Obesity and COVID-19 are pandemics that negatively affect the health and well-being of children. The disease of childhood obesity has risen to pandemic levels in United States (U.S.) youth with the fastest rise seen in severe obesity (Skinner, Ravanbakht, Skelton, Perrin, & Armstrong, 2018). COVID-19 is a highly contagious disease in humans causing significant rates of illness, hospitalization, and death. The World Health Organization (World Health Organization, 2020) declared COVID-19 a pandemic on March 11, 2020. Obesity is identified as an independent risk factor for COVID-19 disease severity (Lighter et al., 2020). Children with obesity may experience a more severe COVID-19 trajectory, including the need for respiratory support (Zachariah et al., 2020).
Responses to the COVID-19 pandemic evoked major lifestyle changes including stay-at-home orders and physical distancing. Schools closed and children lost the safety net of access to nutritious food, a safe place to be, and mandatory physical activity as well as their social networks and familiar routines. Potential consequences of being restricted to home, as addressed in this clinical report, threaten the health and well-being of children with obesity. This report will address the impact of COVID-19 on children with obesity, describe how stress exacerbates both conditions, and identify interventions to reduce the negative impact.
Bronfenbrenner's bioecological model
Childhood obesity is a complex disease, with multiple influences and varied outcomes. Urie Bronfenbrenner's Social Ecological Model (SEM) has been a useful framework for describing the multi-factorial interactions associated with childhood obesity (Davison & Birch, 2001; Feeg, Candelaria, Krenitsky-Korn, & Vessey, 2014; Golden & Earp, 2012; Lemus et al., 2016; Ohri-Vachaspati et al., 2015). Bronfenbrenner's early work on the SEM emphasized the environment context. However, over time, the model has evolved to address developmental experiences of continuity and change through four dynamic, interrelated components: proximal processes (interaction between organisms and their environment), person characteristics, context and time (Bronfenbrenner & Ceci, 1994; Bronfenbrenner & Morris, 2006; Rosa & Tudge, 2013).
Bronfenbrenner's model is a constructive framework for exploring the impact of COVID-19 on childhood obesity. Fig. 1 depicts five nested or multi-layered systems and their subsystems. The Chronosystem connotes lifespan development (ontogeny) and the time during which an individual lives (history). The Macrosystem entails healthcare policy and societal impacts, along with influences of culture, traditions, values, and beliefs. The Exosystem reflects the multiple institutions that affect the context of a person's existence, including government, the legal system, mass media, the school system, industry or the workforce. The Mesosystem captures the bidirectional relationships and linkages between Microsystems which are vital parts of a person's immediate or most proximal environment, such as family, neighborhood, school, and peers.
Fig. 1.
Bronfenbrenner’s Bioecological Model.
Examination of the impact of COVID-19 on childhood obesity from an ecological perspective and framed by Bronfenbrenner's Bioecological model reveals a plethora of biopsychosocial antecedents, risks and potential consequences. The current COVID-19 pandemic along with overlapping economic and social crises have triggered a cascade of demands on children and their parents. With schools and daycare centers closed or using hybrid models, workers furloughed or laid off, and peer group activities cancelled, families are coping with a myriad of stressors including uncertainty about the future. The Bioecological Model creates a context for effective assessment and intervention to assist children and families in their understanding and management of obesity in the current environment.
Definitions and prevalence
Obesity, a chronic disease resulting from breakdown of the body's energy regulatory system (ERS), is impacted by genetic, environmental, and psychosocial factors. The Centers for Disease Control and Prevention (Centers for Disease Control and Prevention, 2020) standardized growth charts define excess adiposity in youth as overweight (85th–94th percentiles), obesity (95-98th percentiles), and severe obesity (≥99th percentile). Obesity affects over 337 million children globally with 213 million youth classified as overweight and 124 million with obesity and severe obesity (NCD Risk Factor Collaboration (NCD-RisC), 2017). Pediatric obesity rates vary by age, ethnicity, location, and social determinate factors (Ogden et al., 2018; Yusuf et al., 2020).
The U.S. prevalence of COVID-19 in children and adolescents is 1053 cases per 100,000 (792,188 cases) which is 11% of all COVID-19 U.S. cases (American Academy of Pediatrics and the Children's Hospital Association, 2020). The number of cases not confirmed by testing is unknown. A severe form of COVID-19, classified as multisystemic inflammatory syndrome in children (MIS-C), was first reported in the U. S. in March, 2020. By July 2020, 53 U.S. hospitals had reported 186 MIS-C cases in all pediatric age groups (Feldstein et al., 2020). As of October 2020, the CDC reports 1097 confirmed MIS-C cases with 20 deaths (Centers for Disease Control and Prevention, 2020d).
Pathophysiology
Understanding of the human energy regulation system (ERS) has evolved from a simplistic “calories in = calories out” to recognition of a complex system modulated by genetics and environment (Roh, Song, & Kim, 2016; Timper & Brüning, 2017). Ingested energy (calories) triggers multiple pathways designed to assess, process, store, and expend energy as the body perceives its acute and long-term needs. When working well, energy needs are accurately assessed, managed in a timely manner, and weight is stable (Berthoud, Münzberg, & Morrison, 2017).
Individuals with an injured ERS are less capable of efficient energy management. Adipose tissue is an active endocrine organ that plays a critical role in maintaining energy balance (Reilly & Saltiel, 2017). When excess nutrients enter the adipocyte (specialized cell for storage of fat), a cellular stress response initiates which results in a sustained increase in cortisol production and chronic inflammation. Chronic inflammation is marked by the over-expression of inflammatory mediators and decreased adiponectin (an anti-inflammatory adipokine) production (Ellulu, Patimah, Khaza'ai, Rahmat, & Abed, 2017). Unchecked, chronic inflammation leads to ERS dysfunction manifesting as cardiovascular disease, metabolic abnormalities, depression, cancer, and other metabolic conditions.
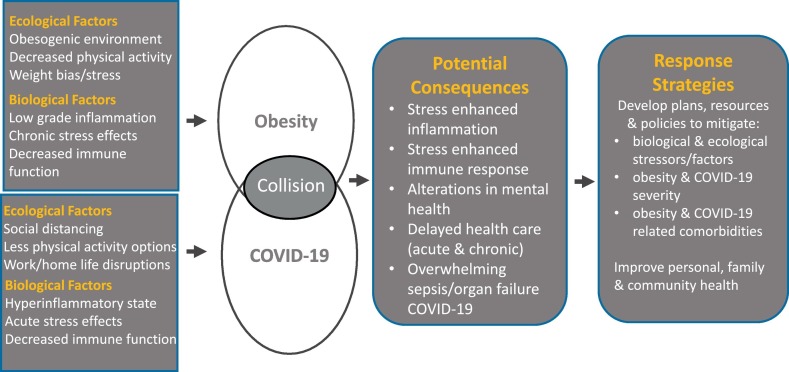
Obesity is a risk factor for increased severity of COVID-19, as excess weight decreases an individual's immune response. A decreased immune response results from chronic inflammation exacerbated by stress, causing associated metabolic complications (Yuki, Fujiogi, & Koutsogiannaki, 2020). Inflammation from the disease of obesity combined with COVID-19 hyperinflammation and weakened immune response (Frydrych, Bian, O'Lone, Ward, & Delano, 2018; Korakas et al., 2020) increases the risk of individuals developing overwhelming sepsis and organ failure (Shekerdemian et al., 2020). Fig. 2 depicts the relationship between the two pandemics.
