Abstract
Compared with mortality, the impact of weather and climate on human morbidity is less well understood, especially in the cold season. We examined the relationships between weather and emergency department (ED) visitation at hospitals in Roanoke and Charlottesville, Virginia, two locations with similar climates and population demographic profiles. Using patient-level data obtained from electronic medical records, each patient who visited the ED was linked to that day’s weather from one of 8 weather stations in the region based on each patient’s ZIP code of residence. The resulting 2010–2017 daily ED visit time series were examined using a distributed lag non-linear model to account for the concurrent and lagged effects of weather. Total ED visits were modeled separately for each location along with subsets based on gender, race, and age.
The relationship between the relative risk of ED visitation and temperature or apparent temperature over lags of one week was positive and approximately linear at both locations. The relative risk increased about 5% on warm, humid days in both cities (lag 0 or lag 1). Cold conditions had a protective effect, with up to a 15% decline on cold days, but ED visits increased by 4% from 2–5 days after the cold event. The effect of thermal extremes tended to be larger for non-whites and the elderly, and there was some evidence of a greater lagged response for non-whites in Roanoke. Females in Roanoke were more impacted by winter cold conditions than males, who were more likely to show a lagged response at high temperatures. In Charlottesville, males sought ED attention at lower temperatures than did females.
The similarities in the ED response patterns between these two hospitals suggest that certain aspects of the response may be generalizable to other locations that have similar climates and demographic profiles.
Keywords: weather, emergency department, distributed lag non-linear model, Virginia
Introduction
Unusually high and low temperatures present environmental stresses to individuals who are not acclimated to seasonal weather changes or extremes, resulting in physiological strain that can be manifested as morbidity or mortality (e.g., Anderson and Bell, 2009; Barnett et al., 2012; Kalkstein and Davis, 1989; Ye et al., 2012). One example of a morbidity impact from weather is an increase in emergency department (ED) visits. Whereas mortality has understandably been the emphasis of most prior research, there is a growing interest in determining how less severe but nonetheless important health consequences, such as ED visits and hospitalizations, are related to weather and climate (Basu et al. 2012; Chen et al., 2017; Davis and Novicoff, 2018; Fletcher et al., 2012; Fuhrmann et al. 2016; Li et al., 2015; Sherbakov et al., 2018; Tian et al., 2016; Wang and Lin, 2014; Winquist et al., 2016).
Overall ED visits have been shown to increase in association with unusually hot and/or humid days in the warm season in many mid-latitude locations (Bishop-Williams et al., 2015; Chen et al., 2017; Gronlund et al., 2014; Li et al., 2015; Winquist et al., 2016; Xu et al., 2013; Ye et al., 2012). Specific stratification by heat stress codes (syncope, heat exhaustion, heat stroke) are less useful than overall visit counts, because heat-related comorbidities tend to be under-reported, thereby masking the overall net impact of heat exposure on health (Greenberg et al., 1983; Kalkstein and Davis, 1989; Kilbourne 1997; Luber and McGeehin, 2008). As is the case with mortality, time lags for heat-related ED visits tend to be short, with higher visitation occurring on the day of or one day after the heat event (Davis et al., 2020; Green et al., 2010; Ye et al., 2012).
Considerably less research has been conducted on cold-season morbidity. In the cold season, ED visits or hospitalizations tend to increase in conjunction with cold days and/or cold waves (Bunker et al., 2016; Conlon et al. 2011, Monterio et al., 2013; Son and Bell, 2014; Song et al., 2017; Wang and Lin, 2014; Ye et al., 2012), although the lags between the putative weather event and subsequent health impact tend to be longer and the peaks less pronounced than in summer (McGeehin and Mirabelli, 2001; Nastos and Matzarakis, 2006; Tian et al., 2016; Wang and Lin, 2014; Ye et al., 2012).
In this research, we analyze the potential influence of weather on ED visits in two mid-sized cities in Virginia that have similar climates and comparable population demographic profiles. By comparing the variability of ED responses between these two locations, we hope to shed light on the extent to which natural variability in the response variable might impact researchers’ ability to generalize the results of climate-morbidity studies.
Materials and Methods
Study Setting and Data
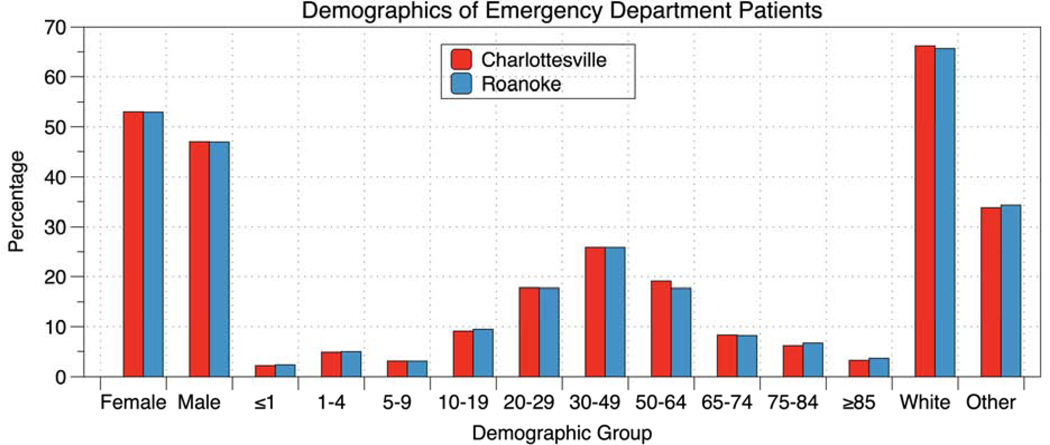
Both Charlottesville and Roanoke, Virginia are mid-sized university towns that are affiliated with a major medical center. Located in Charlottesville, UVA Health includes a hospital, level I trauma center, nationally recognized cancer and heart centers, and primary and specialty clinics throughout Central Virginia with 612 beds, more than 300 practice sites, and over 900 full-time faculty. Each year, this facility has nearly 923,000 outpatient visits, 29,000 inpatient admissions, and approximately 65,000 ED visits. As a quaternary care center, UVA Health serves a large geographic region, including large population from outside the Commonwealth of Virginia. The Carilion Clinic in Roanoke is comprised of seven hospitals, including a children’s hospital, with 1026 beds, 226 practice sites, and over 730 physicians with more than 972,000 primary care visits, 52,700 admissions, and 172,000 ED visits annually. The Roanoke Metropolitan Statistical Area had a 2010 population of almost 310,000 people, making it the largest metropolitan region in southwestern Virginia. The Carilion Clinic serves approximately 1 million patients throughout an extended footprint of 20 counties in central and southwestern Virginia and southern West Virginia. A comparison of the age/race/ethnicity profiles of patients who utilized the EDs in the two cities shows that the demographics are quite similar (Fig. 1). UVA Health has slightly more ED visits for people age 50–64 and relatively fewer patients aged 75 or older.
Figure 1.
Comparison of the demographics of ED patients at UVa Health (Charlottesville) and the Carilion Clinic (Roanoke) from 2010–2017.
With respect to the health burden in the two locations, the health region that includes Charlottesville has 285 cardiovascular deaths per 100,000 population. Over 29% of the population is obese, 8% has diabetes, 22% are smokers and 12% are uninsured. In Roanoke, the data are compiled separately for the city proper and the surrounding Alleghany Health District. For the city of Roanoke, 18% smoke, 13% are uninsured, both lower than in Charlottesville, but cardiovascular deaths are twice as high (546 per 100,000), and diabetes (10%) and obesity (35%) are more prevalent. However, the surrounding region has a similar profile to Charlottesville (30% obese, 9% diabetic, 18% smokers, 8% uninsured), yet cardiovascular mortality is much higher, at 390 deaths per 100,000.
