Abstract
Background
Patients with cardiovascular disease (CVD) and type 2 diabetes (DM2) have a high residual risk for experiencing a major adverse cardiac event. Dysregulation of epigenetic mechanisms of gene transcription in innate immune cells contributes to CVD development but is currently not targeted by therapies. Apabetalone (RVX-208) is a small molecule inhibitor of bromodomain and extra-terminal (BET) proteins—histone acetylation readers that drive pro-inflammatory and pro-atherosclerotic gene transcription. Here, we assess the impact of apabetalone on ex vivo inflammatory responses of monocytes from DM2 + CVD patients.
Results
Monocytes isolated from DM2 + CVD patients and matched controls were treated ex vivo with apabetalone, interferon γ (IFNγ), IFNγ + apabetalone or vehicle and phenotyped for gene expression and protein secretion. Unstimulated DM2 + CVD monocytes had higher baseline IL-1α, IL-1β and IL-8 cytokine gene expression and Toll-like receptor (TLR) 2 surface abundance than control monocytes, indicating pro-inflammatory activation. Further, DM2 + CVD monocytes were hyper-responsive to stimulation with IFNγ, upregulating genes within cytokine and NF-κB pathways > 30% more than control monocytes (p < 0.05). Ex vivo apabetalone treatment countered cytokine secretion by DM2 + CVD monocytes at baseline (GROα and IL-8) and during IFNγ stimulation (IL-1β and TNFα). Apabetalone abolished pro-inflammatory hyper-activation by reducing TLR and cytokine gene signatures more robustly in DM2 + CVD versus control monocytes.
Conclusions
Monocytes isolated from DM2 + CVD patients receiving standard of care therapies are in a hyper-inflammatory state and hyperactive upon IFNγ stimulation. Apabetalone treatment diminishes this pro-inflammatory phenotype, providing mechanistic insight into how BET protein inhibition may reduce CVD risk in DM2 patients.
Keywords: Bromodomain, Transcription regulation, Innate immune response, Cardiovascular, Apabetalone
Background
Low-density lipoprotein cholesterol (LDL-C) lowering is the key strategy to prevent cardiovascular disease (CVD). However, even a substantial reduction in LDL-C still leaves patients at a significant residual risk of cardiovascular adverse events. Amongst others, type 2 diabetes mellitus (DM2) is recognized as a contributor to CVD risk [1]. This comorbidity is likely caused by organ exposure to chronic systemic low-grade inflammation caused by elevated circulating levels of cytokines IL-6 and IL-1β, glucose, free fatty acids and reactive oxygen species (ROS) [2–6]. Such a microenvironment favours monocyte infiltration into the arterial wall, where these cells differentiate into macrophages that contribute to initiation and progression of atherosclerosis. Ultimately, macrophage activity in atherosclerotic plaque precipitates atherothrombosis and clinical cardiovascular events [7].
Monocyte activity is not restricted to the arterial wall as circulating monocytes are also a major source of pro-inflammatory and pro-oxidant factors [7]. In fact, monocytes from patients with advanced atherosclerosis and/or hypercholesterolemia are hyper-responsive and therefore produce more pro-inflammatory cytokines, such as interleukin (IL) 6, IL-1β and TNFα [8–10]. This pro-inflammatory state is partially ascribed to hypercholesterolemia, which reprograms myeloid progenitors in the bone marrow to produce hyperactive monocytes and macrophages in experimental atherosclerosis models [11–13]. The resulting “immunological memory” is encoded by epigenetic changes to chromatin in the form of DNA methylation and histone post-translational modification [14]. The contribution of histone marks to persistent immune cell activation has been demonstrated in atherosclerotic mouse models [15, 16], in human monocytes isolated from DM2 and CVD patients’ blood or from atherosclerotic plaques [9, 10, 17–19]. This evidence of widespread epigenetic dysregulation in activated immune cells opens the window for epigenetic regulators as therapeutic agents in DM2 and CVD [14].
Bromodomain and extraterminal (BET) proteins (BRD2, BRD3, BRD4 and BRDT) are histone acetylation “readers” generally linked to the induction of gene transcription [20]. BET proteins are recruited to gene enhancers and promoters via direct binding to acetylated chromatin or to acetylated transcription factors, such as the nuclear factor κ-light-chain-enhancer of activated B cells (NF-κB) and the signal transducer and activator of transcription (STAT) [21–25]. Once chromatin-bound, BETs recruit chromatin remodeling and transcription elongation factors, leading to activation of RNA polymerase II and transcription of proximal genes [26]. Since BET proteins play a critical role in transcription of cytokine response genes involved in inflammation, lipid metabolism and vascular function [23, 27–30], inhibiting their activity could prove beneficial for the treatment of chronic inflammatory and metabolic diseases.
Apabetalone (RVX-208) is an orally available small molecule BET inhibitor (BETi) that mimics the endogenous ligand of BET proteins, the acetylated lysine residue. Apabetalone preferentially binds to the second of two conserved BET protein bromodomains (with > 20-fold higher affinity) [31–33], countering BET protein recruitment to chromatin. Consequently, apabetalone inhibits transcription of BET-dependent genes [31, 34]. In vitro treatment with apabetalone reduces pro-inflammatory gene expression in cellular models of atherosclerosis, including endothelial cells [34, 35], monocytes [34] and vascular smooth muscle cells [36]. Apabetalone also reduces vascular inflammation and atherosclerosis in mouse models [23, 35]. These data suggest that apabetalone could correct the pro-inflammatory phenotype of innate immune cells characteristic of DM2 and CVD.
Here, we demonstrate that monocytes isolated from patients with DM2 and CVD (DM2 + CVD) have an enhanced pro-inflammatory phenotype as compared to matched controls. Moreover, challenging DM2 + CVD monocytes ex vivo with interferon gamma (IFNγ), a key cytokine that triggers monocyte differentiation into the pro-inflammatory macrophage M1 subtype [37], provokes a hyperactive transcriptional response as compared to controls. Ex vivo apabetalone treatment diminishes this hyper-inflammatory state, suggesting that BET protein inhibition can mitigate monocyte-driven inflammation in patients with high residual risk for major adverse cardiovascular events.
Results
Apabetalone suppresses pro-inflammatory cytokine secretion in monocytes from DM2 + CVD patients
For this study, we recruited patients with DM2 and stable CVD (DM2 + CVD) (n = 14), and age- and gender-matched control subjects (n = 12) (Table 1). DM2 + CVD patients, on standard of care including insulin and/or statins, had higher glucose levels (mean 8.05, [7.30–10.15]) than controls (mean 5.35, [5.20–5.60]). They also had increased systolic blood pressure (142.93 (13.38)), elevated triglycerides levels (1.39, [1.13–1.70]), and reduced HDL levels (1.31 (0.22)). Control subjects were not on any medication.
Table 1.
Baseline clinical characteristics of enrolled subjects
| Clinical characteristics | DM2 + CVD (n = 14) | Controls (n = 12) | p value |
|---|---|---|---|
| Age | 68.39 (5.08) | 68.09 (5.16) | 0.9 |
| Gender (male %) | 7 (50) | 8 (66.7) | 0.7 |
| BMI (mean (SD)) | 31.06 (6.85) | 26.71 (5.66) | 0.09 |
| Lifestyle | |||
| Current smoker | 0 (0) | 0 (0) | 1 |
| Former smoker | 7 (50) | 6 (50.0) | 1 |
| Past smoker | 7 (50) | 6 (50.0) | 1 |
| Pack-years (mean (SD)) | 9.50 [0–45] | 4.00 [0–10.5] | 0.06 |
| Systolic BP (mean (SD)) | 142.93 (13.38) | 127.5 (15.21) | 0.01 |
| Medical history | |||
| AP (%) | 7 (50) | 0 (0) | 0.02 |
| MI (%) | 4 (28.6) | 0 (0) | 0.1 |
| CVA (%) | 2 (14.3) | 0 (0) | 0.5 |
| PAD (%) | 6 (42.9) | 0 (0) | 0.03 |
| CRP (median [IQR]) | 1.50 [1.30–3.15] | 1.35 [0.85–2.02] | 0.3 |
| Leukocytes (mean (SD)) | 6.59 (1.35) | 5.57 (1.65) | 0.1 |
| Monocytes (mean (SD)) | 0.56 (0.17) | 0.50 (0.13) | 0.4 |
| Glucose (median [IQR]) | 8,05 [7.30–10.15] | 5.35 [5.20–5.60] | < 0.001 |
| Creatinine (median [IQR]) | 89.5 [84–113.75] | 84.5 [66.5–92] | 0.08 |
| Total cholesterol (mean (SD)) | 3.97 (0.77) | 5.48 (1.21) | 0.001 |
| HDL cholesterol (mean (SD)) | 1.31 (0.22) | 1.73 (0.69) | 0.04 |
| LDL cholesterol (mean (SD)) | 1.93 (0.47) | 3.23 (0.79) | < 0.001 |
| Triglycerides (median [IQR]) | 1.39 [1.13–1.70] | 0.85 [0.71–1.29] | 0.02 |
| Lp(a) (median [IQR]) | 103 [90–120.5] | 87.5 [45.25–148.75] | 0.9 |
| Hba1c (median [IQR]) | 63 [54.5–66.75] | 38.5 [38–39.25] | < 0.001 |
| Statin use (%) | 12 (85.7) | 0 | < 0.001 |
| Insulin use (%) | 10 (71.4) | 0 | 0.001 |
Data are presented as the mean (SD), median (IQR) or n (%)
BMI body mass index, BP blood pressure, AP angina pectoris, MI myocardial infarction; CVA cerebrovascular accident, PAD peripheral arterial disease, CRP C-reactive protein, HDL high-density lipoprotein, LDL low-density lipoprotein; Lp(a) lipoprotein (a)
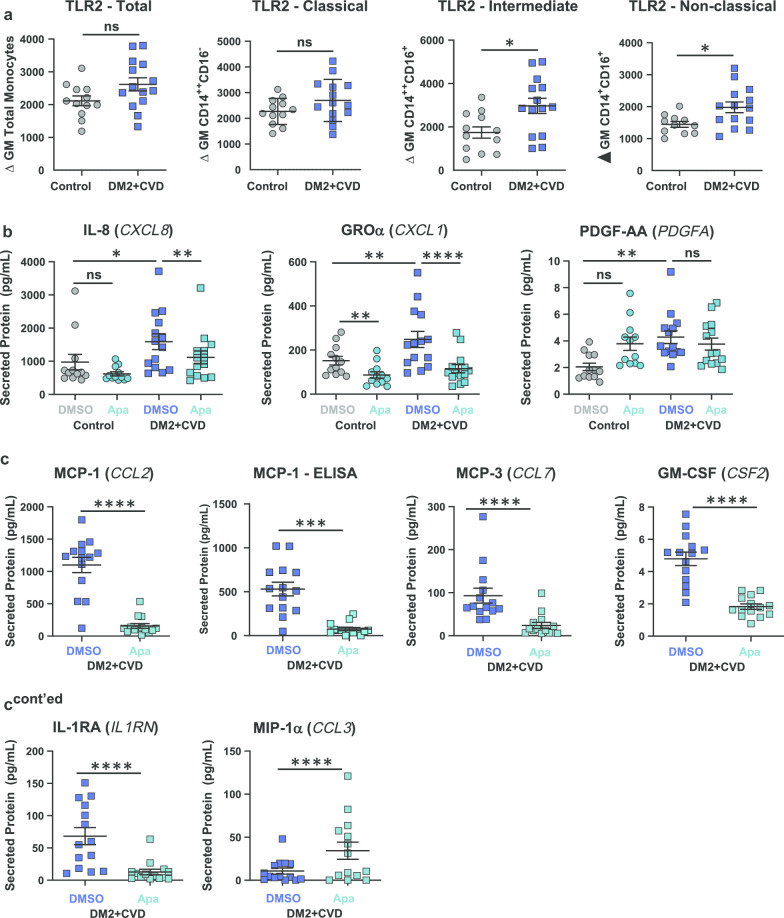
Monocytes were isolated from whole blood of patients with DM2 + CVD or matched control subjects. Total monocyte number (Table 1) and distribution across subset classifications (Additional file 1) were similar in both cohorts. Profiling of 16 monocyte surface receptors revealed higher expression of Toll-like receptor (TLR) 2 on intermediate (CD14++CD16+) and non-classical (CD14+CD16+) DM2 + CVD monocytes (n = 14) as compared to controls (n = 12) (Fig. 1a), consistent with published observations [38–40]. No change in TLR2 abundance was noted in the total or classical monocyte population (Fig. 1a).
