Abstract
Total Hip Arthroplasty (THA) is a well-accepted treatment for established hip arthritis following acetabular fractures. If a conservatively managed or operated case progresses to non-union/mal-union failing to restore the joint integrity, it may eventually develop secondary arthritis warranting a total hip arthroplasty. Also, in recent years, acute total hip arthroplasty is gaining importance in conditions where the fracture presents with pre-existing hip arthritis, is not amenable to salvage by open reduction and internal fixation, or, a poor prognosis is anticipated following fixation.
There are several surgical challenges in performing total hip arthroplasty for acetabular fractures whether acute or delayed. As a separate entity elderly patients pose a distinct challenge due to osteoporosis and need stable fixation for early weight bearing alleviating the risk of any thromboembolic event, pulmonary complications and decubitus ulcer. The aim of surgery is to restore the columns for acetabular component implantation rather than anatomic fixation. Meticulous preoperative planning with radiographs and Computed Tomography (CT) scans, adequate exposure to delineate the fracture pattern, and, availability of an array of all instruments and possible implants as backup are the key points for success. Previous implants if any should be removed only if they are in the way of cup implantation or infected. Press fit uncemented modern porous metal acetabular component with multiple screw options is the preferred implant for majority of cases. However, complex fractures may require major reconstruction with revision THA implants especially when a pelvic discontinuity is present.
Keywords: Acetabular fracture, Total hip arthroplasty, Post traumatic osteoarthritis, Pelvic discontinuity
1. Introduction
Acetabular fractures are the result of significant trauma in young patients compared to their elderly counterparts who are more likely to sustain these injuries as a result of low-energy mechanism. Open Reduction and Internal Fixation (ORIF) remains the gold standard treatment for these fractures.1 However, the surgery is challenging in view of anatomic location and complexity of three dimensional structure. Restoration of congruency of the joint plays an important role in treatment outcome. Nevertheless, post-traumatic arthritis can occur even after anatomical reduction. Overall, high incidence of arthritis has been reported following acetabular fractures ranging from 12 to 57%.2,3 These patients are indicated for total hip arthroplasty (THA) if they present with painful end stage arthritic hip.
Historically, the total hip arthroplasty had been reserved for the late sequelae of acetabular fractures treated with or without surgery. There has been a shift in paradigm where acute total hip arthroplasty is indicated in a selected subset of patients.4, 5, 6 Acute THA provides benefit of immediate postoperative weight bearing thereby alleviating the risk of any thrombotic events, decubitus ulcers and pulmonary complications among these patients.7 The intent of this review article is to provide important insights into the current indications, challenges, surgical technique, implant selection and outcomes of total hip arthroplasty in acetabular fractures based on the recent literature over the last ten years.
1.1. Indications
The main indications for THA after acetabular fractures can be summed up as 4Es as follow8,9:
-
I
Established post-traumatic arthritis or Avascular Necrosis of Femoral Head following fixation or conservative treatment
-
II
Existing hip arthritis or associated fracture of head and/or neck of femur not amenable to satisfactory outcome with fixation
-
III
Elderly patient with comminuted acetabular fractures and osteoporotic bone
-
IVExpected undesirable outcome at an early follow up period after fixation
-
(a)Associated severe articular cartilage injury and marginal impaction of the acetabulum.
-
(b)Persistently subluxated head or neglected fracture dislocation with risk of Avascular Necrosis of Femoral head.
-
(c)Thin and compromised posterior wall or column with risk of fixation failure.
-
(a)
The authors consider indications II to IV as ‘joint at risk’ signs which indicate that these fractures with associated features would likely end up in developing secondary arthritis or avascular necrosis of femoral head warranting total hip arthroplasty.
2. Timing of surgery
Broadly, for management purpose THA in acetabular fractures are classified as acute or chronic and in young or elderly. An acute acetabular fracture has potential for bone healing which makes fragments more likely to heal with THA with or without plate fixation. The healing potential of a chronic fracture is variable and is considered as fibrous non-union thereby warranting a stable construct that bridges the fracture.10Scanty evidence exists to guide when to perform THA for a fractured acetabulum. THA can be considered at three time periods8:
-
1
Early or Acute THA: from the day of injury to 3 weeks
-
2
Delayed THA: from 3 weeks to 3 months
-
3
Late THA: More than 3 months after fracture
3. Radiological assessment and classification
Attention should be given to study the morphology of fracture and plan the fixation accordingly. A complete radiological work up is needed, which includes the following:
-
I
Pelvis with both hips: Antero - Posterior view with 100% magnification, Lateral view of hip and Judet views. These views are mostly sufficient for planning, templating and also to rule out other pelvic injuries.
-
II
CT scan with 3D reconstruction: In complex scenarios including suspected pelvic discontinuity or compromised column support. A 3D model may be needed in cases with grossly distorted fracture anatomy.11
-
III
CT Angiography of pelvis and lower limb especially in cases with prior surgery where bone fragments or implants have migrated into the pelvis.12
-
IV
USG Doppler of the lower limbs in cases who are bedridden for prolonged period and DVT is suspected.13
3.1. Classification
The most common classification system used for acetabular fractures is by Judet and Letournel.14 However, for THA, available articular surface in continuity with stable bone and bone stock for screw insertion are of important considerations. Accordingly, Marmor et al. gave a new classification system based on CT Scan and 3D mapping as shown in Table 115
Table 1.
Classification system for acetabular fractures based on articular surface and bone stock described by Marmor et al.15
| 1. Based on the available zone of articular surface that was fully or partially connected to stable bone | 2. Based on the bone stock available for screw fixation |
|---|---|
| D - Dome zone only P - Posterior zone only A - Anterior zone only DP - Dome and Posterior DA - Dome and Anterior DAP - All zones |
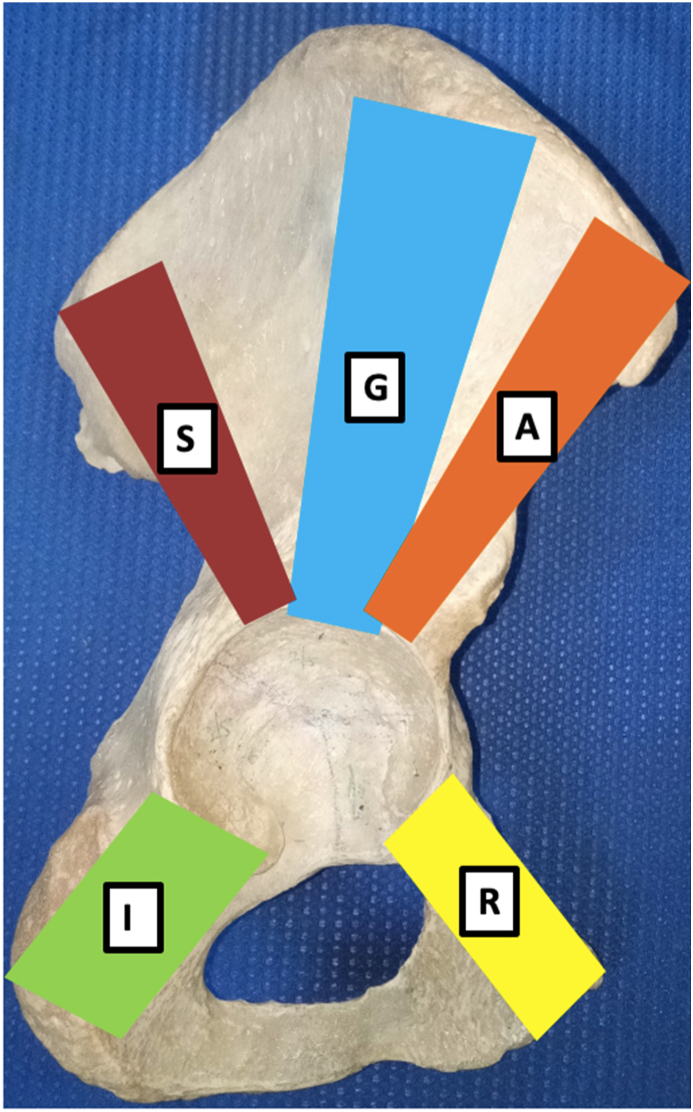
R - Superior ramus pubic corridor A - Anterior corridor G - Gluteal pillar corridor S - Sciatic Buttress corridor I - Ischium corridor |
4. Surgical challenges
There are several surgical challenges that the surgeon has to face while performing a total hip arthroplasty in acetabular fracture whether acute or delayed as enumerated in Table 2 16,17
Table 2.