Weather Data
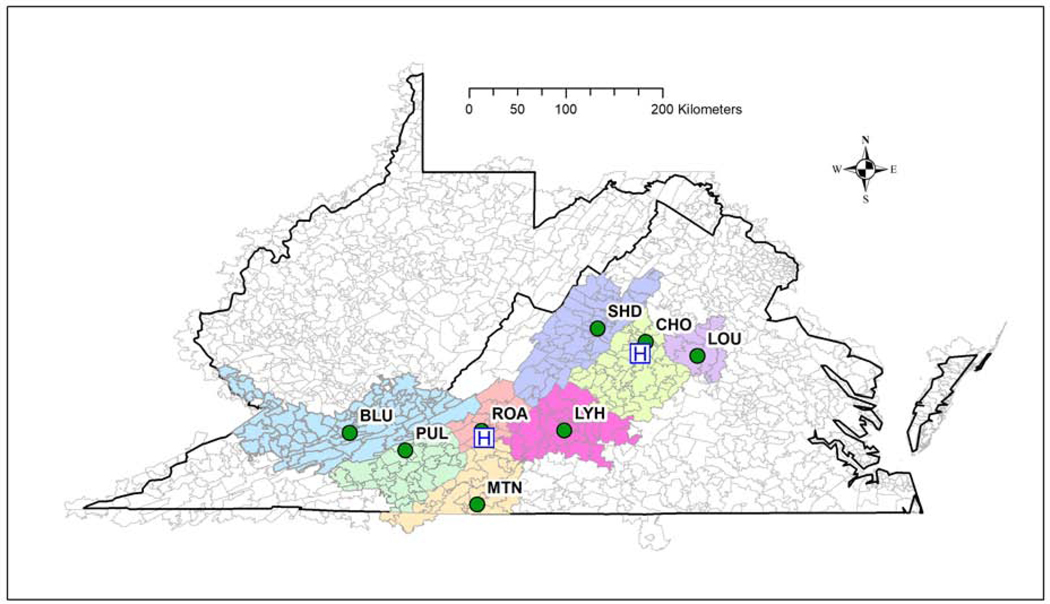
Weather data were downloaded from U.S. National Weather Service (NWS) archived measurements taken at weather stations throughout central and southwestern Virginia. Weather data from the Roanoke (station code ROA) and the Charlottesville-Albemarle County (station code CHO) airports account for the primary weather data sources, but data are also utilized from six additional surrounding stations (see Fig. 2). All are first-order weather stations that make routine measurements at hourly or finer resolution of a variety of weather variables, including air temperature, humidity, wind, atmospheric pressure, cloud cover, and precipitation. Based on the zip code of residence provided by each ED patient, we identified a list of zip code tabulation areas (ZCTAs) in the vicinity of each weather station (Fig. 2).
Figure 2.
Zip code tabulation areas of residents included in the study and associated with the following weather stations: Charlottesville-Albemarle County Airport (CHO); Roanoke-Blacksburg Regional Airport (ROA); Shenandoah Valley Regional Airport (SHD; Louisa County Airport (LOU); Lynchburg Regional Airport (LYH); Martinsville (Blue Ridge Airport) (MTN); Pulaski County Airport (PUL); and Mercer County Airport near Bluefield, WV (BLU). Weather data were recorded at the respective airports (green dots) and the hospital locations are indicated by an “H.”
Weather data are automatically collected and archived using standard instrumentation as established by the NWS. The Automated Surface Observing System (ASOS) is the standard data collection platform and protocol for providing essential operational weather observations for the Federal Aviation Administration and the Department of Defense. The ASOS data-processing procedures include routine quality control checks. Data were retrieved at the observation time closest to 1 a.m., 7 a.m., 1 p.m., and 7 p.m. local standard time, along with each day’s maximum and minimum temperature. If data for these times were missing, we substituted the closest time that was within 90 minutes of the target time. If only a single variable was still missing, it was replaced via linear interpolation using data from the adjacent times; otherwise, the observation was coded as missing with no substitution. The weather variables used in this study, either directly or to calculate other parameters, included air temperature, relative humidity, sea-level pressure, and dew point temperature. (The daily temperature time series for CHO and ROA is including in the Supplemental Figures.)
Apparent temperature (AT) was calculated from the raw data. AT is a combination of air temperature and humidity that serves as the basis of the “Heat Index” used to estimate the added stress placed on the body during hot conditions based on the efficiency of evaporative cooling (Steadman, 1979). AT is only applicable above 21.1°C (70.0°F)—AT equals air temperature below this value. We calculated AT using the algorithm developed by the NWS (Anderson et al., 2013).
To account for the weather conditions experienced by each ED patient, the weather on the day of the visit was linked to each patient based on their ZCTA of residence, as shown in Fig. 2. The weather variable used to characterize each day is the weighted average of the values of the weather stations associated with each ZCTA based on that day’s distribution of ED visitors. For example, assume 100 patients visited UVA Health on January 1, 2010 and they included 85 patients from the CHO region, 10 from LOU and 5 from SHD. The 1 p.m. air temperature (for example) would reflect this 85/10/5 split by weighting the observed temperatures from each of the three weather stations. This procedure was repeated for all meteorological variables.
To consider possible influences of longer-duration events on ED visits, heat and cold waves were defined. Heat waves were classified based on consecutive days of 1 p.m. air temperature exceeding a selected threshold. We tested a variety of thresholds (Table 1) and incorporated the one related to the strongest ED response in the final model. Heat waves must last a minimum of three days and are terminated by two consecutive days that do not exceed the given threshold (Davis and Novicoff, 2018). A similar procedure was used for cold waves (Table 1). The specific thresholds tested were chosen based on the overall air temperature distributions for each station and a sensitivity analysis.
Table 1.
Various temperature thresholds used to define heat and cold waves in Roanoke (ROA) and Charlottesville (CHO) and the percentile of each threshold.
| Station | Low | Medium | High |
|---|---|---|---|
| ROA: Heat | 31.0°C – 81% | 33.0°C – 91% | 36.0°C – 98.3% |
| CHO: Heat | 33.5° – 87% | 35.5°C – 93% | 38.5°C – 98% |
| ROA: Cold | 3.0°C – 20% | 1.0°C – 11% | –2.5°C – 4% |
| CHO: Cold | 3.5°C – 22% | 1.5°C – 12% | 0.0°C – 8% |
Finally, important snow events were identified at ROA and CHO based on at least 5 inches of snow accumulation observed over a 48-hour period. These were included to account for the impact of heavy snow on road travel volume and the likely reduction in ED visits.
Patient Data
Study subjects included all patients who visited any of the EDs that were part of the Carilion health network (for Roanoke) and UVA Health (for Charlottesville) from 2010–2017. To be included, patients must live in the surrounding area based on their ZCTA of residence (Fig. 2). The full dataset was subdivided by age, gender, and race/ethnicity. The latter variable was coded as white/non-white because the small sample sizes for specific non-white groups impacted statistical robustness. The Carilion Institutional Review Board determined that this study posed minimal risk to the subjects and thus did not require individual consent. This work was approved by the UVA Health System’s Institutional Review Board (HSR# 20059).
Data for each patient who utilized the ED facilities were entered routinely into an electronic data warehouse. From this archive, individual patient information was collapsed into a daily time series of frequencies of total ED counts and ED counts for each subcategory, and these data served as the dependent variables in the study. Subcategories for this analysis included elderly (≥65 years), white/non-white, and male/female.
Over the period of record, there were an average of 167±18.8 daily ED visits in Roanoke and 99±13.7 in Charlottesville. The UVA Hospital count is lower because we included only those patients for whom demographic data were also available (the UVA Hospital mean daily visit count is 160). In both locations, mean ED visits are highest on Monday and lowest on Saturday.