Fig. 1.
Ex vivo treatment with apabetalone (Apa) abolishes pro-inflammatory protein secretion in monocytes isolated from DM2 + CVD patients. a Flow cytometry analysis of the pro-inflammatory surface receptor TLR2 in DM2 + CVD versus control monocytes. b Quantification of secreted cytokines 24 h post-plating (Milliplex®) in DMSO or apabetalone (25 μM)-treated control and DM2 + CVD monocytes. c Effect of apabetalone (25 μM) treatment on secretion of key pro- and anti-inflammatory cytokines in DM2 + CVD monocytes. Statistics: a Unpaired Student’s t-test, *p < 0.05; ns, non-significant. b, c 2-Way repeated measures ANOVA followed by Tukey’s multiple comparisons correction for within-group comparisons, or Bonferroni’s test for between-group comparisons; *p < 0.05; **p < 0.01; ***p < 0.001; ****p < 0.0001. Individual patient data are shown as a mean ± SEM
The multianalyte immunoprofiling Milliplex® panel detected 12 cytokines that were secreted by monocytes cultured ex vivo for 24 h. At baseline, monocytes from DM2 + CVD patients (n = 14) showed higher levels of chemokine IL-8 (encoded by the CXCL8 gene), growth-related oncogene-α (GRO-α, encoded by the CXCL1 gene) and PDGF-AA, as compared to controls (n = 12) (Fig. 1b). Notably, apabetalone (25 μM) lowered the enhanced secretion of IL-8 and GROα in DM2 + CVD monocytes (Fig. 1b). Similarly, apabetalone decreased the secretion of monocyte chemoattractant protein 1 (MCP-1) (also detected by ELISA), MCP-3, granulocyte-macrophage colony stimulating factor (GM-CSF) and interleukin 1 receptor antagonist IL-1RA) (Fig. 1c). Macrophage inflammatory protein MIP-1α (CCL3) was the only protein whose secretion increased with apabetalone treatment (Fig. 1c); no changes were detected in CCL3 mRNA transcript levels (data not shown). IL-1β, TNFα, IP-10 and RANTES were not differentially secreted at baseline nor affected by apabetalone treatment (not shown). No toxicity was noted across all treatments and time points (Additional file 2). These data indicate that DM2 + CVD monocytes secreted higher levels of pro-inflammatory cytokines ex vivo, which was abolished by treatment with apabetalone.
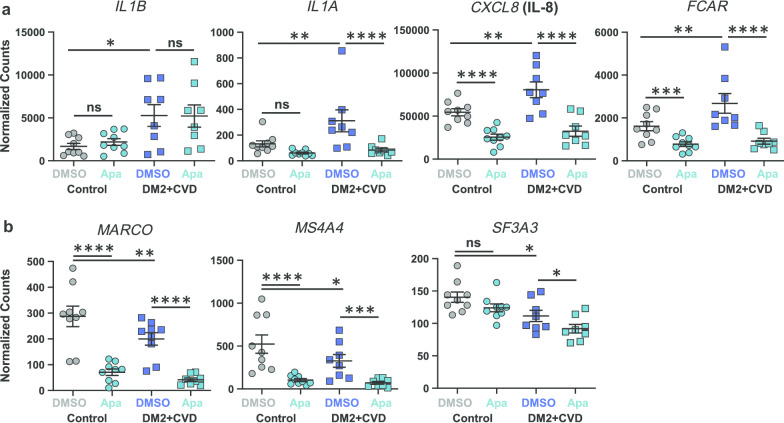
Apabetalone abolishes “hyperactive” gene expression in monocytes from DM2 + CVD patients
The monocyte gene transcription profile was generated for DM2 + CVD monocytes (n = 8) and control monocytes (n = 9) using the NanoString nCounter® Vantage 3D™ Innate Immunity Panel (0.025% DMSO, 4 h). Transcripts for 109 of the 180 genes in the panel were detected (endogenous control-normalized counts > 50) in at least one treatment condition. Between-cohort baseline comparison showed that mRNA transcripts encoding pro-inflammatory cytokines (IL1B, IL1A and CXCL8) and the receptor for the Fc region of IgA (FCAR) were more abundant in monocytes from DM2 + CVD patients than controls (Fig. 2a). In contrast, transcripts encoding the macrophage receptor with collagenous structure (MARCO), the membrane-spanning 4-domains subfamily A member 4A (MS4A4A) and the splicing factor 3A subunit 3 (SF3A3) were lower in abundance in monocytes from DM2 + CVD patients. Collectively, these results indicate that the monocytes of DM2 + CVD patients exhibit a hyperactive pro-inflammatory transcriptional state.
Fig. 2.
Monocytes from DM2 + CVD patients and control subjects exhibit differential gene expression that is inhibited by 25 μM apabetalone (Apa). a Pro-inflammatory genes that show elevated expression in DM2 + CVD monocytes as compared to controls. b. Genes that show reduced expression in DM2 + CVD monocytes as compared to controls. Gene expression is expressed as endogenous control-normalized counts (NanoString™). Statistics: 2-Way repeated measures ANOVA followed by Tukey’s multiple comparisons correction for within-group comparisons, or Bonferroni’s test for between-group comparisons; *p < 0.05; **p < 0.01; ***p < 0.001; ****p < 0.0001; ns, non-significant. Individual patient data are shown as a mean ± SEM
To examine whether the hyperactive pro-inflammatory gene transcription can be diminished by BET inhibition, monocytes from patients and control subjects were treated ex vivo with apabetalone (5 or 25 μM) or DMSO (vehicle control) for 4 h. With the exception of IL1B, mRNA transcripts overexpressed in DM2 + CVD monocytes (IL1A, CXCL8, FCAR) were downregulated by treatment with 25 μM apabetalone (Fig. 2a). mRNA transcripts expressed at lower levels in DM2 + CVD monocytes versus controls (MARCO, MS4A4A and SF3A3) were further reduced by apabetalone (Fig. 2b). Transcription of BRD4, the gene encoding the BRD4 BET protein, was also reduced by apabetalone (Additional file 3), while the abundance of BRD2 or BRD3 transcripts was unaltered (data not shown). A decrease in BRD4 levels could potentially reduce BET-dependent transcriptional regulation in monocytes.
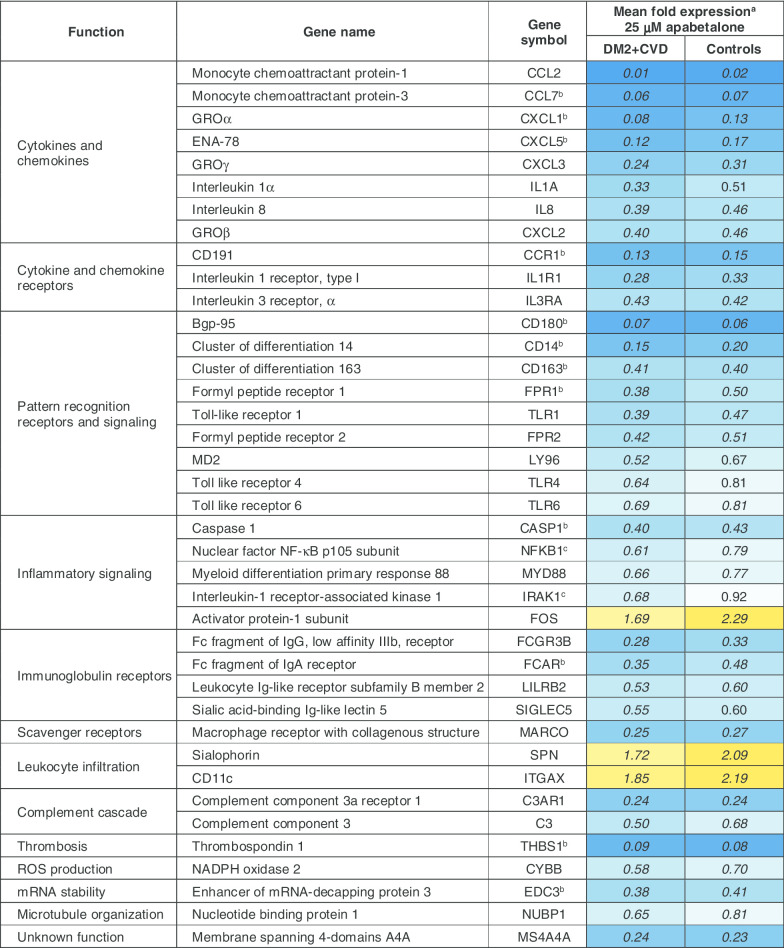
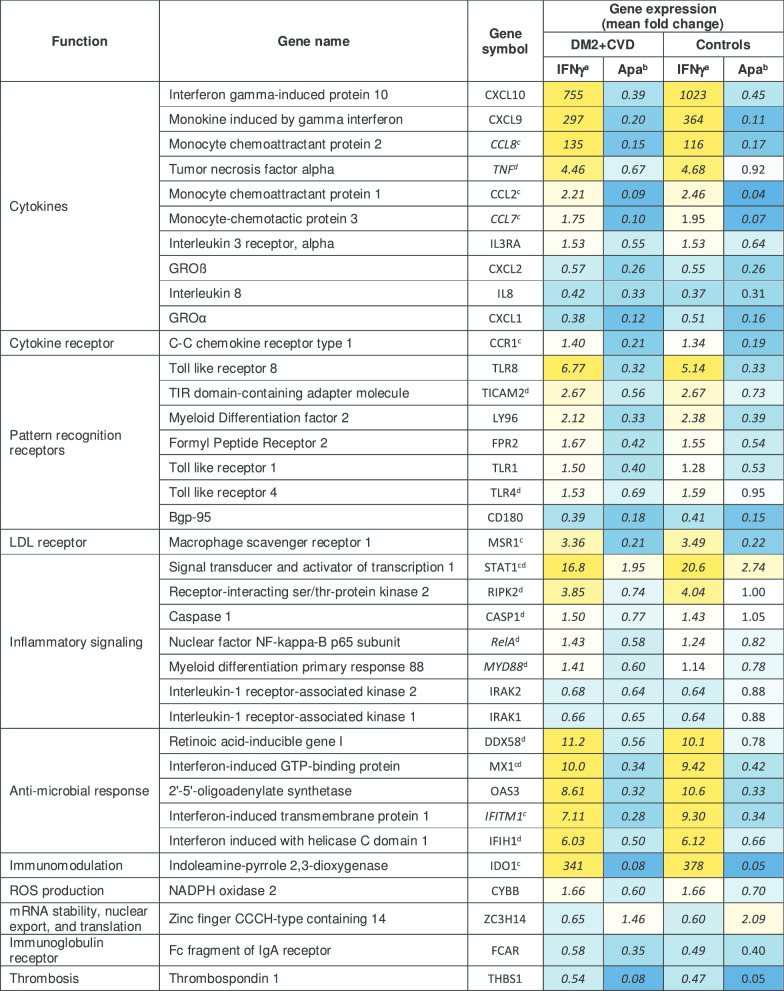
Overall, treatment of DM2 + CVD monocytes with 25 μM apabetalone altered the abundance of 39 out of 109 transcripts detected by the NanoString Innate Immunity Panel (> 30% change with adjusted p < 0.05) (Table 2). 36 of 39 transcripts were downregulated, whereas 3 of them were upregulated by apabetalone treatment (Table 2). Ten gene transcripts were also sensitive to 5 μM apabetalone (marked by asterisks in Table 2). Gene transcription in control monocytes was similarly altered by apabetalone, but with several notable exceptions (Fig. 3a). Target genes associated with NF-κB pathway activation, including TANK-binding kinase 1 (TBK1) and IL-1 receptor-associated kinase 1 (IRAK1), as well as the NF-κB subunit 1 (NFKB1), were more efficiently suppressed by apabetalone in DM2 + CVD monocytes versus controls. Similarly, apabetalone differentially reduced gene expression of the phagocytic macrophage receptor CD68 [41], of the IL-10 receptor subunit IL10RB implicated in pro- and anti-inflammatory homeostasis [42], and of MTMR14 encoding a phosphoinositide phosphatase involved in metabolic dysregulation in obesity [43]. FOS, a transcription factor involved in myeloid differentiation [44], was induced by apabetalone treatment to a lesser extent in DM2 + CVD cells compared to control monocytes (Fig. 3a).
