Abstract
The negative effects of long-term stress on health outcomes are well-documented. Emerging technologies that harness mobile technologies have been linked to positive effects on stress management. However, the ways in which existing inter- and intrapersonal theories of behavior change are integrated into development processes of these mHealth technologies for stress coping are limited. In this paper, we present a novel theory-driven approach to develop and implement a sustainable mobile application for stress education and management. Specifically, we integrate the taxonomy of Behavior Change Techniques and user engagement framework to model and adapt theory-driven techniques in the context of mobile technologies. A total of 12 behavior change techniques were incorporated into our mobile application. Initial user evaluation and usability testing was conducted. Results indicate heuristic modifications could improve overall delivery of content, and potential user satisfaction is likely. We conclude that this novel approach may have implications well beyond stress management.
Keywords: Psychological stress, behavior therapy, telemedicine
Introduction
Psychological stress (in lay terms, stress) occurs when the demands on an individual exceed the ability to cope [1]. The negative effects of long-term stress on human health has been well-documented [2]. Stress includes mental health symptoms such as anxiety and depression [3]. The global cost of mental illness is estimated at one trillion dollars and affects 300 million people [4]. Americans’ average stress levels are 4.8 out of 10, 45% experience sleeplessness due to stress, and 75 % experienced 1 or more symptoms of stress in the previous month, including nervousness or anxiousness [5]. Stress costs the U.S. enterprise economy up to 2.6% of the GDP annually and in Europe the cost can be as much as 3.3% [6]. Stress can be managed using self-care behaviors, such as avoiding alcohol, finding social support, eating and sleeping well, and staying active [7]. Literature shows that evidence-based practice can reduce perceived stress [8]. Recently, mHealth applications promoting behavioral change were found to have positive effects on workers’ perceived stress [9].
Emerging trends in mobile smartphone apps can provide new frontiers to management of chronic conditions such as stress [10]. 77% of Americans own mobile smartphones, and 90% own a mobile phone of some kind [11]. With mobile network capabilities and affordable smartphones reaching well beyond other infrastructure in countries with low- and mid-range economies, mHealth and health promotion efforts in these areas are able to be offered in new ways via mobile phone technology, such as personalized care or public health [12]. Literature suggests that cost effectiveness of mHealth solutions is likely [13]. Platforms for mHealth or eHealth with designs that allow for innovation in aspects such as use, utility, financial impact, sustainability, scalability, and impact will be needed for advancement [14,15]. Mobile health technology can improve user adherence in a variety of health behaviors [16,17]. It is known that mHealth also can deliver education and patient selfcare, among other health benefits [18]. Evidence-based smartphone apps for mental health have been shown to be effective and to have the potential to reach beyond current treatment limitations [19]. Large-scale clinical trials establishing effectiveness and efficacy of using app based modalities are sparse and often indecisive. Despite the overall lack of evidence-based smartphone apps in existence, there is potential for successful delivery of evidence-based stress management strategies [20]. Efforts have been made to understand the utility and manifestation of behavior change techniques, however, specific software development approaches to generate synergistic collaborations between technology developers and health research are limited [21]. In this paper, we present an integrative approach to infuse theory-driven techniques and engagement features to develop novel, evidence-based, and engaging mHealth applications. Specifically, we utilized the taxonomy of Behavior Change Techniques (BCT taxonomy) [22] and the Patient engagement framework [23] to consolidate uniquely identified behavior change concepts and user engagement features in a mobile format. In the next sections of the paper, we describe in detail our approach for the development of a mobile application, NewCope, and initial results of the system evaluation through user testing and usability analysis.
Related Works
Existing work focusses on reviews of smartphone apps that deliver stress management behavior therapy. For example, the “Tension Tamer” app, which uses systolic blood pressure as a measure of stress, focused on breathing awareness meditation [24]. Similarly, heartrate has been used as a measure of stress in the “It’s Time to Relax” app, which focuses on mindfulness [25]. Similarly, the “Virtual Hope Box” app was designed based on Cognitive Behavioral Therapy (CBT) [26]. “Headspace,” which utilizes mindfulness and meditation, has been used for stress management delivery in multiple mHealth stress management studies [27, 28].