Methods
The impact of weather on ED visits was examined separately at each station using a generalized additive model (gam) to relate weather factors to the relative risk (RR) of ED visits. Within the gam framework, smoothing cubic splines were fit to predictor variables to account for variations in the temporal behavior of potential predictors. The smoothed predictors, along with other potential categorical variables, were added in a manner similar to that of multiple linear regression. Specific lagged effects were then addressed with a distributed lag non-linear model (dlnm) (Gasparrini, 2011) that accounts for both simultaneous and delayed relationships between the predictor variables and the response. This approach is commonly used in environmental epidemiology research and has been utilized in studies similar to this one (Guo et al., 2016; Lee et al., 2018).
Potential predictor variables included air temperature (T), dew point temperature (Td), apparent temperature (AT), diurnal temperature range (DTR, daily maximum minus minimum air temperature), heat and cold waves, and snowstorms, as well as a variable to account for ED visit anomalies associated with holidays (Thanksgiving and Christmas), and a day of the week (DOW) variable to address fluctuations related to the weekly cycle in ED visits.
In general, the model assumed the following form:
| (1) |
where “Y” is the daily ED visit count, “t” is time (the time step is daily), “a” is the y-intercept, “l” is lag (in days), “T” is a temperature variable (either air temperature or apparent temperature), “DTR” is diurnal temperature range with “x” degrees of freedom, “S” is a natural cubic spline, “Td” is dew point temperature with “y” degrees of freedom, “trend” is a term that accounts for inter- and intra-annual variations with z degrees of freedom, “DOW” is a nominal variable representing the day of the week, “HeatWave” and “ColdWave” are binary variables used to identify consecutive anomalously warm or cold days (see earlier text for definitions), and “b”–”g” are fitted coefficient vectors. The dependent variable is related to the predictor variables through a quasi-Poisson link function that accounts for overdispersion in the admissions count. We included the DTR variable here in consideration of recent and ongoing research that shows a positive relationship between DTR and morbidity (Cheng et al., 2014; Davis et al., 2020; Lim et al., 2012). The specific variables used in each model varied as a function of dependent variable and location (Table 2) and arose after testing a variety of combinations of models using different potential predictors. We initially examined a larger suite of potential predictors, including pressure and winds, humidex, the temperature-humidity index, a variety of humidity variables, and wind chill. Equation 1 shows only those variables that were included in at least one of the final models.
Table 2.
Variables used in the various generalized additive models for Charlottesville (CHO) and Roanoke (ROA). The variable that served as the cross-basis (cb) in the dlnm is indicated for each model; other values for the temperature variables indicate the number of degrees of freedom used in the spline term (8×10 in the “trend” term is 10 degrees of freedom for each of 8 years). T=1 p.m. temperature; AT=1 p.m. apparent temperature; Td=1 p.m. dew point temperature, DTR=diurnal temperature range; HW= heat wave; CW=cold wave, both using the “medium” thresholds (see Table 1); “Holi”=holidays, “DOW”=day of week; and “Snow”=snow events with precipitation over up to two days of at least 5 inches. The last column shows the adjusted R2 of the gam.
| T | AT | Td | DTR | HW | CW | Holi | DOW | Snow | Trend | Adj. R2 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| CHO | |||||||||||
| Total | cb | x | x | x | 8×10 | 0.275 | |||||
| White | cb | 10 | x | x | x | 8×10 | 0.212 | ||||
| Non-white | cb | 10 | x | x | x | 8×10 | 0.274 | ||||
| Male | cb | 10 | x | x | x | 8×10 | 0.199 | ||||
| Female | cb | 10 | x | x | 8×10 | 0.176 | |||||
| Elderly | cb | 10 | x | x | x | 8×10 | 0.159 | ||||
| ROA | |||||||||||
| Total | cb | 10 | 10 | x | x | x | x | x | 8×10 | 0.473 | |
| White | cb | 10 | x | x | x | 8×10 | 0.376 | ||||
| Non-white | cb | 10 | x | x | x | 8×10 | 0.273 | ||||
| Male | x | x | x | x | 8×10 | 0.363 | |||||
| Female | x | x | x | x | 8×10 | 0.292 | |||||
| Elderly | cb | 10 | x | x | x | x | x | 8×10 | 0.405 |
The simultaneous and lagged effects of various temperature and humidity variables on ED visits were modeled using a natural cubic spline function with three equally spaced knots per year for the continuous dependent variables, and lags were examined through 7 days in the dlnm. (We also ran models for 14 days and these results are included in Supplemental Figures.) The median value of AT was chosen to center the RR estimates. A variety of combinations of variables and lags were used to select the final model shown in equation 1 and Table 2. Candidate models, which including considerable testing for variations in degrees of freedom, were compared using the model adjusted r-squared value and a modified Akaike Information Criterion.
Results
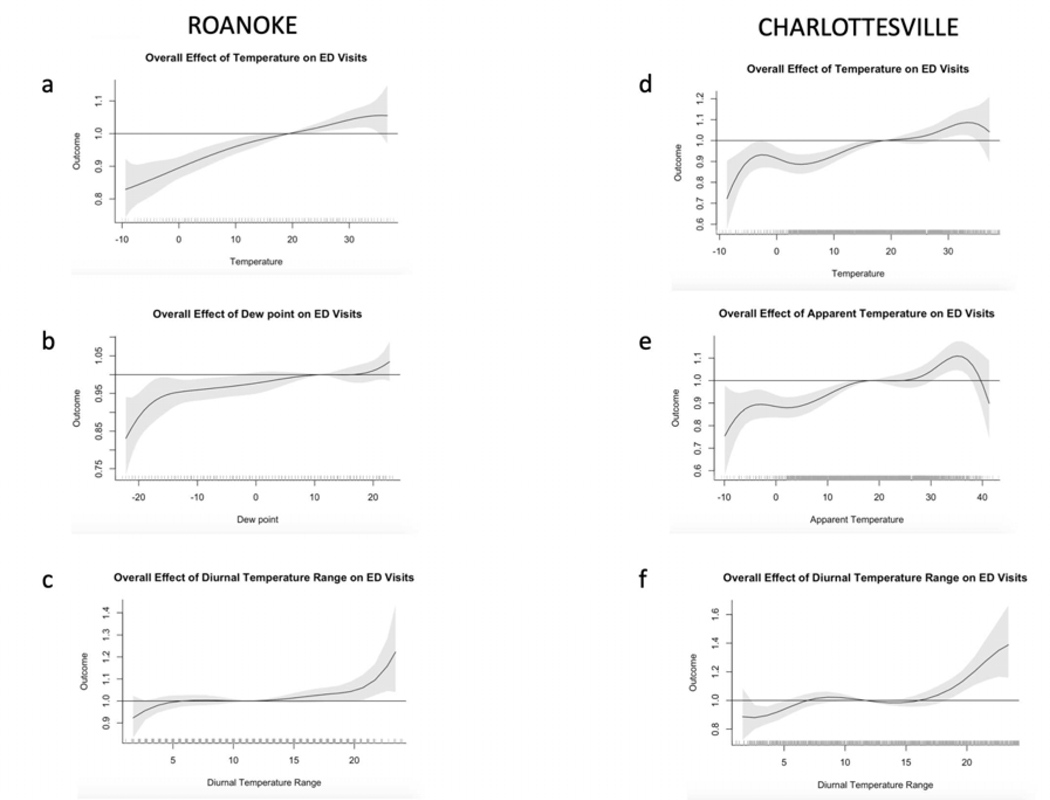
In Roanoke over a 7-day period, the RR of total ED visits exhibit a positive and almost linear relationship to 1 p.m. temperature, with a RR of about 1.05 on days above 30°C (Fig. 3a). Cold is protective of ED visits, with a near-linear decline of ED visits as a function of temperatures below 12°C. The influence of humidity (modeled using dew point temperature) is similar to the temperature response but weaker (Fig. 3b), and DTR shows a strong positive relationship, but only on rare days with very high DTRs above 21°C (Fig. 3c). Overall, the variables in this model account for almost half of the variance in total daily ED visitation (Table 2).
