Abstract
Purpose
To evaluate pooled prevalence, sensitivity, and specificity of chest computed tomography (CT) and radiographic findings for novel coronavirus-2019 (COVID-19) pneumonia.
Methods
We performed systematic literature search in PubMed and Embase to identify articles reporting baseline imaging findings of COVID-19 pneumonia. The quality of the articles was assessed using NIH quality assessment tool for case series studies. The pooled prevalence, sensitivity, specificity, and diagnostic odds ratio of imaging findings were calculated.
Results
Fifty-six studies (6007 patients, age, 2.1–70 years, 2887 females, 5762 CT, 396 radiographs,) were included. The mean interval between onset of symptoms and CT acquisition was 1–8 days. On CT, the pooled prevalence of ground glass opacities (GGO), GGO plus consolidation, and consolidation only was 66.9% (95% CI 60.8–72.4%), 44.9% (38.7–51.3%), and 32.1 (23.6–41.9%) respectively. Pooled sensitivity and specificity of GGO on CT was 73% (71%–80%) and 61% (41%–78%), respectively. For GGO plus consolidation and consolidation only, the pooled sensitivities/ specificities were 58% (48%–68%)/ 58% (41%–73%) and 49% (20%–78%)/ 56% (30%–78%), respectively. The pooled prevalence of GGO and consolidation on chest radiograph was 38.7% (22.2%–58.3%) and 46.9% (29.7%–64.9%), respectively. The diagnostic accuracy of radiographic findings could not be assessed due to small number of studies.
Conclusion
GGO on CT has the highest diagnostic performance for COVID-19 pneumonia, followed by GGO plus consolidation and consolidation only. However, the moderate to low sensitivity and specificity suggest that CT should not be used as the primary tool for diagnosis. Chest radiographic abnormalities are seen in half of the patients.
Abbreviations: COVID-19, novel coronavirus; CT, computed tomography; GGO, ground-glass opacity; RT-PCR, reverse transcriptase-polymerase chain reaction; AUC, area under the curve
Keywords: Covid-19, Imaging, Systematic review
1. Introduction
World Health Organization (WHO) declared coronavirus disease 2019 (COVID-19) a “public health emergency” at the end of January 2020.1 The disease is highly infectious, and the reported modes of spread are via aerosol and feco-oral route.2 The initial symptoms are indistinguishable from other viral diseases. Pneumonia is the most frequent presentation and manifests as fever, cough, dyspnea. Although most patients have mild disease with complete recovery, patients with advanced age and underlying co-morbidities have higher mortality.3 There are no specific clinical or radiological features reliably distinguishing COVID-19 from other viral infections of the respiratory system.4 The definitive diagnosis of COVID-19 disease is based on the analysis of the respiratory specimens (expectorated sputum, nasopharyngeal, oropharyngeal or nasal swabs and/or bronchoalveolar lavage) by the reverse transcriptase polymer chain reaction (RT-PCR).5 The detection rates vary from 32 to 93% according to the site and method of obtaining the specimen.5 Bronchoalveolar lavage fluid specimen has the highest positivity rates followed by sputum, and nasal swabs.5
Imaging is invaluable in the assessment of the COVID-19 patients. Standard frontal chest radiographs reveal ground-glass opacities (GGO) or consolidation.4 The most common CT finding is bilateral, peripheral GGO. Consolidation, combination of consolidation and GGO, and crazy paving pattern are the other commonly reported findings.6 , 7 The CT features of COVID-19 pneumonia depend on the duration of infection.8 , 9 CT may be normal in the early phase. The CT findings peak between 6 and 11 days and comprise mainly of GGO. Between 12 and 17 days, a mixed pattern of findings (GGO and consolidation) predominate. Majority of the patients have residual findings on CT at the time of discharge. Additionally, the CT findings may progress over time. In one study, worsening of GGO and progression to consolidation was reported in 85.7% of the patients.10 CT involvement scores, architectural distortion, and traction bronchiectasis may aid in evaluation of disease severity.7 Despite some reports of better diagnostic accuracy of chest CT compared with RT-PCR, the American College of Radiology (ACR) does not recommend the use of a CT chest for screening purposes.[11], [12], [13] CT scans can be efficiently utilized in a selected group of hospitalized COVID-19 patients to assess the extent, severity, and prognosis of the disease and to detect associated complications. The visual as well as quantitative maps of the affected lungs, may provide an objective assessment of the severity of involvement.
Most of the published systematic reviews on the imaging findings in COVID-19 comprise studies conducted in the early period of the disease outbreak.[14], [15], [16], [17] The quantitative analyses were limited to pooled prevalence estimates. The present systematic review and meta-analysis is aimed to evaluate the pooled prevalence and the diagnostic accuracy of individual imaging findings on chest CT scans and radiographs in patients with COVID-19 pneumonia.
2. Materials and methods
This meta-analysis complied with the Preferred Reporting Items for Systematic reviews and Meta-Analysis guidelines.18
2.1. Literature search
Two reviewers searched Pubmed and Embase and screened the titles and abstracts independently. The disagreement regarding the inclusion of a potential article was resolved in consensus. There was no language restriction for the search. The search was limited to the articles reporting COVID-19 infection only. The initial search was completed on 2nd April and again updated on 7th April 2020. The detailed search strategy is shown in Table 1 . Studies were first screened by examining their titles and abstracts. Their references were also checked for other relevant publications. The full texts of potentially eligible studies were retrieved for review.
