Abstract
Introduction
and aim: Traumatic peri-prosthetic fractures are relatively rare fractures that pose a significant surgical challenge. They have a fracture pattern that is different from its iatrogenic counterpart. This study aimed at reviewing the modalities of treatment of such injuries, proposing a treatment algorithm and reporting the outcomes of these injuries.
Patients and methods
We propose an algorithm for management of traumatic peri-prosthetic acetabular fractures which depends on fracture displacement, implant stability and associated bone loss.
Twelve patients with traumatic peri-prosthetic acetabular fractures were treated between January 2012 and December 2018. All patients were treated surgically. Patients were allowed immediate weight bearing as pain allowed. Assessment was carried out using the Oxford Hip Score (OHS) and the Merle D’aubigné score (MDP).
Results
Mean patient age 71 (range: 59–80). 8 patients underwent implant removal, fracture fixation and re-implantation of revision acetabular cup (displaced fracture, unstable implant, adequate bone stock). Three patients required acetabular reconstruction (inadequate bone stock). One patient underwent revision acetabular component. One patient suffered from recurrent dislocation that required surgical intervention. Mean follow up was 27 Months (range 12–48). Mean OHS was 36 (range 10–47). Mean MDP was 12 (range 9–18) with 80% excellent and good results.
Conclusion
Surgical management of peri-prosthetic acetabular fractures can produce good to excellent results provided adequate assessment and surgical planning have been carried out. Fracture displacement, implant stability and bone stock should be carefully assessed.
Keywords: Peri-prosthetic acetabular fracture, Acetabular trauma, Revision arthroplasty
1. Introduction
Periprosthetic fractures of the acetabulum pose a significant surgical challenge. They can be iatrogenic; mainly during implantation of an uncemented acetabular component or during revision THA. They can also occur late due to trauma or a pathological process around the acetabular socket such as a neoplasm. They may be associated with acetabular loosening or infection. The incidence of traumatic acetabular fractures have been reported to be around 0.07% in one retrospective analysis,1 with most published series including a very small number of cases over a relatively long period of time.1, 2, 3
Traumatic fractures differ from their atraumatic counterparts in the degree of displacement and fracture patterns; Iatrogenic fractures usually affect the medial wall of the acetabulum and/or one column of the acetabulum, whereas traumatic fractures maybe associated with fracture patterns similar to those described by Judet and Louternel.4
In our institution, they are managed by an orthopaedic surgeon with experience in both revision THA and acetabular fracture fixation.
This article aims at reviewing the current modalities of treatment, proposes a management algorithm for these fractures and reports the outcome of these injuries.
2. Classification
A simple way of classifying periprosthetic acetabular fractures is based on implant stability. This was first proposed by Petersen and Lewallen who classified these fractures into stable and unstable.1 The most commonly used classification method to date is that proposed by Della Valle et al. and commonly known as the Paprosky classification. It takes into account timing of fracture (Iatrogenic during implant insertion or removal, traumatic, spontaneous or pelvic discontinuity), implant stability and associated bone loss.5
A recent classification by Pascarella et al. took three parameters into consideration; timing (intraoperative – post operative), implant stability (stable and unstable), and whether or not there was pre-existing loosening and migration prior to trauma.6 The presence of pre-existing loosening or migration before the traumatic event is an important factor to consider prior to surgery as it may affect the modality of management, and may help providing an indication of existing bone stock.
However, in traumatic peri-prostheric acetabular fractures it is important to consider the columns of the acetabulum, as they are often disrupted as a result of the trauma, and stability of the construct may rely on restoration of these columns. Thus another important classification system that should be considered in traumatic periprosthetic acetabular fractures is that proposed by Letournel for acetabular fractures.7 The Letournel classification can help the surgeon understand the morphology of the fracture and identify the disrupted columns and help plan the surgical approach and method of fixation.
3. Diagnosis
Unlike iatrogenic fractures; which can go unnoticed, the traumatic counterpart is preceded by a traumatic event. This can be a high energy injury or a minor injury particularly in older patients. Older patients may have pre-existing loosening and the traumatic event in this case acts as a precipitation factor that causes a break in the columns of the acetabulum. Patients should be asked about history of pre-existing hip pain, this can be a clue in distinguishing traumatic fractures from cases presenting with aseptic loosening. High energy trauma patients should be managed as per ATLS guidelines with careful examination including the documentation of the neurovascular status and special attention to the function of the sciatic nerve.
