Abstract
Background
The COVID-19 pandemic has disrupted surgical practice worldwide. There is widespread concern for surgeon and provider safety, and the implications of hospital lockdown on patient care during epidemics.
Methods
Medline, EMBASE, CENTRAL, and PubMed were systematically searched from database inception to July 1, 2020 and ongoing monthly surveillance will be conducted. We included studies that assessed postoperative patient outcomes or protection measures for surgical personnel during epidemics.
Results
We included 61 studies relevant to the COVID-19 pandemic and past epidemics. Lockdown measures were noted globally including cancellation of elective surgeries and outpatient clinics. The pooled postoperative complication rate during epidemics was 21.0% among 2095 surgeries. 31 studies followed the health of surgical workers with the majority noting no adverse outcomes with proper safety measures.
Conclusions
This review highlights postoperative patient outcomes during worldwide epidemics including the COVID-19 pandemic and identifies specific safety measures to minimize infection of healthcare workers.
Keywords: COVID-19, Surgical outcomes, Epidemic, Health care worker, Lockdown
Introduction
The current COVID-19 pandemic has disrupted health services worldwide.1 , 2 There is a concern of nosocomial transmission, shortage of personal protective equipment (PPE), and limited resources for critical patients.3, 4, 5, 6 As a result, many hospitals have undergone lockdown procedures in which staffing and services are limited. These lockdown procedures have inconsistent policies, often occurring on an urgent basis with little notice or preparation. In previous outbreaks such as severe acute respiratory syndrome (SARS) and Ebola, these precautionary measures have lasted several months with downstream effects on health outcomes.7 , 8
Surgical practice is particularly at risk for lockdowns during outbreaks and epidemics.9 In particular, there may be a heightened risk for transmission of airborne pathogens during aerosolizing procedures in laparoscopic surgeries, though current evidence is unclear. In addition, there is risk of transmission of blood-borne viruses such as Ebola during accidental injuries.9 , 10 Operation techniques and equipment management may also be altered to reduce contact with potential vectors.9 In addition, intensive care units and emergency departments are often overwhelmed with critical care patients, with a limited supply of ventilators and bedspace.4 As such, the Centers for Disease Control and Prevention recently published an interim recommendation that all elective procedures should be cancelled during the COVID-19 pandemic.11 Surgical residents and staff may also be diverted to other specialties to provide frontline care if needed, as hospital volumes drastically increase.9 , 12
While there are numerous guidelines and editorials on the topic, there has not yet been a systematic assessment of the literature regarding surgical care and epidemics. Our living rapid systematic review aims to assess all research literature related to changes in surgical practice during disease outbreaks and epidemics, especially during the current COVID-19 pandemic.
Methods
Outcomes
The primary research question for the review was to investigate the impact of epidemics on surgical outcomes of patients undergoing urgent or elective surgery amidst periods of hospital lockdown. The specific outcomes included: (1) the number and type of surgical procedures performed during lockdowns (urgent, elective, or oncologic) (2) the number of non-OR procedures performed and its complications (3) the incidence of infected patients (confirmed and presumed) at the time of the procedure, or after the procedure, and the number of patients testing negative for infection after procedure.
The secondary aim of the review was to investigate the impact of an epidemic-caused lockdown on surgical practice. The following outcomes were collected: (1) the number of HCW, the incidence of HCW infected or not infected after procedures, and the incidence of mortality among HCW (2) the type of PPE items used by HCW, modified perioperative logistics, precautionary measures and interventions enforced for HCW protection, modified OR arrangements, and duration of protection (3) the description of lockdown, and outpatient clinic volume.
Data sources and search strategy
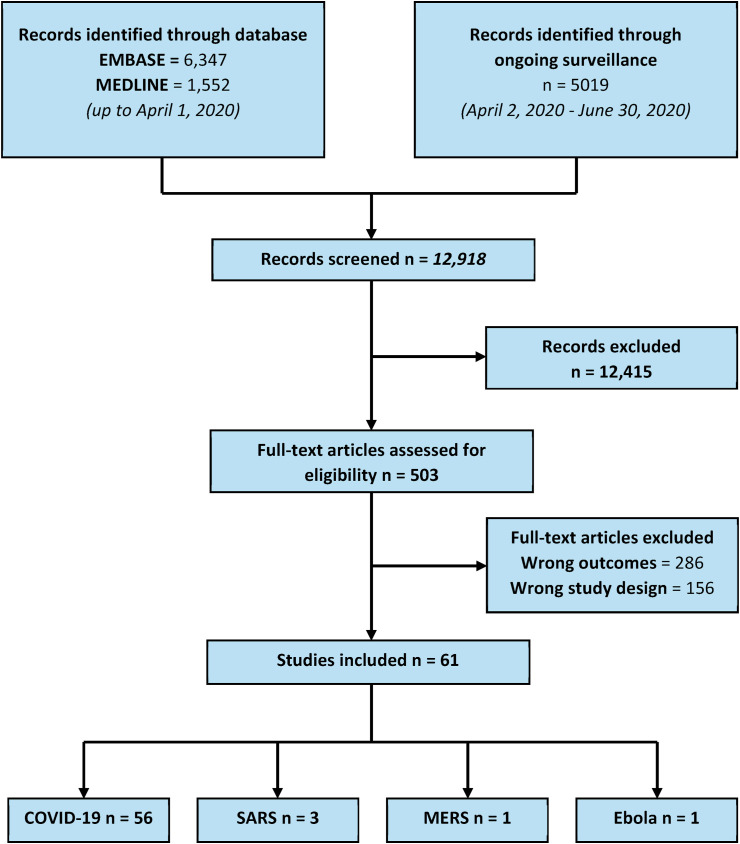
Medline, EMBASE, Cochrane Central Register of Controlled Trials (CENTRAL), and PubMed were systematically searched from database inception to April 2020, and ongoing surveillance was carried out until May 29, 2020. The search strategy (see Appendix 1) was designed in consultation with a medical librarian. This systematic review is reported in accordance with the Preferred Reporting items for Systematic Reviews and Meta-Analyses (PRISMA), with the PRISMA flow diagram presented in Fig. 1 .13
Fig. 1.
PRISMA Diagram – transparent reporting of systematic reviews and meta-analysis flow diagram outlining the search strategy results from initial search to included studies. Coronavirus disease 2019, COVID-19; Middle East respiratory syndrome-related coronavirus, MERS; Severe acute respiratory syndrome-related coronavirus, SARS.
Eligibility criteria and data abstraction
Studies reporting outcomes of patients undergoing surgery during an epidemic-caused hospital lockdown and studies investigating the impact of lockdown on surgical HCW and surgical practice were included. Articles were excluded from our review if they (1) were a review article, case report, letter to the editor, opinion, commentary, or editorial (2) did not contain at least one relevant outcome of interest (3) investigated a lockdown caused by a local hospital outbreak. No language or geographical restrictions were applied. Titles, abstracts, and full-text citations were screened, and conflict was resolved by the third reviewer. Two investigators extracted study data using a standardized spreadsheet, and verification of the extracted data was carried out by a third investigator. The following variables were abstracted from the included studies: study characteristics (e.g. author, year of publication, study design, study duration, country, type of epidemic, type of institution), patient demographics (e.g. number of patients included, age, sex), and study outcomes. Surgical outcomes were reported using the Clavien-Dindo Classification.14 The Accreditation Council of Graduate Medical Education (ACGME) Staging System was used reflect the degree of disruption caused by epidemics.15
Study quality assessment
Risk of bias of included studies was assessed using the Methodological Index for Non-Randomized Studies (MINORS), a 12 items-tool that evaluates the methodological quality of non-randomized studies.16 Discrepancies were discussed until consensus was reached. Studies were not excluded on the basis of quality.
Data synthesis
A narrative synthesis of study findings is provided along with a tabular summary of our primary and secondary outcomes of interest. Findings were reported and grouped into the following four outcome categories: (1) surgical procedures and outcomes, (2) surgical clinics and non-surgical procedures, (3) protection measures during outbreaks, and (4) patient exposures and HCW outcomes. Patient demographic data and quantitative outcomes across studies were pooled and reported using descriptive statistics. Measures of protection employed by HCW during outbreaks were further categorized into four groups: (1) PPE, PRE-OR, OR SETUP, LOGISTICS. These categories were developed via content analysis of the included studies. The synthesis without meta-analysis (SWiM) reporting guideline was followed closely for this systematic review.17
Living and rapid review
Due to the timing and relevance of our research questions during the ongoing COVID-19 pandemic, both rapid and living review approaches were employed to streamline the systematic review process, and to ensure that relevant emerging data was not omitted from our study.18, 19, 20 Ongoing surveillance for studies will be maintained on a two-to three-month basis, and updates to our manuscript will be made accordingly. Methods for study selection and data abstraction will remain consistent.
Results
Patient and hospital characteristics
34 retrospective studies, 16 case series, 5 descriptive studies, and 6 prospective studies represented a combined 3948 patients across 17 countries up to June 2020 (Table 1 ). Studies conducted during COVID-19 accounted for 98.6% of the included patients, while 1.2% were from studies during SARS, and 0.15% were from studies during MERS. Among papers describing patient demographics, 53.9% were female and median age was 62.0 years (range 1–100 years). A total of 455 health care workers were also represented with 70.1% HCW included during COVID-19, 28.1% included during SARS, and 1.8% included during Ebola epidemics.
Table 1.