Table 1.
Search strategy.
| S·no | Search term | Citations |
|---|---|---|
| PUBMED | ||
| 1 | ((((((((((Wuhan Coronavirus) OR (COVID 19 virus)) or (COVID-19 virus)) OR coronavirus disease 2019 virus)) OR SARS-CoV-2)) OR (SARS-2)) OR (2019-nCoV)) OR (2019 novel Coronavirus)) OR (Severe acute respiratory syndrome coronavirus 2)) OR (coronavirus)) OR (nCoV) | 16,438 |
| EMBASE | ||
| 2 | Wuhan AND coronavirus OR (covid19 AND virus) OR ‘covid 19’ OR (covid AND 19 AND virus) OR (coronavirus AND disease AND 2019 AND virus) OR (sars AND cov AND 2) OR sars2 OR (2019 AND ncov) OR ‘2019 novel coronavirus’ OR ‘severe acute respiratory syndrome coronavirus 2’ OR coronavirus OR ncov | 20,543 |
2.2. Inclusion and exclusion criteria
Criteria for inclusion of studies were as follows: (a) Confirmed COVID-19 based on positive RT-PCR on one of the respiratory specimens (b); Studies reporting the imaging findings in COVID-19 pneumonia on a baseline CT (c) the absolute numbers of patients with positive imaging findings should have been directly reported or was derivable and (d) more than ten patients should have been reported.
Review articles, case series (≤10), case reports, pictorial essays, letter to the editor (on already published papers), unpublished data, conference abstracts, and proceedings on the topic of interest were excluded.
2.3. Data extraction and quality assessment
The data was extracted on an excel sheet by two reviewers independently. The following details were obtained: type of study, country of origin, imaging modality (CT or chest radiograph); reference standard for diagnosis; patient demographic information (age, gender); numbers of true-positive (TP), true-negative (TN), false-positive (FP), and false-negative (FN); distribution of findings (central, peripheral, or both; unilateral or bilateral; upper lobe, middle or lower lobe); the interval from symptom onset to CT acquisition; the number of patients with normal CT scans; the number of patients with co-morbidities and number of patients requiring mechanical ventilation. The data entered by both the reviewers was matched, and any discrepancy was resolved after the re-evaluation of the paper in consensus.
Two reviewers assessed the methodologic and reporting quality of each study independently by using the NIH quality assessment tool for case series studies.19 This tool comprised nine questions. The responses to each of these questions were “yes”, “no” or others (cannot determine, CD; not reported, NR; or not applicable, NA). The overall assessment was “good”, “fair” or “poor”.
2.4. Statistical analysis
The statistical analysis was performed using R statistical software (version 3.6.1). In addition to the base package, the additional packages used include meta, mada, and readxl.[20], [21], [22], [23] The studies providing the number of patients with individual imaging findings and the total number of patients were summarized as pooled prevalence. Studies reporting the sensitivity as well as specificity were used to extract TP, TN, FP, and FN for evaluating pooled sensitivity, specificity, and diagnostic odds ratio. The meta-analysis was done using the inverse variance method with logit transformation along with the Clopper-Pearson confidence interval for individual studies. The pooling of the diagnostic odds ratio was also computed by the inverse variance method. The Forest plots were constructed for pooled prevalence, sensitivity, specificity, and diagnostic odds ratio. For the pooled analysis, heterogeneity was quantified using the I 2 test statistic, including 95% CI. The I 2 statistic reports the percentage of total variation across studies that is due to heterogeneity rather than chance. A value of I 2 statistic greater than 50% implies heterogeneity. Wilson method was used for the calculation of CI for both pooled analysis as well as the summary results. A bivariate diagnostic random-effect model was used for computing the combined sensitivity and specificity. For the computation of the bivariate model, a minimum of 4 studies was essential. Hierarchical summary receiver operating plot (hsROC) with 95% predictive and calculated region was plotted, and area under the curve (AUC) was determined.
3. Results
3.1. Literature search and article selection
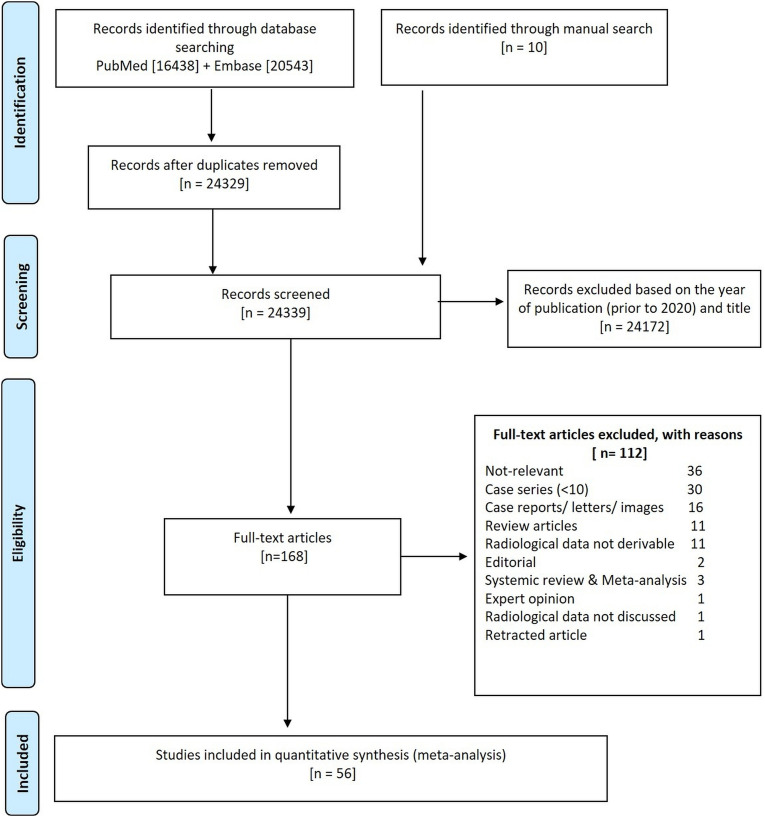
The study selection process is detailed in the flowchart (Fig. 1 ). The initial search yielded 16,438 articles in Pubmed and 20,543 articles in Embase. Manual restriction to articles reporting COVID-19 in 2020 resulted in 1136 articles in Pubmed and 1393 articles in Embase. After screening titles and abstracts, and removing duplicates, the full texts of 168 articles were reviewed. Finally, 56 articles were selected.[6], [7], [8], [9] , [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62], [63], [64], [65], [66], [67], [68], [69], [70], [71], [72], [73], [74] The details of these studies are given in Supplementary Table 1. There were four studies in the Chinese language. Most of the studies were from the Chinese population. Three studies were reported from the United States (n = 3) and one study each from Japan (n = 1) and Italy (n = 1).