Table 2.
Apabetalone suppresses the expression of inflammatory genes in unstimulated monocytes obtained from DM2 + CVD patients and control subjects
aGene expression is expressed as mean fold difference in response to 25 μM apabetalone treatment relative to vehicle (DMSO). bGenes significantly downregulated in response to 5 μM apabetalone. cGenes differentially sensitive to apabetalone treatment in DM2 + CVD versus control cells (also shown in Fig. 3a). Italics numbers indicate a fold change of > 30% with an adjusted p value < 0.05 (two-way repeated measures ANOVA)
Fig. 3.
Enhanced downregulation of inflammatory mediators and pathways by apabetalone in ex vivo-treated DM2 + CVD monocytes as compared to controls. a Transcription of several genes is suppressed more robustly by apabetalone in monocytes from DM2 + CVD patients. mRNA expression levels are shown as % change following apabetalone treatment (25 μM) relative to the DMSO-treated baseline (100% dotted line). 2-Way repeated measures ANOVA with Bonferroni’s multiple comparisons test, *p < 0.05, **p < 0.01, ***p < 0.001. b, c Predicted effect of apabetalone on b IPA® canonical pathways and c IPA® upstream regulators. IPA® output was based on the input of gene expression changes of more than 20% with apabetalone treatment (versus DMSO, p < 0.05). IPA® z-scores compare changes in gene expression (“activating” or “inhibiting”) in the experimental dataset to changes predicted by the literature. z < − 2 predicts a downregulation within a gene set associated with a canonical pathway or a transcriptional regulator. iNOS inducible nitric oxide synthase, RXR retinoid X receptor, MIF macrophage migration inhibitory factor, LXR liver X receptor, LPS lipopolysaccharide, APP amyloid protein precursor, EGR1 early growth response protein 1
Apabetalone target genes (> 20% change, p < 0.05 following a 4 h treatment) were further examined with Ingenuity® pathway analysis (IPA®) software to predict affected canonical pathways and upstream regulators (Fig. 3b, c). Apabetalone was predicted to downregulate key canonical pathways associated with monocyte inflammatory responses, such as the NF-κB signalling, the TLR signalling, the IL-1 signalling and the NLRP3 inflammasome pathway (Fig. 3b and Additional file 4). IPA® upstream regulator analysis predicted that apabetalone would suppress multiple transcriptional targets associated with cytokine signalling (TNFα, IFN, IL-17, IL-1, GM-CSF) and TLR signalling (LPS, TLR4, NF-κB, RELA, HMGB1, TICAM2, MYD88) (Fig. 3c and Additional file 5). Apabetalone had a greater inhibitory impact on these pathways and regulators in DM2 + CVD monocytes than in controls (as indicated by z-scores < −2 predicting a significant suppression of Upstream Regulator targets) (Fig. 3b, c). The data suggest that monocytes from diseased patients are activated via BET protein-dependent pathways and that these monocytes are more sensitive to BET inhibition by apabetalone than those of matched subjects without CVD or DM2.
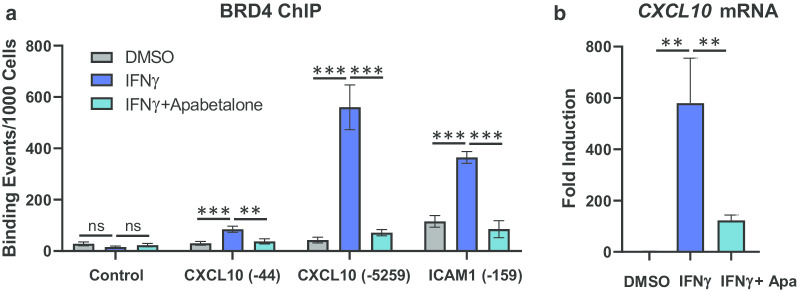
Apabetalone counters DM2 + CVD monocyte hyper-responsiveness to IFNγ
IFNγ is a pro-inflammatory cytokine produced by immune cells in the atherosclerotic plaque that initiates monocyte polarization into pro-inflammatory and tissue-destroying M1 macrophages [37]. BETi have previously been shown to regulate IFNα signalling in monocytes through inhibition of BRD4 association with gene expression regulatory elements [45]. To determine if apabetalone could impact BRD4 chromatin binding in response to IFNγ, we probed BRD4 occupancy of two IFNγ-sensitive genes, CXCL10 and ICAM1, in THP-1 monocytes [46, 47]. As expected, cytokine stimulation (4 h) induced a significant enrichment of BRD4 on the CXCL10 promoter (− 44 bp, 2.8-fold) and enhancer (− 5259 bp, 13-fold), but not in a BRD4-lacking control region (Fig. 4a). A similar induction was observed for the ICAM1 gene promoter (− 159 bp, 3.2-fold). This BRD4 enrichment was countered by co-treatment with apabetalone (56%, 87% and 77% reduction, respectively), indicating that it was BD-dependent. Inhibition of BRD4 chromatin occupancy by apabetalone was consistent with the decrease in CXCL10 gene transcript levels measured after treatment (Fig. 4b). The ICAM1 mRNA transcript was not detectable 4 h post-induction (not shown).
Fig. 4.
Apabetalone treatment decreased BRD4 occupancy at transcription regulatory elements of IFNγ-responsive genes. IFNγ stimulation (4 h) increases BRD4 occupancy on the CXCL10 and ICAM1 gene regulatory regions, but not in a BRD4 protein-lacking region (Control) as determined by chromatin immunoprecipitation (ChIP). Co-treatment with apabetalone (25 μM) reduces BRD4 association with gene regulatory regions. b Apabetalone (25 μM) also suppressed CXCL10 mRNA transcript induction by IFNγ in these same samples. Samples were processed in triplicate. Data are presented as the mean ± S.D. Statistical significance was determined through ANOVA followed by Tukey’s Multiple Comparison Test, where **p < 0.01, ***p < 0.001 and ns, no significant difference
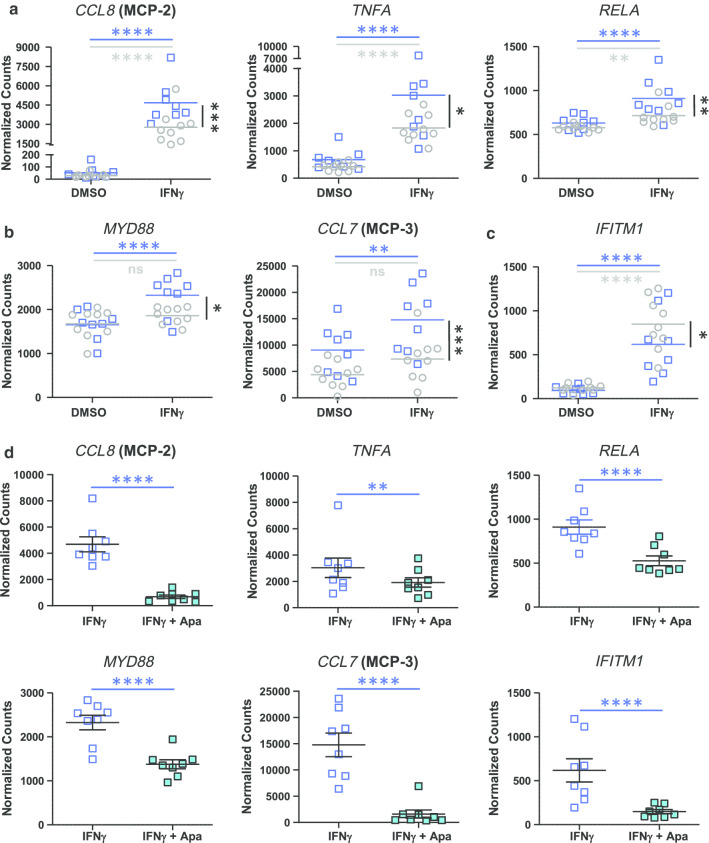
To compare cell responses to IFNγ, DM2 + CVD and control monocytes were treated ex vivo with IFNγ for 4 h, followed by gene expression and protein secretion analysis. Significantly, IFNγ evoked a greater induction of pro-inflammatory genes CCL8, TNF and RELA, relative to baseline, in DM2 + CVD monocytes as compared to control monocytes (blue squares versus grey circles) (Fig. 5a, between-group statistical significance is indicated by black vertical bars and asterisks). MYD88 and CCL7 transcripts were increased by IFNγ only in DM2 + CVD monocytes; no significant change was detected in control monocytes, indicating differential sensitivity to the cytokine treatment between cohorts (Fig. 5b) (blue versus grey horizontal bars and asterisks). IFITM1 transcripts increased in both monocyte populations with IFNγ stimulation, but were enhanced more in control monocytes (Fig. 5c). Overall, these data indicate that DM2 + CVD monocytes are hyperactivated by the pro-M1 stimulant IFNγ, leading to an enhanced expression of chemokines and genes within the NF-κB pathway.
Fig. 5.
