Abstract
Like rest of the world, the South Asian region is facing enormous challenges with the coronavirus disease 2019 (COVID-19) pandemic. The socioeconomic context of the eight South Asian countries is averse to any long-term lockdown program, but the region still observed stringent lockdown close to two months. This paper analyzed major measures in public health preparedness and responses in those countries in the pandemic. The research was based on a situation analysis to discuss appropriate plan for epidemic preparedness, strategies for prevention and control measures, and adequate response management mechanism. Based on the data from March 21 to June 26, 2020, it appeared lockdown program along with other control measures were not as effective to arrest the exponential growth of fortnightly COVID-19 cases in Afghanistan, Bangladesh, India, Nepal and Pakistan. However, Bhutan, Maldives and Sri Lanka have been successfully limiting the spread of the disease. The in-depth analysis of prevention and control measures espoused densely populated context of South Asia needs community-led intervention strategy, such as case containment, in order to reverse the growing trend, and adopt the policy of mitigation instead of suppression to formulate COVID-19 action plan. On the other hand, mechanism for response management encompassed a four-tier approach of governance to weave community-led local bodies with state, national and international governance actors for enhancing the countries’ emergency operation system. It is concluded resource-crunch countries in South Asia are unable to cope with the disproportionate demand of capital and skilled health care workforce at the time of the pandemic. Hence, response management needs an approach of governance maximization instead of resource maximization. The epidemiologic management of population coupled with suitable public health prevention and control measures may be a more appropriate strategy to strike a balance between economy and population health during the time of pandemic.
Keywords: Coronavirus disease 2019, COVID-19, Pandemic, Intervention strategy, Epidemiological management, Public health, South Asia
1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic has brought the world to a standstill. The World Health Organization (WHO) declared the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus causing the COVID-19 disease a public health emergency of international concern on January 30, 2020, and raised the alert level to pandemic urgency on March 11, 2020.1 Subsequent to the pandemic's announcement and as a result of the exponential growth in infections followed by the collapse of healthcare service delivery systems in Italy and Spain, countries across the world (except Antarctica) went into “lockdown” mode to contain the spread of the SARS-CoV-2 virus. At the time, while a third of the global population (until April 17, 2020) was in lockdown,2 it was important from a public health perspective to examine the impact of such a pandemic on developing countries that generally struggle to maintain a balance between economic stability and population-level health outcomes. This paper was a situation assessment of South Asian (SA) countries at the onset of the COVID-19 pandemic and up until the present.
Historically South Asian countries are not new to outbreaks of infectious diseases—cholera being the single most important example.3 The region is comprised of eight countries, namely, Afghanistan, Bangladesh, Bhutan, India, the Maldives, Nepal, Pakistan, and Sri Lanka, and collectively represent 25% of the global population—over 1.8 billion people—but account only for 5% of world's gross domestic product (GDP).4 The region has a high level income inequality and on average, 45% of the SA region's total income or consumption can be attributed to the richest quintile of the population.5 South Asian countries account for 33.4% of the world's low-income population, of which almost half live in India (21.2%) and Bangladesh (18.5%). A low-income population is defined as living below the international poverty threshold of 1.90 USD per day.6
Health systems, especially at a primary level, in the South Asia region are characterized by inadequate public investment, a scarcity of healthcare workers, and excessive out-of-pocket expenditure.7 Over the past decade, healthcare systems have shifted toward medical-centric care based on an insurance model for service provision from the private sector.8 The a lack of information on public health is a major reason for the high burden of morbidity and mortality, especially due to communicable diseases. Malnutrition continues to be a serious public health problem—nearly half of the world's children with stunted growth (i.e., low weigh-height ratio) live in South Asia (26.9 million children as of 2018).9 Except for Sri Lanka, all the South Asia countries lack adequate public health capacity and competence for disease surveillance. This is a major barrier for the effective management and control of infectious diseases, and interventions.10
Stuck between poverty inequality and a fragile health system, the lockdown imposed as a result of the pandemic lowered the region's GDP growth forecast from 6.3% to 1.8%–2.8% for 2020.11 Amid this bleak macro-economic scenario, the effectiveness of these countries’ aggressive implementation of lockdown to contain COVID-19 in the region remains doubtful owing to three longstanding factors: first, the availability of and access to water, chiefly in summer, for hand washing; second, high population density that defies physical distancing; and last, the poor state of health system organization and management.12
Lockdown is a protective short-term measure in the absence of any vaccine and/or well-defined clinical treatment. South Asian countries could not afford to bear the burden of a complete lockdown for a very long time. The nation-wide lockdown may not have provided a solution, but rather created a problem for South Asia. At present, routine vaccinations are under threat in Bangladesh, Nepal, Pakistan, and Afghanistan.13 India had alarmingly reported a very low number of tuberculosis (TB) cases during the weeks of lockdown—11,367 compared to the average pre-lockdown weekly number of 45,875 in 2020.14 Access to HIV medication, cancer treatment (in India)15- 16 and maternal care services (in Nepal) were hindered due to restrictions to movement.17 The international experience of managing the pandemic is equally disturbing. Due to a lack of public health planning and preparedness, countries across the world had to bear high COVID-19 related mortality rates at the cost of social and economic disruption.18 In order to tackle the pandemic, countries urgently need to raise their own COVID-19 epidemic preparedness and response management profiles.
Epidemic preparedness is epitomized by planning, epidemiological projections, and public health prevention and control measures (screening, lockdown, testing, contact tracing, and risk communication). The result section of this paper analytically describes all these three key features of epidemic preparedness in order to discuss an operational plan followed by an intervention strategy (including clinical management) for South Asian countries. Furthermore, a response management system is explored that can prioritize the importance of governance robustness to aid preparedness activities and successfully manage prevention and control operations.
South Asian countries have already faced several contextual challenges in the social, economic, and political spheres. The arrival of the pandemic aggravated them and posed severe challenges to current health policies and planning mechanisms. The research aimed to address this complexity by analyzing the region's epidemic preparedness, guidelines for prevention and control measures, operational plans and intervention strategies, and response management mechanisms.
2. Methods
This health policy research analyzed the situation in the South Asia region in the wake of the COVID-19 pandemic. A situation analysis is a widely held method in health policy research to understand the present condition of any given context. The WHO recommends it in order to study or develop countries’ national health policies, planning, and strategies.19 It is a method evolved from grounded theory to map out context and complexity in various situations.20 The adoption of situation analysis has helped the researchers to set priority actions for health policy and planning in South Asian countries to combat the pandemic in the long run.
Narrative and systemic reviews of literature were conducted to assess journal articles, edited books, monographs and other secondary materials. Since the pandemic is still ongoing and there is a dearth of scientific research literature, reputed newspaper reportage, blogs, websites, and magazines were also reviewed to collect real-time information/data for assessing the situation at ground level. Databases of the World Bank, WHO Situation Reports, and other quantitative sources were also utilized for descriptive statistical analyses to assess the situation and argue for strategic moderation in public health approaches.
3. Results and findings
3.1. Epidemic preparedness
Epidemic preparedness is a comprehensive emergency management planning framework that, in consultation with epidemiological projections, devises prevention and control measures. This type of management in any epidemic (or pandemic as is currently the case) is a continuous process to predict, avert, identify, as well as respond in order to mitigate the effect of outbreaks.21 Epidemic preparedness is often a policy-based action at national and provincial level. South Asian countries need dedicated epidemic management teams, monitoring taskforces, and decision-making bodies for inter-departmental coordination. Apart from epidemic management teams, all other policy bodies must also have an adequate representation of public health professionals. The epidemic management team should ideally be comprised of experts in public health, epidemiology, medical care treatment, hospital management, community medicine, and urban planning. The technical body of an epidemic management team is expected to provide insights and suggestions to other politico-administrative constituent bodies for decision-making purposes. There is a requirement of basic information outflow with regards to epidemic management decisions for the health workers at all the levels (including medical care providers).
In order to plan for prevention and control measures, the epidemiology of COVID-19 first needs to be understood. The South Asia region until June 26, 2020 had collectively a total of 885,048 confirmed COVID-19 cases, where India (508,953) had the largest caseload (fifth highest in the world) and Bhutan (70) the lowest. Large cohorts of confirmed COVID-19 cases were reported in Pakistan (198,883), Bangladesh (130,474), and Afghanistan (30,616). So far, a total 22,130 COVID-19 deaths have been recorded in the countries of South Asia, with India (15,685), Pakistan (4035), and Bangladesh (1661) all reporting four-digit figures. Bhutan, the least populated country in South Asia reported no deaths, while Afghanistan (703), Nepal (27), Sri Lanka (11), and the Maldives (8) also reported deaths from COVID-19. Although the figures are inconclusive because of under-reporting as well as a lack of information on case distribution in terms of age and sex, India (3%) had the highest crude case fatality rate followed by Afghanistan (2.29%), and Pakistan (2%), as of June 26, 2020 based on the WHO Situation Report (No. 159) of June 27, 2020.22
Reporting on COVID-19 cases that include socioeconomic classifications, such as age, sex, religion, and income, is not readily available for South Asian countries. According to the WHO Situation Report, the male to female ratio for infected cases among all the age groups is 1.03∶1. The infectivity rate is proportionately higher (40%–45% of the total case load) and stable in the age group 40–59 years, and trends upward (roughly from 10% to 25%) in the category 20–39 years. In the category 60 years and older caseloads trended downward from 50% to 25% with the progression of pandemic, probably because of stricter intervention measures that started from the second half of March in various part of the world.23
The natural history of COVID-19 is still not well understood so reported periods of infectiousness and transmissibility also vary in research findings.24 A scoping review indicated different estimations for the average incubation period (from 4.8 to 5.6 to 7 days) in COVID-19 with a broad range of 2 to 14 days’ variation.25 This limitation hampers the process of effective case management and also attempts to estimate the basic reproduction number (R0) of COVID-19 for assessing its transmission potential. Nevertheless, the most up-to-date research findings suggest that age gradient and condition of comorbidity are definite markers in the probability of hospitalization requirement and risk of death.26- 27 In terms of epidemic preparedness, South Asian countries should in coming months plan their activities based on the three key analytical tools, namely, epidemiological projection, better clarity about the distribution of COVID-19 in communities, and technical know-how about the natural history of the disease, in order to prevent and control the pandemic.