Fig. 1.
Flowchart of study inclusion.
3.2. Quality assessment
The results of the quality assessment are presented in Supplementary Table 2. Most of the studies were rated as “fair” by both the reviewers.
3.3. Pooled prevalence of the imaging findings
There were 6007 patients, with 2910 (48.5%) males and 2887 (48.1%) females. In a few studies, the number of males and females was not specifically reported. However, as the rest of the data was complete, these studies were included for analysis. Baseline CT scans were performed in 5762 patients and chest radiographs in 282 patients. The information regarding the laterality of involvement was reported in 30 studies (3141 patients). Unilateral disease was reported in 286 (9.1%) CT scans and bilateral disease in 1358 (44%) CT scans. The preferential involvement of peripheral vs. central lung was reported in 31 studies (1960 patients). Central, peripheral, and central plus peripheral involvement was reported in 314 (16%), 1147 (58.5%), and 382 (19.4%) CT scans, respectively. The mean interval from the onset of symptoms to CT acquisition was 1–8 days. Co-morbidities were reported in 773 patients (29.9%), and 232 (15.6%) patients required mechanical ventilation.
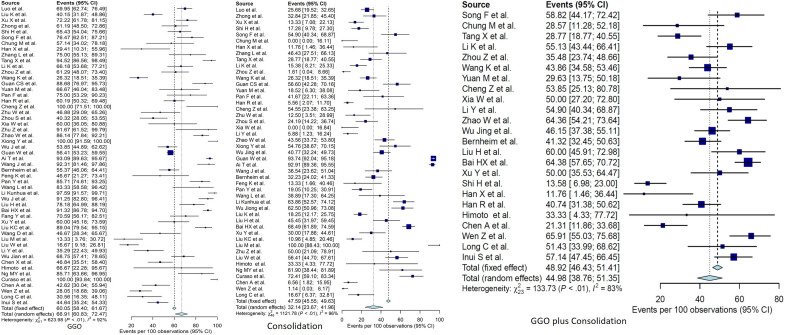
The pooled prevalence of GGO was 66.9% (95%CI 58.4–72.4%, I2 92%) (Fig. 2A), consolidation only was 32.1% (23.6–41.9%, I2 96%) (Fig. 2B), and GGO plus consolidation was 44.9% (38.7–51.3%, I2 83%) (Fig. 2C). The pooled prevalence of other CT abnormalities were 29.1% (19.6–40.8, I2 93%) for crazy paving, 23.6% (11.7–41.8, I2 93%) for halo sign, 8.9% (5.7–13.8, I2 65%) for nodules, 5.6% (4.2–7.4, I2 51%) for pleural effusion, and 2.7% (1.3–5.5, I2 84%) for lymphadenopathy (Supplementary Figs. 1 and 2).
Fig. 2.
Forest plots demonstrate the pooled prevalence of GGO, GGO plus consolidation and consolidation only on CT.
Findings of chest radiographs were reported by five studies comprising 396 patients. The pooled prevalence of GGO and consolidation was 38.7% (22.2%–58.3%, I2 83%) and 46.9% (29.7%– 64.9%, I2 84%), respectively (Supplementary Fig. 3). The diagnostic accuracy meta-analysis for radiographic abnormalities could not be conducted due to a limited number of studies.
