Abstract
Pelvic ring fractures have increased in incidence and operative fixation over the past several decades. These are dynamic injuries but decisions on operative management are still often made on the basis of static imaging. Expert opinion varies greatly on which injuries require fixation and how much fixation. Examination under anaesthesia has been shown to guide management of pelvic injuries by more accurately assessing levels of instability.
Keywords: Pelvis, Trauma, Fracture, Instability, Osteosynthesis
1. Introduction
Pelvic ring fractures have increased in incidence over the past several decades. During this time rates of operative fixation have increased while mortality and hospital length of stay has declined.1
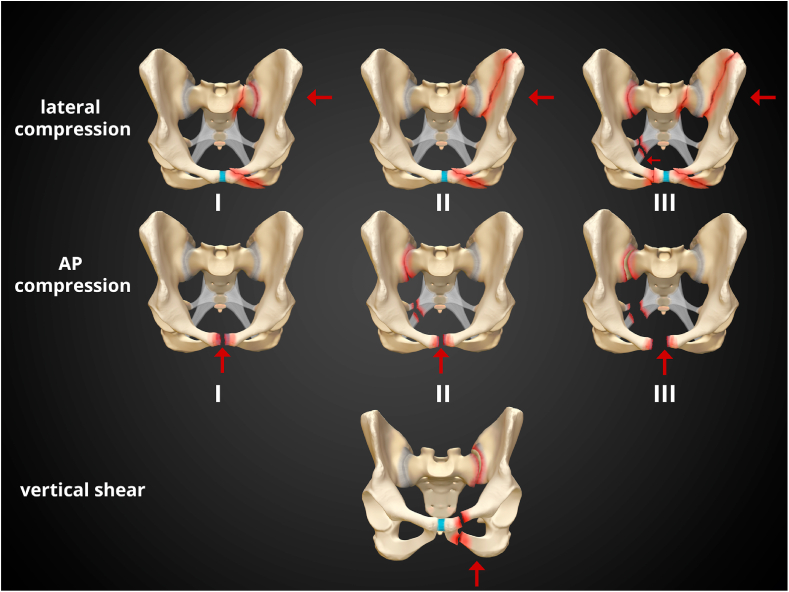
Pennal2 et al. were the first to systematically describe the force vector responsible for pelvic ring injury as AP compression (APC), lateral compression (LC), or vertical shear (VS) (Fig. 1). Later, Tile et al. added the concept of stability.3 In 1986 Young et al. described 142 patient with ring injuries and classified their injuries by mechanism.4
Fig. 1.
Case courtesy of Dr Matt Skalski, Radiopaedia.org, rID: 37824.
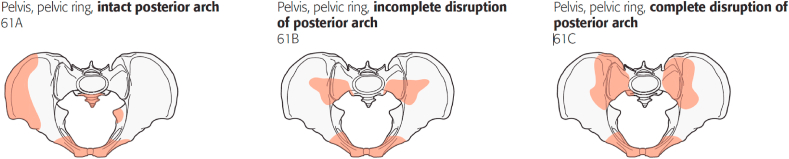
In 2007 the AO and Orthopaedic Trauma Association (OTA) combined their classification system for pelvic ring injuries5 (Fig. 2). These broadly split pelvic fractures into A-type (no posterior ring disruption), B-type (incomplete posterior ring disruption) and C-type (complete posterior ring disruption). B-types can include LC and APC type fractures.
Fig. 2.
Reproduced from fracture and dislocation classification compendium - 2018, J Orthop trauma • Volume 32, number 1 Supplement, January 2018.
All of the currently used classification systems rely upon static imaging, be it plain radiograph or CT. The increased use of pre-hospital and in ER sheets and binders has improved outcomes6 but can mask the true extent of injury.7,8 Additionally pelvic fractures undergo recoil. Gardner et al. showed that in cadavers B-type APC fractures recoiled by up to 48% and LC fractures by 80%.9 The aim of this review is to look at the benefits of using dynamic imaging to assess instability in B-type pelvic fractures.
