Abstract
Since the Coronavirus disease 2019 (COVID-19) pandemic, caused by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) was announced, we had an unprecedented change in the way we organize ourselves socially and in our daily routine. Children and adolescents were also greatly impacted by the abrupt withdrawal from school, social life and outdoor activities. Some of them also experienced domestic violence growing. The stress they are subjected to directly impacts their mental health on account of increased anxiety, changes in their diets and in school dynamics, fear or even failing to scale the problem. Our aim is to bring up a discussion under different aspects and to alert public health and government agents about the need for surveillance and care of these individuals. We hope that the damage to their mental health as a result of the side effect of this pandemic can be mitigated by adequate and timely intervention.
Keywords: COVID-19, Children, Adolescents, Mental health, Social isolation, Stress
Highlights
-
•
COVID-19 has a multifactorial impact on children and adolescents populations.
-
•
Stressors of COVID-19 pandemic can trigger neuroinflammation and behavioral impairments.
-
•
Social isolation stress can induce neuroimmunoendocrine changes during early life.
-
•
The pandemic stressors early in life may lead to neuropsychiatric outcomes in adulthood.
-
•
Health policies to mitigate mental health outcomes of COVID-19 must be implemented.
1. Introduction
The world has been changing at a dizzying speed since Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), the virus that causes coronavirus disease 2019 (COVID-19), promoted a drastic and sudden change in the way we organize ourselves as social human beings. In March 2020, WHO declared that COVID-19 reached a pandemic status, putting the planet in a state of maximum alert and grew to dimensions that still cannot be measured today (World Health Organization (WHO), 2020a).
The literature has pointed out that older individuals are more susceptible to develop COVID-19, and those with major comorbidities such as diabetes, hypertension and obesity can be more affected and could potentially be at higher risk for severe illness and death (Shahid et al., 2020). Although children apparently present a lower risk of developing the severe form of the disease as well as less hospital care and mechanical ventilation, they can develop a multisystemic inflammatory syndrome (Jones et al., 2020; Harahsheh et al., 2020; She et al., 2020). Recently, some studies have pointed out that some children and adolescents infected with the newly discovered coronavirus developed skin lesions and a picture of Kawasaki syndrome. This unusual syndrome, initially identified in Japan (1967), is a vasculitis caused by a hyperinflammatory state (Jones et al., 2020; Harahsheh et al., 2020; She et al., 2020).
Although youngsters appear to be less vulnerable to COVID-19, the side effects of the pandemic can be devastating. Children and adolescents may be highly exposed to biopsychosocial stressors generated by the pandemic and once population's containment measures to reduce virus spread are required, they could be potentially affected by the disruption in daily life routine as a result of social isolation and their unseasoned ability to conceive and comprehend the short- and long-term consequences of this outbreak (Spinelli et al., 2020; Crescentini et al., 2020).
Commonly, although children and adolescents have experienced a drastic routine disruption due to the closure of schools and the absence of outdoor activities, they may not be completely isolated. In most cases, parents are at home. In this case, some youngsters may not necessarily experience an evident feeling of loneliness, as they may compensate for this by spending more time with their family members and also increasing time spent with social media and the internet (Guessoum et al., 2020; Keles et al., 2020). However, this situation also brings up some concerns. It was already observed that children with parents diagnosed with some psychiatric disturbance are more susceptible to developing psychopathologies (Maciejewski et al., 2018). In the context of the ongoing COVID-19 pandemic, most parents had to reorganize their lives to deal with working at home in addition to children's management. As a result, this sudden overload has been putting parents under extra stressful conditions, potentially increasing the risk of children face emotional and behavioral problems (Crescentini et al., 2020).
This particular moment we are facing is an unprecedented global situation with numerous idiosyncratic factors. People are being affected in multifaceted ways, having their physical, psychological and emotional well-being compromised, along with social and economic problems (Esterwood and Saeed, 2020). The heterogeneity and plurality of biopsychosocial stressors bring a multifactorial approach to the COVID-19 pandemic, which leads to unpredictable consequences on the mental health of vulnerable populations such as children and adolescents.
Recently, a study has evaluated 1036 quarantined children and adolescents in China in an age range from 6 up to 15 years, of which 112, 196, and 68 presented depression, anxiety, and both, respectively (Chen et al., 2020). Another study demonstrated a high prevalence of psychological distress in quarantined children and adolescents due to the COVID-19 pandemic in India. These individuals have experienced helplessness (66.11%), worry (68.59%) and fear (61.98%), compared to non-quarantined children (Saurabh and Ranjan, 2020). Moreover, it was also reported in China that children and adolescents aged 3–18 years presented symptoms of inattention, clinging, worry and irritability during this pandemic (Jiao et al., 2020).
Accordingly, in light of a large body of literature that unveiled several mechanisms behind the potential harms on brain development and/or behavioral outcomes result from different stressors during childhood and adolescence, we proposed herein a reflexive discussion addressing the following issues: (i) Stress and neuroinflammation; (ii) Social isolation and diet; (iii) Brain plasticity: social behavior; social inequalities, neglect and distress; playing and nature environment; and (iv) Public health and support, to shed light on points that should be considered by governments and health authorities to start a follow-up on the young population. It is the nature of human beings to be social and, despite the need for these restraint measures, it should be of great concern how this pandemic period can affect the young brain that is under development and it is more susceptible to stressors. Therefore, the search for strategies to mitigate a harmful long-term impact on it should be sought. These points will bring us information and guide us, in the future, if we have to face another situation like this COVID-19 pandemic.
2. Stress and neuroinflammation
Stress is usually approached under medical or biological aspects. It causes physiological damages or psychological disturbances to an organism and is generated by external or internal adverse stimuli (Gunnar and Quevedo, 2007). The adequate body response to stress helps to preserve and achieve an allostasis condition (Gunnar and Quevedo, 2007). However, uncontrolled or chronic responses to stress may have health harmful effects. There is already evidence of the multiple and negative psychological impacts of COVID-19 pandemic on children and adolescents quarantined populations (social isolation stressors) (Gunnar and Quevedo, 2007; Chen et al., 2020; Saurabh and Ranjan, 2020; Fegert et al., 2020), turning these individuals more susceptible to develop long-term psychiatric disorders. Although it is still under speculation the extent of the damages caused by the stressors of COVID-19 pandemic, it was recently proposed that dysregulated neuroendocrine-immune interactions can be behind psychiatric manifestations observed in quarantined people (Raony et al., 2020).
Under normal acute stress stimuli, the hypothalamic-pituitary-adrenal (HPA) axis activation leads to a release of glucocorticoids (e.g. cortisol) on the bloodstream that regulates the levels of pro- and anti-inflammatory molecules, which, in turn, also controls the secretion of these hormones by the HPA pathway, a mechanism of negative feedback that prevents an exacerbated inflammatory response (Del Rey and Besedovsky, 2017; Hänsel et al., 2010). However, persistent and enhanced stressful events during early life (childhood and adolescence) can drive responses by the immune, endocrine and nervous systems mainly through a dysfunction of the HPA axis (Dahmen et al., 2018; Juruena et al., 2020) and alterations on inflammatory mediators levels in the brain (Brenhouse and Schwarz, 2016), and/or systemically (Jiang et al., 2018), predisposing these individuals to psychopathological conditions in adulthood (e.g. anxiety and depression). Moreover, the stress can be one of the possible triggers for neuroinflammation, a term used to designate an imbalance or exacerbation of the immune signaling in the brain (Jiang et al., 2018) that can lead to several disorders (e.g. aggressive, psychosis, depression, and anxiety disorders) (Calcia et al., 2016; Ibi et al., 2008; Veenema, 2009).