3.4. Diagnostic performance evaluation of various imaging modalities
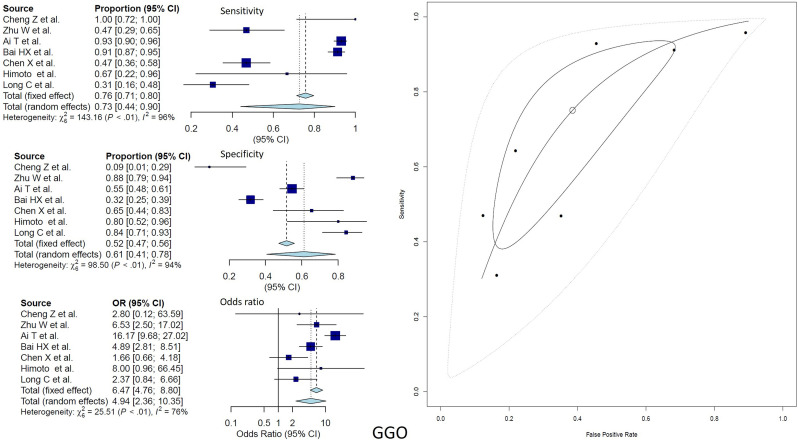
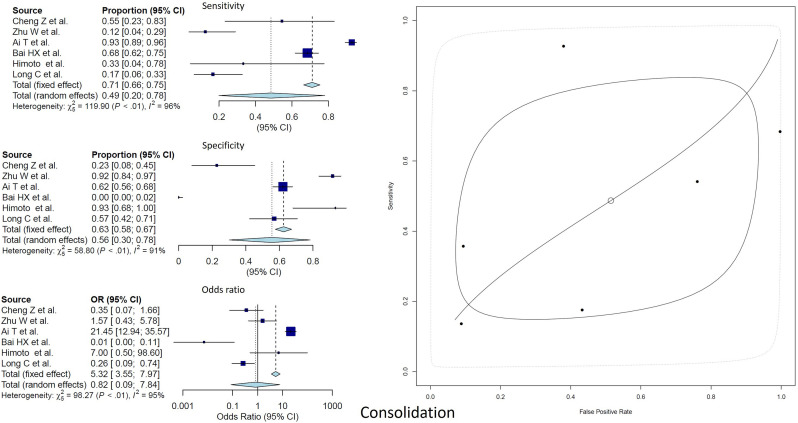
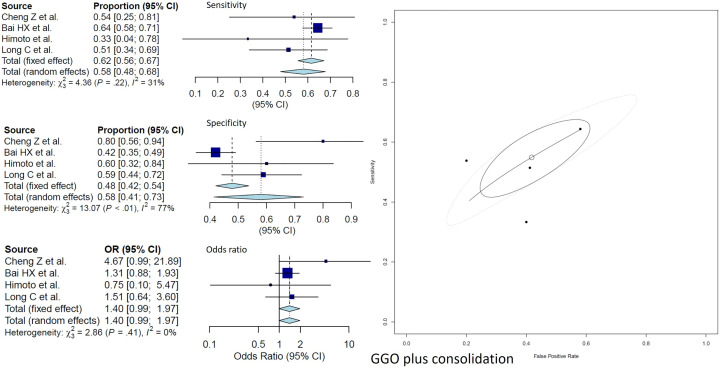
Pooled sensitivities and specificities of GGO on CT were 73% (71%–80%, I 2 96%) and 61% (41%–78%, I 2 94%) respectively. For GGO plus consolidation and consolidation only, the pooled sensitivities/ specificities were 58% (48%–68%, I2 31%)/ 58% (41%–73%, I 2 77%) and 49% (20%–78%, I 2 96%)/ 56% (30%–78%, I 2 91%), respectively. The pooled diagnostic odds ratio of GGO, GGO plus consolidation, and consolidation only was 4.97 (2.36–10.35), 1.4 (0.99–1.97), and 0.82 (0.09–7.84), respectively. AUC for GGO was 0.728 compared with 0.575 for GGO plus consolidation and 0.472 for consolidation only (Fig. 3, Fig. 4, Fig. 5 ). Table 2 shows the results of the pooled prevalence and diagnostic accuracy meta-analysis of CT findings. Table 3 shows the pooled prevalence of chest radiographic abnormalities.
Fig. 3.
Forest plots demonstrate the pooled sensitivity, specificity, diagnostic odds ratio and hsROC of GGO on CT.
Fig. 4.
Forest plots demonstrate the pooled sensitivity, specificity, diagnostic odds ratio and hsROC of GGO plus consolidation on CT.
Fig. 5.
Forest plots demonstrate the pooled sensitivity, specificity, diagnostic odds ratio and hsROC of consolidation only on CT.
Table 2.
Pooled prevalence and diagnostic accuracy estimates of imaging findings on CT.
| Findings | Pooled prevalence (95% CI) | I2 | Pooled sensitivity (95% CI) | I2 | Pooled specificity (95% CI) | I2 | Pooled DOR (95% CI) | I2 | AUC |
|---|---|---|---|---|---|---|---|---|---|
| CT chest | |||||||||
| GGO | 66.9% (60.8–72.4) | 92% | 73% (71–80) | 96% | 61% (41–78) | 94% | 4.97 (2.36–10.35) | 76% | 0.728 |
| GGO + Consolidation | 44.9% (38.7–51.3) | 83% | 58% (48–68) | 31% | 58% (41–73) | 77% | 1.4 (0.99–1.97) | 0.575 | |
| Consolidation only | 32.1% (23.6–41.9) | 96% | 49% (20–78) | 96% | 56% (30–78) | 91% | 0.82 (0.09–7.84) | 0.477 | |
| Crazy paving | 29.1% (19.6–40.8) | 93% | * | * | * | * | |||
| Halo sign | 23.6% (11.7–41.8) | 94% | * | * | * | * | |||
| Nodule | 8.9% (5.7–13.8) | 65% | * | * | * | * | |||
| Pleural effusion | 5.6% (4.2–7.4) | 51% | * | * | * | * | |||
| Lymphadenopathy | 2.7% (1.3–5.5) | 84% | * | * | * | * | |||
GGO: ground glass opacity; CI: confidence interval, DOR: diagnostic odds ratio, AUC: area under the curve, *-Diagnostic accuracy meta-analysis not performed due to limited number of studies reporting these findings.
