Abstract
Aim
To establish contact lens wear and care practices during the COVID-19 pandemic in Spain.
Method
A 58-item anonymous online survey was distributed during the period 30th April to 10th May via Qualtrics. The survey explored: a) demographic characteristics (age, sex, general health and where they were living during lockdown), b) changes in their contact lens use during lockdown, c) hygiene and contact lens compliance and d) concerns associated with contact lens wear and ways to support wearers during the pandemic.
Results
Two hundred and sixty responses were analysed (38.8 ± 11.4 years old, 75% female). Three-quarters of participants reported that they were self-isolating or rigorously following social distancing advice. Sixty-seven percent of participants reported using their contact lenses less during the pandemic. Respondents were found to be compliant with handwashing prior to inserting and removing contact lenses (in both cases 97% doing this ‘most times’ or ‘every time’). However, only 44 % complied with the ‘20 s rule’ and 48 % used a shared towel to dry their hands. A higher proportion of hydrogen peroxide users replaced the lens case monthly compared to multi-purpose users (64% vs.49%; p < 0.001). Twenty-four percent admitted wearing lenses whilst showering and 16% did not consider ceasing lens wear if feeling unwell with flu/cold symptoms.
Conclusion
Eye care practitioners should continue to educate contact lens wearers to ensure safe contact lens wear to minimise the chance of developing contact lens related complications during the pandemic. Modifiable factors that need particular attention in Spain include: handwashing for at least 20s before lens handling, drying hands with single use paper towels, including a rub-and-rinse step for reusable lenses, lens case cleaning and renewal, avoidance of water exposure and when to cease lens wear during the pandemic.
Keywords: Contact lens, COVID-19, Compliance, Education, Complications, Microbial keratitis, Acanthamoeba
1. Introduction
Coronavirus disease 2019 (COVID-19) has experienced a rapid spread globally since December 2019 [1], with the World Health Organisation (WHO) declaring it a pandemic on 11th March 2020. Spain was one of the first European countries affected by the COVID-19 outbreak [2] leading to one of Europe’s strictest and longest lockdowns (state of alarm started on 14th March and ended on 21st June). Spanish residents were mandated to stay at home except to purchase food/medicines, to travel to work or to attend emergencies. Non-essential shops and businesses (including optical/optometric practices) were closed. Stress and anxiety increased significantly during lockdown [3], promoted by concerns about how to avoid infection and the continuously increasing number of deaths. This was exacerbated by significant amounts of misinformation and speculation [4] including inaccurate information around the increased risk of COVID-19 associated with contact lens wear [5].
The COVID-19 pandemic has highlighted the importance of optimal hygiene and lens care to avoid contact lens related complications [5]. The aim of the current study was to evaluate by means of a survey the behaviours associated with contact lens wear (compliance with hand hygiene and adherence to contact lens wear and care recommendations) as well as to elucidate the best ways to support wearers during the COVID-19 pandemic in Spain. To date, limited information exists about contact lens compliance in Spain before [6] and during the COVID-19 pandemic [7]. Similar work related to contact lens compliance during the COVID-19 pandemic has been conducted in the UK [8]. Given the prescribing differences between markets, with a larger number of reusable and rigid/orthokeratology wearers in Spain compared with the UK [9], and different government approaches to control the virus impact, it is important to identify country-specific wearer behaviours that need addressing during these challenging clinical times.
2. Materials and methods
The study was conducted in agreement with the tenets of the Declaration of Helsinki. The Faculty of Science and Engineering Research Ethics Panel at Anglia Ruskin University (ARU) reviewed and approved the study protocol. Qualtrics software (Qualtrics, Provo, UT) was used to collect data via an online questionnaire. Only one submission from each IP address was permitted by the survey software. Non-identifiable data were collected, and all participants gave their informed consent online after reading a participant information sheet at the start of the survey. The inclusion criteria included adults older than 18 who were using contact lenses and living in Spain during the lockdown due to the COVID-19 pandemic.