During infancy, early childhood or even in adolescence, the central nervous system (CNS) is in a vulnerable developmental window, in which the occurrence of any stressful challenges at the time of critical periods can trigger short- and long-term physiological (Danese et al., 2009; Gunnar and Quevedo, 2007), cognitive and behavioral damages (Danese et al., 2009; Ibi et al., 2008; Nugent et al., 2011). The main brain regions that respond to environmental stimuli (e.g. stress) are amygdala, hippocampus, and prefrontal cortex. The response occurs via an intricate network of hormonal, immune and neurotransmitter responses, which can, in turn, change the response patterns of glial cells and monoamines metabolism, leading to cell death and/or mental health disturbances (Calcia et al., 2016; Danese et al., 2009).
Longitudinal studies have significantly correlated the presence of psychosocial stressors such as social isolation during childhood and adolescence with high levels of C-reactive protein (an inflammatory biomarker) later in life (Danese et al., 2009; Lacey et al., 2014). Moreover, Danese et al. (2009) also positively associated social isolation in childhood as a risk factor for depression in adult life (Danese et al., 2009). Since dysfunctional systemic inflammation has been extensively demonstrated to impair the neurodevelopmental processes and lead to cognitive and mood disturbances (Jiang et al., 2018), it seems reasonable that inflammatory alterations in children exposed to the harmful effects of COVID-19 outbreak could lead to long-term physiological and psychological damages and should be a public health concern.
Another important concern comes from the impact of fear in children and adolescents. A recent study reported a high prevalence of fear in quarantined children and adolescents during COVID-19 pandemic, a feeling that was mainly associated with financial worries or concerns regarding being exposed to COVID-19 or having infected others (Saurabh and Ranjan, 2020). Moreover, it is not surprising that adolescence represents a stress-sensitive developmental window relative to fear regulation (Tottenham and Galvan, 2016). Indeed, there is evidence showing chronic stress have a great impact on amygdala-prefrontal cortex connectivity and activity, impairing, for instance, the extinction of fear memory (Tottenham and Galvan, 2016). These questions claim for further studies addressing the harmful fear effects on the developing brain in the context of the COVID-19 pandemic.
3. Social isolation and diet: From animals to humans
The chronic stress caused by social isolation conditions in mice is also associated with an increased motivation to consume palatable foods (Sumis et al., 2016). In this context, studies using animal models suggest that intake of caloric foods can act as “comfort food” and would be an alternative to alleviate the negative effects of stress (Pecoraro et al., 2004; Ulrich-Lai et al., 2010). Chronic high-fat diet, induced by social isolation stress, reduces anxiety- and depression-like behaviors in animal models (Ulrich-Lai et al., 2010; Finger et al., 2011) and in humans (Tomiyama et al., 2011). Moreover, it was rescued the memory impairment on the object recognition test as well as the changes in brain-derived neurotrophic factor levels caused by social isolation conditions in rats (Arcego et al., 2016; Cavaliere et al., 2019).
Social isolation stress can induce an increased food intake and weight gain both in animal models (Krolow et al., 2013) and in humans (Mengin et al., 2020), and can be associated with increased hypothalamic production of neuropeptide Y (Kuo et al., 2007). Indeed, neuropeptide Y is involved with appetite control and insulin resistance in the brain (Kuo et al., 2007). Accordingly, the relationship between a stressful environment and the consequent increase in the search for such types of food early in life may be one of the reasons for an increase in obesity among children and young people (Ogden et al., 2016). In addition to obesity, access to both high-fat diets during development and social isolation can lead to structural synaptic changes (Cavaliere et al., 2019), impacting cognitive processes in adult life such as learning and memory in rodents (Granholm et al., 2008; Valladolid-Acebes et al., 2011) as well as in humans (Francis and Stevenson, 2011).
Furthermore, it has been shown that a short period of social isolation during adolescence is able to induce long-term effects on dopaminergic pathways in rats (Lampert et al., 2017). However, a high-fat diet has controversial results on the dopaminergic pathways due, in part, to different dietary lipid compositions. While administering a high- fat diet composed of saturated fatty acids leads to perturbations in mesolimbic dopaminergic signaling, a diet composed of unsaturated fatty acid does not (Barnes et al., 2020; Hryhorczuk et al., 2016).
A possible relationship between social isolation stress during childhood and access to high-fat diets may involve the activation of the HPA axis. In this sense, the leptin released by this type of diet can reduce the activation of the HPA axis (Bonnavion et al., 2015) and inhibit the hypothalamic neuropeptide Y synthesis and release (Stephens et al., 1995) triggered by stress, minimizing the effects of social isolation. However, the way, the duration and the localization in the brain of the effects of how caloric food intake acts to counteract stress effects in the brain deserve further investigation. In addition, the intake of highly caloric foods and the exposure to a social stressor can also affect the composition of the intestinal microbiota (Galley et al., 2014; Deshpande et al., 2019) leading to changes in the brain, since metabolic products of the intestinal microbiota can influence brain functions (and vice versa) during development and adult life (Valles-Colomer et al., 2019).
Evidently, we must be careful when extrapolating data from animal models to human conditions, since protocols of social isolation stress with animals mismatch the circumstances produced by the COVID-19 lockdown. Yet, studies with animal models are useful when trying to understand certain molecular mechanisms behind the observed behavioral changes in humans. In addition, we want to highlight that the nutritional status during neurodevelopment is critical to children and adolescents' proper development. It is also important to adequate nutrition and to enhance the immune system in order to provide effective protection against possible diseases, including COVID-19, and to guarantee the rapid recovery from the disease. As social isolation is capable of changing our relationship with food, the importance of social ties for an adequate diet becomes more evident during this period of quarantine.
4. Brain plasticity
4.1. Social behavior
Humans are inherently social and since early in development they have the ability to become apt cooperators with a strong motivation to communicate with other individuals (Tomasello, 2014; Boyd and Richerson, 2009). Evolutionarily, the formation of social bonds was fundamental to both human survival and to guarantee a healthy cognitive, emotional, endocrine and immune development (Ertel et al., 2008; Miyazaki et al., 2005). In fact, staying close to significant others is essential to create and maintain social bonds in humans (Dunbar, 2010). In normal circumstances (i.e. in the absence of threats), spatial distancing is unnatural for us. This is more pronounced during threatening contexts, like this COVID-19 pandemic, where our affiliative tendencies and the desire to seek physical contact become even stronger (Mawson, 2017). In the same vein, a recent paper showed that people can crave social cues just like they crave food (Tomova et al., 2020).
From this perspective, the adolescence period is considered a time of deep learning about the social environment when several key aspects of social cognition continue to develop, including the comprehension of other people's emotions, intentions, and beliefs (Blakemore and Mills, 2014; Blakemore, 2008). It is a time of psychosocial changes between childhood and adulthood, and a period of heightened sensitivity to social contexts during which adolescents spend more time with peers (Larson and Richards, 1991; Blakemore and Mills, 2014; Burnett et al., 2011; Blakemore, 2008). In fact, for most teenagers, school is one of the most important social environments and one in which peers increasingly affect adolescents' self-concept, well-being and behavior (Gorrese and Ruggieri, 2013; O'Brien and Bierman, 1988).
Unfortunately, many adolescents during the COVID-19 pandemic are unable to attend schools which culminated in limited interaction with peers, imposing a gap on their social network (Spinelli et al., 2020) that has been tentatively supplied by virtual interaction. It was shown by Crone and Konijn (2018) that the use of social media by adolescents builds not only the connection among peers, but also their brain connectivity. However, a recent study showed that school routines are important coping mechanisms specifically for young people with mental health issues (Lee, 2020). Furthermore, it was shown that periods without school are also associated with decreased physical activity; increased screen time, irregular sleep patterns, and less appropriate diets in children and adolescents (Wang et al., 2020).
