Abstract
Background
Painful diabetic neuropathy is an important therapeutic challenge as the efficacy of analgesic drugs in this setting is still unsatisfactory. Monotherapy with available treatments is often not sufficient and a combination of drugs is necessary. Trazodone (TRZ) is a compound with a multi-modal mechanism of action, being a serotonin-2 antagonist/reuptake inhibitor developed and approved for the treatment of depression in several countries. Previous clinical trials suggest a possible beneficial effect of low doses of trazodone for the treatment of patients affected by painful diabetic neuropathy.
Objective
This phase II study was designed to collect data on the efficacy and safety of low doses of TRZ combined with gabapentin after 8 weeks of treatment in patients affected by painful diabetic neuropathy.
Methods
This was a randomized, double-blind, placebo-controlled, multi-center, international, prospective study. Male and female diabetic patients aged 18–75 years and affected by painful diabetic neuropathy were eligible for enrollment. Subjects were randomized (1:1:1 ratio) to TRZ30 (10 mg three times daily for 8 weeks) or TRZ60 (20 mg three times daily for 8 weeks) or placebo. Gabapentin as background therapy was administered in open-label conditions to all patients. The primary endpoint was the change from baseline of the Brief Pain Inventory Short Form item 5 to week 8. Secondary endpoints included the other Brief Pain Inventory Short Form items, and the assessment of anxiety, sleep, quality of life, patient’s improvement, and safety.
Results
One hundred and forty-one patients were included in the intention-to-treat population: 43 allocated to the TRZ30 group, 50 to the TRZ60 group, and 48 to the placebo group. After 8 weeks, the mean changes of Brief Pain Inventory Short Form item 5 from baseline were − 3.1, − 2.6, and − 2.5 in the TRZ30, TRZ60, and placebo groups, respectively. No statistically significant differences between groups were seen. Nevertheless, a better trend was observed for TRZ30 vs placebo (95% confidence interval − 1.30, 0.15; p = 0.1179), on top of the background effect of gabapentin administered to all study groups. 62.8% of patients achieved a ≥ 50% reduction in the TRZ30 group, 54% in the TRZ60 group, and 45.8% in the placebo group. At the same time, a statistically significant improvement was observed in Brief Pain Inventory Short Form item 6 for TRZ30 vs placebo (95% confidence interval − 1.54, − 0.07; p = 0.0314). No serious adverse event occurred during the trial and the most frequent treatment-emergent adverse events involved nervous system, QT prolongation, and gastrointestinal disorders.
Conclusions
All treatment groups showed a clinically meaningful pain improvement; nevertheless, patients in the TRZ30 treatment group reported better efficacy outcomes. This finding suggests that low doses of TRZ could be useful for treating painful diabetic neuropathy, and support further adequately powered confirmatory trials investigating the efficacy of TRZ.
Clinical Trial Registration
NCT03202979, date of registration: 29/06/2017.
Key Points
| Painful diabetic neuropathy represents a major challenge in clinical practice in terms of pain control, impairment of functioning, and quality of life. |
| Previous clinical trials suggest a possible beneficial effect of low doses of trazodone for the treatment of patients affected by painful diabetic neuropathy. |
| Low doses of trazodone on top of a full dosage of gabapentin were well tolerated by patients and improved pain, sleep, and quality of life. |
Introduction
Painful diabetic neuropathy (PDN) is one of the most common long-term complications in patients with type 1 and 2 diabetes mellitus [1]. About 7.5% of the patients already experience painful diabetic peripheral neuropathy at the initial diagnosis and approximately 45–50% have this complication after 25 years [2]. Painful diabetic neuropathy may interfere with general activity, mood, mobility, work, social relations, sleep, leisure activities, and enjoyment of life and patient generally have a poor quality of life [3].
The pathogenesis of PDN is not fully understood. However, several theories have been proposed such as changes in the blood vessels that supply the peripheral nerves, metabolic and autoimmune disorders with glial cell activation, changes in sodium and calcium channel expression, and central pain mechanisms, such as increased thalamic vascularity and imbalance of the facilitatory/inhibitory descending pathways [2]. Recent studies also demonstrated that gain-of-function mutations of voltage-gated sodium channels may contribute to PDN [4]. Moreover, several risk factors are associated with PDN including worsening glucose tolerance, older age, longer diabetes duration, alcohol, and smoking [5].
Current treatment options include approved drugs such as serotonin-norepinephrine reuptake inhibitors, e.g., duloxetine, gabapentinoids such as pregabalin and gabapentin, topical treatment with capsaicin, and several off-label use drugs such as other antidepressants (e.g., tricyclic antidepressants), antiepileptic drugs, and weak and strong opioids. Unfortunately, there is no consensus on the single most effective drug and monotherapy rarely provides adequate pain relief [6]. Clinical management of diabetic peripheral neuropathic pain continues to represent a therapeutic challenge and the response to existing treatments is often inadequate [7]. International guidelines also suggest the use of both approved and off-label treatments, alone or in combination [8]. Combinations and add-on therapies are encouraged as potential solutions to improve safety and efficacy, which can be achieved by lowering doses with the aim to reduce side effects [9].
Some antidepressants are considered as an essential component of the therapeutic strategy for the treatment of different types of persistent pain [10]. It is supposed that antidepressants such as tricyclic antidepressants or the serotonin norepinephrine reuptake inhibitors may be involved in the reinforcement of the descending inhibitory pathways by increasing the amount of norepinephrine and serotonin in the synaptic cleft at both supra-spinal and spinal levels [11].
Trazodone (TRZ) is a compound with a multi-modal mechanism of action, being a serotonin-2 antagonist/reuptake inhibitor approved in several countries for the treatment of depression with or without anxiety, with a daily dosage range of 150–600 mg [12]. Regarding the pharmacological actions in humans, TRZ is thought to have more than one mechanism of therapeutic action, making it a multi-functional drug with dose-dependent pharmacological actions [13]. Being an antidepressant belonging to the class of serotonin-2 antagonist/reuptake inhibitors, TRZ is a potent and selective postsynaptic 5-HT2A antagonist and a moderately potent serotonin reuptake inhibitor, with high affinity for 5-HT2A receptors and moderate affinity for 5-HT1A and 5-HT2C receptors [14–16]. Because of its combined serotoninergic receptor antagonism and serotonin reuptake inhibition, TRZ has demonstrated unique therapeutic flexibility, which has given rise to its potential use in a broad range of co-morbidities associated with major depressive disorder as well as off-label use, including insomnia, anxiety, dementia, Alzheimer’s disease, substance abuse, schizophrenia, bulimia, and fibromyalgia [15]. In addition, the fewer adverse drug reactions potentially related to the stimulation of 5-HT2A receptors in comparison with serotonin selective reuptake inhibitors (i.e., agitation, anxiety, sexual dysfunction, and sleep disturbances), associated with a moderate effect on the QT interval, confirm the very good tolerability profile of TRZ [15].