3.2. Epidemiological projection
Epidemiological projection is the single most important priority task in epidemic preparedness. Projection provides an early prediction in order to prepare a blue-print for planning and operation. Epidemiological projection is a comparative exercise to explore and analyze the effectiveness of different control measures in epidemic management.28, 29, 30, 31, 32 However, the latest projection exercises have been shifting towards stochastic simulation models instead of traditional analytical models, which are otherwise good to understand the complexity of the disease and to explain the theoretical basis of epidemiological interventions.33, 34, 35
In this pandemic, mathematical models have become the most preferred forecasting tool for projection exercises. Four mathematical models for epidemiological forecasting in India have been developed by the Indian Council of Medical Research (ICMR) study, the Michigan study, the Hopkins study, and the Cambridge study.36 These mathematical computational models have data limitations, so are unable to capture the dynamicity of virus-human interaction in real lives.37 For example, standard epidemiological forecasting models like Susceptible-Exposed-Infectious-Recovered (SEIR) may not necessarily know the infectivity of sub-clinical cases, effectiveness of contact tracing, or even the success of quarantine measures, which are all vital in reducing susceptibility and/or exposure rates in communities.38 Forecasting models work better only when all the variables remain static, which is why their predictions may have worked during lockdowns where dynamic observations are remote. Concomitantly, it is also true that long term lockdown is impractical irrespective of economy size and social composition.
An epidemiological projection should consider the merits of forecasting models, and try to incorporate these approaches in an overall projection exercise. National-level forecasting in the context of South Asian countries is not very effective, however. The Indian example shows that India's eight northeastern states collectively accounted for only 52 cases out of a total of 16,116 cases as of April 19, 2020 but still had to face the implications of the initial 25-day lockdown, which commenced at midnight on March 25, 2020 just like the rest of the country.39 Similarly, the low number of cases in geographically smaller countries (Bhutan had 5 and Nepal 30 as of April 17, 2020) question the logic behind a nation-wide lockdown.23 The Maldives’ (28 positive cases by April 17, 2020) tactical deployment of a 14-day lockdown on its capital Male is well understood since it is a popular tourist destination and therefore a potential hotspot.40 In South Asia, where urban-rural disparity and intra-country regional or inter-state deprivation are common, these forecasting models are usually good for state-level or provincial management of epidemic preparedness. It would be an advantage to go for context-specific local models in order to have to make fewer assumptions and be mindful of local behaviors.
Considering the challenges highlighted by forecasting models, there is an urgent need that projection exercises should be based on a system of epidemiological intelligence and qualitative prediction for data processing and analysis. Epidemiological intelligence is an organizational network that comprises both public health surveillance and community action. An intelligence network is mandated for the ad hoc detection of unverified events and responsible for verifying, processing, and communicating unstructured information gathered from official, community, or even internet-based sources.41 In order to initiate that, secondary (or facility-specific) disease surveillance programs should be converted into field-based surveillance at least in most or severely affected districts or urban municipalities. Apart from sentinel surveillance sites, cluster surveillance practices based on the demarcation of hotspots or high-risk zones are also urgently required.
An intelligence network needs a trained workforce, which is a time consuming and a resource intensive process. Governments and health systems should take up the responsibility for developing this network by creating dedicated district-level posts for senior public health experts who could serve as disease detectives. The involvement of the community is also required where participatory epidemiologic methods can be followed up by investing in key community resources for developing capacity in field-based surveillance, control measures (like, suspected/active case finding), and communication actions.42 This network should remain active for at least the next two years with a gradual increase in strength and growth in quality. Epidemiological intelligence gathering and qualitative prediction should aim to seek data on both bio-social and bio-medical conditions of COVID-19 cases as well as on the general population in order to assess the situation and predict the future scenario. It thus is a timely call for the countries especially in low- and middle-income countries (LMICs) to further strengthen information architecture and to infuse a positive atmosphere for real-time data collection and reporting.43 The analysis of the intelligence network's processed feed should be based on context-relevant factors for better qualitative prediction. This prediction along with situation-specific forecasting models on a local level should be discussed, compared, and analyzed for a reliable epidemiological projection and to help develop and improve control measures accordingly.
3.3. Prevention and control measures
South Asian countries, known for their poorly resourced healthcare systems, are facing enormous challenges in combating the COVID-19 pandemic in the absence of viable antiviral drugs or vaccines. As a novel infectious disease, COVID-19 is epidemiologically classified as a human-to-human transmitted disease,44 and clinically classified as a respiratory disease.45 However, of late the WHO has acknowledged the likelihood of airborne transmission in specific circumstances and settings.46 The epidemiological classification predominantly guides and shapes prevention and control measures. Prevention and control measures are different, and they should not be used impulsively. For example, screening for travel history details, temperature monitoring, and testing for the virus were the first preventive measures to detect COVID-19 among travelers arriving at airports, crossing land borders, and entering ports from foreign countries to prevent imported COVID-19 cases. Consequently, as the infection rates picked up within a country/state controlling measures like contact tracing, isolation and quarantine, social distancing policy measures, travel restrictions, clinical management such as plasma therapy, oxygen support, intensive care unit (ICU) admissions, and lockdowns to ensure physical distancing have been progressively utilized in order to stop the spread and transmission of the SARS-CoV-2 virus. Hence, preventive measures should always be employed to prevent the occurrence of the disease, and control measures should be chosen in accordance with the epidemiological features of the disease to stop transmission in a geographically defined population.
3.3.1. Screening
Screening is an established preventive tool. Since the SARS-CoV-2 virus has now reached all the South Asian countries, screening measures will no longer be limited to international travelers but also needs to be expanded for intra-country mobility purposes. Recent research on the effectiveness of symptom and risk screening has estimated that even in a best-case scenario, airport screening would miss more than half of the infected cases due to the undetectability of sub-clinical cases, especially during the incubation period, and in cases where people are unaware of their risk exposure.47 Experience from South Asian countries adduced the same: outbreaks in several places could not be stopped despite all the countries imposing screening measures for international travelers by January 29, 2020.48 Thus, apart from thermal and symptom monitoring, individual risk assessment of travelers, such as pre- and post-travel interviews including assessment of recall bias, local authority certification from the source of travel, and post-travel quarantine options, should also be included. Additionally, rapid testing subject to screening verification of selected (or suspected) travelers as a preventive measure could also be a good option for most of the South Asian countries because of the high degree of mobility.
3.3.2. Lockdown
Non-pharmaceutical interventions (NPI) include contact tracing, case isolation, quarantine, social distancing, and lockdown. Lockdown has been the single most popular measure during the COVID-19 pandemic to ensure of physical distancing and stop human-to-human transmission. The rationale behind lockdown was to reduce the basic R0 of SARS-CoV-2.49 This control measure is generally aided by other major control measures, chiefly case testing, followed by case isolation, contact tracing, and quarantine. But South Asian countries came under severe criticism for their low testing rates and consequently being unsuccessful in finding active cases.50 In terms of policy implications, South Asia may have missed an opportunity presented by the lockdown window.
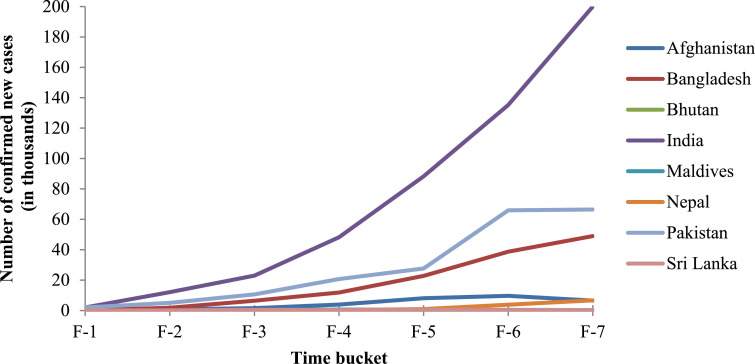
This technical error occurred because the estimated number of cases derived from mathematical models was been given more priority than epidemiological projections in the planning of the lockdown. Hence, from a technical perspective operative function (physical distancing to reduce R0) had become lockdown's sole objective in order to “flatten the curve”. As a result, the epidemic management ignored lockdown's strategic goal, namely, to contain the infection within a geographical area and accordingly make it infection free—succinctly a disease containment strategy in a given geographical area. This requires a quick spotting of outbreak sites and a rapid deployment of micro-management operations to hotspots. For instance, a modeling study in Wuhan, China suggests that active surveillance, contact tracing, quarantine, and early measures of stringent social distancing could be effective to stopping or slowing down virus transmission.51 Fig. 1 (and thereafter Table 1 ) show that strict lockdown measures in South Asian countries clearly curbed the growth of infection, but failed to reverse the growth trend.
Fig. 1.
Fortnightly number of new COVID-19 cases in South Asia*
*Source: As mentioned in Table 1, values of fortnightly country-wise corresponding cases are given in the table below. F-1: Fortnight-1 (2020/03/21‒2020/04/03); F-2: Fortnight-2 (2020/04/04‒2020/04/17); F-3: Fortnight-3 (2020/04/18‒2020/05/01); F-4: Fortnight-4 (2020/05/02‒2020/05/15); F-5: Fortnight-5 (2020/05/16‒2020/05/29); F-6: Fortnight-6 (2020/05/30‒2020/06/12); F-7: Fortnight-7 (2020/06/13‒2020/06/26).