The social touch is essential to develop cognition, emotions, attachment and relationships (Cascio et al., 2019). In addition, it also contributes to the physiological regulation of the body's responses to acute stressors as well as other short-term challenges. Gallace and Spence (2010) reviewed the importance of the social touch to human development under different aspects. It was discussed that, even when virtual relationships are established, they cannot cater to physical needs which are essential to improvement of interpersonal connections that contribute to the global development of the individual (Gallace and Spence, 2010). In the context of quarantine, the questions to the discussion we bring here are if this “virtual contact” will be enough to social behavior constructions and if it will change the course of brain development. Could social isolation stress and adversities that were installed during the pandemic result in a poor relational experience and affect the brains under development? What will be the effects of this long-term switch to “virtual contact” on human interactions? It is also important to highlight that the impact of COVID-19 is not uniform across adolescents, considering families with medium to high-income resources being able to provide adolescents with additional opportunities to interact with peers through technology, while other families cannot.
In addition, it should be considered that adolescence is also characterized by multiple biological changes that include a cascade of hormonal and physical changes, leading to a substantial development of the brain, burst of activity dynamically strengthening and weakening connections among key brain regions in response to environmental input (Galvan, 2014). Therefore, the developmental transition between childhood and adulthood brains circuits involves maturation in frontal cortical neural systems and in social and affective circuitry that occurs in response to social experiences (e.g. relationships and interactions that a person experiences with others, including that from the same age), socioeconomic status and culture (Crone and Dahl, 2012; Foulkes and Blakemore, 2018).
However, this benefit of increased plasticity also renders vulnerability to stressors and to mental health issues. In fact, adolescence is the peak age of onset for the most common psychiatric disorder such as attention-deficit/hyperactivity disorder (ADHD), anxiety, mood and schizophrenia (Kessler et al., 2005), and it is also a time of high risk for substance abuse and suicidal behavior. The peak onset of mental illness during the teenage years could be explained by the surges of sex hormones and neurobiological changes that target specific brain regions as well as cell populations (Casey et al., 2005). During development, the CNS undergoes an intense process of formation and maintenance of synaptic connections until adulthood. Environmental factors constantly act in this process, influencing the formation of individual cognitive and emotional aspects (Burggren and Mueller, 2015; Knudsen, 2004; Takesian and Hensch, 2013; Vickers, 2014).
The pandemic situation that we have plunged into showed multiples outspread on the individual's mental health. However, how will it affect adolescents' brains in adulthood, especially those key regions associated with action-emotion regulation (e.g. impulsive behavior), empathy, and decision-making skills? In pandemic times, there is a pressing need to mitigate the impact the young population is subjected to, particularly the more vulnerable ones who suffer from social inequalities in which families with low income cannot face education, remote learning and virtual contact with peers and family members.
4.2. Social inequalities, neglect and distress
The pandemic has been widening and exposing the social inequality in every country affected by the economic shutdown, especially in underdeveloped countries. Social isolation also brought elevated levels of domestic violence, including childhood maltreatment or neglect as a result of parenthood insecurities and inabilities (Fegert et al., 2020). Parenting during the pandemic is an additional challenge to deal with remote learning, home office working, and endless house chores (Spinelli et al., 2020). Children at home represent high costs from feeding to internet access. Moreover, the internet often has to be shared with all family members. To those who live in a low-income situation or a crowded house, this is even harder to manage. Adding to this scenario, children who have special needs, those who have had a previous COVID-19 diagnosis, or were already under treatment for any condition are more vulnerable (Fegert et al., 2020).
During childhood, adverse experiences such as trauma can induce long-term impacts on brain development as well as promote mental and behavioral disturbances through neurochemical and physiological imbalance related to neuroimmunoendocrine regulatory mechanisms (De Bellis and Zisk, 2014). Copeland et al. (2018) followed children of different age groups for 22 years and pointed out that the outcome of trauma during childhood results in much more than a mental health issue and it became a public health issue. Moreover, it was shown by Copeland et al. (2018) that childhood trauma can trigger mental disorders, including addiction in adulthood. Therefore, it is necessary to look at this subject very carefully, in the way people is managing the COVID-19 pandemic stress. We need to guarantee that children and adolescents, as well as their families, receive the proper psychological help to support their mental health. If an emotional neglect already exists, this will most likely be intensified by the work overload that parents and/or caregivers are subjected to, as well as by social inequalities, that may be related to the economic crash and the employment discharges around the world. The sum of the trauma effects can be devastating, and the damage might not be detected only in a few years after-pandemic.
4.3. Playing and nature environment
In the last few years, there has been a growing number of works demonstrating that a direct contact with nature is associated with great health benefits (McCurdy et al., 2010). Among the suggested mechanisms by which stimuli from nature can impact on individual well-being and mental health include regulation of blood pressure, regulation of the immune system, reduction of pro-inflammatory cytokines after walks in a forest (outside urbanized areas), regulation of autonomous activity (through the reduction of sympathetic activity opposed to an increase in the parasympathetic activity), and a deep feeling of relaxation and concentration (for review see Kuo, 2015).
Nature exposure can also reduce stress during early childhood in comparison to the ones that did not have much access to similar outside stimuli (Wells and Evans, 2003). Children highly exposed to nature also present great health and physical development (development and refinement of locomotor skills, for example), improved self-control (reduces inappropriate in-class behaviors), better communication and social development (more complex language), besides proper cognitive development (multi-sensorial stimuli that raise curiosity and creativity) (Kemple et al., 2016).
Sunlight exposures have also positive effects on human health (Alfredsson et al., 2020). Suitable sunlight exposure is essential for vitamin D synthesis, which is involved in several physiological functions (Föcker et al., 2017). However, insufficient sunlight exposure along with a low status of vitamin D may be responsible for critical public health issues and neuropsychiatric disturbances such as cardiovascular diseases, metabolic syndrome, hypertension, multiple sclerosis, asthma, type 1 diabetes, autism, Alzheimer's disease, schizophrenia and depression (Alfredsson et al., 2020; Brouwer-Brolsma et al., 2013; Föcker et al., 2017; Humble et al., 2010; Itzhaky et al., 2012). Accordingly, it was demonstrated that adults with depression exposed to low sunlight showed a decrease in interleukin-6 (IL-6) serum levels, a pro-inflammatory cytokine, when compared to adults with depression who were exposed to high sunlight (Levandovski et al., 2013), which supports the well described benefits of proper sunlight exposition (Alfredsson et al., 2020). Also, there was already observed that increased serum levels of IL-6 during childhood have been associated with a greater risk of developing depression and psychosis in young adulthood (Khandaker et al., 2014). Therefore, we can comprehend the importance of appropriate sunlight exposure, mainly during childhood, regarding mental health conditions since this prolonged lockdown period may be potentially limiting youngsters to have a proper sunlight exposition.
Unfortunately, because of quarantine, children are not allowed to play in outdoor areas and explore unstructured play. This means that we are switching from the “play-outside mode” to the “play-indoor mode”, which includes spending more time on the screen. The negative impact of media and technology use was analyzed in children (aged 4–8), preteens (9–12), and teenagers (13–18). It seems that increasing the screen time use correlates positively with unhealthy eating, lack of physical exercise, more total ill-being as well as attention and physical problems (Rosen et al., 2014). A meta-analysis review showed a negative correlation between the amount of screen use and language development in younger children. However, if exposed to better quality content with an educational bias, the use of screens can be beneficial for children's language in an age-dependent manner (Madigan et al., 2020).