Surgical challenges in performing total hip arthroplasty in acetabular fracture.
| THA in old case of acetabular fracture | Acute THA in acetabular fracture | |
|---|---|---|
| Conservatively treated | Previously operated | 1. Distorted anatomy 2. Multiple fragments not allowing primary stability 3. Bone defect 4. Acute Pelvic Discontinuity 5. Osteoporosis |
| 1. Distorted anatomy 2. Scar tissue and fibrosis between the bone fragments 3. Possible necrosis of bone fragments 4. Multiple fragments not allowing primary stability 5. Bone defect 6. Mal union 7. Chronic Pelvic Discontinuity |
1. Prior hardware 2. Infection 3. Possible necrosis of bone fragments 4. Bone defect 5. Mal union 6. Chronic Pelvic discontinuity |
|
Tannast et al. identified negative predictors for hip survival following Acetabular fractures treated with open reduction and internal fixation and developed a nomogram which may predict the need for THA within 2 years. Nine independent significant outcome predictors were identified of which six were related to injury or initial evaluation and three with surgical intervention (Table 3).18
Table 3.
Negative outcome predictors following fixation for acetabular fractures.18.
| Related to Injury | Related to surgery |
|---|---|
| Age over 40 years Anterior dislocation Femur head cartilage loss (full thickness) Posterior wall involvement Marginal impaction (40% acetabular cartilage) Initial displacement >20 mm |
Non anatomic reduction Postoperative acetabular roof incongruence Use of extended ilio-femoral approach |
5. Surgical considerations
THA in acetabular fractures should aim at stable fixation of fracture fragments, restoration of the overall shape of acetabulum, and, implantation of stable acetabular component in correct orientation. The need for anatomic reduction of the fracture fragments is obviated as long as the shape of the acetabulum is restored.2The subchondral bone beneath the anterior inferior iliac spine (AIIS) and the ischium in postero-interior acetabulum are the most important regions for acetabular component stability (Fig. 1).The strategy should be to wedge the acetabular component between these two areas.19 If primary stability is not obtained and/or these bony landmarks do not have a stable relationship then an additional fixation with a plate is required to achieve the component stability. Although, careful judgement of the preoperative computed tomography (CT) scan or Judet views may help the surgeon to decide whether THA alone is sufficient or a concomitant plate fixation is required to manage the injury, the confirmation can only be done on operation table during the surgery.
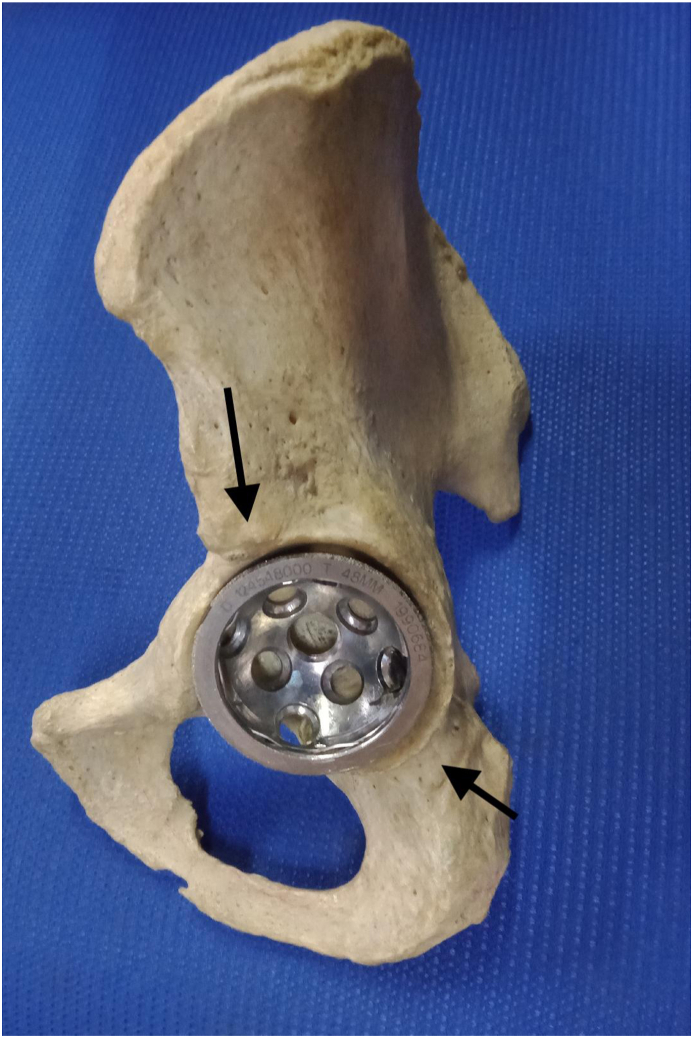
Fig. 1.
Figure showing the important bony landmarks (black arrows) for acetabular component placement during total hip arthroplasty for acetabular fractures. The vertical arrow shows subchondral bone beneath the AIIS and the oblique arrow is showing the ischium supporting posteroinferior acetabulum.
5.1. Principles of total hip arthroplasty in acetabular fractures
-
I
Ascertain that the cause of painful hip is related to acetabular fracture e.g. post traumatic osteoarthritis, avascular necrosis of femoral head, non-union, or, pelvic discontinuity.
-
II
Details of initial trauma, status of sciatic nerve following trauma and/or surgery (if previously operated), prior hardware in situ must be documented. The patient should be explained regarding the risk of sciatic nerve injury as well as the prognosis if already injured.
-
III
Infection must be ruled out in all previously operated cases by hip aspiration if the serum markers (ESR & CRP) are raised and, if infection cannot be ruled out, it is better to perform THA in stages.
-
IV
Bone defects should be classified intraoperatively after debriding fibrosis and freshening of fracture ends as the real defect may be different from that anticipated preoperatively.
-
V
In chronic non-union, aggressive debridement of the fragments must be discouraged to avoid destabilization of the non-union. Rather, only the superficial layer must be debrided to identify the extent of non-union. Loose fragments without any soft tissue attachments and/or too small to be fixed can be taken out and used as autograft.20
-
VI
Implant and instrument inventory should be available over the shelf, including implant removal set and high speed metal cutting drill to address the metalware coming on the way of THA.
-
VII
Any implants which do not interfere with the preparation and implantation of components can be left in situ (Fig. 2 A & B).
-
VIII
THA must permit the patient mobilization as early as possible post-surgery which is an ultimate goal.