Genes hyper-sensitive to IFNγ stimulation are inhibited by 25 μM apabetalone (Apa) in DM2 + CVD monocytes. a Hyper-activation of the transcriptional response to IFNγ in monocytes obtained from DM2 + CVD patients (blue squares) compared to control cohort (grey circles). Gene expression changes are presented as means of endogenous control-normalized counts (Nanostring). b MYD88 and CCL7 are IFNγ inducible in DM2 + CVD monocytes only. c IFITM2 is hyper-responsive in control monocytes. d Genes differentially responsive to IFNγ are suppressed by apabetalone. Endogenous control-normalized counts are shown (NanoString). Statistics: 2-Way repeated measures ANOVA followed by Tukey’s multiple comparisons test (within-group comparisons; blue bars and asterisks) or Bonferroni’s test (between-group comparison; black bars and asterisks); *p < 0.05; **p < 0.01; ***p < 0.001; ****p < 0.0001; ns non-significant. Individual patient data were shown as a mean ± SEM
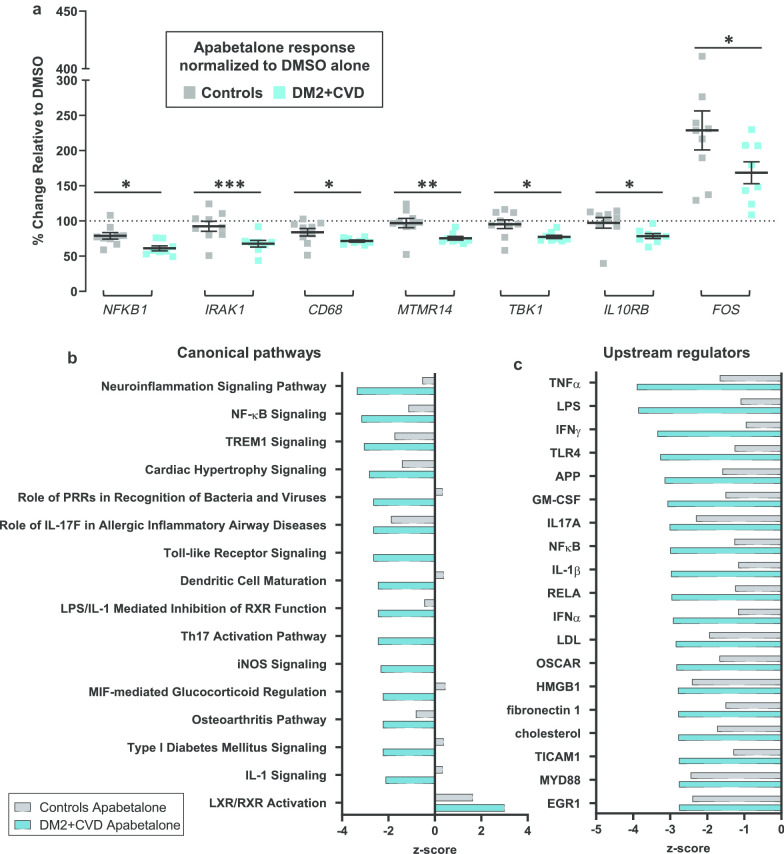
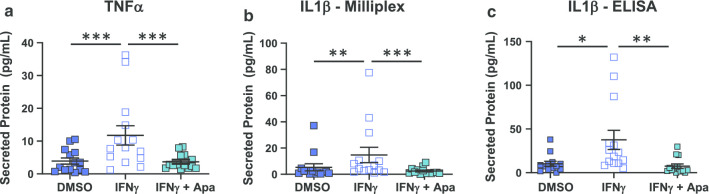
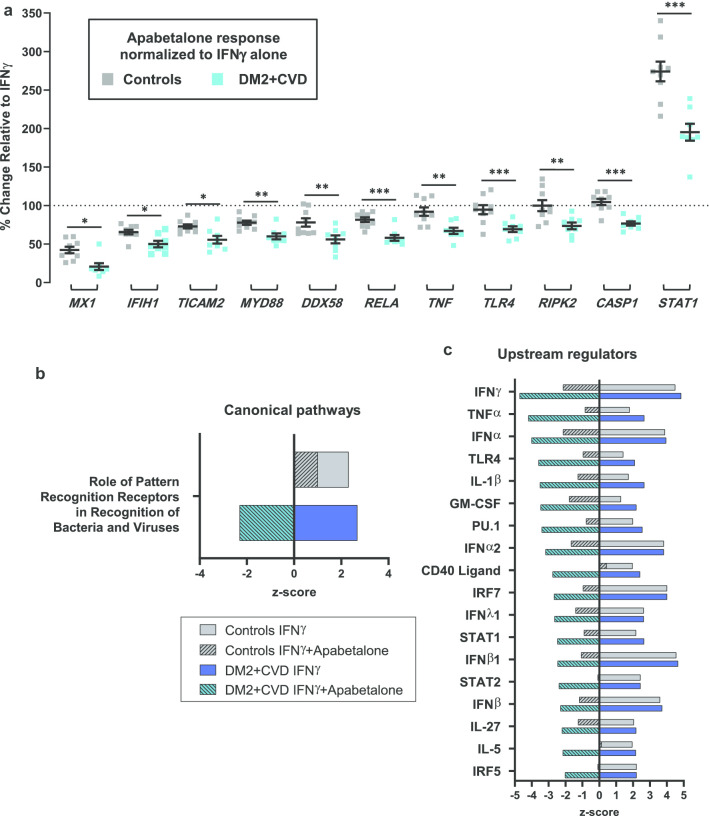
Previous reports have indicated that IFNγ signalling is sensitive to BET inhibition [25, 45, 48, 49]. Ex vivo treatment with apabetalone suppressed the transcription of genes that responded differentially to IFNγ, namely CCL8, TNF, RELA, MYD88, CCL7 and IFITM1 (Fig. 5d and italics gene symbols in Table 3). The drug also countered IFNγ-stimulated secretion of the TNFα protein, consistent with gene expression data in DM2 + CVD monocytes (Fig. 6a). Secretion of IL-1β, as measured by Milliplex® and ELISA assays, also declined with apabetalone treatment (Fig. 6b, c, respectively), even though the IL1B transcription was not induced by IFNγ nor suppressed by apabetalone (data not shown). This may be due to apabetalone-mediated downregulation of the CASP1 gene which is required for secretion of mature IL-1β (Tables 2, 3; see Discussion) [50]. While apabetalone reduced the transcription of numerous genes induced by IFNγ in both cohorts (Table 3), several IFNγ-induced genes were differentially suppressed in DM2 + CVD monocytes as compared to controls (Fig. 7a). In most cases, apabetalone suppressed inflammatory gene transcription more efficiently in DM2 + CVD monocytes (MX1, IFIH1, TICAM2, MYD88, RELA). Transcripts of several genes (DDX58, TNFA, TLR4, RIPK2 and CASP1) were significantly decreased by BETi treatment only in DM2 + CVD monocytes (Fig. 7a, Table 3). Uniquely, induction of IFNγ target gene STAT1 was differentially enhanced by apabetalone (Fig. 7a, Table 3). Overall, these data suggest that the transcriptional response induced by IFNγ has a greater BET-dependency and is more sensitive to apabetalone in DM2 + CVD monocytes than in control cells.
Table 3.
Ex vivo treatment with apabetalone counters IFNγ-mediated induction of gene expression in monocytes
aGene induction in response to IFNγ is expressed as a mean fold change relative to vehicle (DMSO). bEffect of 25 μM apabetalone in the presence of IFNγ is shown as a mean fold change in gene expression relative to IFNγ stimulation alone. cGenes significantly downregulated in response to 5 μM apabetalone. Italics gene symbols indicate an enhanced response to IFNγ in DM2 + CVD monocytes (as compared to controls, also Fig. 5). dGenes differentially sensitive to apabetalone treatment in DM2 + CVD versus control cells (also Fig. 7a). Italics numbers indicate fold change with an adjusted p value < 0.05 (2-way repeated measures ANOVA)
Fig. 6.
Apabetalone counters stimulated cytokine secretion in DM2 + CVD monocytes. a, b Secretion of proteins induced by IFNγ in DM2 + CVD monocytes is countered by 25 μM apabetalone (Apa) 24 h post-treatment (Milliplex®). c Secretion of IL-1b in DM2 + CVD monocytes was confirmed by ELISA. Statistics: 2-Way repeated measures ANOVA followed by Tukey’s multiple comparisons test; *p < 0.05; **p < 0.01; ***p < 0.001. Individual patient data were shown as a mean ± SEM
Fig. 7.
Differential effects of apabetalone treatment on IFNγ-sensitive inflammatory mediators and pathways in DM2 + CVD monocytes as compared to controls. a Apabetalone suppresses select IFNγ-induced genes more robustly in monocytes from DM2 + CVD patients as compared to controls. Apabetalone’s effect on gene expression in the presence of IFNγ was calculated relative to IFNγ only condition (100% dotted line). Statistical significance was determined using 2-way repeated measures ANOVA with Bonferroni’s multiple comparisons test, *p < 0.05, **p < 0.01, ***p < 0.001. b, c Predicted effect of IFNγ and IFNγ + apabetalone treatment on IPA®-curated canonical pathways and upstream regulators. IPA® output was based on the input of gene expression changes of more than 20% with apabetalone treatment (versus DMSO, p < 0.05). IPA® z-scores compare changes in gene expression (“activating” or “inhibiting”) in the experimental dataset to changes predicted by the literature. z < −2 predicts a downregulation and z > 2 predicts an upregulation within a gene set associated with a canonical pathway or a transcriptional regulator. n/d no predicted directional change, IRF interferon response factor; PRRs pattern recognition receptors, RIG-I retinoic acid-inducible gene I
Functionally, the gene transcripts responsive to IFNγ and regulated by apabetalone can be categorized as cytokines, pattern recognition receptors, inflammatory signalling and anti-microbial response molecules (Table 3). Based on gene expression changes following IFNγ treatment of control and DM2 + CVD monocytes (> 20%, p < 0.05), IPA® predicted a significant upregulation of a canonical pathway linked to pattern recognition receptor (PRR) signalling (p < 0.0001, z-score > 2) (Fig. 7b and Additional file 6). Apabetalone treatment was predicted to significantly reverse the activation of the PRR signalling pathway only in DM2 + CVD monocytes (z-score < − 2) as no significant directional effect of apabetalone was predicted in control monocytes (2 > z-score > − 2) (Fig. 7b). The IPA® upstream regulator analysis showed that IFNγ target genes play a role downstream of key cytokines and transcription factors involved in macrophage differentiation and activation (Fig. 7c and Additional file 7). While apabetalone also had a significant inhibitory effect on the IFNγ-dependent inflammatory pathways in control monocytes (Fig. 7c; grey hatched bars), the predicted suppression of gene signatures was more pronounced in DM2 + CVD monocytes (Fig. 7c; teal hatched bars). Taken together, IFNγ-mediated gene transcription was countered by BET inhibition more efficiently in DM2 + CVD monocytes as compared to controls. Overall, our findings suggest that the transcriptional responsiveness of IFNγ-regulated genes is more dependent on BET proteins in the diseased state.
Discussion
In this study, we compared the pro-inflammatory activity of monocytes derived from DM2 + CVD patients on standard of care therapy versus matched control subjects. Monocytes from DM2 + CVD patients exhibited a hyper-inflammatory state characterized by increased gene expression of pro-inflammatory cytokines IL-8, IL-1α and IL-1β and of the IgA receptor FCAR (also known as CD89). At the protein level, we observed enhanced surface expression of TLR2 in intermediate (CD14++CD16+) and non-classical (CD14+CD16+) DM2 + CVD monocytes and increased secretion of chemoattractants IL-8 and GROα (CXCL1) (Fig. 1). These changes in gene and protein abundance suggest that the monocytes circulating in DM2 + CVD patients adopt a pro-inflammatory phenotype despite standard of care therapy including statins.
Enhanced TLR2 expression had previously been reported on monocytes from DM2 and metabolic syndrome patients [38–40]. TLR2 is a pattern recognition receptor that recognizes molecular danger signals that are linked to microbial infection or sterile tissue injury. It is also crucial in the initiation and progression of atherosclerosis, since it stimulates foam cell formation [51]. Statins are reported to decrease monocyte TLR expression in DM patients [52–54]. However, statin therapy did not normalize monocyte TLR2 expression in our DM2 + CVD cohort. TLR2 activation induces the expression of cytokines, chemokines and cell adhesion molecules by immune cells, promoting na pro-inflammatory phenotype [55]. Similarly, FCAR activation by immunoglobulin A enhances production of pro-inflammatory cytokines, prostaglandins and leukotrienes [56–58]. Enhanced TLR and/or FCAR surface expression may underlie the observed hyperactive transcription of IL1A, IL1B and CXCL8 as well as enhanced secretion of IL-8 and GROα in DM2 + CVD monocytes observed in this study. Elevated levels of these cytokines have previously been described in DM2 and CVD patients [59–61]. These pro-inflammatory mediators are highly pro-atherogenic as they promote differentiation to a M1-like macrophage phenotype, enhanced vascular wall recruitment and increased endothelial transmigration [62–66]. Thus, their overproduction likely contributes to the pathogenesis of atherosclerosis in DM2 + CVD patients on standard of care therapy.