Figure 3.
Change in relative risk of ED visits over a 7-day period as a function of various weather variables at Roanoke (left) and Charlottesville (right). Tick marks along the x-axis indicate observations at those values. Shading indicates one standard error. The RR is centered at the median value of the predictand.
The Charlottesville model is similar but slightly more complex, with an increased RR of ED visits at temperatures above 28°C. However, the RR declines slightly at very high temperatures, probably because of the rarity of these events and the difficulty of modeling a small sample (Fig. 3d). As in Roanoke, cold is protective of ED visits when 1 p.m. temperatures are below 13°C. The overall effect using AT instead of temperature is slightly stronger, so we chose to model Charlottesville using AT because it implicitly incorporates humidity (Fig. 3e). The DTR pattern is similar to that of temperature (Fig. 3f). The overall goodness-of-fit for the Charlottesville model is lower than that for Roanoke (Table 2).
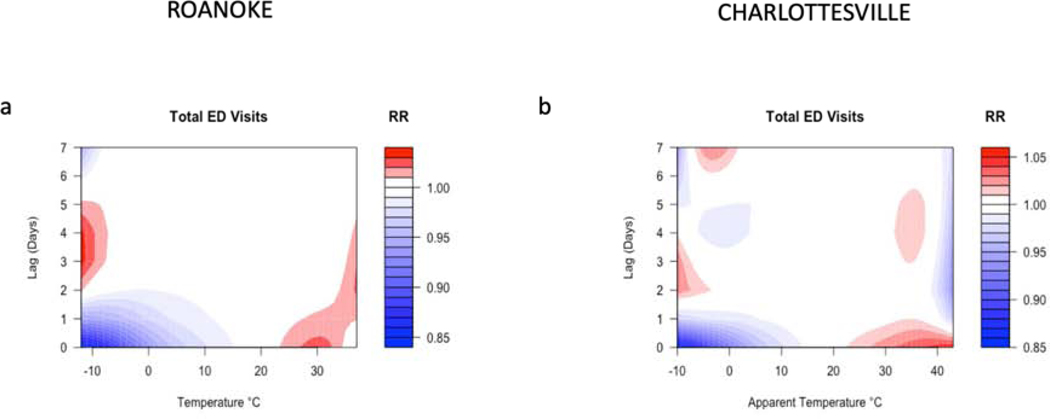
We next examined lags explicitly using the dlnm. In Roanoke at short lags (0 or 1 day), the results of the linear effects model are confirmed, with about a 4% increased RR at temperatures above 28°C and a protective effect at low temperatures, when the RR is less than 0.85 at temperatures below –5°C (Fig. 4a). However, the RR of ED visits increase by 1–3% from 2–5 days following a very cold day. There is also evidence of a similar, but weaker and shorter, lagged effect on very warm days.
Figure 4.
Relative risk of daily total ED visits as a function of air temperature or apparent temperature and lag for Roanoke (a) and Charlottesville (b).
The Charlottesville total ED visit results are generally similar to those from Roanoke. At lag zero, days with AT>30°C have a RR > 1.05 (Fig. 4b). As in Roanoke, low temperatures are protective with a similar RR. (Recall that below 21°C, AT is equivalent to air temperature.) Charlottesville also exhibits a 2–4 day lag with elevated risks on the coldest days. However, there are other, small RR values at longer lags that are difficult to interpret. The low RR at AT>40°C can be seen in Figure 3e and is likely a function of the small sample size (only 8 days had 1 p.m. AT > 40°C over the entire period of record).
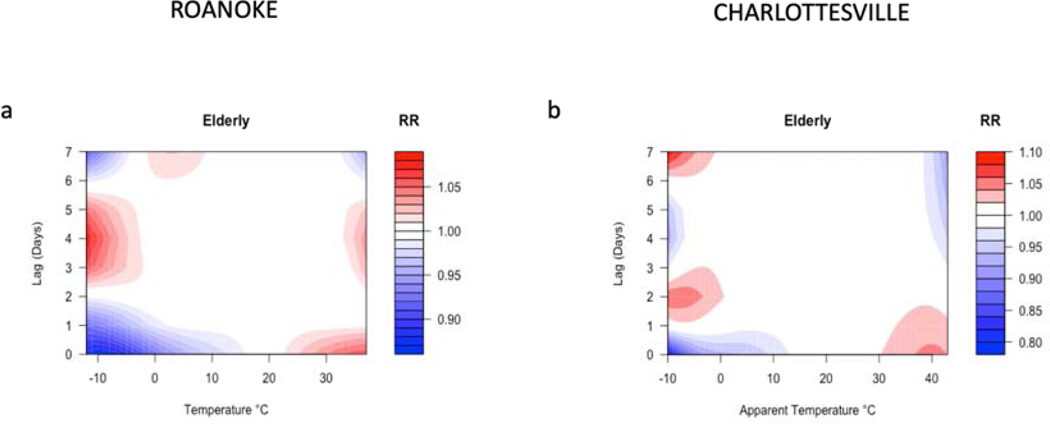
The Roanoke elderly model (age 65 and older) is quite similar to the overall ED visit results (Fig. 5a). The main differences are that the effect size is larger and the lagged cold effect is evident at a slightly higher temperature. The Charlottesville dlnm results for elderly patients are somewhat different (Fig. 5b). At high temperatures, the unlagged response begins around 30°C (a much higher threshold than at Roanoke) but the effect is much stronger. The elderly cold lag also peaks one day earlier than the overall ED visit model.
Figure 5.
Relative risk of elderly (age≥65) ED visits as a function of air temperature or apparent temperature and lag for Roanoke (a) and Charlottesville (b).
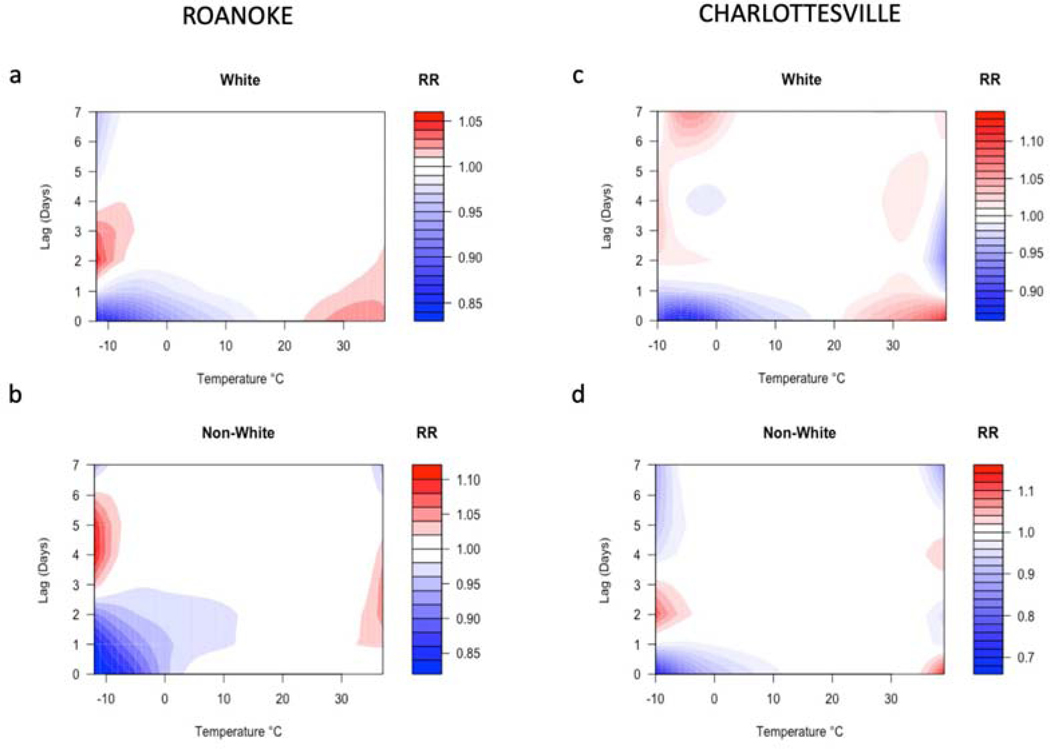
A comparison of the white vs. non-white ED visit patterns for Roanoke display some interesting differences (Fig. 6 a, b). Cold conditions appear to have a disparate impact on the non-white subgroup—the RR for lagged cold days is approximately 1.10 for nonwhites and 1.05 for whites. However, the RR on hot days is about 1.05 for both groups. Furthermore, non-whites exhibit a greater lagged response for both hot and cold days, with the peak response about two days after the white subgroup. In Charlottesville, there is evidence of an extensive lagged ED visit peak on cold days for whites at lags 2–7, with an effect size over 10% (Fig. 6 c, d). In contrast, the non-white cold peak shows only a 2–3 day lag, as in the overall ED model. On warm days and at no lag, whites appear to visit the ED at lower temperatures than non-whites, but the effect size on the warmest days is similar for white and non-whites.