Study characteristics.
| Author, year | Virus | Country | Institution type | Study type | N patients | N hospital personnel | % female | n female | Mean age (SD) |
|---|---|---|---|---|---|---|---|---|---|
| Angel, 2020 | COVID-19 | United States | Single institution | Retrospective chart review | 98 | 8 | 18.0% | 18 | 57 |
| Barca, 2020 | COVID-19 | Italy | Single institution | Retrospective study | 33 | 27.3% | 9 | 60.53 (range 20–80) | |
| Berardi, 2020 | COVID-19 | Italy | Single institution | Retrospective chart review | 72 | 34.7% | 25 | 64 (53–74) | |
| Bogani, 2020 | COVID-19 | Italy | Single institution | Retrospective review | 5 | 100.0% | 5 | Mean 68yrs (SD 7.1 yrs) | |
| Bundu, 2014 | Ebola | Sierra Leone | Single institution | Retrospective cohort | 8 | – | |||
| Cai, 2020 | COVID-19 | China | Single institution | Descriptive Study | – | ||||
| Cai, 2020 | COVID-19 | China | Single institution | Case series | 7 | 28.6% | 2 | Median age, 60 (IQR, 57–66) | |
| Chao, 2020 | COVID-19 | United States | Multi-institution | Prospective cohort study | 53 | 38.0% | 20 | Mean 62.0 years (±14.3yrs; range 23.5–81.7 yrs) | |
| Chee, 2004 | SARS | Singapore | Single institution | Retrospective chart review | 41 | 124 | – | ||
| Chen, 2020 | COVID-19 | China | Single institution | Case series | 17 | 48 | 100.0% | 17 | Epidural anesthesia patients 29.5 (3.1); General anesthesia patients 28.7 (1.6) |
| Cheung, 2020 | COVID-19 | USA | Single institution | Retrospective cohort | 10 | 20.0% | 2 | 80.5 (67–90) | |
| Chow 2020 | COVID-19 | Hong Kong | Single institution | Retrospective observational | 5 | – | |||
| Couto, 2020 | COVID-19 | United States | Single institution | Retrospective cohort study | 300 | Median 54.6 (range 1–90). Mean age 27. | |||
| Cruz, 2020 | COVID-19 | United States | Single institution | Retrospective review | 14 | 14.3% | 2 | Median 61.9 (range 43–83) | |
| Cui, 2020 | COVID-19 | China | Multi-institution | Case series | 20 | 45.0% | 9 | Median age 63 (range, 32–72) | |
| Deng 2020 | COVID-19 | China | Single institution | Retrospective Observational | 4 | 15 | 50.0% | 2 | 57.5 (14.1) |
| Doglietto, 2020 | COVID-19 | Italy | Single institution | Retrospective matched cohort study | 42 | 56.1% | 23 | Mean 75.95 (SD 15.17) | |
| Doran, 2020 | COVID-19 | United Kingdom | Single institution | Case series | 3 | 0.0% | 0 | 65 (10.4) | |
| Fregatti, 2020 | COVID-19 | Italy | Single institution | Retrospective cohort | 85 | 100.0% | 85 | ||
| Gallego, 2020 | COVID-19 | Spain | Single institution | Prospective cohort study | 189 | 49 | 57.2% | 108 | Elective surgery: 59.5; Urgent surgery: 81 |
| Gao, 2020 | COVID-19 | China | Single institution | Case series | 4 | 25.0% | 1 | 56.8 (11.3) | |
| Garcia-Portabella, 2020 | COVID-19 | Spain | Single institution | Retrospective case series | 11 | 63.6% | 7 | Mean 64.8 (SD 13.5) | |
| Gou, 2020 | COVID-19 | China | Single institution | Case series | 26 | – | |||
| Hassan 2020 | COVID-19 | USA | Single institution | Retrospective study | 91 | 40.7% | 37 | 52.9 (19.3) | |
| He, 2020 | COVID-19 | China | Single institution | Case series | 4 | 25.0% | 1 | 55.75 (range, 51–62) | |
| Huang, 2020 | COVID-19 | China | Single institution | Case series | 3 | 66.7% | 2 | 69.6 (14.6) | |
| Khalafallah, 2020 | COVID-19 | USA | Single institution | Retrospective descriptive | 51 | – | – | ||
| LeBrun, 2020 | COVID-19 | USA | Multi institution | Retrospective cohort | 59 | 75.0% | 44 | 85 (65–100) | |
| Lei, 2020 | COVID-19 | China | Single institution | Retrospective chart review | 34 | 58.8% | 20 | Median age, 55 (IQR, 43–63) | |
| Leong, 2020 | COVID-19 | Singapore | Single institution | Retrospective Descriptive Study | |||||
| Li 2020 | COVID-19 | China | Single-institution | Retrospective observational | 18 | – | |||
| Luong-Nguyen, 2020 | COVID-19 | France | Multi-institution | Retrospective study | 15 | 40.0% | 6 | Median age, 62 (range, 35–68) | |
| Madanelo, 2020 | COVID-19 | Portugal | Single institution | Retrospective chart review | 122 | 32.7% | 40 | 56.93 | |
| Maniscalco 2020 | COVID-19 | Italy | Multi-institution | Retrospective observational | 121 | 73.5% | 89 | 81.8 (NR) | |
| Maniscalco, 2020 | COVID-19 | Italy | Single institution | Retrospective review | 21 | 0 | |||
| Meyer 2020 | COVID-19 | France | Single institution | Prospective observational | 62 | – | |||
| Morrison 2020 | COVID-19 | USA | Single institution | Retrospective observational | 103 | – | |||
| Nazer, 2007 | MERS | Saudi Arabia | Single institution | Case series | 6 | 0.0% | 0 | 63 (18.2) | |
| Ng 2020 | COVID-19 | Singapore | Single institution | Retrospective study | 144 | 8 | – | – | |
| Oh, 2020 | COVID-19 | Korea | Single institution | Case series | 8 | 100.0% | 8 | 30 (25–39) | |
| Paramore 2020 | COVID-19 | UK | Single institution | Prospective observational | 52 | 13.5% | 7 | 66 (NR) | |
| Patel, 2020 | COVID-19 | UK | Single institution | Retrospective review | 75 | 45.0% | 34 | Median 47 (32–63); Mean 59 | |
| Peng, 2020 | COVID-19 | New Zealand | Single institution | Case series | 11 | 27.3% | 3 | Median age, 61 (51–69) | |
| Ralli, 2020 | COVID-19 | Italy | Single institution | Retrospective study | 96 | – | |||
| Rossi, 2020 | COVID-19 | Italy | Single institution | Descriptive Study | 79 | NR | |||
| Saban, 2020 | COVID-19 | Israel | Single institution | Retrospective Review | 142 | 11 | 54.2% | 77 | Mean 72.8 (13.6); Median 74 (range 21–98) |
| Schneider, 2020 | COVID-19 | Germany | Single institution | Retrospective review | 66 | ||||
| Shrikhande, 2020 | COVID-19 | India | Single institution | Prospective observational study | 494 | 65.0% | 321 | Median 48 (range 27–85) | |
| Taha, 2020 | COVID-19 | USA | Single institution | Prospective cohort study | 152 | – | |||
| Tan, 2020 | COVID-19 | China | Single institution | Descriptive study | – | ||||
| Tankel, 2020 | COVID-19 | Israel | Multi-institution | Retrospective comparative study | 130 | 45.4% | 64 | 23.3 (16.8) | |
| Tien, 2005 | SARS | Canada | Single institution | Case series | 4 | 4 | 25.0% | 1 | Median age of 3 patients 58; age of last patient 54 |
| Turri-Zanoni, 2020 | COVID-19 | Italy | Single institution | Case series | 32 | 33.0% | 11 | 62 (range, 32–74) | |
| Valdivia, 2020 | COVID-19 | Spain | Single institution | Retrospective chart review | 50 | 14 | – | – | |
| Wang, 2020 | COVID-19 | USA | Single institution | Case series | 5 | 20.0% | 1 | 52.8 | |
| Wong, 2004 | SARS | Hong Kong | Single institution | Case series | 3 | 100.0% | 3 | – | |
| Yang, 2020 | COVID-19 | China | Single institution | Retrospective chart review | 3 | 100.0% | 3 | Median age, 48 (range, 47–59) | |
| Yang, 2020 | COVID-19 | China | Single institution | Retrospective cohort | 55 | 28 | 32.7% | 18 | 65.1 (13.1) |
| Zagra 2020 | COVID-19 | Italy | Single institution | Retrospective chart review | 664 | ||||
| Zhang 2020 | COVID-19 | China | Single institution | Retrospective observational | 11 | 36.4% | 4 | 66.2 (range 32–93) | |
| Zhang, 2020 | COVID-19 | China | Single institution | Retrospective comparative study | 61 | 100.0% | 61 | (24–40 yrs) |
Hospital lockdown measures were described in 26 studies (Table 2 ). The most common measures included cancelation of elective surgery as specified in 84.6% of those studies, and a reduction or cancellation altogether of outpatient clinics specified in 23.1% of studies. One study reported stopping all planned activities to convert its center into a dedicated COVID-19 hospital.21 Another study described a MERS outbreak resulting from an index case admitted to the cardiac surgery ward with no specific precautions described.22 None of the included studies reported complete stoppage of educational activities to focus solely on patient care, as reflected by the ACGME Staging System scores.
Table 2.
Surgical data and patient outcomes.
