Abstract
Objective:
To compare the risk of ectopic pregnancy among women with and women without antidepressant prescriptions around conception and examine whether this risk differs by prepregnancy depression status.
Methods:
We conducted a cohort study of all pregnancies between November 1, 2008, and September 30, 2015, identified in the nationwide (American) IBM® MarketScan® Databases. At least one day’s supply of antidepressants in the 3 weeks after a woman’s last menstrual period defined active antidepressant use around conception. At least one depression diagnosis in the year before the last menstrual period defined prepregnancy depression. Relative risk (RR) of ectopic pregnancy was estimated using unadjusted and inverse probability of treatment (IPT)-weighted log-binomial models.
Results:
Of the 1,703,245 pregnancies, 106,788 (6.3%) women had a prepregnancy depression diagnosis. Among women with a depression diagnosis, 40,287 (37.7%) had an active antidepressant prescription around conception; the IPT-weighted risk of ectopic pregnancy was similar among women who did and did not fill an antidepressant prescription around conception (IPT-weighted RR = 1.01; 95% CI, 0.93 to 1.10). Overall, the risk of ectopic pregnancy was higher among women who had a prepregnancy depression diagnosis than women who did not have a prepregnancy depression diagnosis (IPT-weighted RR = 1.09; 95% CI, 1.04 to 1.15).
Conclusions:
This study’s findings suggest that women who have a prepregnancy depression diagnosis are at a slightly increased risk of ectopic pregnancy, and among women who have a prepregnancy depression diagnosis, the use of antidepressants around conception does not increase the risk of ectopic pregnancy.
Keywords: antidepressants, depression, ectopic pregnancy, cohort
Abstract
Objectif :
Comparer le risque de grossesse ectopique chez les femmes ayant et n’ayant pas de prescriptions d’antidépresseurs en période de conception, et examiner si le risque diffère selon l’état de la dépression pré-grossesse.
Méthodes :
Nous avons mené une étude de cohorte de toutes les grossesses entre le 1 er novembre 2008 et le 30 septembre 2015 identifiées à l’échelle nationale (américaine) dans les bases de données IBM® MarketScan®. Un approvisionnement d’au moins un jour d’antidépresseurs dans les trois semaines suivant les dernières menstruations d’une femme définissait l’utilisation active d’antidépresseurs en période de conception. Au moins un diagnostic de dépression dans l’année précédant les dernières menstruations définissait la dépression pré-grossesse. Le risque relatif (RR) de grossesse ectopique était estimé à l’aide de modèles log-binomiaux pondérés de probabilité non ajustée et de probabilité inverse de traitement (PIT).
Résultats :
Sur les 1 703 245 grossesses, 106 788 femmes (6,3 %) ont eu un diagnostic de dépression pré-grossesse. Chez les femmes ayant reçu un diagnostic de dépression, 40 287 (37,7 %) avaient une prescription d’antidépresseurs en période de conception; le risque de grossesse ectopique pondéré selon la PIT était semblable chez les femmes qui avaient et n’avaient pas fait remplir une prescription d’antidépresseurs en période de conception (RR pondéré selon la PIT = 1,01; IC à 95 % 0,93 à 1,10). En général, le risque de grossesse ectopique était plus élevé chez les femmes ayant reçu un diagnostic de dépression prégrossesse que chez celles qui n’avaient pas reçu de diagnostic de dépression pré-grossesse (RR pondéré selon la PIT = 1,09; IC à 95 % 1,04 à 1,15).
Conclusions :
Les résultats de cette étude suggèrent que les femmes qui ont un diagnostic de dépression pré-grossesse sont à risque légèrement accru d’une grossesse ectopique, et parmi les femmes qui ont un diagnostic de dépression pré-grossesse, l’utilisation d’antidépresseurs en période de conception n’accroît pas le risque de grossesse ectopique.
Introduction
Approximately 126,000 of the 6.3 million annual recognized pregnancies in the United States are ectopic.1,2 Ectopic pregnancies often result in complications, and if left untreated or treated too late, they can be fatal.3–5 There are several known risk factors for ectopic pregnancy, including pelvic infections, use of reproductive technology, intrauterine devices, smoking, and older age; however, around half of ectopic pregnancies occur in women who do not have a known risk factor.6–12 Unstudied but potential risk factors for ectopic pregnancy could include antidepressant use around conception and depression.
Most ectopic pregnancies (>98%) implant in the fallopian tube; these early implantations are thought to be a result of changes to smooth muscle contractions and ciliary beating in the fallopian tube.13–15 Selective serotonin reuptake inhibitors (SSRIs) have stimulating effects on smooth muscle cells in the fallopian tube.16 Additionally, antidepressants potentially affect cilia function in the fallopian tubes through nitric oxide modulation.17,18 A recent study using employer-based claims between 2008 and 2013 found that more than 15% of reproductive-age women filled at least one antidepressant prescription in a 1-year period.19 It is known that women who use antidepressants in pregnancy are at increased risk of adverse pregnancy outcomes such as spontaneous abortion, preterm birth congenital malformations, neonatal adaptation, and persistent pulmonary hypertension of the newborn.20–23 Despite their common use and plausible mechanism, it is unknown whether antidepressant use around conception increases the risk of ectopic pregnancy.
