Abstract
Objectives:
To examine the relationship between prepregnancy chronic medical conditions (CMCs) and the risk of acute perinatal psychiatric health-care encounters (i.e., psychiatric emergency department visits, hospitalizations) among refugees, nonrefugee immigrants, and long-term residents in Ontario.
Methods:
We conducted a population-based study of 15- to 49-year-old refugees (N = 29,189), nonrefugee immigrants (N = 187,430), and long-term residents (N = 641,385) with and without CMC in Ontario, Canada, with a singleton live birth in 2005 to 2015 and no treatment for mental illness in the 2 years before pregnancy. Modified Poisson regression was used to estimate the relative risk of a psychiatric emergency department visit or hospitalization from conception until 1 year postpartum among women with versus without CMC, stratified by migrant status. An unstratified model with an interaction term between CMC and migrant status was used to test for multiplicativity of effects.
Results:
The association between CMC and risk of a psychiatric emergency department visit or hospitalization was stronger among refugees (adjusted relative risk [aRR] = 1.87; 95% confidence interval [CI], 1.36 to 2.58) compared to long-term residents (aRR = 1.39; 95% CI, 1.30 to 1.48; interaction P = 0.047). The strength of the association was no different in nonrefugee immigrants (aRR = 1.26; 95% CI, 1.05 to 1.51) compared to long-term residents (interaction P = 0.45).
Conclusion:
Our study identifies refugee women with CMC as a high-risk group for acute psychiatric health care in the perinatal period. Preventive psychosocial interventions may be warranted to enhance supportive resources for all women with CMC and, in particular refugee women, to reduce the risk of acute psychiatric health care in the perinatal period.
Keywords: chronic disease, depression, postpartum, emigration and immigration
Abstract
Objectifs :
Examiner la relation entre les conditions médicales chroniques (CMC) pré-grossesse et le risque de soins de santé psychiatriques périnataux actifs rencontrés (c.-à-d., lors de visites au service d’urgence psychiatrique, d’hospitalisations) chez les réfugiés, les immigrants non réfugiés, et les résidents de longue durée de l’Ontario.
Méthodes :
Nous avons mené une étude dans la population auprès de réfugiés de 15 à 49 ans (N = 29 189), d’immigrants non réfugiés (N = 187 430), et de résidents de longue durée (N = 641 385) souffrant ou non de CMC en Ontario, Canada, ayant donné naissance à un seul enfant de 2005 à 2015, et n’ayant eu aucun traitement de santé mentale dans les deux années précédant la grossesse. La régression de Poisson modifiée a servi à estimer le risque relatif d’une visite au service d’urgence psychiatrique ou d’une hospitalisation de la conception jusqu’à 1 an du postpartum chez les femmes souffrant de CMC contre celles n’en souffrant pas, stratifié selon le statut de migrant. Un modèle non stratifié avec un terme d’interaction entre les CMC et le statut de migrant a été utilisé pour vérifier la multiplicativité des effets.
Résultats :
L’association entre les CMC et le risque d’une visite au service d’urgence psychiatrique ou d’une hospitalisation était plus forte chez les réfugiés (risque relatif ajusté [RRa] 1,87, intervalle de confiance [IC] à 95 % 1,36 à 2,58) comparativement aux résidents de longue durée (RRa 1,39; IC à 95 % 1,30 à 1,48) (interaction P = 0,047). La force de l’association ne différait pas chez les immigrants non réfugiés (RRa 1,26; IC à 95 % 1,05 à 1,51) comparativement aux résidents de longue durée (interaction P = 0,45).
Conclusion :
Notre étude identifie les femmes réfugiées souffrant de CMC comme étant un groupe à risque élevé de soins de santé psychiatriques actifs à la période périnatale. Les interventions psychosociales préventives peuvent être indiquées afin d’améliorer les ressources de soutien pour toutes les femmes souffrant de CMC, et en particulier les femmes réfugiées, en vue de réduire le risque de soins de santé psychiatriques actifs dans la période périnatale.
