The ankle-brachial index (ABI) is the standard diagnostic test for peripheral artery disease (PAD). This test uses a handheld Doppler ultrasound to measure the systolic blood pressure of the brachial artery in both arms and the posterior tibial and dorsalis pedis arteries in both ankles to generate a ratio for each leg. This test is safe, noninvasive, accurate, standardized, and uniformly agreed to be the first diagnostic test in the evaluation of a patient. Most clinicians order the ABI (CPT [Current Procsedure Terminology] code 93922) through a vascular laboratory to ensure reliable test results.
Medicare administrative contractors (MACs) are private healthcare insurers who manage the Medicare Part A and Part B (A/B) medical claims and durable medical equipment claims for Medicare fee-for-service beneficiaries for specific geographic jurisdictions. MACs serve as the primary contact between the Medicare fee-for-service program and healthcare providers. In this position, MACs exert extraordinary influence over coverage of services through the local coverage determination process with neither mandate nor incentive to coordinate services across locales. The issue of inconsistency is significant enough to have warranted an investigation from the Office of Inspector General. In this case, varying MAC reimbursement criteria for coverage of the ABI limits access and has led to adverse care variation.1 We believe that governance of Medicare benefit through this administrative structure prevents millions of patients with PAD from diagnosis and life- and limb-saving medical therapies.
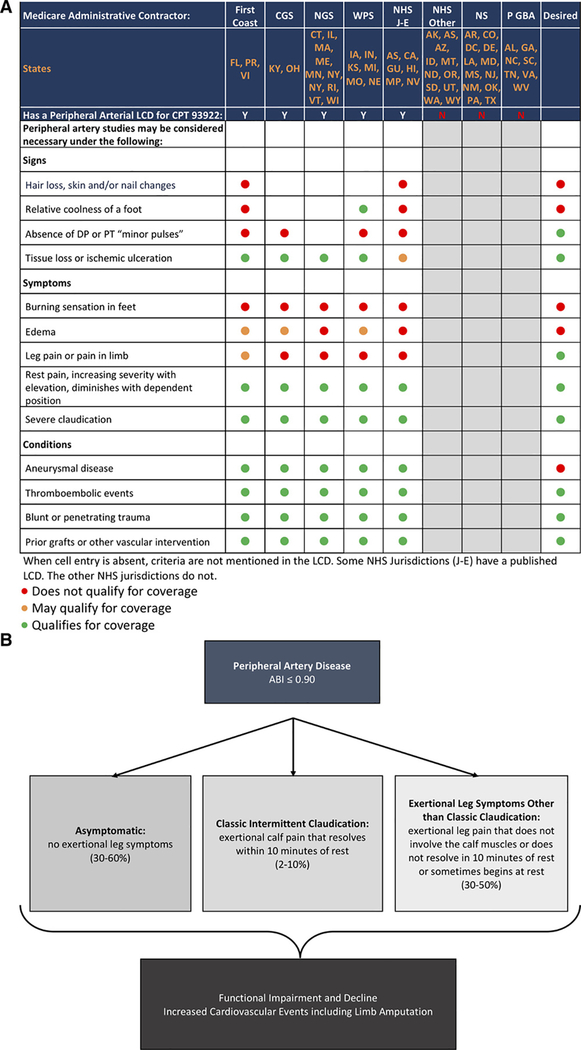
Currently, Centers for Medicare and Medicaid Services coverage for the ABI (CPT 93922) varies widely across the 7 MACs (Figure, panel A). CGS Administrators, First Coast Service Options, National Government Services, Wisconsin Physicians Services, and Noridian Healthcare Solutions Jurisdictions J-E provide limited coverage for the ABI, with significant indication variability. One particularly important indication—absence of pulses, a highly specific physical finding for PAD3—is not covered by any MAC. Noridian Healthcare Solutions other than Jurisdictions J-E, Novitas Solutions, and Palmetto GBA do not have a relevant local coverage determination, thus leaving clinicians in 30 states and territories without any guidance on Centers for Medicare and Medicaid Services ABI coverage.
Figure. Variation in coverage of ABI and clinical presentations of peripheral artery diseases.
A, Variation in coverage of the ABI by Medicare administrative contractor with the desired criteria listed. B, Peripheral artery disease presentation prevalence estimates from community-based cohorts and primary care practices.2 ABI indicates ankle-brachial index; CGS, CGS Administrators; CPT, Current Procedural Terminology; DP, dorsalis pedis; LCD, local coverage determination; N, no; NGS, National Government Services; NHS, Noridian Healthcare Solutions; NHS J-E, Noridian Healthcare Solutions, Jurisdictions J-E; NS, Novitas Solutions; P GBA, Palmetto GBA; PT, posterior tibial; WPS, Wisconsin Physician Service Government Health Administrators; and Y, yes.