Figure 6.
Relative risk of ED visits for whites (top) and non-whites (bottom) as a function of air temperature and lag for Roanoke (left) and Charlottesville (right).
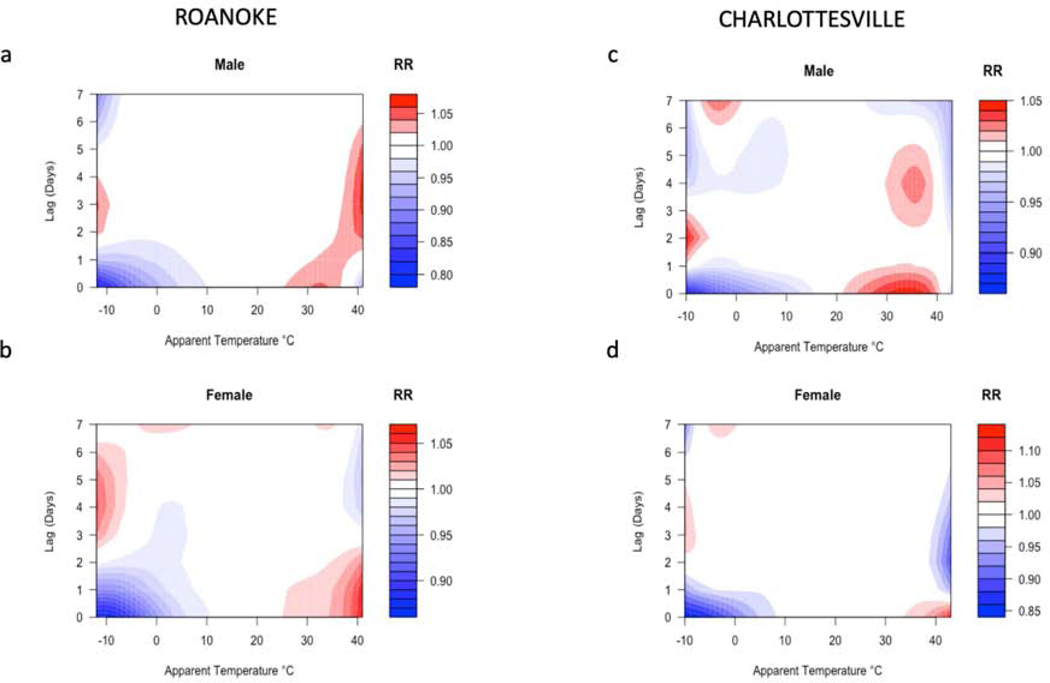
In Roanoke, the RR of ED visits is comparable between the male and female subgroups, but the lagged response differs (Fig. 7 a, b). On cold days. there is a much stronger ED visit peak for females 3–6 days after the event. Conversely, on the warmest days, males exhibit the same lagged effect whereas females show a decline (RR = 0.97) at these lags. In Charlottesville, the overall patterns are quite similar for males and females in the cold season. However, in the warm season, there is a stronger effect size for females but ED visits on warm days begin increasing at lower temperatures for males (Fig. 7 c, d).
Figure 7.
Relative risk of ED visits for males (top) and females (bottom) as a function of apparent temperature and lag for Roanoke (left) and Charlottesville (right).
Discussion
Temperature (or AT) extremes increase the risk of total daily ED visits by up to 5%. This effect size is generally consistent with similar studies (Bishop-Williams et al., 2015; Gronlund et al., 2014; Li et al., 2015; Song et al., 2018; Winquist et al., 2016; Ye et al., 2012), although cold morbidity has been understudied compared to cold mortality. Our finding of an overall approximately linear increase of ED visits and thermal variables is somewhat inconsistent with studies for morbidity at other locations. Although increased morbidity during hot conditions seems to be generalizable across most locations, our evidence showing an overall protective effect of cold weather differs from a number of other studies showing elevated morbidity at low temperatures (Conlon et al., 2011; Son and Bell, 2014; Wang and Lin, 2014; Ye et al., 2012) although effects of cold are not universal and tend to vary based on the specific disease (Ebi et al., 2004; Green et al., 2010; Wang and Lin, 2014).
The impact of heat on ED events is fairly immediate (Basu et al., 2012; Li et al., 2015; Ye et al., 2012) with lags of one day or less, whereas ED visits are lagged 2–4 days after cold weather. These longer lags at low temperatures are also consistent with prior research that primarily focused on cold-season mortality (Davidkovová et al. 2014; Ma et al., 2014; Ye et al., 2012; Zhou et al., 2014). The immediate protective effect of cold weather, which reduces the risk of ED visitation by 5–15% at temperatures below 10°C, could be related to both disease latency and human behavioral patterns, as people may be less willing to seek medical attention on cold days.
The pattern for the elderly in each location is quite similar to the overall ED visit pattern. This is not necessarily expected, as elderly patients account for less than one-fifth of all ED visits. In both locations, the effect size is several percent higher for the elderly, which is consistent with some of the literature suggesting that elderly morbidity is disproportionately impacted by temperature extremes (Bunker et al., 2016; Conlon et al., 2011; Kenny et al., 2010; Kovats and Ebi, 2006; Li et al., 2012, 2015; McGeehin and Mirabelli, 2001; Panagiotakos et al., 2004; Winquist et al., 2016; Wu et al., 2014). Heat impacts the elderly across a variety of diseases, including cardiovascular, respiratory, genitourinary and infectious diseases, and diabetes (Bunker et al., 2016). With respect to direct influences of high heat and humidity, the elderly exhibit a decreased sweating response (Anderson et al., 1996; Foster et al., 1976), and their underlying comorbidities tend to exacerbate heat impacts (Jones et al., 1982). In contrast, the impacts of cold conditions appear to be primarily on the respiratory system (Bunker et al., 2016). Influenza, along with pneumonia and related comorbid conditions, has a prominent winter peak (Reichert et al., 2004), disproportionately impacts the elderly (Menec et al., 2003), and may be related to periods of low temperature and humidity via enhanced opportunities for viral transmission (Davis et al., 2012, 2016).