Additionally, other mHealth solutions have been developed to address the needs facing delivery of stress management therapy. Method of Levels transdiagnostic cognitive therapy was used in the development of the “MindSurf” app, which showed positive results in preliminary function and usability testing [29]. And importantly, the Virgin Pulse Global Initiative (VPGI) was an mHealth solution that overcame existing paradigms to show a positive outcome for workers completing the mHealth behavioral program [9].
Methods
Theoretical Rationale
Taxonomy of Behavior Change Techniques
Michie et al. [22] defined a set of theory-linked techniques that can be used to integrate, implement, and harness multiple theoretical constructs to unify inter- and intra-personal processes of human behavior into technology features that can assist and support sustainable positive health behaviors. Their taxonomy of 93 theory-linked techniques is the first step towards creating a model that provides a snapshot of intervention content in the context of theory-driven behavior change constructs [22]. The taxonomy provides a common vocabulary to understand the ways that sociobehavioral and cognitive constructs of the existing behavior change theories can be operationalized in a specific intervention. The complete list of techniques of the taxonomy with definitions and detailed examples can be found here [22].
Patient Engagement Framework (PEF)
The PEF has been developed by the Healthcare Information and Management Systems Society (HIMSS) through a cumulative layering of five phases: “inform me,” “engage me,” “empower me,” “partner with me,” and “support my e-community.” A total of nine features have been specified at the highest engagement level, including ‘information and way-finding’, ‘e-tools’, ‘forms’, ‘patient-specific education’, ‘patient access and use’, ‘patient generated data’, ‘interoperable records’, ‘collaborative care and community support’[23]. This framework was used in our study to sketch the functionality of the mHealth infrastructure which potentially facilitates the adoption of the tool, self-management, goal setting and reinforcement, peer support, and patient-provider communication.
Technology-Theory-Engagement Mapping
A mapping process was conducted to identify BCT techniques in conjunction with user engagement features that could be used to operationalize the delivery of stress management-related content to users. The BCT techniques allowed us to understand the characteristics of the information that should be delivered to the user. We also specified the level of intended user engagement to characterize the granularity and complexity of the system features. Tables 1 and 2 provide a summary of the BCTs and engagement functions that were selected for implementation at feature level and content level.
Table 1–
Theory Mapping for App Content and Functions
| BCT name | Definition | Example |
|---|---|---|
| Instruction on how to perform the behavior | Advise or agree on how to perform the behavior | Education |
| Social comparison | Draw attention to others’ performance to allow comparison with the person’s own performance | Education |
| Self-talk | Prompt positive self-talk before and during the behavior | Daily task |
| Valued self-identity | Advise the person to write or complete rating scales about cherished value or personal strength as a means of affirming the person’s identity as part of behavior change strategy | Journal |
| Information about health consequences | Provide information about health consequences of performing the behavior | Education |
| Incentive | Inform that a reward will be delivered if and only if there has been effort and/or progress in achieving the behavioral outcome | Daily task |
| Self-monitoring of behavior | Establish a method for the person to monitor and record their behavior(s) as part of a behavior change strategy | Progress |
| Behavior practice/rehearsal | Prompt practice or rehearsal of the performance of the behavior one or more times in a context or at a time when the performance may not be necessary, in order to increase habit and skill | Daily task |
| Focus on past success | Advise to think about or list previous successes in performing the behavior | Daily task |
| Social support (emotional) | Advise on, arrange, or provide emotional social support for performance of the behavior | Daily task |
| Credible source | Present verbal or visual communication from a credible source in favor of or against the behavior | Education |
| Restructuring the social environment | Change, or advise to change the social environment in order to facilitate performance of the wanted behavior | Daily task |
Table 2-.