2.1. Survey characteristics and distribution
The survey used was translated and adapted to accommodate for the Spanish lockdown characteristics from a survey distributed in the UK [8]. The survey had 58 questions divided into 4 sections. The first section focused on assessing the demographic characteristics of the participants such as age, sex, general heath, and where they were living during the lockdown. The second section asked about potential changes in their habits related to the use of contact lenses (CLs) due to the lockdown. The third section focused on hygiene and contact lens compliance during the COVID-19 pandemic (e.g. washing hands, lens care, lens case replacement). The questions related to lens care disinfection and lens case care were only displayed if the participant used reusable CLs. The final section focused on assessing concerns associated with contact lens wear and ways to best support wearers during the COVID-19 pandemic. Respondents were also asked about compliance with recommendations regarding safe contact lens wear given by their eye care professionals (ECPs).
The translation into English followed a multi-step process to ensure optimal accuracy. Initial drafts were compared to the original English questionnaire to ensure the meaning of the questions were kept. The survey was then reviewed by a team of four Spanish optometrists (all authors of this manuscript, NG-P, MV-E, DP and LSM) as a final step during the translation process to refine the final wording of the questions. The final version was inputted into Qualtrics (Qualtrics, Provo, UT) and then reviewed by team members to ensure functionality. The survey was distributed using social media and was open from 30th April to 10th May 2020 when optical/optometric practices in Spain were either closed or only offered urgent/emergency care. A copy of the full questionnaire can be requested by contacting the corresponding author.
2.2. Data analysis
The Statistical Package for Social Sciences version 26.0 (SPSS Inc., Chicago, IL, USA) was used to carry out the statistical analysis. Chi-square statistics for categorical variables (or Fisher’s exact test if the number of participants in any group was 5 or less) was used to assess differences between lens types (daily disposable vs reusable CL) and between lens care products (multi-purpose disinfecting solution vs hydrogen peroxide). A significant level of p ≤ 0.05 was used for all analyses.
3. Results
3.1. Patient demographics
A total of 396 participants completed the anonymous online survey. Before data analysis, responses were removed under the following circumstances: those living outside of Spain (n = 38), those not consenting to take part in the study (n = 19), when only some initial questions regarding sex and location were completed (n = 78) and those younger than 18 years (n = 1). A total of 260 respondents were suitable for analysis. The mean age of the respondents was 38.8 ± 11.4 years old (range 18-72 years) and 75% were female. Respondents’ demographics and COVID-19 symptomatology are shown in Table 1 .
Table 1.
Demographics characteristics of the respondents (n = 260).
| Characteristics | Percentage (n) | |
|---|---|---|
| Sex | Female | 75 (196) |
| Male | ||
| 25 (64) | ||
| Do you suffer from any chronic disease? | Yes | 17 (45) |
| No | ||
| 83 (215) | ||
| Do you have any COVID-19 symptoms? | Yes | 7 (17) |
| No | ||
| 94 (243) | ||
| Does anyone in your household have symptoms of COVID-19? | Yes | 10 (27) |
| No | ||
| 90 (233) | ||
| Are you a smoker? | Yes | 14 (37) |
| No | ||
| 86 (223) | ||
| Where do you live? | City | 71 (185) |
| Village or rural area | ||
| 29 (75) | ||
| Does your house/flat have outdoor space (garden/patio)? | Yes | 50 (131) |
| No | ||
| 50 (129) | ||
| To what extent are you following social distancing advice? | Self-isolating or rigorously following advice | 75 (196) |
| Going to work | ||
| 25 (64) | ||
3.2. Contact lenses and lens care products used during the pandemic
The reported frequency of contact lens modality and use of lens care products for lens disinfection is presented in Tables 2 and 3 .
Table 2.
Reported frequency of contact lens modality worn by the respondents (n = 260); OK = orthokeratology.
| Lens modality | n | Percentage |
|---|---|---|
| Daily disposable | 82 | 32% |
| Soft reusable | 161 | 62% |
| Rigid (including OK) | 17 | 7% |
Table 3.