Relationships between weather-related morbidity and gender and race/ethnicity are less clear. Whereas some research identifies higher coronary and stroke risk for females during cold conditions (Barnett et al., 2005; Hong et al., 2003; Panagiotakos et al., 2004), other studies found no overall differences (Ebi et al., 2004; Green et al., 2010). There is some evidence of greater heat stroke impact on males (Piver et al., 1999), but sex differences tend to vary considerably based on illness (Ye et al., 2001). Our results show a lower male heat threshold but also a weaker net effect on the warmest days. Likewise, differences based on race/ethnicity are unclear and/or inconsistent (Green et al., 2010). Some research has shown very high variability as a function of ethnicity and disease (Knowlton et al., 2009), but it is inherently difficult to disentangle effects of low socioeconomic status that might be correlated with these factors (Kravchenko et al., 2013). The longer lagged response for non-whites in Roanoke may be linked to socioeconomic status such as insurance availability and to community characteristics related to access to primary care, especially for patients who use EDs as a point of entry into the healthcare system (Cheung et al., 2012; Johnson et al., 2012; Lowe et al., 2009; Mannix et al., 2012). However, in Charlottesville the lagged responses between whites and non-whites are fairly similar, as are the effect sizes. Here, the major difference is the much lower heat threshold for whites compared to non-whites, a topic that has garnered comparatively little attention to date (Taylor, 2006).
In general, the ED visit response patterns between these two cities are more similar than they are different. This is encouraging, as it suggests that certain aspects of the relationship between weather and morbidity are generalizable for populations with similar demographic characteristics. There is abundant evidence that humans respond to thermal extremes in a relative rather than absolute manner (e.g., Davis et al., 2003; Gosling et al., 2009; Kalkstein and Davis, 1989; Kinney et al., 2008), so the similar patterns to abnormal heat and cold in Roanoke and Charlottesville would be expected. Yet there are interesting differences, particular for the subgroups. This might be anticipated as the sample sizes decline, especially given that the daily counts are not exceptionally large for either hospital. Clearly, additional comparative studies that examine race, ethnicity, and gender response differences are needed to sort out the lack of clarity on this aspect of human biometeorology.
As is the case with all retrospective, population-based studies, we do not have information on the actual exposure of individual subjects, so the weather conditions experienced by each person who visited the ED is unknown. By design, we hoped to restrict the spatial variability of exposures by limiting the area around each city from which visits are included. Nevertheless, there can be microclimatic variations that will be missed by using data from a single weather station. However, a comparison of a single station vs. a network of monitors suggests that this is not likely to be a major source of error (Barnett et al., 2010). Although the daily sample sizes are sufficiently large to provide robust daily estimates, these estimates are more subject to error for the smaller subgroups (elderly and non-white). Finally, the lack of long-term air quality data at sufficient temporal resolution at these sites is a limitation, although because of their size and climate, these cities are not typically prone to episodes of unusually poor air quality.
Conclusions
In both Charlottesville and Roanoke, the RR of ED visits is elevated 4–5% on warm and humid days and with a 2–4 day lag after cold days. ED visits are reduced (RR ≤ 0.85) on the day of and one day following cold events. The similarities in RR between two hospitals with similar regional demographic profiles and similar climates provides some evidence that these ED visit patterns could be extrapolated to other locations with similar profiles. For the more granular ED data, we found differences in heat and cold thresholds across gender and ethnicities that are inconsistent between locations. Although these results certainly merit additional study, it is premature to assume that they are likely representative of responses that could be generalized beyond the facilities in this study.
Future research on the patient-specific diseases associated with seasonally-varying ED visit patterns is needed. This kind of information could be used in targeted health campaigns that are linked to weather forecasts in an effort to mitigate against poor health outcomes and to reduce surges in ED visitations.
Supplementary Material
Acknowledgements:
The authors thank David M. Hondula (Arizona State University), Philip J. Stenger (University of Virginia Climate Office), and Martha M. Tenzer (Carilion Clinic) for their assistance with components of this project. Furthermore, we appreciate the suggestions provided by two anonymous reviewers whose comments have improved the clarity of our manuscript.
Funding:
This work was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health (UL1TR003015 and KL2TR003016), is solely the responsibility of the authors, and does not necessarily represent the official views of the National Institutes of Health. Additional support was provided by the University of Virginia’s Environmental Resilience Institute, College of Arts and Sciences, and School of Engineering and Applied Science.
Abbreviations
- ASOS
Automated Surface Observing System
- AT
apparent temperature
- BLU
Mercer County Airport
- CB
cross-basis
- CHO
Charlottesville-Albemarle County Airport
- DLNM
distributed lag non-linear model
- DOW
day of week
- DTR
diurnal temperature range
- ED
emergency department
- GAM
generalized additive model
- LOU
Louisa County Airport
- LYH
Lynchburg Regional Airport
- MTN
Blue Ridge Airport
- NWS
National Weather Service
- PUL
Pulaski County Airport
- ROA
Roanoke-Blacksburg Regional Airport
- RR
relative risk
- SHD
Shenandoah Valley Regional Airport
- T
air temperature
- Td
dew point temperature
- ZCTA
zip code tabulation area
Footnotes
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Anderson GB, Bell ML, 2010. Heat waves in the United States: mortality risk during heat waves and effect modification by heat wave characteristics in 43 US communities. Environmental Health Perspectives 119(2):210–18, 10.1289/ehp.1002313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson GB, Dominici F, Wang Y, McCormack MC, Bell ML, Peng RD, 2013. Heat-related emergency hospitalizations for respiratory diseases in the medicare population. ATS Journals 187(10), 10.1164/rccm.201211-1969OC,10.1007/BF02425488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson GS, Meneilly GS, Mekjavic IB, 1996. Passive temperature lability in the elderly. European Journal of Applied Physiology and Occupational Physiology 73(3–4): 278–286. [DOI] [PubMed] [Google Scholar]
- Barnett AG, Dobson AJ, McElduff P, Salomaa V, Kuulasmaa K, Sans A, 2005. Cold periods and coronary events: an analysis of populations worldwide. Journal of Epidemiology & Community Health 59(7):551–557, 10.1136/jech.2004.028514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett AG, Greenberg S, Gasparrini A, Rocklöv J, 2012. Cold and heat waves in the United States. Environmental Research 112:218–224, 10.1016/j.envres.2011.12.010 [DOI] [PubMed] [Google Scholar]
- Barnett AG, Tong S, Clements ACA, 2010. What measure of temperature is the best predictor of mortality? Environmental Research 110(6):604–611, 10.1016/j.envres.2010.05.006 [DOI] [PubMed] [Google Scholar]
- Basu R, Pearson D, Malig B, Broadwin R, Green R, 2012. The effect of high ambient temperature on emergency room visits. Epidemiology 23:813–820, 10.1097/EDE.0b013e31826b7f97 [DOI] [PubMed] [Google Scholar]