Diagnosis should include plain radiographs and fine cut CT scans with metal suppression. In cases with superior or posterior migration of the acetabular component and compromise of the sciatic nerve, skeletal traction can be considered as an emergency procedure until definitive procedure can be undertaken. This technique can be used as a method of pain control and can relieve the pressure off the sciatic nerve. Sometimes the acetabular component migrates centrally and again in these cases it may be helpful to apply traction to help with pain control and also to help with the soft tissues if there is going to be a delay to surgery.
Radiological assessment should consist of Pelvic AP radiographs and Judet views when available to assess the integrity of the acetabular columns. The fine cut CT will provide information about bone stock, stability of the acetabular component and pre-existing lysis and help formulate a plan. Serial radiographs taken over the post-operative follow up period are also useful if available, they can help identify areas of suspected bone loss and differentiate between traumatic cases and cases with progressive loosening.
4. Management
The majority of these patients may be elderly and frail. They can have several co-morbidities plus the added insult of the injury. Thus it is of vital importance that before embarking on major surgery such as revision hip surgery,the individual circumstances and risks should be carefully assessed. These patients should be managed with protocols similar to that of fragility hip fractures.8,9 Such patients require input from the orthogeriatric team or the medical team for rapid assessment and optimization for surgery, input from physiotherapy and occupational therapy teams to asses rehabilitation goals, fall risk assessment and liaison with other services such as bone health and mental health services.
The mainstay of surgical management depends on identifying the fracture pattern, the implant stability and the remaining bone stock.
Miller reported a case series of 9 periprosthetic acetabular fractures treated conservatively in 1972, and none of them progressed to full bony union. Thus, Non-Operative treatment is reserved for patients with minimally displaced fractures and stable implants, or for low demand or surgically unfit patients.
Rarely, a displaced fracture could be found with a stable implant. This could be the case if the fracture does not affect the weight bearing portion of the acetabulum. This could be treated with fixation of the acetabular fracture alone without revising the acetabular component.
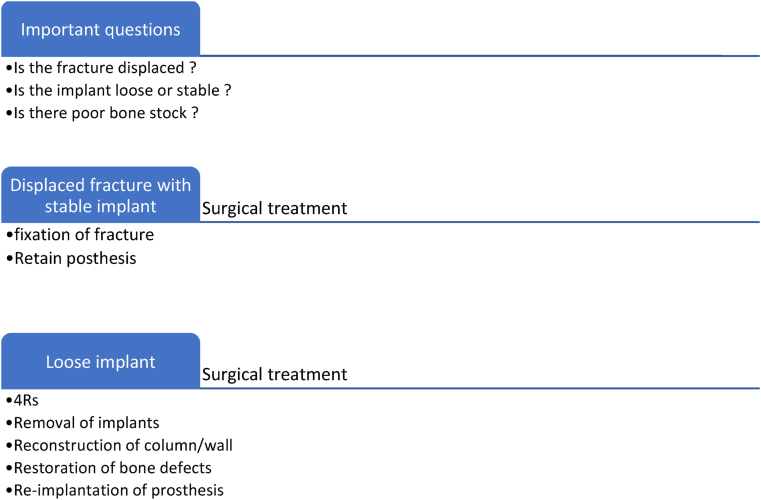
More commonly, a fracture would compromise implant stability and in such cases surgery would entail removal of the implant to help aid fracture reduction and fixation, followed by fracture fixation, and finally reconstruction of the acetabulum with a revision acetabular component (4R approach, Fig. 1). It is helpful to think about surgical management of these injuries in 4 stages.
Fig. 1.
The 4R approach to assessing peri-prosthetic acetabular fractures.
The femoral stem can be retained if it remains well fixed and compatible with the new implants being used for acetabular reconstruction. Knowledge of the femoral stem manufacture and design is an important part of pre-operative planning to ensure compatibility with the acetabular component.