Fig. 2.
Collision of obesity and COVID-19 pandemics.
Mental health stressors exacerbated during pandemic
The COVID-19 pandemic introduced potentially traumatic events into the lives of children and their families (Fegert, Vitiello, Plener, & Clemens, 2020; Human Rights Watch, 2020). Stress triggers activation of our body's stress response systems. “Toxic stress” ensues with prolonged activation of the stress response system with children experiencing stress that is strong, frequent, and protracted (Condon, Sadler, & Mayes, 2018; Reichel, 2019; Shonkoff et al., 2012). Sustained activation of stress response systems can lead to chronic health issues, including obesity.
A supportive relationship with adults can help “buffer” a stressful experience and support the child's adaptation. However, high levels of parental stress due to job loss, isolation, and unexpectedly working from home (Fegert et al., 2020) increases the difficulty for parents in providing a supportive buffering presence for their children. Parental stress is associated with childhood obesity in some studies, most recently in non-Hispanic Black families (Baskind et al., 2019). Disturbances in the social environment during infancy and early childhood appear to play a critical role in weight gain and obesity (Hemmingsson, 2018).
COVID-19 stressors disproportionally affect vulnerable populations already experiencing toxic stress from poverty, racism and structural inequality (Bailey et al., 2017; Bowleg, 2020). Lack of, or decreased access, to treatments for chronic physical and/or mental illness conditions can exacerbate negative outcomes (Fegert et al., 2020). Rates of domestic violence and child abuse have increased during the pandemic (Fegert et al., 2020; The Guardian, 2020) and children with pre-existing conditions may be particularly at risk. Studies demonstrate a relationship between exposure to toxic stress from adverse childhood events and the risk for childhood obesity (Bethell, Newacheck, Hawes, & Halfon, 2014; Garasky, Stewart, Gundersen, Lohman, & Eisenmann, 2009; Lohman, Stewart, Gundersen, Garasky, & Eisenmann, 2009).
Responding to an unpredictable threat like the COVID-19 pandemic evokes stress responses (Brooks et al., 2020; Vinkers et al., 2020; Table 1 ). Post-traumatic stress disorder (PTSD) was reported in about one-third of children who were isolated or quarantined after the H1N1 and SARS epidemics in Central and North America (Sprang & Silman, 2013). The impact of the COVID-19 pandemic is having a similar impact with 27% of parents self-reporting worsening mental health and 14% reporting worsening behavioral health for their children (Patrick et al., 2020).
Table 1.
Common sources and responses to stress from the COVID-19 pandemic.
| Sources of stress | Responses to stress |
|---|---|
| Quarantine | Decreased concentration |
| Social isolation | Irritability |
| Less interaction with peers | Sleep disturbances |
| Threat to food insecurity | Anxiety |
| Changes in routines and schedules | Interpersonal conflict |
| Threat to stable family finances | Depression |
| Limits to physical activity | Anger |
| Adaptation to online learning | Emotional exhaustion |
| Parental stress | Weight gain |
| Fear of COVID-19 disease |
The relationship between stress, mental health, and childhood obesity is complex (Small & Aplasca, 2016). Children experiencing obesity have a higher risk for depression (Smith, Fu, & Kobayashi, 2020) because of stigma and isolation. Children with overweight or obesity report more stress (Thaker et al., 2020) and eat in response to stress to a greater degree than normal weight peers (Miller et al., 2019). Promoting resilience is an important approach to successful stress management. However, this strategy is more difficult when experiencing poverty, isolation and mental health issues (Vinkers et al., 2020).
Social distancing issues
As COVID-19 spread across the globe, many countries employed school closure as a part of their social distancing policies to slow the transmission and ease the burden on the healthcare systems. It is estimated that 138 countries have closed schools worldwide, affecting 80% of children across the world (Van Lancker & Parolin, 2020). It is anticipated that COVID-19 related school closures will have detrimental social and health consequences for children, especially for those living in poverty and underserved communities. Out of school time has been associated with weight gain especially for Hispanics, African Americans, and children with overweight (Rundle, Park, Herbstman, Kinsey, & Wang, 2020). School closure may affect children and their ability to maintain a healthy weight in the many ways (Table 2 ).
Table 2.
Impact of school closure due to COVID-19 on children.
| Lack of family expertise with facilitating learning and accessing resources |
| Exacerbation of food insecurity |
| Change in availability of healthy foods |
| Change in physical activity |
| Regression in academic progress and decrease in exposure to art, music, library, and physical education |
| Online learning challenges including inadequate computers and internet |
| Negative impact on mental health and well being |
| Lack of access to healthcare and immunizations through school-based health centers |
For many children, school provides access to healthy food. Thirty million children in the U.S. receive lunch from the National School Lunch Program and over 14.7 million children participate in the School Breakfast Program (Hess, 2020). Access to food for children in these programs during the COVID-19 pandemic varies depending on location and school district, as well as family and community support. A recent national study found that food insecurity increased from 32.6 to 36% from March–July 2020 (Patrick et al., 2020).
Regression of academic progress is linked to time out of school and home schooling (Van Lancker & Parolin, 2020). Limited parental availability and discomfort with home schooling may influence this regression. Isolation from peers and disruption of normal routines may also impact children's mental health and well-being.
Finally, the school closures resulting from stay-at-home orders and social distancing may impact access to health care provided in the schools. There are currently 6.3 million students who access health care through the 2584 school-based health centers in 48 of the 50 states, the District of Columbia, and Puerto Rico (Love, Schlitt, Soleimanpour, Panchal, & Behr, 2019). These health centers, (51% are Federally Qualified Health Centers) serve 10,629 schools and provide access to primary care for many poor and underserved populations. In addition to primary care and immunizations, health centers provide behavioral health, oral health care, vision screening, and health/nutrition education. Many centers are housed in the schools and have been impacted by school closure thus, preventing these vulnerable children from accessing healthcare.
Home concerns
Family financial constraints
During COVID-19, families have experienced the stress of increased job losses, furloughs, and layoffs, limiting financial resources. At the same time, many communities have seen significant increases in food costs (Fore, 2020). Data suggest that families are stocking shelf-stable foods that are ultra-processed, calorie dense comfort foods (Almandoz et al., 2020; Rundle et al., 2020). Higher caloric foods can negatively impact all children, placing them at risk for weight gain. In times of increased stress, meals can easily morph away from healthy nutrition.