2. Antero-posterior compression injury
APC pelvic injury are classified from 1 to 3 with increasing instability and disruption. Tile described these through cadaveric video studies. He determined that if the pubic symphyseal disruption was less than 2.5 cm, the pelvic floor and sacroiliac joint remained intact. This is the same situation as occurs during passage of the foetus during labour. Once anterior disruption is greater than 2.5 cm, the pelvic floor and anterior sacroiliac ligaments rupture. The posterior ligaments remain intact thought, so partial stability is maintained.10
Doro et al. re-looked at this with a cadaveric study of their own. They did confirm that the mean diastasis in male specimens was indeed 2.5 cm. However, it was lower in female specimens (1.8 cm). More importantly though, 80% of the specimens recorded diastasis outside of the 2–3 cm range. They were able to confirm that anterior sacroiliac disruption is unlikely under 1.8 cm of diastasis and likely with displacement greater than 4.5 cm.11 This clearly leaves a wide group of patients in a zone where it is unclear if they are APC 1 or 2.
Gary et al. performed MRI imaging and found that contrary to the Young–Burgess classification system, patients with anterior–posterior compression type II injuries had damage to the sacrospinous ligament in only 50% of the cases.12
It is clear from the above that static imaging alone cannot accurately predict stability in these injuries. It is important to be able to differentiate which APC-1s are in fact occult APC-2s. Also which APCs have attenuated posterior sacroiliac ligaments and multiplanar instability.
Sagi et al. described a15 view examination under anaesthetic for occult pelvic ring injury. These consist of static resting films, internal and external rotation stress films, and push-pull manoeuvres of both lower extremities. These are each carried out in the AP, inlet and outlet planes. They found 50% of injuries that had previously been thought of to be APC-1 were sufficiently unstable to warrant anterior fixation. This was defined as greater that 2.5 cm of horizontal rotation. Nearly 40% of APC-2s were shown to have sufficient multiplanar instability to warrant additional posterior ring fixation. This was defined as greater than 2.5 cm of horizontal rotation and greater than 1 cm of vertical rotation.13 Suzuki et al. performed stress exams on all APC-1 presumed injuries over a 4 year period and found 27% were in fact occult APC-2 injuries.14
The latter finding may go some way to explaining why posterior fixation of APC-2 pelvic ring injuries decreases rates of anterior plate failure and malunion.15 Avilucea et al. found a 40% failure rate of anterior only fixation versus only 5% in those fixed posteriorly also. These failures may correlate with the occult multiplanar unstable identified during EUA in other studies.
It is clear that basing treatment on static imaging alone leads to inadequate fixation in some cases with potentially life altering effects on patient outcome.
3. How we treat B-type APC injuries
We suggest using EUA to assess APC injuries dynamically and guide treatment. Our current protocol is to stress all APC injuries. If they are stable on EUA they are treated conservatively and allowed to weight bear as tolerated. Stability is defined as less 2.5 cm of horizontal displacement and less than 1 cm of vertical displacement under stress. If they are found to be unstable on EUA they receive both anterior and posterior fixation. They are kept toe touch weight-bearing on the injured side. Negative stress examination under anaesthesia reliably predicts pelvic ring union without displacement.16
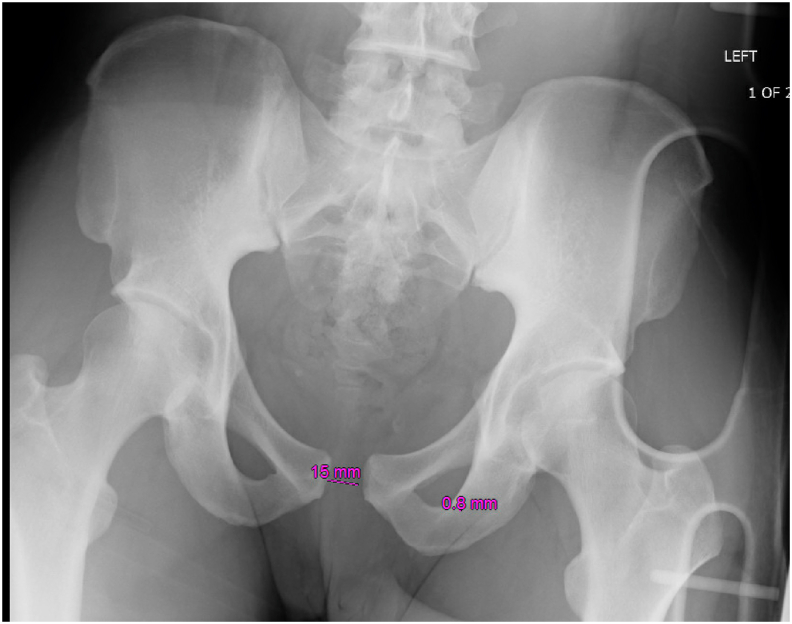
4. B-type APC case
A 25 year old male presented to our unit following a motorcycle crash. He complained of pelvic pain, with no other injuries. His initial AP pelvis out of binder showed a 15 mm symphyseal diastasis (Fig. 3). Doro et al.‘s study would suggest anterior sacroiliac disruption is unlikely with this degree of anterior diastasis. CT following binder placement showed no posterior injury and a further reduction of symphyseal widening.