Table 3.
Pooled prevalence of chest radiographic findings in COVID-19 pneumonia.
| Findings | Pooled prevalence (95% CI) | I2 |
|---|---|---|
| GGO | 38.7% (22.2–58.3) | 83% |
| Consolidation | 46.9% (29.7–64.9) | 84% |
GGO: ground glass opacity; CI: confidence interval.
4. Discussion
We reported a systematic review and meta-analysis of chest CT and radiographic findings in 5993 patients with COVID-19 pneumonia. We included 56 studies that reported the chest imaging findings at baseline. Besides evaluating the prevalence of various findings in COVID-19 pneumonia, we also conducted diagnostic accuracy meta-analysis for certain studies where the required data was available. We found that GGOs, GGO plus consolidation, and consolidation only were the frequent imaging findings in that order. The diagnostic odds ratio of GGO was the highest (4.97, 95% CI: 2.36–10.35) with the AUC of 0.728. Additionally, we found that on chest radiograph, consolidation was more frequently reported than GGOs (46.9%, 95% CI: 29.7–64.9% vs. 38.78%, 95% CI: 22.2–58.3). Pooled prevalence of nodules, halo sign, crazy-paving, lymphadenopathy, and pleural effusion was also reported. Sensitivity, specificity, and diagnostic odds ratio could not be evaluated due to the paucity of studies specifically reporting these findings.
A few previous systematic reviews and meta-analyses have investigated the imaging findings in COVID-19 pneumonia.[14], [15], [16], [17] In the meta-analysis by the Cao Y et al., the clinical and imaging findings from 31 studies were reported. Bilateral pneumonia was the most common finding.14 Among the specific imaging findings, GGOs was reported in 69.9% of the patients. The other commonly reported findings were “halo sign” (54.4%), air bronchogram (51.3%), bronchovascular bundle thickening (39.5%), grid form shadows (24.4%) and pleural effusion (18.5%). The bilateral findings were reported in 75.7% and unilateral findings in 23.4% of the included subjects. Some of the findings reported in this study e.g. grid form shadows and bronchovascular bundle thickening are not accepted as standard terminology and have not been recommended by the Radiological Society of North America expert consensus statement on reporting chest CT Findings related to COVID-19 [75].
In another systematic review and meta-analysis by Rodriguez-Morales et al., the imaging features were pooled from 10 studies.15 The only specific imaging finding in this study was GGO reported in 68.5%. Unilateral and bilateral lung involvement was reported in 25% and 72.9%, respectively. The pooled prevalence of GGOs (66.9%) in our study was similar to the study by Rodriguez-Morales et al. However, bilateral involvement was less frequent in our study. Similarly, “halo sign” and pleural effusion was less frequent compared to the study by Cao et al..14 This difference is due to a greater number of studies as well as the exclusion of case reports and smaller case series in our meta-analysis. Another systematic review comprising 999 patients with COVID-19 pneumonia included 30 articles, most (21/30) of which were either case reports or small case series (<10 subjects). The screened articles were restricted to the earlier phase of the pandemic and included studies published in English language only. The largest included series comprised 167 patients. Like the other studies, GGO in the bilateral peripheral distribution was the most common findings. GGOs were reported in 88% of the patients with bilateral and peripheral distribution in 87.5% and 76%, respectively. This study did not report other findings, and meta-analysis was not performed. In the meta-analysis by Xu B et al., data from 16 studies comprising 3186 patients was included.18 The authors reported the overall diagnostic accuracy of CT rather than the individual CT findings. The pooled sensitivity of CT was reported to be 92% while the pooled specificity was reported for only two studies (33% and 25%).18
Our study is the one of the most updated and recent meta-analysis, including the studies published in English as well as non-English literature. We reported most of the findings recommended by the Radiological Society of North America in the context of COVID-19 pneumonia.75 We purposely excluded the case reports and smaller case series (<10 subjects) to avoid misinterpretation of the data.
There were a few limitations to our study. First, we evaluated the findings of only the baseline CT scan and chest radiograph, and so could not assess the pattern of disease progression. However, the inclusion of a baseline CT scan matches well with the primary aim of our meta-analysis. Second, most of the studies were retrospective and included patients with varying degrees of disease severity. Thus, the results of our meta-analysis need to be reviewed carefully. Prospective and systematically conducted studies will strengthen our observations. However, considering the pandemic nature and global impact of this highly infectious viral disease, we believe that our results are timely and highly relevant despite these limitations.
Financial disclosure
None.
Declaration of competing interest
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.clinimag.2020.11.021.