- Bishop-Williams KE, Berke O, Pearl DL, Kelton DF, 2015. A spatial analysis of heat stress related emergency room visits in rural Southern Ontario during heat waves. BMC Emergency Medicine 15(17), 10.1186/s12873-015-0043-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunker A, Wildenhain J, Vandenbergh A, Nenschke N, Rocklöv J, Hajat S, Sauerborn R, 2016. Effects of air temperature on climate-sensitive mortality and morbidity outcomes in the elderly; a systematic review and meta-analysis of epidemiological evidence. The Lancet 6:258–268, 10.1016/j.ebiom.2016.02.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen T, Sarnat SE, Grundstein AJ, Winquist A, Chang HH, 2017. Time-series analysis of heat waves and emergency department visits in Atlanta, 1993 to 2012. Environmental Health Perspectives 125(5), 10.1289/EHP44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng J, Xu Z, Zhu R, Wang X, Jin L, Song J, Su H, 2014. Impact of diurnal temperature range on human health: a systematic review. International Journal of Biometeorology 58(9):2011–2024, 10.1289/EHP44 [DOI] [PubMed] [Google Scholar]
- Cheung PT, Wiler JL, Lowe RA, Ginde AA, 2012. National study of barriers to timely primary care and emergency department utilization among Medicaid beneficiaries. Annals of Emergency Medicine. 60(1):4–10, 10.1016/j.annemergmed.2012.01.035 [DOI] [PubMed] [Google Scholar]
- Conlon KC, Rajkovich NB, White-Newsome JL, Larsen L, O’Neill MS, 2011. Preventing cold-related morbidity and mortality in a changing climate. Maturitas 69(3):197–202, 10.1016/j.maturitas.2011.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davídkovová H, Plavcová E, Kyncl J, Kysely J. 2014. Impacts of hot and cold spells differ for acute and chronic ischaemic heart diseases. BMC Public Health 14(1):480, 10.1186/1471-2458-14-480, 10.1186/1471–2458-14–480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis RE, Dougherty E, McArthur C, Huang QS, Baker MG, 2016. Cold, dry air is associated with influenza and pneumonia mortality in Auckland, New Zealand. Influenza and Other Respiratory Viruses 10(4):310–313, 10.1111/irv.12369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis RE, Hondula DM, Sharif H, 2020. Examining the diurnal temperature range enigma: Why is human health related to the daily change in temperature? International Journal of Biometeorology 64(3):397–407, 10.1007/s00484-019-01825-8 [DOI] [PubMed] [Google Scholar]
- Davis RE, Houck M, Markle E, Windoloski S, Enfield KB, Kang H, Balling RC Jr., Kuehl DR, Burton JH, Farthing W, Rubio ER, Novicoff WM, 2020. The impact of heat waves on emergency department visits in Roanoke, Virginia: Academic Emergency Medicine, 10.1111/acem.13919 [DOI] [PubMed] [Google Scholar]
- Davis RE, Knappenberger PC, Michaels PJ, Novicoff WM, 2003. Changing heat-related mortality in the United States. Environmental health perspectives 111(14):1712–1718, 10.1289/ehp.6336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis RE, Novicoff WM, 2018. The impact of heat waves on emergency department admissions in Charlottesville, Virginia, USA. International Journal of Environmental Research and Public Health 15(7):1436, 10.3390/ijerph15071436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis RE, Rossier CE, Enfield KB, 2012. The impact of weather on influenza and pneumonia mortality in New York City, 1975–2002: a retrospective study. PloS ONE 7(3), 10.1371/journal.pone.0034091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebi KL, Exuzides KA, Lau E, Kelsh M, Barnston A, 2004. Weather changes associated with hospitalizations for cardiovascular diseases and stroke in California, 1983–1998. International Journal of Biometeorology 49(1):48–58, 10.1007/s00484-004-0207-5 [DOI] [PubMed] [Google Scholar]
- Fletcher BA, Lin S, Fitzgerald EF, Hwang SA, 2012. Association of summer temperatures with hospital admissions for renal diseases in New York state: a case-crossover study. American Journal of Epidemiology 175(9):907–916, 10.1093/aje/kwr417 [DOI] [PubMed] [Google Scholar]
- Foster KG, Ellis FP, Dore C, Exton-Smtth AN, Weiner JS, 1976. Sweat responses in the aged. Age and Ageing 5(2):91–101, 10.1093/ageing/5.2.91 [DOI] [PubMed] [Google Scholar]
- Fuhrmann CM, Sugg MM, Konrad CE, Waller A, 2016. Impact of extreme heat events on emergency department visits in North Carolina (2007–2011). Journal of Community Health 41(1):146–156, 10.1007/s10900-015-0080-7 [DOI] [PubMed] [Google Scholar]
- Gasparrini A, 2011. Distributed lag linear and non-linear models in R: the package dlnm. Journal of Statistical Software 43(8):1. [PMC free article] [PubMed] [Google Scholar]
- Gosling SN, Lowe JA, McGregor GR, Pelling M, Malamud BD, 2009. Associations between elevated atmospheric temperature and human mortality: a critical review of the literature. Climatic Change 92(3–4):299–341, 10.1007/s10584-008-9441-x [DOI] [Google Scholar]
- Green RS, Basu R, Malig B, Broadwin R, Kim JJ, Ostro B, 2010. The effect of temperature on hospital admissions in nine California counties. International Journal of Public Health 55(2):113–121, 10.1007/s00038-009-0076-0 [DOI] [PubMed] [Google Scholar]
- Greenberg JH, Bromberg J, Reed CM, Gustafson TL, Beauchamp RA, 1983. The epidemiology of heat-related deaths, Texas−−1950, 1970–79, and 1980. American Journal of Public Health 73(7):805–807, 10.2105/AJPH.73.7.805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gronlund CJ, Zanobetti A, Schwartz JD, Wellenius GA, O’Neill MS, 2014. Heat, heat waves, and hospital admissions among the elderly in the United States. Environmental Health Perspectives 122(11), 10.1289/ehp.1206132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Y, Gasparrini A, Armstrong B, Li S, 2016. Tawatsupa B, Tobias A. Temperature variability and mortality: a multi-country study. Environmental Health Perspectives 124(10):1554–1559, 10.1289/EHP149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong YC, Rha JH, Lee JT, Ha EH, Kwon HJ, Kim H, 2003. Ischemic stroke associated with decrease in temperature. Epidemiology 14(4):473–478, 10.1097/01.ede.0000078420.82023.e3 [DOI] [PubMed] [Google Scholar]
- Johnson PJ, Ghildayal N, Ward AC, Westgard BC, Boland LL, Hokanson JS, 2012. Disparities in potentially avoidable emergency department (ED) care: Ed visits for ambulatory care sensitive conditions. Med Care 50(12):1020–1028, 10.1097/MLR.0b013e318270bad4 [DOI] [PubMed] [Google Scholar]
- Jones TS, Liang AP, Kilbourne EM, Griffin MR, Patriarca PA, Wassilak SGF, 1982. Mullan RJ, Herrick RF, Donnell HDD Jr, Choi K, Thacker SB. Morbidity and mortality associated with the July 1980 heat wave in St Louis and Kansas City, Mo. Journal of the American Medical Association 247(24):3327–3331, 10.1001/jama.1982.03320490025030 [DOI] [PubMed] [Google Scholar]
- Kalkstein LS, Davis RE, 1989. Weather and human mortality: an evaluation of demographic and interregional responses in the United States. Annals of the Association of American Geographers 79(1):44–64, 10.1111/j.1467-8306.1989.tb00249.x [DOI] [Google Scholar]
- Kenny GP, Yardley J, Brown C, Sigal RJ, Jay O, 2010. Heat stress in older individuals and patients with common chronic diseases. CMAJ 182(10):1053–1060, 10.1503/cmaj.081050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilbourne EM, 1997. Heat waves and hot environments In: Noji EK (Ed.), The Public Health Consequences of Disaster. New York:Oxford University Press, pp. 245–269, 10.1017/S1049023X00025255 [DOI] [Google Scholar]
- Kinney PL, O’Neill MS, Bell ML, Schwartz J, 2008. Approaches for estimating effects of climate change on heat-related deaths: challenges and opportunities. Environmental Science & Policy 2008;11(1):87–96, 10.1016/j.envsci.2007.08.001 [DOI] [Google Scholar]