Fig. 3.
AP Pelvis of APC Pelvic injury.
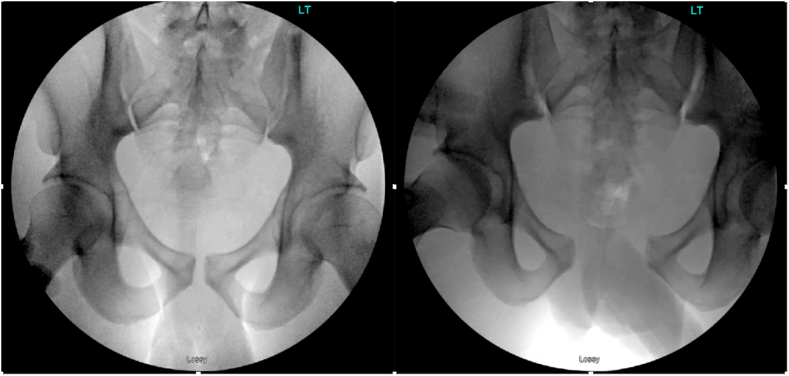
He was taken to the operating room and standard 15 view stress examination was performed. This revealed bilateral posterior ring instability and gross anterior instability (Fig. 4). He therefore received bilateral posterior reduction and stabilisation as well as anterior stabilisation as per our treatment protocol (Fig. 5). At 6 month follow up he was functioning excellently clinically and radiographs showed no loss of reduction (Fig. 6). He is an excellent example of the danger of trusting static imaging alone to assess and APC type pelvic injury.
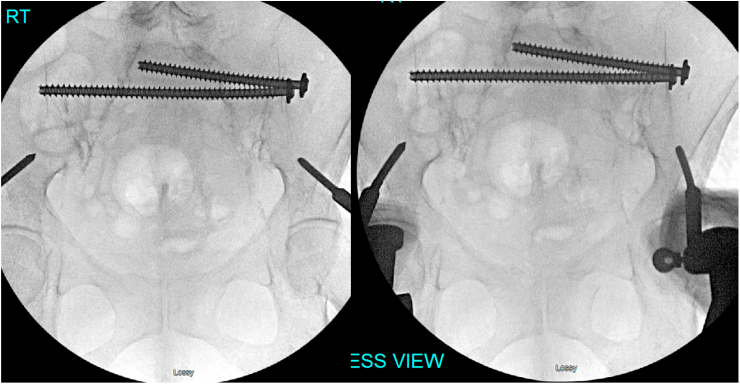
Fig. 4.
AP pelvis with internal (left) and external (right) rotation stress applied.
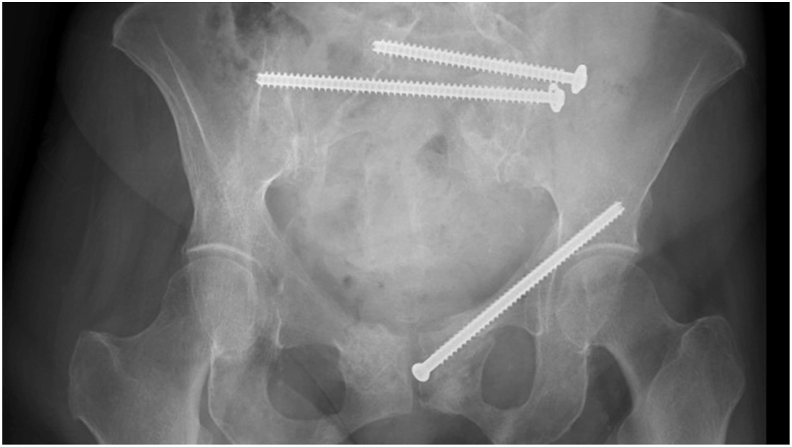
Fig. 5.
AP, inlet and outlet view of bilateral posterior and anterior stabilised pelvis.
Fig. 6.