Table 1.
Fortnightly number of new COVID-19 cases in South Asia*.
| Time bucket | Afghanistan | Bangladesh | Bhutan | India | Maldives | Nepal | Pakistan | Sri Lanka |
|---|---|---|---|---|---|---|---|---|
| Fortnight-1 | 246 | 37 | 3 | 2018 | 6 | 5 | 1955 | 79 |
| Fortnight-2 | 638 | 1777 | 0 | 12,077 | 9 | 24 | 5031 | 93 |
| Fortnight-3 | 1561 | 6400 | 2 | 22,958 | 440 | 29 | 10,633 | 446 |
| Fortnight-4 | 3933 | 11,827 | 14 | 48,154 | 563 | 217 | 20,685 | 245 |
| Fortnight-5 | 8041 | 22,779 | 12 | 88,273 | 560 | 936 | 27,658 | 623 |
| Fortnight-6 | 9659 | 38,679 | 29 | 135,230 | 412 | 3850 | 65,948 | 322 |
| Fortnight-7 | 6514 | 48,951 | 8 | 199,960 | 280 | 6693 | 66,478 | 134 |
| Total** | 30,592 | 130,450 | 68 | 508,670 | 2270 | 11,754 | 198,388 | 1942 |
*Source: Compiled from different WHO situational reports: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports;21,23,55, 56, 57, 58, 59, 60, 61 **Figures mentioned here record the country-wise total number of confirmed COVID-19 cases from 21 March to 26 June 2020. Fortnight-1: 2020/03/21‒2020/04/03; Fortnight-2: 2020/04/04‒2020/04/17; Fortnight-3: 2020/04/18‒2020/05/01; Fortnight-4: 2020/05/02‒2020/05/15; Fortnight-5: 2020/05/16‒2020/05/29; Fortnight-6: 2020/05/30‒2020/06/12; Fortnight-7: 2020/06/13‒2020/06/26.
South Asian countries, except the Maldives (where lockdown was prescribed for the capital Male and adjacent peri-urban areas only), went into lockdown mode between March 19 and April 1, 2020.49 , 52, 53 Lockdown continued with varied degrees of movement control in all these countries more or less till the end of May.54 From the first week of June onwards, South Asian countries (except Nepal) gradually started to move out of lockdown.
Lockdown was unable to arrest the exponential growth of new COVID-19 cases as shown in Fig. 1, especially in Afghanistan, Bangladesh, India, and Pakistan where caseloads are mostly concentrated. The doubling time for new cases was close to a fortnight for all four countries during the lockdown period March 21 to May 29, 2020. For example, in India fortnightly reported cases of COVID-19 leapfrogged from Fortnight-2 (12,077) to Fortnight-3 (22,958) to Fortnight-4 (48,154) to Fortnight-5 (88,273). Initially, Bhutan, the Maldives, and Sri Lanka appeared to have averted the exponential growth, and managed to keep individual caseloads to a satisfactory level during the last three months of lockdown. In contrast, Nepal, another small country, did not succeed in containing the infection. Nepal witnessed a spike in COVID-19 cases from Fortnight-5 (May 16–29) onwards, when other countries were in the process of easing their lockdown restrictions in order to restart their economies.
The lockdown was initially beneficial for all eight South Asia countries. Afghanistan, Bangladesh, India, and Pakistan have managed to contain the initial spike in the number of new cases reported fortnightly. Thus the spike between Fortnight-2 (22,958) and Fortnight-3 (48,154) was not as high as it was between Fortnight-1 (2018) and Fortnight-2 (12,077) for India. A similar pattern was observed for Pakistan. Afghanistan and Bangladesh also had a parallel trajectory, although they started to regulate the spike from fortnight three onwards instead of fortnight two. But overall, these four countries were accumulating a sizeable number of new cases every fortnight. This meant that during the period of lockdown, either new areas within these countries were getting affected from where the new cases were emerging (failure of governance), or the same affected areas were reporting more cases (failure of operation strategy). At the time of lockdown, the first proposition, in general, does not hold much merit, except in sporadic cases in new places owing to a relaxation of lockdown measures, due to mobility constraints. For instance, in India, the number of districts reporting new COVID-19 cases decreased from 356 on April 15, 2020 to 216 on May 8, 2020, whereas the total number of infected cases increased.62
The post-lockdown period from May 30 to June 26, 2020 a complex picture emerges. The ease of lockdown measures had not adversely impacted the growth of COVID-19 cases in the four most affected countries (Afghanistan, Bangladesh, India, and Pakistan). For these four countries, the number of fortnightly cases continued to rise in June, but at a lower rate. In fact, Afghanistan registered a negative growth in the last fortnight of June (9659 in Fortnight-6 to 6514 in Fortnight-7). The smaller countries, except Nepal, also remained effective in keeping their caseloads low in the post-lockdown period. Whether this was due to an enhanced operation strategy or the development of community-level immunity or something else, they recorded a slower growth in COVID-19 cases during the post-lockdown period. It is not possible to derive any analytical conclusion by observing only the last two fortnights’ data in the month of June—more time is required to understand the trend and to see the change, if any, in ground-level operational maneuvering. However, from the trajectories (from the beginning of lockdown to the present post-lockdown period) of Afghanistan, Bangladesh, India, Nepal, and Pakistan, it is evident that lockdown was not pursued with a strategic goal (disease containment) in order to rapidly sanitize the containment zone (or hotspots) to make them infection free through various control measures.
Countries need to think carefully before going for another long-term nation-wide lockdown. It is really a contested strategy for a region like South Asia where 36.6% of the population resides in urban areas (which are more exposed to the virus threat because of travel mobility and high population density).63 The urban spaces in South Asia lack proper housing and accommodation, especially for the millions of migrants and vulnerable populations.64 For example, Dharavi in Mumbai, India (Asia's biggest slum) was a hotspot with 214 positive cases and 13 deaths till April 23, 2020. For this place with a population of one million and a population density of 270,000/km2, depending fully on public community toilets (225) and communal water supplies, physical distancing even inside a tiny room was impossible.65, 66 The same concern is pertinent for densely populated Bangladesh (1240 people/ km2) and the Maldives (1719 people/ km2).67 Lockdown alone is not a public health solution for a COVID-19 outbreak in any densely populated area/country. Therefore, it is recommended that based on outbreak reporting, localized lockdown for 14 to 21 days aided by active public health surveillance, adequate testing, case finding, and strict quarantine of the exposed population in hotspot zones should be the outbreak operation structure of control measures in any South Asian country.
This pandemic-driven lockdown was based more on administrative forewarning than public health rationale to contain COVID-19 as strategic goal. This latter strategy has a two-fold approach arresting the transmission rate to make any defined community disease free, and planning for health system preparedness actions. Regarding the first approach, administrative readiness ensured a reduction in the transmission rate but the lack of knowledge related to public health had an undesirable impact on the effectiveness of control measures to contain the disease. The second approach is being actively pursued in order to buy time to prepare the health system by deferring the peak (when the need for medical support will be highest due to an exponential growth in infection rate) by a few weeks. This is especially relevant for the three most populated countries of South Asia (Bangladesh, India and Pakistan). A superficial observation indicates that while both disease containment strategy and health system preparedness actions are clearly public health responsibilities, resource allocation remains at the disposal of governance decisions. So South Asian countries (in fact many other countries in different parts of the world), have on the one hand, deployed bargained resources (testing, contact tracing, and quarantine centers for isolation) to contain the disease, while on the other hand, they are struggling to speed up health system preparedness arrangements (hospital beds, ICU facilities and ventilators, quarantine facilities, searching for stop-gap standard treatment protocol, etc.) likewise to delay a surge in healthcare system.
3.3.3. Testing
Lockdown is one of the few conditionals situations where both disease containment and planning for disease mitigation go hand-in-hand. It is obvious that a lack of resources leaves most South Asian countries stuck between two choices: prioritizing disease containment or mitigation action. Testing as a control measure could contain as well as mitigate the disease since it is primarily a case-finding mechanism. Testing is extremely low in most of the South Asian countries, except Bhutan, Nepal, and the Maldives.50 , 68 The cost of testing and its operation mostly through public provisioning are the main reasons behind governments’ constrained testing practice.69 In addition, COVID-19 confirmatory testing (reverse transcription polymerase chain reaction, RT-PCR) needs skilled human resources, technologically advanced laboratories, and accessible collection-cum-testing centers, which are altogether a challenging combination for most of the South Asian countries.
The South Asian experience indeed revealed the exercise of test rationing in COVID-19 control. The stringent testing guidelines imposed by many governments restricted access to testing to risk exposed population. For example, the ICMR, India's apex health research institute, until April 9, 2020 limited testing to individuals with symptoms arriving from abroad, symptomatic medical care workers, facility reported severe acute respiratory infection (SARI) patients and close contacts of COVID-19 laboratory confirmed cases.70 This strategy in effect excludes all suspected influenza-like illness (ILI) persons without any foreign travel or positive COVID-19 contact history from testing. Hence, institutional testing is strategized as an exclusive control measure.
Concurrently, it is also important to recognize that calling for mass testing may not be justifiable in the current public health situation. At the stage of local transmission and spread, testing coverage should be based on the principle of population risk assessment that builds on the strategy of access to geographical mobility of any defined population. In that order, in the general urban population compared to the peri-urban population, compared to rural population, is more at risk because of the greater chance of mobility and contact with already exposed populations. Similarly, people living in population dense urban slums are more vulnerable than people living in gated communities and high-rise buildings. Hence, the epidemic preparedness should identify the high risk zones of possible outbreaks in advance along with a list of existing hotspots in order to test all the clinically and the socially suspect cases.