It is undeniable that we might have prejudice on their development, including on their mental health, but the results from this switch on our modi operandi will be known in years, not now. A follow up from these children will determine if we had or not an impact on brain organization and changes in social behavior as a consequence of the pandemic.
5. Public health and support
In face of this pandemic scenario, children and adolescents are exposed to stressful situations such as fear of contracting the disease, frustration, boredom, information overload, family financial loss, and drastic changes in daily activity patterns, which make clear the multifaceted threats of COVID-19 (Brooks et al., 2020). All these issues collaborate for future unpredictable damages that could impact not only the own children's health, but also the health systems. For instance, Sprang and Silman (2013) showed a higher incidence of post-traumatic stress disorder symptoms in quarantined children than those who were not quarantined (Sprang and Silman, 2013), evidencing just one aspect of how a pandemic situation may impact on a vulnerable population.
The government and public health authorities need to consider the impact of this unusual situation on children and adolescents by implementing mitigating measures and making investments available to reduce the damages. Notwithstanding this, as the impact on the individual's health is multifactorial, the launched resources and efforts to mitigate these damages must include health authorities, government, communities, organizations, schools, and family members. Some resources currently discussed in the literature address (i) making available a proper online environment for students to develop scholar activities (e.g. create suitable online platforms), (ii) providing motivational videos which can help to improve the daily lifestyle (e.g. how to have a balanced diet, practice exercises at home, and regulate the sleep), (iii) providing access to adequate information (e.g. how to adopt correct hygiene practices) and (iv) providing access to psychological professional support (Wang et al., 2020; Brooks et al., 2020; Liu et al., 2020). Furthermore, social support is widely understood as the presence of positive relationships that create a feeling of belonging, stimulate trust, and encourage self-care (Uchino, 2004). In this case, despite the external essential support, the internal support in the family context is fundamental. Parenting has been often described as the best resource to reduce adverse impacts on children's social-emotional and behavioral development (Perrin et al., 2016). In these circumstances, whenever parents are able to stay close, to care, to love, to play, and to have conversations with their children, it is easier to perceive indicators of psychological issues and, then, interfere appropriately (Wang et al., 2020; World Health Organization (WHO), 2020b). On the other hand, and complementarily, parents should be able to receive psychological, financial and logistic support provided by their government.
Although all resources cited above seem to have great and real applicability, most of them, unfortunately, may be effective only for a portion of the children and adolescents' population. The sad and contrasting reality is that we live in a world with a broad social inequality and neglect in children's care (e.g. domestic violence [Marques et al., 2020]). In this context, some questions are still to be properly addressed such as (i) how to deal with the reality wherein quarantined children are suffering from more domestic violence? And what will be the extent of the psychological damages in these individuals in the future? (ii) How to offer educational online support for children that live in rural or suburban areas where there is no or limited access to the internet or even technological devices? (iii) How motivational resources can work for children whose family members have lost their income source and are living in extreme poverty, and (iv) how to prevent these individuals from the risk of infection when their houses stay in areas with poor sanitary conditions and are neglected by the government? All these concerns make part of a major problem of social inequality present in the current world and have been aggravated with this pandemic situation.
To properly address these two faces of reality, we call attention of governments and authorities to also carefully look for this younger population that is particularly more vulnerable to develop a severe mental illness, considering their hard-living conditions. Moreover, further efforts must be launched to provide suitable care and protection for them. In this context, some strategies have been already implemented such as the development of a public documental material on how to prevent violence during the social isolation period. It has been developed by WHO in association with other organizations (World Health Organization (WHO), 2020c). The proper financial support for families that have lost their income sources must be implemented by government policies in order to reduce a worsening of health conditions in a population that already is severely impaired by social inequalities.
6. Discussion
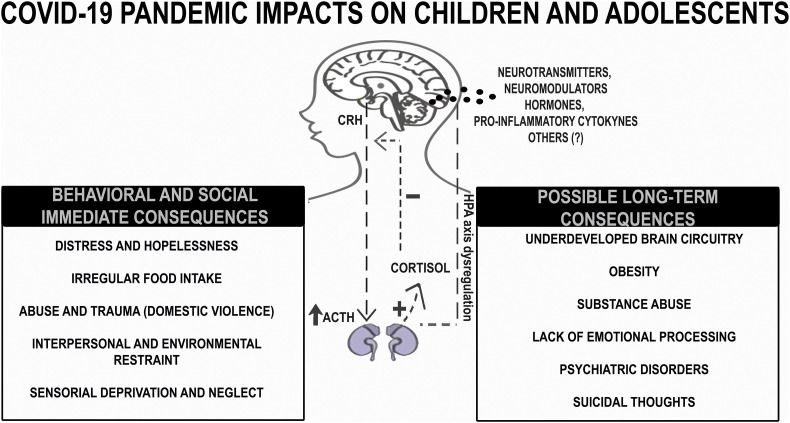
Previous works demonstrated the importance of quarantine and social isolation to contain the spread of the virus and the overload of health systems. However, the impact of this long-lasting social isolation on children and adolescents is still not properly addressed. Moreover, we draw attention not only to the multifaceted and heterogeneous feature of this pandemic which adds new issues and challenges to the population, but also to the fact that this COVID-19 outbreak may heighten pre-existing difficulties and problems in people lives, reaching the broad spectrum of the biopsychosocial framework. Herein, we brought elements for a more comprehensive discussion around the neurobiology changes triggered by the stress caused by the different facets of COVID-19 outbreak (Fig. 1 ). We shed light on the effects of stress on the HPA axis and the possibility of triggering psychiatric disorders such as anxiety and depression, for example. We discussed neuroinflammation, diets, brain plasticity, social behavior and public health and support making an alert to a long-term public health issue and the need for prolonged governmental support (Fig. 1).
Fig. 1.
Possible impacts from COVID-19 pandemic stressors on children and adolescence's life. Under physiological conditions, activation of the HPA axis occurs through production and release of CRH through the paraventricular nuclei of the hypothalamus. CRH stimulates the secretion of ACTH by the anterior portion of the pituitary gland (adenohypophysis). Therefore, ACTH reaches the peripheral circulation and is transported to the cortex of the adrenal glands, inducing the release of glucocorticoids (e.g. cortisol) into the bloodstream. In a negative feedback mechanism, cortisol, in turn, inhibits the secretion of CRH and ACTH. However, during early stages of life, where the child or adolescent are subjected to situations of long-lasting stress, this axis can have its activity dysregulated by inflammatory mediators synthesis and release (e.g. pro-inflammatory cytokines), neurotransmitters, hormones, among other molecules which can interfere with different physiological mechanisms. It includes distinct processes since intake regulation to cognition, for example. Moreover, the homeostasis disruption caused by a dysregulation of the HPA axis in response to stress induces neuroimmunoendocrine changes, which, if persistent, can induce poor health. All probable harmful effects on an individual's health triggered by this imbalance could be related to immune, endocrine, and nervous systems overload, and even a predisposition of these individuals to develop psychiatric disorders in adulthood. In the panel on the left we have gathered some of the possible short-term effects from exposure to stressors of COVID-19 pandemic at this stage of life (e.g. distress and hopelessness, irregular food intake, abuse and trauma, interpersonal and environmental restraint, sensorial deprivation and neglect) and on the right, possible long-term consequences (e.g. underdeveloped brain circuitry, obesity, substance abuse, lack of emotional processing, psychiatric disorders, suicidal thoughts). HPA: hypothalamic-pituitary-adrenal; CRH: corticotrophin-releasing hormone; ACTH: adrenocorticotropic hormone.