Recent preclinical studies suggested a potential role of 5-HT2A and the mGlu2/3 heterodimer both in the brain and the spinal cord accounting for hyperexcitability and a cellular signaling cascade related to glutamate exocytosis and neuropathic pain [17–19]. Based on this cross-talk mechanism, it has been proposed that TRZ, a potent 5-HT2A antagonist, could possibly modulate the glutamate exocytosis [19].
Indeed, low doses of TRZ (starting from 50 mg/day) have been already used in neuropathic pain, suggesting a potential beneficial effect for pain relief [20, 21]. Consequently, the present phase II study was designed to collect preliminary data on the efficacy and safety of low doses of TRZ for the treatment of patients affected by PDN in a randomized controlled clinical trial.
Methods
Study Design and Populations
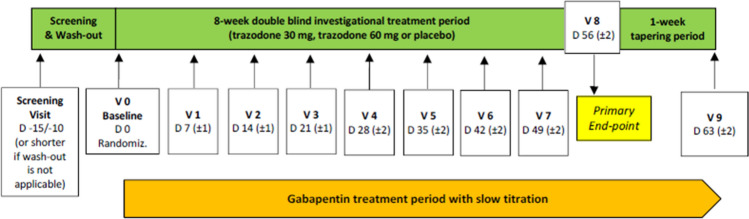
This was a phase II, randomized, double-blind, placebo-controlled, double-dummy, dose-finding, parallel-group, multi-center, international, prospective pilot study performed in 20 investigational sites in three European countries (Czech Republic, Hungary, and Poland). The EudraCT trial number was 2016-002772-27. The study consisted of three main study periods: the screening and wash-out, the 8-week double-blind investigational treatment period, and the 1-week tapering period, for a maximum of 11 visits in total (Fig. 1).
Fig. 1.
Study design. D day, Randomiz randomization, V visit
The patients were eligible to enter the study if the following inclusion criteria were met: male or female patient between 18 and 75 years of age (limits included) affected by PDN manifesting with distally distributed neuropathic pain (the diagnosis of neuropathy was based on a structured clinical examination); stable glycemic control with a glycosylated hemoglobin value of ≤ 10% at the screening visit; pain persisting for at least 3 months; neuropathic pain confirmed by a Douleur Neuropatique 4 score ≥ 4 at the screening visit; Brief Pain Inventory Short Form (BPI-SF) 24-h average pain score (item 5) ≥ 4 at the screening and baseline visits; patient who was currently not receiving treatment for PDN or a patient who was receiving treatment, with drug/s other than gabapentin, and had completed the required washout; women of childbearing potential had to have a negative pregnancy test at the screening visit; patients legally capable to give their consent to participate in the study and available to sign and date the written informed consent. Main exclusion criteria included: other forms of neuropathic pain or non-neuropathic pain; concomitant treatment with other medications for pain management; use of TRZ or gabapentin in the previous 3 months; active foot ulcer or previous major limb amputation; glomerular filtration rate value < 60 mL/min calculated by the Modification of Diet in Renal Disease formula.
A total of 120 evaluable patients were planned to be enrolled in the study and randomized to one of the following three treatment groups in double-blind conditions:
Group 1: TRZ 20 mg three times daily (t.i.d.) for 8 weeks. The total daily dose was 60 mg.
Group 2: TRZ 10 mg t.i.d. for 8 weeks. The total daily dose was 30 mg.
Group 3: placebo (PLB) t.i.d. for 8 weeks.
In addition, gabapentin as background therapy was administered in open-label conditions to all patients, according to the following regimen:
100 mg (one capsule) t.i.d., from day 0 to day 6 (± 1);
100 mg (two capsules) t.i.d., from day 7 (± 1) to day 13 (± 1);
300 mg (one capsule) t.i.d., from day 14 (± 1) to day 20 (± 1);
400 mg (one capsule) t.i.d., from day 21 (± 1) to day 27 (± 2);
300 mg (two capsules) t.i.d., from day 28 (± 2) to day 34 (± 2);
400 mg (two capsules) t.i.d., from day 35 (± 2) to the end of the trial.
A slow titration of gabapentin was applied to control possible side effects when co-administered with TRZ. The target dosage of gabapentin was 2400 mg daily by week 5. For patients presenting with a glomerular filtration rate value between 60 and 79 mL/min at the screening visit, the target maximum total daily dose was 1800 mg.
After the 8-week treatment period, patients started 1 week of tapering off in double-blind conditions. Thus, patients allocated to group 1 received TRZ 10 mg t.i.d., while patients allocated to groups 2 and 3 received a PLB oral solution.
During the study, medications for pain management, including but not limited to tricyclic antidepressants, serotonin and norepinephrine reuptake inhibitors, other gabapentinoids different from gabapentin, opioids, mexiletine hydrochloride, carbamazepine, phenytoin, valproate sodium, dextromethorphan, capsaicin, corticosteroids, non-steroidal anti-inflammatory drugs, skeletal muscle relaxants, benzodiazepines, and over-the-counter medications with centrally acting properties, were prohibited and discontinued for a period specific to the taper schedule (based on five elimination half-lives of the used medication) before randomization. In case of need, only paracetamol as an analgesic and aspirin for prophylaxis of a myocardial infarction or transient ischemic attack were allowed, both administered in accordance with their Summary Product Characteristics.
Randomization and Blinding
At visit 0 (day 0), patients were randomized in a 1:1:1 ratio to the three parallel groups, based on a computer-generated sequence. Double blinding was maintained throughout all treatment periods by using a TRZ solution matching PLB solution and the same dosing regimen for all groups in terms of timing and number of drops. Only gabapentin as background therapy (100-, 300-, and 400-mg capsules; Neurontin®, Pfizer, Latina - Italy) was administered in open-label conditions. In case of medical emergency, the investigator was able to unblind the treatment code through the blinded labels provided by the sponsor.
Study Outcome Measures
The primary endpoint of the study was the change from baseline of the BPI-SF item 5 ‘24-hour average pain score’ to week 8. The BPI-SF is a patient-completed numeric rating scale that assesses the severity of pain, its impact on daily functioning, and other aspects of pain (e.g., location of pain, relief from medications) and it has been specifically validated for PDN [22, 23]. The BPI-SF item uses a 0–10 numeric rating scale anchored at zero for “no pain” or “does not interfere” and 10 for “pain as bad as you can imagine” or “completely interferes”.
As secondary endpoints, this study assessed the following parameters: the neuropathic pain symptoms using the Neuropathic Pain Symptom Inventory and the other items of the BPI-SF; anxiety using the Hamilton Anxiety Rating Scale; sleep using the Leeds Sleep Evaluation Questionnaire; quality of life using the SF-36; patient’s improvement using the Patient Global Impression of Change; and safety and tolerability.