Ensuring the health of children, especially those with the chronic condition of childhood obesity, requires ongoing monitoring by healthcare specialists (Almandoz et al., 2020; Kumar & Kelly, 2017; Spear et al., 2007). However, as parental income was lost due to the COVID-19 pandemic (Board of Governors of the Federal Reserve System, 2020), health insurance for families also disappeared. Loss of health insurance has impacted especially vulnerable populations (Pifer, 2020), where elevated childhood obesity rates are the highest (Yusuf et al., 2020) as well as access to well child care and immunizations. Many primary care providers transitioned to telemedicine during the COVID-19 pandemic, but immunizations require an in-person visit. Immunizations administered through the Vaccines for Children Program that is responsible for 50% of immunizations given to U.S. children were substantially reduced (decreased by 100,000 orders) after the COVID-19 emergency declaration (Santoli et al., 2020).
Health disparities: vulnerable populations
The exacerbation of poverty by COVID-19 highlights ongoing health disparities, including childhood obesity, amongst vulnerable populations (Li, Mustillo, & Anderson, 2018). Non-essential employees lost jobs and health insurance at high rates due to the pandemic (Kochhar, 2020). Essential employees, who did not have the option to work from home, were placed at greater risk of COVID-19 exposure (Dubey et al., 2020; Fegert et al., 2020). A major risk factor for poor outcomes from COVID-19 disease includes having pre-existing chronic health conditions, including obesity (Centers for Disease Control and Prevention, 2020c; Dubey et al., 2020).
Working from home: screen time and decreased extracurricular activities
COVID-19 stay-at-home orders have placed children with obesity at risk for disease progression (Falbe et al., 2013). Excess screen time and sedentary activities may increase during quarantine as normal rules and supervision adjust. School and daycare closures due to COVID-19 require families to organize children's educational and social needs along with parental work responsibilities (Fegert et al., 2020). Parents retain less control over regular routines and the ability to maintain healthy behaviors. Overwhelmed parents struggle to ensure healthy behaviors within the family, especially for children at risk for excess weight gain (Kakinami, Barnett, Séguin, & Paradis, 2015).
Exercise/physical activity
An essential component to a healthy lifestyle is physical activity (Hagan et al., 2017). Physical activity fosters psychological well-being, increases self-esteem, capacity for learning, and helps children handle stress (U.S. Department of Health and Human Services, 2018). COVID-19 increases risk factors for obesity through increased stress and decreased physical activity related to environmental, academic and social changes. Online education lacks physical education class, recess time, and normal levels of active movement for the school-aged child and adolescent. Hybrid education often schedules physical education as virtual sessions. With children at home and isolated, access to opportunities and environments that support physical activity are decreased (Centers for Disease Control and Prevention, 2020a).
Depending on location of home residence, the availability of green space and safe walking areas may be limited during COVID-19 due to public health regulations. Children with no place to go or no one to play with are less likely to engage in running, jumping, and performing large motor skills (Fegert et al., 2020). A recent systematic review suggests that body mass index may be related to living in a lower-income community (Johnson et al., 2019). Data from two international studies found that better macro-economic indicators were related to lower rates of childhood obesity (Olaya et al., 2015), and distance to green space was the most significant factor contributing to obesity in urban children (Manandhar et al., 2019). Vrijheid et al. (2020) also found that children who live in densely populated areas or neighborhoods with fewer recreational facilities have increased childhood obesity rates. A recent study looking at the communities of Columbus, Ohio and Atlanta, Georgia demonstrated that larger disparities in access to green space in inner suburbs was associated with income in Columbus and race in Atlanta (Park & Gulmann, 2020).
With children spending more time inside due to COVID-19 restrictions, indoor pollution especially from parental smoking, fine particulate matter, and nitrogen dioxide increase the likelihood of the child having overweight or obesity (Vrijheid et al., 2020). Children exposed to primary care giver's smoking showed an increase in odds ratios for obesity at age three and five years, and it is hypothesized that tobacco smoke's chemicals may lead to impaired metabolic and immune functions of the child increasing susceptibility to obesity (Sunday & Kabir, 2019).
Changes in daycare/camp state regulations
Due to COVID-19, childcare and social activity environments have changed significantly. Families returning to the office or those temporarily working at home need to make the decision regarding if, and when, their children return to childcare and social activities. The Centers for Disease Control and Prevention (2020a) has developed guidelines and toolkits to protect staff, children, and their families during childcare and social activities from the spread of COVID-19; similar regulations apply to the summer camp environment (American Camp Association, 2020; Centers for Disease Control and Prevention, 2020b; The Ohio State University Extension, 2020; Today, 2020). With field trips cancelled and fewer children allowed to participate simultaneously in recreational activities, it is speculated that levels of physical activity are decreased. Children and adolescents, who grow and develop in the context of peer interactions, are missing these social opportunities (Erikson, 1950; Hagan et al., 2017; Piaget, 1974). The risk for childhood obesity and the inability to follow prevention and treatment guidelines for healthy weight present a challenge for parents and children.
Fear of COVID-19 ongoing health threat
In a dynamic environment, the ongoing fear of COVID-19, as well as predicted resurgences are a source of chronic stress. Lack of comfort with returning full-time or in hybrid form to the office and daycare/school includes fear that public health regulations will not be followed. Not knowing if others will wear masks properly and how one should proceed with interactions outside of the family are worries for parents, children and adolescents. Earlier this year, anxieties prevailed as academic environments evaluated plans for the current school year including face-to-face or hybrid learning models with carefully constructed safe environments ((AAP. American Academy of Pediatrics, 2020); Centers for Disease Control and Prevention, 2020a; NAPNAP. The National Association of Pediatric Nurse Practitioners, 2020). In school districts deciding to offer online education or hybrid models, parents may be forced to choose between employment or facilitating their child's education or daycare.
Bias/Stigma
The extensive and longstanding evidence on weight bias and stigma raises great concern about the potential impact of COVID-19 on childhood obesity (Gudzune, Bennett, Cooper, & Bleich, 2014; Puhl & King, 2013; Tomiyama et al., 2018). The obesogenic environment has become the norm during the COVID-19 pandemic, placing children at risk for gaining weight (An, 2020; Li et al., 2018). The colliding pandemics of childhood obesity and COVID-19 increase children's exposure to stress which increases inflammation and threatens their immune response (Dolsen, Crosswell, & Prather, 2019; Singer & Lumeng, 2017). In other words, the convergence of obesity and COVID-19 places children at increased risk for physical and psychosocial sequelae. Parental perceptions of their provider's attitudes toward children with obesity can impact patient-provider trust and influence whether parents seek or follow up with care (Puhl, Peterson, & Luedicke, 2013).
Virtual classrooms necessitate children, even those at very young ages, have access to phones or computers to complete on-line learning (Fore, 2020). A harmless social communication between classmates may become a route through which children can bully the child with obesity. An especially tough element of cyberbullying is its anonymous or indirect nature, making it difficult to stop the practice (Mateu et al., 2020). Children who are bullied may not feel comfortable sharing their plight with a parent or sibling, prolonging their exposure to the bullying and its accompanying stress.