As discussed throughout the above topics, changes in daily routine particularly harm children and adolescents (Wang et al., 2020), and this could, in turn, become a critical public health problem in the future. Moreover, we emphasize that youngsters can experience not only short- but also long-term consequences of COVID-19 stressors, as they present individual responses. The opening of cities and the uncontrolled re-establishment of some daily activities led to peaks of new cases, which also generates waves of expectations and frustration especially among youngsters who do not know how to deal with this.
It is our obligation to emphasize the notorious urgency of psychological monitoring of quarantined children and adolescents, for an expected long period, especially for those who suffer domestic abuse, which grows in the same proportion to unemployment, financial bankruptcy and social inequalities. Moreover, we cannot forget the ones who lost their family members to COVID-19 or are separated from their parents or caregivers for safety reasons, and also those who already had a disorder and cannot receive proper health treatment. The withdrawal from social life, daily activities, as attending to school, combined with fear, anxiety and the feeling of the unpredictable, increase the risks for this group to develop psychiatric disorders in the future, even those who do not have such histories. Besides, children whose parents are under high stressful conditions at home due to pandemic also have a higher risk of developing psychiatric disorders (Maciejewski et al., 2018).
Health authorities and government have to treat this as a public health issue, and not as something whose outcome is short-lived. However, more investment to research is needed to evaluate the impact of COVID-19 pandemic stressors on youngsters developing brains, so we can prevent or mitigate mental health outcomes by offering support and/or proper treatment. We reinforce the need to follow up these children, adolescents and also their families and caregivers in order to develop strategies that will be able to mitigate, in a long term, the COVID-19 pandemic effects.
Authors contributions
POSB conceived and designed the study idea. CSF, PCS, LCLP, TMO, LSC, IR, ESF, ARS and POSB managed literature searches and wrote the manuscript. EGA, ARS and POSB critically reviewed the manuscript. POSB, LSC and ESF designed the figure. All authors contributed to and have approved the final manuscript.
Funding
This work was supported by CNPq, CAPES and FAPERJ (Brazil). This work was developed in the frameworks of the Brazilian National Institute of Science and Technology on Neuroimmunomodulation (CNPq) and the Rio de Janeiro Neuroinflammation Research Network (Faperj). They had no further role in study design, preparation, writing of the report, and in the decision to submit this paper for publication.
Declaration of Competing Interest
The authors declare no conflict of interest.
Acknowledgments
We are grateful to Arnaldo P. Andrade for his valuable suggestions in writing this article.
References
- Alfredsson L., Armstrong B.K., Butterfield D.A., Chowdhury R., de Gruijl F.R., Feelisch M. Insufficient sun exposure has become a real public health problem. Int J Environ Res Public Health. 2020;17(14):5014. doi: 10.3390/ijerph17145014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arcego D.M., Krolow R., Lampert C., Toniazzo A.P., Berlitz C., Lazzaretti C. Early life adversities or high fat diet intake reduce cognitive function and alter BDNF signaling in adult rats: interplay of these factors changes these effects. Int. J. Dev. Neurosci. 2016;50:16–25. doi: 10.1016/j.ijdevneu.2016.03.001. [DOI] [PubMed] [Google Scholar]
- Barnes C.N., Wallace C.W., Jacobowitz B.S., Fordahl S.C. Reduced phasic dopamine release and slowed dopamine uptake occur in the nucleus accumbens after a diet high in saturated but not unsaturated fat. Nutr Neurosci. 2020 doi: 10.1080/1028415X.2019.1707421. 1-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blakemore S.J. The social brain in adolescence. Nat. Rev. Neurosci. 2008;9(4):267–277. doi: 10.1038/nrn2353. [DOI] [PubMed] [Google Scholar]
- Blakemore S.J., Mills K.L. Is adolescence a sensitive period for sociocultural processing? Annu. Rev. Psychol. 2014;65:187–207. doi: 10.1146/annurev-psych-010213-115202. [DOI] [PubMed] [Google Scholar]
- Bonnavion P., Jackson A.C., Carter M.E., de Lecea L. Antagonistic interplay between hypocretin and leptin in the lateral hypothalamus regulates stress responses. Nat. Commun. 2015;6:6266. doi: 10.1038/ncomms7266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd R., Richerson P.J. Culture and the evolution of human cooperation. Philos. Trans. R. Soc. Lond. Ser. B Biol. Sci. 2009;364(1533):3281–3288. doi: 10.1098/rstb.2009.0134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brenhouse H.C., Schwarz J.M. Immunoadolescence: Neuroimmune development and adolescent behavior. Neurosci Biobehav Rev. 2016;70:288–299. doi: 10.1016/j.neubiorev.2016.05.035. S0149-7634(16)30105-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brouwer-Brolsma E.M., Feskens E.J., Steegenga W.T., de Groot L.C. Associations of 25-hydroxyvitamin D with fasting glucose, fasting insulin, dementia and depression in European elderly: the SENECA study. Eur. J. Nutr. 2013;52(3):917–925. doi: 10.1007/s00394-012-0399-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burggren W.W., Mueller C.A. Developmental critical windows and sensitive periods as three-dimensional constructs in time and space. Physiol. Biochem. Zool. 2015;88(2):91–102. doi: 10.1086/679906. [DOI] [PubMed] [Google Scholar]
- Burnett S., Sebastian C., Cohen Kadosh K., Blakemore S.J. The social brain in adolescence: evidence from functional magnetic resonance imaging and behavioural studies. Neurosci. Biobehav. Rev. 2011;35(8):1654–1664. doi: 10.1016/j.neubiorev.2010.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calcia M.A., Bonsall D.R., Bloomfield P.S., Selvaraj S., Barichello T., Howes O.D. Stress and neuroinflammation: a systematic review of the effects of stress on microglia and the implications for mental illness. Psychopharmacology. 2016;233(9):1637–1650. doi: 10.1007/s00213-016-4218-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cascio C.J., Moore D., McGlone F. Social touch and human development. Dev Cogn Neurosci. 2019;35:5–11. doi: 10.1016/j.dcn.2018.04.009. S1878-9293(17)30196-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey B.J., Tottenham N., Liston C., Durston S. Imaging the developing brain: what have we learned about cognitive development? Trends Cogn Sci. 2005;9(3):104–110. doi: 10.1016/j.tics.2005.01.011. S1364-6613(05)00030-6. [DOI] [PubMed] [Google Scholar]