Moreover, the criteria that both permit and deny access to this service do not reflect commonly recognized clinical signs and symptoms of PAD. For example, it is unclear why the diagnosis of aneurysm is a covered indication, but pain in the limb is not. This variability impairs efforts to encourage appropriate and guideline-recommended ABI use systematically across the nation, contributing to heterogeneity in rates of diagnosis, heterogeneity in intensity of treatment, and heterogeneity in outcomes.1
These limitations in Medicare coverage render millions of Americans with PAD unable to access inexpensive diagnostic testing when preventive therapies could have their greatest impact to reduce major cardiovascular events. Underuse of risk-reduction therapies is associated with worse outcomes, including high rates of heart attack, stroke, cardiovascular death, and limb loss. In fact, intensive medical therapy before an adverse cardiovascular event has occurred decreases the need for costly revascularization procedures, hospitalization for threatened limb loss, limb amputation, and the high costs of postdischarge rehabilitative services and prosthetic devices for patients presenting with untreated and advanced disease.4
Indications to be covered
We are very concerned that the absence of pedal pulses is not a covered indication for ABI testing. Worse, these pulses are termed “minor” by 2 of the MACs. The misunderstanding of the importance of these pulses and the strong relationship between their absence and the presence of PAD gravely undermines the MAC criteria. These pulses are not minor. The absence of pedal pulses is a strong predictor for morbidity and mortality. Absent pulses are significantly associated with an increase in risk of myocardial infarction, stroke, and death.5 Moreover, pulse examination strongly indicates the presence of PAD. In a prospective assessment of the pedal pulse examination as part of the Viborg Vascular Screening trial, 18 378 participants, aged 65 to 75 years, were screened using handheld Doppler ABI measurement, and 2215 were found to have PAD.3 The absence of any pulse (of the 4 in the ankles) was associated with a sensitivity of 71.7% and specificity of 72.3%. If all 4 pulses were present, there was a 5% false-negative rate.
Similarly, persons with severe and typical claudication symptoms (exertional calf pain that resolves within 10 minutes of rest) may undergo testing in most coverage areas having a local coverage determination. However, the majority of patients with PAD in the community or primary care setting do not have typical symptoms (Figure, panel B). Many are asymptomatic, reporting no exertional symptoms. Patients with PAD and leg symptoms other than typical claudication attribute their discomfort to more recognized conditions (eg, musculoskeletal disorders); thus, the diagnosis is often missed. As to prognosis, in a cohort of PAD patients identified consecutively at an outpatient vascular lab, two-thirds did not have typical intermittent claudication. When followed-up over 2 years for functional outcomes, an atypical presentation was associated with the greatest annual decline in walking capacity compared with other clinical presentations. With the exception of exertional leg symptoms that do not stop the individual while walking, all leg pain categories were associated with a 3- to 4-fold higher risk of becoming unable to complete 6 minutes of continuous walking.2 Thus, atypical exertion-limiting leg symptoms signal accelerated functional decline in those diagnosed with PAD and should permit diagnostic testing.
We believe that Medicare beneficiaries who have an abnormal physical examination, exertional leg symptoms, or evidence of critical limb ischemia (pain at rest, nonhealing ulcers, or gangrene) deserve and should be eligible for the ABI (CPT code 93922). To ensure that the appropriate Medicare beneficiaries have access to this standard diagnostic test, we believe that MACs must reconsider their current coverage policies. We further recommend that the MACs join together to develop one consistent coverage policy that will apply to all Medicare beneficiaries regardless of where they live. The policy should cover beneficiaries who have one of the clinical indications as outlined in the final column of the Figure (panel A).
References
- 1.Vemulapalli S, Greiner MA, Jones WS, Patel MR, Hernandez AF and Curtis LH 1. Vemulapalli S, Greiner MA, Jones WS, Patel MR, Hernandez AF, Curtis LH Peripheral arterial testing before lower extremity amputation among Medicare beneficiaries, 2000 to 2010. Circ Cardiovasc Qual Outcomes. 2014;7:142–150. doi: 10.1161/CIRCOUTCOMES.113.000376 [DOI] [PubMed] [Google Scholar]
- 2.McDermott MM. Lower extremity manifestations of peripheral artery disease: the pathophysiologic and functional implications of leg ischemia. Circ Res. 2015;116:1540–1550. doi: 10.1161/CIRCRESAHA.114.303517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Londero LS, Lindholt JS, Thomsen MD, Hoegh A Pulse palpation is an effective method for population-based screening to exclude peripheral arterial disease. J Vasc Surg. 2016;63:1305–1310. doi: 10.1016/j.jvs.2015.11.044 [DOI] [PubMed] [Google Scholar]
- 4.Lindholt JS, Søgaard R Population screening and intervention for vascular disease in Danish men (VIVA): a randomised controlled trial. Lancet. 2017;390:2256–2265. doi: 10.1016/S0140-6736(17)32250-X [DOI] [PubMed] [Google Scholar]
- 5.Ostergren J, Sleight P, Dagenais G, Danisa K, Bosch J, Qilong Y, Yusuf S; HOPE Study Investigators. Impact of ramipril in patients with evidence of clinical or subclinical peripheral arterial disease. Eur Heart J. 2004;25:17–24. doi: 10.1016/j.ehj.2003.10.033 [DOI] [PubMed] [Google Scholar]