Stage 1 Removal of existing implants
Stage 2 Reconstruction of the columns & walls of the acetabulum
Stage 3 Restoration of the bone defects
Stage 4 Re- implantation of a revision prosthetic construct
In our unit, these fractures are managed by orthopaedic surgeons with experience in both acetabular fractures and revision hip arthroplasty. They are surgically challenging cases that require careful planning.
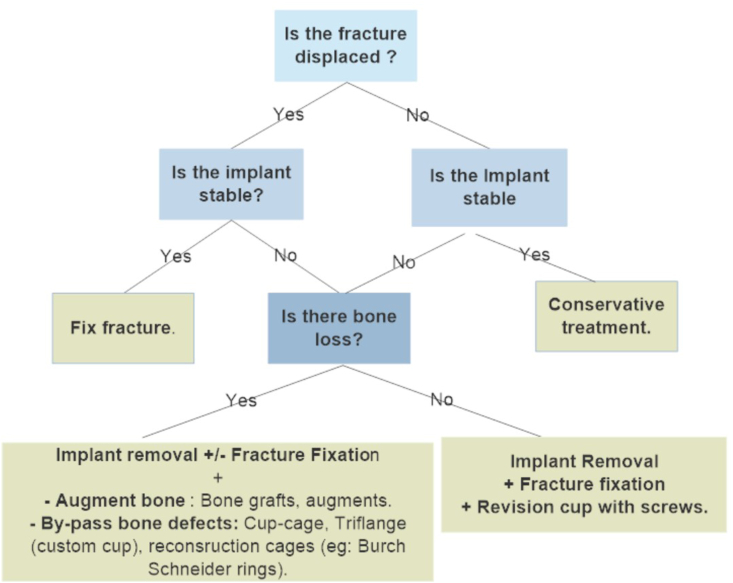
It is important to understand the morphology and the configuration of the acetabular fracture to plan the surgical approach. The choice of approach depends of the site of acetabular fracture displacement whether anterior or posterior. However, in most cases removal of the implant prior to fixing the acetabulum would aid in fracture reduction and fixation (Fig. 2).
Fig. 2.
Algorithm for surgical management of traumatic peri-prosthetic acetabular fractures.
5. Implant removal and fracture fixation, followed by re-implantation
This is suitable in the presence of good bone stock, particularly in the younger population. With the implant being loose, removal would be a straight forward process in the majority of cases, however removal instruments should be available if