Introduction
Perinatal mental illness impacts 1 in 5 pregnant or postpartum women1 and can have lasting adverse effects on mothers, their children, and families.2 Perinatal mental illness exists on a spectrum of severity and at its most severe can require acute psychiatric health care, involving emergency department visits or hospitalization.1 Although rare, severe perinatal mental illness can have significant negative consequences such as increased risk of maternal suicide, making prevention a priority.2 Migrant women have nearly twice the risk of perinatal mental illness compared to native-born women, with refugees having the greatest risk.3–7 Further, refugees have higher rates of acute psychiatric health-care use in the postpartum period compared to nonrefugees.8 The migrant population is increasing and now represents one-fifth of the Canadian population, with 14% of these being refugees.9,10 Most migrant women arrive during their reproductive years.11 Therefore, understanding risk factors for perinatal mental illness requiring psychiatric care in a hospital setting among migrant women is needed to better serve this vulnerable and growing maternal population.
There is evidence that chronic medical conditions (CMCs), such as diabetes and cardiovascular disease, increase the risk of perinatal mental illness.12 This association has been attributed to biological factors such as chronic inflammation and psychosocial factors related to the stress of living with a CMC.12 An estimated 1 in 5 pregnancies are affected by CMC, with this rate expected to increase with advancing maternal age, rising rates of obesity, and medical advances that improve fertility in women with CMC.13,14 Yet, the association between CMC and perinatal mental illness has not been examined within specific subgroups of women who may be at elevated risk. The impact of CMC on perinatal mental illness risk could be stronger among migrant women due to marginalization, acculturative stress, decreased social resources, and barriers to health-care access, including lower enrollment in primary care compared to long-term residents,15 in addition to their documented increased risk of perinatal mental illness in general.3–7 There may also be heterogeneity in this association by refugee status, time since immigration, and region of origin, with the strongest impact of CMC on perinatal mental health expected among the most marginalized groups: refugees, recent migrants, and those migrating from regions other than North America or Europe. An understanding of the association between CMC and perinatal mental illness among migrants is crucial to mitigating the debilitating effects of perinatal mental illness through early identification and treatment of subgroups at greatest risk and providing more responsive care for migrant women with CMC.
We examined the relationship between CMC and acute psychiatric health-care encounters in the perinatal period among a population-based cohort of refugees, nonrefugee immigrants, and long-term residents in Ontario, Canada.
Materials and Methods
Study Design and Population
We conducted a population-based cohort study of all Ontario singleton live births conceived between April 1, 2005 and March 31, 2015 and delivered in hospital at ≥20 weeks gestational age. Women were indexed from the conception date, with a 2-year look back window to assess exposures and baseline characteristics. We then followed women through pregnancy and for 1 year after delivery, to a maximum of December 31, 2016, to measure study outcomes. Because we wanted to obtain a measure of new-onset mental illness in the perinatal period, women with any diagnosis of mental illness recorded in the 2 years before conception were excluded, since one would expect most women with active mental illness to have at least one psychiatric health-care encounter during this period.16 We used validated algorithms to ascertain CMCs, all of which use a combination of Ontario Health Insurance Plan (OHIP) codes and diagnoses in emergency department visits and/or hospitalizations. The base population from which our cohort was derived captures only permanent residents eligible for OHIP, which ensures accurate ascertainment of CMC in all study groups using these algorithms. Although a small number of migrants who are not yet eligible for OHIP would not be included (e.g., asylum seekers who do not yet have permanent residency status and therefore receive federal health care instead), the median waiting period for an OHIP card is only 3 months (and in some cases less),17 making the expected impact of this limitation minimal.
Data Sources
Data for this study came from ICES (formerly the Institute for Clinical Evaluative Sciences), an independent research institute that holds databases of health administrative data for Ontario residents. To identify live births, we used the MOMBABY data set, which links mother–newborn pairs from the Canadian Institute for Health Information Discharge Abstract Database (CIHI-DAD). Four databases were used to identify CMCs and perinatal mental illness: the OHIP database for visits to a general practitioner or psychiatrist, CIHI-DAD and the Ontario Mental Health Reporting System for hospitalizations, and the National Ambulatory Care Reporting System for emergency department visits. For data on migrants, the Immigration, Refugees and Citizenship Canada (IRCC)’s Permanent Resident Database was linked to these data sets. Covariates were derived from the Registered Persons Database and the 2011 census as well as those listed above. Individual-level data were linked using a unique encoded identifier and analyzed at ICES, in Toronto. The use of data in this project was authorized under section 45 of Ontario’s Personal Health Information Protection Act, which does not require review by a research ethics board.
