Abstract
BACKGROUND AND PURPOSE: The most common cause of spinal cord disease among patients with AIDS or those infected with HIV-1 is AIDS-associated myelopathy. The purpose of this study was to determine the MR characteristics of the spinal cord in this patient population and to correlate these findings with the clinical severity of myelopathy.
METHODS: MR images of the spinal cord in 21 patients with documented HIV-1 infection or AIDS and a clinical diagnosis of AIDS-associated myelopathy were assessed retrospectively for atrophy, intrinsic signal abnormality, and abnormal enhancement. The clinical severity of myelopathy was graded by a neurologist on the basis of physical examination, and a qualitative correlation was made with the MR findings.
RESULTS: MR findings were abnormal in 18 of the 21 patients. The most common feature was spinal cord atrophy (n = 15), typically involving the thoracic cord with or without cervical cord involvement, followed by intrinsic cord signal abnormality (n = 6), and normal-appearing cord (n = 3). Three patients had both cord atrophy and intrinsic cord signal abnormality. The cord signal abnormality was diffuse, without predilection for any specific distribution pattern. Enhancement was not seen in any of the 10 patients who received intravenous contrast material. Only one of 16 patients with moderate to severe myelopathy had normal MR findings, as compared with two of five patients with mild myelopathy.
CONCLUSION: MR findings in the spinal cord are abnormal in the majority of patients with AIDS-associated myelopathy, typically showing spinal cord atrophy, with or without intrinsic cord signal abnormality. Patients with moderate to severe myelopathy have an increased frequency of spinal cord abnormalities, but a definite correlation between clinical severity of myelopathy and extent of MR abnormalities remains to be established.
Neurologic complications are common in patients with AIDS. Between 40% and 50% of patients with AIDS or AIDS-related complex have neurologic symptoms, with approximately 10% presenting with neurologic symptoms as initial complaints (1–4). The most common cause of spinal cord disease in AIDS patients is AIDS-associated myelopathy, with a reported prevalence of 20% to 55% in different series (5–10). Other causes of myelopathy in AIDS patients include opportunistic infections, neoplasms, and vascular lesions. These are, however, far less frequent than AIDS-associated myelopathy.
AIDS-associated myelopathy generally manifests late in the course of AIDS and is more likely to occur in patients with more AIDS-defining illnesses (7, 9). The antemortem diagnosis is suggested by the typical clinical findings of an insidious onset of progressive spastic paraparesis, ataxia, urinary problems, and sensory loss (11). Somatosensory evoked potential measurements reveal central conduction abnormalities consistent with myelopathy.
The purpose of this study was to determine the MR findings of the spinal cord in patients with AIDS or those infected with HIV-1 and with a clinical diagnosis of AIDS-associated myelopathy and to correlate the MR findings with the clinical severity of myelopathy.
Methods
MR images of the spinal cord in 21 consecutive patients with HIV-1 infection or AIDS by CDC criteria (12) and a clinical diagnosis of AIDS-associated myelopathy were reviewed retrospectively by two experienced neuroradiologists, who conferred on the imaging findings in consensus and who were blinded to the clinical rating of the severity of myelopathy. Eighteen patients were men and three were women, with ages ranging from 29 to 64 years (mean age, 41 years).
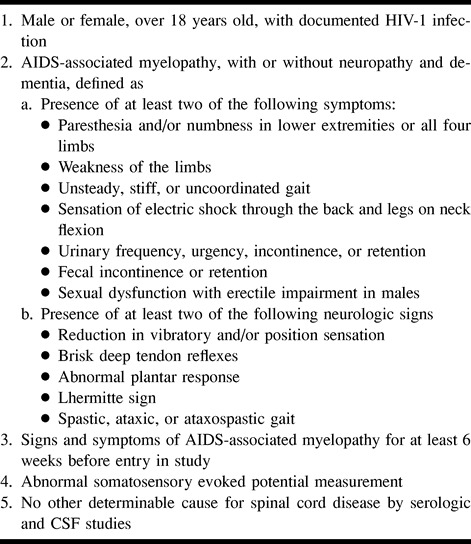
The clinical diagnosis of AIDS-associated myelopathy was based on an insidious onset of slowly progressive myelopathy for at least 6 weeks before entry in the study without fever, acute encephalopathy, or an identifiable causative organism. Clinical symptoms and signs of myelopathy included spastic paraparesis, gait disturbance, urinary problems, impotence in males, hyperreflexia, and a variable degree of sensory loss. Exclusion criteria were spinal cord disease due to any cause other than HIV infection as determined by clinical evaluation; serum or CSF VDRL; cytomegalovirus titer, toxoplasma, and HTLV-1 antibodies; vitamin B12, folate, and methylmalonic acid measurements; and extrinsic or intrinsic mass lesions on spinal MR images (Table 1).
