any standard approach for anterior column including the AIP approach.
Thus with the incorporation of all recent concepts in plate design, it is presumed that the proposed AQP is likely to be useful in the reduction and maintenance of acetabulum fractures in elderly osteoporotic bones as well as in younger patients.
Author statement
The conceptualization, draft preparation, investigation, reviewing and editing has been done by Ramesh K Sen
Declaration of competing interest
The authors have none to declare.
References
- 1.Henry P.D.G., Kreder H.J., Jenkinson R.J. The osteoporotic acetabular fracture orthop. Clin N Am. 2013;44:201–215. doi: 10.1016/j.ocl.2013.01.002. [DOI] [PubMed] [Google Scholar]
- 2.Lansinger O., Romanus B., Goldie I.F. Fracture mechanism in central acetabular fractures. Arch Orthop Trauma Surg. 1979;94:209–212. doi: 10.1007/BF00618448. [DOI] [PubMed] [Google Scholar]
- 3.Ferguson T.A., Patel R., Bhandari M., Matta J.M. Fractures of the acetabulum in patients aged 60 years and older. J Bone Joint Surg. 2020;92B:250–257. doi: 10.1302/0301-620X.92B2.22488. [DOI] [PubMed] [Google Scholar]
- 4.Matta J.M. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after injury. J Bone Joint Surg. 1996;78A:1632–1645. [PubMed] [Google Scholar]
- 5.Miller A.N., Prasarn M.L., Lorich D.G. The radiological evaluation of acetabular fractures in the elderly. J Bone Joint Surg. 2010;92-B:560–564. doi: 10.1302/0301-620X.92B4.23494. [DOI] [PubMed] [Google Scholar]
- 6.Ortega Briones A., Smith S., Rickman M. Acetabulum fractures in the elderly: midterm outcomes of column stabilization and primary arthroplasty. BioMed Res Int. 2017:4651518. doi: 10.1155/2017/4651518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Osterhoff G., Morgan E.F., Shefelbine S.J., McNamara L.M., Augat P. Bone mechanical properties and changes with osteoporosis. Injury. 2016;47(Suppl 2):S11–S20. doi: 10.1016/S0020-1383(16)47003-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grant K.D., Busse E.C., Park D.K., Baker K.C. Internal fixation in osteoporotic bone. J Am Acad Orthop Surg. 2018;126(5):166–174. doi: 10.5435/JAAOS-D-16-00142. [DOI] [PubMed] [Google Scholar]
- 9.Cornell C.N. Internal fracture fixation in patients with osteoporosis. J Am Acad Orthop Surg. 2003;11(2):109–119. doi: 10.5435/00124635-200303000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Boguniovic L., Chemey S.M., Rothermich M.A., Gardner M.J. Biomechanical considerations for surgical stabilization of osteoporotic fractures Orthop. Clin Nam. 2013;44:183–200. doi: 10.1016/j.ocl.2013.01.006. [DOI] [PubMed] [Google Scholar]
- 11.Karim M.A., Abdelazeem A.H., Youness M. Fixation of quadrilateral plate fractures of the acetabulum using the buttress screw: a novel technique. Injury. 2017;48:1813–1818. doi: 10.1016/j.injury.2017.05.028. [DOI] [PubMed] [Google Scholar]
- 12.Zhang R., Yin Y., Li S. Fixation of displaced acetabular fractures with an anatomic quadrilateral surface plate through the Stoppa approach. Orthopedics. 2019;42:180–186. doi: 10.3928/01477447-20181227-03. [DOI] [PubMed] [Google Scholar]
- 13.Zha G.C., Tulumuhan D.M., Wang T., Wan G.Y., Wang Y., Sun J.Y. A new internal fixation technique for acetabular fractures involving the quadrilateral plate. Orthop Traumatol Surg Res. 2020 Sep;106(5):855–861. doi: 10.1016/j.otsr.2019.09.026. [DOI] [PubMed] [Google Scholar]