required, similarly more complex reconstruction options such as bone graft, augments and cages should be available if needed. The aim would be implant removal without compromising the bone stock.
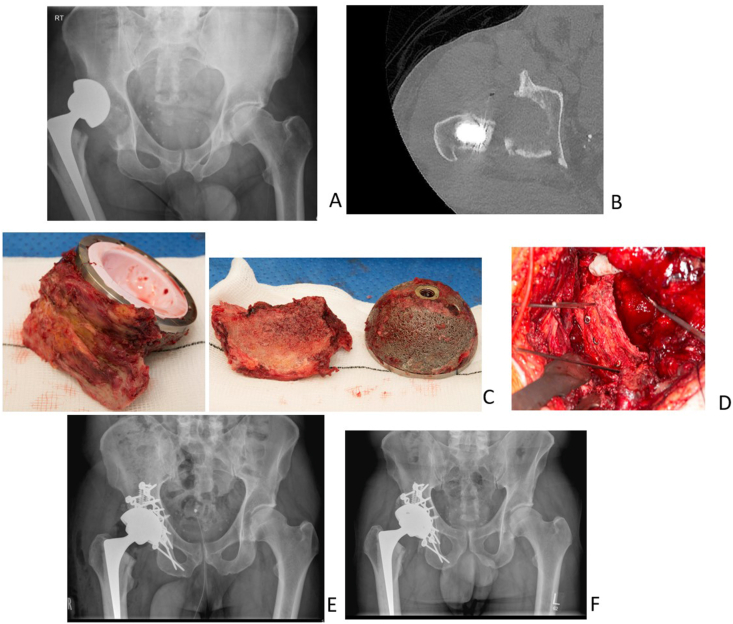
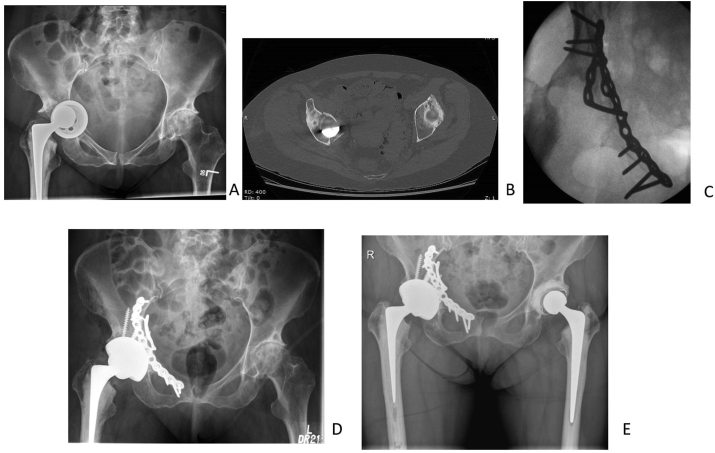
After implant removal the fracture can be reduced and fixed with standard acetabular reconstruction plates, followed by implanting a new revision shell using a line to line technique and allowing as much screw fixation as possible to achieve primary stability. Femoral stem can be retained or revised as necessary (Fig. 3, Fig. 4).
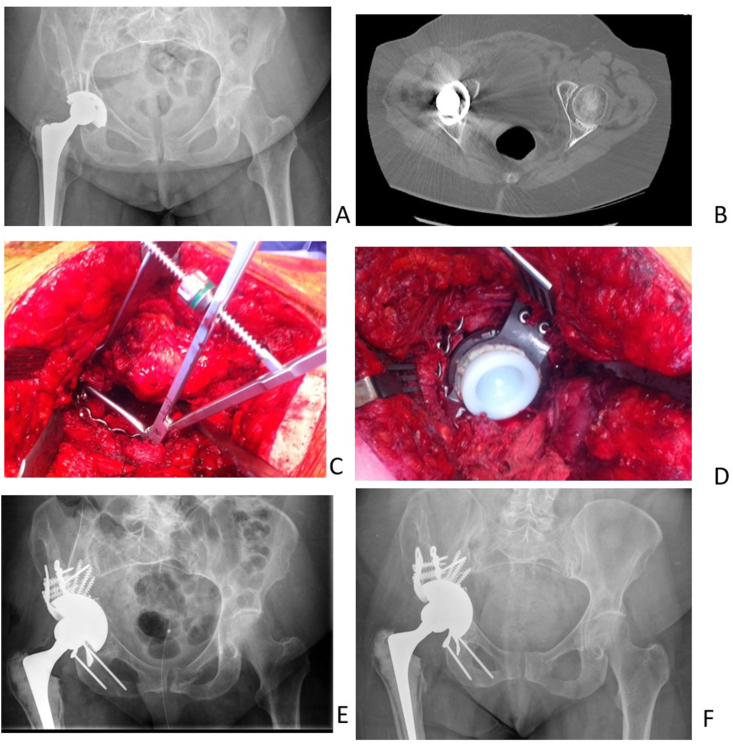
Fig. 3.
A: 59 year old male, fall at home 6 weeks after primary THA for osteoarthritis. B: CT showing posterior wall and posterior column fracture. C: Implant removed with large portion of posterior wall and column which was attached to the implant and was carefully removed from the implant. D: intra-operative image after fixing the posterior wall and posterior column. E: post operative image showing fixation of the posterior acetabular fracture with two reconstruction plates and implanting a revision shell, fixed in situ with multiple screws. F: One year follow up AP radiograph.