As safety variables, adverse events were monitored throughout the whole study period from the signature of the informed consent form up to the last visit. A complete physical examination (including the measurement of vital signs) was performed at all applicable visits, while laboratory analyses (hematology, serum chemistry, and urinalysis) were performed at the screening visit, visit 4, and visit 8. Blood and urine samples were analyzed by the Central Laboratory ACM located in the UK and laboratory reports were assessed by the investigator. At all visits, the patients were also monitored for cardiac safety: 12-lead electrocardiograms (ECGs) were evaluated by the Central Cardiac Laboratory Bioclinica located in USA.
Statistical Analysis
This clinical trial planned to collect preliminary information on the efficacy outcome measures. In this context, a sample size of 40 patients per group was considered adequate for this purpose. In further confirmatory clinical trials, which may be conducted to prove the effect of the drug, the sample size calculation will be based on the preliminary evidence collected during this study.
For statistical purposes, the intention-to-treat (ITT) population was defined as all randomized patients who took at least one dose of the study medication, having a baseline evaluation and at least one post-baseline BPI-SF evaluation. The last observation carried forward method was implemented as the imputation scheme for missing data in the ITT population. Efficacy endpoints were reported descriptively as the 95% confidence interval (CI) around the mean change from baseline. In addition, an analysis of covariance model was applied and the relevant least-square mean change from baseline to the endpoint was estimated and compared between treatment groups. If statistical assumptions underlying the analysis of covariance model were not satisfied, an analysis of variance model was applied. No adjustment for multiple comparisons were implemented. Results from hypothesis testing were treated as preliminary and interpreted with caution.
Results
Patient Disposition and Baseline Characteristics
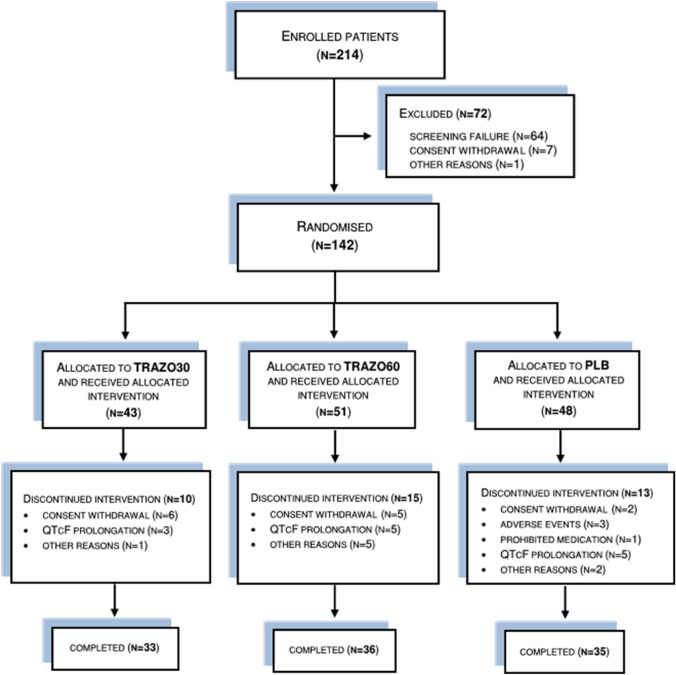
The trial was conducted from May 2017 (first patient-in) to August 2018 (last patient-out). Two hundred and fourteen patients were evaluated for eligibility, 72 patients were excluded for different reasons (64 screening failure, seven requested to be excluded, one other), while 142 patients were randomized and received the allocated treatment: 43 in the TRZ30 group, 51 in the TRZ60 group and 48 in the PLB group. One patient in the TRZ60 group was excluded from the ITT population because of the lack of a post-baseline BPI-SF evaluation. Consequently, the ITT population included 141 patients (43 in the TRZ30 group, 50 in the TRZ60 group, and 48 in the PLB group). Reasons for discontinuation as well as the number of patients completing the study, are reported in Fig. 2. Patient characteristics (Table 1), neuropathic pain efficacy measures, and mood assessments (Table 2) at baseline were similar in each treatment group and no statistically significant differences were seen.
Fig. 2.
Patient disposition. PLB placebo, QTcF Fridericia’s Correction Formula, TRZ trazodone
Table 1.
Baseline characteristics
| TRZ30 (n = 43) | TRZ60 (n = 51) | PLB (n = 48) | |
|---|---|---|---|
| Age (years), mean (SD) | 62.1 (8.55) | 63.2 (8.45) | 62.3 (7.19) |
| Sex, mean (%) | |||
| Male | 25 (58.1) | 26 (51.0) | 23 (47.9) |
| Female | 18 (41.9) | 25 (49.0) | 25 (52.1) |
| Race, mean (%) | |||
| White | 43 (100.0) | 51 (100.0) | 48 (100.0) |
| BMI, mean (SD) | 30.1 (5.47) | 30.2 (5.09) | 31.7 (5.20) |
| DN4 score, mean (SD) | 6.8 (1.33) | 7.3 (1.39) | 6.9 (1.35) |
| Concomitant disease, n (%) | |||
| Hypertension | 36 (16.4) | 38 (15) | 38 (14.5) |
| Hypercholesterolemia | 8 (3.7) | 8 (3.2) | 7 (2.7) |
| Dyslipidemia | 7 (3.2) | 11 (4.3) | 7 (2.7) |
| Obesity | 7 (3.2) | 8 (3.2) | 13 (5.0) |
| HbA1c (%), mean (SD) | 7.2 (1.18) | 7.0 (1.24) | 6.8 (1.00) |
|
GFR value, mL/min (mL/min/1.73 m2) mean (SD) |
84.7 (16.92) | 81.0 (15.09) | 87.2 (16.46) |
| Systolic blood pressure—lying position, mmHg, mean (SD) | 136.9 (15.68) | 134.6 (10.19) | 137.0 (13.96) |
| Diastolic blood pressure—lying position, mmHg, mean (SD) | 79.8 (6.96) | 81.0 (7.60) | 80.1 (8.74) |
| Heart rate—lying position, bpm, mean (SD) | 72.4 (11.89) | 70.3 (9.59) | 72.6 (11.25) |
| QTcF value, ms, mean (SD) | 423.5 (14.50) | 417.3 (18.62) | 419.5 (17.61) |
All investigational groups also received gabapentin as background therapy
BMI body mass index, bpm beats per minute, DN4 Douleur Neuropatique 4, GFR glomerular filtration rate, HbA1c glycosylated hemoglobin, PLB placebo, QTcF Fridericia’s Correction Formula, SD standard deviation, TRZ trazodone
Table 2.