Using American cross-sectional data from 2007 to 2014, a study of 3,705 nonpregnant women of reproductive age found that almost 5% had major depression, and more than 4% had minor depression.24 Although no study to date has examined the risk of ectopic pregnancy specifically for women with depression, a German study found that women with psychiatric conditions—including depression, anxiety, adjustment disorder, and somatoform disorders—were at 1.8 times higher risk of ectopic pregnancy than women without psychiatric conditions.25 They suggest that psychiatric conditions increase stress, which has been shown to exacerbate endometriosis and inflammation in animal models and could increase risk of ectopic pregnancy.26
To gain insight into potential associations between antidepressant use around conception, prepregnancy depression, and risk of ectopic pregnancy, we conducted a cohort study using a large national database of privately insured women in the United States. Specifically, among women who had a prepregnancy depression diagnosis, we examined whether those who had an active antidepressant prescription around conception were at increased risk of ectopic pregnancy, and whether specific types of antidepressants had differing effects on risk of ectopic pregnancy. Next, we examined whether women who had a prepregnancy depression diagnosis (regardless of antidepressant use around conception) were at increased risk of ectopic pregnancy. Third, we assessed whether the use of antidepressants among women without a prepregnancy depression diagnosis affected the risk of ectopic pregnancy.
Methods
Materials and Study Population
We used the IBM® MarketScan® Research Databases (MarketScan) to identify a cohort of women who became pregnant. MarketScan is a large administrative claims database including information on a portion of the U.S. population covered by employer-sponsored insurance.27 Through an individual identifier across data sets, we were able to link inpatient services, outpatient services, outpatient pharmacy prescription claims, and healthcare plan enrollment information.
Pregnancies were identified using International Classification of Diseases (ICD-9) diagnosis and procedure codes, Diagnosis Related Group codes, Current Procedural Terminology codes, and Healthcare Common Procedure Coding System codes from inpatient and outpatient services, and National Drug Codes (NDC) from outpatient pharmaceutical claims.1,28,29 Due to lack of information on when a pregnancy began, we used an algorithm to estimate the last menstrual period; this algorithm estimates ectopic pregnancy to end at 56 days gestation and intrauterine pregnancies to end between 56 and 301 days gestation.28,30 Gestational age is defined based on the specific diagnoses included in the claims data; however, not all claims include information that can be used to estimate gestational age. In cases with nonspecific claims, live births are estimated to occur at 40-week gestation.28 Detailed information on identification of pregnancies in the MarketScan database is provided in Supplemental Tables S1 to S4.
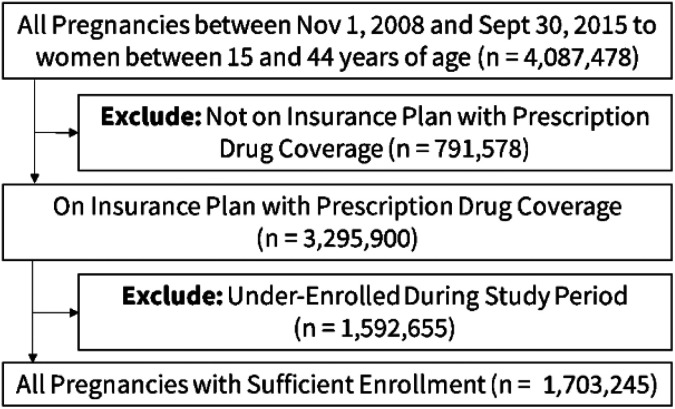
The cohort included pregnancies identified in the Marketscan databases between November 1, 2008, and September 30, 2015, among women aged 15 to 44. We excluded women whose insurance plan did not include prescription drug coverage and women who did not have continuous insurance coverage in the year before to 1 month after their last menstrual period. Our final cohort included 1,703,245 pregnancies (Figure 1).
Figure 1.
Cohort selection process.
Measures
Antidepressant prescriptions were identified from outpatient pharmacy files through NDC and generic drug names and divided into 4 classes of drugs: SSRIs, serotonin-norepinephrine reuptake inhibitor (SNRI), tricyclic antidepressants (TCAs), and other (see Table S5 in Supplemental Materials for complete list of drugs).31 To capture pregnancies with active antidepressant use around conception, we defined exposure as having an antidepressant prescription that had at least a 1-day supply in the 3 weeks after a woman’s estimated last menstrual period. An active antidepressant is identified by the dispensation date and number of days’ supply. This definition was selected as ovulation generally occurs 11 to 21 days after the start of a woman’s last menstrual cycle.32
Prepregnancy depression was defined as having at least one diagnosis of depression in the year before their last menstrual period. Depression diagnoses were obtained from inpatient and outpatient claims and identified through ICD-9 diagnosis codes (296.2x, 296.3x, 298.0x, 300.4x, 309.1x, or 311.xx).33
Statistical Analysis
We first examined whether women who had a prepregnancy depression diagnosis, who had an active antidepressant prescription around conception (i.e., 3 weeks after their last menstrual period) were at higher risk of ectopic pregnancy than women who had a prepregnancy depression diagnosis and did not have an active antidepressant prescription around conception. To do this, we examined ectopic pregnancy risk differences per 10,000 pregnancies and relative risks (RRs) of ectopic pregnancy, which were estimated using log-linked binomial models, for any antidepressant and by class. When examining specific classes of antidepressants, the reference group was women who did not fill a prescription for that specific class of antidepressant, meaning they could be exposed to an antidepressant, just not that class.
Next, we examined whether women who had a prepregnancy depression diagnosis were at increased risk of ectopic pregnancy compared to women with no prepregnancy depression diagnosis. Again, we examined ectopic pregnancy risk differences per 10,000 pregnancies and RRs of ectopic pregnancy, estimated using log-linked binomial models.