Reported frequency of lens care disinfection used by the respondents ; OK = orthokeratology.
| Lens care disinfection method used with SOFT REUSABLE CLs (n = 161) | n | Percentage | Lens care disinfection method used with RIGID/OK CLs (n = 17) | n | Percentage |
|---|---|---|---|---|---|
| Multi-purpose solution | 144 | 90% | Multi-purpose solution | 8 | 47% |
| Hydrogen peroxide | 6 | 4% | Hydrogen peroxide | 5 | 29% |
| Saline | 9 | 6% | Saline | 1 | 6% |
| Not provided | 2 | 1% | Cleaner & conditioner solutions | 3 | 18% |
3.3. Contact lens wear before and during the COVID-19 pandemic
Sixty-seven percent of respondents reported using their contact lenses less during the pandemic, 30% about the same amount of time and only 2% more during the pandemic. The most common reason for reduced wearing time was ‘less need at home’ (56%) followed by ‘less effort to wear specs’ (20%) and ‘fear of infection/touching eyes’ (10%). At the time of the survey, 65% of the respondents had not needed to buy any contact lenses during the lockdown period, 28% were purchasing them from their optometrist, 4% from the internet and 3% through eye clinics or hospital departments. There were no statistically significant differences in wearing time between daily disposable wearers and reusable contact lens wearers (p = 0.143).
3.4. Handwashing
Seventy-five percent of respondents reported a change in their handwashing routine during the pandemic. Self-reports of hand washing prior to inserting and after removing contact lens with either ‘most times’ or’ every time’ were similar (both 97%). In addition, 97% also responded using soap and water during handwashing. In contrast, only 44% reported following the 20-second rule ‘every time’ (with a further 43% doing it ‘most times’) and 25% reported washing their hands ‘every time’ after coughing, sneezing or blowing their nose (with a further 43% doing it ‘most times’). When asked about how they dried their hands, the responses included: cloth towel shared with other family members (48%), cloth towel only used by themselves (39%), paper towel (12%). There were no statistically significant differences between daily disposable and reusable lens wearers for handwashing before inserting and removing contact lenses (p = 0.716 and p = 0.214 respectively), handwashing method (i.e. using soap and water, water only, antibacterial wipes/solutions p = 0.214) and for drying habits (as per above options, p = 0.151).
3.5. Compliance with the cleaning routine of lenses and lens cases for wearers of soft reusable contact lenses (n = 144)
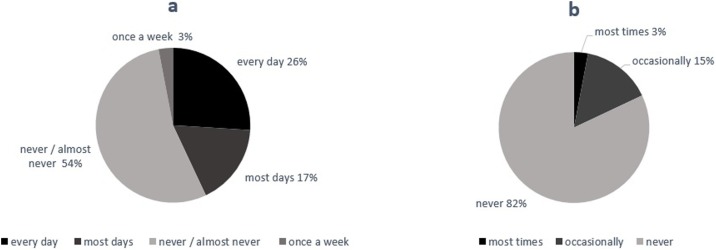
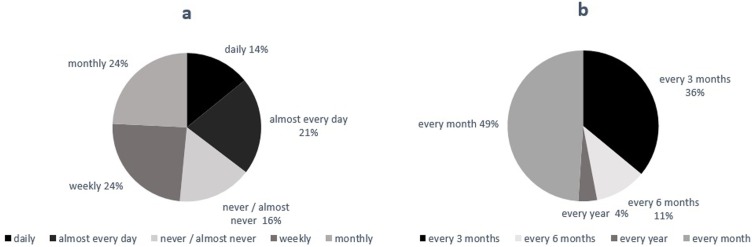
As shown in Table 3, the majority of respondents used a multi-purpose lens solution for disinfection of their reusable contact lenses. First, the survey assessed aspects related to the cleaning of the lenses after use (Fig. 1 a–b). The survey found that 54% of respondents ‘never’ rubbed the lenses before soaking and 18% either topped up the lens care solution ‘most times’ or ‘occasionally’ (rather than filling up the case with fresh solution). The survey also evaluated aspects related to the care of the lens case. Fig. 2 a–b summarises the findings pertaining to cleaning routines for lens cases. Eighty-six percent of respondents admitted to cleaning the lens case less often than daily. The frequency of replacement of lens cases during the pandemic varied ranging from monthly (49%), 3-monthly (36%), 6-monthly (11%) and annually (4%). Respondents also reported their daily routine for cleaning the lens case which included the following non-optimal behaviours: 46% rinsed with tap water (with 2 respondents specifically using boiled water) and 8% not cleaning the lens case at all. The remaining responses included: 26% rinsing with lens solution, 7% rinsing the case with contact lens solution and wiping it with a clean tissue (optimal technique [10]), 2% wiping with a tissue only and 9% replacing the solution only without rinsing/wiping.