| Author, year | Surgical service | Study Duration | Description of lockdown | N total number of surgeries | N elective surgeries (total; before outbreak; during outbreak) | N urgent surgeries (total; before outbreak; during outbreak) | N cancer surgeries (total; before outbreak; during outbreak) | CD I-II | CD III-IV | CD V | ACGME Stage |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Angel, 2020 | ICU | Mar 10 to Apr 15, 2020 | – | – | – | – | – | 2 | |||
| Barca, 2020 | Maxillofacial surgery | Feb to Apr 2020 | – | 33 | 0 | 20 | 13 | 2 | |||
| Berardi, 2020 | Surgical oncology, transplant surgery | Mar 9 2020 to Apr 24 2020 | Only major oncologic surgeries and transplantations. Outpatient clinics were significantly reduced. Multidisciplinary meetings were moved to a webinar platform. | 2019: 115; 2020: 72 | 0 | 12 | 60 | Major complications not specified (n = 5) | Death due to hyperacute allograft dysfunction (n = 1) | 2 | |
| Bogani, 2020 | Gynecologic oncology | Feb to Mar 2020 | – | 5 | 5 | Prolonged hospital course (n = 2); Post-op COVID-19 diagnosis (n = 5) | Death (n = 2) | – | |||
| Bundu, 2014 | Various | Jun 2013 to Feb 2015 | Elective surgeries cancelled starting July 2014 | 1444 | – | – | – | – | |||
| Cai, 2020 | Head and Neck | Feb 1 to Mar 10, 2020 | In-hospital treatment of benign or slow-progressing tumors postponed until after epidemic stabilization | 97 | 97 | Postop fever (n = 7) | 2 | ||||
| Cai, 2020 | Thoracic | Jan 2020 | None (before the outbreak was official declared) | 139 | – | – | 7 | Death due to COVID-19 pneumonia (n = 3) | – | ||
| Chao, 2020 | ICU | – | 2 | ||||||||
| Chee, 2004 | Various | Feb to Apr 2003 | Elective surgeries cancelled | 41 | – | – | – | – | |||
| Chen, 2020 | Obstetrics | Jan to Feb 2020 | – | 17 | 14 | 3 | 0 | None | None | – | |
| Cheung, 2020 | Orthopedics | Mar 1 to May 22 2020 | – | 10 | 0 | 10 | 0 | Supplemental oxygen (n = 5); blood transfusion (n = 10); presumed VTE (n = 1) | Acute Kidney injury (n = 1) | Death due to respiratory failure (n = 1) | – |
| Chow 2020 | ENT | Apr 1, 2020 and Apr 17, 2020 | – | 5 | – | – | 2/5 during outbreak | – | |||
| Couto, 2020 | Various | Mar to Apr 2020 | Elective aesthetic and reconstructive surgery cases were stopped after recommendations by the state of Texas. | – | |||||||
| Cruz, 2020 | ICU | Apr 2020 | – | – | |||||||
| Cui, 2020 | ENT | Jan to Mar 2020 | Outpatient clinics and emergency departments were closed for two of the hospitals. The larger hospital eliminated nonurgent visits, cancelled elective surgery, and avoided upper tract endoscopic exams | 3 | 1/6 as many elective surgeries performed during the pandemic | 3 | 0 | Coma (n = 2) | Death due to epistaxis (n = 1) | – | |
| Deng 2020 | ENT | Feb to March 2020 | – | – | – | – | – | – | |||
| Doglietto, 2020 | Various | Feb to Apr 2020 | Most elective surgeries were stopped. | 41 | 4 | 37 | Local complications n = 3); post-op COVID-19 diagnosis (n = 8) | Thrombotic complications (n = 4), hemorrhagic complications (n = 15), pneumonia (n = 18), delirium (n = 1) | Acute respiratory failure (n = 6), cardiogenic shock (n = 2), | – | |
| Doran, 2020 | HPB and Liver Transplant | Mar 2020 | Routine patient isolation for 7 days before surgery | 2 | 0 | 0 | 2 | Post-operative COVID pneumonia requiring oxygen (n = 1) | – | ||
| Fregatti, 2020 | Surgical oncology | Mar 9 to Apr 9 2020 | – | 85 | 0 | 0 | 85 | 2 | |||
| Gallego, 2020 | General Surgery | Mar 2020 | Elective surgeries cancelled after pandemic declared | 189 (number of admission and interventions decreased by 52.7%) | 153 | In the preceding month, 104 performed; after outbreak, 36 performed | NS but oncology procedures reported as urgent | Death due to respiratory failure from COVID-19 (n = 3) | 2 | ||
| Gao, 2020 | General surgery | Jan 23 to Mar 23, 2020 | – | 4 | 0 | 4 | 0 | None | None | – | |
| Garcia-Portabella, 2020 | Orthopedic Surgery | Mar to Apr 2020 | – | 11 | 11 | – | |||||
| Gou, 2020 | Pancreatic | Feb 2020 | – | 1 | 0 | 1 | – | Post-operative COVID-19 diagnosis (n = 1) | – | ||
| Hassan 2020 | Neurosurgery | Mar 23 – Apr 2020 | Elective procedures were cancelled | 91 | 0 | 91 | Death (n = 7) | 2 | |||
| He, 2020 | Vascular surgery/Anesthesiology | – | – | 4 | – | 4 | – | – | |||
| Huang, 2020 | Thorascopic lung surgery | Jan 1 2020 to Mar 31 2020 | Lung surgeries suspended since Jan 20 2020 | 3 | – | – | 3 (during outbreak) | COVID-19 infection (n = 3) | Death due to COVID-19 (n = 2) | – | |
| Khalafallah, 2020 | Neurosurgery | Mar 18 to Apr 17 2020 | Elective and nonelective procedures were cancelled (7600 cancelled during study period). A 68.89% reduction in total cases between Apr 2019 and Apr 2020. Increased adoption of telemedicine in outpatient setting, and teleconferencing services for educational activities. | 20 | 20 | 2 | |||||
| LeBrun, 2020 | Orthopedic | Mar 20 to Apr 24 2020 | – | 59 | 0 | 59 | Postoperative hypoxia (n = 18) | Hypoxia requiring intubation and admission to ICU (n = 3) | Death due to COVID-19 (n = 5), 2/5 preoperative 3/5 postoperative; Death due to cardiac arrest intraoperatively (n = 1); | – | |
| Lei, 2020 | Various | Jan to Feb 2020 | – | 34 | 29 | 0 | 5 | COVID pneumonia (n = 34), secondary infection (n = 10), arrhythmia (n = 8) | Acute respiratory distress syndrome (n = 11), shock (n = 10), acute cardiac injury (n = 5), acute kidney injury (n = 2) | Death (n = 7) | – |
| Leong, 2020 | Neurosurgery | Feb to Apr 2020 | All non-essential leave (inclusive of overseas and local conference leave) was cancelled. Strict social distancing policy. | 2 | |||||||
| Li 2020 | Kidney Transplant | Jan 20 to Mar 1, 2020 | 0 | 18 | – | 18 (100%) during outbreak | – | Delayed recovery of transplanted kidney function (n = 1) | Acute transplant rejection (n = 1) | – | |
| Luong-Nguyen, 2020 | General surgery | Mar to Apr 2020 | – | 11 | – | – | 5 | One unspecified post-op complication (n = 11) | Death secondary to respiratory failure (n = 1), death from candidal septicemia (n = 1) | – | |
| Madenelo, 2020 | Urology | Mar 11th 2020 to Apr 1st 2020 | State of emergency declared and social isolation instituted | 11 | – | 11; 18 during same period in 2019; | – | – | |||
| Maniscalco 2020 | Orthopedics | Feb 22 2020–Apr 18 2020 | – | 121; 169 during same period in 2019 | – | 121 (100%) during outbreak | – | Death (cardiac arrest n = 8; multi-organ failure n = 3; progression of neoplasm n = 2; renal failure n = 1; brain hemorrhage n = 1; septic shock n = 1; total n = 17); Death total n = 6 during same period in 2019 | – | ||
| Maniscalco, 2020 | Orthopedics and Traumatology | Feb 25 to Mar 31 2020 | All planned activities stopped, ICU capacity troped, hospital converted into designated “COVID-19 hospital” | 96; 125 same time period 2019 | – | 96 | – | – | |||
| Meyer 2020 | Spine | Mar 17 2020–Apr 17 2020 | Elective surgeries were cancelled | 62 | 0 | 62 (100%) during outbreak | – | – | |||
| Morrison 2020 | ENT | Mar 18 – Apr 21–2020 | Elective surgeries were cancelled, limited OR space, limited clinics | 103 | 0 | 103 (100%) during outbreak | – | 2 | |||
| Nazer, 2007 | Cardiac | Jan to Feb 2015 | None | 6 | 1 | 5 | 0 | Subdural hematoma (n = 1), perioperative MI (n = 1) | |||
| Ng 2020 | Vascular | Feb–Mar 2020 | Elective surgeries were cancelled | 291 | 2 | ||||||
| Oh, 2020 | Obstetrics | Feb 26 to Apr 3 2020 | The hospital’s delivery center was designated for suspected or confirmed mothers of COVID-19 only | 8 | 0 | 8 | 0 | No complications | – | ||
| Paramore 2020 | Urology | Mar 23 2020–Apr 9 2020 | Cancellation of routine elective surgery, limit surgical resources to risk-stratified patients | 52 | – | 6 (11.5%) during outbreak | – | UTI (n = 2) | – | ||
| Patel, 2020 | General Surgery | Mar to Apr 2020 | Outpatient clinics and endoscopic procedures decreased to limit spread of virus; elective non-cancer surgery cancelled. | 20 | 20 | – | |||||
| Peng, 2020 | Thoracic | Jan 2020 | Elective surgeries cancelled on last day of study period | 121; 11 | 84 cancelled | 121; 0 | 4/11 patients in case series had cancer surgery; 11 | Prolonged air leak (n = 1) | Sudden cardiac arrest from hypokalemia (n = 1) | Death from respiratory failure due to COVID-19 (n = 3) | – |
| Ralli, 2020 | Otolaryngology | Feb to Apr 2020 | Elective surgeries cancelled. Emergent and oncology cases only. | 96 (50.77% decrease in overall number of surgical procedures) | 0 | 22 | Same timepoint 1 year ago, 195 procedures; 74 after outbreak | – | |||
| Rossi, 2020 | Orthopedic Oncology | Dec 2019–Apr 2020 | Elective orthopedic surgery was forced to stop to allow the healthcare system to face the emergency. | 79 | 79 | 0 | 0 | 0 | – | ||
| Saban, 2020 | Ophthalmology | – | – | 3 | – | ||||||
| Schneider, 2020 | Orthopedic Surgery | – | Temporary ban on elective surgery and outpatient clinics, rigorous visitor restrictions, and compulsory facemasks for all HCW | – | |||||||
| Shrikhande, 2020 | Various | Mar to Apr 2020 | 494 | 494 | Minor CDI-II + postop COVID-19 | – | |||||
| Taha, 2020 | Otolaryngology | Mar to Apr 2020 | Elective surgeries cancelled | 12 | 0 | 12 | 0 | – | |||
| Tan, 2020 | Neurosurgery | - (published Mar 2020) | Operations for patients with relatively stable condition postponed | – | – | – | – | – | |||
| Tankel, 2020 | General Surgery | Feb to Apr 2020 | – | 130 | 0 | 130 (202 in 7 wks preceding) | 0 | “Serious complication " (n = 1) | – | ||
| Tien, 2005 | ICU; Emergency OR | May 2013 | – | 1 | 0 | 1 | 0 | Death from presumed abdominal compartment syndrome (n = 1) | – | ||
| Turri-Zanoni, 2020 | Otolaryngology | Feb to Apr 2020 | – | 13 | 13 (tracheostomy procedures labeled as elective in the study, performed in OR) | – | – | Death due to COVID-19 (n = 5) | – | ||
| Valdivia, 2020 | Vascular surgery | Mar 14 to May 14 2020 | Only urgent surgeries were performed, vascular surgery department was partially converted to COVID-19 unit | 60 | 0 | 60 | 0 | Death due to acute respiratory distress syndrome (n = 1) | 2 | ||
| Wang, 2020 | Neurosurgery | – | – | 5 | 0 | 5 | 0 | Death due to COVID-19 related complications (n = 3) | – | ||
| Wong, 2004 | Obstetrics | Apr-03 | – | 3 | 0 | 3 | – | Wound infection (n = 2) | – | ||
| Yang, 2020 | Gynecologic oncology | Jan to Feb 2020 | – | 189 | 0 | 0 | 189 | COVID pneumonia (n = 3) | – | ||
| Yang, 2020 | Neurosurgery | Jan 23 to Mar 7 2020 | – | 55 | 0 | 55 | 0 | – | |||
| Zagra 2020 | Orthopedics | February 24th to April 10th, 2020 | Cancellation of elective surgeries | 823 | 664 | 268 | 2 | ||||
| Zhang 2020 | ENT | Jan 23 2020–April 6 2020 | – | – | – | – | – | – | |||
| Zhang, 2020 | Obstetrics | Jan to Feb 2020 | – | 61 | – | 61 | – | Neonatal bacterial pneumonia (n = 3/10) | – |
Surgical procedures and outcomes
Data were reported for a total of 3850 surgeries, with 96.1% of those performed during COVID-19, 2.5% during Ebola, 1.2% during SARS, and 0.16% during MERS epidemics (Table 2). The following surgical specialties were represented in the included studies: otolaryngology and maxillofacial surgery (16.4%); orthopedics (13.1%); obstetrics and gynecology (9.8%); neurosurgery (9.8%); general surgery (8.2%); vascular surgery (6.6%); surgical ICU (6.6%); thoracic surgery (4.9%); hepatobiliary, pancreatic, and liver transplant (3.3%); urology (3.3%); surgical oncology (3.3%); kidney transplant (1.6%); cardiac surgery (1.6%); and spine surgery (1.6%). Of the included studies, 6.6% included data on more than one surgical specialty. Among all included surgeries, 36.5% were urgent, 23.2% were elective, and 10.8% were oncologic.