Appendix A. Supplementary data
Supplementary material
References
- 1.World Health Organization Director-General's remarks at the media briefing on 2019-nCoV on 11 February 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020 (Accessed on February 12, 2020)
- 2.Centers for Disease Control and Prevention Interim guidelines for collecting, handling, and testing clinical specimens from persons under investigation (PUIs) for coronavirus disease 2019 (COVID-19). February 14, 2020. https://www.cdc.gov/coronavirus/2019-nCoV/lab/guidelines-clinical-specimens.html
- 3.van Doremalen N., Bushmaker T., Morris D.H. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382(16):1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen N., Zhou M., Dong X. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang W., Xu Y., Gao R. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020;323(18):1843–1844. doi: 10.1001/jama.2020.3786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shi H., Han X., Jiang N. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20(4):425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhao W., Zhong Z., Xie X., Yu Q., Liu J. Relation between chest CT findings and clinical conditions of coronavirus disease (COVID-19) pneumonia: a multicenter study. AJR Am J Roentgenol. 2020;214(5):1072–1077. doi: 10.2214/AJR.20.22976. [DOI] [PubMed] [Google Scholar]
- 8.Wang Y., Dong C., Hu Y. Temporal changes of CT findings in 90 patients with COVID-19 pneumonia: a longitudinal study. Radiology. 2020;296(2):E55–E64. doi: 10.1148/radiol.2020200843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bernheim A., Mei X., Huang M. Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology. 2020;295(3):200463. doi: 10.1148/radiol.2020200463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pan Y., Guan H., Zhou S. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): a study of 63 patients in Wuhan, China. Eur Radiol. 2020;30(6):3306–3309. doi: 10.1007/s00330-020-06731-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ai T., Yang Z., Hou H. Correlation of chest CT and RT-PCR testing for coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020;296(2):E32–E40. doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huang P., Liu T., Huang L. Use of chest CT in combination with negative RT-PCR assay for the 2019 novel coronavirus but high clinical suspicion. Radiology. 2020;295(1):22–23. doi: 10.1148/radiol.2020200330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.ACR Recommendations for the use of chest radiography and computed tomography (CT) for suspected COVID-19 infection. https://www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection
- 14.Cao Y., Liu X., Xiong L., Cai K. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2: a systematic review and meta. J Med Virol. 2020 doi: 10.1002/jmv.25822. (10.1002/jmv.25822) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rodriguez-Morales A.J., Cardona-Ospina J.A., Gutiérrez-Ocampo E. Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Travel Med Infect Dis. 2020;34:101623. doi: 10.1016/j.tmaid.2020.101623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Salehi S., Abedi A., Balakrishnan S., Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19): a systematic review of imaging findings in 919 patients. AJR Am J Roentgenol. 2020;215(1):87–93. doi: 10.2214/AJR.20.23034. [DOI] [PubMed] [Google Scholar]
- 17.Xu B., Xing Y., Peng J. Chest CT for detecting COVID-19: a systematic review and meta-analysis of diagnostic accuracy. Eur Radiol. 2020:1–8. doi: 10.1007/s00330-020-06934-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McInnes M.D.F., Moher D., Thombs B.D., McGrath T.A., Bossuyt P.M., the PRISMA-DTA Group Preferred reporting items for a systematic review and meta-analysis of diagnostic test accuracy studies: the PRISMA-DTA statement. JAMA. 2018;319(4):388–396. doi: 10.1001/jama.2017.19163. [DOI] [PubMed] [Google Scholar]
- 19.National Heart, Lung, and Blood Institute website Study quality assessment tools. www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (Accessed April 4, 2020)
- 20.R Core Team . R Foundation for Statistical Computing; Vienna, Austria: 2019. R: A language and environment for statistical computing.https://www.R-project.org/ URL. [Google Scholar]
- 21.Schwarzer G. meta: An R package for meta-analysis. R News. 2007;7(3):40–45. [Google Scholar]
- 22.Doebler P. Mada: Meta-analysis of diagnostic accuracy. R package version 0.5.9. 2019. https://CRAN.R-project.org/package=mada
- 23.Wickham H., Bryan J. readxl: read excel files. R package version 1.3.1. 2019. https://CRAN.R-project.org/package=readxl
- 24.Luo S., Zhang X., Xu H. Don’t overlook digestive symptoms in patients with 2019 novel coronavirus disease (COVID-19) Clin Gastroenterol Hepatol. 2020;18(7):1636–1637. doi: 10.1016/j.cgh.2020.03.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu K., Fang Y.Y., Deng Y. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chin Med J (Engl) 2020;133(9):1025–1031. doi: 10.1097/CM9.0000000000000744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Xu X., Yu C., Qu J. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2. Eur J Nucl Med Mol Imaging. 2020;47(5):1275–1280. doi: 10.1007/s00259-020-04735-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhong Q., Li Z., Shen X. Zhejiang Da Xue Xue Bao Yi Xue Ban. 2020;49(2):198–202. doi: 10.3785/j.issn.1008-9292.2020.03.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Song F., Shi N., Shan F. Emerging 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology. 