A recently published international consensus statement about the stigma of obesity addressed the impact of unproven assumptions that attribute body weight to a lack of self-discipline and personal responsibility (Rubino et al., 2020). Weight stigma, discrimination, and bullying can lead to maladaptive eating which increases risk for unhealthy weight in susceptible children (Bomberg et al., 2019; Puhl, Himmelstein, & Pearl, 2020). Weight-based teasing, whether in person or in cyber space, can lead to further weight gain as a response to stress (Schvey et al., 2019). Children with obesity experiencing weight-based teasing and bullying are also susceptible to developing mental health disorders, especially anxiety and depression (Thaker et al., 2020; van Geel, Vedder, & Tanilon, 2014). Prolonged time at home contributes to children developing psychosocial issues, boredom (Dubey et al., 2020), and loneliness. Social isolation threatens a child's sense of security and exacerbates pre-existing anxiety or depression. Timely access to medical and mental health services is crucial.
Strategies and resources
The deleterious effects from pediatric obesity & COVID-19 disease demand maximum efforts to support families and children. Internet resources can be used to support children with obesity to achieve a healthier lifestyle. Tailored interventions that include parents and the family unit show promise (Kaakinen, Kyngäs, & Kääriäinen, 2018; Knowlden & Conrad, 2018). However, it is important that time on a computer not replace physical activity (Bozkurt, Özer, Şahin, & Sönmezgöz, 2018) or interrupt sleep which is associated with obesity and trunk fat mass (Park, Kim, & Shim, 2020). Policy interventions are needed to provide appropriate oversight to limit internet advertising used to market food products high in salt, fat and sugar (Kent, Dubois, Kent, & Wanless, 2013). Please see Table 3 for helpful online resources.
Table 3.
Resources.
Physical fitness is related to attention capacity in youth with obesity (García-Hermoso et al., 2020). Thus, sustaining safe opportunities for activity during the COVID-19 pandemic is essential. Availability of parks, trails, and water activities, along with hydration and restroom access, is important for family outings. Establishing a social distance plan is key for all recreational activities. Working with neighbors for planned outdoor opportunities for youth activity promotes supervised small group socialization and interactions. Care needs to be taken to prevent the spread of COVID-19 at all levels of organized sporting events and competition including those with close friends and family.
Strategies for better nutrition may be possible while families spend more time at home. Meal preparation can become a family activity, involving children in searching for recipes and preparing vegetables, fruit, and higher fiber meals. Families can engage children in identifying the healthiest snack from several choices. In contrast, less meal preparation time may lead to increased fast food or non-nutritious snack food (Lappan, Parra-Cardona, Carolan, & Weatherspoon, 2020). To address this, parents can help children choose the healthiest items on menus and work to reduce fast food consumption to no more than once a week.
The internalization of weight stigma may lead to disordered eating and unhealthy weight. Strategies to address obesity and mental health include tailoring interventions to children's developmental level and involving parents in multi-disciplinary team approaches (Cardel, Atkinson, Taveras, Holm, & Kelly, 2020). One important strategy by healthcare and clinical research professionals is using person first language which reduces the stigmatization of children with obesity and their families (Crocker & Smith, 2019). Prior negative healthcare experiences may impact an open and trusting relationship with new providers. A sensitive office environment with appropriate chairs, blood pressure cuffs, gowns, and privacy (especially with obtaining weight measurements) reduces anxiety and stress for the child and family (Fruh et al., 2016). Other evidence-based interventions to reduce stress include:
-
1.
Mindfulness interventions incorporating parental engagement (Jastreboff et al., 2018).
-
2.
Structured physical activity, advance meal preparation, and watching television with children (Parks, Kazak, Kumanyika, Lewis, & Barg, 2016).
-
3.
Improving parenting skills through attachment and attunement to infant feeding cues (Ordway et al., 2018).
Parenting styles may be a factor in the development of childhood obesity. Authoritative parenting is associated with smaller gains in BMI and lower likelihood of obesity while authoritarian or permissive parenting strategies are associated with higher child body mass percentile (Sokol, Qin, & Poti, 2017). Parents practicing authoritative parenting encourage choices (ex. which vegetables for dinner) rather than telling the child to eat vegetables or allowing the choice of no vegetables. Involving children in selecting after-school and summer physical activity programs are authoritative effective parenting strategies. Alternate strategies include regular family meals together at the table (Bohnert, Loren, & Miller, 2020) and collaborating with school nurses to address their child's weight (Frenn, Kaugars, Garcia, & Garnier-Villarreal, 2020).
Recommendations for policy
Policy changes that raise the nutrient standards of foods marketed to children show promise (Dunford, Popkin, & Ng, 2020). Several countries have adopted regulations related to food advertising and foods offered free to children or provided in schools to address the obesity epidemic (Corvalán, Reyes, Garmendia, & Uauy, 2019). Obesity prevention policies for children that include parental partnership programs are needed. Parents may be rallied as supporters of school-based initiatives to combat childhood obesity (Wolfson, Gollust, Niederdeppe, & Barry, 2015).
As policy options are considered for the colliding pandemics of COVID-19 and childhood obesity, ethical considerations of what is the best for the most people are essential. COVID-19 restrictions, for the good of all, have reduced many healthy food and physical activity options for children. Clinicians, families and communities must create and prioritize alternate, safe options. The many effects of the COVID-19 pandemic on childhood obesity must be considered in creating effective health policy going forward.
Conclusion
The evidence is clear - childhood obesity and COVID-19 are international pandemics. The clashing of the two diseases and the subsequent changes in the bioecological environment have placed children and adolescents at increased risk to develop obesity and exacerbate obesity disease severity. The once familiar environments of family, home, school, and community and their multi-factorial interactions have changed to unrecognizable scenarios, increasing stress for children and families. The impact of stress on both diseases, characterized by inflammation and weakened immune response and exacerbated by disparities, affects health, economic, and social outcomes. As healthcare providers focus on the comprehensive care of children and their families, a systematic assessment of their health and biopsychosocial needs is critical to the reduction of the negative impact of obesity and COVID-19.
Credit statement
All authors contributed to the conceptualization, writing of the original draft, and the writing of the review and editing of all drafts. All authors had final approval of submitted and published versions. Nancy Browne administered the project. No funding was connected with this manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interest
None.
References
- AAP. American Academy of Pediatrics COVID-19 planning considerations: Guidance for school reentry. 2020, June 25. https://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/clinical-guidance/covid-19-planning-considerations-return-to-in-person-education-in-schools/
- Almandoz J.P., Xie L., Schellinger J.N., Mathew M.S., Gazda C., Ofori A.…Messiah S.E. Impact of COVID-19 stay-at-home orders on weight-related behaviours among patients with obesity. Clinical Obesity. 2020:e12386. doi: 10.1111/cob.12386. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Academy of Pediatrics & the Children'’s Hospital Association Children & COVID-19: State data report. 2020, October 16. https://downloads.aap.org/AAP/PDF/AAP%20and%20CHA%20-%20Children%20and%20COVID-19%20State%20Data%20Report%207.30.20%20FINAL.pdf Updated October 16, 2020.
