Abstract
Background:
Respiratory system involvement and fever are considered as a cardinal manifestation of Covid-19 infection for the screening of case detection. We (India) are into the fourth month of Covid-19 and cases are still rising, this could mean that fever and respiratory symptoms may not be the only initial symptoms. Therefore, we intend to investigate whether neurological symptoms can precede the cardinal symptoms.
Methods:
Totally, 391 Covid-19 RTPCR positive hospitalized patients were enrolled. All included subjects were presented with a questionnaire pertaining to systemic symptoms. For analysis of the chronology of symptoms, the study population was sub-grouped according to onset of their systemic involvement e.g., (1) Fever (2) Respiratory symptoms (3) Neurological symptoms (4) Gastrointestinal symptoms.
Results:
New-onset neurological symptoms were found in 106 (27.1%) out of 391 patients irrespective of their chronology to the onset of other symptoms. Of these 106 patients, altered taste (33.1%), altered smell (24.5%), and headache (22.6%) were the most common neurological symptoms. However, 38 (9.7%) subjects recognized neurological symptoms, as the initial manifestation of their illness. Mean duration of neurological symptoms before the onset of respiratory symptoms or fever was 2 ± 1.57 days.
Conclusion:
New-onset headache, altered taste, and smell were the most common neurological symptoms. In the context of the current pandemic, a high index of suspicion should be kept in patients presenting with these symptoms even in the absence of fever and respiratory symptoms. To the best of our knowledge, this is the first study from India comparing chronology of neurological symptoms with cardinal symptoms.
Keywords: Coronavirus, Covid-19, pandemic, screening of Covid-19, neurological manifestations in Covid-19
INTRODUCTION
Novel coronavirus infection is known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV2). The novel coronavirus (Covid-19) outbreak originated from Wuhan city, China in Dec. 2019. Chinese authorities reported unusual cases of pneumonia of undetermined etiology.[1,2] World health organization (WHO) declared it a pandemic on 11 March 2020.[3]
Respiratory system involvement (cough, throat pain, breathlessness) and fever are considered as a cardinal early manifestation of Covid-19 infection, and they are being used as a screening tool for case detection in a given individual.[4,5] We (India) are into the fourth month of Covid-19 and cases are still on rising, this could mean that fever and respiratory symptoms may not be the only initial symptoms. Therefore, we intend to investigate the possible early neurological symptoms and whether these symptoms can precede the cardinal respiratory symptoms.
MATERIAL AND METHODS
This observational cross-sectional study was conducted in the tertiary care teaching hospital of central India. The hospital is designated as COVID 19 hospital (code Red with bed capacity 1145 reserved for Covid 19 patients), for the care of hospitalized patients who have positive Real-time reverse transcription-polymerase chain reaction (RTPCR) as per guidelines. All RTPCR Positive hospitalized patients of age more than 12 years were included. Patients with negative RTPCR (report not confirmed or pending), unconscious and patient on the ventilator (unable to communicate), patients of age <12 years, and non-consenting patients were excluded. 391 Patients were enrolled from April 2020 to May 2020 (study duration 30 days). One of the investigators (RG) presented a questionnaire incorporating information of patients, symptoms pertaining to systemic involvement including respiratory, neurological, and gastrointestinal systems. The chronology of the onset of different systemic symptoms was recorded cautiously. Focused neurological examination was done as and when required. New-onset neurological symptoms; that are neurological symptoms appearing within ±7 days of Covid-19 diagnosis were taken into consideration. Preexisting neurological symptoms were not considered. The study was approved by the Institutional Scientific and Research Committee.
All subjects were sub-grouped into two as per those having new-onset neurological symptoms and without neurological symptoms. A comparison of the demographic profile of two sub-groups was analyzed according to age, gender, religion, and comorbidities [Table 1].
Table 1.