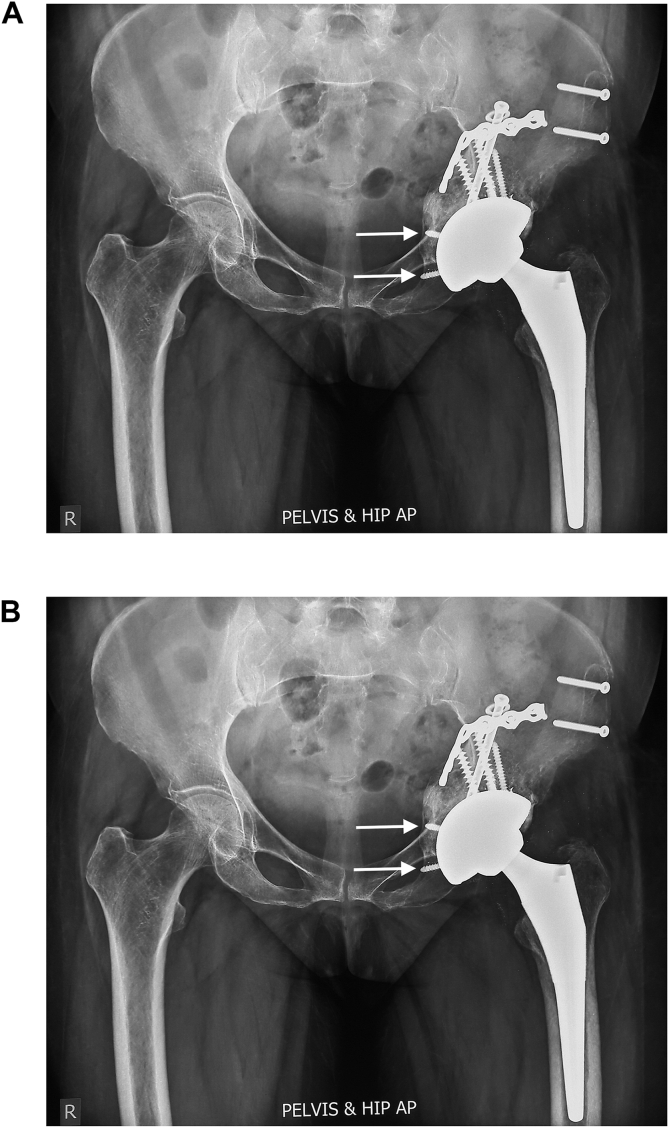
Fig. 2.
Radiograph of Pelvis with both hips in Anteroposterior view showing post traumatic arthritis in left hip following fixation for acetabular fractures (A) Post-operative radiograph following Total Hip Arthroplasty (B). Note the hardware in situ which was retained as they were not coming on the way of THA. Also note the kick-stand screws in the superior pubic ramus as well as the ischium (white arrows).
6. Choice of implants
The choice of THA implant depends on the fracture type, location and comminution. Cementless multihole porous metal cups have been the preferred implants for reconstruction.4,21 Studies have shown high failure rates of cemented acetabular components as compared to press fit acetabular implants.16,22However, few studies have reported satisfactory results even with cemented cups combined with impaction bone grafting.23,24
Complexity of these cases is at par with revision THA scenario; hence, apart from plates an additional back up of implants including metal augments, buttresses and cages may be required. Central contained defects can be addressed with impaction grafting alone while segmental uncontained defects may require structural graft from femoral head autograft or allograft, metal augments or buttresses.25,26 Complex cases with pelvic discontinuity, unstable non-union and major structural defects may require pelvic reinforcement cages combined with structural and impaction grafting with or without a revision shell.
Instability remains a significant issue postoperatively in these cases with dislocation rate reported up to 23%.27,28 Dual mobility cup is helpful in reducing the incidence of dislocation in these cases, and is being preferred these days while treating acetabular fractures by THA.29, 30, 31 These cups can be cemented or uncemented. The uncemented cups can be used in cases with malunited acetabular fractures with good bone in the acetabular bed. The cemented dual mobility cup can either be cemented directly onto the acetabulum or over a Trabecular Metal Revision Shell or Cage.
7. Surgical technique
The critical steps of surgery are outlined as below:
7.1. Approach
Although, the surgical approach is based on the fracture location and comminution, Kocher-Langenbeck approach is the most commonly used approach. Simultaneous fracture fixation and THA implantation becomes easier via this approach. Few authors have advised additional approaches as per fracture pattern e.g. anterior approach especially when there is associated anterior column fracture or direct anterior (Levine) approach.32 For better exposure, incision can be placed a little more superior and anterior than usual. The gluteus maximus attachment at its femoral side can be divided to improve exposure, visualize and protect the sciatic nerve, and, aid in rotation of the limb without any inadvertent femoral fracture.
7.2. Acetabular exposure
Circumferential exposure of the acetabulum is a prerequisite in all cases. Caution should be exercised in all steps to protect the sciatic nerve and branch of inferior gluteal artery. The authors prefer to prepare the femur first in these cases.4,33 After neck osteotomy, the femoral head is kept aside to prepare autograft if required and the preparation for femoral stem done with sequential broaches. The last fitting broach is kept in situ and the femur is pushed anteriorly with the help of a curved retractor against the antero-superior acetabulum. The gluteus minimus and reflected head of rectus femoris are divided to ease displacement of the femur anteriorly so as to achieve wide exposure of the acetabulum.4,33 Radial release of inferior capsule and placement of inferior retractor in the obturator foramen help to identify the Transverse Acetabular Ligament (TAL). A posterior Hohman retractor against the posterior wall of acetabulum, if intact, finally gives a 360° exposure of the acetabulum.
7.3. Assessment of fracture pattern and bone loss
The acetabulum is thoroughly inspected for contained cavitary or uncontained segmental defects. Medial wall is looked for any central defect in the floor. Most severe types include pelvic discontinuity, column fracture with bone loss, or ununited transverse fracture of acetabulum. Pelvic discontinuity is diagnosed when superior part of the pelvis is no longer in continuity with the inferior part.34,35
7.4. Intraoperative bony landmarks
As explained above, the two most important landmarks are subchondral bone in continuity with Ischium and Antero-Inferior Iliac Spine (AIIS) between which the cup is wedged. Continuity of these two points is disrupted in most of the cases including transverse, T type, both column, anterior column-posterior hemitransverse, and, anterior or posterior column fracture, thereby warranting simultaneous fixation before reaming and cup placement.19 Relative exception is isolated posterior wall fracture where continuity between AIIS and ischium is maintained and thus ORIF may not be needed before THA. Posterior and anterior walls are not as crucial to stability.21
7.5. Reduction and stabilization of the column fracture
Although an anatomical reduction is not essential, any major deformity must be corrected to restore the overall shape of the acetabulum for cup implantation. Standard acetabular reduction techniques using pelvic reduction clamps over cortical screws can be utilized to reduce displaced fragments and hold them while plate is applied. Schantz screw placed in ischial tuberosity can be used to derotate inferior fragment. AO femoral distractor can be used to apply traction or distraction intra-operatively. Failure to reduce and approximate a displaced non-union may result in premature failure of THA.36
7.6. Fixation, reaming and grafting
Minimally displaced non-union or acute fractures can be managed alone with reaming and in situ grafting. In cases with displaced non-unions, fracture fragments need to be mobilised, reduced and fixed before reaming and impacting graft in between the freshened fracture gaps. Once the reduction is achieved, contoured curved pelvic reconstruction plate is used to fix the fracture and achieve stable fixation of the columns.
Once stable fixation of column is achieved, one can proceed with acetabular reaming. During reaming of acetabulum, one should assure the fit between AIIS and Ischium by feeling the catch of the reamer. The acetabular reaming is restricted till bleeding surface of bone is achieved in order to conserve peripheral sub-chondral bone.
Contained and cavitary defects can be filled up by impacting the autograft chips or slices from femoral head. In cases with segmental defects, femoral head autograft can be used to reconstruct the defect and reaming is done after fixing bone graft to achieve final shape.23,26 If the bone graft is inadequate or not available, the trabecular metal augments/buttress can be used to build up the defect (Fig. 3 A &B). Once the defect is addressed and final reaming is done, the trial component can be used to assess the size of final acetabular component.