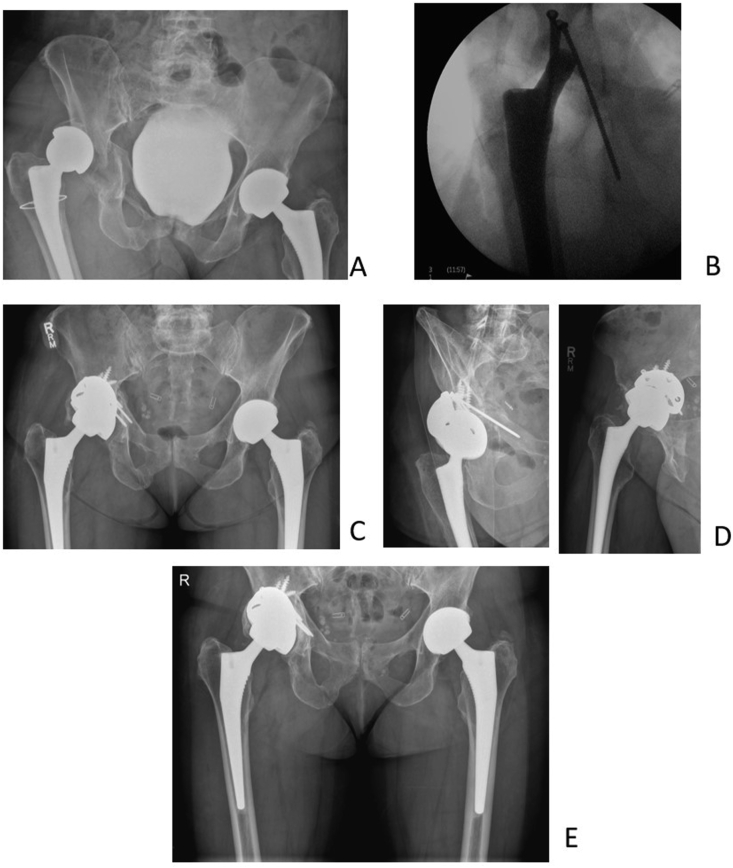
Fig. 4.
A: 64 year old female with bilateral hip OA. Had right THA and fell early onto her right hip sustaining the injury below. B: Axial CT cut. Fracture classified as anterior column posterior hemi-transverse. C: intra-operative fluroscopy after implant removal and fracture fixation. D: Post operative radiograph after fracture fixation and revision with a tacetabular metal socket. E: Five year post-perative AP radiograph.
6. Implant removal and acetabular reconstruction
In cases with poor bone stock this can be due to pre-existing loosing or secondary to the fracture configuration, reconstruction of the acetabulum might be necessary. This can be achieved by the use of trabecular metal augments, acetabular cage, or allografts (Fig. 5, Fig. 6, Fig. 7).
Fig. 5.
A: 69 year old lady, fall at home following right hip arthroplasty dating more than 10 years prior to injury. B: CT scan showing transverse type fracture with medial bone defect. C: intra-operative image of posterior wall/column reduction and fixation, bone stock was poor and deficient medially and posteriorly. D: Reconstruction with cup-cage construct. E: post-operative AP radiographs. F: One year post-operative AP radiographs.
Fig. 6.
A: 63 year old female, road traffic injury. Transverse fracture pattern with superior implant migration and postero-superior acetabular defect. B: Intra-operative fluoroscopy showing column fixation with column screws after implant removal. C&D: Post operative images showing outcome after acetabular reconstruction with augments to restore postero-superior defect. E: Three year post-operative follow up AP radiograph.
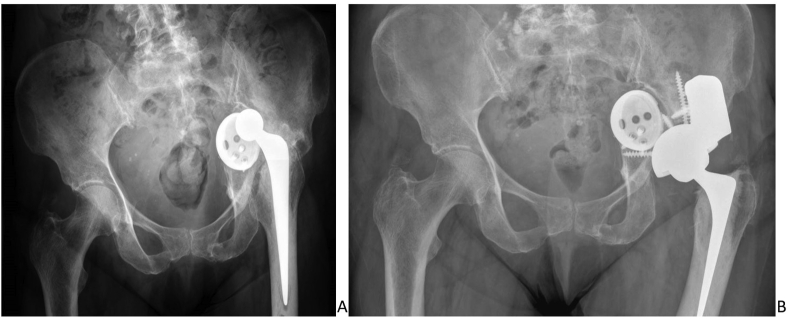
Fig. 7.