Demographic profile of study population
| Variable | Total n=391 (100%) | Significance | Neurological (n=106) | Non Neurological (n=285) | Significance | OR (95% CI) |
|---|---|---|---|---|---|---|
| Demography | ||||||
| Age (in years) | ||||||
| <50 yrs | 183 (46.80%) | 0.07 (ns)# | 16 (8.74%) | 167 (91.26%) | 0.001* | |
| >50 yrs | 208 (53.20%) | 90 (43.27%) | 118 (56.73%) | |||
| Gender | ||||||
| Male | 241 (61.6%) | <0.0001 (s)# | 62 | 179 | 0.48* | 0.83 (0.52-1.3) |
| Female | 150 (38.4%) | 44 | 106 | |||
| Religion | ||||||
| Hindu | 243 (62.1%) | <0.0001 (s)# | ||||
| Non-Hindu | 148 (37.8%) | |||||
| Comorbidities | ||||||
| T2DM | ||||||
| Yes | 91 (23.2%) | 50 (54.9%) | 41 (45.05%) | <0.0001* | 5.3 (3.2-8.8) | |
| No | 300 (76.72%) | 56 (18.66%) | 244 (81.33%) | |||
| HTN | ||||||
| Yes | 54 (13.8%) | 30 (55.5%) | 24 (44.44%) | <0.0001* | 4.3 (2.3-7.7) | |
| No | 337 (86.2%) | 76 (22.55%) | 261 (77.44%) |
# Comparison on means * Fischer exact test
For analysis of the chronology of symptoms, the study population was sub-grouped according to the onset of their systemic involvement. The study population (n = 391) was categorized into 4 subgroups, (1) fever, (2) respiratory symptoms, (3) new-onset neurological symptoms, and (4) new-onset gastrointestinal symptoms [Table 2].
Table 2.
Frequency of initial systemic symptoms
| Initial symptoms | Total patients n=391 (100%) |
|---|---|
| Fever n=183 (46.8%) | |
| Initial Respiratory symptoms (new onset) n=122 (31.2%) | |
| Cough | 76 (19.4%) |
| Throat pain | 36 (9.2%) |
| Breathlessness | 9 (2.3%) |
| Initial Neurological symptoms (new onset) n=38 (9.7%) | |
| Headache | 15 (3.8%) |
| Altered taste | 8 (2.0%) |
| Altered smell | 5 (1.3%) |
| Vertigo | 4 (1.0%) |
| Myalgia | 4 (1.0%) |
| Insomnia | 2 (0.5%) |
| Initial Gastrointestinal symptoms (new onset) n=48 (12.3%) | |
| Anorexia | 34 (8.7%) |
| Abdominal pain | 10 (2.5%) |
| Diarrhea | 4 (1.0%) |
The statistical analysis was done using software like Medcalc, Graphpad, Excel 2010, and SPSS version 17.0 Trial. Results of continuous data are presented as Mean ± Standard Deviation (SD) and the results of the categorical measurements are given as a percentage (%). As and when required, Pearson's Chi-Square test, two-tailed Fisher Exact test, and comparison of proportions were deployed to know the association between the variable. The probability value P ≤ 0.05 and OR > 1 (at 95% CI) was considered significant.
RESULTS
Demographic profile of patients
The mean age of the study group (n = 391) was 49.07 ± 15.74 years. Males constitutes 61% (n = 241) of total enrolled patients. On comparing demographic profiles significant (P < 0.0001) difference was found between genders, religion, with male and Hindu predominance, while the difference of age did not reach statistical significance. Out of 391 subjects, new-onset neurological symptoms were detected in 106 (27.1%) while 285 (72.8%) had no neurological complaints. On comparing the demographic profile and comorbidities among two subgroups, subjects with age 50, presence of Diabetes mellitus, and hypertension were found to have significantly higher odds of having neurological symptoms with P values of <0.001, <0.0001, and <0.0001, respectively [Table 1].
Fever
Out of the total study population (n = 3 91) subjects, 320 (81.9%) reported having a fever during their course of illness, while remaining 71 (18.2%) did not have a fever any time during the course of their illness. Out of 71 subjects, those did not have a fever, 53 (74.6%) had respiratory symptoms, 21 (29.6%) had new-onset neurological symptoms and 27 (38.1%) had new-onset gastrointestinal symptoms during the course of their illness.