Fig. 1.
a-b Reported frequencies of multi-purpose solution users (n = 144): a) rubbing soft reusable contact lenses after each use and b) topping up solution.
Fig. 2.
a-b Reported frequencies of: a) contact lens case cleaning and b) contact lens case replacement for soft reusable lens wearers using multi-purpose solution (n = 144).
3.6. Compliance with the cleaning routine of lenses and lens cases for wearers of rigid contact lenses (n = 11)
Similar analyses were conducted to establish the cleaning routine of wearers of rigid lenses, using either a multi-purpose solution or two-step cleaning routine (cleaner and conditioner, Table 3). When asked about rubbing prior to soaking, 45% of respondents admitted they ‘never/almost never’ did this step and a further 18% did it only once a week (with the remaining doing it ‘daily’/’almost every day’). Respondents showed a more compliant behaviour with regards to topping up the solution, 82% indicated they ‘never’ topped up and the remainder only did it ‘occasionally’. With regards to the care of the lens case, 30% reported cleaning the case ‘daily’ with a further 20% cleaning it ‘most days’ and the remaining respondents cleaning less frequently or never. In addition, 50% of the respondents admitted using tap water. Only one respondent used the optimal method (rinsing and dying with paper tissue). During the pandemic, the majority of respondents were planning on replacing the lens case monthly (40%) or 3-monthly (30%) with the remaining planning on changing it less often.
3.7. Compliance with Hydrogen Peroxide solutions for soft and rigid lens wearers (n = 11)
A separate analysis was conducted with all reusable lens wearers using hydrogen peroxide as part of their lens disinfection in this study (n = 11 for both soft and rigid lens wearers as shown in Table 3). Around half (55%) of the respondents rubbed their lenses prior to soaking ‘daily’/’almost daily’ (remaining respondents ‘never/almost never’ included this step as part of their cleaning routine). In addition, 73% ‘never’ topped up the used solution, with the remaining respondents doing this ‘always’ (9%) or ‘frequently’ (18%). Non-compliance was observed with aspects relating to the care of the lens case including 64% cleaning the lens case ‘weekly’ or ‘monthly’ or ‘not at all’. A further 50% admitted using tap water whilst cleaning the contact lens case and 64% were planning on replacing the case monthly during the pandemic (with the remaining 36% planning on replacing it yearly).
A statistically significant difference was found between the lens case replacement frequency of contact lens wearers using hydrogen peroxide and those using multi-purpose solutions (p < 0.001). Sixty-four percent of peroxide users replace their lens case monthly whilst only 49% of multi-purpose solution users reported doing this.
3.8. Compliance with general Eye Care Professional (ECP) recommendations for safe contact lens wear
Ninety-seven percent said that they were not exceeding the wearing time during the pandemic (e.g. sleeping in lenses if not previously recommended) and 88% also followed the recommendations regarding disposal of their contact lenses. The main reasons given by the 31 respondents that did not follow recommendations on disposal included ‘forgetting when to replace’, ‘to save money’ and ‘doesn’t hurt my eyes’ (28%, 21% and 21% respectively).
The survey explored if wearers wore contact lenses whilst showering, with 76% responding negatively to this question. In addition, the survey explored if users checked the health of their eyes daily before inserting lenses with 28% admitting skipping this health check. A further 16% responded that they would not consider ceasing lens wear during the pandemic if feeling unwell with cold or flu symptoms. Of all respondents, 6% did not own a pair of up to date spectacles. The survey also asked how often respondents cleaned their spectacles with soap and water: 33% admitted doing this ‘hardly ever’ or ‘never’, 24% ‘daily/almost daily’ and 44% ‘frequently’.