Post-operative complications were reported in 59.0% of studies. Four studies noted no complications following surgery.23, 24, 25, 26 A total of 440 complications were reported, with the most common ones being all-cause mortality accounting for 14.3% of complications, postoperative diagnosis of COVID-19 accounting for 12.0%, and hemorrhagic complications accounting for 7.3%. Of those studies reporting on complications, the pooled complication rate among 2095 surgeries was 21.0%. The pooled rate of minor complications (Clavien-Dindo Grades I-II) was 12.3%, the rate of major complications (Clavien-Dindo Grade III-IV) was 5.3%, and the rate of all-cause mortality (Clavien-Dindo Grade V) was 3.4%. The complication rate among COVID-19 surgeries alone was 20.9%. Mortality secondary to complications from COVID-19 was reported in 1.1% of postoperative patients during the COVID-19 pandemic. Of note, multiple complications occurred in a single patient in some instances.
Non-surgical procedures and surgical clinics
Non-surgical procedures (defined in this study as procedures performed outside of an OR) were performed in 21.3% of studies and included tracheostomy, nasal endoscopy, central venous catheterization, balloon dilatation of hepaticojejunostomy, intravitreal injections, peritoneal dialysis, and percutaneous drainage of various anatomical compartments (Table 3 ). A total of 346 procedures were specified during epidemics, with a pooled post-operative complication rate of 14.5% among studies reporting on complications. The most common complications included death accounting for 41.9% of complications and post-procedural bleeding accounting for 29.0%. As described above for surgical complications, multiple complications may have been reported following a single procedure.
Table 3.
Non-OR procedures and outpatient clinics.
| Author, year | Surgical service | Study duration | Non-surgical procedures performed (e.g. endoscopy, tracheostomy) | N of procedures performed (total; before outbreak; during outbreak) | Complications | Outpatient clinic volumes (total; before outbreak; after outbreak) |
|---|---|---|---|---|---|---|
| Angel, 2020 | ICU | Mar to Apr 2020 | Percutaneous dilational tracheostomy (PDT) | 98 | Post-tracheostomy bleeding (n = 5), Accidental tracheostomy tube removal (n = 2), death (n = 7) due to respiratory and multiorgan failure | – |
| Barca, 2020 | Maxillofacial surgery | Feb to Apr 2020 | – | – | – | – |
| Berardi, 2020 | Surgical oncology, transplant surgery | Mar 9 2020 to Apr 24 2020 | – | – | – | – |
| Bogani, 2020 | Gynecologic Oncology | Feb to Mar 2020 | – | – | – | – |
| Bundu, 2014 | All | Jun 2013 to Feb 2015 | – | – | – | – |
| Cai, 2020 | Head and Neck | February 1 to March 10, 2020 | – | – | – | – |
| Cai, 2020 | Thoracic | Jan-20 | – | – | – | – |
| Chao, 2020 | ICU | – | Tracheostomy | 53 | Minor: cellulitis (n = 1), bleeding (n = 1). Death (n = 6) |
– |
| Chee, 2004 | All | Feb to Apr 2003 | – | – | – | |
| Chen, 2020 | Obstetrics | Jan to Feb 2020 | – | – | – | – |
| Cheung, 2020 | Orthopedics | March 1 to May 22 2020 | – | – | – | – |
| Chow 2020 | ENT | April 1, 2020 and April 17, 2020. | – | – | – | – |
| Couto, 2020 | Various | Mar to Apr 2020 | – | – | – | – |
| Cruz, 2020 | ICU | Apr-20 | Peritoneal Dialysis | 14 | bleeding (n = 1), catheter non-function (n = 1) | |
| Cui, 2020 | ENT | Jan to Mar 2020 | Percutaneous dilatational tracheotomy | 3 | Bleeding and obstruction of extracorporeal membrane oxygenation (ECMO) flow leading to death (n = 1) | ¼ as many outpatient visits during pandemic, 5765 telemedicine encounters |
| Deng 2020 | ENT | Feb to March 2020 | Tracheotomy | 4 during outbreak | Postop incision bleeding (n = 1) | – |
| Doglietto, 2020 | Various | Feb to Apr 2020 | – | – | – | – |
| Doran, 2020 | HPB and Liver Transplant | Mar-20 | Biliary drainage and balloon dilatation of hepaticojejunostomy | 1 | Asymptomatic post-operative COVID pneumonia (n = 1; CD I) | – |
| Fregatti, 2020 | Surgical oncology | Mar 9 to Apr 9 2020 | – | – | – | – |
| Gallego, 2020 | General Surgery | Mar-20 | – | – | – | – |
| Gao, 2020 | General surgery | Jan to Mar 2020 | – | – | – | – |
| Garcia-Portabella, 2020 | Orthopedic Surgery | Mar to Apr 2020 | – | – | – | – |
| Gou, 2020 | Pancreatic | Feb-20 | Central venous catheterization and percutaneous drainage of the thoracic cavity, abdominal cavity, retroperitoneum, and gallbladder | 7 | Hypoxemia during percutaneous retroperitoneal drainage (n = 1) | – |
| Hassan 2020 | Neurosurgery | March 23 2020–April 20 2020 | – | – | – | – |
| He, 2020 | Vascular surgery/Anesthesiology | – | – | – | – | – |
| Huang, 2020 | Thorascopic lung surgery | Jan 1 2020 to March 31 2020 | – | – | – | – |
| Khalafallah, 2020 | Neurosurgery | Mar 18 to Apr 17 2020 | – | – | – | NR; 281 (Apr 2019); 9 (Apr 2020) |
| LeBrun, 2020 | Orthopedics | Mar 20 to Apr 24 2020 | – | – | – | – |
| Lei, 2020 | All | Jan to Feb 2020 | – | – | – | – |
| Leong, 2020 | Neurosurgery | Feb to Apr 2020 | – | – | – | – |
| Li 2020 | Transplant | January 20 to March 1, 2020 | – | – | – | 220 telemedicine appointments (during pandemic); 68 outpatient visits (during pandemic) |
| Luong-Nguyen | General Surgery | Mar to Apr 2020 | – | – | – | – |
| Madanelo, 2020 | Urology | Mar to Apr 2020 | – | – | – | 122 during COVID; 263 during same period in 2019 |
| Maniscalco 2020 | Orthopedics | Feb 22 2020–Apr 18 2020 | – | – | – | – |
| Maniscalco, 2020 | Orthopedics and Traumatology | Feb to Mar 2020 | – | – | – | 100 (per day?) until Feb 21st; 30 (per day?) since Mar 13th; Outpatient clinic activity reduced by 50% |
| Meyer 2020 | Spine | March 17 2020–April 17 2020 | – | – | – | – |
| Morrison 2020 | ENT | March 18 – April 21–2020 | – | 20 before outbreak, 16 after outbreak | – | 158 before pandemic, 39 after pandemic |
| Nazer, 2007 | Cardiac | Jan to Feb 2015 | – | – | – | – |
| Ng 2020 | Vascular | Feb–March 2020 | – | – | – | Reduced from 10 half-days a week to 5 half-days a week |
| Oh, 2020 | Obstetrics | Feb 26 to Apr 3 2020 | – | – | – | – |
| Paramore 2020 | Urology | Mar 23 2020–Apr 9 2020 | – | – | – | – |
| Patel, 2020 | General surgery | Mar to Apr 2020 | – | – | – | 0 |
| Peng, 2020 | Thoracic | Jan-20 | – | – | – | – |
| Ralli, 2020 | Otolaryngology | Feb to Apr 2020 | – | – | – | – |
| Rossi, 2020 | Orthopedic Oncology | Dec 2019–Apr 2020 | – | – | – | – |
| Saban, 2020 | Ophthalmology | – | Intravitreal injection, panretinal photocoagulation laser therapy | 116 | – | – |
| Schneider, 2020 | Orthopedic Surgery | – | – | – | – | – |
| Shrikhande, 2020 | Various | Mar to Apr 2020 | – | – | – | – |
| Taha, 2020 | Otolaryngology | Mar to Apr 2020 | Nasal endoscopy | >100 | – | – |
| Tan, 2020 | Neurosurgery | – | – | – | – | – |
| Tankel, 2020 | General surgery | Feb to Apr 2020 | – | – | – | – |
| Tien, 2005 | ICU; Emergency OR | May-13 | Tracheostomy | 4 | None | – |
| Turri-Zanoni, 2020 | Otolaryngology | Feb to Apr 2020 | Percutaneous dilatational tracheostomy | 19 | No procedure mortality observed | – |
| Valdivia, 2020 | Vascular surgery | Mar 14 to May 14 2020 | – | – | – | – |
| Wang, 2020 | Neurosurgery | – | – | – | – | – |
| Wong, 2004 | Obstetrics | Apr-03 | – | – | – | – |
| Yang, 2020 | Gynecologic Oncology | Jan to Feb 2020 | (200 non-surgical hospitalizations) | – | – | – |
| Yang, 2020 | Neurosurgery | Jan 23 to Mar 7 2020 | – | – | – | – |
| Zagra 2020 | Neurosurgery | Jan 23 to Mar 7 2020 | – | – | – | – |
| Zhang 2020 | ENT | Jan 23 2020–April 6 2020 | Tracheostomy | 11 (during outbreak) | Wound infection (n = 2); subcutaneous emphysema (n = 1) | – |
| Zhang, 2020 | Obstetrics | Jan to Feb 2020 | – | – | – | – |
Seven studies (11.5%; 7/61) reported active outpatient clinics during epidemics, though there was an overall reduction of clinic volume by 50%–75%. Eight studies, all during the COVID-19 epidemics, also reported the use of telemedicine and virtual care modalities for outpatient consults and follow-up appointments.26, 27, 28, 29, 30, 31, 32, 33, 34
Protection measures during outbreaks
Measures to protect surgical personnel during outbreaks were reported in 45 studies (see Table 4 ; detailed overview provided in Supplementary Table 1). For the purpose of analysis, protection measures were classified into one of the following categories: PPE (any form of physical protection used by HCW); PRE-OR (any precautions taken preoperatively including modified patient screening and disinfection processes); OR SETUP (measures taken during surgical intervention, such as the use of negative-pressure or segregated ORs); and LOGISTICS (all other measures including modification of work areas, modification of procedures, new hospital protocols and processes, and limitation/modification of HCW roles to help limit and prevent nosocomial disease transmission).