AP Pelvis at 6 month follow up.
5. Lateral compression fractures
Lateral compression fractures are also classified from 1 to 3 with increasing levels of instability. The LC-1 fracture was historically thought of as being stable vertically and up to 1.5 cm of shortening was deemed acceptable. Stability was thought to be maintained by a relatively intact pelvic floor and/or retention of the posterior ligamentous structure, as well as the impacted fracture.
One of the biggest questions is how can we accurately predict which non-operatively managed lateral compression fractures will displace. Bruce et al. showed that the presence of a complete sacral fracture with rami fracture was a strong predictor of future displacement17 (Table 1).
Table 1.
Reproduced from ‘Bruce B, Reilly M, Sims S. OTA highlight paper predicting future displacement of nonoperatively managed lateral compression sacral fractures: can it be done? [published correction appears in J Orthop Trauma. 2020 Feb; 34(2):e77]. J Orthop Trauma. 2011; 25(9):523–527’.
| Characteristic | Total Number | Number of Displaced | Rate of Displacement |
|---|---|---|---|
| Incomplete sacral fracture + none or unilateral rami fracture | 54 | 0 | 0% |
| Incomplete sacral fracture + bilateral rami fractures | 22 | 2 | 9% |
| Complete sacral fracture + no rami fracture | 2 | 0 | 0% |
| Complete sacral fracture + unilateral rami fracture | 17 | 6 | 33% |
| Complete sacral fracture + bilateral rami fractures | 22 | 15 | 68% |
So the question remains which LC fractures are stable, and which require fixation. Sagi et al. also applied the 15 view EUA which was discussed above for identifying instability in APC injuries to LC fractures. LC-1 fractures with less than 1 cm of overlap were deemed to be stable. 1–2 cm of overlap received anterior fixation only, and greater than 2 cm of overlap received anterior and posterior fixation. 35% of LC-1 fractures were found to be unstable on EUA. Equally interesting only 63% of LC-2s were found to be unstable (any displacement on stressing). As previously discussed with APC injuries a negative stress examination very accurately predicts pelvic union without displacement; with a negative predictive value of 100%. A 2014 survey of 111 OTA members found only a fair agreement rate (K = 0.39) in decisions to operatively or conservatively manage a range of 27 presented LC-1 pelvic fractures. There were only 4 cases where most agreed on operative fixation and 5 where the majority opted for conservative management.18
This type of survey was repeated on a smaller scale in 2020 by Carney et al. but the patients vignettes included EUA findings. 80% of surgeons now agreed on what constituted a stable or unstable injury pattern.19 In theory the gold standard would appear to be EUA of all LC type injuries to assess stability. LC-1 pelvic ring injuries are the most common pelvic ring injury. The disadvantages of EUA include the requirement of sedation, operating room and surgeon utilisation, radiographic exposure, and subjective amount of force used by examiners. A new solution could potentially be the use of lateral decubitus stress radiograph without sedation.20 Parry et al. found 100% correlation with EUA and also all patients were able to tolerate this without any sedation.