Finally, 80% had not sought any form of additional support for managing their contact lens wear during the pandemic, but 13% consulted with their optometrist/ophthalmologist/medical practitioner and 7% searched for information online. Respondents were given space to add free texts regarding ways in which they would like to receive support regarding contact lens wear during the pandemic. Of those that responded, the preferred method was online (n = 116), via telehealth (phone or video call, n = 78) or both (n = 6). They also expressed videos and links to relevant sites through a health portal would be useful to support relevant aspects of contact lens wear, such as the cleaning of contact lenses and the impact of COVID-19 on lens wear (n = 6).
4. Discussion
Since the start of the COVID-19 pandemic, the contact lens community has been interested in how to best support wearers [7,8,11]. The demographics of the respondents in this study are in agreement with data for the Spanish market in terms of sex, age of wearers and types of lenses worn [9], and so are representative. In this study, 75% of respondents were socially distancing and or self-isolating when responding to the survey. The current study is in accordance with other work conducted during the COVID-19 pandemic and shows a reduction in lens wear during lockdown [7,8,11].
Optimal handwashing before contact lens application and removal is essential [5,7]. Effective handwashing with soap and water should take a minimum of 20s [12,13]. However, less than half of respondents admitted to complying with this rule. Garcia-Ayuso et al. [7] also found 27.6% of participants were unaware or did not follow this rule. During the pandemic, Spain emphasised good handwashing technique rather than duration in their public health campaigns [14]. The greater awareness of hand hygiene created by the pandemic may have increased hand washing prior to lens handling as only 2% of respondents admitted to not washing their hands prior to application/removal of lenses. Interestingly, only a quarter of respondents admitted washing their hands after coughing, sneezing or blowing their nose. The use of paper towels does not seem to be an established method for drying hands in this study (only 12% of respondents used this method). Despite recommendations to dry hands with a single use paper towel [5,12], 39% of participants admitted to using their own reusable towel and 48% admitted to sharing a towel. In view of these non-optimal behaviours, ECP are encouraged to discuss optimal handwashing and drying techniques and ensure wearers do not become complacent as inadequate handwashing is a risk factor for contact lens related microbial keratitis and corneal inflammatory events [15].
Despite the known benefits of rubbing contact lens prior to soaking [16,17], reusable lens wearers using multi-purpose solution in this study often skipped this cleaning step. In addition, 27% admitted topping up multi-purpose lens solution frequently or always. In contrast, 67% of soft reusable lens wearers in the UK were non-compliant with topping up highlighting differences between countries during early periods of lockdown in the COVID-19 pandemic [8]. Although the present study asked about rubbing, the survey did not include a specific question about rinsing. Interestingly, there is no specific mention of rinsing in the recommendations for cleaning contact lenses [18]. ECPs in Spain will need to reinforce the importance of rub-and-rinse during the pandemic. Jones et al. [5] indicated, that in principle, the presence of surfactants in multi-purpose solutions together with rubbing/rinsing steps are likely to be effective against SARS-CoV-2 but further work in this area is required. While a recent review suggested (with no cited evidence) that no rubbing/rinsing is required prior to lens disinfection when using hydrogen peroxide solutions [19], the cleanliness (which is linked to comfort and risk of infection) of RGP and soft lenses soaked in multi-purpose or hydrogen peroxide solution is better after rubbing and rinsing [[20], [21], [22], [23]]. The survey data showed that 55% of the respondents rubbed their lenses prior to soaking with hydrogen peroxide solution. The survey did not capture how respondents were instructed on lens care procedures when using hydrogen peroxide solutions but ECPs need to be careful to only adopt evidence-based recommendations. Nichols et al. [19] suggested that peroxide systems should be the first-line recommendation for most wearers of reusable lenses and several organizations [16,17] indicate that peroxide-based solutions should be effective against the virus that causes COVID-19. Finally, Garcia-Ayuso et al. [7] noticed that Spanish wearers changed their frequency of wear to occasional use during the pandemic. Therefore, when providing instructions about the correct use of solutions ECP will also need to include advice regarding storage of irregularly worn reusable lenses and how frequently solutions need to be changed.
