Abstract
Summary: A rheolytic thrombectomy catheter was used to remove thrombus without thrombolytics from the sigmoid and transverse sinuses of a 34-year-old woman. Using small, high-flow fluid jets and Venturi-effect suction, this catheter allowed mechanical removal of thrombus. This technique may obviate the need for thrombolytic agents and the risks associated with their use.
A rheolytic thrombectomy catheter, a device using high-velocity water pulsation to evacuate thrombus, has been shown to be a safe and effective therapeutic technique for the removal of coronary artery thrombosis (1). Recently we used this relatively new catheter technology in a patient with dural sinus thrombosis with excellent results and without the use of thrombolytic agents.
Case Report
A 34-year-old, non-smoking woman using oral contraceptives (norgestimate, ethinyl) with an 8-day history of right ear and neck pain sought medical attention from an otolaryngologist. She was prescribed antibiotics for a middle-ear infection, but returned the next day with worsening pain. A right myringotomy, with ventilation tube placement, was performed. The patient's symptoms continued, and she was sent the next day to a local emergency room where she underwent a complete neurologic examination. The patient was noted to have a left homonymous hemianopsia, photophobia, right-sided scalp tenderness, and impaired left arm and leg response to double, simultaneous stimulation. Testing of the remaining cranial nerves (III–XII), strength, reflexes, coordination, and mental status yielded normal results.
A lumbar puncture was performed. Opening pressure was 22 cm H2O with 1 WBC, 27 RBCs, 66 mg/dL glucose, and 44 mg/dL protein. Complete blood count and routine electrolyte measurements were normal. Coagulation studies showed a prothrombin time of 12.1 seconds, with an international normalized ratio (INR) of 1.1 and a partial prothrombin time of 28.5 seconds.
A CT scan of the head showed increased density in the right transverse and sigmoid sinus suggestive of a dural venous sinus thrombosis. MR imaging was performed confirming thrombus occluding the right transverse and sigmoid sinuses (Fig 1). Along with this finding, a hyperintense signal on fluid-attenuated inversion-recovery sequences in the subarachnoid space and parenchyma of the right parietal lobe was noted, consistent with edema and subarachnoid hemorrhage.
fig 1.
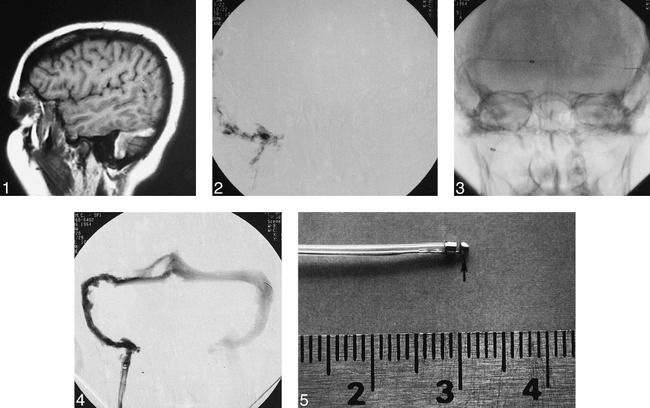
Sagittal T1-weighted (500/20 [TR/TE]) spin-echo MR image shows hyperintense thrombus in the right transverse and sigmoid sinus.
fig 2. Posterior/anterior view of the initial venogram from a right, internal jugular injection shows multiple, irregular filling defects in the right sigmoid and transverse sinus consistent with thrombosis.
fig 3. Posterior/anterior view during thrombectomy catheter placement shows the exchange microwire extending from the right internal jugular vein into the left transverse sinus and the catheter successfully advanced into the torcula beyond the occlusion.
fig 4. Posterior/anterior view of a follow-up venogram performed from the base catheter in the right internal jugular vein reveals marked improvement with a patent channel through the previously occluded transverse and sigmoid sinus.
fig 5. Photograph of the AngioJet® catheter. An arrow points to the high-flow input nozzle.