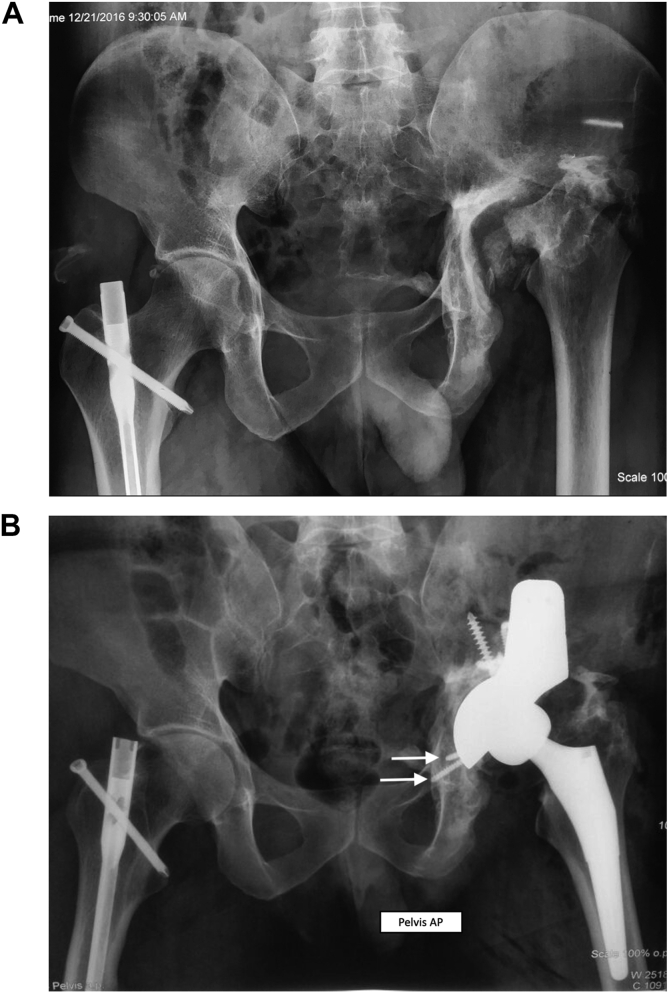
Fig. 3.
Radiograph of Pelvis with both hips in Anteroposterior view showing old acetabular fracture with segmental bone defect in left hip (A) Post-operative radiograph following Total Hip Arthroplasty with use of trabecular metal buttress to address the bone defect as the femoral head autograft was not available (B). Note the hardware in situ which was retained as they were not coming on the way of THA. Also note the kick-stand screws (white arrows).
7.7. Cup implantation and screw placement
Diameter of final reamer dictates the outer diameter of the final cup to be implanted. A minimum of 4 screws with good purchase should be used to fix the cup. Marmor et al. observed that in 93% fractures at least two corridors are available for fixation (Fig. 4). Most commonly sciatic buttress and gluteal pillars are readily available for screw fixation.15 The authors recommend at least one (preferably one each) screw placed inferiorly in superior pubic ramus or ischium to avoid cup failure in abduction, so called “kickstand” screw (Fig. 2, Fig. 3B). Sometimes screw can be directed medially into the quadrilateral surface as well. Modalities to minimize dislocation include use of larger femoral heads and dual mobility cups.37
Fig. 4.
Acetabular corridors for screw fixation. S= Sciatic buttress corridor, G = Gluteal corridor, A = Anterior corridor, I= Ischial corridor, R = Superior pubic ramus corridor.
7.8. Complex fractures requiring major reconstruction
Severe chronic acetabular bone defect or pelvic discontinuity where stable initial acetabular fixation is difficult to achieve may require major reconstruction along with total hip arthroplasty. The following options are described in the literature for such cases:
7.8.1. Cage reconstruction
The cages bridge a defect as well as the fracture with its proximal flange fixed with screws over the ilium and a distal nose buried in ischium. These cages helps to protect the graft while they undergo incorporation and remodelling while allowing early mobilization by fixing the fractures and bypassing the load in fractured acetabulum. They can be used alone or in combination with revision shell as “Cup Cage construct”.38,39 Most of them rely on mechanical fixation alone. Octopus cage®(Depuy Orthopedics, Warsaw, IN) is the only cage with hydroxyapatite coating with potential for osteointegration.40 While using the cages, the superior flange requires an extensive supra acetabular dissection which should be limited within 5 cm of the greater trochanter to prevent injury to superior gluteal nerve and branch of inferior gluteal artery. Inferiorly dissection over ischium should not exceed 2 cm from the postero-inferior part of the acetabular rim to protect the Sciatic nerve.41,42
7.8.2. Cup-cage-construct
Cages are non biological and used alone may pose problems of loosening, breakage and dislocations; hence they are combined with Trabecular metal cups-so called ‘cup cage construct’.38,39 Here, Trabecular metal shell is placed in deficient acetabulum in the position of maximum bone contact with screw fixation, usually retroverted and vertical. A cage is then placed into the cup and fixed to ilium with screws and ischium with flange in the slot. Unitization of the construct is done during cementation of a polyethylene liner or a dual mobility cup over the cage in desired position of maximum stability. The size of the cage predicts the size of cup to be cemented. In such a construct, cage provides initial stability until bone ingrowth occurs over the porous metal shell. In austere environment, Burch-Schneider cage can be used instead of Trabecular Metal Cage to reduce the cost. While using BS cage, the size of TM shell predicts the size of BS cage to be used.33
7.8.3. Acetabular distraction technique
The principle of acetabular distraction technique is to allow lateral and peripheral acetabular distraction while simultaneously generating medial or central compression at the fracture site. Cup is engaged between distracted antero-superior and postero-inferior columns.43,44
7.8.4. Coned hemipelvis reconstruction
The procedure is indicated in most medically frail elderly patients with complex displaced osteoporotic acetabular fractures who are at too high risk for ORIF or ORIF with THA. It bypasses the fracture leading to stable construct and allows immediate full weight bearing. CHP cannot be used in pelvic discontinuity with bone loss.45
7.8.5. Two-stage technique
Two stage technique is used for more severe cases with extensive bone defect or where column fixation is inadequate to support acetabular component during THA. This technique advocates to delay THA by fixing the fractures and grafting the defects in the first stage to allow healing of comminuted fragments making reconstruction easier during the later stage.46, 47, 48, 49 This should not be confused with late THA where the fracture is allowed to consolidate by a year or so before THA is performed. However, two-stage technique has poorly performed historically as compared to other techniques50,51
8. Pearls and pitfalls
Total Hip Arthroplasty in acetabular fractures should not be viewed as a simple solution to a complex issue. The success of total hip arthroplasty in operated case of acetabular fracture depends on the initial reduction and fracture management. The surgeon should be familiar with both pelvic fixation and revision hip arthroplasty. Associated osteoporosis can lead to difficulty in fixation. The surgeon must be familiar with various fixation strategies. Sciatic nerve is at higher risk in view of extensive dissection needed. Intra-operative bleeding can be encountered during scar excision and mobilization of the fragments. Hence, the surgeon must be familiar with the anatomy and methods of achieving hemostasis apart from arrangement of adequate blood and blood products prior to surgery. Post-operative heterotopic ossification is a known complication for which pharmaco-prophylaxis should be started as early as possible.