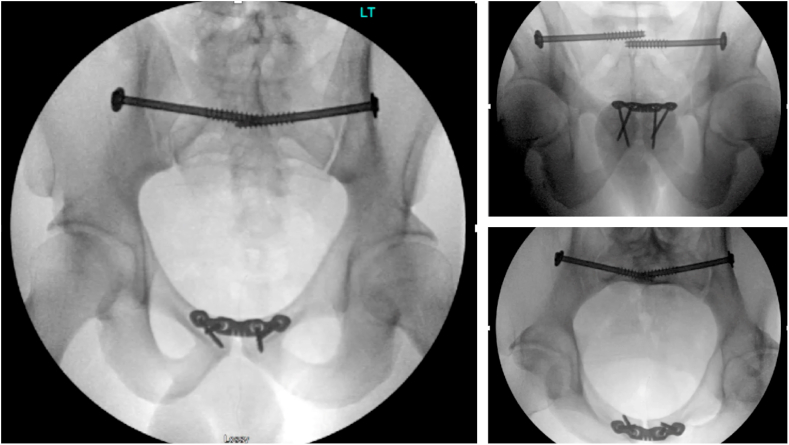
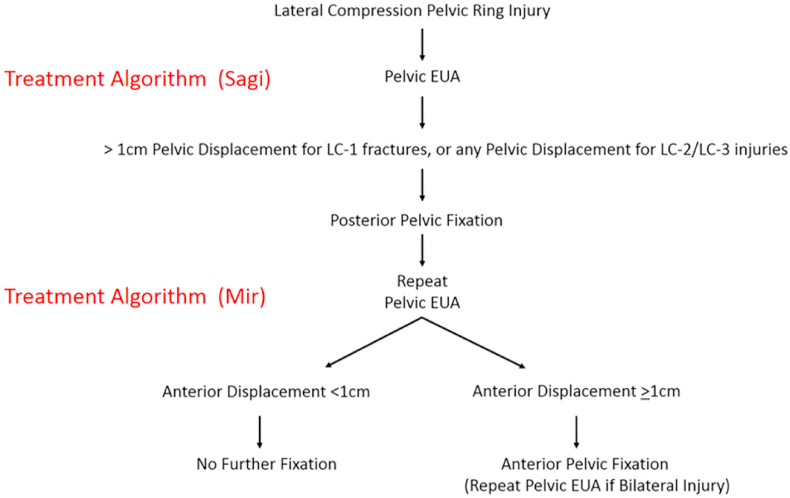
Once the decision has been made to treat an LC fracture surgically, the next question is how much fixation is required. Avilucea et al. described their results of fixation in 74 patients across multiple sites treated by multiple surgeons21 (Fig. 7). They initially fixed the back and then decided upon anterior fixation based on the findings of repeat EUA. Patients who had combined front and back fixation had no late displacement. Those with negative EUAs following posterior fixation, had no anterior fixation placed. Of these patients, those who had a unilateral anterior injury suffered no late displacement. However, those with no anterior fixation on the basis of a negative EUA post posterior fixation with bilateral anterior fractures all displaced within 6 weeks. It would appear, therefore, that all bilateral anterior ring fractures should be fixed regardless of EUA findings.
Fig. 7.
Reproduced with permission from ‘Avilucea FR, Archdeacon MT, Collinge CA, Sciadini M, Sagi HC, Mir HR. Fixation Strategy Using Sequential Intraoperative Examination Under Anaesthesia for Unstable Lateral Compression Pelvic Ring Injuries Reliably Predicts Union with Minimal Displacement. J Bone Joint Surg Am. 2018; 100(17):1503–1508. https://doi.org/10.2106/JBJS.17.01650’.
6. How we treat B-type LC injuries
Incomplete sacral fractures are treated initially non-operatively and allowed to weight-bear as tolerated. If they fail trial by mobilization then they are taken for EUA with likely fixation. If they have a complete sacral fracture they are fixed by sequential EUA protocol starting posteriorly. In cases with bilateral anterior ring injuries at least one side is stabilised regardless of EUA. The patient is then allowed to mobilise touch down or foot flat weight bearing for 12 weeks on the side with posterior injury.
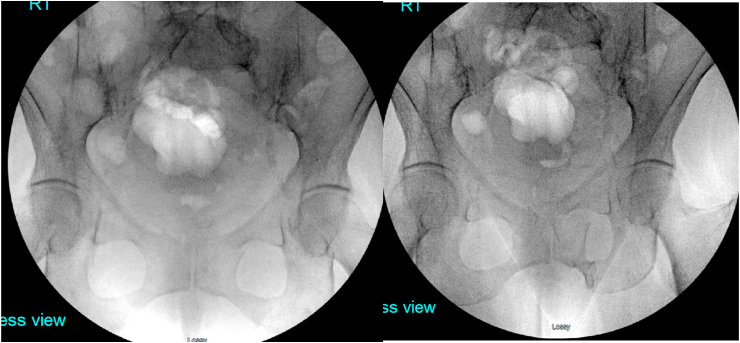
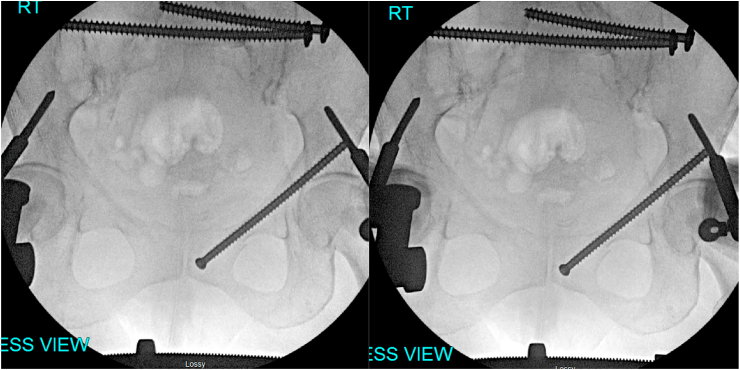
7. B-type LC case
A 70 year old female presented to our unit complaining of low back pain and difficulty mobilising following a fall two days prior. She was evaluated clinically and by plain radiograph (Fig. 8) and CT. She was taken to the operating room and standard 15 view stress examination was performed. Internal rotation revealed instability (Fig. 9). As per our protocol she was fixed initially posteriorly. Repeat stress examination following SI screw placement revealed ongoing instability (Fig. 10). Therefore as per our protocol left sided anterior fixation was placed in the form of a fully threaded retrograde anterior column screw. Stress examination following this additional fixation was negative (Fig. 11). At 6 month follow up she reported excellent clinical outcome and radiographs confirmed union with minimal displacement (Fig. 12).
