Abstract
BACKGROUND AND PURPOSE: Two-dimensional phase-contrast (PC) MR imaging is a known method for evaluating CSF flow after third ventriculostomy. In this study, we attempted to confirm the accuracy of cine PC MR imaging for determining the patency of a third ventriculostomy as compared with direct reexploration of the floor of the third ventricle.
METHODS: We examined 11 patients with third ventriculostomies who had a total of 13 reoperations for symptomatic obstructive hydrocephalus. In 12 of the 13 reexplorations, cine PC MR studies were obtained before repeat surgery, and the diagnoses suggested by imaging were compared with intraoperative findings.
RESULTS: Four of five patients who had no flow on MR images had new membranes that covered the orifice; the fifth patient still had a small perforation visible at the time of operation. Three of four patients who had subtle flow on MR images were found to have occlusion with new membranes; the fourth had an incomplete new membrane. Finally, two of three who had a patent ventriculostomy had completely open perforations without membrane formation; the third patient had nonobstructive early membrane formation. At 3 months' follow-up, two flow studies were read as subtle without any clinical symptoms; however, these eventually progressed to become symptomatic, and occlusion with new membrane formation was confirmed during surgical reexploration.
CONCLUSION: Cine PC MR imaging is a reliable technique for detecting the patency of a third ventriculostomy, but minor flow, as defined in this report, appears to be an early sign of closure.
Although neuroendoscopic third ventriculostomy has been used successfully in the treatment of obstructive hydrocephalus (1, 2), failures occur as a result of external malabsorption or fenestration closure. Since ventricular size may change little after fenestration (2), postoperative follow-up may rely primarily on resolution of clinical symptoms. When a patient presents with residual or recurrent symptoms after a third ventriculostomy, it is important to differentiate fenestration closure from malabsorption, since the former may be explored for refenestration while the later requires shunting.
Efforts to visualize the patency of a third ventriculostomy began with the detection of a flow void in the floor of the third ventricle on T1-weighted MR images (3) and later on cine 2D phase-contrast (PC) MR images (4, 5). Patency on cine PC MR images correlates well with clinical prognosis (4), but whether patency as perceived on MR images represents actual anatomic patency has never been proved. It is important to corroborate the accuracy of cine PC MR findings with tangible anatomic findings to establish this technique as the standard for following up patency of a third ventriculostomy. We had the opportunity to reexamine several patients with symptomatic recurrence after a third ventriculostomy and to compare intraoperative findings with cine PC MR images obtained before the exploration. This retrospective study attempts to clarify the reliability of cine PC MR imaging for detecting patency after endoscopic third ventriculostomy.
Methods
During the 50 months from May 31, 1994, to July 31, 1998, 78 patients underwent third ventriculostomy at our institution. Generally, a transcortical approach to the right frontal horn and subsequently to the third ventricle was performed endoscopically. An orifice was then created in the floor of the third ventricle with flexible forceps under endoscopic visualization. The position of the ventriculostomy was always in the midline, anterior to the mammillary bodies and posterior to the infundibular recess. The orifice was dilated with a Fogerty balloon-type catheter to decrease the risk of vascular injury. Postoperatively, cine PC MR studies were performed the day after surgery, 3 months after surgery, and every 3 to 6 months thereafter. During the follow-up period, 11 patients with symptom recurrence required 13 surgical reexplorations of the third ventriculostomy for further CSF diversion. All patients but one had cine PC MR imaging 2 to 4 days before reexploration. Procedures performed during reoperation included remaking the third ventriculostomy with or without external ventricular drainage and/or a VP shunt. Intraoperative findings during endoscopic observation of the floor of the third ventricle were compared with findings at cine PC MR imaging.
All the reexplorations were made by the same neurosurgeon, who was aware of the results of the cine PC MR studies. The intraoperative findings were grouped into three categories: open, partially occluded, or closed. If there was no membrane formation at the site of the third ventriculostomy, it was considered to be open. If membrane formation was observed, a balloon catheter was carefully advanced, and if no resistance was encountered, the ventriculostomy was considered to be partially occluded. Finally, if there was resistance to catheter passage, requiring recreation of the ventriculostomy with the flexible forceps, it was considered to be closed.