A: 74 year old female. Fell and sustained a periprosthetic fracture around left THA. Presented late with marked displacement and leg length discrepancy with sciatic nerve palsy. CT angiogram scan showed that iliac vessels were adhered to the intra pelvic cup. This was therefore left in situ. B: Reconstruction of the posterior column defect was performed using a trabecular metal buttress augment and a revision acetabular shell with multiple screws.
7. Post operative care
With restoration of the acetabular columns and reconstruction of the acetabulum the patient would be allowed to start immediate full weight bearing as tolerated, this is an integral part of recovery particularly in the elderly group that cannot withstand prolonged bed rest and immobility.
These patients would have undergone lengthy complex surgeries and their post-operative care is more challenging than a standard primary or revision total hip replacement, further input from the multi-disciplinary team will be needed at this point in the majority of the patients to restore them to pre-existing level of mobility.
8. Patients and methods
Seventeen cases with peri-prosthetic acetabular fractures presented to our unit between January 2012 and December 2018. Twelve cases were traumatic, four were iatrogenic and one pathological (metastasis).(Table 1).
Table 1.
Patient demographics and outcome scores.
| Mode of Trauma | Interval between surgery and injury (months) | Fracture type | Surgery | Follow up period | OHS | MDP | ||
|---|---|---|---|---|---|---|---|---|
| 1 | 70 | Fall | 60 | Post Wall, Post Column | Revision THA | 24 | 39 | 17 |
| 2 | 73 | Fall | 72 | Transverse + post wall | ORIF + Revision THA | 48 | 43 | 16 |
| 3 | 71 | Fall | 6 | Transverse | ORIF + Revision THA | 48 | 38 | 16 |
| 4 | 80 | Fall | 18 | Posterior column | ORIF + Revision THA | 3 | N/A | N/A |
| 5 | 78 | Fall | 62 | Anterior column posterior hemi-transverse | ORIF + Revision THA | 48 | 10 | 9 |
| 6 | 76 | Fall | 98 | Transverse | ORIF + Revision THA | 12 | 40 | 16 |
| 7 | 69 | Fall | 203 | Transverse with discontinuity | ORIF + Cup cage construct | 18 | 47 | 16 |
| 8 | 59 | Fall | 1.5 | Posterior wall with migration of cup | ORIF + Revision THA | 12 | 36 | 12 |
| 9 | 80 | Fall | 5 | Posterior wall with migration of cup | ORIF + Revision THA | 12 | 39 | 18 |
| 10 | 63 | Road traffic accident | 60 | Posterior wall with migration of cup | ORIF + Augments + revision THA | 24 | 34 | 16 |
| 11 | 64 | Fall | 2 | Anterior column posterior hemi-transverse | ORIF + Revision THA | 36 | 43 | 17 |
| 12 | 74 | Fall | 58 | Anterior column posterior hemi-transverse with medial migration of the cup | Augment + Revision THA | 23 | 32 | 15 |
Eleven cases were low energy trauma due to falls sustained at home or outdoors. One case of high energy trauma was managed according to ATLS guidelines. History taking and documentation of mechanism of trauma, pre-existing medical conditions, presence of pre-existing ipsilateral hip pain, and level of mobility were documented. Elderly and frail patients were managed in accordance with fragility hip fracture guidelines.8
The mean time between the surgery and the injury was 50 months (approximately 4years), (range: 1.5–203 months).
All the twelve cases were managed surgically. Seven patients had an elementary fracture pattern of the acetabulum according to Letournel and these included three posterior wall fractures, one posterior column fracture and three pure transverse fractures. The remaining five patients had an associated acetabular fracture pattern including one transverse posterior wall, one posterior column with associated posterior wall and three anterior column with associated posterior hemi transverse (Table 1).
Patients were encouraged to start immediate post-operative range of motion exercises and instructed to weight bear as pain allowed. Patients were followed up at 6 weeks, 3 months, 6 months, one year, then on yearly basis.