Engagement Features and Ontology Relations
| Engagement phase | Description | Technology feature |
|---|---|---|
| Engage (Level 2) Self-monitoring Goal setting |
e-Tools | Perceived stress scale integration Daily task |
| Create synergy and extend reach (Level V) Self-management Daily reminders (e.g. Lifestyle tip) |
Education User-specific feedback |
Stress feedback Journal Daily task Progress summary |
Development
NewCope was built on the opensource Ionic Framework (ICL version 4.1.1) [30]. Native Ionic features such as modals, cards, slides and buttons were used in the app design, in addition to custom coded features such as the progress bar and imbedded “fun fact” questions. The NewCope design does not necessitate the collection of any Personal Health Information (PHI) including email address or other personally identifying user information, so Google’s Firebase database was used for the sake of simplicity and ease of set-up. User authentication was handled via a user-generated username and password.
NewCope has five main component pages, including a homepage with primarily informational resources, a dashboard page that provides feedback to the user, a self assessment page, a journal page, and a page that offers information about the app, help to the user, and a place to contact the researchers.
The health education materials provided in the application relate to stress prevalence [31, 32], guides meditation, stress management techniques associated with relatable people as #hashtag signs. The dashboard includes a checklist of three daily tasks designed to help the user adopt and sustain positive health changes that can aid them in stress coping with user-specific feedback, thus promoting self-monitoring habits. As can be seen in Figure 1, examples of tasks on the daily checklist are “listen to music,” “go through old photo albums,” “call a loved one”, and “write your personality strengths.” These tasks are related to the specific BCT techniques, “Restructuring the social environment”, “Valued self-identity”, and “Social support (emotional)” respectively.
Figure 1–
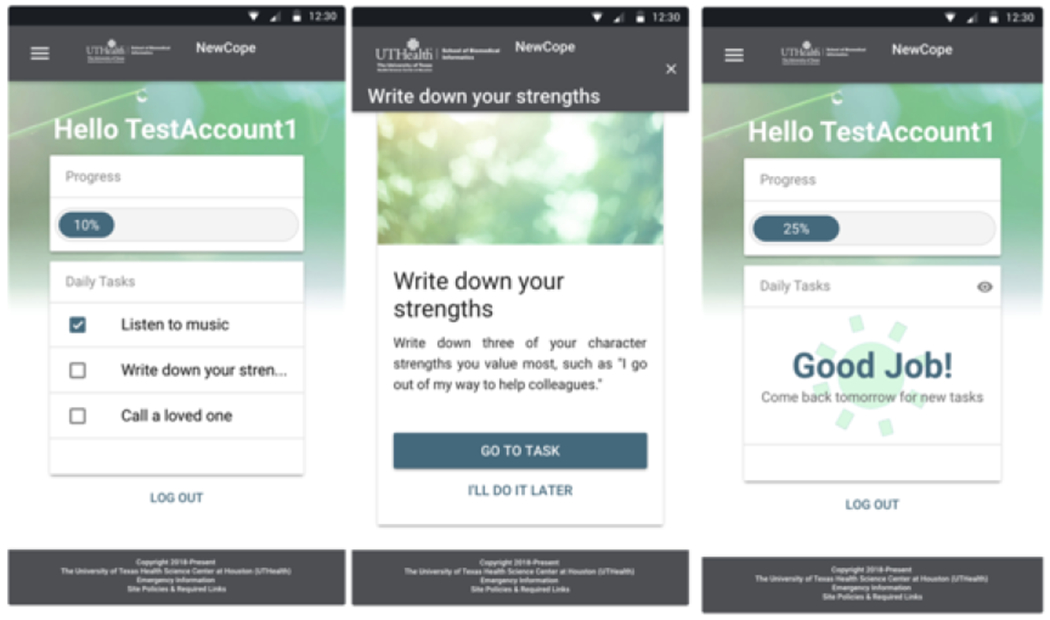
“NewCope” Dashboard
The self-assessment page utilizes the Perceived Stress Scale to evaluate the user’s perceived stress level as low, medium or high [33]. The monitoring instrument addresses specific BCT techniques, “Feedback and monitoring” and “Goals and planning.” The journal page is designed for use both in daily tasks that the user is asked to complete, such as “write down your strengths,” which embodies “Self-belief”, and for general use by the user, which further supports “Identity.” Journal entries are designed to appear on “sticky note” graphic elements that can be edited, deleted, and rearranged by the user.