The patient was taken urgently to the angiography suite where the right jugular vein was catheterized via a right femoral vein approach. Initial images of the right internal jugular vein showed occlusion beginning immediately caudal to the mastoid (Fig 2). A microcatheter (Tracker 18 MX, Target Therapeutics, Freemont, CA) and wire was placed into the thrombus. After great difficulty getting through the length of the thrombus, a patent torcula was reached. The microcatheter and base catheter were then exchanged for a 7F guide catheter and a rheolytic thrombectomy catheter (CF105 AngioJet, POSSIS Medical, Inc., Minneapolis, MN). The exchage wire was positioned across the torcula in the opposite sigmoid sinus during the exchange (Fig 3). The rheolytic thrombectomy catheter followed the 0.014-inch guidewire easily even through the clot had been so resistant earlier. The rheolytic thrombectomy catheter then was activated and slowly withdrawn at 1–2 mm/s. A retrograde venogram obtained via the base catheter showed some patency within 5 minutes. Several more passes were made with the thrombectomy catheter, advancing back to the torcula and withdrawing again. The final venogram (obtained 17 minutes after beginning mechanical disruption) showed excellent flow despite residual thrombus (Fig 4). Thrombolytic infusion was not performed owing to the good angiographic result and rapid clinical improvement.
The patient had immediate relief of pain and gradual resolution of hemianopsia over the next several hours. She was taken off oral contraceptives, initially was placed on heparin, and then was placed on coumadin in order to reach a target INR of 2.0–3.0. During the next 3 months of anticoagulant therapy, she remained asymptomatic.
Discussion
The pneumatic thrombectomy catheter is designed as a therapeutic tool for alleviating acute vascular thrombosis. The catheter has both an inflow and outflow lumen. The inflow lumen carries normal saline under high-pressure (approximately 9000 psi) to a nozzle at the end of the catheter that reverses flow by 180°, and directs it back toward the outflow lumen (Fig 5). By directing input flow into the area around the outflow lumen at a high speed (350–450 km/h), a negative pressure is created around the vortex of the incoming flow to the outflow lumen. The low-pressure area that is created by an adjacent high pressure is referred to as a Venturi effect. Three additional low-flow nozzles (25–40 km/h) from the input lumen are placed just proximal to the high-speed nozzle. These three nozzles are directed perpendicularly to the catheter and create enough force to dislodge small portions of the thrombus and optimize the vortex at the outflow lumen. The combination of these mechanisms allows gentle removal of thrombus from the artery or vein and evacuation into the outflow lumen.
The rheolytic thrombectomy catheter has been evaluated with in vitro studies that show it is minimally traumatic to vascular endothelium. Sharafuddin et al reported the vascular endothelium of canine vessels suffered less trauma after rheolytic catheterization compared with Fogarty balloon angioplasty (88% versus 58% endothelial coverage) (2). In addition, the particulate matter that may escape from the outflow lumen of the thrombectomy catheter and move in the direction of blood flow also has been evaluated with in vitro models. These studies show 12% (2) to 38% (3) of the thrombus volume escapes removal by the output lumen. The size of these particles can be problematic because backwash from intracranial thrombectomy can find an endpoint in the lungs with the potential to result in pulmonary emboli. These same studies, however, indicate that the vast majority (99.83%) of particulate matter used is smaller than 10 μm (2). When these particles were injected in vivo into the renal vascular bed of the canine model, no necrosis was seen, suggesting the insufficiency of the particle size to cause ischemic changes (2). Investigators have shown that the rheolytic thrombectomy catheter can successfully recanalize saphrenous vein grafts and limb vessels that are obstructed by diffuse atherosclerosis and intraluminal thrombus (1, 4). It also has been used successfully for angioscopic evaluation of a coronary vein graft (5). Application in the cerebral vasculature seems to be a reasonable extension of this technology, and its use has recently been reported in a patient with dural sinus thrombosis without an associated intracranial hemorrhage (6).
Thrombosis of the cerebral sinus is a rare occurrence, but is known to have an increased incidence in female patients using oral contraceptives. A retrospective case-control study of 511 patients using oral contraceptives had a 50% greater risk of developing cerebral thromboembolosis compared to non-users (7). Thrombosis of a large cerebral sinus such as the one presented in this case appears well suited for the use of the thrombectomy catheter. For the case reported herein, patency of the lumen was recovered after several minutes once the thrombectomy catheter was in place. Certainly, the anatomy appeared favorable to the flexibility of the catheter, though this may not always be the case.