Previous studies have found that lens cases receive much less cleaning attention than contact lenses [24,25]. In fact, in this study, 64% of users (the same percentage was found for soft multi-purpose users and peroxide users) admitted cleaning the lens case either ‘weekly’, ‘monthly’ or ‘never/almost never’. In contrast, Wu et al. [10] reported that an effective lens case cleaning process should include rubbing the lens case, rinsing it with contact lens disinfecting solution, wiping it with a tissue and drying it face down with air. Current advice suggests regular case replacement [5,10] as infrequent lens case replacement increases the risk of suffering ocular infection [26,27]. Nichols et al. [19] noted that peroxide-based systems improve compliance with lens case replacement. In agreement with this, a statistically significant difference was found in the present work between lens care types (peroxide users were more likely to replace their cases monthly than multi-purpose users). As wearers’ behaviours are clearly sub-optimal with regards to lens case cleaning and replacement, ECPs and the research contact lens community are encouraged to find strategies to further educate wearers on these aspects during the pandemic.
Finally, the survey explored how well respondents were adhering to contact lens recommendations for safe contact lens wear. Overall, wearers adhered to recommendations regarding wearing time and disposal of contact lenses, however, 28% did not check their eyes daily before inserting lenses and 16% would not consider stopping lens wear if feeling unwell with flu/cold symptoms. Twenty four percent admitted wearing lenses whilst showering. Exposure to water during handling (rinsing contact lenses or lens cases with tap water) and/or wearing contact lenses whilst showering has shown to be a risk factor for infection [27]. Unfortunately, respondents of this study showed both behaviours (showering as well as use of tap water during lens case cleaning). Similarly, Vianya-Estopa et al. [8] reported 26% of UK wearers showered with contact lenses during the pandemic. Arshad et al. [28] has demonstrated an improvement in water-contact behaviours with the use of a no-water infographic and similar work should be attempted in countries like Spain (where swimming is a popular activity, especially during the summer months).
The present work highlights modifiable behaviours that need to be improved in contact lens compliance during the COVID-19 pandemic. Respondents indicated their preferred ways to be supported during lockdown which includes telehealth (either phone and/or video consultations) and access to educational tools online. Since the end of the lockdown in June, Spain has already experienced a resurgence of new infections and the affected regions have experienced further restrictions in an attempt to control the spread of the infection [29]. As access to clinical care might continue to be limited over the coming months, ECPs are encouraged to review patient education on safe contact lens wear and care to minimise the chance of contact lens related complications. Daily disposables offer an advantage over reusable lenses in terms of non-compliance with cleaning and care procedures (relying on optimal handwashing only) [30,31]. Nagra et al. [32] highlight that aftercare appointments had traditionally offered an ideal opportunity to assess contact lens compliance, but in the current times ECPs are encouraged to also use alternative ways (e.g. videos or patient information sheets, raising awareness of lens care phone apps). The latter will be necessary particularly if optometric practices need to prioritise face-to-face appointments for urgent and emergency contact lens related complications where non-symptomatic wearers may attend aftercare appointments less regularly.