- American Camp Association COVID-19 resource center for camps. 2020. https://www.acacamps.org/resource-library/coronavirus-information-camps
- An R. Projecting the impact of the coronavirus disease-19 pandemic on childhood obesity in the United States: A microsimulation model. Journal of Sport and Health Science. 2020 doi: 10.1016/j.jshs.2020.05.006. S2095-2546(20)30065-X. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey Z.D., Krieger N., Agénor M., Graves J., Linos N., Bassett M.T. Structural racism and health inequities in the USA: Evidence and interventions. Lancet. 2017;389(10077):1453–1463. doi: 10.1016/S0140-6736(17)30569-X. [DOI] [PubMed] [Google Scholar]
- Baskind M.J., Taveras E.M., Gerber M.W., Fiechtner L., Horan C., Sharifi M. Parent-perceived stress and its association with children’s weight and obesity-related behaviors. Preventing Chronic Disease. 2019;16 doi: 10.5888/pcd16.180368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berthoud H.R., Münzberg H., Morrison C.D. Blaming the brain for obesity: Integration of hedonic and homeostatic mechanisms. Gastroenterology. 2017;152(7):1728–1738. doi: 10.1053/j.gastro.2016.12.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bethell C.D., Newacheck P., Hawes E., Halfon N. Adverse childhood experiences: Assessing the impact on health and school engagement and the mitigating role of resilience. Health Affairs. 2014;33(12):2106–2115. doi: 10.1377/hlthaff.2014.0914. [DOI] [PubMed] [Google Scholar]
- Board of Governors of the Federal Reserve System Report on the Economic Well-Being of U.S. households in 2019 - May 2020. 2020. https://www.federalreserve.gov/publications/2020-economic-well-being-of-us-households-in-2019-financial-repercussions-from-covid-19.htm Retrieved July 11, 2020.
- Bohnert A.M., Loren D.M., Miller A.L. Examining childhood obesity through the lens of developmental psychopathology: Framing the issues to guide best practices in research and intervention. The American Psychologist. 2020;75(2):163–177. doi: 10.1037/amp0000581. [DOI] [PubMed] [Google Scholar]
- Bomberg E.M., Ryder J.R., Brundage R.C., Straka R.J., Fox C.K., Gross A.C.…Kelly A.S. Precision medicine in adult and pediatric obesity: A clinical perspective. Therapeutic Advances in Endocrinology and Metabolism. 2019;10:1–25. doi: 10.1177/2042018819863022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowleg L. We're not all in this together: On COVID-19, intersectionality, and structural inequality. American Journal of Public Health. 2020;110(7):917. doi: 10.2105/AJPH.2020.305766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bozkurt H., Özer S., Şahin S., Sönmezgöz E. Internet use patterns and internet addiction in children and adolescents with obesity. Pediatric Obesity. 2018;13(5):301–306. doi: 10.1111/ijpo.12216. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U., Ceci S.J. Nature-nurture reconceptualized in developmental perspective: A bioecological model. Psychological Review. 1994;101(4):568–586. doi: 10.1037/0033-295x.101.4.568. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U., Morris P.A. In: Handbook of child psychology: Theoretical models of human development. Lerner R.M., Damon W., editors. John Wiley & Sons Inc.; 2006. The bioecological model of human development; pp. 793–828. [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet (London, England) 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cardel M.I., Atkinson M.A., Taveras E.M., Holm J.C., Kelly A.S. Obesity treatment among adolescents: A review of current evidence and future directions. JAMA Pediatrics. 2020 doi: 10.1001/jamapediatrics.2020.0085. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention K-12 schools and child care programs. 2020, June 3. https://www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/schools-faq.html Retrieved June 3, 2020, from. [PubMed]
- Centers for Disease Control and Prevention Suggestions for youth and summer camps. 2020, June 25. https://www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/summer-camps.html Retrieved July 9, 2020, from.
- Centers for Disease Control and Prevention Coronavirus Disease 2019 (COVID-19) 2020, July 26. https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/children.html Retrieved July 26, 2020, from.
- Centers for Disease Control and Prevention Coronavirus Disease 2019 (COVID-19) 2020, October 22. https://www.cdc.gov/mis-c/cases/index.html Retrieved October 26, 2020, from.
- Centers for Disease Control and Prevention Defining childhood obesity. 2020. https://www.cdc.gov/obesity/childhood/defining.html
- Condon E.M., Sadler L.S., Mayes L.C. Toxic stress and protective factors in multi-ethnic school age children: A research protocol. Research in Nursing & Health. 2018;41(2):97–106. doi: 10.1002/nur.21851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corvalán C., Reyes M., Garmendia M.L., Uauy R. Structural responses to the obesity and non-communicable diseases epidemic: Update on the Chilean law of food labelling and advertising. Obesity. 2019;20(3):367–374. doi: 10.1111/obr.12802. [DOI] [PubMed] [Google Scholar]
- Crocker A.F., Smith S.N. Person-first language: Are we practicing what we preach? Journal of Multidisciplinary Healthcare. 2019;12:125–129. doi: 10.2147/JMDH.S140067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davison K.K., Birch L.L. Childhood overweight: A contextual model and recommendations for future research. Obesity Reviews. 2001;2(3):159–171. doi: 10.1046/j.1467789x.2001.00036.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolsen M.R., Crosswell A.D., Prather A.A. Links between stress, sleep, and inflammation: Are there sex differences? Current Psychiatry Reports. 2019;21(2):8. doi: 10.1007/s11920-019-0993-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubey S., Biswas P., Ghosh R., Chatterjee S., Dubey M.J., Chatterjee S.…Lavie C.J. Psychosocial impact of COVID-19. Diabetes & Metabolic Syndrome. 2020;14(5):779–788. doi: 10.1016/j.dsx.2020.05.035. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunford E.K., Popkin B.M., Ng S.W. Recent trends in junk food intake in U.S. children and adolescents, 2003-2016. American Journal of Preventive Medicine. 2020;59(1):49–58. doi: 10.1016/j.amepre.2020.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellulu M.S., Patimah I., Khaza’ai H., Rahmat A., Abed Y. Obesity and inflammation: The linking mechanism and the complications. Archives of Medical Science. 2017;13(4):851–863. doi: 10.5114/aoms.2016.58928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erikson E.H. W. W. Norton, and Company, Inc; 1950. Childhood and society. [Google Scholar]
- Falbe J., Rosner B., Willett W.C., Sonneville K.R., Hu F.B., Field A.E. Adiposity and different types of screen time. Pediatrics. 2013;132(6):e1497–e1505. doi: 10.1542/peds.2013-0887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feeg V.D., Candelaria L.M., Krenitsky-Korn S., Vessey J.A. The relationship of obesity and weight gain to childhood teasing. Journal of Pediatric Nursing. 2014;29(6):511–520. doi: 10.1016/j.pedn.2014.08.011. [DOI] [PubMed] [Google Scholar]