Table 4.
Summary of protective measures.
| Author, Year | Virus | Enhanced PPE | Modified screening practices (confirmed negative test prior to surgery, etc.) | Enhanced disinfection and equipment preparation | Negative-pressure OR/procedure rooms; Dedicated ORs for patients presumed/confirmed infected | Modification of workspace (separate patient notes from patient, etc.) | Procedural modification (open tracheostomy, avoidance of diathermy and suction, etc.) | Modified hospital and patient transfer processes (filters applied prior to transfer, no visitor policy, etc.) | Limit HCW, modified staff roles |
|---|---|---|---|---|---|---|---|---|---|
| Angel, 2020 | COVID-19 | ✓ | ✓ | ✓ | |||||
| Barca, 2020 | COVID-19 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Berardi, 2020 | COVID-19 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Bogani, 2020 | COVID-19 | ||||||||
| Bundu, 2014 | Ebola | ✓ | ✓ | ✓ | |||||
| Cai, 2020 | COVID-19 | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Cai, 2020 | COVID-19 | ||||||||
| Chao, 2020 | COVID-19 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Chee, 2004 | SARS | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Chen, 2020 | COVID-19 | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Cheung, 2020 | COVID-19 | – | – | – | – | – | – | – | – |
| Chow 2020 | COVID-19 | ✓ | – | ✓ | – | ✓ | ✓ | – | – |
| Couto, 2020 | COVID-19 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Cruz, 2020 | COVID-19 | ||||||||
| Cui, 2020 | COVID-19 | ✓ | ✓ | ✓ | |||||
| Deng 2020 | COVID-19 | ✓ | ✓ | ✓ | – | ✓ | ✓ | – | ✓ |
| Doglietto, 2020 | COVID-19 | ✓ | |||||||
| Doran, 2020 | COVID-19 | – | – | – | – | – | – | – | – |
| Fregatti, 2020 | COVID-19 | ✓ | ✓ | ✓ | |||||
| Gallego, 2020 | COVID-19 | ✓ | ✓ | ✓ | |||||
| Gao, 2020 | COVID-19 | ✓ | ✓ | ✓ | ✓ | ||||
| Garcia-Portabella, 2020 | COVID-19 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Gou, 2020 | COVID-19 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Hassan 2020 | COVID-19 | ✓ | ✓ | ✓ | ✓ | ✓ | – | ✓ | ✓ |
| He, 2020 | COVID-19 | ✓ | ✓ | ✓ | ✓ | ||||
| Huang, 2020 | COVID-19 | – | – | – | – | – | – | – | – |
| Khalafallah, 2020 | COVID-19 | ✓ | ✓ | ✓ | |||||
| LeBrun, 2020 | COVID-19 | – | – | – | – | – | – | – | – |
| Lei, 2020 | COVID-19 | – | – | – | – | – | – | – | – |
| Leong, 2020 | COVID-19 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Li, 2020 | COVID-19 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Luong-Nguyen, 2020 | COVID-19 | ✓ | ✓ | ||||||
| Madanelo, 2020 | COVID-19 | – | – | – | – | – | – | – | – |
| Maniscalco 2020 | COVID-19 | – | – | – | – | – | – | – | – |
| Maniscalco, 2020 | ✓ | ✓ | |||||||
| Meyer 2020 | COVID-19 | ✓ | – | – | ✓ | – | ✓ | ✓ | ✓ |
| Morrison 2020 | COVID-19 | ✓ | ✓ | ✓ | – | – | – | ✓ | ✓ |
| Nazer, 2007 | MERS | – | – | – | – | – | – | – | – |
| Ng 2020 | COVID-19 | ✓ | ✓ | ✓ | – | ✓ | ✓ | – | ✓ |
| Oh, 2020 | COVID-19 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Paramore 2020 | COVID-19 | ✓ | ✓ | – | – | – | – | ✓ | – |
| Patel, 2020 | COVID-19 | ||||||||
| Peng, 2020 | COVID-19 | – | – | – | – | – | – | – | – |
| Ralli, 2020 | COVID-19 | – | – | – | – | – | – | – | – |
| Rossi, 2020 | COVID-19 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Saban, 2020 | COVID-19 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Schneider, 2020 | COVID-19 | ✓ | ✓ | ✓ | ✓ | ||||
| Shrikhande, 2020 | COVID-19 | ||||||||
| Taha, 2020 | COVID-19 | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Tan, 2020 | COVID-19 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Tankel, 2020 | COVID-19 | ||||||||
| Tien, 2005 | SARS | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Turri-Zanoni, 2020 | COVID-19 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Valdivia, 2020 | COVID-19 | ✓ | ✓ | ✓ | |||||
| Wang, 2020 | COVID-19 | ✓ | ✓ | ||||||
| Wong, 2004 | SARS | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Yang, 2020 | COVID-19 | – | – | – | – | – | – | – | – |
| Yang, 2020 | COVID-19 | ✓ | ✓ | ✓ | |||||
| Zagra 2020 | COVID-19 | – | – | – | – | – | – | – | ✓ |
| Zhang 2020 | COVID-19 | ✓ | – | – | – | – | ✓ | – | ✓ |
| Zhang, 2020 | COVID-19 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
Modified peri-operative logistics were reported in 40 studies describing protection measures. Examples of workspace modifications as described in 20 studies included establishing ultrasound workstations in areas managing infected patients to perform point-of-care lung imaging, having a designated corner in a dialysis unit for the treatment of patients who were suspected/confirmed infected, and designating doctors’ and nurses’ workstations as the “clean” area of a ward while other areas were considered contaminated.21 , 30 , 35 Procedural and management modification for the purpose of minimizing exposure risk was reported in 25 studies and included measures such as slowing the speed of drilling intra-operatively in neurosurgical procedures, favoring use of percutaneous drainage over ERCP where possible for biliary drainage, and temporarily turning off mechanical ventilation during tracheal incision.35, 36, 37 Modified hospital rules, protocols and patient transfer processes were described in 26 studies and included limiting or preventing visitations for patients, transferring patients between the ward and OR in a negative-pressure isolation transfer cabin, and use of designated transfer “lanes” between sections of the hospital to limit nosocomial spread.23 , 29 , 35 Fourteen studies described modifying the roles of HCW during epidemics, including formation of an “Emergency Incident Command Team” to identify and separate infected patients from other patients, allowing only essential personnel to be present during procedures, and assigning staff to conduct patient screening full-time.30 , 38 , 39
PPE use was the next most frequently reported measure and was implemented in 36 studies describing protection measures. Common PPE items included hair covers, N95 or PAPR masks, surgical masks, face shields, goggles, waterproof gowns, two layers of gloves, and shoe covers. More rigorous measures included use of the Stryker T4 Personal Protection system consisting of standard PPE with the addition of a helmet, short hood, and toga-style gown; use of hoods with built-in HEPA units; and powered air-purifying respirators for anesthesiologists. One study reported that PPE was changed every 3–4 h.40 Another study reported use of surgical masks for patients before and after operation.41 Of note, no HCW infections were described among studies implementing PPE measures.
Measures taken preoperatively for infection control were also described in 36 studies describing protection measures. The majority of these measures focused around improving screening to identify infected patients and HCW prior to operation and implementing rigorous disinfection and equipment preparation processes. Examples of preoperative measures included setting up multi-level triage systems in clinics and prior to patient admission to hospital to identify patients with fevers or concerning epidemiological history, having HCW take their temperature 4 times a day and undergo nucleic acid viral testing multiple times a week, use of disposable anesthetic devices for respiratory procedures, and enhanced decontamination procedures using chlorine disinfectant and anesthesia circuit sterilizer for anesthesia workstations.23 , 28 , 38 , 40
Modification of OR setup to reduce infectious exposure risk was noted in 17 studies describing protection measures. The most common modifications included use of a negative-pressure OR for patients suspected or confirmed to be infected, as reported in 10 of these studies. Other measures included geographically segregating OR complexes to reduce cross-infection, reducing humidity level and temperature of ORs to reduce HCW perspiration, and using plastic drapes around the tracheostomy operative field to create a closed sterile environment.40 , 42 , 43
A summary of protection measures is provided in Table 4. All studies which implemented more than 3 of the listed measures and also reported on HCW outcomes had an infection rate of 0% among HCW.
Patient exposures and HCW outcomes
At the time of operation during epidemics, a total of 381 patients were reported to have confirmed infection (369/381 COVID-19, 6/381 SARS, 6/381 MERS) and 85 patients were presumed to be infected (85/85 COVID-19) (Table 5 ). Following operation, 192 patients (192/192 COVID-19) were confirmed to be infected, while 557 patients (557/557 COVID-19) tested negative for infection. No HCW contracted the illness in studies reporting on HCW outcomes with patients presumed infected during operation. Among studies where patients were confirmed infected after operation and HCW outcomes were also reported, 50.0% (4/8) noted infections in HCW.
Table 5.
