A 39-year-old male with no known comorbidities presented with sudden onset right-sided weakness. On examination, blood pressure was 128/79 mmHg, National Institutes of Health Stroke Scale score was 4 and there were no signs of heart failure. Emergent computerized tomography demonstrated an ischemic infarct of the left middle cerebral artery distribution and brain magnetic resonance imaging later confirmed it (Figure 1). There was no evidence of dysrhythmias on telemetry. Transthoracic echocardiogram revealed prominent trabeculation of the left ventricle (LV) with an ejection fraction (EF) of 25%-30% (Figure 2). There was severe apical hypokinesis with extensive swirling of contrast in the LV apex. Cardiac magnetic resonance imaging (CMR) delineated a ratio of non-compacted to compacted myocardium of 2.5:1 (Figure 3). He was managed with oral anticoagulation for secondary stroke prevention and guideline directed medical therapy for heart failure.
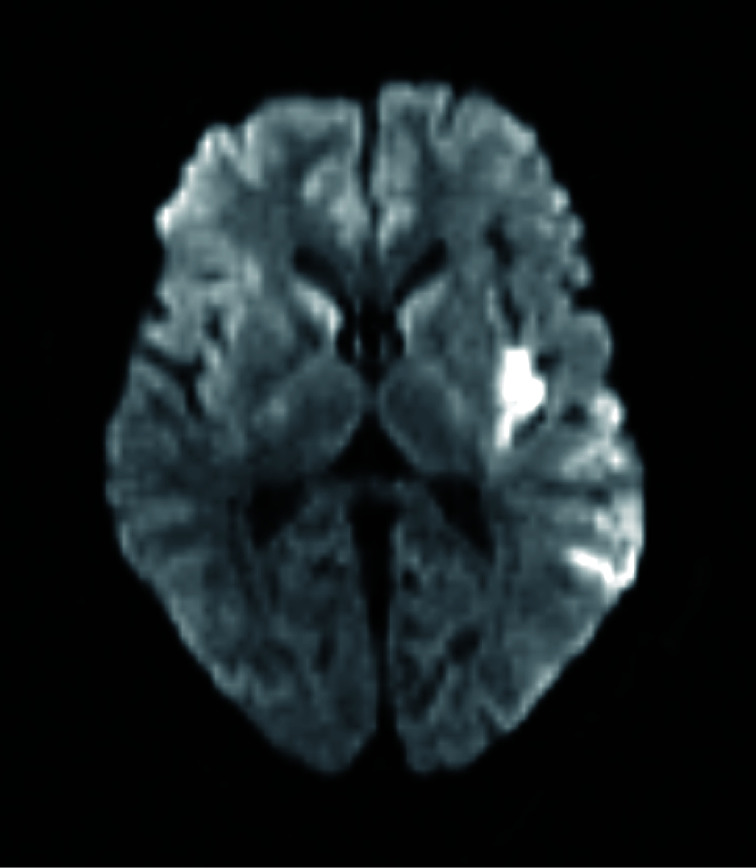
Figure 1.
Magnetic resonance imaging brain w/o contrast-showing acute infarcts in the left middle cerebral artery territory and lateral superior temporal cortex, suggestive of underlying embolic process.
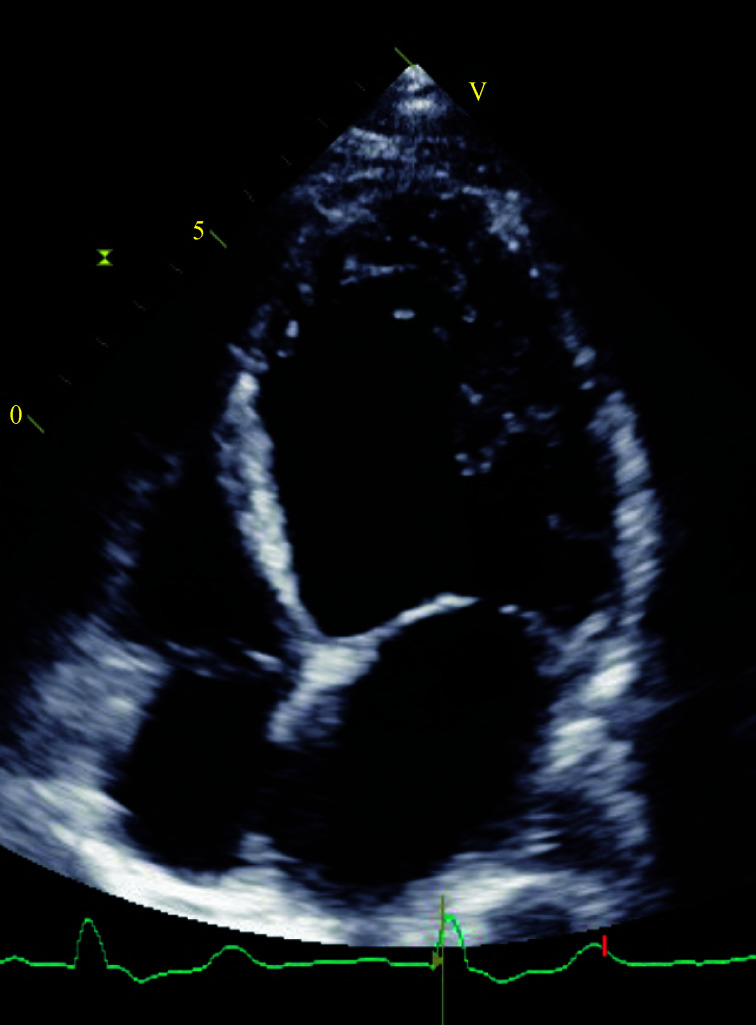
Figure 2.