2020;295(1):210–217. doi: 10.1148/radiol.2020200274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chung M., Bernheim A., Mei X. CT imaging features of 2019 novel coronavirus (2019-nCoV) Radiology. 2020;295(1):202–207. doi: 10.1148/radiol.2020200230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Han X., Cao Y., Jiang N. Novel coronavirus disease 2019 (COVID-19) pneumonia progression course in 17 discharged patients: comparison of clinical and thin-section computed tomography features during recovery. Clin Infect Dis. 2020;71(15):723–731. doi: 10.1093/cid/ciaa271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang L., Zhu F., Xie L. Clinical characteristics of COVID-19-infected cancer patients: a retrospective case study in three hospitals within Wuhan, China. Ann Oncol. 2020;31(7):894–901. doi: 10.1016/j.annonc.2020.03.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tang X., Du R.H., Wang R. Comparison of hospitalized patients with ARDS caused by COVID-19 and H1N1. Chest. 2020;158(1):195–205. doi: 10.1016/j.chest.2020.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li K., Fang Y., Li W. CT image visual quantitative evaluation and clinical classification of coronavirus disease (COVID-19) Eur Radiol. 2020;30(8):4407–4416. doi: 10.1007/s00330-020-06817-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhou Z., Guo D., Li C. Coronavirus disease 2019: initial chest CT findings. Eur Radiol. 2020;30(8):4398–4406. doi: 10.1007/s00330-020-06816-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang K., Kang S., Tian R., Zhang X., Zhang X., Wang Y. Imaging manifestations and diagnostic value of chest CT of coronavirus disease 2019 (COVID-19) in the Xiaogan area. Clin Radiol. 2020;75(5):341–347. doi: 10.1016/j.crad.2020.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Guan C.S., Lv Z.B., Yan S. Imaging features of coronavirus disease 2019 (COVID-19): evaluation on thin-section CT. Acad Radiol. 2020;27(5):609–613. doi: 10.1016/j.acra.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yuan M., Yin W., Tao Z., Tan W., Hu Y. Association of radiologic findings with mortality of patients infected with 2019 novel coronavirus in Wuhan, China. PLoS One. 2020;15(3):e0230548. doi: 10.1371/journal.pone.0230548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pan F., Ye T., Sun P. Time course of lung changes at chest CT during recovery from coronavirus disease 2019 (COVID-19) Radiology. 2020;295(3):715–721. doi: 10.1148/radiol.2020200370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Han R., Huang L., Jiang H., Dong J., Peng H., Zhang D. Early clinical and CT manifestations of coronavirus disease 2019 (COVID-19) pneumonia. AJR Am J Roentgenol. 2020;215(2):338–343. doi: 10.2214/AJR.20.22961. [DOI] [PubMed] [Google Scholar]
- 40.Cheng Z., Lu Y., Cao Q. Clinical features and chest CT manifestations of coronavirus disease 2019 (COVID-19) in a single-center study in Shanghai, China. AJR Am J Roentgenol. 2020;215(1):121–126. doi: 10.2214/AJR.20.22959. [DOI] [PubMed] [Google Scholar]
- 41.Zhu W., Xie K., Lu H., Xu L., Zhou S., Fang S. Initial clinical features of suspected coronavirus disease 2019 in two emergency departments outside of Hubei, China. J Med Virol. 2020 doi: 10.1002/jmv.25763. (10.1002/jmv.25763) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhou S., Wang Y., Zhu T., Xia L. CT features of coronavirus disease 2019 (COVID-19) pneumonia in 62 patients in Wuhan, China. AJR Am J Roentgenol. 2020;214(6):1287–1294. doi: 10.2214/AJR.20.22975. [DOI] [PubMed] [Google Scholar]
- 43.Xia W., Shao J., Guo Y., Peng X., Li Z., Hu D. Clinical and CT features in pediatric patients with COVID-19 infection: different points from adults. Pediatr Pulmonol. 2020;55(5):1169–1174. doi: 10.1002/ppul.24718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhu Z.W., Tang J.J., Chai X.P. Zhonghua Xin Xue Guan Bing Za Zhi. 2020;48(0):E007. doi: 10.3760/cma.j.cn112148-20200218-00093. [DOI] [Google Scholar]
- 45.Xiong Y., Sun D., Liu Y. Clinical and high-resolution CT features of the COVID-19 infection: comparison of the initial and follow-up changes. Invest Radiol. 2020;55(6):332–339. doi: 10.1097/RLI.0000000000000674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wu J., Feng L.C., Xian X.Y. Novel coronavirus pneumonia (COVID-19) CT distribution and sign features. Zhonghua Jie He He Hu Xi Za Zhi. 2020;43(4):321–326. doi: 10.3760/cma.j.cn112147-20200217-00106. [DOI] [PubMed] [Google Scholar]
- 47.Guan W.J., Ni Z.Y., Hu Y. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang J., Liu J., Wang Y. Dynamic changes of chest CT imaging in patients with corona virus disease-19 (COVID-19) Zhejiang Da Xue Xue Bao Yi Xue Ban. 2020;49(2):191–197. doi: 10.3785/j.issn.1008-9292.2020.02.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Feng K., Yun Y.X., Wang X.F. Analysis of CT features of 15 children with 2019 novel coronavirus infection. Zhonghua Er Ke Za Zhi. 2020;58(4):275–278. doi: 10.3760/cma.j.cn112140-20200210-00071. [DOI] [PubMed] [Google Scholar]