Determination of patency was made qualitatively in the cine format by a single neuroradiologist who was completely blinded to the patients' condition and treatment. Every study was examined for biphasic flow and compared with an anatomic MR study to confirm the position of the third ventricular floor. The finding of patency was defined as pulsating in-phase flow in the third ventricle, which extends through its floor into the prepontine cistern. Because midline cuts on sagittal MR images may deviate a few millimeters to either side and may result in failure to detect a patent orifice, discontinuous flow, when limited to the floor of the third ventricle on cine PC MR images, was also considered patent. Flow was considered subtle when there was in-phase but discontinuous flow in the third ventricle where a gap in the flow extended into the third ventricle. The diagnosis was considered unclear when the studies contained artifacts, such as from motion, dental implants, or postoperative air in the ventricle. When no or some flow but not in-phase flow was observed in the third ventricle, a diagnosis of no flow was made. The original interpretations, made on the day of the MR study, were used in this study.
The parameters of the cine PC MR imaging sequences were as follows: 52.0/15.8/1 (TR/TE/excitations), 15° flip angle, 22-cm field of view, 192 × 256 matrix, and 3-mm-thick sections. The velocity encoding was 3 to 5 cm. A 1.5-T MR scanner was used in every study. The direction of flow-encoding for all studies was superior to inferior. The peripheral pulse was used for detection of the R wave of the cardiac cycle.
Results
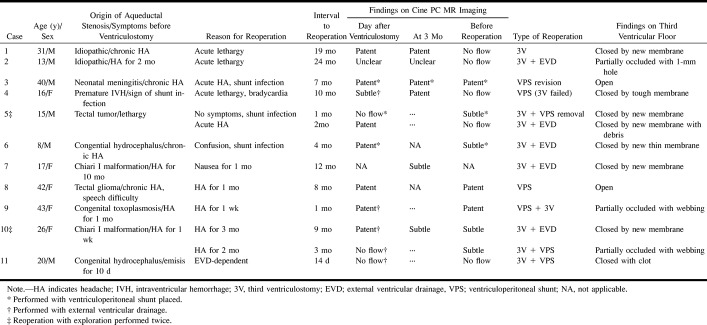
All patients except one (case 11) experienced significant improvement in their symptoms after the third ventriculostomy. The clinical characteristics of the 11 patients studied are summarized in the Table. Six patients were male and five female; the mean age was 25 years (range, 8 to 43 years). The mean interval between the third ventriculostomy and reexploration was 8 months (range, 14 days to 24 months). Figure 1 shows typical patent flow in one patient (case 3). An anatomic study was used to confirm the position of the third ventricular floor (Fig 1A). Downward flow projects in white and upward flow in black (Fig 1B and C, respectively).
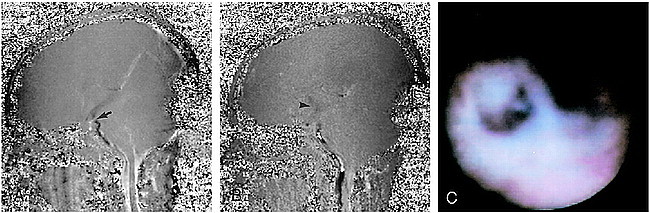
Table: Summary of clinical and imaging findings in 11 patients who underwent reoperation with exploration of third ventricular floor after ventriculostomy
fig 1.
Case 3.
A, Sagittal midline T1-weighted image (500/12/1) obtained before the third ventriculostomy. Large lateral ventricles and the third ventricle are apparent. The aqueductal canal is not visible and the fourth ventricle is relatively small. This anatomic MR image was used to confirm the location of the third ventricular floor.
B and C, Sagittal cine PC midline MR images (52.0/15.8/1) on the day after the third ventriculostomy. Continuous (patent) CSF flow is observed from the foramen of Monro to the prepontine cistern. Superior to inferior flow is shown in white (B) and inferior to superior flow in black (C).
Five of 12 ventriculostomies were considered to have no flow before exploration: the orifice was completely occluded by new membranes (case 1 and 4), by membrane with debris (second exploration of case 5), or by blood clot (case 11); in the fifth case, the orifice was almost but incompletely covered with new membrane (case 2). In four cases, flow was considered subtle before exploration; in three, the orifices were occluded by newly formed membrane (first exploration of cases 5 and 6 and first exploration of case 10) and, in one, it was partially occluded by membrane (second exploration of case 10). In three cases, flow was categorized as patent; two had an open orifice (cases 3 and 8) and one had partial membrane formation but the orifice was open (case 9).