Patient exposures and healthcare worker outcomes.
| Author, year | Surgical service | Virus | Timepoint | N (%) patients confirmed infected at time of procedure | N (%) of patients presumed infected at time of procedure | N (%) of patients confirmed infected after procedure | N (%) of patients confirmed not infected after procedure | N (%) HCW healthy after procedure | Outcomes of HCW |
|---|---|---|---|---|---|---|---|---|---|
| Angel, 2020 | ICU | COVID-19 | Mar to Apr 2020 | 100% (98/98) | – | – | – | 8 (100%) | All were healthy |
| Barca, 2020 | Maxillofacial surgery | COVID-19 | Feb to Apr 2020 | 0/33 (100%) | – | – | – | – | – |
| Berardi, 2020 | Surgical oncology, transplant surgery | COVID-19 | Mar 9 2020 to Apr 24 2020 | – | – | – | – | – | – |
| Bogani, 2020 | Gynecologic oncology | COVID-19 | Feb to Mar 2020 | 0/5 (0%) | 5/5 (100%) | ||||
| Bundu, 2014 | All | Ebola | Jun 2013 to Feb 2015 | – | 6 (75%) | 2/8 surgeons died after contracting infection | |||
| Cai, 2020 | Head and Neck | COVID-19 | February 1 to March 10, 2020 | 0% | 0% | 0% | 1 | 100% | No fever symptoms |
| Cai, 2020 | Thoracic | COVID-19 | Jan-20 | – | – | 7/139 (5.0%) | – | – | 8 HCW contracted COVID-19 |
| Chao, 2020 | ICU | COVID-19 | 53/53 (100%) | 100% | No cases COVID-19 among HCW | ||||
| Chee, 2004 | All | SARS | Feb to Apr 2003 | – | 124 (100%) | All were healthy | |||
| Chen, 2020 | Obstetrics | COVID-19 | Jan to Feb 2020 | 17/17 (100%) | – | – | – | 48/48 (100%) | All were healthy |
| Cheung, 2020 | Orthopedics | COVID-19 | March 1 to May 22 2020 | 7/10 (70%) | – | 3/10 (30%) | 0/10 (0%) | – | – |
| Chow 2020 | ENT | COVID-19 | April 1, 2020 and April 17, 2020. | – | 0 (0%) | – | – | – | – |
| Couto, 2020 | Various | COVID-19 | Mar to Apr 2020 | 0/300 (0%) | 0/300 (0%) | 0/300 (0%) | 300/300 (100%) | 100% | None tested positive for COVID-19 |
| Cruz, 2020 | ICU | COVID-19 | Apr-20 | 11/14 (78.6%) | |||||
| Cui, 2020 | ENT | COVID-19 | Jan to Mar 2020 | 6/6 (100%) | – | – | – | NR (100%) | All were healthy |
| Deng 2020 | ENT | COVID-19 | Feb to March 2020 | 4 (100%) | – | 4 (100%) | – | 15 (100%) | – |
| Doglietto, 2020 | Various | COVID-19 | Feb to Apr 2020 | 33/41 (80.5%) | 8/41 (19.5%) | ||||
| Doran, 2020 | HPB and Liver Transplant | COVID-19 | Mar-20 | 0 (0%) | 1 (33%) | 3 (100%) | 0 (0%) | – | – |
| Fregatti, 2020 | Surgical oncology | COVID-19 | Mar 9 to Apr 9 2020 | 0/85 (0%) | – | – | – | – | No HCW developed COVID-19 |
| Gallego, 2020 | General Surgery | COVID-19 | Mar-20 | 6/189 (3.2%) | – | 7/189 (3.7%) | – | 37/49 (75.5%) | 12 HCW total diagnosed with COVID-19 |
| Gao, 2020 | General surgery | COVID-19 | Jan to Mar 2020 | 0 (0%) | 4 (100%) | – | 4 (100%) | – | – |
| Garcia-Portabella, 2020 | Orthopedic Surgery | COVID-19 | Mar to Apr 2020 | 1/11 (9.1%) | 0/10 (0%) | 100% | No cases of COVID-19 among HCW | ||
| Gou, 2020 | Pancreatic | COVID-19 | Feb-20 | 0/8 (0%) | – | – | |||
| Hassan 2020 | Neurosurgery | COVID-19 | March 23 2020–April 20 2020 | – | – | – | – | – | – |
| He, 2020 | Anesthesiology/vascular surgery | COVID-19 | – | 2/4 (50%) | 2/4 (50%) | – | – | – | – |
| Huang, 2020 | Thorascopic lung surgery | COVID-19 | Jan 1 2020 to March 31 2020 | – | – | 3 (100%) | – | – | – |
| Khalafallah, 2020 | Neurosurgery | COVID-19 | Mar 18 to Apr 17 2020 | – | – | – | – | – | 2/51 (3.9%) HCW tested positive for COVID-19. HCW have recovered and returned to work. |
| LeBrun, 2020 | Orthopedics | COVID-19 | Mar 20 to Apr 24 2020 | 7/59 (11.8%) | 1/59 (1.7%) | 2/59 (3.4%) | 40/59 (68%) | – | – |
| Lei, 2020 | All | COVID-19 | Jan to Feb 2020 | – | 34/34 (100%) | 34/34 (100%) | – | – | – |
| Leong, 2020 | Neurosurgery | COVID-19 | Feb to Apr 2020 | 100% | No cases COVID-19 among HCW | ||||
| Li 2020 | Transplant | COVID-19 | January 20 to March 1, 2020 | 0 (0%) | 0 (0%) | 0 (0%) | 51 (100%) | – | – |
| Luong-Nguyen, 2020 | General Surgery | COVID-19 | Mar to Apr 2020 | – | – | 15 (4.9%) | – | – | 7 HCW contracted COVID-19 |
| Madanelo, 2020 | Urology | COVID-19 | Mar to Apr 2020 | – | – | – | – | – | – |
| Maniscalco 2020 | Orthopedics | COVID-19 | Feb 22 2020–Apr 18 2020 | 32/121 (26.4%) | – | – | – | – | – |
| Maniscalco, 2020 | Orthopedics and Traumatology | COVID-19 | Feb to Mar 2020 | – | – | – | – | 12/21 (57.1%) | Of the 21 orthopedics and traumatology team members, 6 were COVID+, treated at home with hydroxychloroquine and antiviral therapy and recovered. 1 developed ARDS and was in ICU at time of writing. 2 also tested positive and were quarantined at time of writing. 37.5% of nursing staff also tested positive, though they were not specific to traumatology team. One nurse had died from the illness. Notably, there was a delay in PPE availability. |
| Meyer 2020 | Spine | COVID-19 | March 17 2020–April 17 2020 | 1/62 (1.6%) | – | 2/62 (3.2%) | – | 100% | – |
| Morrison 2020 | ENT | COVID-19 | March 18 – April 21–2020 | – | – | – | – | – | No confirmed COVID-19 cases |
| Nazer, 2007 | Cardiac | MERS | Jan to Feb 2015 | 6 (100%) | – | – | |||
| Ng 2020 | Vascular | COVID-19 | Feb–March 2020 | – | – | – | – | – | – |
| Oh, 2020 | Obstetrics | COVID-19 | Feb 26 to Apr 3 2020 | 1/8 (12.5%) | 7/8 (87.5%) | – | 8/8 (100%) | – | – |
| Paramore 2020 | Urology | COVID-19 | Mar 23 2020–Apr 9 2020 | 0 (0%) | – | 0 (0%) | – | 100% | – |
| Patel, 2020 | General surgery | COVID-19 | Mar to Apr 2020 | ||||||
| Peng, 2020 | Thoracic | COVID-19 | Jan-20 | – | – | 11/11 (100%) | – | – | – |
| Ralli, 2020 | Otolaryngology | COVID-19 | Mar to Apr 2020 | – | 0/96 (100%) didn’t mention this explicitly but patients were all screened | – | – | – | – |
| Rossi, 2020 | Orthopedic Oncology | COVID-19 | Dec 2019 to Apr 2020 | 0/79 (0%) | 0/79 (0%) | 100% | No cases COVID-19 among HCW | ||
| Saban, 2020 | Ophthalmology | COVID-19 | 0/142 (0%) | 142/142 (100%) | 11/11 (100%) | 11 personnel had COVID-19 contacts. All quarantined for 14 days though none tested positive for COVID-19. | |||
| Schneider, 2020 | Orthopedic Surgery | COVID-19 | 66/66 (100)% | Fourteen HCW (21%) reported clinical symptoms compatible with a SARS-CoV-2 infection, though all tested negative. Due to testing limitations, asymptomatic HCW were not routinely tested. | |||||
| Shrikhande, 2020 | Various | COVID-19 | Mar to Apr 2020 | 0/494 (0%) | 0/494 (0%) | 6/494 (1.21%) | |||
| Taha, 2020 | Otolaryngology | COVID-19 | Mar to Apr 2020 | 26/152 (17.1%) | 35/152 (23%) | – | 11/152 (7.2%) | NR (100%) | All were healthy |
| Tan, 2020 | Neurosurgery | COVID-19 | – | – | – | – | – | 100% | No infections among doctors and nurses |
| Tankel, 2020 | General surgery | COVID-19 | Feb to Apr 2020 | ||||||
| Tien, 2005 | ICU; Emergency OR | SARS | May-13 | 3 (100%) | 4 (100%) | All were healthy | |||
| Turri-Zanoni, 2020 | Otolaryngology | COVID-19 | Feb to Apr 2020 | 32/32 (100%) | – | – | – | NR (100%) | All were healthy |
| Valdivia, 2020 | Vascular surgery | COVID-19 | Mar 14 to May 14 2020 | – | – | – | – | – | Notably, there was considerable lack of testing capability in initial stages of pandemic. |
| Wang, 2020 | Neurosurgery | COVID-19 | – | 5/5 (100%) | – | – | – | – | – |
| Wong, 2004 | Obstetrics | SARS | Apr-03 | 3 (100%) | 100% | All were healthy | |||
| Yang, 2020 | Gynecologic oncology | COVID-19 | Jan to Feb 2020 | – | – | 3/189 (1.59%) | – | – | – |
| Yang, 2020 | Neurosurgery | COVID-19 | Jan 23 to Mar 7 2020 | 0/21 (0%) | 1/21 (4.8%) | – | – | – | – |
| Zagra 2020 | Orthopedics | COVID-19 | February 24 – April 10 2020 | – | – | 79/664 (11.9%) | – | – | – |
| Zhang 2020 | ENT | COVID-19 | Jan 23 2020–April 6 2020 | 11 (100%) | – | – | – | 100% | No confirmed infections |
| Zhang, 2020 | Obstetrics | COVID-19 | Jan to Feb 2020 | 16 (26.2%) | – | – | – | – | – |
Health care workers, HCW; Intensive Care Unit, ICU; Coronavirus disease 2019, COVID-19; Severe acute respiratory syndrome-related coronavirus, SARS; Middle East respiratory syndrome-related coronavirus, MERS; Ear Nose and Throat, ENT; Hepato-pancreato-biliary, HPB; Acute respiratory distress syndrome, ARDS.