Fig. 8.
AP Pelvis LC1 type fracture.
Fig. 9.
AP Pelvis with application of external (left image) and internal rotation stress (right image).
Fig. 10.
AP Pelvis following posterior fixation with application of internal rotation stress (right image).
Fig. 11.
AP Pelvis resting (left image) and internal rotation stress (right image).
Fig. 12.
6 month follow up AP radiograph.
8. Discussion
Current indications for the surgical stabilisation of pelvic ring fractures are pain and instability. Tornetta et al. have already shown that stabilisation of sacral fractures improves pain.22 Though it is still not clear whether or not this is to a clinically relevant level. The second indication of instability is where consensus has yet to be reached. Olson defined pelvic stability as one that could withstand the physiologic forces incurred with protected weightbearing, and/or bed to chair mobilization without abnormal deformation of the pelvis, until bony union or soft tissue healing could occur.23 Pelvic instability in C-type fractures is readily appreciated. There is very little consensus though in the treatment of B-type fractures. Pelvic fractures are dynamic and undergo significant recoil. The amount of displacement seen on presentation films can wildly underestimate the maximal displacement that occurred time of injury. The increasingly regular use of potentially lifesaving pelvic binders serves to further mask level of displacement. Landmark papers which tried to classify levels of injury based on fixed levels of displacement, have since been shown to be inaccurate.
LC-1 fractures alone describe a wide spectrum of injury.24 Which of these are deemed to be stable or unstable based on static imaging alone is largely based on expert opinion of the surgeon. There are cases where agreement is more common, such as complete sacral fractures with bilateral ramus fractures. But in many cases there is little or no agreement as shown by the OTA survey papers mentioned above. Vallier et al.‘s retrospective review looked at three hundred and thirty three unilateral sacral fractures treated at 16 different trauma centers.25 Most patients who were treated operatively had less than 5 mm of sacral displacement. Zone 2 fractures were more commonly fixed. Yet in Soles et al.‘s retrospective review 118 patients with less than 10 mm of sacral displacement were treated non-operatively with only one failure.26 The key finding was that a large number of radiographically similar fractures were receiving both operative and non-operative management based on the treating surgeon’s practice.
We believe that this is further evidence for the necessity of EUA to assess the stability and requirement for operative management of pelvic fractures. Our unit believes that the Vallier study demonstrates that centers not utilizing EUA appear to have inconsistent indications for the necessity and type of pelvic fixation. We believe these centers and others should consider adding EUA to their repertoire to help guide their future treatment strategies.27
The counter arguments to EUA include that the thresholds were set by a single expert surgeon. That the forces applied between surgeons vary; and that there is currently no evidence that fixation of fractures deemed to be unstable on EUA is associated with improved patient outcomes.28
It is clear that the negative predictive value of a negative pelvic EUA is very high and useful. Given the level of variability of treatment due to the limitations described above in static imaging, we believe the EUA at the very least should be an adjunct in the armoury of a surgeon looking to determine stability of pelvic ring injuries.
9. Conclusion
The challenges of assessing instability start with the fact that pelvic injuries are dynamic yet the vast majority our decision making is still based on static imaging; be that X-ray, CT or MRI. Examination under anaesthesia can help guide the need for fixation and sequential EUA can help guide fixation strategy. More aggressive surgical treatment can clearly lead to reduced late displacement and early pain. However, fixation of fractures which would have been stable with conservative management increases risks of complications and has associated costs. We are also, still judging treatment success, largely by imaging. More studies are needed to determine the effect of late displacement on functional outcomes.