Funding
None received for this study
References
- 1.Spiteri G., Fielding J., Diercke M., Campese C., Enouf V., Gaymard A. First cases of coronavirus disease 2019 (COVID-19) in the WHO European Region, 24 January to 21 February 2020. Euro Surveill. 2020:25. doi: 10.2807/1560-7917.ES.2020.25.9.2000178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ceylan Z. Estimation of COVID-19 prevalence in Italy, Spain, and France. Sci Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.138817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ozamiz-Etxebarria N., Dosil-Santamaria M., Picaza-Gorrochategui M., Idoiaga-Mondragon N. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cad Saude Publica. 2020;36 doi: 10.1590/0102-311X00054020. [DOI] [PubMed] [Google Scholar]
- 4.Hernandez-Garcia I., Gimenez-Julvez T. Characteristics of YouTube Videos in Spanish on How to Prevent COVID-19. Int J Environ Res Public Health. 2020:17. doi: 10.3390/ijerph17134671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jones L., Walsh K., Willcox M., Morgan P., Nichols J. The COVID-19 pandemic: Important considerations for contact lens practitioners. Cont Lens Anterior Eye. 2020;43:196–203. doi: 10.1016/j.clae.2020.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morgan P.B., Efron N., Toshida H., Nichols J.J. An international analysis of contact lens compliance. Cont Lens Anterior Eye. 2011;34:223–228. doi: 10.1016/j.clae.2011.08.001. [DOI] [PubMed] [Google Scholar]
- 7.Garcia-Ayuso D., Escamez-Torrecilla M., Galindo-Romero C., Valiente-Soriano F.J., Moya-Rodriguez E., Sobrado-Calvo P. Influence of the COVID-19 pandemic on contact lens wear in Spain. Cont Lens Anterior Eye (In press) 2020 doi: 10.1016/j.clae.2020.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vianya-Estopa M., Wolffsohn J.S., Beukes E., Trott M., Smith L., Allen P. Soft contact lens wearers’ compliance during the COVID-19 pandemic. Cont Lens Anterior Eye (In press) 2020 doi: 10.1016/j.clae.2020.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.W.C. Morgan PB, Tranoudis I.G., Efron N., Jones L., Merchan N.L. International contact lens prescribing in 2019. Cont Lens Spectr. 2020;(January):26–32. [Google Scholar]
- 10.Wu Y.T., Willcox M., Zhu H., Stapleton F. Contact lens hygiene compliance and lens case contamination: a review. Cont Lens Anterior Eye. 2015;38:307–316. doi: 10.1016/j.clae.2015.04.007. [DOI] [PubMed] [Google Scholar]
- 11.Morgan P.B. Contact lens wear during the COVID-19 pandemic. Cont Lens Anterior Eye. 2020;43:213. doi: 10.1016/j.clae.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organisation; 2020. Clean care is safer care: clean hands protect against infection.https://www.who.int/gpsc/clean_hands_protection/en/ [Accessed 17 Aug 2020] [Google Scholar]
- 13.Centers for Disease Control and Prevention; 2020. When and how to wash your hands.https://www.cdc.gov/handwashing/when-how-handwashing.html [Accessed 17 Aug 2020] [Google Scholar]
- 14.Spanish Ministry of Health; 2020. Programa Higiene de Manos – diez preguntas clave sobre la higiene de manos.https://www.seguridaddelpaciente.es/es/practicas-seguras/programa-higiene-manos/diez-preguntas-clave-sobre-higiene-manos/#n7 [Accessed 17 Aug 2020] [Google Scholar]
- 15.Fonn D., Jones L. Hand hygiene is linked to microbial keratitis and corneal inflammatory events. Cont Lens Anterior Eye. 2019;42:132–135. doi: 10.1016/j.clae.2018.10.022. [DOI] [PubMed] [Google Scholar]
- 16.Spanish General Council of Optometry; 2020. Protocolos de higienización y seguridad en los establecimientos sanitarios de óptica y otros lugares de ejercicio professional version 1.1.http://cgcoo.es/descargas/protocolos/Protocolos%20de%20higienizacion.pdf [Accessed 17 Aug 2020] [Google Scholar]