These results demonstrate that if no flow or subtle flow is observed, it is highly suggestive of complete anatomic occlusion (eight of 10) or at least of some early membrane formation (two of 10). Patent flow may be considered confirmatory of an open orifice, even in the presence of some minor membrane formation observed at the time of surgery. At 3 months' follow-up, two readings of subtle flow were obtained in patients who did not have any clinical deterioration at that time. Eventually, however, symptoms did recur (in case 7 and at the first exploration of case 10), and complete occlusion was noted at reexploration. In three patients, a determination of no flow was made the day after the third ventriculostomy; one of these patients (case 11) required reoperation 14 days later to remove a blood clot at the orifice. The other two improved transiently, but required further CSF diversion within 3 months (first exploration of case 5 and second exploration of case 10). In one patient (case 4), subtle flow the day after the third ventriculostomy changed to patent flow 3 months later. All patients in whom no flow or subtle flow was observed on the first postoperative day had external ventricular drains or VP shunts placed.
Four cases are described briefly below.
Illustrative Cases
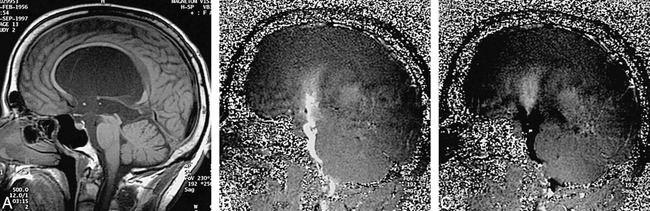
Case 2
A 13-year-old boy with long-standing minor headaches had a CT study of the brain following head trauma. An incidental finding of enlarged lateral and third ventricles with a normal fourth ventricle was made. After the injury, the headaches progressed in severity and became continuous. Idiopathic late-onset aqueductal stenosis was diagnosed, and a third ventriculostomy was performed. The headaches resolved, but owing to artifacts from dental implants at the time, the cine PC MR study was inconclusive. Twenty-four months after the operation, the patient became suddenly lethargic, and a cine PC MR study at this time revealed no flow (Fig 2A). At surgical reexploration, the ventriculostomy orifice was nearly completely covered; however, a small residual hole was patent on probing (Fig 2B). The third ventriculostomy was reexpanded, and the patient's level of consciousness recovered. A postoperative cine PC MR image revealed patent flow (Fig 2C), and the patient has been asymptomatic for 8 months. This case illustrates the association of symptom recurrence with no flow at cine imaging, even though a small hole is still patent. In this situation, it is possible that functional flow was inadequate or absent, indicating the need for refenestration with hole expansion.
fig 2.
Case 2.
A, Cine PC MR image (52.0/15.8/1) 24 months after the third ventriculostomy when the patient became lethargic. No flow was detected in the third ventricle.
B, At exploration 24 months after the third ventriculostomy, a small residual hole is seen in the membrane formation that covers the orifice. The balloon-type catheter is approaching to confirm the presence of the hole, which is considered partially occluded.
C, Cine PC MR image (52.0/15.8/1) on the day after the third ventriculostomy shows continuous (patent) flow from the prepontine cistern to the third ventricle, inferior to superior flow (in black) is seen, although there is a small discontinuation in the floor of the third ventricle (arrow). In the lateral ventricle, the artifact of air can be seen.
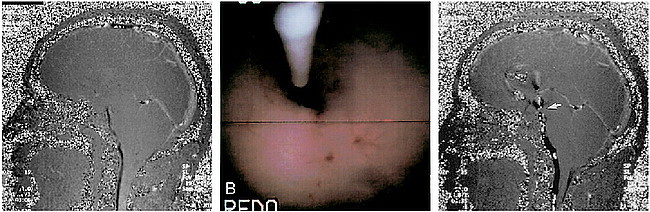
Case 6
An 8-year-old boy with congenital hydrocephalus underwent VP shunting at age 2 days. He required multiple VP shunt revisions for infections, and it became difficult to control his intracranial pressure after slit ventricle syndrome developed. His VP shunt valve had already been replaced with a Codman HAKIM programmable valve (Johnson & Johnson, Lelocle, Switzerland) when the slit ventricles became apparent. The valve pressure was adjusted to 200 mm H2O, causing some enlargement of the lateral ventricles. A third ventriculostomy was subsequently performed, with postoperative cine PC MR images showing patency (Fig 3A). He presented 4 months later with lethargy and confusion, and cine PC MR imaging at that time showed subtle flow (Fig 3B). Reexploration revealed a new, thin membrane covering the orifice (Fig 3C). The third ventriculostomy was recreated, and the VP shunt exchanged for an external ventricular drain because of infection. A new VP shunt was implanted 10 days later as a back-up system because of the patient's long and complicated history. This case illustrates the association of subtle flow with complete new membrane formation. Scar membrane may evolve in a short period of time, perhaps as a result of infection or minor hemorrhage.
fig 3.