Respiratory symptoms
Out of the total study population (n = 391) subjects, 312 (79.8%) reported having respiratory (cough, throat pain, and breathlessness) symptoms while remaining 79 (20.2%) subjects did not have any respiratory symptoms during the course of their illness. Out of 79 subjects, those did not have respiratory symptoms, 74 (93.7%) had fever, 18 (22.8%) had new-onset neurological symptoms, and 31 (39.3%) had new-onset gastrointestinal symptoms.
Neurological symptoms
Neurological symptoms were found in 106 (27.1%) out of 391 patients irrespective of their onset to other symptoms. Of these 106 patients, altered taste (n = 35, 33.1%), altered smell (n = 26, 24.5%), and headache (n = 24, 22.6%) were the most common neurological symptoms, followed by vertigo (n = 20, 18.8%), myalgia (n = 20, 18.8%), cognitive problems (n = 15, 14.2%), insomnia (n = 8, 7.5%), sensory disturbances (n = 8, 7.5%), tinnitus (n = 2, 1.8%), tremor (n = 2, 1.8%), and left hemiparesis (n = 1, 0.9%) were reported less frequently [Figure 1].
Figure 1.
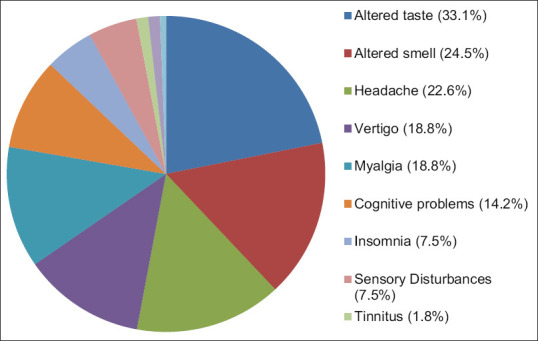
Spectrum of neurological symptoms
One of our patients had an acute ischemic stroke within seven days of onset of fever. She was 55 years female who developed left hemiparesis on the third day of hospitalization. Her MRI brain showed lacunar infarct in Right subcortical white matter.
Out of a total of 106 patients with neurological symptoms, 15 patients reported cognitive changes. Among them, common symptoms reported were, decreased attention, agitation, depressed mood. Increased somnolence to drowsiness was reported in seven patients, those who had impaired blood gases or serum electrolytes and requiring supportive oxygen inhalation.
Two patients reported new-onset hand tremors during their illness. Both patients had symmetrical, intention action tremors, without other cerebellar features. Eight patients reported new-onset positive sensory symptoms (burning, crawling, and pins and needles) at feet.
Gastrointestinal symptoms
Gastrointestinal symptoms were present in 95 (24.3%) patients irrespective of their onset to other symptoms. Anorexia (n = 68, 17.5%) was most common among them, followed by abdominal pain (n = 17, 4.3%) and diarrhea (n = 10, 2.5%).
The laboratory findings of the patient cohort have been described in Table 3. Among patients with neurological findings, leukopenia was found in 7.55%, leukocytosis was seen in 15.74%, neutropenia was found in 1.89%, neutrophilia was found in 33.33%, lymphopenia was found in 33.01% and lymphocytosis was found in 4.72% patients. In the total population, most common lab derangement was raised ESR (30.9%), followed by raised Ferritin (10.5%), and then raised CRP (9.9%).
Table 3.