TABLE 1:
Criteria for clinical diagnosis of AIDS-associated myelopathy
A clinical rating of the severity of the myelopathy was established by a neurologist blinded to the MR findings. The myelopathy was rated as mild, moderate, or severe: mild if there were only subjective complaints of leg stiffness, heaviness, cramps, or subjective bladder dysfunction (not incontinence), together with objective findings of increased tone, hyperreflexia, or extensor plantar responses; moderate if there was objectively demonstrable weakness of the lower extremities or incontinence; and severe if the patient was not independently ambulatory.
Somatosensory evoked potential measurements were performed in all patients with stimulation of the tibial nerve at the ankle and recording at the lumbosacral area and the vertex of the head. The conduction time from the lumbosacral area to the vertex was recorded as the central conduction time. A prolonged or absent central conduction time was considered consistent with myelopathy.
The MR studies were performed between October 1994 and July 1997 on 1.5-T units. Only spin-echo noncontrast sagittal T1-weighted (600–800/9–15 [TR/TE]) and sagittal and axial T2-weighted (2700–4000/85–120) images were evaluated. The postcontrast sagittal T1-weighted images of 10 patients who received intravenous contrast material (0.1 mmol/kg) were also assessed.
MR features evaluated included the presence and location of spinal cord atrophy, intrinsic cord signal abnormality, abnormal cord enhancement if contrast material was administered, and other extramedullary processes. Determination of spinal cord atrophy was based on an approximation of the cervical and thoracic spinal cord cross-sectional area or diameter of less than 50% of that of the thecal sac (13, 14). The MR findings of the spinal cord were subsequently correlated with the clinical rating of the severity of the myelopathy.
Results
The results of the MR findings and the clinical rating of myelopathy are summarized in Table 2. Five of the 21 patients had clinically mild myelopathy, 11 had moderate myelopathy, and five had severe myelopathy. Three (60%) of the five patients with mild myelopathy had spinal cord atrophy, of whom one had both cord atrophy and intrinsic cord signal abnormality. Two (40%) of them had normal MR findings in the spinal cord. All 11 patients with moderate myelopathy had abnormal spinal cord MR findings. Nine (82%) of them had cord atrophy, and the remaining two (18%) had intrinsic cord signal abnormality with normal cord size. Three (60%) of the five patients with severe myelopathy had cord atrophy, of whom two had both atrophy and intrinsic cord signal abnormality. One patient (20%) had intrinsic cord signal abnormality with normal cord size, and one (20%) had normal MR findings of the spinal cord. Only one (6%) of 16 patients with moderate to severe myelopathy had normal MR findings, as compared with two (40%) of five patients with mild myelopathy.
TABLE 2:
Summary of results of MR findings and clinical rating of myelopathy in 21 patients
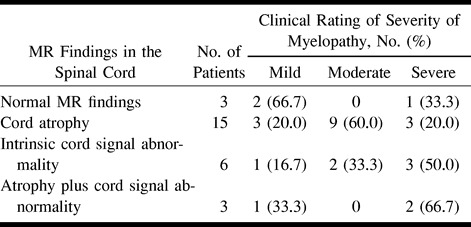
The spinal cord MR features were abnormal in 18 (86%) of the 21 patients. The most common finding was spinal cord atrophy, seen in 15 patients (71%). The atrophy involved the cervical and thoracic cord in seven patients, whereas eight had localized thoracic cord atrophy. Myelopathy was mild in three of these patients, moderate in nine, and severe in three.
On the T2-weighted images, six (29%) of the 21 patients had abnormal intrinsic cord signal hyperintensity distributed in a diffuse pattern, with no predilection for the lateral or posterior columns. The lesions involved the cervical (n = 1), lower cervical and upper thoracic (n = 1), upper and midthoracic (n = 2), and both the cervical and thoracic (n = 2) cord. Myelopathy was mild in one patient, moderate in two, and severe in three. There was no definite correlation between the extent of cord involvement on MR images and the clinical severity of myelopathy. Of the two patients with both cervical and thoracic cord signal abnormality, one had severe and the other had mild myelopathy.