Evaluation
The prototyped app was reviewed for usability and accessibility and for use by human participants. One usability expert evaluated the user interface and generated a list of heuristic violations according to the Nielsen–Shneiderman Heuristics [34]. For each violation a severity rating (scale 1 – 4 where 1-Minor, 2-Moderate, 3-Major, 4-Catstrophic) was assigned. The design was refined to meet shortfalls that were most relevant to user testing. A secondary usability evaluation was conducted with five participants, selected based on recruitment by the researchers. The participants were recruited to test the app via a protocol of six timed tasks and the System Usability Scale (SUS) [35]. The UTHealth Internal Review Board approved the study for human participants.
Results
Initial Evaluation
The results from the heuristic evaluation revealed a total of 47 violations, eight of which were minor, 14 moderate, 19 major, and six catastrophic. Most violations represented issues with consistency (see Table 3).
Table 3–
Heuristic Evaluation Summary
| Violations | Minor | Moderate | Major | Catastrophic | Total |
|---|---|---|---|---|---|
| Consistency | 5 | 3 | 7 | 1 | 16 |
| Control | 1 | 1 | 1 | 3 | |
| Flexibility | 1 | 1 | 2 | ||
| Help | 2 | 1 | 1 | 4 | |
| Language | 2 | 1 | 4 | 1 | 8 |
| Match | 4 | 1 | 1 | 6 | |
| Memory | 1 | 1 | |||
| Minimalism | 1 | 1 | |||
| Visibility | 2 | 3 | 1 | 6 | |
| Total | 8 | 14 | 19 | 6 | 47 |
The results from the user evaluation were as follows: All users were successful in completing all tasks, though some required assistance. The percentage of independent user completion was between 40 and 80% for all tasks, with user satisfaction maintaining a score between 1.2 and 1.8 for all tasks. The average completion time for tasks was between 8.0 and 126.8 seconds (see Table 4).
Table 4–
Task Completion Summary
| Task Area |
||||||
|---|---|---|---|---|---|---|
| Create Account | Self Assessment | Checklist | Video | Journal Entry | Article | |
| User completed independently | 80% | 40% | 60% | 80% | 80% | 80% |
| Average completion time (sec) | 50.4 | 126.8 | 8.0 | 88.4 | 38.4 | 59.0 |
| Average user satisfaction 1-high 5-low | 1.6 | 1.8 | 1.8 | 1.5 | 1.2 | 1.2 |
As seen in Table 5, the SUS scale results for positively correlated items showed an average of 4.04 out of 5, while negatively correlated items showed an average of 1.28 out of 5. Average item scores for positively correlated items were between 3.6 and 5.0, while average negatively correlated item scores were between 1.0 and 1.4.
Table 5–
SUS Summary
| Positive Items | Frequency | Easy | Integration | Learnable | Confident |
|---|---|---|---|---|---|
| Mean | 3.6 | 3.8 | 3.8 | 5.0 | 4.0 |
| Range | 1-5 | 2-5 | 2-5 | 5 | 2-5 |
| Negative Items | Complex | Technical | Inconsistent | Cumbersome | Acquisition |
| Mean | 1.4 | 1.2 | 1.4 | 1.4 | 1.0 |
| Range | 1-2 | 1-2 | 1-3 | 1-2 | 1-1 |
Discussion
While the sample size limits the statistical validity of the quantitative data, we do observe the clustering of responses on the SUS items, particularly the negatively correlated items. This potentially indicates that participants in the trial were more consistently not put off by the system than that there was a consistent desire among the participants to use the system. As participants were not screened for stress level or desire for stress management, this result may not be unexpected. In fact, our findings from the evaluation determined that the average user stress level was 21.2 out of 40, which is classified as “moderate stress.” Qualitative user data has indicated that users were often uncertain if task completion for the purposes of the trial included clicking buttons, with 5 of 11 trial administrator interventions based on helping the user to decide on button pressing behavior. This was primarily seen in the Self-assessment task (n = 3). Additionally, qualitative data shows that users had trouble locating the task checklist on the dashboard screen when described as a “checklist.” This accounted for the 40% administrator assistance rate on the View Checklist task, and 20% of the administrator assistance rate on the Self-Assessment task. User suggestions included using larger font sizes for the buttons, moving the “quit assessment” button further away from the “next question” button, and having Google prompt the user to automatically remember the password. User results do not, however, indicate a barrier to delivering BCTs via a smartphone app. All heuristic and user-identified barriers to the usage of the app were based on the user experience and user interface critiques. Design features can be further refined to create a smoother user experience while maintaining the necessary BCT components.