Laboratory parameters
| Laboratory parameter | Median/Range |
|---|---|
| White blood cell count (4,000-11,000/cmm) | 6,500/cmm (600-20,900) |
| Neutrophil count (40-70% of WBC count) | 63% (30-94) |
| Lymphocyte count (20-40% of WBC count) | 27% (1-68) |
| Ferritin (10-291 ng/ml) | 369.9 ng/ml (3.65-72,000) |
| Lactate dehydrogenase (313-618 IU/L) | 296 IU/L (109-3,475) |
| C reactive protein (<0.06 mg/dl) | 1.2 mg/dl (0.6-4.8) |
| Erythrocyte sedimentation rate (0-9 mm/hr) | 16 mm/hr (2.6-45) |
| D- dimer (>250 mg/L) | 600 mg/L (200-71,000) |
Initial symptoms chronology
For analysis of the chronology of symptoms, the study population was sub-grouped according to the onset of their systemic involvement. The study population (n = 391) was categorized into 4 subgroups, (1) fever, (2) respiratory symptoms, (3) new-onset neurological symptoms, and (4) new-onset gastrointestinal symptoms as shown in Table 2.
Fever and respiratory symptoms were the initial symptoms in 183 (46.8%), and 122 (31.2%) patients, respectively. However, 38 (9.7%) subjects recognized neurological symptoms, 48 (12.3%) subjects recognized gastrointestinal symptoms, as the earliest manifestation of their illness, even before the onset of fever and respiratory symptoms [Table 2].
The mean duration of neurological symptoms before respiratory symptoms or fever was 2 ± 1.57 days and of gastrointestinal symptoms was 2.5 ± 1.25 days.
DISCUSSION
Fever and respiratory system involvement are the cardinal manifestations of Covid 19 infection.[4,5,6] Wang et al. reported fever in 98.6%, dry cough in 59.4%, and dyspnea in 31.2% of patients, in his retrospective analysis of 138 patients.[7] Other recent studies also reported fever and cough to be the most common symptom.[6,8] We found fever in 318 (81.2%), cough in 238 (60.9%), throat pain in 150 (38.4%), and breathlessness in 38 (9.7%) patients. Our results are comparable with previous data except for fewer patients with breathlessness. The difference may be due to exclusion of patients with severe disease who were unable to answer the questionnaire.
The disease affected all age groups; however, disease severity varies in different age groups. Wei-Jie Guan et al. reported the mean age of patients to be 47 years with males accounting for 58.1% in a study of 1099 patients.[4] Similar results were shown by Huang et al. with the median age of 49.0 years (n = 41).[8] Mao et al. reported the mean age to be 52.7 years (n = 214).[6] Our results were comparable with other studies with a mean age of 49.0 years and males constitute 61% of the study population.
Similarly, various studies have reported comorbidities especially diabetes mellitus leads to severe illness and poor outcomes.[4,9,10,11] We compared demographic profile and a subset of subjects having new-onset neurological symptoms and found that subjects of age >50 years, presence of diabetes mellitus, and hypertension lead to significantly increased involvement of the neurological system.
Recently (Mao et al.)[6] a study from china reported neurological symptoms in Covid-19-infected patients (n = 214). They found 36.4% of patients had neurological manifestations with headache, dizziness, decreased consciousness, olfactory dysfunction, and gustatory dysfunction being the most common. In our study (n = 391) we found 27.1% of patients had neurological symptoms with altered taste (8.9%), altered smell (6.6%) followed by headache (6.1%), and vertigo (5.1%) being the most common.
Lechien et al. did a prospective study in 417 patients and reported altered smell in 86% of 417 patients.[12] American Academy of otolaryngology-head neck surgery has also reported anosmia and dysgeusia as significant symptoms associated with Covid-19.[13] Loss of taste and smell can be a marker of Covid-19.[14]
Few recent studies have highlighted the importance of early gastrointestinal symptoms in the screening of Covid-19 patients.[7,15,16] However, we could not find any previous study reporting the chronology of neurological symptoms with respect to respiratory symptoms and fever. In our study 38 (9.7%) patients had an initial presentation with neurological symptoms, which preceded typical fever and respiratory symptoms. New-onset headache, altered taste, and altered smell were common initial complaints before the fever and cough.