HCW outcomes were reported in 31 studies with 11 studies reporting the number of HCW included in the study. A total of 405 HCW were represented in these 11 studies, with 6.2% (25/405) having been infected during epidemics. During the COVID-19 pandemic, 8.6% (23/269) of HCW were infected. The other two infections among HCW occurred during the Ebola epidemics, where 25% (2/8) contracted the illness. Both of these HCW had died from the illness and were the only instances of death reported among the 405 HCW included in this review. One study did report the death of a nurse in its traumatology department during COVID-19, though the total number of HCW in the department was not specified and this instance was not captured in the pooled analysis.21 No infections or adverse outcomes were reported for HCW during the SARS epidemics (0/128) from the included studies.
The rate of HCW infection based on the number of surgeries performed was 3.61% (41 HCW/1136 surgeries) among studies that reported both the number of HCW infected, and the number of surgeries conducted. One HCW was infected for every 27.7 operations performed. Among studies during the COVID-19 pandemic, the HCW infection rate was 3.92% (39 HCW/995 surgeries) and one HCW was infected for every 25.5 operations performed.
Risk of bias assessment
The methodological index for non-randomized studies (MINORS) was used to assess risk of bias in the included studies (Supplementary Table 2). 56 studies included in this review were non-comparative with a mean global score of 10.2 (SD 1.7), indicating fair methodological quality.16 All 56 studies had a clearly stated aim and a loss to follow-up of less than 5% (56/56). The majority of the studies adequately included consecutive patients (45/56), had adequate endpoints in relation to the stated aims (42/56), and had an appropriate follow-up period (44/56). One study adequately conducted a prospective calculation of study size (1/56). The remaining 5 studies included in this study were comparative studies with a mean global score of 14 (SD 2.9). Two of these studies had adequate control groups, 2 had adequate baseline equivalence of groups, and 3 had adequate statistic calculations. Prospective collection of data was reported in 7 studies (7/61). Adequately unbiased assessments of study endpoints were found in 7 studies (7/61).
Discussion
This rapid, living systematic review investigated the impact of hospital lockdown secondary to epidemics on surgical practice. We included 61 studies relevant to the Ebola, SARS, COVID-19, and MERS outbreaks. Lockdown measures, including cancellation of elective surgeries, surgical outpatient clinics, telehealth services, and hospital-based referrals were noted in approximately half of studies. Measures to protect surgical personnel, including adequate PPE and OR modifications, were reported in 45 studies. 31 studies followed the health of surgical HCWs during the epidemic, with the majority noting no adverse health outcomes with proper safety measures. However, there was minimal research on how epidemics impacted surgical practice in terms of patient care, healthcare workers, and waitlists. Specifically, there was no information reported regarding the clinical impact of delaying surgical care during lockdowns. In addition, there was insufficient comparative evidence related to institutional transmission control policies. As such, there remain significant evidence gaps for health systems to implement evidence-based surgical care during epidemics.
Overall, our findings contribute to the growing literature on surgical care during the current COVID-19 pandemic.44 The worldwide shortages in PPE as well as the numerous cases of HCW infection have highlighted the importance of infection control, which has been outlined in our review.44 In addition, as the novel coronavirus can be transmitted via aerosol particles, there is particular risk of exposure during certain procedures such as endoscopy. Our review outlines potential strategies that have been used to mitigate risk in previous outbreaks, such as the use of negative pressure ORs for intubation. There is also concern for triaging surgical oncology cases, due to preliminary evidence that COVID-19 is dangerous for patients for cancer.45 , 46 As a result, the American College of Surgeons has released recommendations for both the triage of non-emergent surgical procedures as well as recommendations for management of elective procedures.47 , 48 Many of their guidelines, such as the limitation of non-essential visitors, were similar to the strategies reported in our included studies. The American College of Surgeons especially stresses the importance of PPE, which was highlighted in the included studies that discussed infection control.
However, while the American College of Surgeons recommends the postponement of elective surgeries, this systematic review demonstrates that there is a lack of long-term evidence regarding the potential impact on patient outcomes, particularly patient morbidity and mortality due to cancellations.47 Of note, our review also found that the overall complication rate did not seem to be increased based on the distribution of elective and emergency cases, as any association with elective surgeries is most likely due to the volume of patients rather than the distribution. In addition, while the American College of Surgeons has oncology-specific guidelines regarding deferral of surgeries and guidelines for multidisciplinary care, more pandemic-specific research is required to substantiate recommendations.49 Of the included studies, 8 reported on postoperative outcomes following cancer surgeries. None of these studies examined oncology-related outcomes, such as remission rates or changes to chemotherapy cycles.
In addition, none of the included studies analyzed the motivations of surgeons to continue working during epidemics. During the COVID-19 pandemic, there has been increasing concern regarding HCW absenteeism and willingness to work in hazardous environments, particularly due to shortages in PPE. Previous literature has demonstrated that perceived personal safety was a large factor in whether HCW continue to practice during the previous SARS and influenza outbreaks.50 , 51 As our review outlines several strategies to protect surgical HCW, implementation could be useful in alleviating the anxieties of HCW and encourage frontline practice.
Finally, we did not review the impact of COVID-19 on surgical graduate medical education, which is an emerging area of concern. There is growing evidence that surgical residencies and postgraduate medical education has been significantly impacted by the COVID-19 pandemic.52, 53, 54 Literature has suggested that residents have decreased opportunity to participate in surgical cases. Similarly, one of our included studies noted that operations were more likely to be performed by staff surgeons in comparison to trainees during epidemics. This may be due to university-based safety guidelines, the redirection of trainees to other specialties, as well as reduced surgical volume. Technological options such as virtual curriculums and simulations have been posed in the interim to maintain the education of surgical residents.55
The main limitation of our systematic review is the lack of published research on surgical care during epidemics. Due to the unpredictable and demanding nature of epidemics, it is often difficult for physicians to prioritize research while in the midst of disease outbreaks. This significantly limits the ability to collect prospective information. As such, much of the available literature was limited to case series and smaller scale retrospective reviews. In addition, considerations from previous pandemics may not necessarily translate to relevance for the COVID-19 pandemic or any future epidemics. The included studies have diverse health systems and delivery models, which reduce generalizability of considerations such as infection control and lockdown guidelines. This is especially relevant for low-resourced health systems, which may face additional shortages. Another limitation of our review is that we were unable to stratify our results in terms of lockdown measures taken, given that this information was reported in fewer than half of the included studies. We are therefore unable to comment on the impact of specific lockdown measures on patient and HCW outcomes.
Ultimately, it is often difficult for institutions to balance providing timely surgical care while ensuring safety during epidemics. While lockdown precautions have been used in previous outbreaks, it is unclear how the reduced access to surgical care will affect patient care in the long-term. In addition, it is unclear how to prioritize surgical care when lockdown precautions are eventually lifted. Future research should analyze the impact of COVID-19 on surgical wait-times and related complications, as well as patient and provider satisfaction. In the meantime, institutions should cooperate with policymakers to determine best precautions for surgical care. Surgical practice during epidemics affects all levels of the hospital, from creating a new demand on PPE to alleviating burden within the emergency department. As such, decisions regarding surgical care during epidemics should not occur in isolation from other medical specialties.
Declaration of competing interest
The authors declare no conflict of interest.
†Age reported either as mean (standard deviation) or median (range).
Coronavirus disease 2019, COVID-19; Middle East respiratory syndrome-related coronavirus, MERS; Severe acute respiratory syndrome-related coronavirus, SARS; Not reported, NR; Interquartile Range, IQR.
Coronavirus disease 2019, COVID-19; Middle East respiratory syndrome-related coronavirus, MERS; Severe acute respiratory syndrome-related coronavirus, SARS; Ear Nose and Throat, ENT; Hepato-pancreato-biliary, HPB; Myocardial Infarction, MI; Urinary tract infection, UTI; Clavien-Dindo Classification, CD; Accreditation Council for Graduate Medical Education, ACGME.
Intensive Care Unit, ICU; Ear Nose and Throat, ENT; Hepato-pancreato-biliary, HPB; Coronavirus disease 2019, COVID-19.
Coronavirus disease 2019, COVID-19; Health care workers, HCW; Middle East respiratory syndrome-related coronavirus, MERS; Severe acute respiratory syndrome-related coronavirus, SARS; ✓, yes; blank, no; -, not reported.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amjsurg.2020.11.019.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Appendix A. Supplementary data
The following are the supplementary data to this article:
References
- 1.Zhu N., Zhang D., Wang W., et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Emanuel E.J., Persad G., Upshur R., et al. Fair allocation of scarce medical resources in the time of covid-19. N Engl J Med. 2020;382(21):2049–2055. doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Shortage of Personal Protective Equipment Endangering Health Workers Worldwide.
- 4.Truog R.D., Mitchell C., Daley G.Q. The toughest triage — allocating ventilators in a pandemic. N Engl J Med. 2020;382(21):1973–1975. doi: 10.1056/NEJMp2005689. [DOI] [PubMed] [Google Scholar]
- 5.Li Q., Guan X., Wu P., et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382(13):1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schwartz J., King C.C., Yen M.Y. Protecting health care workers during the COVID-19 coronavirus outbreak -lessons from Taiwan’s SARS response. Clin Infect Dis. 2020;2019 doi: 10.1093/cid/ciaa255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wilder-Smith A., Chiew C.J., Lee V.J. Can we contain the COVID-19 outbreak with the same measures as for SARS? Lancet Infect Dis. 2020;20(5):e102–e107. doi: 10.1016/S1473-3099(20)30129-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Elston J.W.T., Cartwright C., Ndumbi P., Wright J. The health impact of the 2014–15 Ebola outbreak. Publ Health. 2017;143:60–70. doi: 10.1016/j.puhe.2016.10.020. [DOI] [PubMed] [Google Scholar]
- 9.Zheng M.H., Boni L., Fingerhut A. Minimally invasive surgery and the novel coronavirus outbreak: lessons learned in China and Italy. Ann Surg. 2020;272(1) doi: 10.1097/SLA.0000000000003924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoyt D.B. JHU Press; 2017. Operation Ebola: Surgical Care during the West African Outbreak. [Google Scholar]
- 11.Interim U.S. Guidance for Risk Assessment and Work Restrictions for Healthcare Personnel with Potential Exposure to COVID-19 | CDC.