- Fegert J.M., Vitiello B., Plener P.L., Clemens V. Challenges and burden of the coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: A narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child and Adolescent Psychiatry and Mental Health. 2020;14:20. doi: 10.1186/s13034-020-00329-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldstein L.R., Rose E.B., Horwitz S.M., Collins J.P., Newhams M.M., Son M.…Randolph A.G. Multisystem inflammatory syndrome in U.S. children and adolescents. The New England Journal of Medicine. 2020 doi: 10.1056/NEJMoa2021680. NEJMoa2021680. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fore H.H. A wake-up call: COVID-19 and its impact on children’s health and wellbeing. The Lancet. Global Health. 2020;8(7):e861–e862. doi: 10.1016/S2214-109X(20)30238-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frenn M., Kaugars A., Garcia J., Garnier-Villarreal M. Child body fat and body mass index: Which determinants are most important? Western Journal of Nursing Research. 2020;42(8):593–602. doi: 10.1177/0193945919879960. [DOI] [PubMed] [Google Scholar]
- Fruh S.M., Nadglowski J., Hall H.R., Davis S.L., Crook E.D., Zlomke K. Obesity stigma and bias. The Journal for Nurse Practitioners. 2016;12(7):425–432. doi: 10.1016/j.nurpra.2016.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frydrych L.M., Bian G., O’Lone D.E., Ward P.A., Delano M.J. Obesity and type 2 diabetes mellitus drive immune dysfunction, infection development, and sepsis mortality. Journal of Leukocyte Biology. 2018;104(3):525–534. doi: 10.1002/JLB.5VMR0118-021RR. [DOI] [PubMed] [Google Scholar]
- Garasky S., Stewart S.D., Gundersen C., Lohman B.J., Eisenmann J.C. Family stressors and child obesity. Social Science Research. 2009;38(4):755–766. doi: 10.1016/j.ssresearch.2009.06.002. [DOI] [PubMed] [Google Scholar]
- García-Hermoso A., Hormazábal-Aguayo I., Fernández-Vergara O., Izquierdo M., Alonso-Martínez A., Bonilla-Vargas K.J.…Ramírez-Vélez R. Physical fitness components in relation to attention capacity in Latin American youth with overweight and obesity. Scandinavian Journal of Medicine & Science in Sports. 2020;30(7):1188–1193. doi: 10.1111/sms.13649. [DOI] [PubMed] [Google Scholar]
- van Geel M., Vedder P., Tanilon J. Are overweight and obese youths more often bullied by their peers? A meta-analysis on the correlation between weight status and bullying. International Journal of Obesity. 2014;38:1263–1267. doi: 10.1038/ijo.2014.117. [DOI] [PubMed] [Google Scholar]
- Golden S.D., Earp J.A. Social ecological approaches to individuals and their contexts: Twenty years of health education & behavior health promotion interventions. Health Education & Behavior. 2012;39(3):364–372. doi: 10.1177/1090198111418634. [DOI] [PubMed] [Google Scholar]
- Gudzune K.A., Bennett W.L., Cooper L.A., Bleich S.N. Patients who feel judged about their weight have lower trust in their primary care providers. Patient Education and Counseling. 2014;97(1):128–131. doi: 10.1016/j.pec.2014.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagan J.F., American Academy of Pediatrics, Shaw J.S., Duncan P.M. 4th ed. American Academy of Pediatrics; 2017. Bright futures: Guidelines for health supervision of infants, children, and adolescents. [Google Scholar]
- Hemmingsson E. Early childhood obesity risk factors: Socioeconomic adversity, family dysfunction, offspring distress, and junk food self-medication. Current Obesity Reports. 2018;7(2):204–209. doi: 10.1007/s13679-018-0310-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hess A. CNBC; 2020, March 14. Widespread school closures mean 30 million kids might go without meals.https://www.cnbc.com/2020/03/14/widespread-school-closures-mean-30-million-kids-might-go-without-meals.html [Google Scholar]
- Human Rights Watch COVID-19's devastating impact on children. April 9, 2020. https://www.hrw.org/news/2020/04/09/covid-19s-devastating-impact-children
- Jastreboff A.M., Chaplin T.M., Finnie S., Savoye M., Stults-Kolehmainen M., Silverman W.K., Sinha R. Preventing childhood obesity through a mindfulness-based parent stress intervention: A randomized pilot study. The Journal of Pediatrics. 2018;202:136–142. doi: 10.1016/j.jpeds.2018.07.011. (e1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson K.A., Showell N.N., Flessa S., Janssen M., Reid N., Cheskin L.J., Thornton R.L.J. Do neighborhoods matter? A systematic review of modifiable risk factors for obesity among low socio-economic status black and Hispanic children. Childhood Obesity. 2019;15(2):71–86. doi: 10.1089/chi.2018.0044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaakinen P., Kyngäs H., Kääriäinen M. Technology-based counseling in the management of weight and lifestyles of obese or overweight children and adolescents: A descriptive systematic literature review. Informatics for Health & Social Care. 2018;43(2):126–141. doi: 10.1080/17538157.2017.1353997. [DOI] [PubMed] [Google Scholar]
- Kakinami L., Barnett T.A., Séguin L., Paradis G. Parenting style and obesity risk in children. Preventive Medicine. 2015;75:18–22. doi: 10.1016/j.ypmed.2015.03.005. [DOI] [PubMed] [Google Scholar]
- Kent M.P., Dubois L., Kent E.A., Wanless A.J. Internet marketing directed at children on food and restaurant websites in two policy environments. Obesity. 2013;21(4):800–807. doi: 10.1002/oby.20124. [DOI] [PubMed] [Google Scholar]
- Knowlden A.P., Conrad E. Two-year outcomes of the enabling mothers to prevent pediatric obesity through web-based education and reciprocal determinism (EMPOWER) randomized control trial. Health Education & Behavior. 2018;45(2):262–276. doi: 10.1177/1090198117732604. [DOI] [PubMed] [Google Scholar]
- Kochhar R. PEW Research Center; 2020. Hispanic women, immigrants, young adults, those with less education hit hardest by COVID-19 job losses.https://www.pewresearch.org/fact-tank/2020/06/09/hispanic-women-immigrants-young-adults-those-with-less-education-hit-hardest-by-covid-19-job-losses/ retrieved July 11, 2020 from. [Google Scholar]
- Korakas E., Ikonomidis I., Kousathana F., Balampanis K., Kountouri A., Raptis A.…Lambadiari V. Obesity and COVID-19: Immune and metabolic derangement as a possible link to adverse clinical outcomes. American Journal of Physiology, Endocrinology and Metabolism. 2020;319(1):E105–E109. doi: 10.1152/ajpendo.00198.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar S., Kelly A.S. Review of childhood obesity: From epidemiology, etiology, and comorbidities to clinical assessment and treatment. Mayo Clinic Proceedings. 2017;92(2):251–265. doi: 10.1016/j.mayocp.2016.09.017. [DOI] [PubMed] [Google Scholar]
- Lappan S.N., Parra-Cardona J.R., Carolan M., Weatherspoon L. Risk and protective factors associated with childhood obesity in a sample of low-income, single female, parent/guardian households: Implications for family therapists. Family Process. 2020;59(2):597–617. doi: 10.1111/famp.12440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemus B., Mercado F., Bryars T., Mouttapa M., Conkey T., Robertson T. Reflections regarding the social ecological model to address obesity in Southern California youth. California Journal of Health Promotion. 2016;14(3):64–69. [Google Scholar]