Functional assessment was conducted at end of the follow up period using the 12 question, patient reported Oxford Hip Score (OHS),10 and the Merle D’aubigné score (MDP) where a score of 18 signifies an excellent outcome, 15–17 good, 13 and 14 fair, while a score of 12 or below was considered as a poor outcome.11
9. Results
Mean patient age was 71 years (Range:59–80). One patient underwent acetabular component revision without fixation, eight patients underwent implant removal, acetabular fixation and re-implantation of a revision cup. Three patients required reconstruction; two with acetabular augments and the other with a cup cage construct.
One patient suffered recurrent dislocation and was later revised to a constrained liner, Two patients had a pre-operative partial sciatic nerve palsy, one eventually recovered at 6 months and the second had not recovered at final follow up.
One patient moved out of the area and had a follow up period of 3 months then was lost to follow up, the remainder had a mean follow up of 27 months (range: 12–48). The mean OHS was 36 (range 10–47). The mean MDP score was 12 (range 9–18), with 80% excellent and good outcome.
10. Discussion
Traumatic peri-prosthetic fractures are rare injuries and are expected to increase due to rise in patient population and an increase in the number of hip replacements conducted.12,13 The main difference from their a-traumatic counterpart are the fracture pattern, relatively good bone stock and lack of pre-existing hip pain in the majority of the cases.
Adequate imaging, understanding of the fracture pattern and bone stock is crucial. However, inadequate bone stock might not be easily appreciated on the radiographs, and after intra-operative assessment fracture fixation might not be possible, thus reconstruction options such as augments and acetabular cages should be available as a salvage option. Marongiu et al.14 proposed a 3D printed model to help evaluate the fracture pattern and plan for fixation, this has also been proposed in difficult revision arthroplasty scenarios.15 However, there are cost and time implications with these techniques and they may not be readily available in all centres.
This study aimed at formulating an algorithm to help guide management of traumatic peri-prosthetic acetabular fractures, and reported the outcome of 12 patients with traumatic peri-prosthetic acetabular fractures treated with such algorithm. Some of the reconstruction options for these injuries where the bone stock is sufficient and also where the bone stock is deficient are detailed with specific examples.
It is important to distinguish between acute traumatic acetabular fractures and chronic pelvic discontinuity that happens due to progressive lysis over time. The former can be fixed and reduced. The majority of the cases (75%) in this series had sufficient bone stock that allowed fracture reduction and fixation, followed by re-implantation. The fracture patterns tend to follow the patterns described by Letournel and Judet.11
In our series of 12 patients, we achieved 80% excellent and good outcomes with one patient requiring revision to a constrained liner. Pascarella et al. in their series of 8 traumatic per-prosthetic acetabular fractures reported no need for return to surgery after a minimum of 12 months follow up. In contrast, Peterson et al. reported 8 revisions in 10 patients who were treated non operatively after a mean of 15 months from injury.1
Similar algorithms to ours have been proposed previously. Benazzo et al.16 suggested that if the implant is stable after a traumatic fracture it can be treated conservatively but needs to be reviewed regularly to ensure that the situation does not change. They also suggest that if an implant is unstable then this requires surgery with the view of obtaining stability of the pelvis, restoring bone stock and using either a porous coated implant with screws or a cage and a cemented acetabular component. Pascarella et al.6 looked at both intra operative and traumatic acetabular periprosthetic acetabular fractures. Sixteen out of the 24 cases in their series were fractures that occurred intraoperatively with only 8 cases associated with trauma post operatively. They also recommended conservative management of implants that were deemed stable and surgery for the unstable implants with or without bone loss. Only 5 out of the 8 patients with traumatic periprosthetic acetabular fractures were associated with an unstable acetabular component requiring revision hip surgery.
We believe that the algorithm we propose for traumatic periprosthetic acetabular fractures allows one to answer 3 simple questions which lead you to decide how best to treat the injury. We also provide a very simple and easy to remember aide memoire for surgeons wanting to consider undertaking complex surgery for patients with unstable implants with or without poor bone stock. The simple 4R stages of surgery including removal of implants, reconstruction of the columns, restoration of bony defects and re implantation of a revision prosthesis help surgeons understand, plan and execute the surgical procedure.
The strength of this paper lies in the relatively large number of traumatic peri-prosthetic acetabular fractures reported, which to the best of our knowledge is the largest in literature. The algorithm and aide memoire help guide decision making and also help formulate a peri operative management plan. The weakness is the retrospective design and the relatively short follow up.