9. Results and literature review
There have been multitude of advances and revamping of principles in managing acetabular fractures. The current literature supports moving from “fix or replace” towards “fix and replace” when a poor outcome is anticipated. Despite the difficulties associated in performing THA, it provides significant improvement in pain and function. In a systematic review by Stibolt et al., the mean Harris Hip Score (HHS) improved from 41.5 pre-operatively to 87.6 at 4–20 years follow up in 448 patients with acetabular fractures.52 However, these patients have higher likelihood of developing complications like infection, dislocation, sciatic nerve palsy and heterotopic ossification. The 10-year survival is inferior when comparing these patients with a matched cohort of patients undergoing THA for primary osteoarthritis or AVN.53
Literature favours acute THA in elderly due to the fact that the one year mortality rate is as high as up to 25% in these population following ORIF.3 Moreover the conversion rate to total hip arthroplasty has also been reported up to 28% at 2.5 years.3 Acute THA generally yields good clinical results in these patients, however, it must be combined with proper stable fracture fixation.36,54 The conclusion from recent studies and authors’ recommendations are depicted in Table 4.
Table 4.
The results of various recent studies on total hip arthroplasty for acetabular fractures.
| Study (Year) | Type of THA | No. of Patients | Mean age in years (Range) | Mean follow up (Range) | Conclusion/Recommendation |
|---|---|---|---|---|---|
| 1. Aprato et al.55 | Acute | 67 | 71 (65–84) | 27 months (6–53) | Fractures of posterior column and/or wall with severe cartilage involvement, Isolated anterior column and Posterior column with anterior hemitransverse fracture in elderly, Transverse and T type may be treated safely with acute THA. |
| 2. Nicol et al.56 | Acute vs Delayed |
Acute THA – 12 Delayed THA – 14 |
Acute: 81 ± 7 Delayed:76 ± 8 |
5 ± 4 years. | Conversion to THA occurred in 1.8 ± 2.0 years in delayed group. In elderly, acute THA had favourable outcomes as compared to delayed THA. Acute THA be strongly considered in patients with risk factors for failure requiring delayed THA. |
| 3. Liaw et al.57 | Acute | 20 | 73 (60–90) | 26 months | Primary THA with Burch-Schneider anti-protrusio cage provides immediate weight bearing in osteoporotic elderly with acetabular fractures. |
| 4. Lannes et al.29 | Acute | DM-CHP – 26 ORIF – 25 |
DM-CHP - 78 ± 6 ORIF - 75 ± 8 |
12 (1–96) | DM-CHP could be a good therapeutic option in selected patients who are at risk of poor outcomes with ORIF and in case of higher instability risk. |
| 5. Rommens et al.58 | Delayed | 70 | 79 (65–104) | 30 months (17–55) | THA is recommended over ORIF in cases with negative predictive factors (Non-anatomic reduction, subchondral impaction, damage of femoral head & multiple fragments). |
| 6. Milenkovic et al.59 | Delayed | 23 | 51.5 ± 13.8 | – | Conversion to THA occurred in 4.28 years (1–8 following previous fixation. THA gives the best results in the treatment of post-traumatic OA of the hip and AVN of the femoral head after previous osteosynthesis of the acetabular fracture |
| 7. Do MU et al.60 | Delayed | 25 | 58 (36–85) | 50 months | Conversion to THA occurred at 70 months (7–213 months). Outcomes of cementless THA after failed ORIF were satisfactory but with high incidence of postoperative dislocation. |
| 8. Busch et al.23 | Delayed | 67 | 59 (25–87) | 8 years | Conversion to THA occurred at 107 months (1–504 months). Overall, arthroplasty due to posttraumatic osteoarthritis after acetabular fracture resulted in decreased overall survival rates and poorer clinical outcome as compared to primary arthroplasty. |
| 9. Malhotra et al.4 | Acute | 18 | 46.4 (21–57) | 57.6 months (48–70 months) | Modern porous metal cup provides sufficient primary stability and appear suitable for primary THA in acute acetabular fractures |
| 10. Dawson et al.61 | Delayed | 25 | 53.8 | 22 months | Conversion to THA occurred at 2.3 years. Acceptable post-operative outcomes were demonstrated with THA throughout the case series. |
| 11. García-Rey et al.62 | Delayed Group 1 - THA after initial non operative treatment Group 2 - THA after previous Osteosynthesis |
Group 1 - 49 Group 2 - 29 |
Group 1–58.5 Group 2–41.5 |
11.7 years (5–23 years) | THA following failed osteosynthesis had more complications than a primary THA in conjunction with acetabular reconstruction |
| 12. Borg et al.54 | Acute ORIF Vs CHP |
ORIF - 14 CHP - 13 |
72.2 (50–89) | 2 years | CHP confers a considerably reduced need of further surgery when compared with ORIF alone in elderly patients with complex acetabular fractures. |
| 13. Lont et al.63 | Acute | Acute THA with ORIF - 34 ORIF alone - 25 |
Acute THA with ORIF – 71 (56–92) ORIF alone – 69 (58–83) |
2.6 (0–9) years | 9/25 in ORIF alone group developed posttraumatic OA necessitating secondary THA at a median of 12 months (7–37). Acute THA should be a first-line treatment for complex acetabular fractures in elderly patients |
| 14. Giunta et al.64 | Acute | 27 | 68.5 years (57–84) | 4 years | Primary THA for acetabular fracture in selected group of elderly population might be a good therapeutic option that allows return to the previous daily life activity. |
AbbreviationsTHA = Total Hip Arthroplasty, ORIF= Open Reduction and Internal Fixation; CHP= Combined Hip Procedure (ORIF + THA), DM-CHP= Combined Hip Procedure with Dual Mobility Cup.
10. Conclusion
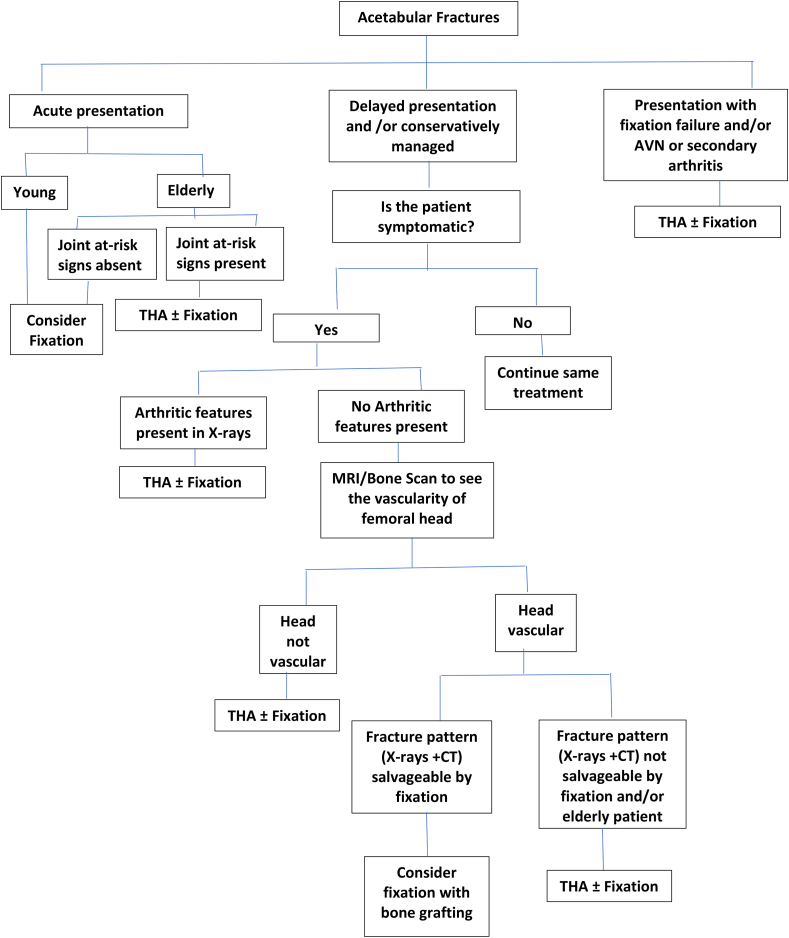
Total Hip Arthroplasty, either acute or delayed is a reliable option in the management of acetabular fractures. Both of them are surgically challenging. In acute stage, the anatomy is grossly distorted and may require an additional fixation to support the acetabular component within the columns. In delayed stage, apart from distorted anatomy, possible necrosis of fragments, scar and fibrous tissue between the fragments, and, presence of implants from prior fixation create challenges during THA. The current literature inclines more towards performing an acute total hip arthroplasty with or without additional fixation rather than performing THA in delayed stage for a failed fixation or a developed arthritis and avascular necrosis of femoral head. The authors’ algorithm for management of acetabular fractures with total hip arthroplasty in depicted in the flow chart (Fig. 5).