Methodical integration of known behavior change techniques has resulted in the convergence of constructs from multiple theories of behavior change including the Transtheoretical Model of Change [36], Social Cognitive Theory [37], and Health Belief Model [38], thereby ensuring our application harnesses inter- and intra-personal processes of behavior change [39]. Further, predetermined engagement levels allowed rapid prototyping with a generalized understanding of software features and malleable modes of theory-driven content delivery. This, while leaving room for clinical partner and wellness service integration, which is vital for large-scale dissemination of health promotion technologies.
Limitations
There are several limitations to our study. We have used a specific theoretical taxonomy to guide the development process. While the taxonomy is integrative, participatory and crowdsourced design activities that employ social listening can result in a holistic development approach. Additional features, including online communities and smart technology synching, are important to improve the user experience and sustained use of NewCope. Our evaluation results are limited by the size of the participant pool and did not account for long term user engagement measures. Future studies should consider large-scale evaluations for better understanding of the acceptance of technologies such as NewCope.
Conclusions
Mental well-being, chronic disease management, and general health are affected by an individual’s ability to manage stress, playing a role in one’s happiness and productivity. Our paper describes a novel approach for the integration of evidence-based, theory-driven techniques in the digital era. The proposed approach is generalizable to other health conditions and can have implications well beyond stress management. Integration of theoretical models of human behavior into emerging technological domains such as mobile applications is important to facilitate effective dissemination of evidence-based strategies at scalable and sustainable levels. Attrition with the use of technology-based health promotion can be addressed with the proper implementation of user engagement principles.
Acknowledgements
Research reported in this publication was partially supported by the National Cancer Institute of the National Institutes of Health under Award Number R21CA220670 and funds by the Patient Safety Quality Care project. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- [1].Lazarus RS, and Folkman S. Stress, Appraisal and Coping, Springer, New York, 1984. [Google Scholar]
- [2].National Institute of Mental Health. 5 Things You Should Know About Stress, (n.d). https://www.nimh.nih.gov/health/publications/stress/index.shtml (accessed October 25, 2018).
- [3].American Heart Association Lower Stress: How does stress affect the body? (n.d.). http://www.heart.org/en/healthy-living/healthy-life-style/stress-management/lower-stress-how-does-stress-affect-the-body (accessed October 25, 2018).
- [4].WHO | Mental health in the workplace, WHO; (n.d.). http://www.who.int/mental_health/in_the_workplace/en/ (accessed October 25, 2018). [Google Scholar]
- [5].American Psychological Association. Stress in America, (2017). https://www.apa.org/news/press/release/stress/2017/state-nation.pdf (accessed October 11, 2018).
- [6].Brun JP. Work-related stress: scientific evidence-base of risk factors, prevention and costs, (n.d.). https://www.who.int/occupational_health/topics/brunpres0307.pdf?ua=1 (accessed October 22, 2018).
- [7].Centers for Disease Control and Prevention. Coping with Stress, (2018). https://www.cdc.gov/features/copingwith-stress/index.html (accessed October 21, 2018).