Efficacy measures at baseline
| TRZ30 (n = 43) | TRZ60 (n = 50) | PLB (n = 48) | |
|---|---|---|---|
| BPI-SF | |||
| 24-h average pain (item 5), mean (SD) | 5.7 (1.01) | 5.6 (1.05) | 5.7 (1.14) |
| Pain at its worst in the last 24 h (item 3), mean (SD) | 6.7 (1.59) | 7.1 (1.54) | 6.5 (1.80) |
| Pain at its least in the last 24 h (item 4), mean (SD) | 3.7 (1.73) | 3.7 (1.88) | 4.1 (1.79) |
| Pain right now (item 6), mean (SD) | 4.9 (2.03) | 4.9 (2.08) | 4.8 (1.90) |
| Pain relief provided in the last 24 h (item 8), mean (SD) | 13.0 (21.77) | 14.0 (26.48) | 12.9 (20.42) |
| How much the pain impacted in the last 24 h on: | |||
| General activity (item 9A), mean (SD) | 5.3 (2.20) | 5.3 (1.83) | 5.3 (1.89) |
| Mood (item 9B), mean (SD) | 4.3 (2.37) | 4.4 (2.41) | 4.0 (2.14) |
| Walking ability (item 9C), mean (SD) | 5.3 (2.37) | 5.1 (2.49) | 5.4 (1.94) |
| Normal work (item 9D), mean (SD) | 4.7 (2.21) | 5.0 (2.19) | 4.9 (2.10) |
| Relations with other people (item 9E), mean (SD) | 3.6 (2.14) | 2.7 (2.30) | 2.9 (2.45) |
| Sleep (item 9F), mean (SD) | 4.8 (2.68) | 5.2 (2.25) | 5.0 (2.45) |
| Enjoyment of life (item 9G), mean (SD) | 3.9 (2.42) | 3.9 (2.67) | 3.7 (2.53) |
| NPSI | |||
| Total score, mean (SD) | 40.1 (20.75) | 42.5 (21.71) | 42.6 (18.77) |
| HAM-A | |||
| Total score, mean (SD) | 10.3 (10.06) | 8.8 (7.74) | 11.4 (10.48) |
All investigational groups also received gabapentin as background therapy
BPI-SF Brief Pain Inventory Short Form, HAM-A Hamilton Anxiety Rating Scale, NPSI Neuropathic Pain Symptom Inventory, PLB placebo, SD standard deviation, TRZ trazodone
Primary Efficacy Result
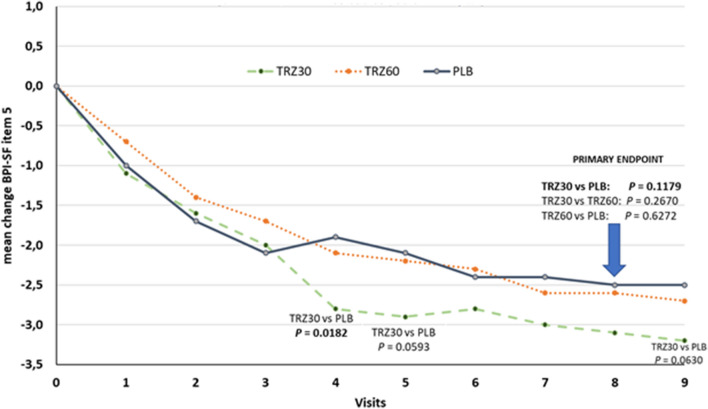
After 8 weeks of treatment, the mean ± standard deviation of the BPI-SF item 5 score was reduced from 5.7 ± 1.01 (baseline) to 2.6 ± 1.68 (visit 8) in the TRZ30 group; from 5.6 ± 1.05 (baseline) to 3.0 ± 1.86 (visit 8) in the TRZ60 group, and from 5.7 ± 1.14 (baseline) to 3.2 ± 1.80 (visit 8) in the PLB group. The mean changes were − 3.1, − 2.6, and − 2.5 in the TRZ30, TRZ60, and PLB groups, respectively. No significant (p > 0.05) differences between groups were observed. Nevertheless, a better effect was observed for TRZ30 vs PLB (95% CI − 1.30, 0.15; p = 0.1179). A statistically significant difference resulted for TRZ30 vs PLB at visit 4 (day 28) [95% CI − 1.57, − 0.15; p = 0.0182) and a strong trend was observed at visit 5 (day 35) [95% CI − 1.51, 0.03; p = 0.0593] and visit 9 (day 63) [95% CI − 1.41, 0.04; p = 0.0630] (Fig. 3). The clinical relevance of the effect showed by TRZ30 could be meaningful as it is on top of the well-known effect performed by gabapentin that was administered to all study groups as background therapy. Similarly, a numerically, but non-significantly, larger proportion of patients in the TRZ30 group (n = 27 [62.8%]) compared with the TRZ60 group (n = 27 [54%]) and the PLB group (n = 22 [45.8%]) achieved a ≥ 50% reduction in BPI-SF item 5 score (Table 3).
Fig. 3.
Change from baseline of the Brief Pain Inventory Short Form (BPI-SF) item 5 in the intention-to-treat with last observation carried forward population. Item 5 measurement: please rate your pain by circling the one number that best describes your pain on average [0-No pain; 10-Pain as bad as you can imagine]. PLB placebo, TRZ trazodone
Table 3.
Percentage of responders in the intention-to-treat (ITT) population
| ITT with LOCF population | TRZ30 (n = 43) | TRZ60 (n = 50) | PLB (n = 48) | p value |
|---|---|---|---|---|
| Responder, n (%) | 27 (62.8) | 27 (54.0) | 22 (45.8) | 0.428a |
| Non-responder, n (%) | 16 (37.2) | 23 (46.0) | 26 (54.2) |
All investigational groups also received gabapentin as background therapy
LOCF last observation carried forward, PLB placebo, TRZ trazodone
aVariables were compared by the Cochran–Mantel–Haenszel test
Secondary Efficacy Results
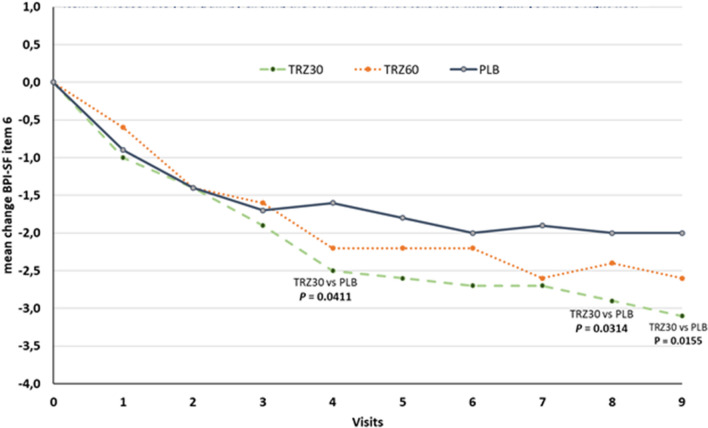
All treatment arms were similarly effective on secondary outcomes including the Neuropathic Pain Symptom Inventory, Hamilton Anxiety Rating Scale, and Patient Global Impression of Change. Among the other items of BPI-SF, statistically significant differences were observed for item 6 ‘how much pain you have right now’ for TRZ30 vs PLB at visit 4 (day 28) [95% − 1.49, − 0.03; p = 0.0411], at visit 8 (day 56) [95% − 1.54, − 0.07; p = 0.0314], and visit 9 (day 63) [95% − 1.74, − 0.19; p = 0.0155] (Fig. 4).