Fig. 5.
Flow chart showing algorithm for Total Hip Arthroplasty in management of acetabular fractures.
Future directions
Considerations are being given to role of CT Guided/Navigated Screw insertion to maximize the utilization of corridors for screw fixation.65 Also custom made cups with clustering of screw holes in the direction of corridors and use of screw augmentation technology with polymethyl methacrylate can be used.15
References
- 1.Ferguson T.A., Patel R., BhandariM Matta JM. Fractures of the acetabulum in patients aged 60 years and older: an epidemiological and radiological study. J Bone Joint Surg Br. 2010;92(2):250–257. doi: 10.1302/0301-620X.92B2.22488. [DOI] [PubMed] [Google Scholar]
- 2.Giannoudis P.V., Grotz M.R.W., Papakostidis C. Operative treatment of displaced fractures of the acetabulum. A meta-analysis. J Bone Joint Surg Br. 2005;87B:1–9. [PubMed] [Google Scholar]
- 3.O’Toole R.V., Hui E., Chandra A., Nascone J.W. How often does open reduction and internal fixation of geriatric acetabular fractures lead to hip arthroplasty? J Orthop Trauma. 2014;28(3):148–153. doi: 10.1097/BOT.0b013e31829c739a. [DOI] [PubMed] [Google Scholar]
- 4.Malhotra R., Gautam D. Acute total hip arthroplasty in acetabular fractures using modern porous metal cup. J Orthop Surg. 2019;27(2) doi: 10.1177/2309499019855438. 2309499019855438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mears D.C., Velyvis J.H. Acute total hip arthroplasty for selected displaced acetabular fractures. 2- 12 year results. J Bone Joint Surg Am. 2002;84(1) doi: 10.2106/00004623-200201000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Murphy C.G., Carrothers A.D. Fix and replace; an emerging paradigm for treating acetabular fractures. Clin Cases Miner Bone Metab. 2016 Sep-Dec;13(3):228–233. doi: 10.11138/ccmbm/2016.13.3.228. Epub 2017 Feb 10. PMID: 28228787; PMCID: PMC5318177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rickman M., Young J., Trompeter A., Pearce R., Hamilton M. Managing acetabular fractures in the elderly with fixation and primary arthroplasty: aiming for early weight bearing. Clin Orthop Relat Res. 2014;472:3375–3382. doi: 10.1007/s11999-014-3467-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mears D.C., Velyvis J.H. Primary total hip arthroplasty after acetabular fracture. J Bone Joint Surg Am. 2000;82:1328–1353. [Google Scholar]
- 9.Anglen J.O., Burd T.A., Hendricks K.J., Harrison P. The “Gull sign”: a harbinger of failure for internal fixation of geriatric acetabular fractures. J Orthop Trauma. 2003;17(9):625–634. doi: 10.1097/00005131-200310000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Mohanty K., Taha W., Powell J.N. Non-union of acetabular fractures. Injury. 2004 Aug;35(8):787–790. doi: 10.1016/j.injury.2003.11.022.PMID:15246802. [DOI] [PubMed] [Google Scholar]
- 11.Wang P., Kandemir U., Zhang B., Fei C., Zhuang Y., Zhang K. The effect of new preoperative preparation method compared to conventional method in complex acetabular fractures: minimum 2-year follow-up. Arch Orthop Trauma Surg. 2020 May 26 doi: 10.1007/s00402-020-03472-w. Epub ahead of print. PMID: 32458075. [DOI] [PubMed] [Google Scholar]
- 12.Zhou X., Zhang Q., Song W., Zhou D., He Y. Clinical significance of three-dimensional skeleton-arterial model in the management of delayed reconstruction of acetabular fractures. BMC Surg. 2018 May 29;18(1):30. doi: 10.1186/s12893-018-0362-y. . PMID: 29843704; PMCID: PMC5975535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moed B.R., Miller J.R., Tabaie S.A. Sequential duplex ultrasound screening for proximal deep venous thrombosis in asymptomatic patients with acetabular and pelvic fractures treated operatively. J Trauma Acute Care Surg. 2012 Feb;72(2):443–447. doi: 10.1097/TA.0b013e318241090d. PMID: 22327985. [DOI] [PubMed] [Google Scholar]
- 14.Letournel E., editor. Fractures of the Acetabulum. second ed. Springer-Verlag; New York: 1993. [Google Scholar]
- 15.T Marmor M., Huang A., Knox R., Herfat S., Firoozabadi R. Mapping of the stable Articular surface and available bone corridors for cup fixation in geriatric acetabular fractures. J Am Acad Orthop Surg. 2020;28(13):e573–e579. doi: 10.5435/JAAOS-D-18-00445. [DOI] [PubMed] [Google Scholar]
- 16.Ranawat A., Zelken J., Helfet D., Buly R. Total hip arthroplasty for posttraumatic arthritis after acetabular fracture. J Arthroplasty. 2009;24(5):759–767. doi: 10.1016/j.arth.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 17.Jouffroy P. Bone and Joint Trauma Study Group (GETRAUM). Indications and technical challenges of total hip arthroplasty in the elderly after acetabular fracture. OrthopTraumato lSurg Res. 2014 Apr;100(2):193–197. doi: 10.1016/j.otsr.2014.01.001. Epub 2014 Feb 26. PMID: 24582289. [DOI] [PubMed] [Google Scholar]
- 18.Tannast M., Najibi S., Matta J.M. Two to twenty-year survivorship of the hip in 810 patients with operatively treated acetabular fractures. J Bone Joint Surg Am. 2012;94(17):1559–1567. doi: 10.2106/JBJS.K.00444. [DOI] [PubMed] [Google Scholar]
- 19.Manson T.T. Open reduction and internal fixation plus total hip arthroplasty for the acute treatment of older patients with acetabular fracture: surgical techniques. Orthop Clin N Am. 2020;51(1):13–26. doi: 10.1016/j.ocl.2019.08.006. [DOI] [PubMed] [Google Scholar]
- 20.Berry D.J. Total hip arthroplasty following acetabular fracture. Orthopaedics. 1999;22:837–839. doi: 10.3928/0147-7447-19990901-14. [DOI] [PubMed] [Google Scholar]
- 21.Berry D.J., Halasy M. Uncemented acetabular components for arthritis after acetabular fracture. Clin Orthop. 2002;405:164–167. doi: 10.1097/00003086-200212000-00020. [DOI] [PubMed] [Google Scholar]
- 22.Scott C.E.H., MacDonald D., Moran M., White T.O., Patton J.T., Keating J.F. Cemented total hip arthroplasty following acetabular fracture. Bone Joint Lett J. 2017 Oct;99-B(10):1399–1408. doi: 10.1302/0301-620X.99B10.BJJ-2016-1261.R2. PMID: 28963163. [DOI] [PubMed] [Google Scholar]
- 23.Busch V.J., Gardeniers J.W., Verdonschot N., Slooff T.J., Scheurs B.W. Acetabular reconstruction with impaction bone-grafting and cemented cup in patients younger than fifty years old: aconcise follow-up, at twenty to twenty-eight years, of a previous report. J Bone Joint Surg. 2011;93:367–371. doi: 10.2106/JBJS.I.01532. [DOI] [PubMed] [Google Scholar]