- Cavaliere G., Trinchese G., Penna E., Cimmino F., Pirozzi C., Lama A., M. P. High-fat diet induces neuroinflammation and mitochondrial impairment in mice cerebral cortex and synaptic fraction. Front. Cell. Neurosci. 2019;13:509. doi: 10.3389/fncel.2019.00509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen F., Zheng D., Liu J., Gong Y., Guan Z., Lou D. Depression and anxiety among adolescents during COVID-19: a cross-sectional study. Brain Behav Immun. 2020;88:36–38. doi: 10.1016/j.bbi.2020.05.061. S0889-1591(20)30891-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland W.E., Shanahan L., Hinesley J., Chan R.F., Aberg K.A., Fairbank J.A. Association of Childhood Trauma Exposure with Adult Psychiatric Disorders and Functional Outcomes. JAMA Netw. Open. 2018;1(7) doi: 10.1001/jamanetworkopen.2018.4493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crescentini C., Feruglio S., Matiz A., Paschetto A., Vidal E., Cogo P., Fabbro F. Stuck outside and inside: an exploratory study on the effects of the COVID-19 outbreak on Italian parents and Children’s internalizing symptoms. Front. Psychol. 2020;11:586074. doi: 10.3389/fpsyg.2020.586074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crone E.A., Dahl R.E. Understanding adolescence as a period of social-affective engagement and goal flexibility. Nat. Rev. Neurosci. 2012;13(9):636–650. doi: 10.1038/nrn3313. [DOI] [PubMed] [Google Scholar]
- Crone E.A., Konijn E.A. Media use and brain development during adolescence. Nat. Commun. 2018;9(1):588. doi: 10.1038/s41467-018-03126-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahmen B., Puetz V.B., Scharke W., von Polier G.G., Herpertz-Dahlmann B., Konrad K. Effects of early-life adversity on hippocampal structures and associated HPA Axis functions. Dev. Neurosci. 2018;40(1):13–22. doi: 10.1159/000484238. [DOI] [PubMed] [Google Scholar]
- Danese A., Moffitt T.E., Harrington H., Milne B.J., Polanczyk G., Pariante C.M. Adverse childhood experiences and adult risk factors for age-related disease: depression, inflammation, and clustering of metabolic risk markers. Arch Pediatr Adolesc Med. 2009;163(12):1135–1143. doi: 10.1001/archpediatrics.2009.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Bellis M.D., Zisk A. The biological effects of childhood trauma. Child Adolesc. Psychiatr. Clin. N. Am. 2014;23(2):185–222. doi: 10.1016/j.chc.2014.01.002. vii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Del Rey A., Besedovsky H.O. Immune-neuro-endocrine reflexes, circuits, and networks: physiologic and evolutionary implications. Front. Horm. Res. 2017;48:1–18. doi: 10.1159/000452902. [DOI] [PubMed] [Google Scholar]
- Deshpande N.G., Saxena J., Pesaresi T.G., Carrell C.D., Ashby G.B., Liao M.K., Freeman L.R. High fat diet alters gut microbiota but not spatial working memory in early middle-aged Sprague Dawley rats. PLoS One. 2019;14(5) doi: 10.1371/journal.pone.0217553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunbar R.I.M. The social role of touch in humans and primates: behavioural function and neurobiological mechanisms. Neurosci. Biobehav. Rev. 2010;34:260–268. doi: 10.1016/j.neubiorev.2008.07.001. [DOI] [PubMed] [Google Scholar]
- Ertel K.A., Glymour M.M., Berkman L.F. Effects of social integration on preserving memory function in a nationally representative US elderly population. Am. J. Public Health. 2008;98(7):1215–1220. doi: 10.2105/AJPH.2007.113654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esterwood E., Saeed S.A. Past epidemics, natural disasters, COVID19, and mental health: learning from history as we deal with the present and prepare for the future. Psychiatry Q. 2020 doi: 10.1007/s11126-020-09808-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fegert J.M., Vitiello B., Plener P.L., Clemens V. Challenges and burden of the coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: a narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc. Psychiatry Ment. Health. 2020;14:20. doi: 10.1186/s13034-020-00329-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finger B.C., Dinan T.G., Cryan J.F. High-fat diet selectively protects against the effects of chronic social stress in the mouse. Neuroscience. 2011;192:351–360. doi: 10.1016/j.neuroscience.2011.06.072. [DOI] [PubMed] [Google Scholar]
- Föcker M., Antel J., Ring S., Hahn D., Kanal Ö., Öztürk D. Vitamin D and mental health in children and adolescents. Eur Child Adolesc Psychiatry. 2017;26:1043–1066. doi: 10.1007/s00787-017-0949-3. [DOI] [PubMed] [Google Scholar]
- Foulkes L., Blakemore S.J. Studying individual differences in human adolescent brain development. Nat. Neurosci. 2018;21(3):315–323. doi: 10.1038/s41593-018-0078-4. [DOI] [PubMed] [Google Scholar]
- Francis H.M., Stevenson R.J. Higher reported saturated fat and refined sugar intake is associated with reduced hippocampal-dependent memory and sensitivity to interoceptive signals. Behav. Neurosci. 2011;125(6):943–955. doi: 10.1037/a0025998. [DOI] [PubMed] [Google Scholar]
- Gallace A., Spence C. The science of interpersonal touch: an overview. Neurosci. Biobehav. Rev. 2010;34(2):246–259. doi: 10.1016/j.neubiorev.2008.10.004. [DOI] [PubMed] [Google Scholar]
- Galley J.D., Nelson M.C., Yu Z., Dowd S.E., Walter J., Kumar P.S. Exposure to a social stressor disrupts the community structure of the colonic mucosa-associated microbiota. BMC Microbiol. 2014;14:189. doi: 10.1186/1471-2180-14-189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galvan A. Insights about adolescent behavior, plasticity, and policy from neuroscience research. Neuron. 2014;83(2):262–265. doi: 10.1016/j.neuron.2014.06.027. S0896-6273(14)00549-2. [DOI] [PubMed] [Google Scholar]
- Gorrese A., Ruggieri R. Peer attachment and self-esteem: a meta-analytic review. Per. Individ Dif. 2013;55:559–568. doi: 10.1016/j.paid.2013.04.025. [DOI] [Google Scholar]
- Granholm A.C., Bimonte-Nelson H.A., Moore A.B., Nelson M.E., Freeman L.R., Sambamurti K. Effects of a saturated fat and high cholesterol diet on memory and hippocampal morphology in the middle-aged rat. J. Alzheimers Dis. 2008;14(2):133–145. doi: 10.3233/jad-2008-14202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guessoum S.B., Lachala J., Radjacka R., Carretiera E., Minassiana S., Benoita L., Moroa M.R. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 2020;291:113264. doi: 10.1016/j.psychres.2020.113264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunnar M., Quevedo K. The neurobiology of stress and development. Annu. Rev. Psychol. 2007;58:145–173. doi: 10.1146/annurev.psych.58.110405.085605. [DOI] [PubMed] [Google Scholar]
- Hänsel A., Hong S., Cámara R.J., Von Kaenel R. Inflammation as a psychophysiological biomarker in chronic psychosocial stress. Neurosci. Biobehav. Rev. 2010;35(1):115–121. doi: 10.1016/j.neubiorev.2009.12.012. [DOI] [PubMed] [Google Scholar]
- Harahsheh A.S., Dahdah N., Newburger J.W., Portman M.A., Piram M., Tulloh R., Burns J.C. Missed or delayed diagnosis of Kawasaki disease during the 2019 novel coronavirus disease (COVID-19) pandemic. J Pediatr. 2020;222:261–262. doi: 10.1016/j.jpeds.2020.04.052. S0022-3476(20)30556–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hryhorczuk C., Florea M., Rodaros D., Poirier I., Daneault C., Des Rosiers C. Dampened mesolimbic dopamine function and signaling by saturated but not monounsaturated dietary lipids. Neuropsychopharmacology. 2016;41(3):811–821. doi: 10.1038/npp.2015.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humble M.B., Gustafsson S., Bejerot S. Low serum levels of 25-hydroxyvitamin D (25-OHD) among psychiatric out-patients in Sweden: relations with season, age, ethnic origin and psychiatric diagnosis. J. Steroid Biochem. Mol. Biol. 2010;121(1–2):467–470. doi: 10.1016/j.jsbmb.2010.03.013. [DOI] [PubMed] [Google Scholar]