Lastly, we examined the risk of ectopic pregnancy among women who used antidepressants around conception but did not have a prepregnancy depression diagnosis. The most common use of antidepressants is to treat depression; however, antidepressants are also used to treat other conditions, such as anxiety and panic disorders and obsessive-compulsive disorder, and are used adjunctively for bipolar depression.34 Again, we used log-linked binomial regression models to examine the risk of ectopic pregnancy for those who had an antidepressant prescription around conception (any antidepressant prescription and prescription from each specific class).
To reduce bias from confounding in our RR estimates, we applied high-dimensional propensity score adjustments to each of our RR estimates. High dimensional propensity scores are derived from a multistep algorithm that identifies potential confounders from a database by selecting variables correlated to both the exposure and outcome, prioritizing covariates by prevalence and potential for bias.35,36 Covariates were drawn from three data dimensions in the year before a woman’s last menstrual period: (1) inpatient and outpatient diagnostic codes (3-digit ICD-9-CM codes), (2) inpatient and outpatient procedure codes (4-digit ICD-9-CM codes), and (3) outpatient prescription medication claims (11-digit NDCs).35–37 The inclusion of near-instruments in the high-dimensional propensity score model could amplify bias; thus, we excluded antidepressant use and depression diagnoses from the high-dimensional propensity score dimensions.38 In addition to the health variables obtained from these data, we also included the year of pregnancy (2007 to 2011, 2012 to 2015), women’s age at the end of the pregnancy (15 to 19, 20 to 24, 25 to 29, 30 to 34, 35 to 39, 40 to 44), and 5 predefined conditions identified as being risk factors for ectopic pregnancy: pelvic infections, sexually transmitted infections, assisted reproductive technology, intrauterine devices, and smoking in the year before a woman’s last menstrual period;39–43 codes used to define these variables are presented in Supplemental Table S6.
High-dimensional propensity scores were estimated using demographic and predefined conditions, as well as the top 500 covariates selected from the health databases. These high-dimensional propensity scores were then used to derive inverse probability of treatment (IPT) weights, and weights were stabilized. To minimize the influence of outlier weights, stabilized IPT weights were truncated beyond the prespecified range of 0.10 and 10.44 To examine whether the high-dimensional propensity scores balanced the covariates in our unexposed and exposed groups, unweighted and weighted standardized differences are presented in Supplemental Tables S7 to S17; covariates are considered balanced if the standardized difference is less than 0.25.45 All data management, programming, and analyses were performed using SAS, version 9.4.46
Results
In our study of 1,703,245 women who were pregnant, 106,788 (6.3%) were diagnosed with depression in the year before conception. Among women with a depression diagnosis, 40,287 (37.7%) had an active antidepressant prescription around conception. Women with a prepregnancy depression diagnosis who had an active antidepressant prescription around conception were more likely to be 30 years or older at the time of their pregnancy and to have a comorbid anxiety diagnosis than women who had a prepregnancy depression diagnosis and did not have an active antidepressant prescription around conception (Table 1).
Table 1.
Baseline Characteristics among Women Who Had a Depression Diagnosis in the Year Before Conception, by Antidepressant Prescription Status around Conception.
| Characteristics at the End of Pregnancy | Had an Antidepressant Prescription around Conception (n = 40,287) | Did Not Have an Antidepressant Prescription around Conception (n = 66,501) | Unweighted Standardized Differences | IPT-Weighted Standardized Differences |
|---|---|---|---|---|
| n (%) | n (%) | |||
| Age | ||||
| 15 to 19 | 2,197 (5.45) | 6,332 (9.52) | 0.16 | 0.00 |
| 20 to 24 | 4,569 (11.34) | 10,176 (15.3) | 0.12 | 0.00 |
| 25 to 29 | 8,944 (22.2) | 14,966 (22.5) | 0.01 | 0.00 |
| 30 to 34 | 13,099 (32.51) | 19,540 (29.38) | 0.07 | 0.00 |
| 35 to 39 | 8,774 (21.78) | 12,069 (18.15) | 0.09 | 0.00 |
| 40 to 44 | 2,704 (6.71) | 3,418 (5.14) | 0.07 | 0.00 |
| Year | ||||
| 2008 to 2011 | 17,452 (43.32) | 29,009 (43.62) | 0.01 | 0.00 |
| 2012 to 2015 | 22,835 (56.68) | 37,492 (56.38) | 0.01 | 0.00 |
| Medical conditions in the year before a woman’s last menstrual period | ||||
| Sexually transmitted infection | 768 (1.91) | 1,523 (2.29) | 0.03 | 0.00 |
| Assisted reproductive technology | 268 (0.67) | 478 (0.72) | 0.01 | 0.00 |
| Pelvic infection | 373 (0.93) | 751 (1.13) | 0.02 | 0.00 |
| Intrauterine device | 2,060 (5.11) | 3,401 (5.11) | 0.00 | 0.00 |
| Smoking | 2,884 (7.16) | 4,953 (7.45) | 0.01 | 0.00 |
| Health in the year before a woman’s last menstrual perioda | ||||
| ICD-9 Diagnosis Code 300: Anxiety | 15,684 (38.93) | 19,417 (29.2) | 0.21 | 0.00 |
| ICD-9 Diagnosis Code 401L Essential hypertension | 2,797 (6.94) | 3,711 (5.58) | 0.06 | 0.00 |
| ICD-9 Diagnosis Code 616: Inflammatory disease of cervix vagina and vulva | 4,531 (11.25) | 9,055 (13.62) | 0.07 | 0.00 |
| NDC Code 00093-0074-01: Zolpidem tartrate | 1,678 (4.17) | 1,612 (2.42) | 0.10 | 0.01 |
| NDC code 59746-0001-03: Methylprednisolone | 1,554 (3.86) | 1,763 (2.65) | 0.07 | 0.00 |
Note. n = 106,788. ICD-9 = International Classification of Diseases, 9th edition; NDC = National Drug Codes; HDPS = high dimensional propensity score; IPT = inverse probability of treatment.
a This table presents the top 5 health variables included in the HDPS model—see Supplemental Table S7 for the top 60 health variables included in the HDPS model; ICD-9 diagnosis and procedure codes from Inpatient and Outpatient Services, NDC codes for Outpatient Pharmaceutical Claims.