11. Conclusion
Surgical management of traumatic periprosthetic acetabular fractures can yield good and excellent results provided that adequate assessment and planning had been carried out. In cases with adequate bone stock implant removal, fracture fixation and re-implantation is a viable option, whereas in cases with inadequate bone stock more complex acetabular reconstruction techniques may be required.
References
- 1.Peterson C.A., Lewallen D.G. Periprosthetic fracture of the acetabulum after total hip arthroplasty. J Bone Joint Surg Am. 1996;78(8):1206–1213. doi: 10.2106/00004623-199608000-00011. [DOI] [PubMed] [Google Scholar]
- 2.Miller A.J. Late fracture of the acetabulum after total hip replacement. J Bone Joint Surg Br. 1972;54(4) doi: 10.1302/0301-620x.54b4.600. [DOI] [PubMed] [Google Scholar]
- 3.Sanchez-Sotelo J., McGrory B.J., Berry D.J. Acute periprosthetic fracture of the acetabulum associated with osteolytic pelvic lesions: a report of 3 cases.[Erratum appears in J Arthroplasty 2000 Jun;15(4):544] J Arthroplasty. 2000;15(1):126–130. doi: 10.1016/S0883-5403(00)91467-0. [DOI] [PubMed] [Google Scholar]
- 4.Judet R., Letournel E. Fractures of the acetabulum: classification and surgical approaches for open reduction. preliminary report. J Bone Joint Surg Am. 1964;46(4):1615–1646. [PubMed] [Google Scholar]
- 5.Della Valle C.J., Momberger N.G., Paprosky W.G. Periprosthetic fractures of the acetabulum associated with a total hip arthroplasty. Instr Course Lect. 2003;52:281–290. [PubMed] [Google Scholar]
- 6.Pascarella R., Sangiovanni P., Cerbasi S. Periprosthetic acetabular fractures: a new classification proposal. Injury. 2018;49:S65–S73. doi: 10.1016/j.injury.2018.09.061. [DOI] [PubMed] [Google Scholar]
- 7.Letournel E. Acetabulum fractures: classification and management. Clin Orthop Relat Res. 1980;151:81. [PubMed] [Google Scholar]
- 8.National Institute for Health and Clinical Excellence The management of hip fracture in adults. Clinical guidline. 2011;2011 [PubMed] [Google Scholar]
- 9.Chesser T., Kelly M. Management of hip fractures in the elderly. Surgery. 2013;31(9):456–459. doi: 10.1016/j.mpsur.2013.06.001. [DOI] [Google Scholar]
- 10.Murray D.W., Fitzpatrick R., Rogers K. The use of the Oxford hip and knee scores. Bone Joint Lett J. 2007;89-B(8):1010–1014. doi: 10.1302/0301-620X.89B8.19424. [DOI] [PubMed] [Google Scholar]
- 11.Matta J. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am. 1996;78(11):1632–1645. [PubMed] [Google Scholar]
- 12.16th Annual Report of the National Joint Registry for England, Wales. Northen Irland and the Isle of Man; uk: 2019. www.njrreports.org [Google Scholar]
- 13.Department of Economic and Social Affairs, Population Division U-N. World Population Prospects. The 2015 Revision.
- 14.Marongiu G., Prost R., Capone A. A new diagnostic approach for periprosthetic acetabular fractures based on 3D modeling: a study protocol. Diagnostics. 2020;10(1) doi: 10.3390/diagnostics10010015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kavalerskiy G., Murylev V., Rukin Y., Elizarov P., Lychagin A., Tselisheva E. Three-dimensional models in planning of revision hip arthroplasty with complex acetabular defects. Indian J Orthop. 2018;52(6):625–630. doi: 10.4103/ortho.IJOrtho_556_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Benazzo F., Formagnana M., Bargagliotti M., Perticarini L. Periprosthetic acetabular fractures. Int Orthop. 2015;39(10):1959–1963. doi: 10.1007/s00264-015-2971-8. [DOI] [PubMed] [Google Scholar]