Abstract
Summary: Recently, a young woman presented acutely with a left hemispheric stroke and differing blood pressures in the arms as her initial manifestation of Takayasu's arteritis. Helical CT angiography, performed to rule out aortic dissection, revealed a thickened wall of the aortic arch with stenoses and occlusions of the great vessels, suggesting the diagnosis. The sequence of imaging studies and findings in this unusually catastrophic presentation of a typically insidious disease are highlighted.
Takayasu's arteritis is a disease that afflicts young women and often goes unrecognized because its clinical signs and symptoms are so nonspecific, particularly during the acute (prepulseless) phase. Later, an occlusive (pulseless) phase ensues and is associated with CNS complications in up to 10% of patients (1, 2). In one study, 75% of the patients presented with stroke as their initial manifestation of Takayasu's arteritis (3). Therefore, when a previously healthy young woman presents with cerebrovascular ischemia, the diagnosis of a vasculitis should be considered.
Case Report
A previously healthy 22-year-old woman presented to the emergency room with aphasia and right hemiparesis. Ten hours before admission, she awoke with a left-sided headache and experienced a syncopal episode. Later, she developed numbness and weakness in her right hand. A physical examination at the time of her arrival revealed a left carotid bruit, left ptosis, left gaze preference, and weakness of the right upper extremity. Her right hand was cold with an absent radial pulse. The blood pressure was 70/40 in the right upper extremity and 100/80 in the left upper extremity.
The initial unenhanced CT scan of the brain (obtained approximately 10 hours after the onset of symptoms) revealed hyperdensity in the M1 and M2 segments of the left middle cerebral artery, suggesting thrombus or embolus. There were no abnormal hypodensities or mass effect. Helical CT angiography of the chest and neck (100 cc of nonionic contrast material, injected at a rate of 2–3 cc/second, with 1:1 table pitch, 3-mm section thickness in the neck, and 5-mm section thickness in the chest) was performed to evaluate for aortic dissection and flow abnormalities in the left neck vessels. This examination failed to reveal an intimal flap or an aortic dissection. It, however, showed circumferential thickening of the wall at the top of the aortic arch (Fig 1A). Axial images at the level of the great vessels revealed an occluded left common carotid artery. Although streak artifact from the right arm injection of contrast material obscured fine evaluation, there was no significant filling of the right brachiocephalic artery, suggesting a tight stenosis (Fig 2). Axial images obtained just above the aortic arch showed a moderate short segment stenosis of the proximal left subclavian artery. Helical CT angiography of the neck showed nonopacification of the left common carotid artery, consistent with occlusion. Color duplex sonography confirmed these findings. The remainder of the images of the extracranial carotid and vertebral arteries showed normal enhancement (Fig 3). The vascular enhancement in the left internal and external carotid arteries indicated that collaterals were filling the external carotid with retrograde flow into the internal carotid artery (Fig 4). CT of the brain performed after the helical CT angiography showed interval development of subtle hypodensity and mass effect involving the left caudate nucleus and loss of gray-white junction in the left frontal lobe, consistent with evolving infarction. There was normal enhancement in the major intracerebral vessels, with no evidence of clot or thrombus even in the left M1 and M2 segments.
fig 1.
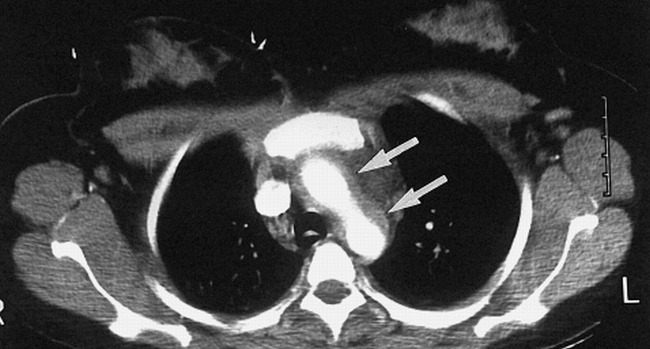
Images from the case of a previously healthy 22-year-old woman who presented to the emergency room with aphasia and right hemiparesis. Axial CT scan, obtained at the aortic arch, reveals thickened walls (arrows).
fig 2.