- Knowlton K, Rotkin-Ellman M, King G, Margolis HG, Smith D, Solomon G, Trent R, English P, 2009. The 2006 California heat wave: impacts on hospitalizations and emergency department visits. Environmental Health Perspectives 117(1): 61–67, 10.1289/ehp.11594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovats RS, Ebi KL, 2006. Heatwaves and public health in Europe. Eur. J. Public Health 16:592–599, 10.1093/eurpub/ckl049 [DOI] [PubMed] [Google Scholar]
- Kravchenko J, Abernethy AP, Fawzy M, Lyerly HK, 2013. Minimization of heatwave morbidity and mortality. American Journal of Preventive Medicine 44:274–282, 10.1016/j.amepre.2012.11.015 [DOI] [PubMed] [Google Scholar]
- Lee W, Bell ML, Gasparrini A, Armstrong BG, Sera F, Hwang S, 2018. Mortality burden of diurnal temperature range and its temporal changes: a multi-country study. Environment International 110:123–130, 10.1016/j.envint.2017.10.018 [DOI] [PubMed] [Google Scholar]
- Li B, Sain S, Mearns LO, Anderson HA, Kovats S, Ebi KL, Bekkedal MYV, Kanarek MS, Patz JA, 2012. The impact of extreme heat on morbidity in Milwaukee, Wisconsin. Climatic Change 110(3–4):959–976, 10.1007/s10584-011-0120-y [DOI] [Google Scholar]
- Li M, Gu S, Bi P, Yang J, Liu Q, 2015. Heat waves and morbidity: current knowledge and further direction-a comprehensive literature review. International Journal of Environmental Research and Public Health 12(5):5256–5283, 10.3390/ijerph120505256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim YH, Hong YC, Kim H, 2012. Effects of diurnal temperature range on cardiovascular and respiratory hospital admissions in Korea. Science of the Total Environment. 2012;417:55–60, 10.1016/j.scitotenv.2011.12.048 [DOI] [PubMed] [Google Scholar]
- Lowe RA, Fu R, Ong ET, McGinnis PB, Fagnan LJ, Vuckovic N, Gallia C, 2009. Community characteristics affecting emergency department use by Medicaid enrollees. Med. Care 47(1):15–22, 10.1097/MRL.0b013e3181844eoc [DOI] [PubMed] [Google Scholar]
- Luber G, McGeehin M, 2008. Climate change and extreme heat events. American Journal of Preventive Medicine 35(5):429–435, 10.1016/j.amepre.2008.08.021 [DOI] [PubMed] [Google Scholar]
- Ma W, Chen R, Kan H, 2014. Temperature-related mortality in 17 large Chinese cities: how heat and cold affect mortality in China. Environmental Research 134:127–133, 10.1016/j.envres.2014.07.007 [DOI] [PubMed] [Google Scholar]
- Mannix R, Stack AM, Chiang V, 2012. Insurance status and the care of adult patients 19 to 64 years of age visiting the emergency department. Academic Emergency Medicine 19(7):808–815, 10.1111/j.1553-2712.2012.01394.x [DOI] [PubMed] [Google Scholar]
- McGeehin MA, Mirabelli M, 2001. The potential impacts of climate variability and change on temperature-related morbidity and mortality in the United States. Environmental Health Perspectives 102(2):185–189, 10.1289/ehp.109-1240665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menec VH, Black C, MacWilliam L, Aoki FY, 2003. The impact of influenza-associated respiratory illnesses on hospitalizations, physician visits, emergency room visits, and mortality. Canadian Journal of Public Health 94(1):59–63, 10.1007/BF03405054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monterio A, Carvalho V, Gois J, Sousa C, 2013. Use of “cold spell” indices to quantify excess chronic obstructive pulmonary disease (COPD) morbidity during winter (November to March 2000–2007): case study in Porto. International Journal of Biometeorology 57(6):857–870, 10.1007/s00484-012-0613-z [DOI] [PubMed] [Google Scholar]
- Nastos PT, Matzarakis A, 2006. Weather impacts on respiratory infections in Athens, Greece. International Journal of Biometeorology 50(6):358–369, 10.1007/s00484-006-0031-1 [DOI] [PubMed] [Google Scholar]
- Panagiotakos DB, Chrysohoou C, Pitsavos C, Nastos P, Anadiotis A, Tentolouris C, Stefanadis C, Toutouzas P, Paliatsos A, 2004. Climatological variations in daily hospital admissions for acute coronary syndromes. International Journal of Cardiology 94(2–3):229–233, 10.1016/j.ijcard.2003.04.050 [DOI] [PubMed] [Google Scholar]
- Piver WT, Ando M, Ye F, Portier CJ, 1999. Temperature and air pollution as risk factors for heat stroke in Tokyo, July and August 1980–1995. Environmental Health Perspectives 107(11):911–916, 10.1289/ehp.99107911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reichert TA, Simonsen L, Sharma A,Pardo SA, Fedson DS, Miller MA, 2004. Influenza and the winter increase in mortality in the United States, 1959–1999. American Journal of Epidemiology 160:492–502, 10.1093/aje/kwh227 [DOI] [PubMed] [Google Scholar]
- Sherbakov T, Malig B, Guirguis K, Gershunov A, Basu R, 2018. Ambient temperature and added heat wave effects on hospitalizations in California from 1999 to 2009. Environmental Research 160:83–90, 10.1016/j.envres.2017.08.052 [DOI] [PubMed] [Google Scholar]
- Son J, Bell ML, 2014. The impact of heat, cold, and heat waves on hospital admissions in eight cities in Korea. International Journal of Biometeorology 58(9): 1893–1903, 10.1007/s00484-014-0791-y [DOI] [PubMed] [Google Scholar]
- Song X, Wang S, Hu Y, Yue M, Zhang T, Liu Y, Tian J, Shang K, 2017. Impact of ambient temperature on morbidity and mortality: An overview of reviews. Science of The Total Environment 586:241–254, 10.1016/j.scitotenv.2017.01.212 [DOI] [PubMed] [Google Scholar]
- Steadman RG, 1979. The assessment of sultriness. Part I: A temperature-humidity index based on human physiology and clothing science. Journal of Applied Meteorology 18(7):861–873, [DOI] [Google Scholar]
- Taylor NAS, 2006. Ethnic differences in thermoregulation: genotypic versus phenotypic heat adaptation. Journal of Thermal Biology 31(1–2):90–104, 10.1016/j.jtherbio.2005.11.007 [DOI] [Google Scholar]
- Tian L, Qiu H, Sun S, Lin H, 2016. Emergency cardiovascular hospitalization risk attributable to cold temperatures in Hong Kong. Circulation: Cardiovascular Quality and Outcomes 9:135–142, 10.1161/CIRCOUTCOMES.115.002410 [DOI] [PubMed] [Google Scholar]
- Wang YC, Lin YK, 2014. Association between temperature and emergency room visits for cardiorespiratory diseases, metabolic syndrome-related diseases, and accidents in metropolitan Taipei. PLoS ONE, 10.1371/journal.pone.0099599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winquist A, Grundstein A, Chang HH, Hess J, Sarnat SE, 2016. Warm season temperatures and emergency department visits in Atlanta, Georgia. Environmental Research 147:314–23, 10.1016/j.envres.2016.02.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu X, Brady JE, Rosenberg H, Li G, 2014. Emergency department visits for heat stroke in the United States, 2009 and 2010. Injury Epidemiology 1(1):8, 10.1186/2197-1714-1-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Z, Huang C, Hu W, Turner LR, Tong S, 2013. Extreme temperatures and emergency department admissions for childhood asthma in Brisbane, Australia. Occupational and Environmental Medicine 70(10):730–735, 10.1136/oemed-2013-101538 [DOI] [PubMed] [Google Scholar]
- Ye F, Piver WT, Ando M, Portier CJ, 2001. Effects of temperature and air pollutants on cardiovascular and respiratory diseases for males and females older than 65 years of age in Tokyo, July and August 1980–1995. Environmental Health Perspectives 109(4):355–359, 10.1289/ehp.01109355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye X, Wolff R, Yu W, Vaneckova P, Pan X, Tong S, 2012. Ambient temperature and morbidity: a review of epidemiological evidence. Environmental Health Perspectives 120(1):19–28, 10.1289/ehp.1003198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou MG, Wang LJ, Liu T, Zhang YH, Lin HL, Luo Y, Xiao JP, Zeng WL, Zhang YW, Wang XF, Gu X, Rutherford S, Chu C, Ma WJ, 2014. Health impact of the 2008 cold spell on mortality in subtropical China: the climate and health impact national assessment study (CHINAs).” Environmental Health 13(1): 60, 10.1186/1476-069X-13-60 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.