Standard treatment for dural sinus thrombosis has involved anticoagulant or thrombolytic therapy. Although high-dose heparin and warfarin have been associated with successful patient outcomes, recanalization of the sinus often has not been observed (8). Patency of the dural sinus has been obtained, however, with selective catheterization and infusion of urokinase in two series of seven (9) and twelve patients (10), though only four of these patients had evidence of hemorrhage on preoperative CT scans.
Despite these few reported cases, we believed the presence of subarachnoid hemorrhage in the immediate area of the thrombus predisposed this patient to further and potentially more devastating hemorrhage with the use of anticoagulants or thrombolytics as primary treatment. These risks were explained to the patient and her family who elected to proceed with thrombectomy by the rheolytic catheter when presented with it as an alternative. Additional risks and lack of prognostic data associated with the use of the thrombectomy catheter were explained to the patient prior to her consent for treatment. An institutionally approved protocol for this procedure was not required.
We believe dural sinus thrombosis cases such as this are well suited for treatment with the rheolytic thrombectomy catheter. Importantly, its use provides a mechanical means of thrombus removal that may obviate the need for thrombolytic agents and the associated risks encountered with them, especially in patients with intracranial hemorrhage.
Footnotes
Address reprint requests to Dr. Alan M. Scarrow, M.D., J.D., UPMC Presbyterian Hospital, Department of Neurosurgery, Suite B-400, Pittsburgh, Pennsylvania 15213.
References
- 1.Ramee SR, Schatz RA, Carrozza JP,, et al. Results of the VeGAS I pilot study of the Possis AngioJet thrombectomy catheter. Circulation 1996;94:I-619 [Google Scholar]
- 2.Sharafuddin MJA, Hicks ME, Jenson ML,, et al. Rheolytic thrombectomy with use of the AngioJet-F105 catheter: preclinical evaluation of safety. J Vasc Interv Radiol 1997;8:939-945 [DOI] [PubMed] [Google Scholar]
- 3.Dick A, Neuerburg J, Schmitz-Rode T,, et al. Declotting of embolized temporary vena cava filter by ultrasound and the Angiojet. Invest Radiol 1998;33:91-97 [DOI] [PubMed] [Google Scholar]
- 4.Silva JA, Ramee SR, Collins TJ,, et al. Rheolytic thrombectomy in the treatment of acute limb-threatening ischemia: immediate results and six-month follow-up of the multicenter AngioJet registry. Cathet Cardiovasc Diagn 1998;45:386-393 [DOI] [PubMed] [Google Scholar]
- 5.Rodes J, Bilodeau L, Bonan R,, et al. Angioscopic evaluation of thrombus removal by the Possis AngioJet® thrombectomy catheter. Cathet Cardiovasc Diagn 1998;43:338-343 [DOI] [PubMed] [Google Scholar]
- 6.Opatowsky MJ, Morris PP, Regan JD,, et al. Rapid thrombectomy of superior sagittal sinus and transverse sinus thrombosis with a rheolytic catheter device. AJNR Am J Neuroradiol 1999;20:414-417 [PMC free article] [PubMed] [Google Scholar]
- 7.Lidegaard O. Oral contraception and risk of a cerebral thromboembolic attack: results of a case-control study. . BMJ 1993;306:956-963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cipri S, Gangemi A, Campolo C,, et al. High-dose heparin plus warfarin administration in non-traumatic dural sinuses thrombosis. A clinical and neuroradiological study. J Neurosurg Sci 1998;42:23-32 [PubMed] [Google Scholar]
- 9.Smith TP, Higashida RT, Barnwell et al. Treatment of dural sinus thrombosis by urokinas infusion. AJNR Am J Neuroradiol 1994;15:801-807 [PMC free article] [PubMed] [Google Scholar]
- 10.Horowitz M, Purdy P, Unwin H,, et al. Treatment of dural sinus thrombosis using selective catheterizaiton and urokinase. Ann Neurol 1995;38:58-67 [DOI] [PubMed] [Google Scholar]