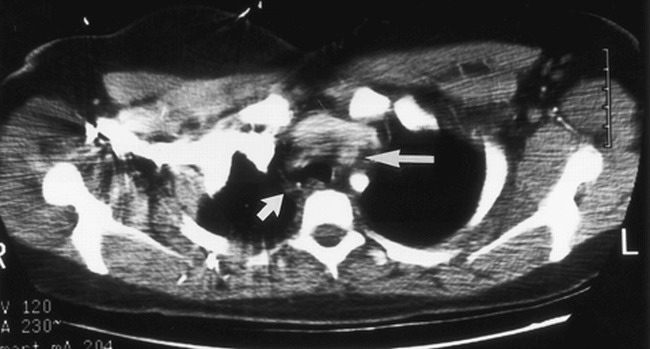
Axial CT scan, obtained at the level of the great vessels, shows nonopacification of the left common carotid artery (right arrow), indicative of occlusion. The right brachiocephalic artery is not well seen because of streak artifact, but no definite enhancement is seen in the expected location of the vessel (left arrow).
fig 3.
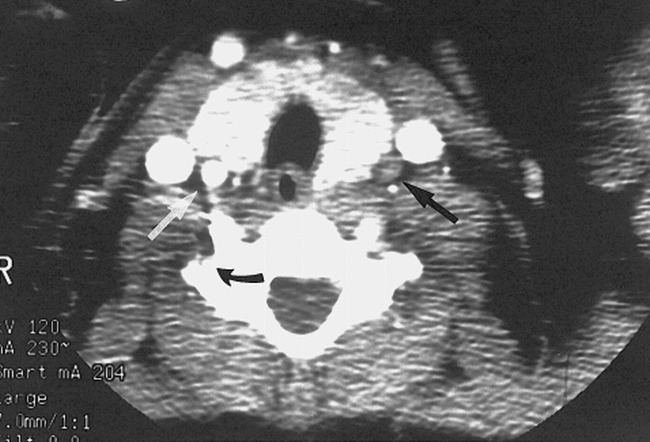
Axial CT scan, obtained at a section higher than that shown in B, shows nonopacification of the left common carotid artery (black arrow) and normal opacification of the right common carotid artery (white arrow). Also noted was delayed opacification of the right vertebral artery (curved black arrow) compared with the left vertebral artery.
fig 4.

Axial CT scan of the mid to upper neck shows contrast opacification in the left internal carotid artery (short arrow) and external carotid artery (long arrow), indicating reconstitution of internal carotid artery flow via retrograde filling of the external carotid artery.
Blood work revealed an elevated sedimentation rate (66 mm/hour), normal coagulation profile, and normal complete blood count. Despite supportive medical treatment, the patient's clinical status deteriorated, necessitating intubation. Ultimately, a decompressive left craniectomy was necessary. Follow-up CT of the brain showed significant progression of the infarct, with increasing mass effect, midline shift, and impending transtentorial herniation.
Cerebral angiography was performed (19 days after presentation) and confirmed the helical CT angiography findings consistent with Takayasu's arteritis. There was complete occlusion of the left common carotid artery at the level of the aortic arch. A 2-cm-long 95% stenosis of the right brachiocephalic artery and a 50% stenosis of the left subclavian artery were also seen (Fig 5). The left vertebral artery provided most of the flow into the anterior and posterior circulations via collaterals into the left external carotid artery and retrograde flow down the right vertebral artery feeding the right common carotid artery.
fig 5.
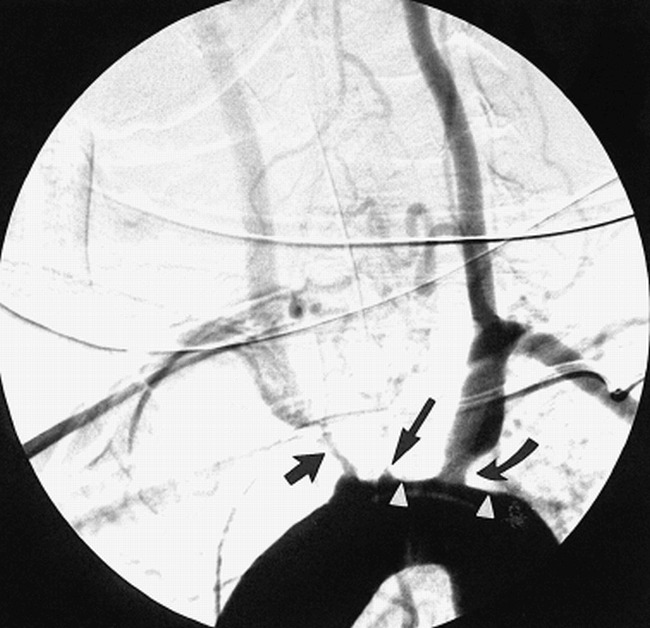
Oblique view of the aortic arch during aortography shows thickening and flattening of the superior wall of the aortic arch (arrowheads). There is no dissection, but study confirms total occlusion at the origin of the left common carotid artery (long arrow), moderate stenosis of the left subclavian artery (curved arrow), and a tight stenosis at the origin of the right brachiocephalic artery (short arrow).