A number of genes were downregulated in monocytes isolated from DM2 + CVD patients (relative to controls), including the mRNA splicing complex encoding gene SF3A3, the scavenger receptor MARCO and the plasma membrane tetraspan gene MS4A4. The latter two genes are expressed on monocytes with anti-inflammatory M2-like characteristics [67, 68], whereas the SF3A3 gene negatively regulates pro-inflammatory TLR signalling [69]. Thus, downregulation of these genes may indicate reprogramming towards a pro-inflammatory phenotype in patients. Upon IFNγ stimulation, monocytes acquire a M1-like phenotype characterized by enhanced cytokine production, phagocytosis and intracellular killing of microbial pathogens [70]. We show that monocytes isolated from DM2 + CVD patients are more responsive to IFNγ ex vivo treatment, with enhanced expression of genes that encode the NF-κB inflammatory pathway components (TNF, MYD88 and RELA) and chemokines (CCL7 and CCL8). Our observations are consistent with previous studies reporting that monocytes from CVD patients (53% of whom also had DM2) overproduce cytokines in response to treatment with IFNγ combined with lipopolysaccharide [8]. Overall, the observed gene expression and secretory profile of DM2 + CVD monocytes indicate a potential phenotypic shift from the M2-like state towards the pro-inflammatory M1-like state.
This persistent hyper-responsive phenotype is likely linked to changes to the epigenetic landscape characteristic of cardiometabolic disease [14, 19]. In human monocytes exposed to hyperglycemic conditions ex vivo, there is a decrease in transcription inhibiting histone methylation marks and an increase in open chromatin marks, potentially enhancing transcription factor accessibility to DNA [17, 71, 72]. Congruently, in monocytes from diabetic patients, transcription-activating acetylation marks are more abundant on the promoters of pro-inflammatory genes encoding TNFα and cyclooxygenase-2 (PTGS) [71, 72]. Transcription-activating acetylation of histone 3 lysine 27 (H3K27) and methylation of H3K4 is also increased in immune and vascular smooth muscle cells isolated from atherosclerotic plaques in human carotids [73]. BET proteins “read” histone acetylation patterns including H3K27, thereby activating aberrant gene expression in diseased or stimulus-activated cells [23, 28, 30]. However, it is unclear if excessive BET activity contributes to pro-inflammatory monocyte response in DM2 + CVD patients.
Here, we demonstrate that the BET inhibitor apabetalone disrupts pro-inflammatory gene expression in hyperactive DM2 + CVD monocytes. Indeed, in unstimulated conditions, apabetalone suppresses numerous genes more efficiently in DM2 + CVD monocytes, including those associated with cytokine, TLR and NF-κB signalling. Of note, even in baseline conditions, apabetalone significantly reduces the IFNγ transcriptional signature in DM2 + CVD monocytes (but not in control cells), suggesting that IFNγ target genes are hyperactive in diabetic monocytes. Our data agrees with previously published observations, showing that IFNγ target genes can be induced by high glucose in ex vivo cultured human monocytes [17]. Further, upon ex vivo IFNγ stimulation, the TLR pathway and the cytokine transcriptional networks were predicted to be downregulated by apabetalone, especially in DM2 + CVD monocytes (Fig. 7). This differential response to apabetalone treatment suggests that BET proteins drive the disease-associated IFNγ signature in DM2 + CVD patients’ monocytes. Interestingly, monocytes from systemic sclerosis patients also display BETi-sensitive IFN signatures, similarly to the DM2 + CVD monocytes studied here [74]. We have shown that apabetalone can dislodge BRD4 from chromatin during IFNγ-mediated induction of model genes CXCL10 and ICAM1 in an in vitro monocyte model, providing insight into the drug’s mechanism of action. However, further epigenetic studies will be required to explain the differential sensitivity to BET inhibition between non-diseased and diseased cells.
Macrophages present in the atherosclerotic plaque are largely derived from circulating monocytes infiltrating blood vessels’ walls [7, 75]. In mice, monocytes have been shown to enter into the plaque more readily in the context of diabetes and hypercholesterolemia [76–78]. In non-stimulated conditions, apabetalone suppressed protein secretion of key monocyte chemoattractants MCP-1, MCP-3, GRO-α and IL-8 (87%, 79%, 55% and 32% reduction in DM2 + CVD monocytes, respectively). Apabetalone treatment also potently downregulated the transcription of genes differentially induced by IFNγ in DM2 + CVD monocytes, including the pro-inflammatory cytokine TNF gene (33% reduction), and monocyte chemokine genes CCL7 and CCL8 (90% and 85% reduction, respectively). Additional chemokines that promote chemotaxis and tissue extravasation, CCL2 [62, 64], CXCL9 [79] and CXCL10 [79], were induced by IFNγ in both monocyte populations and were strongly suppressed by apabetalone (91%, 80% and 61% reduction, respectively) (Table 3). BETi treatment is thus predicted to reduce the migratory phenotype of DM2 + CVD monocytes, potentially preventing atherosclerotic plaque infiltration by activated monocytes.
Upon stimulation with cytokines and PRR agonists, monocytes and macrophages activate the inflammasome pathway, which is responsible for the production of the mature secreted form of IL-1β, a major pro-atherosclerotic cytokine [50]. IFNγ contributes to high IL1B gene expression only when combined with secondary stimuli [80]. Consistent with published data [80], IFNγ did not change the IL1B transcript abundance as a single agent (data not shown), but it enhanced the IL-1β protein secretion by 2.7-fold in DM2 + CVD monocytes (Fig. 6). This induction was countered by apabetalone treatment (84% reduction). IL-1β is synthesized by monocytes in its inactive form (pro-IL-1β), which is then converted into its active mature form by the NLRP3 inflammasome-associated caspase 1 protease (encoded by CASP1 gene) [50]. Apabetalone (25 μM) downregulated CASP1 gene transcription in DM2 + CVD monocytes in non-stimulated (Table 2) and stimulated (Table 3) conditions, potentially explaining the observed decrease in IL-1β. The severity of atherosclerosis correlates with inflammasome activity and NLRP3/caspase 1-mediated generation of IL-1β and IL-1α in human atherosclerotic plaque [81]. Interestingly, the anti-IL-1β monoclonal antibody canakinumab reduced the risk of MACE for CVD patients by 15% in 3.7 years, independently of lipid lowering [82]. This proof-of-concept study demonstrated that countering inflammasome-mediated inflammation significantly reduces residual CVD risk, promoting the development of new anti-inflammatory therapeutic agents.
Conclusions
We have demonstrated that monocytes isolated from DM2 + CVD patients exhibit a hyper-inflammatory phenotype at baseline and a hyper-responsiveness to inflammatory stimuli ex vivo. This activated monocyte state may contribute to the initiation and progression of atherosclerosis and increased cardiovascular risk in these patients. Ex vivo BET-inhibition by apabetalone reduces this enhanced pro-inflammatory phenotype, providing a rationale for further evaluation of BET inhibitors as therapeutic agents for high risk DM2 + CVD patients. Previously, a post hoc analysis of pooled phase 2 trials of CVD patients indicated that apabetalone reduced MACE (5.9% in the treatment group compared to 10.4% in the placebo group; p = 0.02) [83]. In a subgroup analysis of patients with DM2, apabetalone further reduced the MACE hazard ratio to 0.38 (95% CI 0.15–0.99; p = 0.04) [83]. In the recently completed phase 3 cardiovascular outcomes trial (BETonMACE), 2425 patients with DM2 and recent acute coronary syndrome were treated with apabetalone or placebo, and followed for 26 months [84, 85]. Although the primary endpoint of the study, a reduction in time to first occurrence of MACE defined as CV death, non-fatal myocardial infarction or stroke, did not achieve statistical significance, apabetalone did demonstrate benefits on hospitalization for heart failure [85]. As monocyte activation and infiltration contributes to heart failure, apabetalone treatment may counter the detrimental immune inflammatory response in patients with post-acute coronary syndrome and DM2.
Materials and methods
Study design
This observational mono-centre cohort study enrolled subjects diagnosed with DM2 and high CVD risk (myocardial infarction, percutaneous coronary intervention, coronary artery bypass graft, peripheral arterial disease, episode of unstable angina, transient ischemic event, cerebrovascular accident or peripheral arterial disease, but event-free in past 3 months) and age and gender matched volunteers (Table 1). Exclusion criteria consisted of a history of chronic kidney disease stage 3b-5, malignant diseases or any clinically significant medical condition within the past 2 years that could interfere with the conduct of the study in the opinion of the investigator, treatment with immunosuppressants within the 3 months prior to visit 1 and evident drug or alcohol use. The study protocol was approved by the medical ethical committee of the Amsterdam Medical Centre in Amsterdam, the Netherlands. Each subject provided written informed consent.
Biochemical measurements
Blood was collected while patients were in a fasting state. Plasma total cholesterol, high-density lipoprotein (HDL) cholesterol, triglycerides and lipoprotein(a) levels were analysed using commercially available methods. Low-density lipoprotein cholesterol levels were calculated using the Friedewald equation.
PBMC isolation and monocyte culture
Peripheral blood mononuclear cells (PBMCs) were isolated from DM2 + CVD subjects and healthy controls by Ficoll density gradient centrifugations (Axis-Shield) as described in detail previously [86]. In brief, after washing PBMCs, CD14+ monocytes were isolated using human CD14 magnetic beads and MACS® cell separation columns according to manufacturer’s instructions (Miltenyi Biotec, Leiden, The Netherlands). Then, these CD14+ monocytes were ex vivo treated with IFNγ and/or apabetalone, and phenotyped for gene expression (NanoString) and protein secretion (Millipore Milliplex® Human Cytokine/Chemokine Array).
Flow cytometry
Whole blood was collected from DM2 + CVD patients and matched controls in EDTA tubes. After lysis of red blood cells with red blood cell lysis buffer 10× (eBioscience), white blood cells were stained with antibodies for cell surface markers CCR2, CD11c, CD36, CD29, CCR5, CD33, CD32, TLR2, CD11b,CCR7, CD163, TLR4, HLA-DR, CD14, CD16, IVIG. Fluorescence was measured using a FACS CANTO II (BD) and analysed with FlowJo software version V10.6. Monocyte area was gated based on forward and side scatter, CD14+ and/or CD16+ and HLA-DR. Monocytes were classified as classical (CD14++CD16−), intermediate (CD14++CD16+) or non-classical (CD14+CD16+). The expression of cell surface markers was calculated as the delta geometric mean (∆GM). ∆GM = GM surface staining—GM unstained control. Statistical differences in cell surface marker abundance between DM2 + CVD patient monocytes and controls were determined using a Student’s t-test.
Multiplexed gene expression analysis via nanostring
CD14+ monocytes from 8 DM2 + CVD patients and 9 control subjects were pre-incubated with DMSO (0.025%) or apabetalone (5 or 25 μM) for 1 h, followed by IFNγ (25 U/ml) co-stimulation for 4 h. Non-stimulated samples received DMSO or apabetalone for 4 h. Monocytes were lysed with TriPure (Roche, Basel, Switzerland), and total RNA was isolated and analysed using the nCounter® Vantage 3D™ Innate Immunity Panel (NanoString) (University of Alberta) for multiplexed single molecule counting of 180 human gene transcripts. Data were analysed using nSolver™ and Ingenuity® Pathway Analysis (IPA®). IPA® z-scores compare the observed differential regulation of a gene (“activating” or “inhibiting”) in the dataset to changes predicted by the literature. z < − 2 predicts a downregulation, and z > 2 predicts an upregulation within a gene set associated with a canonical pathway or a transcriptional regulator. p value < 0.01 indicates a statistically significant overlap between the dataset genes and the curated gene sets (Fisher’s exact test).
Real-time PCR
To assess BRD2, BRD3 and BRD4 expression, total RNA extracted from monocytes was reverse transcribed with High-Capacity cDNA RT Kit (Thermofisher Scientific) and amplified using TaqMan™ Gene Expression Master Mix and TaqMan Real-Time PCR assays (Applied Biosystems). Gene expression was normalized to the endogenous control cyclophilin A (duplex reaction). Data were acquired using the ViiA-7 rtPCR System (Applied Biosystems).