- Ibi D., Takuma K., Koike H., Mizoguchi H., Tsuritani K., Kuwahara Y. Social isolation rearing-induced impairment of the hippocampal neurogenesis is associated with deficits in spatial memory and emotion-related behaviors in juvenile mice. J. Neurochem. 2008;105(3):921–932. doi: 10.1111/j.1471-4159.2007.05207.x. [DOI] [PubMed] [Google Scholar]
- Itzhaky D., Amital D., Gorden K., Bogomolni A., Arnson Y., Amital H. Low serum vitamin D concentrations in patients with schizophrenia. Isr. Med. Assoc. J. 2012;14(2):88. [PubMed] [Google Scholar]
- Jiang N.M., Cowan M., Moonah S.N., Petri W.A., Jr. The impact of systemic inflammation on neurodevelopment. Trends Mol Med. 2018;24(9) doi: 10.1016/j.molmed.2018.06.008. 794-804. S1471-4914(18)30135-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiao W.Y., Wang L.N., Liu J., Fang S.F., Jiao F.Y., Pettoello-Mantovani M., Somekh E. 2020. Behavioral and Emotional Disorders in Children during the COVID-19 Epidemic. 264–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones V.G., Mills M., Suarez D., Hogan C.A., Yeh D., Segal J.B. COVID-19 and Kawasaki disease: novel virus and novel case. Hosp Pediatr. 2020;10(6):537–540. doi: 10.1542/hpeds.2020-0123. [DOI] [PubMed] [Google Scholar]
- Juruena M.F., Eror F., Cleare A.J., Young A.H. The role of early life stress in HPA Axis and anxiety. Adv. Exp. Med. Biol. 2020;1191:141–153. doi: 10.1007/978-981-32-9705-0_9. [DOI] [PubMed] [Google Scholar]
- Keles B., McCrae N., Grealish A. A systematic review: the influence of social media on depression, anxiety and psychological distress in adolescents. Int. J. Adolesc. Youth. 2020;25(1):79–93. doi: 10.1080/02673843.2019.1590851. [DOI] [Google Scholar]
- Kemple K.M., Oh J., Kenney E., Smith-Bonahue T. The power of outdoor play and play in natural environments. Child. Educ. 2016;92(6):446–454. doi: 10.1080/00094056.2016.1251793. [DOI] [Google Scholar]
- Kessler R.C., Berglund P., Demler O., Jin R., Merikangas K.R., Walters E.E. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. 62/6/593. [DOI] [PubMed] [Google Scholar]
- Khandaker G.M., Pearson R.M., Zammit S., Lewis G., Jones P.B. Association of serum interleukin 6 and C-reactive protein in childhood with depression and psychosis in young adult life: a population-based longitudinal study. JAMA Psychiatry. 2014;71(10):1121–1128. doi: 10.1001/jamapsychiatry.2014.1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knudsen E.I. Sensitive periods in the development of the brain and behavior. J. Cogn. Neurosci. 2004;16(8):1412–1425. doi: 10.1162/0898929042304796. [DOI] [PubMed] [Google Scholar]
- Krolow R., Noschang C., Arcego D.M., Huffell A.P., Marcolin M.L., Benitz A.N. Sex-specific effects of isolation stress and consumption of palatable diet during the prepubertal period on metabolic parameters. Metabolism. 2013;62(9):1268–1278. doi: 10.1016/j.metabol.2013.04.009. [DOI] [PubMed] [Google Scholar]
- Kuo M. How might contact with nature promote human health? Promising mechanisms and a possible central pathway. Front. Psychol. 2015;6:1093. doi: 10.3389/fpsyg.2015.01093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuo L.E., Kitlinska J.B., Tilan J.U., Li L., Baker S.B., Johnson M.D. Neuropeptide Y acts directly in the periphery on fat tissue and mediates stress-induced obesity and metabolic syndrome. Nat Med. 2007;13(7):803–811. doi: 10.1038/nm1611. nm1611. [DOI] [PubMed] [Google Scholar]
- Lacey R.E., Kumari M., Bartley M. Social isolation in childhood and adult inflammation: evidence from the National Child Development Study. Psychoneuroendocrinology. 2014;50:85–94. doi: 10.1016/j.psyneuen.2014.08.007. [DOI] [PubMed] [Google Scholar]
- Lampert C., Arcego D.M., de Sa Couto-Pereira N., Dos Santos Vieira A., Toniazzo A.P., Krolow R. Short post-weaning social isolation induces long-term changes in the dopaminergic system and increases susceptibility to psychostimulants in female rats. Int J Dev Neurosci. 2017;61:21–30. doi: 10.1016/j.ijdevneu.2017.05.003. S0736-5748(17)30052-7. [DOI] [PubMed] [Google Scholar]
- Larson R., Richards M.H. Daily companionship in late childhood and early adolescence: changing developmental contexts. Child Dev. 1991;62(2):284–300. doi: 10.1111/j.1467-8624.1991.tb01531.x. [DOI] [PubMed] [Google Scholar]
- Lee J. Mental health effects of school closures during COVID-19. The Lancet. Child & Adolescent Health. 2020;4(6):421. doi: 10.1016/S2352-4642(20)30109-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levandovski R., Pfaffenseller B., Carissimi A., Gama C.S., Hidalgo M.P. The effect of sunlight exposure on interleukin-6 levels in depressive and non-depressive subjects. BMC Psychiatry. 2013;13:75. doi: 10.1186/1471-244X-13-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S., Yang L., Zhang C., Xiang Y.T., Liu Z., Hu S., Zhang B. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7(4) doi: 10.1016/S2215-0366(20)30077-8. e17-e18. S2215-0366(20)30077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maciejewski D., Hillegers M., Penninx B. Offspring of parents with mood disorders: time for more transgenerational research, screening and preventive intervention for this high-risk population. Curr. Opin. Psychiatry. 2018;31:349–357. doi: 10.1097/yco.0000000000000423. [DOI] [PubMed] [Google Scholar]
- Madigan S., McArthur B.A., Anhorn C., Eirich R., Christakis D.A. Associations between Screen Use and Child Language Skills: A Systematic Review and Meta-analysis. JAMA Pediatr. 2020 doi: 10.1001/jamapediatrics.2020.0327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marques, E. S., Moraes, C. L., Hasselmann, M. H., Deslandes, S. F., and Reichenheim, M. E. (2020). Violence against women, children, and adolescents during the COVID-19 pandemic: overview, contributing factors, and mitigating measures. Cad Saude Publica, 36(4), e00074420. Doi: S0102-311X2020000400505. [DOI] [PubMed]
- Mawson A., R . Mass Panic and Social Attachment: The Dynamics of Human Behavior. Routledge; London: 2017. pp. 1–330. [DOI] [Google Scholar]
- McCurdy L.E., Winterbottom K.E., Mehta S.S., Roberts J.R. Using nature and outdoor activity to improve children’s health. Curr Probl Pediatr Adolesc Health Care. 2010;40(5):102–117. doi: 10.1016/j.cppeds.2010.02.003. [DOI] [PubMed] [Google Scholar]
- Mengin A., Alle M.C., Rolling J., Ligier F., Schroder C., Lalanne L. Psychopathological consequences of confinement. Encephale. 2020;46(3S) doi: 10.1016/j.encep.2020.04.007. S43-S52. S0013-7006(20)30075-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyazaki T., Ishikawa T., Nakata A., Sakurai T., Miki A., Fujita O. Association between perceived social support and Th1 dominance. Biol Psychol. 2005;70(1):30–37. doi: 10.1016/j.biopsycho.2004.09.004. S0301-0511(05)00077-3. [DOI] [PubMed] [Google Scholar]