Case 6.
A, Cine PC MR image (52.0/15.8/1) on the day after the third ventriculostomy shows continuous (patent) flow from the prepontine cistern to the third ventricle, with a small discontinuation in the third ventricular floor (arrow).
B, Cine PC MR image (52.0/15.8/1) 4 months after the third ventriculostomy when the patient presented with confusion. Minor (subtle) flow is seen in the third ventricle (arrowhead) in phase with the prepontine cistern, but there is discontinuation in the third ventricle.
C, At exploration 4 months after the third ventriculostomy, the orifice is covered with a thin membrane and is considered to be a closure.
Case 8
A 42-year-old woman was found to have a tectal tumor at MR imaging, but no ventricular enlargement was noted. She reported long-standing headache and some episodes of slurred speech. Lumbar puncture revealed elevated pressure at 200 mm H2O, and withdrawal of CSF relieved her headache. Cine PC MR imaging showed no flow in the cerebral aqueduct (Fig 4A). Obstructive hydrocephalus without apparent enlargement of the ventricles was diagnosed, and a third ventriculostomy was performed. Cine PC MR imaging the next day showed patent flow (Fig 4B). Her symptoms improved, but 7 months later, the headache recurred without any change in the size of the ventricles or the tectal glioma. Cine PC MR imaging again showed patency, and reexploration with a possible VP shunt was scheduled. At surgery, the orifice was open (Fig 4C), but mildly increased CSF pressure was noted during the operation. These findings led to the assumption that the patient had an element of CSF absorption disturbance, and a VP shunt was placed. Her headaches resolved after the procedure. In this case, cine PC MR imaging predicted the open fenestration found at surgery. Residual communicating hydrocephalus after a third ventriculostomy may take several months to become symptomatic.
fig 4.
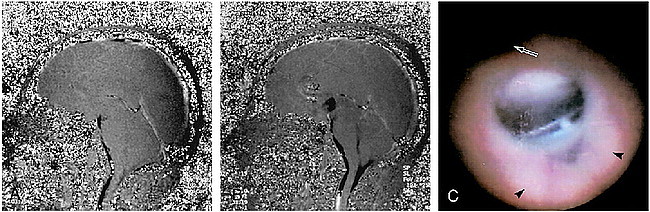
Case 8.
A, Preoperative cine PC MR image (52.0/15.8/1) reveals obstructive hydrocephalus with no flow in the aqueduct. No flow is apparent in the third ventricle.
B, Cine PC MR image (52.0/15.8/1) after the third ventriculostomy shows obvious in-phase third ventricular flow, which is categorized as patent. In the anterior horn of the lateral ventricle, an artifact of air is observed.
C, At exploration 8 months after the third ventriculostomy, the orifice is completely open. The orifice is located posterior to the infundibular recess (arrow) and anterior to the mammillary bodies (arrowheads).
Case 10
A 26-year-old woman with a history of suboccipital decompression and VP shunt placement for Chiari I malformation 4 years earlier presented with slit ventricle syndrome. Her shunt had been revised twice with a high-pressure valve, which unfortunately became infected. The hardware was removed and a third ventriculostomy performed. Initially, the flow on cine PC MR images was patent, changing to subtle at 3-months' follow-up, without symptoms. Six months later, her headache recurred, and the cine PC MR finding was subtle once again (Fig 5A). Reexploration revealed the orifice to be covered with membrane (Fig 5B). The third ventriculostomy was redone, and cine PC MR imaging the next day revealed mixed intensity in the third ventricle not in phase with the prepontine cistern, and was classified as no flow. After a 1-month headache-free interval, the symptoms recurred and cine PC MR imaging revealed subtle flow (Fig 5C). A second exploration was done, whereupon the same webbing was seen to have formed on the orifice, although it was still open. A third ventriculostomy was performed again, but, owing to the patient's complex history of recurrence, a VP shunt was added at that time. In this case, the finding of subtle flow twice correlated with membrane formation. In the first instance, a change to subtle flow presaged the development of symptoms by 3 months, suggesting the possibility that cine PC MR imaging may predict future closure of the orifice.
fig 5.