Multianalyte immunoprofiling
In unstimulated conditions, monocytes were treated with DMSO (0.025%, vehicle control) or with apabetalone (25 μM) for 24 h. In stimulated conditions, monocytes were incubated with DMSO, IFNγ (25 U/ml) + DMSO or IFNγ + apabetalone (25 μM) for 24 h. Supernatants were collected from triplicate treatments, pooled and analysed using the Millipore Milliplex® Human Cytokine Array / Chemokine Array 42-Plex with IL-18 (HD42) (Eve Technologies, Calgary, AB) to quantify EGF, Eotaxin-1, FGF-2, Flt-3L, Fractalkine, G-CSF, GM-CSF, GROα, IFNα2, IFNγ, IL-1α, IL-1β, IL-1RA, IL-2, IL-3, IL-4, IL-5, IL-6, IL-7, IL-8, IL-9, IL-10, IL-12 (p40), IL-12 (p70), IL-13, IL-15, IL-17A, IL-18, IP-10, MCP-1, MCP-3, MDC, MIP-1α, MIP-1β, PDGF-AA, PDGF-AB/BB, RANTES, sCD40L, TGFα, TNFα, TNFβ and VEGF-A.
ELISA
Cytokine levels were measured in samples used for multianalyte immunoprofiling by commercially available enzyme-linked immunosorbent assay kits for MCP-1, IL-8 and IL-1β according to the manufacturer’s instructions (Invitrogen). High binding half area 96 well plates were used for these assays.
Chromatin immunoprecipitation
To assess BET protein chromatin occupancy, THP-1 cells were pre-treated with BET inhibitors for 1 h before addition of IFNγ (25 U/ml) for a 4 h co-incubation period. After cross-linking cells with formaldehyde, Active Motif Inc. (Carlsbad, CA) performed chromatin isolation and immunoprecipitation with BRD4 antibodies (Bethyl). Samples were processed in triplicate. Statistical significance was determined through 2-way ANOVA followed by Tukey’s Multiple Comparison Test.
Statistical analysis
Differences in gene expression were determined to be statistically significant by comparing endogenous control-normalized raw counts (calculated by nSolver™) using a 2-way repeated measures ANOVA test followed by Tukey’s multiple comparisons correction for within-group comparisons, or Bonferroni’s test for between-group comparisons (PRISM 8). Statistically significant differences in protein secretion were determined by comparing absolute concentrations (obtained by Milliplex® immunoprofiling). Percent change in gene expression was calculated versus each subject’s DMSO-treated sample or IFNγ-treated sample and compared between cohorts with 2-way ANOVA followed by Tukey’s test. Results are presented as mean or median values ± SEM. p value ≤ 0.05 was considered statistically significant.
Supplementary information
Additional file 1–3. Additional file 1. Analysis of monocyte subpopulations in control (CTL) and DM2+CVD patients. Monocytes were classified as classical (CD14++CD16−), intermediate (CD14++CD16+) or non-classical (CD14+CD16+). Fluorescence was measured using a FACS CANTO II (BD) and analysed with FlowJo software. Additional file 2. Monocytes were stimulated ex vivo with IFNγ (1.5, 3.12, 6.25, 12.5 or 25 U/ml), apabetalone (1.5, 3.12, 6.25, 12.5 or 25 μM), or a combination of both stimuli for 24h. Subsequently, cytotoxicity was determined by measuring the enzyme lactate dehydrogenase (LDH) in the supernatant using the CytoTox 96® non-radioactive cytotoxicity assay (Promega). There was no difference between ‘unstimulated’ and ‘stimulated’ conditions, except for the positive control where p < 0.0001. Statistics: One-way ANOVA with Dunnett’s multiple comparisons test. Additional file 3. BRD4 mRNA expression is reduced by ex vivo treatment with apabetalone in DM2+CVD monocytes (4h ex vivo treatment, 25 μM). BRD4 expression was measured by real-time PCR and normalized to cyclophilin A (endogenous control). Statistics: Unpaired Student’s t-test, ****, p < 0.0001.
Additional file 4–7. Additional file 4. Apabetalone’s gene targets in IPA® canonical pathways gene sets: Unstimulated control and DM2+CVD monocytes treated with apabetalone ex vivo. Additional file 5. Apabetalone’s gene targets that converge on IPA® upstream regulators: unstimulated monocytes treated with apabetalone ex vivo. Additional file 6. Apabetalone’s gene targets within IPA® canonical pathways: IFNγ stimulated monocytes treated with apabetalone ex vivo. Additional file 7. Apabetalone’s gene targets in IPA® upstream regulators gene sets: IFNγ stimulated control and DM2+CVD patient monocytes treated with apabetalone ex vivo.
Acknowledgements
We would like to thank Resverlogix’s lab members for intellectual input and manuscript review.
Abbreviations
- BD
Bromodomain
- BET
Bromodomain and extraterminal
- BETi
BET inhibitor
- CASP1
NLRP3 inflammasome-associated caspase 1 protease
- CVD
Cardiovascular disease
- DM2
Type 2 diabetes mellitus
- FCAR
Fc region of IgA
- GM-CSF
Granulocyte-macrophage colony stimulating factor
- GRO
Growth-regulated oncogene
- HDL
High-density lipoprotein
- IFNγ
Interferon gamma
- IL
Interleukin
- IL-1RA
Interleukin 1 receptor antagonist IL-1RA
- IPA®
Ingenuity® Pathway Analysis
- LDL
Low-density lipoprotein
- MACE
Major acute cardiac event
- MARCO
Macrophage receptor with collagenous structure
- MCP
Monocyte chemoattractant protein
- MS4A4A
Membrane-spanning 4-domains subfamily A member 4A
- NF-κB
Nuclear factor κ-light-chain-enhancer of activated B cells
- PBMC
Peripheral blood mononuclear cells
- PRR
Pattern recognition receptor
- ROS
Reactive oxygen species
- TLR
Toll-like receptor
- TNF
Tumor necrosis factor
- SF3A3
Splicing factor 3A subunit 3
Authors’ contributions
EK, NCWW, JOJ and MS conceived the project. EK, SW, BDR, ESGS, KED and MB designed the study. ESGS, JK and EK supervised the research. JK, KED, MV, MB, LF and SW collected, analysed and/or interpreted the data. BR managed the project and performed the statistical analysis. YK recruited patients. SW, SCS, EK, ESGS, KED and JK wrote and revised the manuscript. All authors read and approved the final manuscript.
Funding
This work was financially supported by Resverlogix Corp. and the Netherlands CardioVascular Research Initiative: the Dutch Heart Foundation, Dutch Federation of University Medical Centers, the Netherlands, Organization for Health Research and Development and the Royal Netherlands Academy of Sciences for the GENIUS-II project ‘Generating the best evidence-based pharmaceutical targets for atherosclerosis-II’ (CVON 2017-20). This work was furthermore financially supported by the Netherlands Organization for Scientific Research (VENI Grant from ZonMW; 91619098 to JK).
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Ethics approval and consent to participate
The study protocol was approved by the medical ethical committee of the Amsterdam Medical Centre in Amsterdam, the Netherlands. Each subject provided written informed consent.
Consent for publication
Not applicable.
Competing interests
S.W., B.D.R., S.C.S, L.F., J.O.J., M.S., N.C.W.W. and E.K. are employed by Resverlogix Corp. & hold company’s shares and stock options. All other authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Sylwia Wasiak and Kim E. Dzobo are co-first authors
Jeffrey Kroon and Ewelina Kulikowski are co-senior authors
Supplementary information
Supplementary information accompanies this paper at 10.1186/s13148-020-00943-0.
References
- 1.Einarson TR, Acs A, Ludwig C, Panton UH. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovasc Diabetol. 2018;17:83. doi: 10.1186/s12933-018-0728-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Akash MS, Rehman K, Chen S. Role of inflammatory mechanisms in pathogenesis of type 2 diabetes mellitus. J Cell Biochem. 2013;114:525–531. doi: 10.1002/jcb.24402. [DOI] [PubMed] [Google Scholar]
- 3.Ebtehaj S, Gruppen EG, Parvizi M, Tietge UJF, Dullaart RPF. The anti-inflammatory function of HDL is impaired in type 2 diabetes: role of hyperglycemia, paraoxonase-1 and low grade inflammation. Cardiovasc Diabetol. 2017;16:132. doi: 10.1186/s12933-017-0613-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Groh L, Keating ST, Joosten LAB, Netea MG, Riksen NP. Monocyte and macrophage immunometabolism in atherosclerosis. Semin Immunopathol. 2018;40:203–214. doi: 10.1007/s00281-017-0656-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yuan T, Yang T, Chen H, Fu D, Hu Y, Wang J, et al. New insights into oxidative stress and inflammation during diabetes mellitus-accelerated atherosclerosis. Redox Biol. 2019;20:247–260. doi: 10.1016/j.redox.2018.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Spranger J, Kroke A, Mohlig M, Hoffmann K, Bergmann MM, Ristow M, et al. Inflammatory cytokines and the risk to develop type 2 diabetes: results of the prospective population-based European Prospective Investigation into Cancer and Nutrition (EPIC)-Potsdam Study. Diabetes. 2003;52:812–817. doi: 10.2337/diabetes.52.3.812. [DOI] [PubMed] [Google Scholar]
- 7.Amengual J, Barrett TJ. Monocytes and macrophages in atherogenesis. Curr Opin Lipidol. 2019;30:401–408. doi: 10.1097/MOL.0000000000000634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shirai T, Nazarewicz RR, Wallis BB, Yanes RE, Watanabe R, Hilhorst M, et al. The glycolytic enzyme PKM2 bridges metabolic and inflammatory dysfunction in coronary artery disease. J Exp Med. 2016;213:337–354. doi: 10.1084/jem.20150900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bekkering S, Stiekema LCA, Bernelot Moens S, Verweij SL, Novakovic B, Prange K, et al. Treatment with statins does not revert trained immunity in patients with familial hypercholesterolemia. Cell Metab. 2019;30:1–2. doi: 10.1016/j.cmet.2019.05.014. [DOI] [PubMed] [Google Scholar]
- 10.Bekkering S, van den Munckhof I, Nielen T, Lamfers E, Dinarello C, Rutten J, et al. Innate immune cell activation and epigenetic remodeling in symptomatic and asymptomatic atherosclerosis in humans in vivo. Atherosclerosis. 2016;254:228–236. doi: 10.1016/j.atherosclerosis.2016.10.019. [DOI] [PubMed] [Google Scholar]
- 11.Christ A, Gunther P, Lauterbach MAR, Duewell P, Biswas D, Pelka K, et al. Western diet triggers NLRP3-dependent innate immune reprogramming. Cell. 2018;172:162–175. doi: 10.1016/j.cell.2017.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Seijkens T, Hoeksema MA, Beckers L, Smeets E, Meiler S, Levels J, et al. Hypercholesterolemia-induced priming of hematopoietic stem and progenitor cells aggravates atherosclerosis. FASEB J. 2014;28:2202–2213. doi: 10.1096/fj.13-243105. [DOI] [PubMed] [Google Scholar]
- 13.Mitroulis I, Ruppova K, Wang B, Chen LS, Grzybek M, Grinenko T, et al. Modulation of myelopoiesis progenitors is an integral component of trained immunity. Cell. 2018;172:147–161. doi: 10.1016/j.cell.2017.11.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Neele AE, Van den Bossche J, Hoeksema MA, de Winther MP. Epigenetic pathways in macrophages emerge as novel targets in atherosclerosis. Eur J Pharmacol. 2015;763:79–89. doi: 10.1016/j.ejphar.2015.03.101. [DOI] [PubMed] [Google Scholar]