- Li M., Mustillo S., Anderson J. Childhood poverty dynamics and adulthood overweight/obesity: Unpacking the black box of childhood. Social Science Research. 2018;76:92–104. doi: 10.1016/j.ssresearch.2018.05.009. [DOI] [PubMed] [Google Scholar]
- Lighter J., Phillips M., Hochman S., Sterling S., Johnson D., Francois F., Stachel A. Obesity in patients younger than 60 years is a risk factor for Covid-19 hospital admission. Clinical Infectious Diseases. 2020 doi: 10.1093/cid/ciaa415. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lohman B.J., Stewart S., Gundersen C., Garasky S., Eisenmann J.C. Adolescent overweight and obesity: Links to food insecurity and individual, maternal, and family stressors. The Journal of Adolescent Health. 2009;45(3):230–237. doi: 10.1016/j.jadohealth.2009.01.003. [DOI] [PubMed] [Google Scholar]
- Love H.E., Schlitt J., Soleimanpour S., Panchal N., Behr C. Twenty years of school-based health care growth and expansion. Health Affairs. 2019;38(5):755–764. doi: 10.1377/hlthaff.2018.05472. [DOI] [PubMed] [Google Scholar]
- Manandhar S., Suksaroj T.T., Rattanapan C. The association between green space and the prevalence of overweight/obesity among primary school children. The International Journal of Occupational and Environmental Medicine. 2019;10(1):1–10. doi: 10.15171/ijoem.2019.1425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mateu A., Pascual-Sanchez A., Martinez-Herves M., Hickey N., Nicholls D., Kramer T. Cyberbullying and post-traumatic stress symptoms in UK adolescents. Archives of Disease in Childhood. 2020;105(10):951–956. doi: 10.1136/archdischild-2019-318716. Epub 2020 Jun 23. PMID: 32576564. [DOI] [PubMed] [Google Scholar]
- Miller A.L., Riley H., Domoff S.E., Gearhardt A.N., Sturza J., Kaciroti N., Lumeng J.C. Weight status moderates stress-eating in the absence of hunger associations in children. Appetite. 2019;136:184–192. doi: 10.1016/j.appet.2019.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NAPNAP. The National Association of Pediatric Nurse Practitioners Prioritizing return to school for children in COVID-19 policy planning. 2020, July 1. https://www.napnap.org/prioritizing-return-school-children-covid-19-policy-planning
- NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390(10113):2627–2642. doi: 10.1016/S0140-6736(17)32129-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden C.L., Fryar C.D., Hales C.M., Carroll M.D., Aoki Y., Freedman D.S. Differences in obesity prevalence by demographics and urbanization in US children and adolescents, 2013-2016. JAMA. 2018;319(23):2410–2418. doi: 10.1001/jama.2018.5158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohri-Vachaspati P., DeLia D., DeWeese R.S., Crespo N.C., Todd M., Yedidia M.J. The relative contribution of layers of the social ecological model to childhood obesity. Public Health Nutrition. 2015;18(11):2055–2066. doi: 10.1017/S1368980014002365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olaya B., Moneta M.V., Pez O., Bitfoi A., Carta M.G., Eke C.…Kovess V. Country-level and individual correlates of overweight and obesity among primary school children: A cross-sectional study in seven European countries. BMC Public Health. 2015;15:475. doi: 10.1186/s12889-015-1809-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ordway M.R., Sadler L.S., Holland M.L., Slade A., Close N., Mayes L.C. A home visiting parenting program and child obesity: A randomized trial. Pediatrics. 2018;141(2) doi: 10.1542/peds.2018-0770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park H.K., Kim J., Shim Y.S. Association between sleep duration and body composition in girls ten to eighteen years of age: A population-based study. Childhood Obesity. 2020;16(4):281–290. doi: 10.1089/chi.2019.0191. [DOI] [PubMed] [Google Scholar]
- Park Y., Gulmann J.M. Understanding disparities in community green accessibility under alternative green measures: A metropolitan-wide analysis of Columbus, Ohio and Atlanta, Georgia. Landscape and Urban Planning. 2020;200(8):10306. doi: 10.1016/j.landurbplan.2020.103806. [DOI] [Google Scholar]
- Parks E.P., Kazak A., Kumanyika S., Lewis L., Barg F.K. Perspectives on stress, parenting, and children’s obesity-related behaviors in black families. Health Education & Behavior. 2016;43(6):632–640. doi: 10.1177/1090198115620418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick S.W., Henkhaus L.E., Zickafoose J.S., Lovell K., Halvorson A., Loch S.…Davis M.M. Well-being of parents and children during the COVID-19 pandemic: A national survey. Pediatrics. 2020 doi: 10.1542/peds.2020-016824. [DOI] [PubMed] [Google Scholar]
- Piaget J. International Universities Press; 1974. The origins of intelligence in children. [Google Scholar]
- Pifer R. HealthcareDive brief. 2020. 27 Million Americans may have lost job-based health insurance due to COVID-19 downturn.https://www.healthcaredive.com/news/27m-americans-may-have-lost-job-based-health-insurance-due-to-covid-19-down/577852/ retrieved July 11, 2020 from. [Google Scholar]
- Puhl R., Peterson J.L., Luedicke J. Motivating or stigmatizing? Public perceptions of weight-related language used by health providers. International Journal of Obesity. 2013;37:612–619. doi: 10.1038/ijo.2012.110. [DOI] [PubMed] [Google Scholar]
- Puhl R.M., Himmelstein M.S., Pearl R.L. Weight stigma as a psychosocial contributor to obesity. The American Psychologist. 2020;75(2):274–289. doi: 10.1037/amp0000538. [DOI] [PubMed] [Google Scholar]
- Puhl R.M., King K.M. Weight discrimination and bullying. Best Practice & Research. Clinical Endocrinology & Metabolism. 2013;27(2):117–127. doi: 10.1016/j.beem.2012.12.002. [DOI] [PubMed] [Google Scholar]
- Reichel C. Harvard Kennedy School, Shorenstein Center on Media, Politics, and Public Policy; 2019. Toxic stress in children has health effects that can last into adulthood.https://journalistsresource.org/studies/society/public-health/aces-toxic-stress-health-research/ [Google Scholar]
- Reilly S.M., Saltiel A.R. Adapting to obesity with adipose tissue inflammation. Nature Reviews. Endocrinology. 2017;13(11):633–643. doi: 10.1038/nrendo.2017.90. [DOI] [PubMed] [Google Scholar]
- Roh E., Song D.K., Kim M.S. Emerging role of the brain in the homeostatic regulation of energy and glucose metabolism. Experimental & Molecular Medicine. 2016;48(3) doi: 10.1038/emm.2016.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosa E.M., Tudge J. Urie Bronfenbrenner’s theory of human development: Its evolution from ecology to bioecology. Journal of Family Theory & Review. 2013;5:243–258. [Google Scholar]