Case 10.
A, Cine PC MR image (52.0/15.8/1) 6 months after the third ventriculostomy, when the patient presented with recurrent headache. Flow around the foramen of Monro is observed in phase with the prepontine cistern, but it is not obvious. Discontinuation of the flow is seen, and it is categorized as subtle.
B, At exploration 9 months after the third ventriculostomy, the orifice is covered with new membrane, which the balloon-type catheter cannot penetrate. It is considered to be a closure.
C, Cine PC MR image (52.0/15.8/1) 3 months after exploration of the third ventricular floor and reoperation of the third ventriculostomy shows flow in the third ventricle to be in phase but discontinuous. It is categorized as subtle.
Discussion
Our results indicate that the study of CSF flow with cine PC MR imaging is highly reliable for detecting obstruction of a third ventriculostomy with readings of no flow or subtle flow. Two of 10 patients with no flow or subtle flow still had partially patent orifices, but it remains unclear whether these were functional pathways or not. Cine PC MR images may show the functional condition of impaired flow even when there are small residual perforations. We classified no flow and subtle flow into different categories, but in this study the outcomes of these two findings were equivalent. The possible mechanism of subtle flow may be true subtle flow into the orifice, due to narrowing, or no flow into the orifice but some pulsating flow in the third ventricle. Lev et al (4) studied flow velocity at the floor of the third ventricle in patients with third ventriculostomies in comparison with that in healthy control subjects. Their results showed that even control subjects had some flow in that region. It has also been reported that patients with aqueductal stenosis have turbulent CSF flow in the third ventricle (6). These reports indicate that it is possible that some CSF flow may occur at the floor of the third ventricle even without a third ventriculostomy. Thus, minor flow should not be taken as an indicator of patency.
Endoscopic third ventriculostomy has been considered a viable and attractive alternative to shunting for the treatment of obstructive hydrocephalus (1, 2). The efficacy of third ventriculostomy is usually judged by improvement in symptoms (7), because reduction in ventricular size is often slow and, in some cases, never observed (2, 8). Although determinations of CSF flow at the site of a third ventriculostomy began with detection of flow voids on anatomic studies (3, 9), examination with cine PC MR imaging is considered more accurate and reliable (10–12). The cine PC MR technique to confirm CSF flow has been regarded as a standard method for evaluating the patency of a third ventriculostomy (13–15); however, the accuracy of patency detection has never been assessed. To our knowledge, this is the first study to anatomically confirm the accuracy of the diagnosis of patency of a third ventriculostomy with cine PC MR imaging.
Although our results are based on findings in patients with recurrent symptoms rather than in asymptomatic patients, some speculation seems fair. If patency is found in patients with no symptom recurrence, it may indicate an open orifice. If subtle flow or no flow is observed during follow-up of patients without symptoms, further careful observation is warranted, since two such cases in this study progressed to occlusion.
On the day after a third ventriculostomy, a CSF flow study is performed routinely as part of our protocol. Four patients were determined to have no flow or subtle flow, although in just one (case 11) was the procedure considered to be an immediate failure, requiring reexploration. In the other three cases, two required reexploration within 3 months, which confirmed new occlusive membranes. This finding indicates rapid growth of membrane. VP shunting has been reported to decrease normal CSF flow through the aqueduct (10), which may imply that even if a patent third ventriculostomy is observed, CSF flow into the orifice may not be sufficient in the presence of another CSF diversion pathway (ie, a VP shunt or external ventricular drainage). This situation may produce a no-flow image, even with an open orifice. Furthermore, VP shunts or external ventricular drains are considered to be potential causes of failure of third ventriculostomies, because of decreased flow into the ventriculostomy orifice with resultant closure (2). In our practice, the primary goal of external ventricular drains is not to drain CSF but to monitor intracranial pressure, so usually drains are clamped. The benefit of the external ventricular drain as part of this operation should not be underestimated; for example, one patient (case 11) could not have been managed safely without it. Among seven other patients with external ventricular drains or simultaneous VP shunting, patent flow was confirmed in four, and flow improved to become patent 3 months after operation in one (case 4). This suggests that the placement of an external ventricular catheter with limited drainage does not necessarily increase the risk of third ventriculostomy closure.