- 15.Cao Q, Wang X, Jia L, Mondal AK, Diallo A, Hawkins GA, et al. Inhibiting DNA methylation by 5-Aza-2'-deoxycytidine ameliorates atherosclerosis through suppressing macrophage inflammation. Endocrinology. 2014;155:4925–4938. doi: 10.1210/en.2014-1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hoeksema MA, Gijbels MJ, Van den Bossche J, van der Velden S, Sijm A, Neele AE, et al. Targeting macrophage Histone deacetylase 3 stabilizes atherosclerotic lesions. EMBO Mol Med. 2014;6:1124–1132. doi: 10.15252/emmm.201404170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Miao F, Chen Z, Zhang L, Wang J, Gao H, Wu X, et al. RNA-sequencing analysis of high glucose-treated monocytes reveals novel transcriptome signatures and associated epigenetic profiles. Physiol Genomics. 2013;45:287–299. doi: 10.1152/physiolgenomics.00001.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miao F, Chen Z, Genuth S, Paterson A, Zhang L, Wu X, et al. Evaluating the role of epigenetic histone modifications in the metabolic memory of type 1 diabetes. Diabetes. 2014;63:1748–1762. doi: 10.2337/db13-1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bekkering S, Quintin J, Joosten LA, van der Meer JW, Netea MG, Riksen NP. Oxidized low-density lipoprotein induces long-term pro-inflammatory cytokine production and foam cell formation via epigenetic reprogramming of monocytes. Arterioscler Thromb Vasc Biol. 2014;34:1731–1738. doi: 10.1161/ATVBAHA.114.303887. [DOI] [PubMed] [Google Scholar]
- 20.Taniguchi Y. The bromodomain and extra-terminal domain (BET) family: functional anatomy of BET paralogous proteins. Int J Mol Sci. 2016;17:1849. doi: 10.3390/ijms17111849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu R, Zhong Y, Li X, Chen H, Jim B, Zhou MM, et al. Role of transcription factor acetylation in diabetic kidney disease. Diabetes. 2014;63:2440–2453. doi: 10.2337/db13-1810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zou Z, Huang B, Wu X, Zhang H, Qi J, Bradner J, et al. Brd4 maintains constitutively active NF-kappaB in cancer cells by binding to acetylated RelA. Oncogene. 2014;33:2395–2404. doi: 10.1038/onc.2013.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brown JD, Lin CY, Duan Q, Griffin G, Federation A, Paranal RM, et al. NF-kappaB directs dynamic super enhancer formation in inflammation and atherogenesis. Mol Cell. 2014;56:219–231. doi: 10.1016/j.molcel.2014.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tian B, Yang J, Zhao Y, Ivanciuc T, Sun H, Garofalo RP, et al. BRD4 couples NF-kappaB/RelA with airway inflammation and the IRF-RIG-I amplification loop in respiratory syncytial virus infection. J Virol. 2017;91:e00007-17. doi: 10.1128/JVI.00007-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Patel MC, Debrosse M, Smith M, Dey A, Huynh W, Sarai N, et al. BRD4 coordinates recruitment of pause release factor P-TEFb and the pausing complex NELF/DSIF to regulate transcription elongation of interferon-stimulated genes. Mol Cell Biol. 2013;33:2497–2507. doi: 10.1128/MCB.01180-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li Y, Liu M, Chen LF, Chen R. P-TEFb: Finding its ways to release promoter-proximally paused RNA polymerase II. Transcription. 2018;9:88–94. doi: 10.1080/21541264.2017.1281864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huang B, Yang XD, Zhou MM, Ozato K, Chen LF. Brd4 coactivates transcriptional activation of NF-kappaB via specific binding to acetylated RelA. Mol Cell Biol. 2009;29:1375–1387. doi: 10.1128/MCB.01365-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Das S, Senapati P, Chen Z, Reddy MA, Ganguly R, Lanting L, et al. Regulation of angiotensin II actions by enhancers and super-enhancers in vascular smooth muscle cells. Nat Commun. 2017;8:1467. doi: 10.1038/s41467-017-01629-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dey A, Yang W, Gegonne A, Nishiyama A, Pan R, Yagi R, et al. BRD4 directs hematopoietic stem cell development and modulates macrophage inflammatory responses. EMBO J. 2019;38:e100293. doi: 10.15252/embj.2018100293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nicodeme E, Jeffrey KL, Schaefer U, Beinke S, Dewell S, Chung CW, et al. Suppression of inflammation by a synthetic histone mimic. Nature. 2010;468:1119–1123. doi: 10.1038/nature09589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Picaud S, Wells C, Felletar I, Brotherton D, Martin S, Savitsky P, et al. RVX-208, an inhibitor of BET transcriptional regulators with selectivity for the second bromodomain. Proc Natl Acad Sci U S A. 2013;110:19754–19759. doi: 10.1073/pnas.1310658110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McLure KG, Gesner EM, Tsujikawa L, Kharenko OA, Attwell S, Campeau E, et al. RVX-208, an inducer of ApoA-I in humans, is a BET bromodomain antagonist. PLoS ONE. 2013;8:e83190. doi: 10.1371/journal.pone.0083190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang Q, Li Y, Xu J, Wang Y, Leung EL, Liu L, et al. Selective inhibition mechanism of RVX-208 to the second bromodomain of bromo and extraterminal proteins: insight from microsecond molecular dynamics simulations. Sci Rep. 2017;7:8857. doi: 10.1038/s41598-017-08909-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tsujikawa LM, Fu L, Das S, Halliday C, Rakai BD, Stotz SC, et al. Apabetalone (RVX-208) reduces vascular inflammation in vitro and in CVD patients by a BET-dependent epigenetic mechanism. Clin Epigenet. 2019;11:102. doi: 10.1186/s13148-019-0696-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jahagirdar R, Zhang H, Azhar S, Tobin J, Attwell S, Yu R, et al. A novel BET bromodomain inhibitor, RVX-208, shows reduction of atherosclerosis in hyperlipidemic ApoE deficient mice. Atherosclerosis. 2014;236:91–100. doi: 10.1016/j.atherosclerosis.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 36.Gilham D, Tsujikawa LM, Sarsons CD, Halliday C, Wasiak S, Stotz SC, et al. Apabetalone downregulates factors and pathways associated with vascular calcification. Atherosclerosis. 2019;280:75–84. doi: 10.1016/j.atherosclerosis.2018.11.002. [DOI] [PubMed] [Google Scholar]
- 37.Boshuizen MC, de Winther MP. Interferons as essential modulators of atherosclerosis. Arterioscler Thromb Vasc Biol. 2015;35:1579–1588. doi: 10.1161/ATVBAHA.115.305464. [DOI] [PubMed] [Google Scholar]
- 38.Dasu MR, Devaraj S, Park S, Jialal I. Increased toll-like receptor (TLR) activation and TLR ligands in recently diagnosed type 2 diabetic subjects. Diabetes Care. 2010;33:861–868. doi: 10.2337/dc09-1799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Devaraj S, Dasu MR, Rockwood J, Winter W, Griffen SC, Jialal I. Increased toll-like receptor (TLR) 2 and TLR4 expression in monocytes from patients with type 1 diabetes: further evidence of a pro-inflammatory state. J Clin Endocrinol Metab. 2008;93:578–583. doi: 10.1210/jc.2007-2185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jialal I, Huet BA, Kaur H, Chien A, Devaraj S. Increased toll-like receptor activity in patients with metabolic syndrome. Diabetes Care. 2012;35:900–904. doi: 10.2337/dc11-2375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Okada K, Arai S, Itoh H, Adachi S, Hayashida M, Nakase H, et al. CD68 on rat macrophages binds tightly to S100A8 and S100A9 and helps to regulate the cells' immune functions. J Leukoc Biol. 2016;100:1093–1104. doi: 10.1189/jlb.2A0415-170RRR. [DOI] [PubMed] [Google Scholar]
- 42.Han X, Boisvert WA. Interleukin-10 protects against atherosclerosis by modulating multiple atherogenic macrophage function. Thromb Haemost. 2015;113:505–512. doi: 10.1160/TH14-06-0509. [DOI] [PubMed] [Google Scholar]
- 43.Yin L, Yong-Bo P, Meng-Fei Y, Weiwei C, Ping Z, Lu X, et al. Mice lacking myotubularin-related protein 14 show accelerated high-fat diet-induced lipid accumulation and inflammation. J Physiol Biochem. 2017;73:17–28. doi: 10.1007/s13105-016-0520-6. [DOI] [PubMed] [Google Scholar]
- 44.Liebermann DA, Gregory B, Hoffman B. AP-1 (Fos/Jun) transcription factors in hematopoietic differentiation and apoptosis. Int J Oncol. 1998;12:685–700. doi: 10.3892/ijo.12.3.685. [DOI] [PubMed] [Google Scholar]
- 45.Chan CH, Fang C, Yarilina A, Prinjha RK, Qiao Y, Ivashkiv LB. BET bromodomain inhibition suppresses transcriptional responses to cytokine-Jak-STAT signaling in a gene-specific manner in human monocytes. Eur J Immunol. 2015;45:287–297. doi: 10.1002/eji.201444862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Most J, Schwaeble W, Drach J, Sommerauer A, Dierich MP. Regulation of the expression of ICAM-1 on human monocytes and monocytic tumor cell lines. J Immunol. 1992;148:1635–1642. [PubMed] [Google Scholar]
- 47.Qi XF, Kim DH, Yoon YS, Jin D, Huang XZ, Li JH, et al. Essential involvement of cross-talk between IFN-gamma and TNF-alpha in CXCL10 production in human THP-1 monocytes. J Cell Physiol. 2009;220:690–697. doi: 10.1002/jcp.21815. [DOI] [PubMed] [Google Scholar]
- 48.Gibbons HR, Mi DJ, Farley VM, Esmond T, Kaood MB, Aune TM. Bromodomain inhibitor JQ1 reversibly blocks IFN-gamma production. Sci Rep. 2019;9:10280. doi: 10.1038/s41598-019-46516-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Marie IJ, Chang HM, Levy DE. HDAC stimulates gene expression through BRD4 availability in response to IFN and in interferonopathies. J Exp Med. 2018;215:3194–3212. doi: 10.1084/jem.20180520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.He Y, Hara H, Nunez G. Mechanism and regulation of NLRP3 inflammasome activation. Trends Biochem Sci. 2016;41:1012–1021. doi: 10.1016/j.tibs.2016.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lin J, Kakkar V, Lu X. Essential roles of toll-like receptors in atherosclerosis. Curr Med Chem. 2016;23:431–454. doi: 10.2174/0929867323666151207111408. [DOI] [PubMed] [Google Scholar]
- 52.Foldes G, von Haehling S, Okonko DO, Jankowska EA, Poole-Wilson PA, Anker SD. Fluvastatin reduces increased blood monocyte toll-like receptor 4 expression in whole blood from patients with chronic heart failure. Int J Cardiol. 2008;124:80–85. doi: 10.1016/j.ijcard.2006.12.024. [DOI] [PubMed] [Google Scholar]
- 53.Kong F, Ye B, Lin L, Cai X, Huang W, Huang Z. Atorvastatin suppresses NLRP3 inflammasome activation via TLR4/MyD88/NF-kappaB signaling in PMA-stimulated THP-1 monocytes. Biomed Pharmacother. 2016;82:167–172. doi: 10.1016/j.biopha.2016.04.043. [DOI] [PubMed] [Google Scholar]
- 54.Methe H, Kim JO, Kofler S, Nabauer M, Weis M. Statins decrease toll-like receptor 4 expression and downstream signaling in human CD14+ monocytes. Arterioscler Thromb Vasc Biol. 2005;25:1439–1445. doi: 10.1161/01.ATV.0000168410.44722.86. [DOI] [PubMed] [Google Scholar]
- 55.Connolly M, Veale DJ, Fearon U. Acute serum amyloid A regulates cytoskeletal rearrangement, cell matrix interactions and promotes cell migration in rheumatoid arthritis. Ann Rheum Dis. 2011;70:1296–1303. doi: 10.1136/ard.2010.142240. [DOI] [PubMed] [Google Scholar]
