Sir,
We report a 27-year-old female with history of cocaine abuse and symptomatic left internal carotid artery (ICA) involvement. High-resolution intracranial vessel wall imaging (VWI) showed concentric wall thickening and enhancement of the left ICA. Cocaine is a powerful vasoconstrictor and cocaine-related neurotoxicity is associated with ischemic stroke, brain hemorrhage, and vasospasm. Cocaine-induced vascular abnormalities have been previously reported and only a few describing changes of vasculitis.[1,2,3,4,5] Recent reports of VWI on magnetic resonance imaging (MRI) and vessel wall biopsy present a new way to confirm a possible vasculitis.[4]
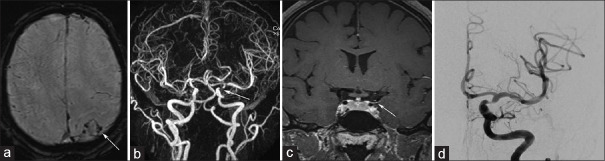
A 27-year-old female with polysubstance abuse initially admitted for severe headache. Head CT and MRI scans showed left fronto-parietal SAH [Figure 1a] with no acute infarct and mass. Magnetic resonance angiography (MRA) showed focal severe stenosis of left supraclinoid ICA [Figure 1b] with no other arterial or venous abnormality. High-resolution T1-VWI with gadolinium showed focal concentric wall thickening and enhancement of the left ICA [Figure 1c]. Diagnostic subtraction angiogram (DSA) showed severe flow-limiting stenosis of the supraclinoid left ICA [Figure 1d] and negative for aneurysm or any other vascular malformation. She was febrile, with a tachycardia and leukocytosis (sepsis). cerebrospinal fluid (CSF) showed RBCs with no leukocytes and protein. Meningitis panel was negative. TEE was negative for endocarditis. Blood cultures positive for Stenotrophomonas maltophilia (bacteremia), most likely from her intravenous drug abuse. Overall, these findings were considered secondary to drug-induced vasculitis, in the setting of polysubstance abuse. She was discharged with antibiotics and scheduled for follow-up diagnostic angiogram and possible balloon angioplasty with stenting in case the stenosis persists after drug discontinuation. After 2 months, she was again admitted with complaints of episodic right-sided numbness, weakness, and loss of consciousness. She denied any confusion, bladder/bowel incontinence, and seizure. Her NIHSS score was zero. She admitted continued using of methamphetamine and intravenous cocaine. Laboratory testing showed a urinary drug screen of positive for cocaine and opiates. Lab report for C-reactive protein, rheumatoid factor, antineutrophil cytoplasm antibody (ANCA) were negative. Follow-up MRI showed focal left fronto-parietal encephalomalacia and persistent focal high-grade stenosis of the left ICA. On follow-up DSA, there was no change in the degree of stenosis and balloon-assisted angioplasty of the supraclinoid left ICA, resulted improvement in the degree of stenosis. In view of clinical presentation, lab investigation, and characteristic imaging findings, a probable diagnosis of cocaine-induced cerebral vasculitis was considered. The patient was treated with nifedipine for blood pressure control and was discharged with follow-up drug abuse counseling. Even though a biopsy confirmation was not obtained, the imaging findings support a component of underlying vessel wall inflammation.
Figure 1.