Fig. 4.
Change from baseline of the Brief Pain Inventory Short Form (BPI-SF) item 6 in the intention-to-treat with last observation carried forward population. Item 6 measurement: please rate your pain by circling the one number that tells how much pain you have right now [0-No pain; 10-Pain as bad as you can imagine]. PLB placebo, TRZ trazodone
Interestingly, TRZ30 achieved − 3 points pain relief on BPI items 5 and 6. What determined the different level of significance on the two items was the behavior of the PLB group, which scored − 2 points with item 5 but reached − 2.5 points with item 6. Furthermore, while the PLB curves clearly plateaued between visits 6 and 9, with both items 5 and 6, the TRZ30 curves kept on lowering, even at visit 9, as if the effect was potentiated at longer times of treatment.
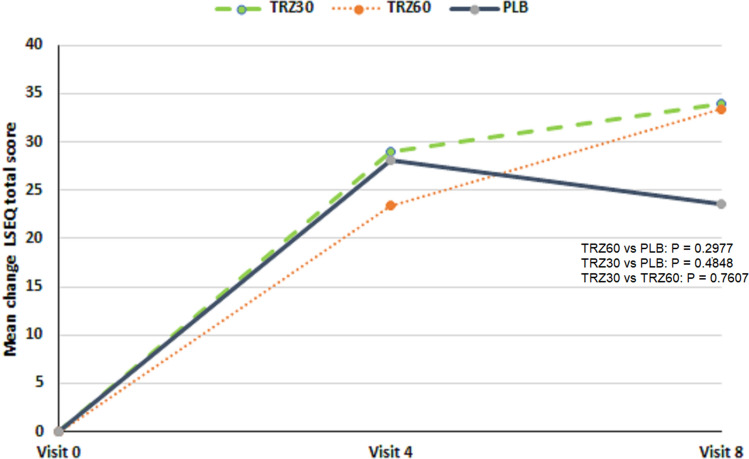
Concerning the effect on sleep, four main aspects were assessed by the Leeds Sleep Evaluation Questionnaire: the ease of getting to sleep (three items), the perceived quality of sleep (two items), the ease of awakening from sleep (two items), and the integrity of early morning behavior following wakefulness (three items). Generally, an improvement in the sleep variables was observed at visit 4 (day 28) in all treatment groups as compared with baseline. However, patients receiving TRZ reported better outcomes at visit 8 (day 56) as compared with the previous visits, even if no statistically significant difference was detected (TRZ30 vs PLB: 95% − 17.91, 37.54; p = 0.4848) (Fig. 5).
Fig. 5.
Change from baseline of the Leeds Sleep Evaluation Questionnaire (LSEQ) total score in the intention-to-treat with last observation carried forward population. PLB placebo, TRZ trazodone
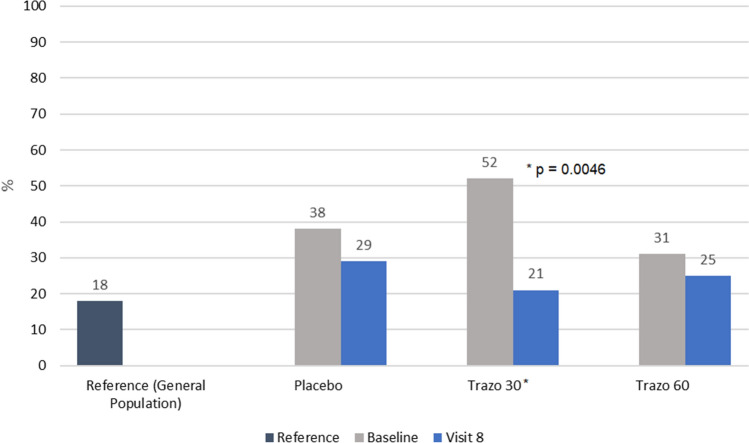
All study groups showed also an improvement in quality of life after 8 weeks of treatment. The SF-36 questionnaire measured physical functioning, role limitations attributable to physical problems, social functioning, bodily pain, general mental health, emotional problems, vitality, and general health problems. In particular, mood disturbances and vitality were restored, reaching values close to those estimated in the general population that can be used as an indirect control.
When the SF-36 questionnaire was used to assess the percentage of the positive risk for depressive disorder, a marked effect of TRZ30 on top of gabapentin as background therapy was shown in reducing the risk of depression in patients with PDN. Although at baseline a higher percentage (52%) of patients in the TRZ30 group had a positive risk for depression as compared with the TRZ60 (31%) and PLB (38%) groups, at visit 8, the percentage of risk in the TRZ30 group was reduced to 21% vs 25% in the TRZ60 group and 29% in the PLB group. Patients in the TRZ30 group showed a statistically significant reduction in this risk (p = 0.0046), reaching a value very close to the risk for depression estimated in the general population (indirect control) (18%) (Fig. 6).
Fig. 6.
Percent of patients with a positive risk for depressive disorder assessed by the SF-36 questionnaire (intention-to-treat with last observation carried forward population). TRZ trazodone
Safety and Tolerability Results
A total of 142 patients were included in the safety analysis. No serious adverse event occurred during the trial and a total of 133 treatment-emergent adverse events were recorded during the study, as displayed in Table 4.
Table 4.
Overall summary of treatment-emergent adverse events (TEAEs) in the safety population
| TRZ30 (n = 43) | TRZ60 (n = 51) | PLB (n = 48) | |
|---|---|---|---|
| TEAE, n (%) | 53 (39.8) | 35 (26.3) | 45 (33.8) |
| SAE, n (%) | 0 (0) | 0 (0) | 0 (0) |
| Patients with TEAEs, n (%) | 27 (62.8) | 21 (41.2) | 20 (41.7) |
| TEAEs leading to discontinuation, n (%) | 9 (17.0) | 6 (17.1) | 9 (20.0) |
All investigational groups also received gabapentin as background therapy
PLB placebo, SAE serious adverse event, TRZ trazodone
The most frequent treatment-emergent adverse events involved principally the nervous system disorders (28 events: ten in TRZ30, ten in TRZ60, and eight in PLB) and investigations (27 events: six in TRZ30, nine in TRZ60, and 12 in PLB) followed by gastrointestinal disorders (15 events: seven in TRZ30, three in TRZ60, and five in PLB), as summarized in Table 5.
Table 5.