- Nugent N.R., Tyrka A.R., Carpenter L.L., Price L.H. Gene-environment interactions: early life stress and risk for depressive and anxiety disorders. Psychopharmacology. 2011;214(1):175–196. doi: 10.1007/s00213-010-2151-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Brien S.F., Bierman K.L. Conceptions and perceived influence of peer groups: interviews with preadolescents and adolescents. Child Dev. 1988;59(5):1360–1365. doi: 10.1111/j.1467-8624.1988.tb01504.x. [DOI] [PubMed] [Google Scholar]
- Ogden C.L., Carroll M.D., Lawman H.G., Fryar C.D., Kruszon-Moran D., Kit B.K., Flegal K.M. Trends in obesity prevalence among children and adolescents in the United States, 1988-1994 through 2013-2014. JAMA. 2016;315(21):2292–2299. doi: 10.1001/jama.2016.6361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pecoraro N., Reyes F., Gomez F., Bhargava A., Dallman M.F. Chronic stress promotes palatable feeding, which reduces signs of stress: feedforward and feedback effects of chronic stress. Endocrinology. 2004;145(8):3754–3762. doi: 10.1210/en.2004-0305. [DOI] [PubMed] [Google Scholar]
- Perrin E.C., Leslie L.K., Boat T. Parenting as primary prevention. JAMA Pediatr. 2016;170(7):637–638. doi: 10.1001/jamapediatrics.2016.0225. [DOI] [PubMed] [Google Scholar]
- Raony I., de Figueiredo C.S., Pandolfo P., Giestal-de-Araujo E., Oliveira-Silva Bomfim P., Savino W. Psycho-neuroendocrine-immune interactions in COVID-19: potential impacts on mental health. Front. Immunol. 2020;11:1170. doi: 10.3389/fimmu.2020.01170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen L.D., Lim A.F., Felt J., Carrier L.M., Cheever N.A., Lara-Ruiz J.M. Media and technology use predicts ill-being among children, preteens and teenagers independent of the negative health impacts of exercise and eating habits. Comput. Hum. Behav. 2014;35:364–375. doi: 10.1016/j.chb.2014.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saurabh K., Ranjan S. Compliance and psychological impact of quarantine in children and adolescents due to Covid-19 pandemic. Indian J. Pediatr. 2020;87(7):532–536. doi: 10.1007/s12098-020-03347-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shahid Z., Kalayanamitra R., McClafferty B., Kepko D., Ramgobin D., Patel R. COVID-19 and older adults: what we know. J. Am. Geriatr. Soc. 2020;68(5):926–929. doi: 10.1111/jgs.16472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- She J., Liu L., Liu W. COVID-19 epidemic: disease characteristics in children. J. Med. Virol. 2020;92(7):747–754. doi: 10.1002/jmv.25807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spinelli M., Lionetti F., Pastore M., Fasolo M. Parents’ stress and Children’s psychological problems in families facing the COVID-19 outbreak in Italy. [original research] Frontiers in Psychology. 2020;11(1713) doi: 10.3389/fpsyg.2020.01713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sprang G., Silman M. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Med Public Health Prep. 2013;7(1):105–110. doi: 10.1017/dmp.2013.22. [DOI] [PubMed] [Google Scholar]
- Stephens T.W., Basinski M., Bristow P.K., Bue-Valleskey J.M., Burgett S.G., Craft L. The role of neuropeptide Y in the antiobesity action of the obese gene product. Nature. 1995;377(6549):530–532. doi: 10.1038/377530a0. [DOI] [PubMed] [Google Scholar]
- Sumis A., Cook K.L., Andrade F.O., Hu R., Kidney E., Zhang X.…Hilakivi-Clarke L. Social isolation induces autophagy in the mouse mammary gland: link to increased mammary cancer risk. Endocr Relat Cancer. 2016;23(10):839–856. doi: 10.1530/ERC-16-0359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takesian A.E., Hensch T.K. Balancing plasticity/stability across brain development. Prog. Brain Res. 2013;207:3–34. doi: 10.1016/B978-0-444-63327-9.00001-1. [DOI] [PubMed] [Google Scholar]
- Tomasello M. The ultra-social animal. Eur. J. Soc. Psychol. 2014;44(3):187–194. doi: 10.1002/ejsp.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomiyama A.J., Dallman M.F., Epel E.S. Comfort food is comforting to those most stressed: evidence of the chronic stress response network in high stress women. Psychoneuroendocrinology. 2011;36(10):1513–1519. doi: 10.1016/j.psyneuen.2011.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomova L., Wang K., Thompson T., Matthews G., Takahashi A., Tye K., Saxe R. 2020. The need to connect: acute social isolation causes neural craving responses. Preprint from bioRxiv, 25 Mar 2020. PPR: PPR127005. [DOI] [Google Scholar]
- Tottenham N., Galvan A. Stress and the adolescent brain: amygdala-prefrontal cortex circuitry and ventral striatum as developmental targets. Neurosci Biobehav Rev. 2016;70 doi: 10.1016/j.neubiorev.2016.07.030. 217-227. S0149-7634(16)30081-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uchino B.N. Social support and physical health: Understanding the health consequences of relationships. American Journal of Epidemiolog. 2004;161 doi: 10.12987/yale/9780300102185.001.0001. 297–298. [DOI] [Google Scholar]
- Ulrich-Lai Y.M., Christiansen A.M., Ostrander M.M., Jones A.A., Jones K.R., Choi D.C., Herman J.P. Pleasurable behaviors reduce stress via brain reward pathways. Proc. Natl. Acad. Sci. U. S. A. 2010;107(47):20529–20534. doi: 10.1073/pnas.1007740107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valladolid-Acebes I., Stucchi P., Cano V., Fernandez-Alfonso M.S., Merino B., Gil-Ortega M. High-fat diets impair spatial learning in the radial-arm maze in mice. Neurobiol. Learn. Mem. 2011;95(1):80–85. doi: 10.1016/j.nlm.2010.11.007. [DOI] [PubMed] [Google Scholar]
- Valles-Colomer M., Falony G., Darzi Y., Tigchelaar E.F., Wang J., Tito R.Y. The neuroactive potential of the human gut microbiota in quality of life and depression. Nat. Microbiol. 2019;4(4):623–632. doi: 10.1038/s41564-018-0337-x. [DOI] [PubMed] [Google Scholar]
- Veenema A.H. Early life stress, the development of aggression and neuroendocrine and neurobiological correlates: what can we learn from animal models? Front Neuroendocrinol. 2009;30(4):497–518. doi: 10.1016/j.yfrne.2009.03.003. S0091-3022(09)00004-1. [DOI] [PubMed] [Google Scholar]
- Vickers M.H. Early life nutrition, epigenetics and programming of later life disease. Nutrients. 2014;6(6):2165–2178. doi: 10.3390/nu6062165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang G., Zhang Y., Zhao J., Zhang J., Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet. 2020;395(10228):945–947. doi: 10.1016/S0140-6736(20)30547-X. S0140-6736(20)30547-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells N.M., Evans G.W. Nearby nature: a buffer of life stress among rural children. Environ. Behav. 2003;35(3):311–330. doi: 10.1177/0013916503035003001. [DOI] [Google Scholar]
- World Health Organization (WHO) WHO characterizes COVID-19 as a pandemic. Available from. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen [Accessed in 2020 July 23]
- World Health Organization (WHO) Helping children cope with stress during the 2019-nCoV outbreak. Available from. 2020. https://www.who.int/docs/default-source/coronaviruse/helping-children-cope-with-stress-print.pdf?sfvrsn=f3a063ff_2 [Accessed in 2020 July 23]
- World Health Organization (WHO) Coronavirus disease (COVID-19) advice for the public: healthy parenting. Available from. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/healthy-parenting [Accessed in 2020 July 23]