Three patients (14%) had both cord atrophy and intrinsic cord signal abnormality. One had thoracic cord atrophy, with intrinsic cervical and thoracic cord signal abnormality, and was mildly myelopathic (Fig 1). The other two patients had cervical and thoracic cord atrophy, with intrinsic cord signal abnormality involving the cervical cord in one and the cervical and thoracic cord in the other. Both were severely myelopathic (Fig 2).
fig 1.
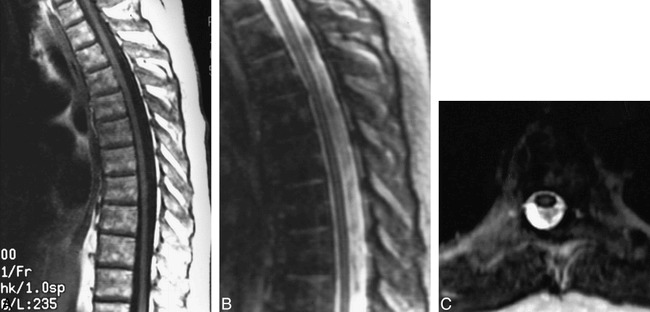
A–C, T1-weighted sagittal (A), T2-weighted sagittal (B), and T2-weighted axial (C) MR images through the thoracic spine of an AIDS patient with mild myelopathy show cord atrophy and intramedullary cord signal abnormality
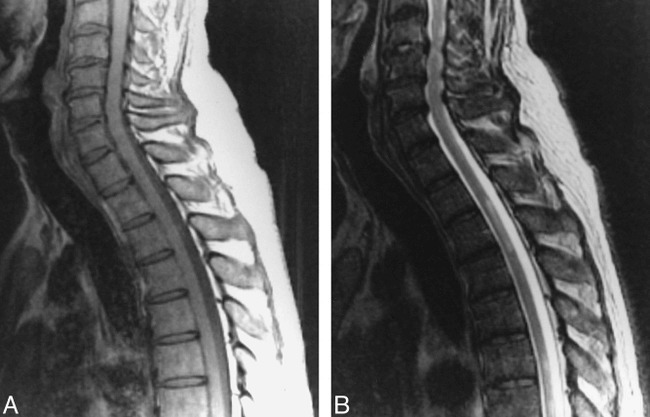
fig 2.
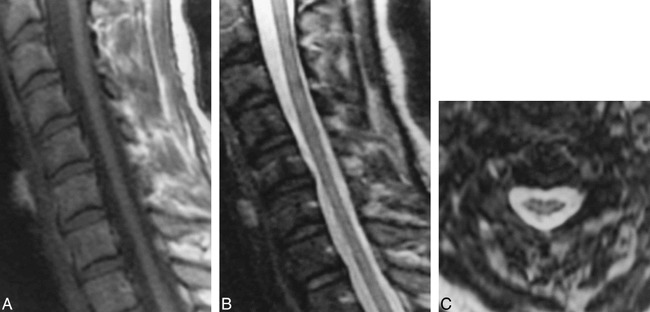
A–C, Sagittal T1-weighted (A), sagittal T2-weighted (B), and axial T2-weighted (C) MR images of the cervical spine in a patient with severe myelopathy show cervical cord atrophy and extensive abnormal intrinsic cord signal intensity
None of the 10 patients who received intravenous contrast agent had evidence of abnormal enhancement of the cord, although nine of them had abnormal spinal cord MR characteristics, of whom three had intrinsic cord signal abnormality (Fig 3). No extramedullary lesions were seen in any of the patients to account for the myelopathy.
fig 3.
A and B, Noncontrast sagittal T1-weighted (A) and T2-weighted (B) images show a normal-sized cervicothoracic cord with intramedullary thoracic cord signal abnormality and no associated cord enlargement. There was no evidence of abnormal enhancement in the postcontrast study (not shown)
Discussion
The diagnosis of AIDS-associated myelopathy is one of exclusion, based on clinical, laboratory, and radiologic findings. MR imaging plays an important role in the evaluation of myelopathy in HIV-infected patients, and is essential in the exclusion of other extrinsic or intrinsic processes, such as lymphoma, primary or metastatic neoplasm, tuberculosis, toxoplasmosis, and other opportunistic infections (15). MR imaging may also be valuable in diagnosing Cytomegalovirus polyradiculomyelitis, which is a rare complication of HIV infection and is usually distinguishable from AIDS-associated myelopathy by the prominent clinical manifestations of radiculopathy, absence of spasticity, and typical MR findings (16). Contrast-enhanced MR imaging contributes to the differential diagnosis of spinal cord disease in HIV-infected patients, but its role in the specific diagnosis of AIDS-associated myelopathy is not well defined. In our study, contrast enhancement was not seen in any of the patients who received intravenous contrast material, including the three with abnormal intrinsic cord signal.