A 27-year-old woman with history of cocaine abuse, presenting with severe headache. Axial SWI (a) image depict multiple subarachnoid hemorrhage foci in left fronto-parietal lobes (white arrow). 3D-TOF angiography with coronal MIP reconstruction (b) shows absence of flow in the tip of the left internal carotid artery (white arrow). Coronal (c) T1-vessel wall image with contrast depict circumferential wall thickening and enhancement in the corresponding vessel (arrow). Digital subtraction angiography image (d) also demonstrates the left supraclinoid ICA stenosis
Cocaine vasculopathy is a multisystem disease affecting brain, heart, and lung.[6] Cocaine with levamisole adulteration increases euphoric effects of the former and act as an immunomodulatory agent. Pathogenesis is related not only to potent vasoconstriction effects but also to the cocaine-levamisole ability to induce ANCA-like vasculitis.[7] Therefore, radiologic features of cocaine vasculitis may be undistinguishable from other autoimmune vasculitis.[8] Cocaine-induced cerebral vasculitis has been described by the few case reports and diagnosis is mainly based on the angiographic findings in the absence of markers for the primary CNS vasculitis (PCNSV) and presence of cocaine abuse. Exact underlying mechanism is still unknown; however, few studies have shown apoptotic effect of cocaine on smooth muscle cell and leukocyte migration, resulting vessel wall inflammation.[6] Yoon et al. supported the hypothesis that cerebral vasoconstriction due to acute cocaine exposure is via endothelin-1 release and endothelin receptor antagonists may be of therapeutic benefit.[1] Chronic cocaine use results in repeated endothelial damage and subsequent atherosclerotic changes. Late angiographic findings in such patients might attributable to both vasoconstrictive and inflammatory effects of cocaine.[6,9] In such cases, VWI is a useful diagnostic tool to detect vascular inflammation as wall thickening and enhancement. In a case report of cocaine abuse, Han et al. showed the acute left MCA infarct, concentric luminal stenosis, and enhancement of left ICA.[9]
Vasculopathy is a general term used to describe any disease affecting the vessels and diagnosis is not pathologically established. Vasculitis, on the other hand, is a more specific term and is defined as inflammation of the wall of a blood vessel. However, the term vasculopathy is also used for “vasculitis.” Cocaine-induced vascular changes may also mimic reversible cerebral vasoconstriction syndromes (RCVS) or PCNSV but unlike RCVS, it demonstrates arterial wall enhancement.[4,9] Mandell et al.[4] reports preliminary results regarding the difference between RCVS and PCNSV using VWI. Three RCVS patients showed reversible arterial narrowing and wall thickening without enhancement—a finding consistent with transient vasoconstriction. In three CNS vasculitis and one cocaine vasculopathy patients, VWI demonstrated circumferential arterial wall thickening and enhancement.[4] PCNSV is a diagnosis of exclusion with abnormal CSF in more than 90%. Our patient's imaging findings of persistent left ICA focal stenosis and vessel wall enhancement supports the diagnosis of cocaine-induced vasculitis. Although cocaine-related changes reported as vasculopathy, the presence of isolated case reports with enhancement on VWI and biopsy confirmation of inflammation may support the underlying component of vasculitis, even if transient.
This case highlights the importance of high-resolution VWI in differentiating cocaine-induced vasculitis from other mimics such as RCVS and primary CNS vasculitis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Yoon SH, Zuccarello M, Rapoport RM. Acute cocaine induces endothelin-1-dependent constriction of rabbit basilar artery. Endothelium. 2007;14:137–9. doi: 10.1080/10623320701421644. [DOI] [PubMed] [Google Scholar]
- 2.Gradon JD, Wityk R. Diagnosis of probable cocaine-induced cerebral vasculitis by magnetic resonance angiography. South Med J. 1995;88:1264–6. doi: 10.1097/00007611-199512000-00015. [DOI] [PubMed] [Google Scholar]
- 3.Krendel DA, Ditter SM, Frankel MR, Ross WK. Biopsy-proven cerebral vasculitis associated with cocaine abuse. Neurology. 1990;40:1092–2. doi: 10.1212/wnl.40.7.1092. [DOI] [PubMed] [Google Scholar]
- 4.Mandell DM, Matouk CC, Farb RI, Krings T, Agid R, terBrugge K, et al. Vessel wall MRI to differentiate between reversible cerebral vasoconstriction syndrome and central nervous system vasculitis: Preliminary results. Stroke. 2012;43:860–2. doi: 10.1161/STROKEAHA.111.626184. [DOI] [PubMed] [Google Scholar]
- 5.de Souza A, Desai PK, de Souza RJ. Acute multifocal neuropathy following cocaine inhalation. J Clin Neurosci. 2017;36:134–6. doi: 10.1016/j.jocn.2016.10.015. [DOI] [PubMed] [Google Scholar]
- 6.Bachi K, Mani V, Jeyachandran D, Fayad ZA, Goldstein RZ, Alia-Klein N. Vascular disease in cocaine addiction. Atherosclerosis. 2017;262:154–62. doi: 10.1016/j.atherosclerosis.2017.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brunt TM, van den Berg J, Pennings E, Venhuis B. Adverse effects of levamisole in cocaine users: A review and risk assessment. Arch Toxicol. 2017;91:2303–13. doi: 10.1007/s00204-017-1947-4. [DOI] [PubMed] [Google Scholar]
- 8.Berman M, Paran D, Elkayam O. Cocaine-induced vasculitis. Rambam Maimonides Med J. 2016:7. doi: 10.5041/RMMJ.10263. doi: 105041/RMMJ10263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Han JS, Mandell DM, Poublanc J, Mardimae A, Slessarev M, Jaigobin C, et al. BOLD-MRI cerebrovascular reactivity findings in cocaine-induced cerebral vasculitis. Nature Clin Pract Neurol. 2008;4:628–32. doi: 10.1038/ncpneuro0918. [DOI] [PubMed] [Google Scholar]