- [8].Stillwell SB, Vermeesch AL, and Scott JG, Interventions to Reduce Perceived Stress Among Graduate Students: A Systematic Review With Implications for Evidence-Based Practice, Worldviews on Evidence-Based Nursing. 14 (2017) 507–513. doi: 10.1111/wvn.12250. [DOI] [PubMed] [Google Scholar]
- [9].Meyer D, Jayawardana MW, Muir SD, Ho DY-T, and Sackett O, Promoting Psychological Well-Being at Work by Reducing Stress and Improving Sleep: Mixed-Methods Analysis, J Med Internet Res. 20 (2018). doi: 10.2196/jmir.9058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Coulon SM, Monroe CM, and West DS, A Systematic, Multi-domain Review of Mobile Smartphone Apps for Evidence-Based Stress Management, Am J of Preventive Medicine. 51 (2016) 95–105. doi: 10.1016/j.ame-pre.2016.01.026. [DOI] [PubMed] [Google Scholar]
- [11].Pew Research Center. Mobile Fact Sheet, (n.d.). http://www.pewinternet.org/fact-sheet/mobile/ (accessed November 2, 2018).
- [12].Kay M, Santos J, Takane M. MHealth: new horizons for health through mobile technologies, WHO Global Observatory for eHealth and the World Health Organization, Geneva, 2011. http://www.who.int/goe/publications/goe_mhealth_web (accessed November 2, 2018). [Google Scholar]
- [13].Iribarren SJ, Cato K, Falzon L, and Stone PW, What is the economic evidence for mHealth? A systematic review of economic evaluations of mHealth solutions, PloS One. 12 (2017) e0170581. doi: 10.1371/journal.pone.0170581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Depasse J, Caldwell A, Santorino D, Bailey E, Gudapakkam S, Bangsberg D, and Olson K, Affordable medical technologies: bringing Value-Based Design into global health, BMJ Innov.2 (2016) 4–7. doi: 10.1136/bmjinnov-2015-000069. [DOI] [Google Scholar]
- [15].World Health Organization. Monitoring and evaluating digital health interventions: a practical guide to conducting research and assessment, (2016). http://www.who.int/reproductivehealth/publications/mhealth/digital-health-interventions/en/ (accessed October 25, 2018).
- [16].Gandapur Y, Kianoush S, Kelli HM, Misra S, Urrea B, Blaha MJ, Graham G, Marvel FA, and Martin SS, The role of mHealth for improving medication adherence in patients with cardiovascular disease: a systematic review, Eur Heart J Qual Care Clin Outcomes. 2 (2016) 237–244. doi: 10.1093/ehjqcco/qcw018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Ifejika NL, Noser EA, Grotta JC, and Savitz SI, Swipe out Stroke: Feasibility and efficacy of using a smart-phone based mobile application to improve compliance with weight loss in obese minority stroke patients and their carers, International Journal of Stroke. 11 (2016) 593–603. doi: 10.1177/1747493016631557. [DOI] [PubMed] [Google Scholar]
- [18].Alghamdi M, Gashgari H, and Househ M. A systematic review of mobile health technology use in developing countries, Stud Health Technol Inform. 213 (2015) 223–226. doi: 10.3233/978-1-61499-538-8-223 [DOI] [PubMed] [Google Scholar]
- [19].Chandrashekar P, Do mental health mobile apps work: evidence and recommendations for designing high-efficacy mental health mobile apps, Mhealth. 4 (2018). doi: 10.21037/mhealth.2018.03.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Donker T, Petrie K, Proudfoot J, Clarke J, Birch M-R, and Christensen H, Smartphones for Smarter Delivery of Mental Health Programs: A Systematic Review, J Med Internet Res. 15 (2013). doi: 10.2196/jmir.2791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].de Korte E, Wiezer N, Bakhuys Roozeboom M, Vink P, and Kraaij W, Behavior Change Techniques in mHealth Apps for the Mental and Physical Health of Employees: Systematic Assessment, JMIR Mhealth Uhealth. 6 (2018). doi: 10.2196/mhealth.6363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, Eccles MP, Cane J, and Wood CE, The Behavior Change Technique Taxonomy (v1) of 93 Hierarchically Clustered Techniques: Building an International Consensus for the Reporting of Behavior Change Interventions, Ann Behav Med. 46 (2013) 81–95. doi: 10.1007/s12160-013-9486-6. [DOI] [PubMed] [Google Scholar]
- [23].HIMSS Patient Engagement Framework. https://www.himss.org/himss-patient-engagement-framework (accessed November 24, 2018).