- 14.Schäffler A., Freude T., Stuby F., 2. Höntzsch D., Veltkamp J., Stöckle U. Surgical treatment of acetabulum fractures with a new acetabulum butterfly plate, clinical experience and 1-year follow-up. Z für Orthop Unfallchirurgie. 2014;152:26–32. doi: 10.1055/s-0042-106476. [DOI] [PubMed] [Google Scholar]
- 15.Kistler B.J., Smithson I.R., Cooper S.A. Are quadrilateral surface buttress plates comparable to traditional forms of transverse acetabular fracture fixation? Clin Orthop Relat Res. 2014 Nov;472(11):3353–3361. doi: 10.1007/s11999-014-3800-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Egli R.J., Keel M.J.B., Cullmann J.L., Bastian J.D. Secure screw placement in management of acetabular fractures using the suprapectineal quadrilateral buttress plate. BioMed Res Int. 2017;2017:8231301. doi: 10.1155/2017/8231301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Matta J.M. Fractures of the acetabulum: accuracy of reduction and clinical results in 387 patients managed operatively within three weeks after the injury. J Bone Joint Surg Am. 1996;78:1632–1645. [PubMed] [Google Scholar]
- 18.Chesser T.J., Eardley W., Mattin A. The modified ilioinguinal and anterior intrapelvic approaches for acetabular fracture fixation: indications, quality of reduction, and early outcome. J Orthop Trauma. 2015;29(Suppl 2):S25–S28. doi: 10.1097/BOT.0000000000000268. [DOI] [PubMed] [Google Scholar]
- 19.Ma K., Luan F., Wang X. Randomized, controlled trial of the modified Stoppa versus the ilioinguinal approach for acetabular fractures. Orthopedics. 2013;36:e1307–e1315. doi: 10.3928/01477447-20130920-25. [DOI] [PubMed] [Google Scholar]
- 20.Gras F., Marintschev I., Grossterlinden L. The anterior intrapelvic approach for acetabular fractures using approach-specific instruments and an anatomical-preshaped 3-dimensional suprapectineal plate. J Orthop Trauma. 2017 Jul;31(7):e210–e216. doi: 10.1097/BOT.0000000000000829. [DOI] [PubMed] [Google Scholar]
- 21.Acetabular Compression Plate with Dual Cortical Fixation. Patent: International publication no. WO 2018. 069939 A1 publication date 19.04.2018 Mfd by Giaplus co. India
- 22.Herdman M., Gudex C., Lloyd A. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L) Qual Life Res. 2011;20:1727–1736. doi: 10.1007/s11136-011-9903-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Holm N.J. The Internal stress patterns of the Os Coxae. Acta Orthop Scand. 1980;51:421–428. doi: 10.3109/17453678008990818. [DOI] [PubMed] [Google Scholar]
- 24.El Nahal W.A., Karim M.A., Khaled S.A., Abdelazeem A.H., AbdelazeemH Quadrilateral plate fractures of the acetabulum: proposition for a novel classification system. Injury. 2018;49:296–301. doi: 10.1016/j.injury.2017.11.041. [DOI] [PubMed] [Google Scholar]
- 25.Harith H., Malekani J., Schmutz B., Schuetz M., Yarlagadda P.K.D.V. A method for optimal fit of patient specific fracture fixation plates. Proc IMechE Part L: J Materials: Design and Applications. 2016;230(1):28002–28290. [Google Scholar]
- 26.Fouad H. Effects of the bone-plate material and the presence of a gap between the fractured bone and plate on the predicted stresses at the fractured bone. Med Eng Phys. 2010;32(7):783–789. doi: 10.1016/j.medengphy.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 27.Ruden C., Augat P. Failure of fracture fixation in osteoporotic bone. Injury. 2016;47(S2):S3–S10. doi: 10.1016/S0020-1383(16)47002-6. [DOI] [PubMed] [Google Scholar]