- 56.Hansen IS, Hoepel W, Zaat SAJ, Baeten DLP, den Dunnen J. Serum IgA immune complexes promote pro-inflammatory cytokine production by human macrophages, monocytes, and kupffer cells through FcalphaRI-TLR cross-talk. J Immunol. 2017;199:4124–4131. doi: 10.4049/jimmunol.1700883. [DOI] [PubMed] [Google Scholar]
- 57.Ferreri NR, Howland WC, Spiegelberg HL. Release of leukotrienes C4 and B4 and prostaglandin E2 from human monocytes stimulated with aggregated IgG, IgA, and IgE. J Immunol. 1986;136:4188–4193. [PubMed] [Google Scholar]
- 58.Patry C, Herbelin A, Lehuen A, Bach JF, Monteiro RC. Fc alpha receptors mediate release of tumour necrosis factor-alpha and interleukin-6 by human monocytes following receptor aggregation. Immunology. 1995;86:1–5. [PMC free article] [PubMed] [Google Scholar]
- 59.Cimini FA, Barchetta I, Porzia A, Mainiero F, Costantino C, Bertoccini L, et al. Circulating IL-8 levels are increased in patients with type 2 diabetes and associated with worse inflammatory and cardiometabolic profile. Acta Diabetol. 2017;54:961–967. doi: 10.1007/s00592-017-1039-1. [DOI] [PubMed] [Google Scholar]
- 60.Sajadi SM, Khoramdelazad H, Hassanshahi G, Rafatpanah H, Hosseini J, Mahmoodi M, et al. Plasma levels of CXCL1 (GRO-alpha) and CXCL10 (IP-10) are elevated in type 2 diabetic patients: evidence for the involvement of inflammation and angiogenesis/angiostasis in this disease state. Clin Lab. 2013;59:133–137. doi: 10.7754/Clin.Lab.2012.120225. [DOI] [PubMed] [Google Scholar]
- 61.de Oliveira RT, Mamoni RL, Souza JR, Fernandes JL, Rios FJ, Gidlund M, et al. Differential expression of cytokines, chemokines and chemokine receptors in patients with coronary artery disease. Int J Cardiol. 2009;136:17–26. doi: 10.1016/j.ijcard.2008.04.009. [DOI] [PubMed] [Google Scholar]
- 62.Papadopoulou C, Corrigall V, Taylor PR, Poston RN. The role of the chemokines MCP-1, GRO-alpha, IL-8 and their receptors in the adhesion of monocytic cells to human atherosclerotic plaques. Cytokine. 2008;43:181–186. doi: 10.1016/j.cyto.2008.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Meniailo ME, Malashchenko VV, Shmarov VA, Gazatova ND, Melashchenko OB, Goncharov AG, et al. Interleukin-8 favors pro-inflammatory activity of human monocytes/macrophages. Int Immunopharmacol. 2018;56:217–221. doi: 10.1016/j.intimp.2018.01.036. [DOI] [PubMed] [Google Scholar]
- 64.Gerszten RE, Garcia-Zepeda EA, Lim YC, Yoshida M, Ding HA, Gimbrone MA, Jr, et al. MCP-1 and IL-8 trigger firm adhesion of monocytes to vascular endothelium under flow conditions. Nature. 1999;398:718–723. doi: 10.1038/19546. [DOI] [PubMed] [Google Scholar]
- 65.Takahashi M, Ikeda U, Masuyama J, Kitagawa S, Kasahara T, Shimpo M, et al. Monocyte-endothelial cell interaction induces expression of adhesion molecules on human umbilical cord endothelial cells. Cardiovasc Res. 1996;32:422–429. doi: 10.1016/0008-6363(96)00085-5. [DOI] [PubMed] [Google Scholar]
- 66.Kamari Y, Shaish A, Shemesh S, Vax E, Grosskopf I, Dotan S, et al. Reduced atherosclerosis and inflammatory cytokines in apolipoprotein-E-deficient mice lacking bone marrow-derived interleukin-1alpha. Biochem Biophys Res Commun. 2011;405:197–203. doi: 10.1016/j.bbrc.2011.01.008. [DOI] [PubMed] [Google Scholar]
- 67.Lurier EB, Dalton D, Dampier W, Raman P, Nassiri S, Ferraro NM, et al. Transcriptome analysis of IL-10-stimulated (M2c) macrophages by next-generation sequencing. Immunobiology. 2017;222:847–856. doi: 10.1016/j.imbio.2017.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Mattiola I, Tomay F, De Pizzol M, Silva-Gomes R, Savino B, Gulic T, et al. The macrophage tetraspan MS4A4A enhances dectin-1-dependent NK cell-mediated resistance to metastasis. Nat Immunol. 2019;20:1012–1022. doi: 10.1038/s41590-019-0417-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.De Arras L, Alper S. Limiting of the innate immune response by SF3A-dependent control of MyD88 alternative mRNA splicing. PLoS Genet. 2013;9:e1003855. doi: 10.1371/journal.pgen.1003855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Barrat FJ, Crow MK, Ivashkiv LB. Interferon target-gene expression and epigenomic signatures in health and disease. Nat Immunol. 2019;20:1574–1583. doi: 10.1038/s41590-019-0466-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Das S, Reddy MA, Senapati P, Stapleton K, Lanting L, Wang M, et al. Diabetes mellitus-induced long noncoding RNA Dnm3os regulates macrophage functions and inflammation via nuclear mechanisms. Arterioscler Thromb Vasc Biol. 2018;38:1806–1820. doi: 10.1161/ATVBAHA.117.310663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Li Y, Reddy MA, Miao F, Shanmugam N, Yee JK, Hawkins D, et al. Role of the histone H3 lysine 4 methyltransferase, SET7/9, in the regulation of NF-kappaB-dependent inflammatory genes. Relevance to diabetes and inflammation. J Biol Chem. 2008;283:26771–26781. doi: 10.1074/jbc.M802800200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Greissel A, Culmes M, Burgkart R, Zimmermann A, Eckstein HH, Zernecke A, et al. Histone acetylation and methylation significantly change with severity of atherosclerosis in human carotid plaques. Cardiovasc Pathol. 2016;25:79–86. doi: 10.1016/j.carpath.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 74.van der Kroef M, Castellucci M, Mokry M, Cossu M, Garonzi M, Bossini-Castillo LM, et al. Histone modifications underlie monocyte dysregulation in patients with systemic sclerosis, underlining the treatment potential of epigenetic targeting. Ann Rheum Dis. 2019;78:529–538. doi: 10.1136/annrheumdis-2018-214295. [DOI] [PubMed] [Google Scholar]
- 75.Kanter JE, Hsu CC, Bornfeldt KE. Monocytes and macrophages as protagonists in vascular complications of diabetes. Front Cardiovasc Med. 2020;7:10. doi: 10.3389/fcvm.2020.00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Swirski FK, Libby P, Aikawa E, Alcaide P, Luscinskas FW, Weissleder R, et al. Ly-6Chi monocytes dominate hypercholesterolemia-associated monocytosis and give rise to macrophages in atheromata. J Clin Invest. 2007;117:195–205. doi: 10.1172/JCI29950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Parathath S, Grauer L, Huang LS, Sanson M, Distel E, Goldberg IJ, et al. Diabetes adversely affects macrophages during atherosclerotic plaque regression in mice. Diabetes. 2011;60:1759–1769. doi: 10.2337/db10-0778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Nagareddy PR, Murphy AJ, Stirzaker RA, Hu Y, Yu S, Miller RG, et al. Hyperglycemia promotes myelopoiesis and impairs the resolution of atherosclerosis. Cell Metab. 2013;17:695–708. doi: 10.1016/j.cmet.2013.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Szentes V, Gazdag M, Szokodi I, Dezsi CA. The role of CXCR3 and associated chemokines in the development of atherosclerosis and during myocardial infarction. Front Immunol. 2018;9:1932. doi: 10.3389/fimmu.2018.01932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ucla C, Roux-Lombard P, Fey S, Dayer JM, Mach B. Interferon gamma drastically modifies the regulation of interleukin 1 genes by endotoxin in U937 cells. J Clin Invest. 1990;85:185–191. doi: 10.1172/JCI114411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Jiang X, Wang F, Wang Y, Gistera A, Roy J, Paulsson-Berne G, et al. Inflammasome-driven interleukin-1alpha and interleukin-1beta production in atherosclerotic plaques relates to hyperlipidemia and plaque complexity. JACC Basic Transl Sci. 2019;4:304–317. doi: 10.1016/j.jacbts.2019.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med. 2017;377:1119–1131. doi: 10.1056/NEJMoa1707914. [DOI] [PubMed] [Google Scholar]
- 83.Nicholls SJ, Ray KK, Johansson JO, Gordon A, Sweeney M, Halliday C, et al. Selective BET protein inhibition with apabetalone and cardiovascular events: a pooled analysis of trials in patients with coronary artery disease. Am J Cardiovasc Drugs. 2018;18:109–115. doi: 10.1007/s40256-017-0250-3. [DOI] [PubMed] [Google Scholar]
- 84.Ray KK, Nicholls SJ, Buhr KA, Ginsberg HN, Johansson JO, Kalantar-Zadeh K, et al. Effect of apabetalone added to standard therapy on major adverse cardiovascular events in patients with recent acute coronary syndrome and type 2 diabetes: a randomized clinical trial. JAMA. 2020;323(16):1565–1573. doi: 10.1001/jama.2020.3308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ray KK, Nicholls SJ, Ginsberg HD, Johansson JO, Kalantar-Zadeh K, Kulikowski E, et al. Effect of selective BET protein inhibitor apabetalone on cardiovascular outcomes in patients with acute coronary syndrome and diabetes: rationale, design, and baseline characteristics of the BETonMACE trial. Am Heart J. 2019;217:72–83. doi: 10.1016/j.ahj.2019.08.001. [DOI] [PubMed] [Google Scholar]
- 86.Schnitzler JG, Bernelot Moens SJ, Tiessens F, Bakker GJ, Dallinga-Thie GM, Groen AK, et al. Nile red quantifier: a novel and quantitative tool to study lipid accumulation in patient-derived circulating monocytes using confocal microscopy. J Lipid Res. 2017;58:2210–2219. doi: 10.1194/jlr.D073197. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1–3. Additional file 1. Analysis of monocyte subpopulations in control (CTL) and DM2+CVD patients. Monocytes were classified as classical (CD14++CD16−), intermediate (CD14++CD16+) or non-classical (CD14+CD16+). Fluorescence was measured using a FACS CANTO II (BD) and analysed with FlowJo software. Additional file 2. Monocytes were stimulated ex vivo with IFNγ (1.5, 3.12, 6.25, 12.5 or 25 U/ml), apabetalone (1.5, 3.12, 6.25, 12.5 or 25 μM), or a combination of both stimuli for 24h. Subsequently, cytotoxicity was determined by measuring the enzyme lactate dehydrogenase (LDH) in the supernatant using the CytoTox 96® non-radioactive cytotoxicity assay (Promega). There was no difference between ‘unstimulated’ and ‘stimulated’ conditions, except for the positive control where p < 0.0001. Statistics: One-way ANOVA with Dunnett’s multiple comparisons test. Additional file 3. BRD4 mRNA expression is reduced by ex vivo treatment with apabetalone in DM2+CVD monocytes (4h ex vivo treatment, 25 μM). BRD4 expression was measured by real-time PCR and normalized to cyclophilin A (endogenous control). Statistics: Unpaired Student’s t-test, ****, p < 0.0001.
Additional file 4–7. Additional file 4. Apabetalone’s gene targets in IPA® canonical pathways gene sets: Unstimulated control and DM2+CVD monocytes treated with apabetalone ex vivo. Additional file 5. Apabetalone’s gene targets that converge on IPA® upstream regulators: unstimulated monocytes treated with apabetalone ex vivo. Additional file 6. Apabetalone’s gene targets within IPA® canonical pathways: IFNγ stimulated monocytes treated with apabetalone ex vivo. Additional file 7. Apabetalone’s gene targets in IPA® upstream regulators gene sets: IFNγ stimulated control and DM2+CVD patient monocytes treated with apabetalone ex vivo.
Data Availability Statement
All data generated or analysed during this study are included in this published article and its supplementary information files.