Among women who had a prepregnancy depression diagnosis, the risk of ectopic pregnancy was similar for women who had an antidepressant prescription around conception and women who did not have an antidepressant prescription around conception (IPT-weighted RR = 1.01; 95% CI, 0.93 to 1.10; Table 2). However, there were 115 excess ectopic pregnancies per 10,000 pregnancies among women who had an active TCA prescription around conception compared to women who did not fill a prescription for TCAs around conception (IPT-weighted RR = 1.44; 95% CI, 1.00 to 2.06).
Table 2.
Frequency and Relative Risk of Ectopic Pregnancy by Antidepressant Use around Conception Among Women with a Depression Diagnosis in the Year Before Conception.
| Antidepressant Use around Conception | Had Prescription | Did Not Have Prescription | Risk Differenceb (95% CI) | Relative Risk (95% CI) | |||
|---|---|---|---|---|---|---|---|
| N | Eventsa (Riskb) | N | Eventsa (Riskb) | Crude | IPT-Weighted | ||
| Any Antidepressant | 40,287 | 887 (220) | 66,501 | 1,402 (211) | 9 (−9 to 27) | 1.04 (0.96 to 1.13) | 1.01 (0.93 to 1.10) |
| Specific type | |||||||
| Any SSRI | 28,434 | 608 (214) | 78,354 | 1,681 (215) | −1 (−20 to 19) | 1.00 (0.91 to 1.09) | 0.99 (0.90 to 1.08) |
| Any SNRI | 6,620 | 154 (233) | 100,168 | 2,135 (213) | 19 (−18 to 57) | 1.09 (0.93 to 1.28) | 0.96 (0.81 to 1.14) |
| Any TCA | 1,037 | 34 (328) | 105,751 | 2,255 (213) | 115 (6 to 223) | 1.54 (1.10 to 2.15) | 1.44 (1.00 to 2.06) |
| Any Other | 9,432 | 204 (216) | 97,356 | 2,085 (214) | 2 (−29 to 33) | 1.01 (0.88 to 1.16) | 0.93 (0.80 to 1.08) |
Note. n = 106,788. Women can have active prescriptions for more than one type of antidepressant. For each specific antidepressant, the comparison group is women who did not fill a prescription for that specific antidepressant. SSRI = selective serotonin reuptake inhibitor; SNRI= serotonin-norepinephrine reuptake inhibitor; TCA = tricyclic antidepressant; IPT = inverse probability of treatment.
a Number of ectopic pregnancies.
b Per 10,000 pregnancies.
Next, we examined the risk of ectopic pregnancy by prepregnancy depression status, regardless of antidepressant use. The risk of ectopic pregnancy was higher among women who had prepregnancy depression (214 per 10,000 pregnancies) than women who did not have prepregnancy depression (177 per 10,000 pregnancies; Table 3). After IPT weighting, women with prepregnancy depression had a 1.09 (95% CI, 1.04 to 1.15) times higher risk of ectopic pregnancy than women who did have this diagnosis.
Table 3.
Frequency of Pregnancies and Relative Risk of Ectopic Pregnancy by Prepregnancy Depression Status.
| Prepregnancy Depression | N | Eventsa (Riskb) | Risk Differenceb (95% CI) | Relative Risk (95% CI) | |
|---|---|---|---|---|---|
| Crude | IPT-Weighted | ||||
| No | 1,596,457 | 28,244 (177) | Reference | 1.00 (Reference) | 1.00 (Reference) |
| Yes | 106,788 | 2,289 (214) | 37 (29 to 46) | 1.21 (1.16 to 1.26) | 1.09 (1.04 to 1.15) |
Note. IPT = inverse probability of treatment.
a Number of ectopic pregnancies.
b Per 10,000 pregnancies.
Among women who did not have a prepregnancy depression diagnosis, those who had an antidepressant prescription around conception had 1.08 times higher risk (95% CI, 1.01 to 1.15) of ectopic pregnancy than unexposed women. The RRs for specific classes of antidepressants ranged from 1.17 to 1.20, except SSRI, for which the RR was 1.03 (Table 4).
Table 4.
Frequency and Relative Risk of Ectopic Pregnancy by Antidepressant Use Around Conception Among Women who did not have a Depression Diagnosis in the year Before Conception.
| Antidepressant Use around Conception | Had Prescription | Did Not Have Prescription | Risk Differenceb (95% CI) | Relative Risk (95% CI) | |||
|---|---|---|---|---|---|---|---|
| N | Eventsa (Riskb) | N | Eventsa (Riskb) | Crude | IPT-Weighted | ||
| Any antidepressant | 60,829 | 1,258 (207) | 1,535,628 | 26,986 (176) | 31 (20 to 43) | 1.18 (1.11 to 1.24) | 1.08 (1.01 to 1.15) |
| Specific type | |||||||
| Any SSRI | 43,697 | 851 (195) | 1,552,760 | 27,393 (176) | 18 (5 to 31) | 1.10 (1.03 to 1.18) | 1.03 (0.96 to 1.11) |
| Any SNRI | 7,044 | 155 (220) | 1,589,413 | 28,089 (177) | 43 (9 to 78) | 1.25 (1.07 to 1.46) | 1.18 (0.99 to 1.40) |
| Any TCA | 3,698 | 105 (284) | 1,592,759 | 28,139 (177) | 107 (54 to 161) | 1.61 (1.33 to 1.94) | 1.20 (0.93 to 1.53) |
| Any Other | 9,767 | 231 (237) | 1,586,690 | 28,013 (177) | 60 (30 to 90) | 1.34 (1.18 to 1.52) | 1.17 (1.01 to 1.36) |
Note. n = 1,596,457. Women can have active prescriptions for more than one type of antidepressant. For each specific antidepressant, the comparison group is women who did not fill a prescription for that specific antidepressant. SSRI = selective serotonin reuptake inhibitor; SNRI= serotonin-norepinephrine reuptake inhibitor; TCA = tricyclic antidepressant; IPT = inverse probability of treatment.