Contributor Information
Ishvinder Singh Grewal, Email: ishi@doctors.org.uk.
Hasan R. Mir, Email: hmir@floridaortho.com.
References
- 1.Buller L.T., Best M.J., Quinnan S.M. A nationwide analysis of pelvic ring fractures: incidence and trends in treatment, length of stay, and mortality. Geriatr Orthop Surg Rehabil. 2016;7(1):9–17. doi: 10.1177/2151458515616250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pennal G.F., Tile M., Waddell J.P., Garside H. Pelvic disruption: assessment and classification. Clin Orthop Relat Res. 1980;151:12–21. [PubMed] [Google Scholar]
- 3.Tile M., Helfet D., Kellam J. Lippincott Williams & Wilkins; Philadelphia, PA: 2003. Fractures of the Pelvis and Acetabulum. [Google Scholar]
- 4.Young J.W., Burgess A.R., Brumback R.J., Poka A. Pelvic fractures: value of plain radiography in early assessment and management. Radiology. 1986;160(2):445–451. doi: 10.1148/radiology.160.2.3726125. [DOI] [PubMed] [Google Scholar]
- 5.Marsh J.L., Slongo T.F., Agel J. Fracture and dislocation classification compendium - 2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007;21(10 Suppl):S1–S133. doi: 10.1097/00005131-200711101-00001. [DOI] [PubMed] [Google Scholar]
- 6.Hsu S.D., Chen C.J., Chou Y.C., Wang S.H., Chan D.C. Effect of early pelvic binder use in the emergency management of suspected pelvic trauma: a retrospective cohort study. Int J Environ Res Publ Health. 2017;14(10):1217. doi: 10.3390/ijerph14101217. Published 2017 Oct 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Clements J., Jeavons R., White C., McMurtry I. The concealment of significant pelvic injuries on computed tomography evaluation by pelvic compression devices. J Emerg Med. 2015;49(5):675–678. doi: 10.1016/j.jemermed.2015.03.014. [DOI] [PubMed] [Google Scholar]
- 8.Fletcher J., Yerimah G., Datta G. The false security of pelvic binders: 2 cases of missed injuries due to anatomical reduction. J Orthop Case Rep. 2016;6(1):44–47. doi: 10.13107/jocr.2250-0685.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gardner M.J., Krieg J.C., Simpson T.S., Bottlang M. Displacement after simulated pelvic ring injuries: a cadaveric model of recoil. J Trauma. 2010;68(1):159–165. doi: 10.1097/TA.0b013e31819adae2. [DOI] [PubMed] [Google Scholar]
- 10.Tile M. Acute pelvic fractures: I. Causation and classification. J Am Acad Orthop Surg. 1996;4(3):143–151. doi: 10.5435/00124635-199605000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Doro C.J., Forward D.P., Kim H. Does 2.5 cm of symphyseal widening differentiate anteroposterior compression I from anteroposterior compression II pelvic ring injuries? J Orthop Trauma. 2010;24(10):610–615. doi: 10.1097/BOT.0b013e3181cff42c. [DOI] [PubMed] [Google Scholar]
- 12.Gary J.L., Mulligan M., Banagan K., Sciadini M.F., Nascone J.W., Oʼtoole R.V. Magnetic resonance imaging for the evaluation of ligamentous injury in the pelvis: a prospective case-controlled study. J Orthop Trauma. 2014;28(1):41–47. doi: 10.1097/BOT.0b013e318299ce1b. [DOI] [PubMed] [Google Scholar]
- 13.Sagi H.C., Coniglione F.M., Stanford J.H. Examination under anesthetic for occult pelvic ring instability. J Orthop Trauma. 2011;25(9):529–536. doi: 10.1097/BOT.0b013e31822b02ae. [DOI] [PubMed] [Google Scholar]
- 14.Suzuki T., Morgan S.J., Smith W.R., Stahel P.F., Flierl M.A., Hak D.J. Stress radiograph to detect true extent of symphyseal disruption in presumed anteroposterior compression type I pelvic injuries. J Trauma. 2010;69(4):880–885. doi: 10.1097/TA.0b013e3181efbad5. [DOI] [PubMed] [Google Scholar]