In our patient population, lymphopenia was the most consistent derangement found in complete hemogram in patients with neurological findings (33.01%). This finding was consistent with the results found by Mao et al.[6]
CONCLUSION
As an early manifestation of disease non-respiratory symptoms were undermined. Various researchers have raised concerns about the same, we investigated the same and found neurological manifestation can precede the cardinal manifestations in the substantial number of patients. Neurological symptoms especially new-onset headache, altered taste, and smell are the initial presenting symptoms in a large chunk of patients. In the context of the current pandemic, a high index of suspicion should be kept in patients presenting with these symptoms even in the absence of fever and respiratory symptoms. New-onset headache, altered smell, and taste along with new-onset gastrointestinal symptoms should be considered as an early screening tool along with fever and cough for the screening of Covid-19. Keeping this holistic knowledge of the spectrum of neurological symptoms we can get hold and will halt the chain of transmission.
To the best of our knowledge, this is the first study comparing chronology of neurological symptoms with cardinal fever and respiratory symptoms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Zhu N, Zhang D, Wang W, Li X, Yang Bo, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–33. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adhikari S, Meng S, Wu Y, Mao Y, Ye Rui, Wang Q, et al. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: A scoping review. Infect Dis Poverty. 2020;9:29. doi: 10.1186/s40249-020-00646-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO Director-General's opening remarks at the media briefing on COVID 19-11 March 2020. [Last accessed on 2020 Apr 22]. Available from: https://wwwwhoint/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing -on-covid-19-11-march-2020 .
- 4.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of 2019 novel coronavirus infection in China. N Engl J Med. 2020;382:1708–20. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yang Y, Lu Q, Liu M, Wang Y, Zhang A, Jalali N, et al. Epidemiological and clinical features of the 2019 novel coronavirus outbreak in China. MedRxiv. 2020. https://doiorg/101101/2020021020021675 .
- 6.Mao L, Wang M, Chen S, He Q, Chang J, Hong C, et al. Neurological manifestations of hospitalized patients with COVID-19 in Wuhan, China: A retrospective case series study. MedRxiv. 2020. https://doiorg/101101/2020022220026500 .
- 7.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 Novel Coronavirus infected Pneumonia in Wuhan, China. JAMA. 2020;323:1061–9. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang JJ, Dong X, Cao YY, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China [published online ahead of print, 2020 Feb 19] Allergy. 2020 doi: 10.1111/all.14238. doi: 101111/all 14238. [DOI] [PubMed] [Google Scholar]
- 10.Gupta R, Ghosh A, Singh AK, Misra A. Clinical considerations for patients with diabetes in times of COVID-19 epidemic. Diabetes Metab Syndr. 2020;14:211–2. doi: 10.1016/j.dsx.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, Ji R, et al. Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: A systematic review and meta-analysis. Int J Infect Dis. 2020;94:91–5. doi: 10.1016/j.ijid.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lechien J, Chiesa-Estomba C, De Siati D, Horoi M, Le Bon S, Rodriguez A. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): A multicenter European study. Eur Arch Otorhinolaryngol. 2020;2020:1–11. doi: 10.1007/s00405-020-05965-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Anosmia: new! COVID-19 anosmia reporting tool open to all clinicians. American Academy of Otolaryngology-Head and Neck Surgery. [Last accessed on 2020 Apr 1]. Available from: https://wwwentnetorg/content/coronavirus-disease-2019-resources .
- 14.ENT UK. Loss of sense of smell as marker of COVID-19 infection March30, 2020. Available from: https://wwwentukorg/sites/default/files/files/Loss%20of%20sense%20of%20smell%20as%20marker%20of%20COVIDpdf 101016/jdsx 2020 .
- 15.Pan L, Mu M, Yang P, Sun Y, Wang R, Yan J, et al. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: A descriptive, cross-sectional, multicenter study. Am J Gastroenterol. 2020;115:766–73. doi: 10.14309/ajg.0000000000000620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mao R, Qiu Y, He J-S, Tan JY, Hua Li X, Liang J, et al. Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: A systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2020;5:667–78. doi: 10.1016/S2468-1253(20)30126-6. [DOI] [PMC free article] [PubMed] [Google Scholar]