a Number of ectopic pregnancies.
b Per 10,000 pregnancies.
Discussion
In this large cohort study, among women who had a prepregnancy depression diagnosis, those who had an active antidepressant prescription at conception were not at increased risk of having an ectopic pregnancy. Risk of ectopic pregnancy was slightly higher among women who had a prepregnancy depression diagnosis (not considering antidepressant prescriptions around conception). Approximately 60% of women who had an active antidepressant prescription at conception did not have a prepregnancy depression diagnosis; among women who did not have a prepregnancy depression diagnosis, the risk of ectopic pregnancy was slightly higher among those who had an active antidepressant prescription around conception.
To our knowledge, this is the first study to examine the potential effects of antidepressant use on risk of ectopic pregnancy. This hypothesis is supported by mechanistic evidence that antidepressants potentially affect both the cilia function and smooth muscle cells in the fallopian tube.16–18 Among women with a prepregnancy depression diagnosis, those who had an active TCA prescription around conception were at an increased risk of ectopic pregnancy. A study of muscarinic cholinergic receptors found that amitriptyline, a TCA, had very high affinity across all 5 receptor types, including M3, which affects smooth muscle function.47 Since ectopic pregnancies are thought to be caused by changes in the fallopian tube, changes to smooth muscle function could increase risk of ectopic pregnancy. It is important to note that there were very few women in our study that had active TCA prescriptions at conception. Additionally, women who use TCAs may have more severe depression or have treatment-resistant depression;48 thus, unaccounted for confounding could be contributing to the increased risk of ectopic pregnancy.
One previous study examined the association between psychiatric conditions and risk of ectopic pregnancy. This study combined depression, anxiety, adjustment disorder, and somatoform disorders into one category and found that women who had at least one of these conditions were at a 1.8-fold higher risk of ectopic pregnancy.25 Our findings that the risk of ectopic pregnancy was 1.09 times higher for women with a depression diagnosis suggests that other psychiatric conditions—or their treatments—may be stronger risk factors for ectopic pregnancy.
For women without a diagnosis of depression in the year before their pregnancy, the RR of ectopic pregnancy was 1.03, 1.17, 1.18, and 1.20 times higher among women who had an SSRI (the most commonly prescribed antidepressant), “other” antidepressant, SNRI, and TCA prescription, respectively. There are many alternative uses for antidepressants, most commonly anxiety, pain, insomnia, and panic disorders.34 We are unable to determine whether the underlying conditions for the alternative use of antidepressants increased the risk of ectopic pregnancy among women without prepregnancy depression or whether the use of these antidepressants had a different effect on the fallopian tubes of these women than women who had prepregnancy depression. It is also possible that our weighting algorithm was less effective in the subgroup without a depression diagnosis, resulting in residual confounding by indication.
This study provides important information regarding the potential effects of depression and antidepressant use on women’s risk of ectopic pregnancy. Early pelvic ultrasounds to assess whether the pregnancy is ectopic or intrauterine, and early treatment of ectopic pregnancy can prevent tubal rupture, which can be fatal.49,50 When assessing a woman’s risk of ectopic pregnancy to determine whether she should have an early pelvic ultrasound, TCA use around conception and depression diagnoses can be taken into account.
A significant strength of this study is the use of a large cohort with an objective assessment of outpatient drug dispensation, and the linkage to inpatient and outpatient health records and outpatient pharmaceutical records to account for a wide range of potential confounders. However, our study has several limitations. We used an algorithm to identify ectopic and intrauterine pregnancies and last menstrual period and were unable to validate these estimates using data from medical records or birth certificates. This approach could result in misclassification; however, previous studies have validated similar algorithms, demonstrating good to excellent agreement on designation and dating of pregnancy outcomes.29,30 Ectopic pregnancies are generally identified between 42 and 84 days after a pregnant woman’s last menstrual period; given this small range in dates and the accuracy of the algorithm in identifying last menstrual period before an ectopic pregnancy, we are confident that our exposure window includes their last menstrual period.51
Relying on outpatient prescription data to identify antidepressant use could result in over- or underestimation of actual antidepressant consumption. Not all dispensed antidepressants are consumed (resulting in overestimation), and antidepressants consumed during inpatient hospitalizations or paid for out-of-pocket are not captured (resulting in underestimation). Additionally, we used inpatient and outpatient claims to identify prepregnancy depression, which can also lead to misclassification.52 Not all individuals with depression are diagnosed as such by their care provider, and those with diagnosed depression may have been diagnosed outside of the 12-month window we examined. Using claims data to identify depression also does not allow us to determine the severity of the depression.