- 17.Centers for Disease Control and Prevention; 2020. Contact lens care systems and solutions.https://www.cdc.gov/contactlenses/care-systems.html [Accessed 17 Aug 2020] [Google Scholar]
- 18.Spanish General Council of Optometry; 2020. Cuida la higiene de tus lentes de contacto.https://www.cnoo.es/lentes-de-contacto-2/cuida-higiene-de-tus-lentes-de-contacto [Accessed 17 Aug 2020] [Google Scholar]
- 19.Nichols J.J., Chalmers R.L., Dumbleton K., Jones L., Lievens C.W., Merchea M.M. The Case for Using Hydrogen Peroxide Contact Lens Care Solutions: A Review. Eye Contact Lens. 2019;45:69–82. doi: 10.1097/ICL.0000000000000542. [DOI] [PubMed] [Google Scholar]
- 20.Cho P., Poon H.Y., Chen C.C., Yuon L.T. To rub or not to rub? - effective rigid contact lens cleaning. Ophthalmic Physiol Opt. 2020;40:17–23. doi: 10.1111/opo.12655. [DOI] [PubMed] [Google Scholar]
- 21.Cho P., Cheng S.Y., Chan W.Y., Yip W.K. Soft contact lens cleaning: rub or no-rub? Ophthalmic Physiol Opt. 2009;29:49–57. doi: 10.1111/j.1475-1313.2008.00606.x. [DOI] [PubMed] [Google Scholar]
- 22.Zhu H., Bandara M.B., Vijay A.K., Masoudi S., Wu D., Willcox M.D. Importance of rub and rinse in use of multipurpose contact lens solution. Optom Vis Sci. 2011;88:967–972. doi: 10.1097/OPX.0b013e31821bf976. [DOI] [PubMed] [Google Scholar]
- 23.Kilvington S., Lonnen J. A comparison of regimen methods for the removal and inactivation of bacteria, fungi and Acanthamoeba from two types of silicone hydrogel lenses. Cont Lens Anterior Eye. 2009;32:73–77. doi: 10.1016/j.clae.2008.12.008. [DOI] [PubMed] [Google Scholar]
- 24.Yung M.S., Boost M., Cho P., Yap M. Microbial contamination of contact lenses and lens care accessories of soft contact lens wearers (university students) in Hong Kong. Ophthalmic Physiol Opt. 2007;27:11–21. doi: 10.1111/j.1475-1313.2006.00427.x. [DOI] [PubMed] [Google Scholar]
- 25.Boost M.V., Cho P. Microbial flora of tears of orthokeratology patients, and microbial contamination of contact lenses and contact lens accessories. Optom Vis Sci. 2005;82:451–458. doi: 10.1097/01.opx.0000168587.72893.ec. [DOI] [PubMed] [Google Scholar]
- 26.Stapleton F., Edwards K., Keay L., Naduvilath T., Dart J.K., Brian G. Risk factors for moderate and severe microbial keratitis in daily wear contact lens users. Ophthalmology. 2012;119:1516–1521. doi: 10.1016/j.ophtha.2012.01.052. [DOI] [PubMed] [Google Scholar]
- 27.Arshad M., Carnt N., Tan J., Ekkeshis I., Stapleton F. Water Exposure and the Risk of Contact Lens-Related Disease. Cornea. 2019;38:791–797. doi: 10.1097/ICO.0000000000001898. [DOI] [PubMed] [Google Scholar]
- 28.Arshad M., Carnt N., Tan J., Stapleton F. Compliance behaviour change in contact lens wearers: a randomised controlled trial. Eye (Lond) 2020 doi: 10.1038/s41433-020-1015-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Statista; 2020. Number of confirmed coronavirus (COVID-19) cases in Spain between February 12 and August 11.https://www.statista.com/statistics/1107415/confirmed-coronavirus-cases-spain-march/ [Accessed 17 Aug 2020] [Google Scholar]
- 30.Cho P., Boost M.V. Daily disposable lenses: the better alternative. Cont Lens Anterior Eye. 2013;36:4–12. doi: 10.1016/j.clae.2012.10.073. [DOI] [PubMed] [Google Scholar]
- 31.Sulley A., Dumbleton K. Silicone hydrogel daily disposable benefits: the evidence. Cont Lens Anterior Eye. 2020;43:298–307. doi: 10.1016/j.clae.2020.02.001. [DOI] [PubMed] [Google Scholar]
- 32.Nagra M., Vianya-Estopa M., Wolffsohn J.S. Could telehealth help eye care practitioners adapt contact lens services during the COVID-19 pandemic? Cont Lens Anterior Eye. 2020;43:204–207. doi: 10.1016/j.clae.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]