There is a need also to develop a national testing policy instead of testing guidelines so that all states/provinces are able to prepare their own epidemic preparedness profile to geographically assess the population at risk, and to adhere strictly to the rational testing practice with all laboratory reported and/or referred cases. Furthermore, the South Asia region needs to explore and prioritize the option of using rapid-kit testing as soon as possible. This is a much negotiated resource compared to RT-PCR, and could be a primary mode a diagnostic alternative for asymptomatic or moderately symptomatic individuals. This effort could also lower the risk of transmission and death in a community. The tactical use of rapid testing may help in community surveillance on both the occasions of suspect case detection (through Immunoglobulin M, IgM) and reviewing immunity coverage (through Immunoglobulin G, IgG).
3.3.4. Contact tracing
Contact tracing is another mandated control measure. Across the world, all laboratory confirmed positive cases of COVID-19 are mandatorily followed up through contact tracing, testing (as per the symptoms, if needed), and case isolation and/or quarantine. Unless tested positive, the traced contacts should be in quarantine for a fortnight.71 For South Asian countries, the challenge is tracing the contacts given the high mobility and density of the population. The standard R0 (basic reproduction number of a laboratory confirmed cases) in South Asian countries is still unknown. In China (from Wuhan to various parts of Hubei province and the rest of China), the estimated R0 for the COVID-19 outbreak is 2–2.5/2.5.72 A computer simulation exercise estimated that 70% of contacts need to be traced for an R0 of 2.5, similarly, 90% of contacts need to be traced in case of an R0 of 3.5 to avoid any major outbreak.73 It is nearly impossible for countries like Bangladesh, India, or Pakistan to come even close to these percentages, and nearly impossible to achieve them. Hence, contact tracing (in the conventional practice, using humans as tracer) should be a tactical resource in the context of South Asia. It should also be used heavily at the time of sporadic transmission in any geographical area. Likewise, it is not very advisable to use resources for contact tracing in a situation of random transmission in major outbreak sites.
Apart from the conventional form of contact tracing, technology induced app-based surveillance is another tool that can be used to trace contacts as well as avoid large scale lockdown as implemented in South Korea and Singapore.74 But in South Asia the average proportion of the population using the Internet is 32%, and the figure is about 22% for the three most populated countries (as per 2017 data).75 Thus it seems to be an option post-lockdown for South Asia where access to smart phones, Internet availability, and Internet literacy are very low. Similarly, contact tracing as a tool in this region cannot guarantee individual privacy given the behavior of current political dispensations.76 However, this option should not be discarded because the 22% with access to the internet can also be assumed to be the most mobile population especially in an urban context, and thus likely to fall in the broader risk category. Hence, this can be an additional tracing tool provided there is parliament enacted legal safeguards for data protection as well as information security guarantees and a government-run operational framework for data decentralization of mobile-app traced information (against the centralization of data in one server) at a micro-level in COVID-19 surveillance.77
Irrespective of human or intelligence dependent tracing, the method for contact tracing should not be based on a risk exposure assessment of the contacts alone. The categorization as well as demarcation of high risk (primary) and low risk (secondary) contacts does not have much significance in South Asia because of contextual dynamics. Hence, it is advisable to use contact tracing as an overall risk minimization tactic for the contact's own community in order to crossover to risk communication measures. It is of no use if contact tracing is only construed as an act of tracing contacts for the purpose of quarantine or testing. In a densely populated area, contact tracing should be a combination of follow-ups with the contacts and the deployment of effective communication and social mobilization techniques to stop the spreading of panic, false information, and pervasive stigmatization that is attached to the disease. This particular method was successfully used in Nigeria's Ebola response.78
3.3.5. Risk communication
South Asian countries need to develop a context-specific risk communication module for social mobilization of community involvement to not only isolate contacts but also to sensitize the immediate community of contacts in any defined geographical area or space (e.g., workplace). This approach of contact tracing will not only help to sensitize the concerned community about its perceived risk due to prior exposure to contact(s) but also encourage community members to self-assess their risk and to report voluntarily, if need be.
The risk communication is also an independent prevention and control measure in the pandemic as it helps the community to willingly participate in outbreak management. The foremost requirement is to develop communication strategies based on the models of perception behavior attuned to the needs of individual communities. Communication strategies should not only educate the public about the available preventive measures, but also direct the public to reliable information sources. For example, drinking of cow urine as a preventive measure was initially promoted by some politico-religious groups in India.79 Thus effective and context-specific communication strategies could bring about positive outcomes for adhering to public health etiquettes and hygiene practices, and to prevent the spread of misbelieves among the public.
The other part is the management of information. Both misinformation (deducing wrong conclusions due to a lack of information) and disinformation (intentionally constructing untruths to push an agenda) are dangerous at the time of emergency. An analysis of the management of the Wuhan outbreak found that openness and access to information should be the guiding light to devise strategies and content involving a network of government experts and public collaborations with shared accountability to communicate risk.80 The countries need to urgently adopt the policy of COVID-19 information campaign embodying principles of transparency, reliability, trust, and collaboration for a timely and effective risk communication continuum.
3.4. Operational plan
From the onset of the COVID-19 pandemic, the South Asian countries, like the rest of the world, depended heavily on non-pharmaceutical interventions (NPIs). In policy terms, NPIs can be used either for suppression (strict prohibition on population movement indefinitely to halt the infection transmission fully and to keep caseloads extremely low) or mitigation (restricted movement of population to slow down infection transmission and to prevent a healthcare surge while protecting the most vulnerable from the disease) of the disease.49 NPIs in South Asia have by and large focused on a policy of suppression by spear-heading strict lockdown measures to combat COVID-19. Under this policy, the method of cordon sanitaire is applied to geographically quarantine the population and to contain the disease.81 But then again, this method was applied indiscriminately to entire geographical nation-state territories, and without giving much importance to public health planning or ensuring optimal use of control resources.
The region needs an urgent shift from a policy of suppression to mitigation in combatting COVID-19. The goal of a mitigation policy is to reduce the transmission of infection in order to limit a surge in the demand for healthcare services. Therefore, the policy should be built on the objective of distancing regulation that restricts the transmission of virus in the population. Hence, there has to be policy directive to adopt social distancing measures for minimizing social interaction opportunities. This can be done by promoting a work-from-home culture in as many sectors as possible, to encourage appropriate and safe online/phone-in commercial exchanges, an age/gender/time-wise roster for access to malls/markets/restaurants/open-air venues and special protection scheme for older adults.
Similarly, the policy guidance needs to discourage tourism, crowd-drawing sporting events, social/religious/cultural gatherings, and other events in order to limit the possibility of forming any future disease cluster. During the course of the pandemic, disease clusters originating from any form of congregation and then spreading to different geo-populations is a constant threat. Cases where the SARS-CoV-2 virus was transmitted to various geo-populations include a dinner party in Singapore, a church service in South Korea, a ski resort in Austria, a funeral in USA, a music event in Japan, and a religious assembly in India.82, 83 In a nutshell, policy guidelines need to promote social distancing tactics to ensure physical distancing in the social and economic lives of a population.
3.5. Intervention strategy
The execution of a mitigation policy is almost identical to suppression and employs similar control measures. The only change that is required is to switch from a disease containment strategy to a case containment strategy. Under the situation of lockdown within a defined geographic area, the disease containment strategy can contain the disease but not infection in South Asia's densely populated context. Therefore, in this containment strategy any COVID-19 positive case usually has enough time to progress to a disease (or developed severe symptoms), and finally increase the chance of being caught by the intervention. Thus, both the asymptomatic stage of positive COVID-19 cases (including individuals initially presenting with mild symptoms) and the cases that remain asymptomatic throughout the incubation and recovery period may not effectively be tracked and isolated in time by the intervention. These two categories of cases are the active agents of transmission of the SARS-CoV-2 virus in a population. The probability of missing these two categories of cases is high in South Asia because of the living conditions of the population, competition for limited resources, and their improper use as control measures. This interventional slip is a serious operative limitation of a disease containment strategy with regards to COVID-19. It also explains why the fortnightly number of new COVID-19 cases was not going down in South Asia's four most populated countries despite the lockdown.
In South Asia, a containment strategy should operationally (factoring in the population density) and contextually (reasoned with social and economic upheavals) be a feasible public health intervention and it should not be at the cost of economic livelihoods and stifle the social lives and medical needs of a population. The case containment strategy could be an effective approach in this regard. The strategy demands an integrated approach for intervention involving community to act as a bridge between public health operation and medical care mediation. It is an operational arrangement to identify and contain cases rapidly (preferably before the symptoms developed) in a community to eliminate the chance of further transmission. It embodies a model of absolute prevention of SARS-CoV-2 virus transmission from an infected individual.
This type of containment strategy is already in use for Dracunculiasis (guinea-worm disease) eradication in Africa.84 However, it could be redesigned to use as a disease control mechanism to combat COVID-19. Here the strategic change is that the unit of containment should be focused on cases instead of diseased individuals’ area/cluster/zone. Thus within the approach of disease control mechanism, along with regular control measures active in any geographical space, the method of prevention can be applied by focusing on the case to stop the virus's transmission.
The strategy in essence recognizes the community as a caretaker to guard against any invasion of the SARS-CoV-2 virus. The process needs urgent selection of community COVID detectives (CCDs) at a grass-root level and to equip them with the necessary skills to assess and detect any individual carrying the threat of virus infection. The CCDs as spotters need to be extremely familiar with local dynamics. The individual, immediate family members, or neighbors can assist CCDs in spotting and isolating suspect cases based on the standard protocol of community-level syndromic diagnosis including risk assessment exposure in any area (e.g., a municipal ward). Then the individual can be linked to a public health intervention center in the respective area to validate the case clinically. Accordingly, the intervention can provide the case with medical care support either in hospital or in non-hospital set-up. The involvement of communities, building its skill capacity, and risk communication are the key operative features in this strategy. The national case containment strategy is necessary in this regard to develop a country-wide public awareness campaign. This would include a procedural guideline for the containment of cases, the individual's role in preventing the transmission, and incentivizing the community in order to mobilize the entire country. However, it should also be kept in mind that countries or states with lower population densities (Bhutan or Arunachal Pradesh in India) may not need the case containment strategy.85, 86 The existing disease containment strategy with the adoption of a mitigation policy might be more prudent to maintain the low caseload in such a context.