The use of inpatient and outpatient claims allowed us to adjust for a wide range of potential confounders; however, this approach cannot remove confounding by variables that are not well captured in the data and for which there are no suitable proxies. For example, smoking status is underestimated in claims data.53 Additionally, we had limited information on sociodemographic characteristics. Antidepressant use during pregnancy is higher among women who use alcohol around conception or have higher parity;54 these are also risk factors for ectopic pregnancy. Other risk factors of ectopic pregnancy—such as a history of ectopic pregnancy and prior pelvic surgeries—may be missed as they could have occurred more than a year before conception, and given the short windows of continuous insurance coverage, we were also unable to determine parity.55 Lastly, our cohort included only women with employer-based medical insurance coverage. These findings should be replicated in other settings and for women from more diverse sociodemographic backgrounds to assess the generalizability of our results.
Conclusion
There are approximately 126,000 ectopic pregnancies in the United States every year, yet there is no known risk factor for half of these ectopic pregnancies.12 This is the first study to examine the risk of ectopic pregnancy among women who use antidepressants around conception or were diagnosed with depression before the start of their pregnancy. Our findings indicate that the use of most antidepressants around conception does not result in an increased risk of ectopic pregnancy.
Supplemental Material
Supplement_material for Antidepressant Use around Conception, Prepregnancy Depression, and Risk of Ectopic Pregnancy by Elizabeth Wall-Wieler, Thalia K. Robakis, Carolyn E. Cesta, Reem Masarwa, Deirdre J. Lyell, Can Liu, Robert W. Platt and Suzan L. Carmichael in The Canadian Journal of Psychiatry
Footnotes
Authors’ Note: Data access for this project was provided by the Stanford Center for Population Health Sciences Data Core. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded through a Banting Postdoctoral Fellowship and a Stanford Maternal and Child Health Research Institute Postdoctoral Award. The PHS Data Core is supported by a National Institutes of Health National Center for Advancing Translational Science Clinical and Translational Science Award (UL1 TR001085) and internal Stanford funding.
ORCID iD: Elizabeth Wall-Wieler, PhD  https://orcid.org/0000-0003-2480-8875
https://orcid.org/0000-0003-2480-8875
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Hoover K, Tao G, Kent C. Trends in the diagnosis and treatment of ectopic pregnancy in the United States. Obstet Gynecol. 2010;115(3):495–502. doi: 10.1097/AOG.0b013e3181d0c328. [DOI] [PubMed] [Google Scholar]
- 2. Curtin SC, Abma JC, Ventura SJ, Henshaw S. Pregnancy rates for U.S. women continue to drop. NCHS Data Brief. 2013;3(136):1–8. [PubMed] [Google Scholar]
- 3. Chang J, Elam-Evans L, Berg C, et al. Pregnancy-related mortality surveillance—United States, 1991-1999. MMWR Surveill Summ. 2003;52(3):1–8. [PubMed] [Google Scholar]
- 4. Creanga AA, Shapiro-Mendoza CK, Bish CL, Zane S, Berg CJ, Callaghan WM. Trends in ectopic pregnancy mortality in the United States: 1980-2007. Obstet Gynecol. 2011;117(4):837–843. doi: 10.1097/AOG.0b013e3182113c10. [DOI] [PubMed] [Google Scholar]
- 5. Stulberg DB, Cain L, Dahlquist IH, Lauderdale DS. Ectopic pregnancy morbidity and mortality in low-income women, 2004-2008. Hum Reprod. 2016;31(3):666–671. doi: 10.1093/humrep/dev332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mikhail E, Salemi JL, Schickler R, Salihu HM, Plosker S, Imudia AN. National rates, trends and determinants of inpatient surgical management of tubal ectopic pregnancy in the United States, 1998–2011. J Obstet Gynaecol Res. 2018;44(4):730–738. doi: 10.1111/jog.13588. [DOI] [PubMed] [Google Scholar]
- 7. Li C, Zhao WH, Zhu Q, et al. Risk factors for ectopic pregnancy: a multi-center case-control study. BMC Pregnancy Childbirth. 2015;15(1):187 doi: 10.1186/s12884-015-0613-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kamwendo F, Forslin L, Bodin L, Danielsson D. Epidemiology of ectopic pregnancy during a 28 year period and the role of pelvic inflammatory disease. Sex Transm Infect. 2000;76(1):28–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Du T, Chen H, Fu R, et al. Comparison of ectopic pregnancy risk among transfers of embryos vitrified on day 3, day 5, and day 6. Fertil Steril. 2017;108(1):108–116.e1 doi: 10.1016/j.fertnstert.2017.05.027. [DOI] [PubMed] [Google Scholar]
- 10. Backman T, Rauramo I, Huhtala S, Koskenvuo M. Pregnancy during the use of levonorgestrel intrauterine system. Am J Obstet Gynecol. 2004;190(1):50–54. doi: 10.1016/j.ajog.2003.07.021. [DOI] [PubMed] [Google Scholar]
- 11. Bouyer J. risk factors for ectopic pregnancy: a comprehensive analysis based on a large case-control, population-based study in France . Am J Epidemiol. 2003;157(3):185–194. doi: 10.1093/aje/kwf190. [DOI] [PubMed] [Google Scholar]
- 12. Committee on Practice Bulletins—Gynecology, Barnhart K, Franasiak H. ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018;131(3): e91–e103. doi: 10.1097/AOG.0000000000002560. [DOI] [PubMed] [Google Scholar]
- 13. Halbert S, Tabm P, Blandau R. Egg transport in the rabbit oviduct: the roles of cilia and muscle. Science (80-). 1976;191(4231):1052–1053. [DOI] [PubMed] [Google Scholar]
- 14. Walker J. Ectopic pregnancy. Clin Obs Gynecol. 2007;50(1):89–99. [DOI] [PubMed] [Google Scholar]