The patient was eventually extubated, and her clinical status somewhat improved. Presently, she remains aphasic with mild right upper extremity paresis, for which she is undergoing rehabilitation.
Discussion
This case highlights the ability of helical CT angiography to evaluate all portions of the vessels. Most papers cite the utility of helical CT angiography in revealing luminal abnormalities. In the setting of trauma (both penetrating and blunt), helical CT angiography can effectively evaluate the aorta and neck vessels (4, 5). Emboli within the pulmonary arteries and injuries to the renal vascular pedicles are also well evaluated with helical CT angiography (6, 7). Others have used helical CT angiography in the non-emergent setting to evaluate atherosclerotic disease in the extracranial carotid arteries (8).
In this case, the ability of helical CT angiography to delineate mural wall thickening, in addition to the stenoses and occlusions of the great vessels, was critical in making the diagnosis of Takayasu's arteritis. Pathologically, there is involvement of all three vessel layers, resulting in fibrosis and wall thickening, which precedes luminal compromise. Thus, CT may prove critical in suggesting the diagnosis before angiographically detectable luminal changes (9). There have been only a few reports showing wall thickening and calcifications seen on CT scans of patients with Takayasu's arteritis, predominately in the aorta and pulmonary arteries (10, 11). These articles also describe delayed enhancement of the outer wall with a concentric ring of inner media and intima, which does not enhance (10).
Finally, helical CT angiography demonstrated occlusion of the left common carotid artery but normal flow in the left internal carotid artery. CT scans of the brain obtained after the intravenous administration of contrast material also showed flow in the left M1 and M2 segments. Thus, although the stroke was most likely embolic, at the time of imaging, we rapidly confirmed satisfactory flow into the left anterior circulation, obviating the need for revascularization procedures.
Conclusion
In this young woman who presented with an acute stroke and differing upper extremity blood pressures, helical CT angiography was instrumental in excluding aortic dissection and suggesting the diagnosis of Takayasu's arteritis because it revealed both luminal and mural abnormalities of the arch and great vessels.
Footnotes
Send reprint requests to Suzanne D. LeBlang, MD, P.O. Box 016960, Miami, FL 33136.
References
- 1.Matsunaga N, Hayashi K, Sakamoto I, Ogawa Y, Matsumoto T, Takayasu arteritis. Protean radiologic manifestations and diagnosis. Radiographics 1997;17:579-594 [DOI] [PubMed] [Google Scholar]
- 2.Hata A, Noda M, Moriwaki R, Numano F, Angiographic findings of Takayasu arteritis. New classification. Int J Cardiol 1996;54[suppl]:155-163 [DOI] [PubMed] [Google Scholar]
- 3.Del Brutto OH, Lara-Teran J, Sanchez J, Lara-Montiel J, Complicaciones cerebrovasculares de la enfermedad de Takayasu. Rev Neurol 1996;24:803-805 [PubMed] [Google Scholar]
- 4.Mirvis SE, Shanmuganathan K, Miller BH, White CS, Turney SZ, Traumatic aortic injury. Diagnosis with contrast-enhanced thoracic CT. Radiology 1996;200:413-422 [DOI] [PubMed] [Google Scholar]
- 5.Le Blang SD, Nunez DB, Rivas LA, Falcone SF, Pogson SE, Helical CT angiography in penetrating neck trauma. Emerg Radiol 1997;4:200-206 [Google Scholar]
- 6.Van Rossum AB, Pattynama PM, Ton ER, et al. Pulmonary embolism. Validation of spiral CTA in 149 patients. Radiology 1996;201:467-470 [DOI] [PubMed] [Google Scholar]
- 7.Nunez D, Becerra JL, Fuentes D, Pogson SE, Traumatic occlusion of the renal artery. Helical CT diagnosis. Am J Radiol 1996;167:777-780 [DOI] [PubMed] [Google Scholar]
- 8.Schwartz RB, Jones KM, Chernoff DM, et al. Common carotid artery bifurcation. Evaluation with spiral CT. Radiology 1992;185:513-519 [DOI] [PubMed] [Google Scholar]
- 9.Park JH, CT Angiography of Takayasu's Arteritis: Comparison with Conventional Angiography. J Vasc Interv Radiol 8:393-400 [DOI] [PubMed] [Google Scholar]
- 10.Park JH, Conventional and CT angiographic diagnosis of Takayasu arteritis. Int J Cardiol 1996;54[suppl]:165-171 [DOI] [PubMed] [Google Scholar]
- 11.Yogawa K, Sakamoto I, Matsuoka Y, Matsunaga N, Case report. Imaging of Takayasu arteritis in the acute stage. Br J Radiol; 69:189-191 [DOI] [PubMed] [Google Scholar]