- 12.Gagliano A., Villani P.G., Cò F.M., et al. ncov’s epidemic in middle province of northern Italy: impact, logistic & strategy in the first line hospital. Disaster Med Public Health Prep. 2019:1. doi: 10.1017/dmp.2020.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moher D., Liberati A., Tetzlaff J., Altman D.G., Prisma Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339 doi: 10.1136/bmj.b2535. b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Clavien P.A., Barkun J., De Oliveira M.L., et al. The clavien-dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–196. doi: 10.1097/SLA.0b013e3181b13ca2. [DOI] [PubMed] [Google Scholar]
- 15.Three Stages of Gme During the Covid-19 Pandemic Accreditation Council for graduate medical education. 2020. https://www.acgme.org/COVID-19/-Archived-Three-Stages-of-GME-During-the-COVID-19-Pandemic
- 16.Slim K., Nini E., Forestier D., Kwiatkowski F., Panis Y., Chipponi J. Methodological index for non-randomized studies (Minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 17.Campbell M., McKenzie J.E., Sowden A., et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ. 2020;368:1–6. doi: 10.1136/bmj.l6890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chou R., Dana T., Buckley D.I., Selph S., Fu R., Totten A.M. Epidemiology of and risk factors for coronavirus infection in health care workers. Ann Intern Med. May 2020 doi: 10.7326/m20-1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Elliott J.H., Synnot A., Turner T., et al. vol. 91. 2017. (Living Systematic Review : 1 . Introduction D the Why , what , when , and How). [DOI] [PubMed] [Google Scholar]
- 20.Haby M.M., Chapman E., Clark R., Barreto J., Reveiz L., Lavis J.N. What are the best methodologies for rapid reviews of the research evidence for evidence-informed decision making in health policy and practice : a rapid review. Health Res Pol Syst. 2016:1–12. doi: 10.1186/s12961-016-0155-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maniscalco P., Poggiali E., Quattrini F., et al. The deep impact of novel covid-19 infection in an Orthopedics and traumatology department: the experience of the Piacenza hospital. Acta Biomed. 2020;91(2):97–105. doi: 10.23750/abm.v91i2.9635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nazer R.I., Case C.I. Outbreak of Middle East respiratory syndrome-coronavirus causes high fatality after cardiac operations. Ann Thorac Surg. 2017;104(2):3–5. doi: 10.1016/j.athoracsur.2017.02.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen R., Zhang Y., Huang L., Cheng B. Safety and efficacy of different anesthetic regimens for parturients with COVID-19 undergoing Cesarean delivery : a case series of 17 patients. Can J Anesth. 2020 doi: 10.1007/s12630-020-01630-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gao Y., Xi H., Chen L. Publish Ah; 2020. Emergency Surgery in Suspected COVID-19 Patients with Acute Abdomen. Ann Surg. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Oh J., Kim E., Kim H., et al. Infection control of operating room and anesthesia for cesarean section during pandemic Coronavirus disease-19 (COVID-19) outbreak in Daegu, the Republic of Korea – 8 cases report. Kor J Anesthesiol. 2020 doi: 10.4097/kja.20204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rossi B., Zoccali C., Baldi J., et al. Reorganization tips from a sarcoma unit at time of the COVID-19 pandemic in Italy: early experience from a regional referral oncologic center. J Clin Med. 2020 doi: 10.3390/jcm9061868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cai Y., Hao Z., Gao Y., et al. Coronavirus disease 2019 in the perioperative period of lung resection: a brief report from a single thoracic surgery department in Wuhan, People’s Republic of China. J Thorac Oncol. 2020;15(6) doi: 10.1016/j.jtho.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cui C., Yao Q., Zhang D., et al. Otolaryngol - Head Neck Surg (United States); 2020. Approaching Otolaryngology Patients during the COVID-19 Pandemic. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Morrison D.R., Gentile C., McCammon S., Buczek E. Head and neck oncologic surgery in the COVID-19 pandemic: our experience in a deep south tertiary care center. Head Neck. 2020;(April):1–6. doi: 10.1002/hed.26262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li Y., Yang N., Li X., Wang J., Yan T. Strategies for prevention and control of the 2019 novel coronavirus disease in the department of kidney transplantation. Transpl Int. 2020:1–6. doi: 10.1111/tri.13634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Paramore L., Yang B., Abdelmotagly Y., et al. Delivering urgent urological surgery during the COVID-19 pandemic in the United Kingdom: outcomes from our initial 52 patients. BJU Int. 2020 doi: 10.1111/bju.15110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Saban O., Levy J., Chowers I. Risk of SARS-CoV-2 transmission to medical staff and patients from an exposure to a COVID-19-positive ophthalmologist. Graefe’s Arch Clin Exp Ophthalmol. 2020 doi: 10.1007/s00417-020-04790-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Khalafallah A.M., Jimenez A.E., Lee R.P., et al. World Neurosurg; 2020. Impact of COVID-19 on an Academic Neurosurgery Department: The Johns Hopkins Experience. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fregatti P., Gipponi M., Giacchino M., et al. 2020. Breast Cancer Surgery during the COVID-19 Pandemic: An Observational Clinical Study of the Breast Surgery Clinic at Ospedale Policlinico San Martino - Genoa, Italy. In Vivo (Brooklyn) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tan Y., Wang J., Zhao K., et al. Preliminary recommendations for surgical practice of neurosurgery department in the central epidemic area of 2019 coronavirus infection. Curr Med Sci. 2020;40(2):281–284. doi: 10.1007/s11596-020-2173-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Turri-Zanoni M., Battaglia P., Czaczkes C., Pelosi P., Castelnuovo P., Cabrini L. Italy. Otolaryngol - Head Neck Surg (United States); 2020. Elective Tracheostomy during Mechanical Ventilation in Patients Affected by COVID-19: Preliminary Case Series from Lombardy; pp. 2–4. [DOI] [PubMed] [Google Scholar]
- 37.Shanmiao G., Tao Y., Jiongxin X., Tao P., Yao L., River W. 2020. Diagnosis and Treatment of Infection and Prevention and Control of Pancreatic Surgery Patients under the New Coronavirus Pneumonia; pp. 1–7. [Google Scholar]
- 38.Cai Y.C., Wang W., Li C., et al. Treating head and neck tumors during the SARS-CoV-2 epidemic, 2019 to 2020: sichuan Cancer Hospital. Head Neck. 2020;42(6):1153–1158. doi: 10.1002/hed.26161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wong S.F., Chow K.M., Shek C.C., et al. Measures to prevent healthcare workers from contracting severe acute respiratory syndrome during high-risk surgical procedures. Eur J Clin Microbiol Infect Dis. 2004;23(2):131–133. doi: 10.1007/s10096-003-1068-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.He H., Zhao S., Han L., et al. Anesthetic management of patients undergoing aortic dissection repair with suspected severe acute respiratory syndrome COVID-19 infection. J Cardiothorac Vasc Anesth. 2020;34(6):1402–1405. doi: 10.1053/j.jvca.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Meyer M., Prost S., Farah K., et al. Spine surgical procedures during coronavirus disease 2019 pandemic: is it still possible to take care of patients? Results of an observational study in the first month of confinement. Asian Spine J. 2020;14(3):336–340. doi: 10.31616/asj.2020.0197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wei V., Chee T., Med M., et al. 2004. Infection Control Measures for Operative Procedures in Severe Acute Respiratory Syndrome – Related Patients; pp. 1394–1398. 6. [DOI] [PubMed] [Google Scholar]
- 43.Ling V., Chow Y., Chung G., et al. 2020. Tracheostomy during COVID-19 Pandemic — Novel Approach; pp. 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Brindle M., Gawande A. Managing COVID-19 in surgical systems. Ann Surg. 2020 doi: 10.1097/SLA.0000000000003923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kutikov A., Weinberg D.S., Edelman M.J., Horwitz E.M., Uzzo R.G., Fisher R.I. A war on two fronts: cancer care in the time of COVID-19. Ann Intern Med. 2020;172(11):756–758. doi: 10.7326/M20-1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Liang W., Guan W., Chen R., et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21(3):335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.American College of Surgeons . 2020. COVID-19: Recommendations for Management of Elective Surgical Procedures. [Google Scholar]
- 48.American College of Surgeons . 2020. COVID-19: Guidance for Triage of Non-emergent Surgical Procedures. [Google Scholar]
- 49.American College of Surgeons . COVID-19) Pandemic; 2020. ACS Guidelines for Triage and Management of Elective Cancer Surgery Cases during the Acute and Recovery Phases of Coronavirus Disease 2019. [Google Scholar]
- 50.Irvin C.B., Cindrich L., Patterson W., Southall A. 2008. Survey of Hospital Healthcare Personnel. 23(4) [DOI] [PubMed] [Google Scholar]
- 51.Tam C.W.C., Pang E.P.F., Lam L.C.W., Chiu H.F.K. Severe acute respiratory syndrome (SARS) in Hong Kong in 2003: stress and psychological impact among frontline healthcare workers. Psychol Med. 2004;34(7):1197–1204. doi: 10.1017/S0033291704002247. [DOI] [PubMed] [Google Scholar]
- 52.Vargo E., Ali M., Henry F., et al. Cleveland clinic akron general urology residency program’s COVID-19 experience. Urology. 2020;140:1–3. doi: 10.1016/j.urology.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Potts J.R. Residency and fellowship program accreditation: effects of the novel coronavirus (COVID-19) pandemic. J Am Coll Surg. 2020;230(6):1094–1097. doi: 10.1016/j.jamcollsurg.2020.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nassar A.H., Zern N.K., Mcintyre L.K., et al. Emergency restructuring of a general surgery residency program during the coronavirus disease 2019 pandemic: the university of Washington experience. JAMA Surg. 2020:1–4. doi: 10.1001/jamasurg.2020.1219. [DOI] [PubMed] [Google Scholar]
- 55.Chick R.C., Clifton G.T., Peace K.M., et al. Using technology to maintain the education of residents during the COVID-19 pandemic. J Surg Educ. 2020;77(4):729–732. doi: 10.1016/j.jsurg.2020.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.