3.6. Clinical management
Followed by the case (or the context-specific disease) containment strategy, the control intervention instantaneously steps in from epidemiological to clinical aspect of disease. COVID-19 as a respiratory disease can be managed in three different setups based on the clinical status (mild/moderate, severe, or acute) of the cases. According to the WHO, the caseload is more in line with mild/moderate pneumonia-like uncomplicated illnesses (81%), whereas admission to hospital (along with oxygen support) and intensive care are required only for about 14% severe pneumonia and 5% acute respiratory disease syndrome cases, respectively.87 Hence, the countries need to identify on early detection cases for early quarantine either at home or at government facilitated centers to save hospital reserves. Similarly, aged and individuals with a history of comorbidity could in principle be given mandatory hospital coverage to protect the most vulnerable.
In the process of case management measures, the preparedness of health systems, or more specifically the capacity of healthcare systems, should ideally be tested as a part of a response management mechanism in overall epidemic preparedness. The upgrading of a healthcare system is a resource (capital intensive) demanding process. Thus, South Asian countries should give more emphasis to the epidemiological management of a population instead of the clinical management of cases by strategically putting more emphasis on prevention and control measures.
3.7. Response management
Response management is a part of overall epidemic control. In outbreaks the observed number of cases is far greater than the expected number at any particular point of time. In the course of a pandemic, outbreaks can occur at any time and at any place. The 1918 influenza pandemic occurred in three distinct waves over a period of about twelve months.88 Control of an outbreak during a pandemic requires a rapid response once it is detected and confirmed by an epidemic intelligence unit. Thus, the development of response management mechanisms at the onset of this pandemic was a necessity to mobilize, reserve, manage, and coordinate the resources as required. The status of selective health system indicators in Table 2 in regard to COVID-19 preparedness shows that region is in special need of response management mechanism at the earliest.
Table 2.
Selective health system indicators of South Asian countries*.
| Countries | Domestic general government health expenditure (%)a |
Number of hospital (beds/1000) | Out-of-pocket expenditure (%)b |
Population above 65 years of age (%)c |
|---|---|---|---|---|
| Afghanistan | 0.60 | 5 | 76 | 3 |
| Bangladesh | 0.38 | 8 | 73 | 6 |
| Bhutan | 2.37 | 17 | 20 | 8 |
| India | 0.96 | 7 | 63 | 6 |
| Maldives | 6.45 | 4.9 | 19 | 4 |
| Nepal | 1.24 | 3 | 55 | 6 |
| Pakistan | 0.92 | 6 | 63 | 5 |
| Sri Lanka | 1.64 | 3.5 | 50 | 10 |
The overall resource allocation of national governments for health is below 1% of GDP in three of the most populated countries in South Asia (Bangladesh, India, and Pakistan). The availability of beds per thousand populations does not exceed ten, except in the case of Bhutan, which presents a challenge for access to inpatient services. Out-of-pocket share of medical expenses dominates the burden of healthcare expenditure at the cost of more non-public dependent service and the poor who cannot afford healthcare. The situation in Bhutan and the Maldives is much better than in the other countries, but they are also not comparable because of population size and other contextual differences. Considering the poor status of South Asia's key health system indicators, it is implicit that health system preparedness would require the difficult task of expanding healthcare infrastructure (hospital beds, ventilators, etc.) and the resource surplus status of emergency aids (skilled human resource, personal protective equipment, masks, testing kits, etc.).
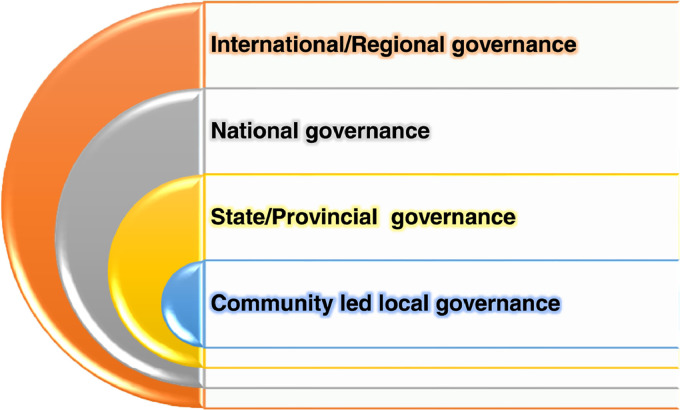
Under these circumstances, the mechanism for response management needs an approach of governance maximization instead of focusing only at resource maximization. For instance, South Asian countries people in the age group 65 years and older account for a small proportion of people in the overall population pyramid. This is a comparative advantage for the region when trying to keep the mortality rate low, as older people are the most vulnerable to COVID-19. Hence, policy actions and their proper implementation to protect the aged (and also persons with comorbidity) in the course of the pandemic will be more beneficial instead of leaving them socially unprotected and thereafter striving for more ventilators to cater for their medical needs. This framework of response management needs governance coordination (between local, state and national governments), collaboration (on a national and international level), and cooperation (within international/regional organizations and among countries).
Fig. 2 depicts the framework for response management when the community is fundamental to the entire scheme. The governance of local bodies needs to engage with the community in order to operate the model of participatory governance management in the COVID-19 response. Similarly, a layered response from the state and national governments is also needed to implement and plan responses. The outer-most circle illustrates the collaborative obligation of international actors with the countries to help in the design of response strategies in terms of planning and resource organization.
Fig. 2.
Response management framework.
3.7.1. Community-led local governance
The local body, urban and rural governance system, is the operative arm of response management. The Kerala state of India is a good example in this instance. The state's response to mitigate the effects of COVID-19 has been so far a great success.91 The community has been the frontrunner in Kerala to complement the government's various social security and grassroots surveillance initiatives.92 Participatory governance should be the principle for promoting or helping with the control measures. The containment strategy has already elaborated on the importance of community involvement in case finding and risk communication. The CCDs should be the “agent of change” in this entire response mechanism. Local governance must be aligned with civic bodies, self-help groups, and social institutions for information campaigns and local-area management (such as, social gatherings in market place/event, usage of community toilets, etc.). Similarly, the resource sharing of vector monitoring/control (of Malaria/Dengue control program) team in surveillance and risk communication measures is also essential.
3.7.2. State/provincial/division level governance
At this level governance is the implementation point for response management. The entire macro-management of COVID-19 response is in the realm of state-level governance. The efforts regarding healthcare system preparedness occurs mostly at this level. In this regard, both the expansion and demarcation of medical facilities and also the arrangement of large-scale quarantine centers is desirable. The role of private care facilities is decisive because of its strength and capacity in service delivery. However, in the case of India, the private sector was found to be driven more by business interests than supporting the government in fighting a common cause.93 The state governments in consultation with the union government need to compile a special policy guideline to utilize the private sector in service provision. The private sector cannot be left alone to decide its own role in care and support treatment during a time of national emergency. Similarly, the state governments also needs to develop district-wise profiles for epidemic planning that include the estimated capacity of the healthcare system at the time of the peak of the pandemic.
The governance needs to perform in a two-fold scheme: emergency response management and regular administrative management should go hand-in-hand. As a result, inter-departmental coordination guidelines should be put in place at ministerial and administrative levels. A decentralized orientation of governance, at least in response management, is required and should be followed in principle, otherwise community-led participatory governance will remain a policy component. State governments should play a central role in overall governance coordination to work with local as well as national governments. The state should not be limited to only implement decisions taken by the national government, but must rather take the lead in formulating and modifying the national response management plan by analyzing the experiences encountered by local governance.
3.7.3. National-level governance
The national response management should be the mechanism for policy, planning, and technical coordination. Over the course of the pandemic, any medical or economic setback can be debilitating for compromised populations’ health. The denial of healthcare services for non-COVID-19 patients or the plight of migrant laborers (economically one of the most vulnerable categories) to access welfare benefits are not anyway less demanding than controlling COVID-19 in South Asia.94- 95 Thus the response management should be mechanized with an aim to reshape governance to address both technical as well as humanitarian challenges posed by the pandemic. The technical amendment of the operative framework of the national health programs in order to develop a minimum convergence approach in the program implementation of a COVID-19 intervention is a priority, and to aspire for zero interruption in regular health service operation. Correspondingly, a carefully crafted pro-poor relief package to address financial, nutritional, and other social security needs should be a constant deliverable from the national governments.
The role of the national governments is to assist and not guide state governments in implementing response management. The coordination with state units to draft policy proposals, assess epidemiological projection, amend technical guidelines, analyze financial cost imperatives for resource generation are a few of the steps in this direction. It is unlikely that state or divisional units would be in a long-term position to allocate or generate adequate additional resources for the expansion of the healthcare system or safeguarding the interest of humanitarian causes. The time is ripe to go beyond fiscal space management conditionality and instead create space to source funds for resource investment (from testing kits to medical care infrastructure), and relief measures. Collaboration with international actors is another task for national governments to pull in financial (or material) resources and to develop technical expertise. One such collaborative example could be to create a positive environment for science and invention. India and Bangladesh have already shown good progress in mapping genetic evaluation and understanding rates of substitution (mutation of virus) of the SARS-CoV-2 virus.96- 97 This would not only help the respective countries but also add value to the work being done all over the world in drug and vaccine research.
3.7.4. International-level governance
Governance at an international level for supporting the cause of South Asia will be a testing period for global health. It will depend on the cooperation of international actors among themselves and between South Asian countries. Governance will need to address the technical capacity building areas to control outbreaks and the looming economic impediments facing the region. The technical form of governance cooperation from the WHO or other bilateral or multilateral partners may not be a cumbersome challenge and will need the assistance of countries on knowledge support (such as, in doing epidemiological projection), intervention design, research operation, and training management etc.