Two-dimensional echocardiogram showing increased apical left ventricular trabeculation in a four chamber view.
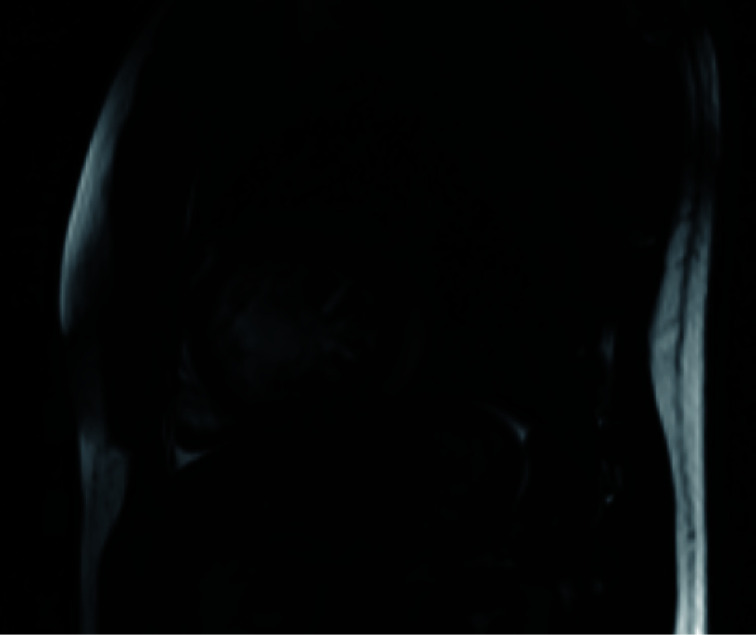
Figure 3.
Cardiac magnetic resonance imaging showing increased trabeculation within the left ventricular apex with increased ratio of non-compacted to compacted myocardium.
Expert opinions on diagnosis of left ventricular non-compaction (LVNC) include echocardiographic or CMR findings of segmental LV myocardial thickening consisting of two layers: a thin, compacted epicardium and a thickened endocardium with prominent trabeculations and deep recesses. Objective features involve ratios between non-compacted and compacted myocardium, usually greater than 2:1.[1]
The leading hypothesis on etiology implicates an embryogenic arrest of myocardial compaction. There are expanding data on culprit genetic mutations.[1] Yet, there have been increasing reports of acquired and reversible LVNC cases, such as in young athletes, which unfold into a benign clinical course.[2]
Whilst some patients exhibit no sign of left ventricular dysfunction, others develop severe systolic and/or diastolic heart failure, arrhythmias and thromboembolic events. A case series of 34 adults with LVNC discovered 24% of patients developing thromboembolic sequela, independent of LV size or function.[3]
Some experts recommend routine anticoagulation for primary thromboembolic prevention in all patients with LVNC whilst others suggest anticoagulation in patients with additional risk factors such as systolic dysfunction (EF < 40%), atrial fibrillation or visible intracardiac.[3, 4] Secondary prevention has not been studied specifically but by categorical extrapolation of guidelines on cardio-embolic stroke, may also warrant anticoagulation. Furthermore, given the possibility of reversibility, surveillance echocardiography may be reasonable to influence the duration of anticoagulation. Lastly, a better understanding of the genetic etiology of LVNC may have significance in screening of relatives, an area yet to be explored.
Our case emphasizes the need for consensus guidelines. Establishing unanimous diagnostic criteria may be the coveted first step to obtaining high quality data on the epidemiology and clinical significance of this entity.
References
- 1.Arbustini E, Favalli V, Narula N, et al. Left ventricular noncompaction: a distinct genetic cardiomyopathy?, , 68: 949-966. J Am Coll Cardiol. 2016;68:949–966. doi: 10.1016/j.jacc.2016.05.096. [DOI] [PubMed] [Google Scholar]
- 2.Gati S, Chandra N, Bennett RL, et al. Increased left ventricular trabeculation in highly trained athletes: do we need more stringent criteria for the diagnosis of left ventricular non-compaction in athletes? Heart. 2013;99:401–408. doi: 10.1136/heartjnl-2012-303418. [DOI] [PubMed] [Google Scholar]
- 3.Oechslin EN, Attenhofer Jost CH, Rojas JR, et al. Long-term follow-up of 34 adults with isolated left ventricular noncompaction: a distinct cardiomyopathy with poor prognosis. J Am Coll Cardiol. 2000;36:493–500. doi: 10.1016/S0735-1097(00)00755-5. doi: 10.1016/S0735-1097(00)00755-5. [DOI] [PubMed] [Google Scholar]
- 4.Kido K, Guglin M. Anticoagulation therapy in specific cardiomyopathies: isolated left ventricular noncompaction and peripartum cardiomyopathy: isolated left ventricular noncompaction and peripartum cardiomyopathy. J Cardiovasc Pharmacol Ther. 2019;24:31–36. doi: 10.1177/1074248418783745. [DOI] [PubMed] [Google Scholar]