- 28.Laflamme G.Y., Hebert-Davies J., Rouleau D., Benoit B., Leduc S. Internal fixation of osteopenic acetabular fractures involving the quadrilateral plate. Injury. 2011;42:1130–1134. doi: 10.1016/j.injury.2010.11.060. [DOI] [PubMed] [Google Scholar]
- 29.Spitler C.A., Kiner D., Swafford R. Generating stability in elderly acetabular fractures—a biomechanical assessment. Injury. 2017;48:2054–2059. doi: 10.1016/j.injury.2017.07.020. [DOI] [PubMed] [Google Scholar]
- 30.Kistler B.J., Smithson I.R., Cooper S.A. Are quadrilateral surface buttress plates comparable to traditional forms of transverse acetabular fracture fixation? Clin Orthop Relat Res. 2014;472:3353–3361. doi: 10.1007/s11999-014-3800-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fan Y., Lei J., Zhu F., Li Z., Chen W., LiuX Biomechanical analysis of the fixation system for T-shaped acetabular fracture. Comput Math Methods Med. 2015;2015 doi: 10.1155/2015/370631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Seebeck J., Goldhahn J., Morlock M.M., Schneider E. Mechanical behavior of screws in normal and osteoporotic bone Osteoporos. Bar Int. 2005;16:S107–S111. doi: 10.1007/s00198-004-1777-0. [DOI] [PubMed] [Google Scholar]
- 33.Mehin R., Jones B., Zhu Q., Broekhuyse H. A biomechanical study of conventional acetabular internal fracture fixation versus locking plate fixation. Can J Surg Can J Surg. 2009;52(3):221–228. [PMC free article] [PubMed] [Google Scholar]
- 34.Marintschev I., Gras F., Schwarz C.E., Pohlemann T., Hofmann G.O., Culemann U. Biomechanical comparison of different acetabular plate systems and constructs--the role of an infra-acetabular screw placement and use of locking plates. Injury. 2012;43(4):470–474. doi: 10.1016/j.injury.2011.11.009. [DOI] [PubMed] [Google Scholar]
- 35.Culeman U., Holstein J.H., Kohler D. Different stabilization techniques for typical acetabular fractures in the elderly_a biomechanical assessment. Injury. 2010;41:405–410. doi: 10.1016/j.injury.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 36.Hak D.J., Toker S., Yi C., Toreson J. The influence of fracture fixation biomechanics on fracture healing. Orthopedics. 2010 Oct;33(10):752–755. doi: 10.3928/01477447-20100826-20. [DOI] [PubMed] [Google Scholar]
- 37.Bottlang M., Schemitsch C.E., Nauth A. Biomechanical concepts for fracture fixation. J Orthop Trauma. 2015;29:S28–S33. doi: 10.1097/BOT.0000000000000467. S: 12(0 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Graces Gl, Rodriguez O., Grau-Bassas E.R., Roiz S., Yanez A., Cuadrado A. Use of screw locking elements improves radiological and biomechanical results of femoral osteotomies. BMC Muscoskel Disord. 2014;15:387. doi: 10.1186/1471-2474-15-387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Philip M., Mang’uriu G.N., Oyawa Analysis of curved plate elements using open source software. International Journal of Scientific and Research Publications. 2014;4(7) [Google Scholar]
- 40.Guerado E., Cano J.R., Cruz E. Fractures of the acetabulum in elderly patients: an update. Injury. 2012;43(52):S33–S41. doi: 10.1016/S0020-1383(13)70177-3. [DOI] [PubMed] [Google Scholar]
- 41.White G., Kanakaris N.K., Faour O., Valverde J.A., Martin M.A., Giannoudis P.V. Quadrilateral plate fractures of the acetabulum: an update. Injury. 2013;44:159–167. doi: 10.1016/j.injury.2012.10.010. [DOI] [PubMed] [Google Scholar]
- 42.Sen R.K., Tripathy S., Aggarwal S., Goyal T. Comminuted quadrilateral plate fracture fixation through the ileofemoral approach. Injury. 2013;44:266–273. doi: 10.1016/j.injury.2012.11.002. [DOI] [PubMed] [Google Scholar]