- Rubino F., Puhl R.M., Cummings D.E., Eckel R.H., Ryan D.H., Mechanick J.I., Nadglowski J., Salas X.R., Schauer P.R., Twenefour D., Apovian C.M., Aronne L.J., Batterham R.L., Berthoud H.-R., Boza C., Busetto L., Dicker D., DeGroot M., Eisenberg D.…Dixon J.B. Joint international consensus statement for ending stigma of obesity. Natura Medicine. March 2020:1–13. doi: 10.1038/s41591-020-0803-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rundle A.G., Park Y., Herbstman J.B., Kinsey E.W., Wang Y.C. COVID-19-related school closings and risk of weight gain among children. Obesity. 2020;28(6):1008–1009. doi: 10.1002/oby.22813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santoli J.M., Lindley M.C., DeSilva M.B., Kharbanda E.O., Daley M.F., Galloway L.…Weintraub E. Centers for Disease Control & Prevention; 2020, May 15. Effects of the COVID-19 pandemic on routine pediatric vaccine ordering and administration – United States, 2020.https://www.cdc.gov/mmwr/volumes/69/wr/mm6919e2.htm [DOI] [PubMed] [Google Scholar]
- Schvey N.A., Marwitz S.E., Mi S.J., Galescu O.A., Broadney M.M., Young-Hyman D.…Yanovski J.A. Weight-based teasing is associated with gain in BMI and fat mass among children and adolescents at-risk for obesity: A longitudinal study. Pediatric Obesity. 2019;14(10) doi: 10.1111/ijpo.12538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shekerdemian L.S., Mahmood N.R., Wolfe K.K., Riggs B.J., Ross C.E.…McKiernan C.A., International COVID-19 PICU Collaborative Characteristics and outcomes of children with coronavirus disease 2019 (COVID-19) infection admitted to US and Canadian pediatric intensive care units. JAMA Pediatrics. 2020 doi: 10.1001/jamapediatrics.2020.1948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shonkoff J.P., Garner A.S., Siegel B.S., Dobbins M.I., Earls M.F., Garner A.S.…Wood D.L. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129:e232–e246. doi: 10.1542/peds.2011-2663. [DOI] [PubMed] [Google Scholar]
- Singer K., Lumeng C.N. The initiation of metabolic inflammation in childhood obesity. The Journal of Clinical Investigation. 2017;127(1):65–73. doi: 10.1172/JCI88882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner A.C., Ravanbakht S.N., Skelton J.A., Perrin E.M., Armstrong S.C. Prevalence of obesity and severe obesity in US children, 1999-2016. Pediatrics. 2018;142(3) doi: 10.1542/peds.2018-1916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Small L., Aplasca A. Child obesity and mental health: A complex interaction. Child and Adolescent Psychiatric Clinics of North America. 2016;25(2):269–282. doi: 10.1016/j.chc.2015.11.008. [DOI] [PubMed] [Google Scholar]
- Smith J.D., Fu E., Kobayashi M.A. Prevention and management of childhood obesity and its psychological and health comorbidities. Annual Review of Clinical Psychology. 2020;16:351–378. doi: 10.1146/annurev-clinpsy-100219-060201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sokol R.L., Qin B., Poti J.M. Parenting styles and body mass index: A systematic review of prospective studies among children. Obesity Reviews. 2017;18(3):281–292. doi: 10.1111/obr.12497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spear B.A., Barlow S.E., Ervin C., Ludwig D.S., Saelens B.E., Schetzina K.E., Taveras E.M. Recommendations for treatment of child and adolescent overweight and obesity. Pediatrics. 2007;120(Suppl. 4):S254–S288. doi: 10.1542/peds.2007-2329F. [DOI] [PubMed] [Google Scholar]
- Sprang G., Silman M. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Medicine and Public Health Preparedness. 2013;7(1):105–110. doi: 10.1017/dmp.2013.22. [DOI] [PubMed] [Google Scholar]
- Sunday S., Kabir Z. Impact of carers’ smoking status on childhood obesity in the growing up in Ireland cohort study. International Journal of Environmental Research and Public Health. 2019;16(15):2759. doi: 10.3390/ijerph16152759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thaker V.V., Osganian S.K., deFerranti S.D., Sonneville K.R., Cheng J.K., Feldman H.A., Richmond T.K. Psychosocial, behavioral and clinical correlates of children with overweight and obesity. BMC Pediatrics. 2020;20(1):291. doi: 10.1186/s12887-020-02145-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Guardian Lockdowns around the world bring rise in domestic violence. 2020. https://www.theguardian.com/society/2020/mar/28/lockdowns-world-rise-domestic-violence
- The Ohio State University Extension COCID-19 updates: a message from our 4-H leaders. 2020. https://franklin.osu.edu/program-areas/4-h-youth-development/club-advisor-resources/covid-19-updates
- Timper K., Brüning J.C. Hypothalamic circuits regulating appetite and energy homeostasis: Pathways to obesity. Disease Models & Mechanisms. 2017;10(6):679–689. doi: 10.1242/dmm.026609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Today Can kids attend camp this summer? What newly released guidelines say. 2020, May 18. https://www.today.com/parents/summer-camp-guidelines-released-amid-coronavirus-pandemic-t181786
- Tomiyama A.J., Carr D., Granberg E.M., Major B., Robinson E., Sutin A.R., Brewis A. How and why weight stigma drives the obesity ‘epidemic’ and harms health. BMJ Medicine. 2018;16:123. doi: 10.1186/s12916-018-1116-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services . 2nd ed. 2018. Physical activity guidelines for Americans.https://health.gov/paguidelines/second-edition/pdf/Physical_Activity_Guidelines_2nd_edition.pdf [Google Scholar]
- Van Lancker W., Parolin Z. COVID-19, school closures, and child poverty: A social crisis in the making. The Lancet Public Health. 2020;5(5):e243–e244. doi: 10.1016/S2468-2667(20)30084-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vinkers C.H., van Amelsvoort T., Bisson J.I., Branchi I., Cryan J.F., Domschke K.…van der Wee N. Stress resilience during the coronavirus pandemic. European Neuropsychopharmacology. 2020;35:12–16. doi: 10.1016/j.euroneuro.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vrijheid M., Fossati S., Maitre L., Márquez S., Roumeliotaki T., Agier L.…Chatzi L. Early-life environmental exposures and childhood obesity: An exposome-wide approach. Environmental Health Perspectives. 2020;128(6):67009. doi: 10.1289/EHP5975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfson J.A., Gollust S.E., Niederdeppe J., Barry C.L. The role of parents in public views of strategies to address childhood obesity in the United States. The Milbank Quarterly. 2015;93(1):73–111. doi: 10.1111/1468-0009.12106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization Novel Coronavirus(2019-nCoV) situation report – 51. 2020, July. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf?sfvrsn=1ba62e57_10
- Yuki K., Fujiogi M., Koutsogiannaki S. COVID-19 pathophysiology: A review. Clinical Immunology. 2020;215:108427. doi: 10.1016/j.clim.2020.108427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yusuf Z.I., Dongarwar D., Yusuf R.A., Bell M., Harris T., Salihu H.M. Social determinants of overweight and obesity among children in the United States. International Journal of MCH and AIDS. 2020;9(1):22–33. doi: 10.21106/ijma.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zachariah P., Johnson C.L., Halabi K.C., Ahn D., Sen A.I., Fischer A.…Columbia Pediatric COVID-19 Management Group Epidemiology, clinical features, and disease severity in patients with Coronavirus Disease 2019 (COVID-19) in a children’s hospital in New York City, New York. JAMA Pediatrics. 2020:e202430. doi: 10.1001/jamapediatrics.2020.2430. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]