- 50.Wang L., Gao Y.H., Lou L.L., Zhang G.J. The clinical dynamics of 18 cases of COVID-19 outside of Wuhan, China. Eur Respir J. 2020;55(4):2000398. doi: 10.1183/13993003.00398-2020. (Published 2020 Apr 23) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Li K., Wu J., Wu F. The clinical and chest CT features associated with severe and critical COVID-19 pneumonia. Invest Radiol. 2020;55(6):327–331. doi: 10.1097/RLI.0000000000000672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wu J., Wu X., Zeng W. Chest CT findings in patients with coronavirus disease 2019 and its relationship with clinical features. Invest Radiol. 2020;55(5):257–261. doi: 10.1097/RLI.0000000000000670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Liu H., Liu F., Li J., Zhang T., Wang D., Lan W. Clinical and CT imaging features of the COVID-19 pneumonia: focus on pregnant women and children. J Infect. 2020;80(5):e7–e13. doi: 10.1016/j.jinf.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bai H.X., Hsieh B., Xiong Z. Performance of radiologists in differentiating COVID-19 from non-COVID-19 viral pneumonia at chest CT. Radiology. 2020;296(2):E46–E54. doi: 10.1148/radiol.2020200823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fang Y., Zhang H., Xie J. Sensitivity of chest CT for COVID-19: comparison to RT-PCR. Radiology. 2020;296(2):E115–E117. doi: 10.1148/radiol.2020200432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Xu Y.H., Dong J.H., An W.M. Clinical and computed tomographic imaging features of novel coronavirus pneumonia caused by SARS-CoV-2. J Infect. 2020;80(4):394–400. doi: 10.1016/j.jinf.2020.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Liu K.C., Xu P., Lv W.F. CT manifestations of coronavirus disease-2019: a retrospective analysis of 73 cases by disease severity. Eur J Radiol. 2020;126:108941. doi: 10.1016/j.ejrad.2020.108941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wang D., Hu B., Hu C. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Liu M., He P., Liu H.G. Clinical characteristics of 30 medical workers infected with new coronavirus pneumonia. Zhonghua Jie He He Hu Xi Za Zhi. 2020;43(3):209–214. doi: 10.3760/cma.j.issn.1001-0939.2020.03.014. [DOI] [PubMed] [Google Scholar]
- 60.Liu W., Tao Z.W., Wang L. Analysis of factors associated with disease outcomes in hospitalized patients with 2019 novel coronavirus disease. Chin Med J (Engl) 2020;133(9):1032–1038. doi: 10.1097/CM9.0000000000000775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Li Y., Xia L. Coronavirus disease 2019 (COVID-19): role of chest CT in diagnosis and management. AJR Am J Roentgenol. 2020;214(6):1280–1286. doi: 10.2214/AJR.20.22954. [DOI] [PubMed] [Google Scholar]
- 62.Wu J., Liu J., Zhao X. Clinical characteristics of imported cases of coronavirus disease 2019 (COVID-19) in Jiangsu Province: a multicenter descriptive study. Clin Infect Dis. 2020;71(15):706–712. doi: 10.1093/cid/ciaa199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Chen X., Yang Y., Huang M. Differences between COVID-19 and suspected then confirmed SARS-CoV-2-negative pneumonia: a retrospective study from a single center [published online ahead of print, 2020 Apr 1] J Med Virol. 2020 doi: 10.1002/jmv.25810. (10.1002/jmv.25810) [DOI] [PubMed] [Google Scholar]
- 64.Himoto Y., Sakata A., Kirita M. Diagnostic performance of chest CT to differentiate COVID-19 pneumonia in non-high-epidemic area in Japan. Jpn J Radiol. 2020;38(5):400–406. doi: 10.1007/s11604-020-00958-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ng M.Y., Lee E., Yang J. Imaging profile of the COVID-19 infection: radiologic findings and literature review. Radiol Cardiothorac Imaging. 2020;2(1) doi: 10.1148/ryct.2020200034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Su L., Ma X., Yu H. The different clinical characteristics of corona virus disease cases between children and their families in China - the character of children with COVID-19. Emerg Microbes Infect. 2020;9(1):707–713. doi: 10.1080/22221751.2020.1744483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Caruso D., Zerunian M., Polici M. Chest CT features of COVID-19 in Rome, Italy. Radiology. 2020;296(2):E79–E85. doi: 10.1148/radiol.2020201237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chen A., Huang J., Liao Y. Differences in clinical and imaging presentation of pediatric patients with COVID-19 in comparison with adults. Radiol Cardiothorac Imaging. 2020 doi: 10.1148/ryct.2020200117. (Published online on Apr 6 2020) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wen Z., Chi Y., Zhang L. Coronavirus disease 2019: initial detection on chest CT in a retrospective multicenter study of 103 Chinese subjects. Radiol Cardiothorac Imaging. 2020 doi: 10.1148/ryct.2020200092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Long C., Xu H., Shen Q. Diagnosis of the coronavirus disease (COVID-19): rRT-PCR or CT? Eur J Radiol. 2020;126:108961. doi: 10.1016/j.ejrad.2020.108961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Inui S., Fujikwa A., Jitsu M. Chest CT findings in cases from the cruise ship “diamond princess” with coronavirus disease 2019 9COVID-2019. Radiol Cardiothorac Imaging. 2020 doi: 10.1148/ryct.2020200110. (Published Online:Mar 17 2020) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wong H.Y.F., Lam H.Y.S., Fong A.H. Frequency and distribution of chest radiographic findings in patients positive for COVID-19. Radiology. 2020;296(2):E72–E78. doi: 10.1148/radiol.2020201160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bhatraju P.K., Ghassemieh B.J., Nichols M. Covid-19 in critically ill patients in the Seattle region - case series. N Engl J Med. 2020;382(21):2012–2022. doi: 10.1056/NEJMoa2004500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Arentz M., Yim E., Klaff L. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington state [published online ahead of print, 2020 mar 19] JAMA. 2020;323(16):1612–1614. doi: 10.1001/jama.2020.4326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Simpson S., Kay F.U., Abbara A. Radiological Society of North America expert consensus statement on reporting chest CT findings related to COVID-19. Endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA. Radiol Cardiothorac Imaging. 2020 doi: 10.1148/ryct.2020200152. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material