Conclusion
We believe that our findings confirm that cine PC MR imaging is a reliable method for evaluating the patency of a third ventriculostomy. Minor flow in the third ventricle should be considered an early sign of obstruction. It is possible that CSF flow studies may detect obstruction before symptom recurrence or clinical deterioration. We should be mindful that an early postoperative flow study may be falsely negative as a result of acute CSF volume drainage or in the presence of another CSF diversion pathway, such as a VP shunt or external ventricular drainage.
Footnotes
Address reprint requests to Mark G. Luciano, MD, PhD, Section of Pediatric Neurosurgery, Department of Neurosurgery S-80, The Cleveland Clinic Foundation, 9500 Euclid Ave, Cleveland, OH 44195.
References
- 1.Grant JA, Mclone DG. Third ventriculostomy: a review. Surg Neurol 1997;47:210-212 [DOI] [PubMed] [Google Scholar]
- 2.Kelly PJ. Stereotactic third ventriculostomy in patients with non-tumoral adolescent/adult onset aqueductal stenosis and symptomatic hydrocephalus. J Neurosurg 1991;75:865-873 [DOI] [PubMed] [Google Scholar]
- 3.Jack CR Jr, Kelly PJ. Stereotactic third ventriculostomy: assessment of patency with MR imaging. AJNR Am J Neuroradiol 1989;10:515-522 [PMC free article] [PubMed] [Google Scholar]
- 4.Lev S, Bhadelia RA, Estin D,, et al. Functional analysis of third ventriculostomy patency with phase-contrast MRI velocity measurements. Neuroradiology 1997;39:175-179 [DOI] [PubMed] [Google Scholar]
- 5.Goumnerova LC, Frim DM. Treatment of hydrocephalus with third ventriculocisternostomy: outcome and CSF flow patterns. Pediatr Neurosurg 1997;27:149-152 [DOI] [PubMed] [Google Scholar]
- 6.Kadowaki C, Hara M, Numoto M,, et al. Cine magnetic resonance imaging of aqueductal stenosis. Childs Nerv Syst 1995;11:107-111 [DOI] [PubMed] [Google Scholar]
- 7.Oka K, Yamamoto M, Ikeda K,, et al. Flexible endoneurosurgical therapy for aqueductal stenosis. Neurosurgery 1993;33:236-243 [DOI] [PubMed] [Google Scholar]
- 8.Wilcock DJ, Jaspan T, Worthington BS,, et al. Neuro-endoscopic third ventriculostomy: evaluation with magnetic resonance imaging. Clin Radiol 1997;52:50-54 [DOI] [PubMed] [Google Scholar]
- 9.Missir O, Dormont D, Pierot L. MR visualization of CSF flow through a ventriculo-cisternostomy. Neuroradiology 1989;31:93-94 [DOI] [PubMed] [Google Scholar]
- 10.Mascalchi M, Arnetoli G, Inzitari D,, et al. Cine-MR imaging of aqueductal CSF flow in normal pressure hydrocephalus syndrome before and after CSF shunt. Acta Radiol 1993;34:586-592 [PubMed] [Google Scholar]
- 11.Quencer RM. Intracranial CSF flow in pediatric hydrocephalus: evaluation with cine-MR imaging. AJNR Am J Neuroradiol 1992;13:601-608 [PMC free article] [PubMed] [Google Scholar]
- 12.Luciano MG, Boonswang A, McAllister JP,, et al. MRI cine CSF flow studies in the selection and follow-up of third ventriculostomy patients. Presented at the annual meeting of Society for Research into Hydrocephalus and Spina Bifida, July, 1996, Utrecht, the Netherlands
- 13.Vetõ F, Horváth Z, Dóczi T. Biportal endoscopic management of third ventricle tumors in patients with occlusive hydrocephalus: technical note. Neurosurgery 1997;40:871-877 [DOI] [PubMed] [Google Scholar]
- 14.Frim DM, Goumnerova LC. Telemetric intraventricular pressure measurements after third ventriculocisternostomy in a patients with noncommunicating hydrocephalus. Neurosurgery 1997;41:1425-1430 [DOI] [PubMed] [Google Scholar]
- 15.Ellenbogen RG, Moores LE. Endoscopic management of a pineal and suprasellar germinoma with associated hydrocephalus: technical case report. Min Invas Neurosurg 1997;40:13-16 [DOI] [PubMed] [Google Scholar]