- 15. Shaw JL V, Dey SK, Critchley HOD, Horne AW. Current knowledge of the aetiology of human tubal ectopic pregnancy. Hum Reprod Update. 2010;16(4):432–444. doi: 10.1093/humupd/dmp057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Milosavljević MN, Janković S V., Janković SM, et al. Effects of selective serotonin reuptake inhibitors on motility of isolated fallopian tube. Clin Exp Pharmacol Physiol. 2019;2(5):780–787. doi: 10.1111/1440-1681.13118. [DOI] [PubMed] [Google Scholar]
- 17. Al-Azemi M, Refaat B, Amer S, Ola B, Chapman N, Ledger W. The expression of inducible nitric oxide synthase in the human fallopian tube during the menstrual cycle and in ectopic pregnancy. Fertil Steril. 2010;94(3):833–840. doi: 10.1016/j.fertnstert.2009.04.020. [DOI] [PubMed] [Google Scholar]
- 18. Dhir A, Kulkarni SK. Nitric oxide and major depression. Nitric Oxide Biol Chem. 2011;24(3):125–131. doi: 10.1016/j.niox.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 19. Dawson AL, Ailes EC, Gilboa SM, et al. Antidepressant prescription claims among reproductive-aged women with private employer-sponsored insurance—United States 2008–2013. MMWR Morb Mortal Wkly Rep. 2016;65(3):41–46. doi: 10.15585/mmwr.mm6503a1. [DOI] [PubMed] [Google Scholar]
- 20. Almeida ND, Basso O, Abrahamowicz M, Gagnon R, Tamblyn R. Risk of miscarriage in women receiving antidepressants in early pregnancy, correcting for induced abortions. Epidemiology. 2016;27(4):538–546. doi: 10.1097/EDE.0000000000000484. [DOI] [PubMed] [Google Scholar]
- 21. Myles N, Newall H, Ward H, Large M. Systematic meta-analysis of individual selective serotonin reuptake inhibitor medications and congenital malformations. Aust N Z J Psychiatry. 2013;47(11):1002–1012. doi: 10.1177/0004867413492219. [DOI] [PubMed] [Google Scholar]
- 22. Jong GWT, Einarson T, Koren G, Einarson A. Antidepressant use in pregnancy and persistent pulmonary hypertension of the newborn (PPHN): a systematic review. Reprod Toxicol. 2012;34(3):293–297. doi: 10.1016/j.reprotox.2012.04.015. [DOI] [PubMed] [Google Scholar]
- 23. Grigoriadis S, VonderPorten EH, Mamisashvili L, et al. The effect of prenatal antidepressant exposure on neonatal adaptation: a systematic review and meta-analysis. J Clin Psychiatry. 2013;74(4):8 doi: 10.4088/JCP.12r07967. [DOI] [PubMed] [Google Scholar]
- 24. Guo N, Robakis T, Miller C, Butwick A. Prevalence of depression among women of reproductive age in the United States. Obstet Gynecol. 2018;131(4):671–679. doi: 10.1097/AOG.0000000000002535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Jacob L, Kalder M, Kostev K. Risk factors for ectopic pregnancy in Germany: a retrospective study of 100,197 patients. GMS Ger Med Sci. 2017;15(3):1–9. doi: 10.3205/000260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Cuevas M, Flores I, Thompson KJ, Ramos-Ortolaza DL, Torres-Reveron A, Appleyard CB. Stress exacerbates endometriosis manifestations and inflammatory parameters in an animal model. Reprod Sci. 2012;19(8):851–862. doi: 10.1177/1933719112438443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. IBM Corporation. IBM Market Scan Research Database; 2018. [Google Scholar]
- 28. Ailes EC, Simeone RM, Dawson AL, Petersen EE, Gilboa SM. Using insurance claims data to identify and estimate critical periods in pregnancy: an application to antidepressants. Birth Defects Res Part A Clin Mol Teratol. 2016;106(11):927–934. doi: 10.1002/bdra.23573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Scholes D, Yu O, Raebel MA, Trabert B, Holt VL. Improving automated case finding for ectopic pregnancy using a classification algorithm. Hum Reprod. 2011;26(11):3163–3168. doi: 10.1093/humrep/der299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hornbrook MC, Dietz PM, Williams SB, et al. Development of an algorithm to identify pregnancy episodes in an integrated health care delivery system. Health Serv Res. 2006;42(2):908–927. doi: 10.1111/j.1475-6773.2006.00635.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Cerner Multum Inc.HEDIS 2018 Medication List Directory of NDC codes. HEDIS measures and technical resources. [accessed 2019 Oct 23] https://www.ncqa.org/hedis/measures/hedis-2018-ndc-license/hedis-2018-final-ndc-lists/.
- 32. Wilcox AJ, Weinberg CR, Baird DD. Timing of sexual intercourse in relation to ovulation. Obstet Gynecol Surv. 1996;51(6):357–358. doi: 10.1097/00006254-199606000-00016. [Google Scholar]
- 33. Loftus E V, Guérin A, Yu AP, et al. Increased risks of developing anxiety and depression in young patients with Crohn’s disease. Am J Gastroenterol. 2011;106(9):1670–1677. doi: 10.1038/ajg.2011.142. [DOI] [PubMed] [Google Scholar]
- 34. Wong J, Motulsky A, Abrahamowicz M, Eguale T, Buckeridge DL, Tamblyn R. Off-label indications for antidepressants in primary care: Descriptive study of prescriptions from an indication based electronic prescribing system. BMJ. 2017:356 doi: 10.1136/bmj.j603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Schneeweiss S, Rassen J, Glynn R, Avorn J, Mogun H, Brookhart M. High-dimensional propensity score adjustment in studies of treatment effects using health care claims data. Epidemiology. 2009;20(4):512–522. doi: 10.1097/EDE.0b013e3181a663cc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Schneeweiss S, Eddings W, Glynn R, Patorno E, Rassen J, Franklin J. Variable selection for confounding adjustment in high-dimensional covariate spaces when analyzing healthcare databases. Epidemiology. 2017;28(2):237–248. doi: 10.1097/EDE.0000000000000581. [DOI] [PubMed] [Google Scholar]
- 37. Rassen J, Doherty M, Huang W, Schneeweiss S. Pharmacoepidemiology toolbox. 2013. [accessed 2019 Mar 12] http://www.hdpharmacoepi.org.