Summary of the most frequent treatment-emergent adverse events (TEAEs) [≥ 5%] by system organ class
| TEAEs | TRZ30 (n = 43) | TRZ60 (n = 51) | PLB (n = 48) |
|---|---|---|---|
| Ear and labyrinth disorders, n (%) | |||
| Vertigo | 2 (3.8) | 2 (5.7) | 0 (0) |
| Gastrointestinal disorders, n (%) | |||
| Nausea | 3 (5.7) | 0 (0) | 3 (6.7) |
| General disorders, n (%) | |||
| Fatigue | 1 (1.9) | 2 (5.7) | 0 (0) |
| Peripheral swelling | 2 (3.8) | 2 (5.7) | 3 (6.7) |
| Investigations, n (%) | |||
| Electrocardiogram QT prolonged | 4 (7.5) | 5 (14.3) | 8 (17.8) |
| Metabolism and nutrition disorders, n (%) | |||
| Hypoglycemia | 1 (1.9) | 0 (0) | 3 (6.7) |
| Musculoskeletal and connective tissue disorders, n (%) | |||
| Back pain | 3 (5.7) | 2 (5.7) | 1 (2.2) |
| Nervous system disorders, n (%) | |||
| Disturbance in attention | 0 (0) | 4 (11.4) | 0 (0) |
| Dizziness | 2 (3.8) | 1 (2.9) | 5 (11.1) |
| Somnolence | 4 (7.5) | 2 (5.7) | 2 (4.4) |
All investigational groups also received gabapentin as background therapy
PLB placebo, TRZ trazodone
The safety review of laboratory (blood and urine) analysis, vital signs, ECG, and physical findings did not show any significant clinical effect of the study treatments. Some clinically significant alterations were mainly related to the underling or concomitant diseases. On the whole, a favorable safety profile of TRZ at low doses was demonstrated in this study, also when administered with a full dosage of gabapentin.
Discussion
Although this phase II, randomized controlled clinical trial, designed to evaluate the efficacy and safety of TRZ for the treatment of PDN, failed to achieve the primary endpoint (i.e., change from baseline of the BPI-SF item 5 at week 8), it showed that patients receiving low doses of TRZ combined with gabapentin reported better outcomes in all the efficacy measures, in comparison with the two other treatment groups, with a favorable safety profile.
Painful diabetic neuropathy is a multi-factorial condition as several pathophysiological mechanisms can simultaneously occur and influence the onset and the course of symptoms. So far, just a few medications proved to be efficacious in the treatment of PDN, owing to the very high rate of failure of clinical trials in the field of chronic pain partially driven by an increasing placebo effect [24]. Accordingly, TRZ, a drug with a multi-modal mechanism of action, approved for the treatment of depression in several countries, is suggested as an alternative treatment for pain relief by the NICE Clinical Guideline Neuropathic pain—Pharmacological Management [7].
The primary efficacy result, i.e., the BPI-SF item 5 score after 8 weeks of treatment, was similar across the three treatment groups. We hypothesize that our randomized controlled clinical trial failed to achieve the primary endpoint possibly owing to the open-label background therapy with gabapentin contributing to the overall improvement of pain measures.
We believe, however, that our clinical trial may support the effect of TRZ in patients with PDN because we found that patients treated with the low dose of TRZ reported better BPI-SF outcomes in comparison with gabapentin. Similarly, a larger proportion of patients in the TRZ30 group (62.8%) achieved a ≥ 50% reduction in BPI-SF item 5 score, in comparison with patients treated with gabapentin only (45.8%).
Our randomized controlled clinical trial demonstrated that low doses of TRZ combined with gabapentin significantly improved depression, sleep, and several BPI-SF items, including the BPI-SF item 6 (i.e., how much pain you have right now). The risk of depression, as assessed with the SF-36 questionnaire, was significantly lower in patients treated with TRZ30 than in patients treated with gabapentin only. This finding may have an important clinical interest, given the well-known association between neuropathic pain and depression [25]. We found that patients receiving TRZ reported favorable sleep outcomes (though this effect was similar across the three groups); our study, therefore, supports previous evidence showing that low doses of TRZ improve sleep. This effect might be particularly important in the clinical management of PDN, given the close association between neuropathic pain and sleep disturbances [26]. Trazodone, unique among antidepressants, has a mixed serotonergic and adrenolytic activity effective for multiple disorders including insomnia and anxiety [12, 27]. At doses lower than those used for the treatment of depression, the hypnotic effect is thought to be attributed to the antagonism of 5-HT2A receptors, histamine H1 receptors, and α1-adrenergic receptors [13].
Our randomized controlled clinical trial showed that TRZ has a favorable safety profile, also when combined with a relatively high dosage of gabapentin. The frequency of adverse events, abnormal laboratory analysis, vital signs, ECG, and physical findings was similar across the three treatment groups.
Previous studies described QT prolongation in patients treated with trazodone [28]. However, in our trial, we found that the frequency of QT prolongation was lower in the TRZ groups (TRZ30: 7.5%; TRZ60: 14.3%) than in the gabapentin group (17.8%). Whereas the other commonly used antidepressants for neuropathic pain (e.g., tricyclic antidepressants) are associated with a distinctive risk for QT prolongation, only a high TRZ dosage affects the QT interval [29]. The cardiovascular safety of TRZ might be clinically important, given the frequent comorbidities and multiple treatments of patients with PDN.
How TRZ might be effective for treating pain remains a possibly controversial problem. Trazodone is a potent 5-HT2A antagonist. Animal studies showed that experimental nerve injuries provoke the upregulation of the 5-HT2A receptor in dorsal horn neurons promoting spinal hyperexcitation [17]. Recent studies suggested a cross-talk mechanism between 5-HT2A and mGlu2/3 receptors both in the brain and in the spinal cord [18, 19]. In particular, in the spinal cord, mGlu2/3 and 5-HT2A receptors colocalize at a presynaptic level and 5-HT2A antagonists trigger positive allosteric modulations of mGlu2/3 autoreceptors in controlling glutamate exocytosis [19]. Accordingly, TRZ might modulate nociceptive second-order activation and thus reduce pain. The functional interaction between 5-HT2A and mGlu2/3 receptors could be specifically elicited by low doses of TRZ, probably owing to specific properties of TRZ pharmacological action on the 5-HT2A receptor. The receptor binding profile of TRZ shows that increasing doses, beyond the saturation of 5-HT2A receptors, recruits additional pharmacological actions, specifically blockade of α1-adrenergic receptors and H1 receptors as well [15]. Further investigations into the mechanism of action of TRZ at the spinal level are ongoing and further clinical studies could be useful to assess the effect of even lower doses of TRZ for treating neuropathic pain.
Limitations
In this clinical trial, we did not calculate a precise sample size estimation, thus increasing the risk that this study was not able to test the hypotheses of interest. It follows that we cannot exclude that the study failed to achieve the primary endpoint because of a low statistical power.
We used the last observation carried forward method for handling missing data in the ITT population. Admittedly, this approach may affect our findings, producing a bias in the treatment estimation [30]. However, last observation carried forward is commonly used in explorative phase II trials, and a more conservative approach such as the baseline observation carried forward method is specifically useful in conditions with a spontaneous improvement over the course of the study.