- 24.Schreurs B.W., Bolder S.B., Gardeniers J.W., Verdonschot N., Slooff T.J., Veth R.P. Acetabular revision with impacted morsellised cancellous bone grafting and a cemented cup. A 15- to 20-year follow-up. J Bone Joint Surg Br. 2004 May;86(4):492–497. PMID: 15174541. [PubMed] [Google Scholar]
- 25.Gill K., Wilson M.J., Whitehouse S.L., Timperley A.J. Results using Trabecular Metal™ augments in combination with acetabular impaction bone grafting in deficient acetabula. Hip Int. 2013;23(6):522–528. doi: 10.5301/hipint.5000053. [DOI] [PubMed] [Google Scholar]
- 26.Dua Aman, Kiran K., Malhotra R., Bhan S. Acetabular reconstruction using fresh frozen allograft. Hip Int. 2010;20(2):143–149. doi: 10.1177/112070001002000203. [DOI] [PubMed] [Google Scholar]
- 27.Salama W., Mousa S., Khalefa A. Simultaneous open reduction and internal fixation and total hip arthroplasty for the treatment of osteoporotic acetabular fractures. Int Orthop. 2017;41(1):181–189. doi: 10.1007/s00264-016-3175-6. [DOI] [PubMed] [Google Scholar]
- 28.Herscovici D., Jr., Lindvall E., Bolhofner B., Scaduto J.M. The combined hip procedure: open reduction internal fixation combined with total hip arthroplasty for the management of acetabular fractures in the elderly. J Orthop Trauma. 2010;24(5):291–296. doi: 10.1097/BOT.0b013e3181b1d22a. [DOI] [PubMed] [Google Scholar]
- 29.Lannes X., Moerenhout K., Duong H.P., Borens O., Steinmetz S. Outcomes of combined hip procedure with dual mobility cup versus osteosynthesis for acetabular fractures in elderly patients: a retrospective observational cohort study of fifty one patients. Int Orthop. 2020 Aug 9 doi: 10.1007/s00264-020-04757-w. Epub ahead of print. PMID: 32772320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Boyer B., Philippot R., Geringer J., Farizon F. Primary total hip arthroplasty with dual mobility socket to prevent dislocation: a 22-year follow-up of 240 hips. Int Orthop. 2012;36:511–518. doi: 10.1007/s00264-011-1289-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Combes A., Migaud H., Girard J., Duhamel A., Fessy M.H. Low rate of dislocation of dual-mobility cups in primary total hip arthroplasty. Clin Orthop Relat Res. 2013;471:3891–3900. doi: 10.1007/s11999-013-2929-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jimenez Matthew L., Tile Marvin, Schenk Richard S. Total hip replacement after acetabular fracture. Orthop Clin N Am. 1997;28(3):435–446. doi: 10.1016/s0030-5898(05)70300-x. [DOI] [PubMed] [Google Scholar]
- 33.Malhotra R., Gautam D. Cup-cage construct using porous cup with burch-schneider cage in the management of complex acetabular fractures. Hip Pelvis. 2019;31(2):87–94. doi: 10.5371/hp.2019.31.2.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Paprosky W.G., Perona P.G., Lawrence J.M. Acetabular defect classification and surgical reconstruction in revision arthroplasty. A six year follow-up evaluation. J Arthroplasty. 1994;9(1):33–44. doi: 10.1016/0883-5403(94)90135-x. [DOI] [PubMed] [Google Scholar]
- 35.D’Antonio J.A., Capello W.N., Borden L.S. Classification and management of acetabular abnormalities in total hip arthroplasty. Clin Orthop Relat Res. 1989;126 [PubMed] [Google Scholar]
- 36.Butterwick D., Papp S., Gofton W., Liew A., Beaulé P.E. Acetabular fractures in the elderly: evaluation and management. J Bone Joint Surg Am. 2015;97(9):758–768. doi: 10.2106/JBJS.N.01037. [DOI] [PubMed] [Google Scholar]
- 37.Hoskins W., Griffin X., Hatton A., de Steiger R.N., Bingham R. THA for a fractured femoral neck: comparing the revision and dislocation rates of standard-head, large-head, dual-mobility, and constrained liners. Clin Orthop Relat Res. 2020 Aug 11 doi: 10.1097/CORR.0000000000001447. Epub ahead of print. PMID: 32876424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Malhotra R., Kancherla R., Kumar V., Soral A. Trabecular metal acetabular revision system (cup-cage construct) to address the massive acetabular defects in revision arthroplasty. Indian J Orthop. 2012 Jul;46(4):483–486. doi: 10.4103/0019-5413.97264. PMID: 22912527; PMCID: PMC3421942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Solomon L.B., Studer P., Abrahams J.M. Does cup-cage reconstruction with oversized cups provide initial stability in THA for osteoporotic acetabular fractures? Clin Orthop Relat Res. 2015 Dec;473(12):3811–3819. doi: 10.1007/s11999-015-4460-1. PMID: 26194560; PMCID: PMC4626507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Malhotra R., Singh D.P., Jain V., Kumar V., Singh R. Acute total hip arthroplasty in acetabular fractures in the elderly using the Octopus System: mid term to long term follow-up. J Arthroplasty. 2013;28(6):1005–1009. doi: 10.1016/j.arth.2012.12.003. Epub 2013 Mar 20. [DOI] [PubMed] [Google Scholar]
- 41.Tidermark J., Blomfeldt R., Ponzer S. Primary total hip arthroplasty with a Burch-Schneider antiprotrusion cage and autologous bone grafting for acetabular fractures in elderly patients. J Orthop Trauma. 2003;17:193–197. doi: 10.1097/00005131-200303000-00007. [DOI] [PubMed] [Google Scholar]
- 42.Symeonides P.P., Petsatodes G.E., Pournaras J.D. The effectiveness of the burch-schneider antiprotrusio cage for acetabular bone deficiency: five to twenty-one years’ follow-up. J Arthroplasty. 2009;24:168–174. doi: 10.1016/j.arth.2007.10.009. [DOI] [PubMed] [Google Scholar]
- 43.Sheth N.P., Melnic C.M., Paprosky W.G. Acetabular distraction: an alternative for severe acetabular bone loss and chronic pelvic discontinuity. Bone Joint J. 2014;96B(11):1–7. doi: 10.1302/0301-620X.96B11.34455. [DOI] [PubMed] [Google Scholar]
- 44.Brown N.M., Hellman M., Haughom B.H., Shah R.P., Sporer S.M., Paprosky W.G. Acetabular distraction: an alternative approach to pelvic discontinuity in failed total hip replacement. Bone Joint Lett J. 2014;96-B(11 Supple A):73–77. doi: 10.1302/0301-620X.96B11.34316. [DOI] [PubMed] [Google Scholar]
- 45.McMahon S.E., Diamond O.J., Cusick L.A. Coned hemipelvis reconstruction for osteoporotic acetabular fractures in frail elderly patients. Bone Joint Lett J. 2020;102-B(2):155–161. doi: 10.1302/0301-620X.102B2.BJJ-2019-0883.R2. [DOI] [PubMed] [Google Scholar]
- 46.Jacquot A., Goetzmann T., Jullion S., Sirveaux F., Molé D., Roche O. Two-stage total hip arthroplasty for complex pelvic abnormalities: example of hip arthrodesis conversion with concomitant treatment of pelvic and acetabular non-union. OrthopTraumato lSurg Res. 2016 Jun;102(4):517–519. doi: 10.1016/j.otsr.2016.02.008. Epub 2016 Apr 1. PMID: 27052938. [DOI] [PubMed] [Google Scholar]