- 38. Myers JA, Rassen JA, Gagne JJ, et al. Effects of adjusting for instrumental variables on bias and precision of effect estimates. Am J Epidemiol. 2011;174(11):1213–1222. doi: 10.1093/aje/kwr364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Military Health Systems. AFHSC surveillance case definitions—Pelvic inflammatory disease. Acute; 2015. [accessed 2019 May 7]. https://www.health.mil/Reference-Center/Publications/2015/06/01/Pelvic-Inflammatory-Disease. [Google Scholar]
- 40. Webb L. Capturing all necessary codes for IUD insertion and removal can be challenging. just coding news: outpatient. [accessed 2019 Apr 30] http://www.hcpro.com/HIM-240086-8160/Capturing-all-necessary-codes-for-IUD-insertion-and-removal-can-be-challenging.html
- 41. Martin AS, Monsour M, Kissin DM, Jamieson DJ, Callaghan WM, Boulet SL. Trends in severe maternal morbidity after assisted reproductive technology in the United States, 2008-2012. Obstet Gynecol. 2016;127(1):59–66. doi: 10.1097/AOG.0000000000001197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. For the Record. Coding for STDs. Rec. 2012;24(12):27 [accessed 2019 May 7]. https://www.fortherecordmag.com/archives/061812p27.shtml. [Google Scholar]
- 43. Prabhu M, Garry EM, Hernandez-Diaz S, MacDonald SC, Huybrechts KF, Bateman BT. Frequency of opioid dispensing after vaginal delivery. Obstet Gynecol. 2018;132(2):459–465. doi: 10.1097/AOG.0000000000002741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Harder V, Stuart E, Anthony J. Propensity score techniques and the assessment of measured covariate balance to test causal associations in psychological research. Psychol Meth. 2010;15(3):234–249. doi: 10.1037/a0019623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Elizabeth AS, Brian KL, Finbarr PL. Prognostic score–based balance measures for propensity score methods in comparative effectiveness research. J Clin Oncol. 2012;30(34):4208–4214. doi: 10.1200/JCO.2012.42.2659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. SAS Institute Inc. SAS 9.4; 2013. [Google Scholar]
- 47. Stanton T, Bolden-Watson C, Cusack B, Richelson E. Antagonism of the five cloned human muscarinic cholinergic receptors expressed in CHO-K1 cells by antidepressants and antihistaminics. Biochem Pharmacol. 1993;45(11):2352–2354. doi: 10.1016/0006-2952(93)90211-E. [DOI] [PubMed] [Google Scholar]
- 48. Nemeroff CB. Prevalence and management of treatment-resistant depression. J Clin Psychiatry. 2007;68(Suppl. 8):17–25. [PubMed] [Google Scholar]
- 49. Barnhart KT. Ectopic pregnancy. N Engl J Med. 2009;361(4):379–387. [DOI] [PubMed] [Google Scholar]
- 50. Cacciatore B, Stenman UH, Ylostalo P. Early screening for ectopic pregnancy in high-risk symptom-free women. Lancet. 1994;343(8896):517–518. doi: 10.1016/S0140-6736(94)91465-6. [DOI] [PubMed] [Google Scholar]
- 51. Matcho A, Ryan P, Fife D, Gifkins D, Knoll C, Friedman A. Inferring pregnancy episodes and outcomes within a network of observational databases. PLoS One. 2018;13(2):1–20. doi: 10.1371/journal.pone.0192033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Doktorchik C, Patten S, Eastwood C, et al. Validation of a case definition for depression in administrative data against primary chart data as a reference standard 11 medical and health sciences 1117 public health and health services. BMC Psychiatry. 2019;19(1):1–8. doi: 10.1186/s12888-018-1990-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Desai R, Solomon D, Shadick N, Iannaccone C, Kim S. Identification of smoking using Medicare data—a validation study of claims-based algorithms. Pharmacoepidemiol Drug Saf. 2016;25:472–475. doi: 10.1002/pds. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Alwan S, Reefhuis J, Rasmussen SA, Friedman JM. Patterns of antidepressant medication use among pregnant women in a united states population. J Clin Pharmacol. 2011;51(2):264–270. doi: 10.1177/0091270010373928. [DOI] [PubMed] [Google Scholar]
- 55. Moini A, Hosseini R, Jahangiri N, Shiva M, Akhoond M. Risk factors for ectopic pregnancy: a case–control study. J Res Med Sci. 2014;19(9):844–849. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplement_material for Antidepressant Use around Conception, Prepregnancy Depression, and Risk of Ectopic Pregnancy by Elizabeth Wall-Wieler, Thalia K. Robakis, Carolyn E. Cesta, Reem Masarwa, Deirdre J. Lyell, Can Liu, Robert W. Platt and Suzan L. Carmichael in The Canadian Journal of Psychiatry