In our study, about 27% of patients did not complete the study (without differences across the three treatment groups). The most frequent reasons for discontinuation were the withdrawal of consent (13 patients) and the QT prolongation (13 patients). The demanding weekly study procedures probably reduced the patients’ willingness to participate in the clinical trial and influenced the drop-out rate. In this trial, we applied stringent ECG safety criteria, thus probably causing a high frequency of discontinuation for the QT prolongation. At each study visit, the QT interval was calculated and corrected according to Fridericia’s Correction Formula. Any Fridericia’s Correction Formula value > 450 ms (male) or 470 ms (female) resulted in patient discontinuation, though no patient reported any cardiac symptoms or signs.
Conclusions
This is the first randomized clinical trial collecting data on the efficacy and safety of low doses of TRZ compared to PLB over a background treatment with gabapentin in patients affected by PDN. Although this clinical trial failed to achieve the primary endpoint, all efficacy results consistently favored TRZ 10 mg t.i.d. (TRZ30) on top of gabapentin as background therapy. These findings, therefore, suggest the potential benefit of low doses of TRZ for treating patients with PDN and support further adequately powered confirmatory trials investigating the efficacy of TRZ.
Acknowledgements
The authors thank all investigators and staff involved in the conduct of this clinical trial. For Czech Republic: Edvard Ehler (Nemocnice Pardubického kraje a.s., Pardubice); Markéta Ceé (Neurologická ambulance. Litoměřice); Ladislav Pazdera (Vestra Clinics s.r.o., Rychnov nad Kněžnou); Dagmar Bartášková (Diabetologická ambulance Milan Kvapil s.r.o., Prague); Karel Zinek (Neurosanatio s.r.o., Litomyšl); Danuše Roubcová (MP-neuro s.r.o., Ostrava); Martin Vališ (NEUROHK s.r.o., Choceň). For Hungary: Mihály Dudás (Békés Megyei Központi Kórház Pándy Kálmán Tagkórház, Gyula); Mihály Gurzó (Bács-Kiskun Megyei Kórház, Kecskemét); Eleonóra Harcsa (Semmelweis Egyetem ÁOK, Budapest); István Takács (Semmelweis Egyetem ÁOK, Budapest); Róbert Takács (Szent-Györgyi Albert Klinikai Központ, Szeged); János Tibor Kis (Budai Irgalmasrendi Kórház Belgyógyászati Centrum, Budapest). For Poland: Ilona Palka-Kisielowska (Silmedic Sp. z o.o., Katowice); Katarzyna Kłodawska (NBR Polska Tomasz Kłodawski, Warszawa); Marcin Nastaj (NZOZ Neuromed M. i M. Nastaj Sp. P., Lublin); Bożena Zapęcka- Dubno (Medycyna Kliniczna, Warszawa); Danuta Wrońska (Pro Familia Altera Poradnia Wielospecjalistyczna, Katowice); Małgorzata Fengler-Czeczko (RCMed Oddział Sochaczew, Sochaczew); Anna Ocicka-Kozakiewicz (Nasz Lekarz Przychodnie Medyczne, Toruń).
Declarations
Funding
This study was sponsored by Angelini Pharma S.p.A. (S. Palomba, Pomezia, Rome, Italy). Open access funding provided by Università degli Studi di Roma La Sapienza within the CRUI-CARE Agreement
Conflict of Interest
Giorgio Cruccu received personal fees for advisory boards or consultancy from Angelini, Grunenthal, and Lilly, and personal fees for educational activity by PTS Global Services. Andrea Truini received honoraria for speaking at symposia or research financial supports from Alpha-Sigma, Angelini Pharma, Epitech, FB Health, Pfizer, and Grunenthal. Edvard Ehler has no conflicts of interest that are directly relevant to the content of this study; however, his institution received a fee for conducting the clinical trial from Angelini Pharma S.p.A. Marcin Nastaj and Ilona Palka-Kisielowska received principal investigator fees from Angelini Pharma S.p.A. Fabrizio Calisti, Agnese Cattaneo, Alessandro Comandini, Alessandra Del Vecchio, Giorgio Di Loreto, Paola Lipone, and Ilena Pochiero are full-time employees of Angelini Pharma S.p.A.
Ethics Approval
The study was approved by the competent authorities and applicable ethics committees of Czech Republic, Hungary, and Poland and was conducted in accordance with Good Clinical Practice guidelines and ethical standards as laid down in the 1964 Declaration of Helsinki.
Consent for Publication
All authors consent to the publication of the manuscript and accept the terms of related agreement.
Consent to Participate
Written informed consent was obtained from all individual participants included in the study prior to starting any study-related procedure.
Availability of Data and Material
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Code Availability
Not applicable.
Author Contributions
Giorgio Cruccu, Andrea Truini, Paola Lipone, Alessandra Del Vecchio, Giorgio Di Loreto, Fabrizio Calisti, and Alessandro Comandini contributed to the study conception and design. Giorgio Di Loreto carried out the statistical analysis of the study. Edvard Ehler, Marcin Nastaj, and Ilona Palka-Kisielowska contributed to the study management and data collection. Ilena Pochiero supervised operational aspects of the trial and data collection. Agnese Cattaneo reviewed and commented on the study results. The first draft of the manuscript was written by Paola Lipone and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
References
- 1.Schreiber AK, Nones CF, Reis RC, Chichorro JG, Cunha JM. Diabetic neuropathic pain: physiopathology and treatment. World J Diabetes. 2015;6(3):432–444. doi: 10.4239/wjd.v6.i3.432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tesfaye S, Wilhelm S, Lledo A, Schacht A, Tolle T, Bouhassira D, et al. Duloxetine and pregabalin: high-dose monotherapy or their combination? The ‘COMBO-DN Study’: a multinational, randomized, double-blind, parallel group study in patients with diabetic peripheral neuropathic pain. Pain. 2013;154(12):2616–2625. doi: 10.1016/j.pain.2013.05.043. [DOI] [PubMed] [Google Scholar]
- 3.Schmader KE. Epidemiology and impact on quality of life of postherpetic neuralgia and painful diabetic neuropathy. Clin J Pain. 2002;18(6):350–354. doi: 10.1097/00002508-200211000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Blesneac I, Themistocleous AC, Fratter C, Conrad LJ, Ramirez JD, Cox JJ, et al. Rare NaV1.7 variants associated with painful diabetic peripheral neuropathy. Pain. 2018;159(3):469–480. doi: 10.1097/j.pain.0000000000001116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gore M, Brandenburg NA, Dukes E, Hoffman DL, Tai KS, Stacey B. Pain severity in diabetic peripheral neuropathy is associated with patient functioning, symptom levels of anxiety and depression, and sleep. J Pain Symptom Manag. 2005;30:374–385. doi: 10.1016/j.jpainsymman.2005.04.009. [DOI] [PubMed] [Google Scholar]