- 15.Avilucea F.R., Whiting P.S., Mir H. Posterior fixation of APC-2 pelvic ring injuries decreases rates of anterior plate failure and malunion. J Bone Joint Surg Am. 2016;98(11):944–951. doi: 10.2106/JBJS.15.00723. [DOI] [PubMed] [Google Scholar]
- 16.Whiting P.S., Auston D., Avilucea F.R. Negative stress examination under Anesthesia reliably predicts pelvic ring union without displacement. J Orthop Trauma. 2017;31(4):189–193. doi: 10.1097/BOT.0000000000000766. [DOI] [PubMed] [Google Scholar]
- 17.Bruce B., Reilly M., Sims S. OTA highlight paper predicting future displacement of nonoperatively managed lateral compression sacral fractures: can it be done? [published correction appears in J Orthop Trauma. 2020 Feb;34(2):e77] J Orthop Trauma. 2011;25(9):523–527. doi: 10.1097/BOT.0b013e3181f8be33. [DOI] [PubMed] [Google Scholar]
- 18.Beckmann J.T., Presson A.P., Curtis S.H. Operative agreement on lateral compression-1 pelvis fractures. a survey of 111 OTA members. J Orthop Trauma. 2014;28(12):681–685. doi: 10.1097/BOT.0000000000000133. [DOI] [PubMed] [Google Scholar]
- 19.Carney JJ, Nguyen A, Alluri RK, Lee AK, Marecek GS. A survey to assess agreement between pelvic surgeons on the outcome of exam under Anesthesia for lateral compression pelvic fractures. J Orthop Trauma. 2020;34(9):e304–e308. doi: 10.1097/BOT.0000000000001759. [DOI] [PubMed] [Google Scholar]
- 20.Parry J.A., Salameh M., Maher M.H., Stacey S.C., Mauffrey C. The lateral stress radiograph identifies occult instability of lateral compression pelvic ring injuries without sedation [published online ahead of print, 2020 may 7] J Orthop Trauma. 2020 doi: 10.1097/BOT.0000000000001805. [DOI] [PubMed] [Google Scholar]
- 21.Avilucea F.R., Archdeacon M.T., Collinge C.A., Sciadini M., Sagi H.C., Mir H.R. Fixation Strategy using sequential intraoperative examination under Anesthesia for unstable lateral compression pelvic ring injuries reliably predicts union with minimal displacement. J Bone Joint Surg Am. 2018;100(17):1503–1508. doi: 10.2106/JBJS.17.01650. [DOI] [PubMed] [Google Scholar]
- 22.Tornetta P., 3rd, Lowe J.A., Agel J. Does operative intervention provide early pain relief for patients with unilateral sacral fractures and minimal or No displacement? J Orthop Trauma. 2019;33(12):614–618. doi: 10.1097/BOT.0000000000001578. [DOI] [PubMed] [Google Scholar]
- 23.Olson S.A., Pollak A.N. Assessment of pelvic ring stability after injury. Indications for surgical stabilization. Clin Orthop Relat Res. 1996;329:15–27. doi: 10.1097/00003086-199608000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Lefaivre K.A., Padalecki J.R., Starr A.J. What constitutes a Young and Burgess lateral compression-I (OTA 61-B2) pelvic ring disruption? A description of computed tomography-based fracture anatomy and associated injuries. J Orthop Trauma. 2009;23(1):16–21. doi: 10.1097/BOT.0b013e31818f8a81. [DOI] [PubMed] [Google Scholar]
- 25.Vallier H.A., Lowe J.A., Agel J. Surgery for unilateral sacral fractures: are the indications clear? J Orthop Trauma. 2019;33(12):619–625. doi: 10.1097/BOT.0000000000001587. [DOI] [PubMed] [Google Scholar]
- 26.Sembler Soles G.L., Lien J., Tornetta P., 3rd Nonoperative immediate weightbearing of minimally displaced lateral compression sacral fractures does not result in displacement. J Orthop Trauma. 2012;26(10):563–567. doi: 10.1097/BOT.0b013e318251217b. [DOI] [PubMed] [Google Scholar]
- 27.Mir H.R. Commentary on: "surgery for unilateral sacral fractures: are the indications clear? J Orthop Trauma. 2019;33(12):625–626. doi: 10.1097/BOT.0000000000001628. [DOI] [PubMed] [Google Scholar]
- 28.Vallier H.A., Tornetta P., 3rd In response. J Orthop Trauma. 2019;33(12):626–627. doi: 10.1097/BOT.0000000000001647. [DOI] [PubMed] [Google Scholar]