- [24].Adams ZW, Sieverdes JC, Brunner-Jackson B, Mueller M, Chandler J, Diaz V, Patel S, Sox LR, Wilder S, and Treiber FA, Meditation smartphone application effects on prehypertensive adults’ blood pressure: Dose-response feasibility trial., Health Psychology. 37 (2018) 850–860. doi: 10.1037/hea0000584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Carissoli C, Villani D, and Riva G, Does a Meditation Protocol Supported by a Mobile Application Help People Reduce Stress? Suggestions from a Controlled Pragmatic Trial, Cyberpsychology, Behavior, and Social Networking. 18 (2015) 46–53. doi: 10.1089/cyber.2014.0062. [DOI] [PubMed] [Google Scholar]
- [26].Bush NE, Smolenski DJ, Denneson LM, Williams HB, Thomas EK, and Dobscha SK, A Virtual Hope Box: Randomized Controlled Trial of a Smartphone App for Emotional Regulation and Coping With Distress, PS. 68 (2016) 330–336. doi: 10.1176/appi.ps.201600283. [DOI] [PubMed] [Google Scholar]
- [27].Laurie J, and Blandford A, Making time for mindfulness, Int J Med Inform. 96 (2016) 38–50. doi: 10.1016/j.ijmedinf.2016.02.010. [DOI] [PubMed] [Google Scholar]
- [28].Wen L, Sweeney TE, Welton L, Trockel M, and Katznelson L, Encouraging Mindfulness in Medical House Staff via Smartphone App: A Pilot Study, Acad Psychiatry. 41 (2017) 646–650. doi: 10.1007/s40596-017-0768-3. [DOI] [PubMed] [Google Scholar]
- [29].Carey TA, Haviland J, Tai SJ, Vanags T, and Mansell W, MindSurf: a pilot study to assess the usability and acceptability of a smartphone app designed to promote contentment, wellbeing, and goal achievement, BMC Psychiatry. 16 (2016) 442. doi: 10.1186/s12888-016-1168-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Ionic Framework. https://ionicframework.com/ (accessed October 25, 2018).
- [31].Need stress relief? Try the 4 A’s, Mayo Clinic; (n.d.). https://www.mayoclinic.org/healthy-lifestyle/stress-management/in-depth/stress-relief/art-20044476 (accessed October 11, 2019). [Google Scholar]
- [32].The Busy Lifestyle. 6 New Stress Statistics from around the World (It’s Time to Take It Easy), The Busy Lifestyle. (2018). https://thebusylifestyle.com/stress-statistics-worldwide/ (accessed October 11, 2019).
- [33].Cohen S, Kamarck T, and Mermelstein R, A Global Measure of Perceived Stress, Journal of Health and Social Behavior. 24 (1983) 385–396. doi: 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- [34].Zhang J, Johnson TR, Patel VL, Paige DL, and Kubose T, Using usability heuristics to evaluate patient safety of medical devices, Journal of Biomedical Informatics. 36 (2003) 23–30. doi: 10.1016/S1532-0464(03)00060-1 [DOI] [PubMed] [Google Scholar]
- [35].System Usability Scale (SUS). https://www.usability.gov/how-to-and-tools/methods/system-usability-scale.html (accessed November 15, 2018).
- [36].Prochaska JO, and Velicer WF. The transtheoretical model of health behavior change, Am J Health Promot. 12 (1997) 38–48. doi: 10.4278/0890-1171-12.1.38 [DOI] [PubMed] [Google Scholar]
- [37].Schwarze RA, and Luszczynska A, Social cognitive theory, in: Conner M, and Norman P (Eds.), Predicting Health Behaviour, 2nd edition, Open University Press, Maidenhead, 2005: pp. 127–169. [Google Scholar]
- [38].Hochbaum G, Rosenstock I, and Kegels S. Health Belief Model, United States Public Health Service, Washington D.C., 1952. [Google Scholar]
- [39].Glanz K, Rimer BK, and Viswanath K, eds., Health Behavior and Health Education: Theory, Research, and Practice, 4th edition, Jossey-Bass, San Francisco, 2008. [Google Scholar]