- 6.Tesfaye S, Selvarajah D. Advances in the epidemiology, pathogenesis and management of diabetic peripheral neuropathy. Diabetes Metab Res Rev. 2012;28(Suppl. 1):8–14. doi: 10.1002/dmrr.2239. [DOI] [PubMed] [Google Scholar]
- 7.Centre for Clinical Practice at NICE (UK). Neuropathic pain: the pharmacological management of neuropathic pain in adults in non-specialist settings. National Institute for Health and Care Excellence (UK). Clinical Guidelines 173, November 2013, last updated July 2019. [PubMed]
- 8.Tesfaye S, Vileikyte L, Rayman G, Sindrup S, Perkins B, Baconja M, On Behalf of the Toronto Expert Panel on Diabetic Neuropathy et al. Painful diabetic peripheral neuropathy: consensus recommendations on diagnosis, assessment and management. Diabetes Metab Res Rev. 2011;27:629–638. doi: 10.1002/dmrr.1225. [DOI] [PubMed] [Google Scholar]
- 9.Dworkin RH, O’Connor AB, Audette J, Baron R, Gourlay GK, Haanpää ML, et al. Recommendations for the pharmacological management of neuropathic pain: an overview and literature update. Mayo Clin Proc. 2010;85(3 Suppl.):S3–S14. doi: 10.4065/mcp.2009.0649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sawnyok J, Esser MJ, Reid AR. Antidepressants as analgesics: an overview of central and peripheral mechanisms of action. J Psychiatry Neurosci. 2001;26:21–29. [PMC free article] [PubMed] [Google Scholar]
- 11.Marks DM, Shah MJ, Patkar AA, Masand PS, Park GY, Pae CU. Serotonin–norepinephrine reuptake inhibitors for pain control: premise and promise. Curr Neuropharmacol. 2009;7(4):331–336. doi: 10.2174/157015909790031201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fagiolini A, Comandini A, Catena Dell’Osso M, Kasper S. Rediscovering trazodone for the treatment of major depressive disorder. CNS Drugs. 2012;26(12):1033–1049. doi: 10.1007/s40263-012-0010-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stahl SM. Mechanism of action of trazodone: a multifunctional drug. CNS Spectr. 2009;14(10):536–546. doi: 10.1017/S1092852900024020. [DOI] [PubMed] [Google Scholar]
- 14.Owens MJ, Morgan WN, Plott SJ, Nemeroff CB. Neurotransmitter receptor and transporter binding profile of antidepressants and their metabolites. J Pharmacol Exp Ther. 1997;283:1305–1322. [PubMed] [Google Scholar]
- 15.Stahl SM. Basic psychopharmacology of antidepressants, part 1: antidepressants have seven distinct mechanism of action. J Clin Psychiatry. 1998;59(Suppl. 4):5–14. [PubMed] [Google Scholar]
- 16.Stahl SM. Essential psychopharmacology of depression and bipolar disorder. 2. New York: Cambridge University Press; 2000. [Google Scholar]
- 17.Aira Z, Buesa I, Gallego M, García del Caño G, Mendiable N, Mingo J, et al. Time-dependent cross talk between spinal serotonin 5-HT2A receptor and mGluR1 subserves spinal hyperexcitability and neuropathic pain after nerve injury. J Neurosci. 2012;32(39):13568–13581. doi: 10.1523/JNEUROSCI.1364-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Delille HK, Becker JM, Burkhardt S, Bleher B, Terstappen GC, Schmidt M, et al. Heterocomplex formation of 5-HT2A-mGlu2 and its relevance for cellular signaling cascades. Neuropharmacology. 2012;62(7):2184–2191. doi: 10.1016/j.neuropharm.2012.01.010. [DOI] [PubMed] [Google Scholar]
- 19.Olivero G, Grilli M, Vergassola M, Bonfiglio T, Padolecchia C, Garrone B, et al. 5-HT2A-mGlu2/3 receptor complex in rat spinal cord glutamatergic nerve endings: a 5-HT2A to mGlu2/3 signalling to amplify presynaptic mechanism of auto-control of glutamate exocytosis. Neuropharmacology. 2018;133:429–439. doi: 10.1016/j.neuropharm.2018.02.030. [DOI] [PubMed] [Google Scholar]
- 20.Khurana RC. Treatment of painful diabetic neuropathy with trazodone. JAMA. 1983;250(11):1392. doi: 10.1001/jama.1983.03340110016015. [DOI] [PubMed] [Google Scholar]
- 21.Wilson RC. The use of low dose trazodone in the treatment of painful diabetic neuropathy. J Am Podiatr Med Assoc. 1999;89(9):468–471. doi: 10.7547/87507315-89-9-468. [DOI] [PubMed] [Google Scholar]
- 22.Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singap. 1994;23:129–138. [PubMed] [Google Scholar]
- 23.Zelman DC, Gore M, Dukes E, Tai KS, Brandenburg N. Validation of a modified version of the brief pain inventory for painful diabetic peripheral neuropathy. J Pain Symptom Manag. 2005;29(4):401–410. doi: 10.1016/j.jpainsymman.2004.06.018. [DOI] [PubMed] [Google Scholar]
- 24.Finnerup NB, Haroutounian S, Baron R, Dworkin RH, Gilron I, Haanpaa M, et al. Neuropathic pain clinical trials: factors associated with decreases in estimated drug efficacy. Pain. 2018;159(11):2339–2346. doi: 10.1097/j.pain.0000000000001340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sheng J, Liu S, Wang Y, Cui R, Zhang X. The Link between Depression and Chronic Pain: Neural Mechanisms in the Brain. Neural Plast. 2017;2017:9724371. [DOI] [PMC free article] [PubMed]
- 26.Ferini-Strambi L. Neuropathic Pain and Sleep: A Review. Pain Ther. 2017;6(Suppl 1):19–23. [DOI] [PMC free article] [PubMed]
- 27.Bossini L, Casolaro I, Koukouna D, Cecchini F, Fagiolini A. Off-label uses of trazodone: a review. Expert Opin Pharmacother. 2012;13(12):1707–17. [DOI] [PubMed]
- 28.Carvalho AF, Sharma MS, Brunoni AR, Vieta E, Fava GA. The safety, tolerability and risks associated with the use of newer generation antidepressant drugs: a critical review of the literature. Psychother Psychosom. 2016;85(5):270–288. doi: 10.1159/000447034. [DOI] [PubMed] [Google Scholar]
- 29.Karki BR, Prasai P, Ruhela A, Sedhai YR. Trazodone Overdose-Induced Prinzmetal's Angina Pectoris. Proc (Bayl Univ Med Cent) 2019;33(1):75–76. [DOI] [PMC free article] [PubMed]
- 30.Lachin JM. Fallacies of last observation carried forward analyses. Clin Trials. 2016;13(2):161–168. doi: 10.1177/1740774515602688. [DOI] [PMC free article] [PubMed] [Google Scholar]