Several studies have suggested a correlation between symptomatic myelopathy and the severity of the pathologic lesions (7, 9, 17). In our study, although there was no clear correlation between the MR findings of the spinal cord in surviving patients and the clinical severity of myelopathy, MR abnormalities were more frequent in patients with more advanced myelopathy. A normal-appearing spinal cord, however, was seen in patients with mild and severe myelopathy. Similarly, patients who had cord atrophy together with intrinsic cord signal abnormality were found in both the mildly and severely myelopathic groups. The small sample population distributed among each grade of myelopathy prevented any conclusive correlation between the MR findings and the clinical severity of disease.
AIDS-associated myelopathy is characterized pathologically by discrete or coalescent intramyelin and periaxonal vacuolation, with cellular debris and lipid-laden macrophages, in the white matter of the spinal cord. The axons are usually intact, but in severe vacuolization, they may become disrupted. It typically involves the lateral and posterior columns of the cervical and thoracic cord (6, 7, 10, 18) (Fig 4). In a postmortem MR study of the spinal cord in AIDS patients, Santosh et al (19) established a pattern of signal abnormality on the T2- and proton density–weighted images involving the white matter tracts laterally and symmetrically on multiple contiguous sections, sufficiently distinct to differentiate it from other spinal cord lesions associated with AIDS. Barakos et al (20) described a patient with a presumed clinical diagnosis of AIDS myelopathy with MR findings of diffuse nonspecific hyperintensity of the spinal cord on the long-TR sequence. Our study showed findings more similar to those described by Barakos et al, with no definite pattern of lateralizing distribution of the intrinsic spinal cord signal abnormality. The MR findings may depend on the stage or extent of the myelopathy, so that imaging findings of necropsy specimens would not necessarily match those of surviving patients.
fig 4.
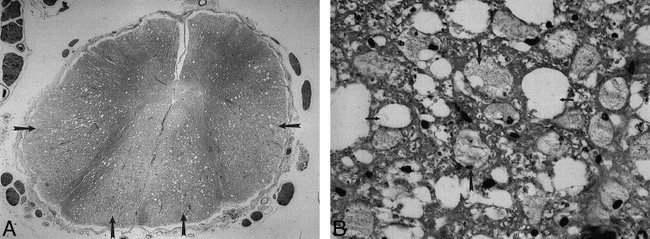
A, Luxol fast blue stain of the spinal cord in a patient with AIDS-associated myelopathy (not from our series) shows pathologic changes predominantly involving the posterior and lateral columns (arrows).
B, A magnified view of the same specimen as in A shows vacuolization (small arrows) and lipid-laden macrophages (large arrows) scattered throughout the involved cord.
(Reprinted with permission from Mandell GL. Atlas of Infectious Diseases, I: AIDS. 2nd ed. Philadelphia: Current Medicine, Inc; 1997.)
Spinal cord atrophy was the most common abnormal MR finding, typically involving the thoracic cord, with or without cervical cord involvement. This observation is consistent with a pathologic study by Tan et al (18) showing that AIDS-associated myelopathy appeared to start in the mid to low thoracic cord, with increasing rostral involvement as the disease progressed.
Conclusion
In our study, the majority of patients (86%) with a clinical diagnosis of AIDS-associated myelopathy had abnormal MR findings in the spinal cord; most commonly, spinal cord atrophy (seen in 72% of patients), followed by intrinsic cord signal abnormality (29%). Fourteen percent of patients had both cord atrophy and intrinsic cord signal abnormality. While no definite correlation was noted between the extent of MR abnormalities and the clinical severity of the disease, patients with advanced myelopathy tended to have a greater frequency of spinal cord MR abnormalities.
Footnotes
Supported in part by NIH grant RO-1 NS 35745.
Address reprint requests to Scott W. Atlas, MD, Department of Radiology, Stanford University Medical Center, S-047, 300 Pasteur Dr, Stanford, CA 94305.