The slowdown in the global economy due to the pandemic and oil price fluctuations will be a more onerous challenge for the region's trade and economy, and also for remittance inflows.98 The international governance should support the South Asian countries from these forthcoming distresses by creating space for debt relief, interest free loans, or loans without conditional measures. In terms of political stability, the pandemic threat is likely to worsen the situation of stateless Rohingya refugee crisis in Bangladesh.99 A similar concern is for the war-torn Afghanistan and to manage COVID-19 there, especially with other existing health service operation shortcomings.100 Both the economic challenges and the political tensions will amplify the humanitarian emergency conditions in the region. International governance must help to address this complexity while dealing with the pandemic in South Asia.
Similarly, international governance also needs to uphold the spirit of global solidarity. The suspension of funding to the WHO announced on the April 15, 2020 by the United States could derail the global fight against the pandemic.101 Global solidarity campaigns like the People's Health Movement highlights that leadership by the WHO is at present most needed not only to steer the global health community but also to help countries, especially those in low-income category, to impart technical guidance and supply emergency medical aid.102 Member states should resolve the crisis at the earliest in order to strengthen the WHO for more effective international governance and to promote multilateralism in the fight to combat COVID-19.
Developing regions like South Asia must use diplomatic channels to rally support for multilateralism. This would also be more prudent for developing a global access agreement to a vaccine based in the spirit of equality. Thus regional consolidation of efforts to fight the pandemic is very important. The South Asian Association for Regional Cooperation (SAARC) has already taken a commendable step on this path by establishing an emergency fund of $18.8 million for the association's eight member countries to fight COVID-19.103
4. Discussions
Based on a situation analysis, this study assessed population-level public health measures to combat COVID-19 within the socioeconomic context of the South Asian region. Due to inadequate public investment in health systems, the South Asian region has relatively scarce healthcare resources. Poverty-inequality and fragile health systems aggravated pressure on medical resources brought on by COVID-19. Since a vaccine is still unavailable for now and a long-term lockdown program is unaffordable, the socioeconomic situation of the South Asian region required health sectors to find cost-effective plans to combat COVID-19 pandemic within limited budgets.
Given the populated density and resource hungry context of South Asia, a COVID-19 action plan should emphasize epidemiological projections, mitigation policies, case containment strategies, and four-tier response management. Based on periodic data collection on both bio-social and bio-medical conditions of COVID-19 cases, context-specific epidemiological projections can be constructed to assess the situation and predict future scenarios. Mitigation policy guidance, case containment strategies, and needs-based clinical management should correspond with prevention and control measures including screening, lockdown, adequate testing for risk-exposed populations, contact tracing in sporadic transmission areas, and context-specific risk communication for social mobilization. Response management needs an approach of governance maximization to cope with scarce and poor resource allocation, comprehensive governance coordination, collaboration, and cooperation.
One major limitation of this study is a lack data resources. In South Asia, where urban-rural disparities and intra-country regional and inter-state deprivation are common, forecasting models are usually only good for state-level or provincial-level management of epidemic preparedness. It would be an advantage to go for context-specific local models in order to have to make fewer assumptions and be mindful of local behaviors. However, this study had little access to timely updated population-level data for each country so that WHO data on a country level was adopted.
5. Conclusions
The pandemics, although infrequent on a global scale, are less so for the South Asian countries. The region has a long history of cohabitation with a number of infectious diseases. Many of them have become endemic over the years. SARS-CoV-2 is a noble virus and thus its infectivity and initial fatality were comparatively high. Prevention and control measures need to strike a chord between the health of the population and that of the economy. At present, neither one is safe until a miraculous medical intervention appears. Conversely, a population achieving herd immunity on its own is still scientifically and practically and remains doubtful time- and risk-consuming project.104
The South Asian region should ideally epitomize a model of governance that is always prepared and ready to suppress any outbreak. This alertness needs active participation of the community in the process of governance response to avert any risk at the earliest. The epidemiological management of the population with the adoption of mitigation policies to ensure the highest level of individual safety and assurance of minimal disruption in economy at the cost of lowest possible risk is the way out to combat the pandemic in South Asia.
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Funding
This paper was supported by the National Natural Science Foundation of China (No. 72042014).
Author contributions
AS, XZ and GL participated in conception of the research ideas, study design, interpretation of the findings. AS wrote the first draft of the manuscript. YJ and ZZ made critical revisions on the manuscript and provided implications of the study findings. All the authors gave final approval of the version to be published.
Acknowledgment
The co-authors wish to dedicate this paper in memory of Professor Zheng Xie, who passed away on June 4, 2020. Professor Xie conceived the idea and helped develop the manuscript. Her passion and dedications to global health will solely be missed by her colleagues and friends. Amitabha Sarkar is a China-India Visiting Scholar for the year of 2020‒2021 in the Department of Global Health, Peking University School of Public Health.
Disclaimer
The paper had consulted all the secondary resources till 15 May 2020, except the data related to total number of COVID-19 cases and deaths in South Asia for which the time-frame of 27 June 2020 has been considered. This excess time has been considered to see the post-lockdown trend also in the analysis while reviewing the paper based on editors' comments.
References
- 1.Rolling updates on coronavirus disease (COVID-19). World Health Organization website. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen. Accessed April 11, 2020.
- 2.A third of the global population is on coronavirus lockdown-here’s our constantly updated list of countries and restrictions. Business Insider India website. https://www.businessinsider.in/international/news/a-third-of-the-global-population-is-on-coronavirus-lockdown-x2014-hereaposs-our-constantly-updated-list-of-countries-and-restrictions/slidelist/75208623.cms. Accessed April 18, 2020.
- 3.Chakrabarti P. Curing cholera: pathogens, places and poverty in South Asia. Int J South Asian Stud (New Delhi) 2010;3:153–168. [PMC free article] [PubMed] [Google Scholar]
- 4.United Nations . United Nations; New York: 2019. World Economic Situation and Prospects 2019. [Google Scholar]
- 5.Poverty & Equity Data Portal. World Bank website. http://povertydata.worldbank.org/poverty/region/SAS. Accessed April 18, 2020.
- 6.Examining poverty trends in South Asian countries: where is Sri Lanka among its South Asian counterparts. The London School of Economics and Political Science website. https://blogs.lse.ac.uk/southasia/2018/07/31/examining-poverty-trends-in-south-asian-countries-where-is-sri-lanka-among-its-south-asian-counterparts/. Accessed April 18, 2020.
- 7.Sengupta A., Zaidi S., Sundararaman T., Onta S., Weerasinghe M.C. Tackling the primary care access challenge in South Asia. BMJ. 2018;363:k4878. doi: 10.1136/bmj.k4878. [DOI] [PubMed] [Google Scholar]
- 8.Zaidi S., Saligram P., Ahmed S., Sonderp E., Sheikh K. Expanding access to healthcare in South Asia. BMJ. 2017;357:j1645. doi: 10.1136/bmj.j1645. [DOI] [PubMed] [Google Scholar]
- 9.Akhtar S. Malnutrition in South Asia – a critical reappraisal. Crit Rev Food Sci Nutr. 2016;56(14):2320–2330. doi: 10.1080/10408398.2013.832143. [DOI] [PubMed] [Google Scholar]
- 10.Zaidi A.K., Awasthi S., deSilva H.J. Burden of infectious diseases in South Asia. BMJ. 2004;328(7443):811–815. doi: 10.1136/bmj.328.7443.811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.South Asia Must Ramp Up COVID-19 Action to Protect People, Revive Economies. World Bank website. https://www.worldbank.org/en/news/press-release/2020/04/12/south-asia-must-act-now-to-lessen-covid-19-health-impacts. Accessed April 14, 2020.
- 12.Coronavirus in South Asia, April 15, 2020: India, Pakistan, and Others Extend Lockdowns; Surge in Bangladesh As Modi, Khan, Hasina, and other leaders tackle COVID-19. Council on Foreign Relations website. https://www.cfr.org/blog/coronavirus-south-asia-april-15-2020-india-pakistan-and-others-extend-lockdowns-surge. Accessed April 17, 2020.
- 13.South Asia Faces Fresh Health Crisis As Children Miss Vaccinations. Barron’s website. https://www.barrons.com/news/south-asia-faces-fresh-health-crisis-as-children-miss-vaccinations-01588071906. Accessed May 1, 2020.
- 14.Worrying dip in TB registration,2020. The Telegraph website. https://epaper.telegraphindia.com/imageview_330610_3158377_4_71_06-05-2020_1_i_1_sf.html. Accessed May 6, 2020.
- 15.India’s focus on coronavirus leaves TB and HIV patients adrift. Scroll. in website. https://scroll.in/article/958400/invisible-crisis-tb-and-hiv-patients-left-adrift-in-indias-focus-on-coronavirus. Accessed April 11, 2020.
- 16.Covid outbreak hinders cancer treatment in hospitals. The Economic Times website. https://economictimes.indiatimes.com/industry/healthcare/biotech/healthcare/covid-outbreak-hinders-cancer-treatment-in-hospitals/articleshow/75033787.cms?from=mdr. Accessed April 11, 2020.
- 17.Fewer women are visiting health facilities for maternal services during lockdown. The Kathmandu Post website. https://kathmandupost.com/health/2020/04/28/fewer-women-are-visiting-health-facilities-for-maternal-services-during-lockdown. Accessed May 1, 2020.
- 18.The pandemic is ravaging the world’s poor, even if they’re untouched by the virus. The Washington Post website. https://www.washingtonpost.com/world/2020/04/15/pandemic-is-ravaging-worlds-poor-even-if-theyre-untouched-by-virus/. Accessed May 12, 2020.