- 47.Hipfl C., Janz V., Löchel J., Perka C., Wassilew G.I. Cup-cage reconstruction for severe acetabular bone loss and pelvic discontinuity: mid-term Results of a Consecutive Series of 35 Cases. Bone Joint Lett J. 2018 Nov;100-B(11):1442–1448. doi: 10.1302/0301-620X.100B11.BJJ-2018-0481.R1. PMID: 30418066. [DOI] [PubMed] [Google Scholar]
- 48.Morita D., Seki T., Takegami Y., Kasai T., Higuchi Y., Ishiguro N. Acetabular fracture non-union with pelvic discontinuity treated with two-stage total hip arthroplasty after intra- and extra-articular plate fixation. Nagoya J Med Sci. 2019 Feb;81(1):113–119. doi: 10.18999/nagjms.81.1.113. PMID: 30962660; PMCID: PMC6433626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shah Nikhil, WJ Henry, Clayson Anthony, Chitre Amol. Management of pelvic discontinuity: two stage technique. In Malhotra Rajesh (Eds) Mastering Orthopedic Techniques: Revision Hip Arthroplasty 2017; (Chapter 39): pp. 453–462. New Delhi, India: Jaypee Brothers Medical Publishers (P) Ltd. Print
- 50.Manson T., Schmidt A.H. Acetabular fractures in the elderly: a critical analysis review. JBJS Rev. 2016 Oct 4;4(10) doi: 10.2106/JBJS.RVW.15.00090. 01874474-201610000-00002. PMID: 27792674. [DOI] [PubMed] [Google Scholar]
- 51.Hamlin K., Lazaraviciute G., Koullouros M., Chouari T., Stevenson I.M., Hamilton S.W. Should total hip arthroplasty be performed acutely in the treatment of acetabular fractures in elderly or used as a salvage procedure only? Indian J Orthop. 2017 Jul-Aug;51(4):421–433. doi: 10.4103/ortho.IJOrtho_138_16. PMID: 28790471; PMCID: PMC5525523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Stibolt R.D., Jr., Patel H.A., Huntley S.R., Lehtonen E.J., Shah A.B., Naranje S.M. Total hip arthroplasty for posttraumatic osteoarthritis following acetabular fracture: a systematic review of characteristics, outcomes, and complications. Chin J Traumatol. 2018 Jun;21(3):176–181. doi: 10.1016/j.cjtee.2018.02.004. Epub 2018 Apr 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Morison Z., Moojen D.J., Nauth A. Total hip arthroplasty after acetabular fracture is associated with lower survivorship and more complications. Clin Orthop Relat Res. 2016 Feb;474(2):392–398. doi: 10.1007/s11999-015-4509-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Borg T., Hernefalk B., Hailer N.P. Acute total hip arthroplasty combined with internal fixation for displaced acetabular fractures in the elderly: a short-term comparison with internal fixation alone after a minimum of two years. Bone Joint Lett J. 2019 Apr;101-B(4):478–483. doi: 10.1302/0301-620X.101B4.BJJ-2018-1027.R2. [DOI] [PubMed] [Google Scholar]
- 55.Aprato A., Giachino M., Messina D., Massé A. Fixation plus acute arthroplasty for acetabular fracture in eldery patients. J Orthop. 2020 Sep 19;21:523–527. doi: 10.1016/j.jor.2020.09.012. PMID: 32999541; PMCID: PMC7516170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nicol G.M., Sanders E.B., Kim P.R., Beaulé P.E., Gofton W.T., Grammatopoulos G. Outcomes of total hip arthroplasty after acetabular open reduction and internal fixation in the elderly-acute vs delayed total hip arthroplasty. J Arthroplasty. 2020 Aug 18;(20):30908–30916. doi: 10.1016/j.arth.2020.08.022. S0883-5403. Epub ahead of print. PMID: 32919846. [DOI] [PubMed] [Google Scholar]
- 57.Liaw F., Govilkar S., Banks D., Kankanalu P., Youssef B., Lim J. Primary total hip replacement using Burch-Schneider cages for acetabular fractures. Hip Int. 2020 Sep 9 doi: 10.1177/1120700020957642. 1120700020957642. Epub ahead of print. PMID: 32905712. [DOI] [PubMed] [Google Scholar]
- 58.Rommens P.M., Schwab R., Handrich K., Arand C., Wagner D., Hofmann A. Open reduction and internal fixation of acetabular fractures in patients of old age. Int Orthop. 2020 Jul 30 doi: 10.1007/s00264-020-04672-0. Epub ahead of print. PMID: 32734382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Milenkovic S., Mitkovic M., Mitkovic M., Stojiljković P. Total hip arthroplasty after acetabular fracture surgery. Int Orthop. 2020 Jul 2 doi: 10.1007/s00264-020-04676-w. Epub ahead of print. PMID: 32617652. [DOI] [PubMed] [Google Scholar]
- 60.Do M.U., Shin W.C., Moon N.H., Kang S.W., Suh K.T. Cementless total hip arthroplasty after failed internal fixation of acetabular fractures: a single center experience of 25 consecutive patients. J Orthop Surg. 2020 Jan-Apr;28(2) doi: 10.1177/2309499020910666. 2309499020910666. doi: 10.1177/2309499020910666.PMID: 32356504. [DOI] [PubMed] [Google Scholar]
- 61.Dawson P., Dunne L., Raza H., Quinn M., Leonard M. Total hip arthroplasty for the treatment of osteoarthritis secondary to acetabular fractures treated by open reduction and internal fixation. Eur J Orthop Surg Traumatol. 2019 Jul;29(5):1049–1054. doi: 10.1007/s00590-019-02406-6. Epub 2019 Feb 22. PMID: 30796512. [DOI] [PubMed] [Google Scholar]
- 62.García-Rey E., Sirianni R., García-Cimbrelo E., Sedel L. Total hip arthroplasty after acetabular fracture: does initial treatment make any difference to the outcome? A 5- to 23-year follow-up with clinical and radiological analysis. Hip Int. 2020 May;30(3):339–346. doi: 10.1177/1120700019836413.Epub2019Mar26. PMID: 30912452. [DOI] [PubMed] [Google Scholar]
- 63.Lont T., Nieminen J., Reito A. Total hip arthroplasty, combined with a reinforcement ring and posterior column plating for acetabular fractures in elderly patients: good outcome in 34 patients. Acta Orthop. 2019 Jun;90(3):275–280. doi: 10.1080/17453674.2019.1597325. Epub 2019 Apr 1. PMID: 30931684; PMCID: PMC6534240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Giunta J.C., Tronc C., Kerschbaumer G. Outcomes of acetabular fractures in the elderly: a five year retrospective study of twenty seven patients with primary total hip replacement. Int Orthop. 2019 Oct;43(10):2383–2389. doi: 10.1007/s00264-018-4204-4. Epub 2018 Oct 18. PMID: 30338339. [DOI] [PubMed] [Google Scholar]
- 65.Yu T., Cheng X.L., Qu Y., Dong R.P., Kang M.Y., Zhao J.W. Computer navigation-assisted minimally invasive percutaneous screw placement for pelvic fractures. World J Clin Cases. 2020;8(12):2464–2472. doi: 10.12998/wjcc.v8.i12.2464. [DOI] [PMC free article] [PubMed] [Google Scholar]