References
- 1.Levy M, Bredesen DE, Rosenblum ML. Neurological manifestations of the acquired immunodeficiency syndrome (AIDS): experience at UCSF and review of the literature. J Neurosurg 1985;6:475-479 [DOI] [PubMed] [Google Scholar]
- 2.Levy RM, Bredesen DE, Rosenblum ML, Davis RL. Central nervous system disorders in AIDS. Immunol Ser 1989;44:371-401 [PubMed] [Google Scholar]
- 3.Levy RM, Pons VG, Rosenblum ML. Central nervous system mass lesions in the acquired immunodeficiency syndrome (AIDS). J Neurosurg 1984;61:9-16 [DOI] [PubMed] [Google Scholar]
- 4.Snider WD, Simpson DM, Nielsen S, Gold JWM, Metroka CE, Posner JB. Neurologic complications of acquired immune deficiency syndrome: analysis of 50 patients. Ann Neurol 1983;14:403-418 [DOI] [PubMed] [Google Scholar]
- 5.Gray F, Gherardi R, Trotot P, Fenelon G, Poirier J. Spinal cord lesions in the acquired immune deficiency syndrome (AIDS). Neurosurg Rev 1990;13:189-194 [DOI] [PubMed] [Google Scholar]
- 6.Henin D, Smith TW, De Girolami U, Sughayer M, Hauw JJ. Neuropathology of the spinal cord in the acquired immunodeficiency syndrome. Hum Pathol 1992;23:1106-1114 [DOI] [PubMed] [Google Scholar]
- 7.Petito CK, Navia BA, Cho ES,, et al. Vacuolar myelopathy pathologically resembling subacute combined degeneration in patients with the acquired immunodeficiency syndrome. N Engl J Med 1985;312:874-879 [DOI] [PubMed] [Google Scholar]
- 8.Goldstick L, Mangybur TI, Bode R. Spinal cord degeneration in AIDS. Neurology 1985;35:103-106 [DOI] [PubMed] [Google Scholar]
- 9.Dal Pan GJ, Glass JD, McArthur JC. Clinicopathologic correlations of HIV-1-associated vacuolar myelopathy: an autopsy-based case-control study. Neurology 1994;44:2159-2164 [DOI] [PubMed] [Google Scholar]
- 10.Artigas J, Grosse G, Niedobitek F. Vacuolar myelopathy in AIDS: a morphologic analysis. Pathol Res Pract 1990;186:228-237 [DOI] [PubMed] [Google Scholar]
- 11.Simpson DM, Tagliati M. Neurologic manifestations of HIV infection. Ann Intern Med 1994;121:769-785 [DOI] [PubMed] [Google Scholar]
- 12. Centers for Disease Control. Revision of the case definition of acquired immunodeficiency syndrome for national reporting: United States. MMWR Morb Mortal Wkly Rep 1985;34:373-374 [PubMed] [Google Scholar]
- 13.Loseff NA, Webb SL, O'Riordan JI,, et al. Spinal cord atrophy and disability in multiple sclerosis: a new reproducible and sensitive MRI method with potential to monitor disease progression. Brain 1996;119:701-708 [DOI] [PubMed] [Google Scholar]
- 14.Filippi M, Campi A, Colombo B,, et al. A spinal cord MRI study of benign and secondary progressive multiple sclerosis. J Neurol 1996;243:502-505 [DOI] [PubMed] [Google Scholar]
- 15.Whiteman MLH, Post MJD, Sklar EML. Neuroimaging of acquired immunodeficiency syndrome. In: Berger JR, Levy RM, eds. AIDS and the Nervous System 2nd ed. Philadelphia: Lippincott-Raven; 1997;297-381
- 16.Whiteman MLH, Dandapani BK, Shebert RP, Post MJD. MRI of AIDS-related polyradiculomyelitis. J Comput Assist Tomogr 1994;18:7-11 [DOI] [PubMed] [Google Scholar]
- 17.Petito CK. Review of central nervous system pathology in human immunodeficiency virus infection. Ann Neurol 1988;23(Suppl):S54–S57 [DOI] [PubMed]
- 18.Tan SV, Guiloff RJ, Scaravilli F. AIDS-associated vacuolar myelopathy: a morphometric study. Brain 1995;118:1247-1261 [DOI] [PubMed] [Google Scholar]
- 19.Santosh CG, Bell JE, Best JJK. Spinal tract pathology in AIDS: postmortem MRI correlation with neuropathology. Neuroradiology 1995;37:134-138 [DOI] [PubMed] [Google Scholar]
- 20.Barakos JA, Mark AS, Dillon WP, Norman D. MR imaging of acute transverse myelitis and AIDS myelopathy. J Comput Assist Tomogr 1990;14:45-50 [DOI] [PubMed] [Google Scholar]