- 19.Situation analysis and priority setting. World Health Organization website. https://www.who.int/nationalpolicies/processes/priorities/en/. Accessed May 1, 2020.
- 20.Clarke A.E. Sage; Thousand Oaks: 2005. Situational Analysis: Grounded Theory After the Postmodern Turn. [Google Scholar]
- 21.Federal Ministry of Health (FMoH) Federal Ministry of Health; Abuja: 2009. National Policy on Integrated Disease Surveillance Response in Nigeria. [Google Scholar]
- 22.World Health Organization. Coronavirus Disease 2019 (COVID-19) Situation Report-159. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200627-covid-19-sitrep-159.pdf?sfvrsn=93e027f6_2. Accessed July 5, 2020.
- 23.World Health Organization. Coronavirus Disease 2019 (COVID-19) Situation Report-89. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200418-sitrep-89-covid-19.pdf?sfvrsn=3643dd38_2. Accessed May 1, 2020.
- 24.Bedford J., Enria D., Giesecke J. COVID-19: towards controlling of a pandemic. Lancet. 2020;395(10229):1015–1018. doi: 10.1016/S0140-6736(20)30673-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Adhikari S.P., Meng S., Wu Y.J. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review. Infect Dis Poverty. 2020;9(1):29. doi: 10.1186/s40249-020-00646-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Verity R., Okell L.C., Dorigatti I. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis. 2020;20(6):669–677. doi: 10.1016/S1473-3099(20)30243-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention. JAMA. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 28.Tildesley M.J., Savill N.J., Shaw D.J. Optimal reactive vaccination strategies for a foot-and-mouth outbreak in the UK. Nature. 2006;440(7080):83–86. doi: 10.1038/nature04324. [DOI] [PubMed] [Google Scholar]
- 29.Ferguson N.M., Keeling M.J., Edmunds W.J. Planning for smallpox outbreaks. Nature. 2003;425(6959):681–685. doi: 10.1038/nature02007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chao D.L., Halloran M.E., Obenchain V.J., Longini IM Jr. FluTE, a publicly available stochastic influenza epidemic simulation model. PLoS Comput Biol. 2010;6(1) doi: 10.1371/journal.pcbi.1000656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Buhnerkempe M.G., Tildesley M.J., Lindström T. The impact of movements and animal density on continental scale cattle disease outbreaks in the United States. PLoS One. 2014;9(3):e91724. doi: 10.1371/journal.pone.0091724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Roche S.E., Garner M.G., Sanson R.L. Evaluating vaccination strategies to control foot-and-mouth disease: a model comparison study. Epidemiol Infect. 2015;143(6):1256–1275. doi: 10.1017/S0950268814001927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mollison D. Spatial contact models for ecological and epidemic spread. J R Stat Soc Series B Stat Methodol. 1977;39(3):283–326. [Google Scholar]
- 34.Anderson R.M., May R.M. Population biology of infectious diseases: part I. Nature. 1979;280(5721):361–367. doi: 10.1038/280361a0. [DOI] [PubMed] [Google Scholar]
- 35.May R., Anderson R. Transmission dynamics of HIV infection. Nature. 1987;326:137–142. doi: 10.1038/326137a0. [DOI] [PubMed] [Google Scholar]
- 36.COVID-19 Pandemic: Should You Believe What the Models Say About India? The Wire Science website. https://science.thewire.in/the-sciences/covid-19-pandemic-infectious-disease-transmission-sir-seir-icmr-indiasim-agent-based-modelling/. Accessed April 21, 2020.
- 37.Is the Coronavirus as Deadly as They Say? The Wall Street Journal website. https://www.wsj.com/articles/is-the-coronavirus-as-deadly-as-they-say-11585088464. Accessed April 21, 2020.
- 38.Karthikeyan G. Tracking the impact of interventions against COVID-19 in absence of extensive testing. Indian J Med Res. 2020;151(2 & 3):114–115. doi: 10.4103/ijmr.IJMR_864_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.COVID-19 INDIA. Ministry of Health and Family Welfare, Government of India website. https://www.mohfw.gov.in/. Accessed April 20, 2020.
- 40.South Asia coronavirus cases hit 22,000 as Maldives locks down capital. Reuters website. https://www.livemint.com/news/world/south-asia-coronavirus-cases-hit-22-000-as-maldives-locks-down-capital-11587128218040.html. Accessed April 17, 2020.
- 41.Barboza P., Vaillant L., Mawudeku A. Evaluation of epidemic intelligence systems integrated in the early alerting and reporting project for the detection of A/H5N1 influenza events. PLoS One. 2013;8(3):e57252. doi: 10.1371/journal.pone.0057252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schwabe C.W. 3rd ed. Williams & Wilkins; Baltimore: 1984. Veterinary Medicine and Human Health. [Google Scholar]
- 43.Betsch C., Wieler L.H., Habersaat K. Monitoring behavioural insights related to COVID-19. Lancet. 2020;395(10232):1255–1256. doi: 10.1016/S0140-6736(20)30729-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shereen M.A., Khan S., Kazmi A., Bashir N., Siddique R. COVID-19 infection: origin, transmission, and characteristics of human coronaviruses. J Adv Res. 2020;24:91–98. doi: 10.1016/j.jare.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Li K., Fang Y., Li W. CT image visual quantitative evaluation and clinical classification of coronavirus disease (COVID-19) Eur Radiol. 2020;30(8):4407–4416. doi: 10.1007/s00330-020-06817-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations. World Health Organization website. https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations#:∼:text=According%20to%20current%20evidence%2C,transmission%20was%20not%20reported. Accessed August 11, 2020.
- 47.Gostic K., Gomez A.C., Mummah R.O., Kucharski A.J., Lloyd-Smith J.O. Estimated effectiveness of symptom and risk screening to prevent the spread of COVID-19. Elife. 2020;9:e55570. doi: 10.7554/eLife.55570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.South Asia Economic Focus, Spring 2020: The Cursed Blessing of Public Banks. World Bank website. https://openknowledge.worldbank.org/handle/10986/33478. Accessed May 1, 2020.
- 49.Ferguson NM, Laydon D, Nedjati-Gilani G, et al. Report 9: Impact of Non-pharmaceutical Interventions (NPIs) to Reduce COVID-19 Mortality and Healthcare Demand. https://www.imperial.ac.uk/media/imperial-college/medicine/sph/ide/gida-fellowships/Imperial-College-COVID19-NPI-modelling-16-03-2020.pdf. Accessed May 1, 2020. [DOI] [PMC free article] [PubMed]
- 50.Coronavirus | South Asia remains an outlier in infections. The Hindu website. https://www.thehindu.com/news/national/coronavirus-south-asia-remains-an-outlier-in-infections/article31378180.ece. Accessed April 20, 2020.
- 51.Sanche S., Lin Y.T., Xu C., Romero-Severson E., Hengartner N., Ke R. High contagiousness and rapid spread of severe acute respiratory syndrome coronavirus 2. Emerg Infect Dis. 2020;26(7):1470–1477. doi: 10.3201/eid2607.200282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bhutan Announces Lockdown With Fourth Coronavirus Positive Cases. New Spotlight Online website. https://www.spotlightnepal.com/2020/03/31/bhutan-announces-lockdown-fourth-coronavirus-positive-cases/. Accessed April 25, 2020.
- 53.Maldives capital lockdown extended for two weeks. Maldives Insider website. https://maldives.net.mv/36466/maldives-capital-lockdown-extended-for-two-weeks/. Accessed April 25, 2020.
- 54.Coronavirus in South Asia, June 2020: Cases in India, Bangladesh, and Pakistan Spike. Council on Foreign Relations website. https://www.cfr.org/blog/coronavirus-south-asia-june-2020-cases-india-bangladesh-and-pakistan-spike. Accessed July 5, 2020.
- 55.World Health Organization. Coronavirus Disease 2019 (COVID-19) Situation Report-117. https://www.who.int/docs/default-source/coronaviruse/situation-2reports/0200516-covid-19-sitrep-117.pdf?sfvrsn=8f562cc_2. Accessed May 17, 2020.
- 56.World Health Organization. Coronavirus Disease 2019 (COVID-19) Situation Report-62. https://www.who.int/docs/default-source/coronaviruse/situation-reports/220200322-sitrep-62-covid-19.pdf?sfvrsn=755c76cd_2. Accessed May 1, 2020.
- 57.World Health Organization. Coronavirus Disease 2019 (COVID-19) Situation Report-75. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200404-sitrep-75-covid-19.pdf?sfvrsn=99251b2b_4. Accessed May 1, 2020.
- 58.World Health Organization. Coronavirus Disease 2019 (COVID-19) Situation Report-89. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200418-sitrep-89-covid-19.pdf?sfvrsn=3643dd38_2. Accessed May 1, 2020.
- 59.World Health Organization. Coronavirus Disease 2019 (COVID-19) Situation Report-103. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200502-covid-19-sitrep-103.pdf?sfvrsn=d95e76d8_6. Accessed May 15, 2020.
- 60.World Health Organization. Coronavirus Disease 2019 (COVID-19) Situation Report-131. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200530-covid-19-sitrep-131.pdf?sfvrsn=d31ba4b3_2. Accessed July 4, 2020.
- 61.World Health Organization. Coronavirus Disease 2019 (COVID-19) Situation Report-145. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200613-covid-19-sitrep-145.pdf?sfvrsn=bb7c1dc9_4. Accessed July 4, 2020.
- 62.After delay, plan for surveillance. The Telegraph website. https://www.telegraphindia.com/india/coronavirus-outbreak-indias-health-ministry-announced-a-plan-to-look-for-the-new-coronavirus-in-every-district-every-month/cid/1772299. Accessed May 12, 2020.
- 63.Southern Asia Population. Worldometer website. https://www.worldometers.info/world-population/southern-asia-population/. Accessed May 1, 2020.
- 64.The COVID-19 paradox in South Asia. The Hindu website. https://www.thehindu.com/opinion/lead/the-covid-19-paradox-in-south-asia/article31417806.ece. Accessed April 25, 2020.
- 65.COVID-19 Comes to Asia’s Most Densely Populated Slum. The Diplomat website. https://thediplomat.com/2020/04/covid-19-comes-to-asias-most-densely-populated-slum/. Accessed April 25, 2020.
- 66.These are the world’s five biggest slums. World Economic Forum website. https://www.weforum.org/agenda/2016/10/these-are-the-worlds-five-biggest-slums/. Accessed May 2, 2020.
- 67.Population density (people per sq. km of land area) - Bangladesh. World Bank website. https://data.worldbank.org/indicator/EN.POP.DNST?locations=BD. Accessed May 2, 2020.
- 68.Bangladesh far behind South Asian countries. Newage website. https://www.newagebd.net/article/105145/bangladesh-far-behind-south-asian-countries. Accessed May 2, 2020.
- 69.India’s private COVID-19 tests cost highest in South Asia. The Caravan website. https://caravanmagazine.in/health/india-private-covid-19-tests-cost-highest-in-south-asia-free-in-bangladesh. Accessed May 1, 2020.
- 70.COVID-19 Testing Strategy. Indian Council of Medical Research website. https://main.icmr.nic.in/content/covid-19. Accessed May 1, 2020.
- 71.European Centre for Disease Prevention and Control. Contact Tracing: Public Health Management of Persons, Including Healthcare Workers, Having Had Contact with COVID-19 Cases in the European Union – Second Update. https://www.ecdc.europa.eu/sites/default/files/documents/Public-health-management-persons-contact-novel-coronavirus-cases-2020-03-31.pdf. Accessed May 1, 2020.
- 72.World Health Organization. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf. Accessed May 1, 2020.
- 73.Hellewell J., Abbott S., Gimma A. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Glob Health. 2020;8(4):e488–e496. doi: 10.1016/S2214-109X(20)30074-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Show evidence that apps for COVID-19 contact-tracing are secure and effective. Nature. 2020;580(7805):563. doi: 10.1038/d41586-020-01264-1. [DOI] [PubMed] [Google Scholar]
- 75.Individuals using the Internet (% of population). World Bank website. https://data.worldbank.org/indicator/IT.NET.USER.ZS?name_desc=false. Accessed May 2, 2020.
- 76.‘Privacy minefield’: India COVID-19 app raises surveillance fears. Al Jazeera website. https://www.aljazeera.com/news/2020/05/minefield-india-covid-19-app-raises-surveillance-fears-200501090057782.html. Accessed May 3, 2020.
- 77.Germany flips to Apple-Google approach on smartphone contact tracing. Reuters website. https://www.reuters.com/article/us-health-coronavirus-europe-tech/germany-flips-on-smartphone-contact-tracing-backs-apple-and-google-idUSKCN22807J. Accessed May 3, 2020.
- 78.Maduka O., Maleghemi S., Komakech W. Effective risk communication and contact tracing for Ebola virus disease prevention and control – experiences from Port Harcourt, Nigeria. Public Health. 2016;135:140–143. doi: 10.1016/j.puhe.2015.10.037. [DOI] [PubMed] [Google Scholar]
- 79.Council on Foreign Relations. Coronavirus: Group hosts ‘cow urine party’, says COVID-19 due to meat-eaters. The Hindu website. https://www.thehindu.com/news/national/coronavirus-group-hosts-cow-urine-party-says-covid-19-due-to-meat-eaters/article31070516.ece. Accessed July 5, 2020.
- 80.Zhang L., Li H., Chen K. Effective risk communication for public health emergency: reflection on the Covid-19 (2019-ncov) outbreak in Wuhan, China. Healthcare. 2020;8(1):64. doi: 10.3390/healthcare8010064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ministry of Health and Family Welfare, Government of India. Containment Plan for Large Outbreaks Novel Coronavirus Disease 2019 (COVID-19). https://www.mohfw.gov.in/pdf/3ContainmentPlanforLargeOutbreaksofCOVID19Final.pdf#:∼:text=The%20Cluster%20Containment%20Strategy%20would,spread%20to%20new%20areas. Accessed May 1, 2020.
- 82.Coronavirus | Why must COVID-19 clusters be identified? The Hindu website. https://www.thehindu.com/sci-tech/health/why-must-covid-19-clusters-be-identified/article31259763.ece. Accessed May 4, 2020.
- 83.Pung R., Chiew C.J., Young B.E. Investigation of three clusters of COVID-19 in Singapore: implications for surveillance and response measures. Lancet. 2020;395(10229):1039–1046. doi: 10.1016/S0140-6736(20)30528-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Case containment strategy for eradication of dracunculiasis in Africa. World Health Organization website. https://www.who.int/docs/default-source/ntds/dracunculiasis/case-containment-strategy-for-eradication-of-dracunculiasis-in-africa.pdf?sfvrsn=c354bb1c_2. Accessed May 3, 2020.
- 85.Bhutan Population 2020. World Population Review website. https://worldpopulationreview.com/countries/bhutan-population/. Accessed May 3, 2020.
- 86.Top 10 Least Densely Populated States of India. Population Census 2011 website. https://www.census2011.co.in/facts/lowstatedensity.html. Accessed May 3, 2020.
- 87.World Health Organization. Clinical Management of Severe Acute Respiratory Infection When COVID-19 is Suspected. https://www.who.int/publications-detail/clinical-management-of-severe-acute-respiratory-infection-when-novel-coronavirus-(ncov)-infection-is-suspected. Accessed May 3, 2020.
- 88.Taubenberger J.K., Morens D.M. 1918 Influenza: the mother of all pandemics. Emerg Infect Dis. 2006;12(1):15–22. doi: 10.3201/eid1201.050979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Out-of-pocket expenditure (% of current health expenditure) - South Asia. World Bank website. https://data.worldbank.org/indicator/SH.XPD.OOPC.CH.ZS?locations=8S. Accessed April 24, 2020.
- 90.Domestic general government health expenditure (% of GDP) - South Asia. World Bank website. https://data.worldbank.org/indicator/SH.XPD.GHED.GD.ZS?locations=8S. Accessed April 26, 2020.
- 91.The Kerala Model. Project Syndicate website. https://www.project-syndicate.org/commentary/kerala-model-for-beating-covid-19-by-shashi-tharoor-2020-05. Accessed May 12, 2020.
- 92.Kerala begins reverse quarantine to protect vulnerable from Covid-19. Hindustan Times website. https://www.hindustantimes.com/india-news/kerala-begins-reverse-quarantine-to-protect-vulnerable-from-covid-19/story-KY3yAlYuKCymaJ5gQkmZVN.html. Accessed May 5, 2020.
- 93.The Government Must Stop Appeasing the Private Healthcare Sector. The Wire website. https://thewire.in/government/coronavirus-private-hospitals. Accessed May 3, 2020.
- 94.Non-COVID-19 Patients Are Paying the Price of India’s Efforts Against the Coronavirus. The Wire Science website. https://science.thewire.in/health/healthcare-non-coronavirus-patients/. Accessed May 6, 2020.
- 95.Stranded Workers Action Network. 21 Days and Counting: COVID-19 Lockdown, Migrant Workers, and the Inadequacy of Welfare Measures in India. The Hindu website. https://www.thehindu.com/news/resources/article31442220.ece/binary/Lockdown-and-Distress_Report-by-Stranded-Workers-Action-Network.pdf. Accessed April 10, 2020.
- 96.Bangladeshi researchers decode the Sars-Cov-2 genome sequence. Dhaka Tribune website. https://www.dhakatribune.com/health/coronavirus/2020/05/13/bangladeshi-researchers-decode-the-sars-cov2-genome-sequence. Accessed May 15, 2020.
- 97.Yadav P.D., Potdar V.A., Choudhary M.L. Full-genome sequences of the first two SARS-CoV-2 viruses from India. Indian J Med Res. 2020;151(2 & 3):200–209. doi: 10.4103/ijmr.IJMR_663_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.World Bank Predicts Sharpest Decline of Remittances in Recent History. World Bank website. https://www.worldbank.org/en/news/press-release/2020/04/22/world-bank-predicts-sharpest-decline-of-remittances-in-recent-history. Accessed May 1, 2020.
- 99.First coronavirus case confirmed in Cox’s Bazar, near world's largest refugee camp. CNN website. https://edition.cnn.com/world/live-news/coronavirus-outbreak-03-25-20-intl-hnk/h_01327d036f142e9132eef4f942b327fd?fbclid=IwAR1EtoXLUonSi0AEE-0IJhQZ3FW36eDCxJzYq4Pr_f80IPqh_jP_Ji5ziRE. Accessed May 3, 2020.
- 100.Shah J., Karimzadeh S., Al-Ahdal T.M.A., Mousavi S.H., Zahid S.U., Huy N.T. COVID-19: the current situation in Afghanistan. Lancet Glob Health. 2020;8(6):e771–e772. doi: 10.1016/S2214-109X(20)30124-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Trump suspends funding to World Health Organization. Financial Times website. https://www.ft.com/content/693f49e8-b8a9-4ed3-9d4a-cdfb591fefce. Access May 15, 2020.
- 102.PHM Condemns US Halt on Funding to WHO. People’s Health Movement website. https://phmovement.org/phm-statement-condemning-us-halt-on-funding-to-who/. Accessed May 1, 2020.
- 103.COVID19 Emergency Fund. South Asian Association for Regional Cooperation website. http://covid19-sdmc.org/covid19-emergency-fund. Accessed May 10, 2020.
- 104.“Immunity passports” in the context of COVID-19. World Health Organization website. https://www.who.int/news-room/commentaries/detail/immunity-passports-in-the-context-of-covid-19. Accessed May 1, 2020.