Exposure
CMCs that are common in women of reproductive age or could impact health in pregnancy13 were identified using validated algorithms: diabetes18; thyroid disease19; diseases of the circulatory system (hypertension, atrial fibrillation, congestive heart failure, myocardial infarction, stroke),20–24 respiratory system (asthma, chronic obstructive pulmonary disease),25 nervous system (multiple sclerosis, epilepsy, chronic migraine),26–28 musculoskeletal system (osteoarthritis, osteoporosis, rheumatoid arthritis),29,30 and skin and subcutaneous tissues (lupus, psoriasis)31; and other diseases (inflammatory bowel disease, chronic kidney disease; Supplemental Table S1).32,33 Cancers were not included, as these differ from the other conditions in their implications for maternal and fetal well-being; they are more immediately life threatening and require different management than other CMCs. Women with CMC were those with one or more of the eligible conditions during the look back period, while women without CMC were those without any of these conditions.
Migrant Variables
Immigrant status was ascertained from the IRCC Permanent Resident Database, which dates back to 1985. As in prior research,34,35 women not linked to this database were classified as long-term residents and may include immigrants who arrived in Canada before 1985. Migrants were those who migrated to Canada in 1985 to 2015, subsequently classified by immigration category (refugees, nonrefugee immigrants), length of stay (<5 years, ≥5 years), and world region of origin (Western [North America and Europe], elsewhere [Africa and the Middle East, the Caribbean and Latin America, and East and South Asia]).
Outcomes
To capture acute perinatal psychiatric health-care encounters, we measured emergency department visits and hospitalizations for mood or anxiety disorders (International Classification of Diseases [ICD-10]: F30-34, F38-39, F40-42,43.0,43.1,44, 45), psychotic disorders (ICD-10: F20, F22-25, F28, F29), substance use disorders (ICD-10: F10-F19, F55), self-harm (ICD-10: X60-X84, Y10-Y19, Y28), and other mental illness (ICD-10: F21, F60-F62, F68, F69) between conception and 365 days after delivery. Because we excluded women with psychiatric health-care encounters in the 2 years before conception, we considered these perinatal psychiatric health-care encounters to represent new-onset mental illness or new episodes.
Covariates
We measured variables that could confound the relationship between CMC and perinatal mental illness: maternal age, parity, neighborhood income, marginalization, rurality, and remote history of mental illness. Neighborhood income was determined by linking residential postal code with census data on median neighborhood income, with those in the lowest 2 income quintiles classified as low income.36 We used the Ontario Marginalization Index to measure material deprivation (the capacity of residents to meet basic material needs), residential instability (the proportion of dwellings that are apartments or unowned), dependency (the proportion of residents who do not receive income from employment), and ethnic concentration (the proportion of residents who belong to a visible minority group).37 Rural residence was defined as a score of ≥45 on the Rurality Index of Ontario,38 which classifies neighborhoods as rural or urban on the basis of factors related to travel distance to providers. Remote history of mental illness was defined as having ≥1 health-care encounters for mental illness > 2 years before conception.
Analysis
We used frequencies and percentages to describe cohort characteristics, stratified by migrant status (long-term residents, immigrants, refugees) and CMC status (no CMC, CMC). Differences between groups were assessed using standardized differences, with long-term residents without CMC being the reference group. Standardized difference >0.10 are clinically meaningful, as this threshold is equivalent to a ϕ coefficient of 0.05.39
Modified Poisson regression was used to directly estimate the relative risk of acute psychiatric health-care encounters in the perinatal period among women with CMC versus without CMC, stratified by migrant status (long-term residents, immigrants, and refugees).40 Generalized estimating equations were used to account for clustering in the data caused by the inclusion of multiple deliveries to the same woman during the study period.41 To determine whether the impact of CMC on acute perinatal psychiatric health-care encounters differed by migrant status, we tested a separate, unstratified, fully adjusted model wherein we included an interaction term between CMC status and migrant status to test for multiplicativity of effects (P < 0.05). Multivariable models were adjusted for age, parity, low neighborhood income, high material deprivation, high residential instability, high dependency, high ethnic concentration, and remote history of mental illness. Although we planned to also control for rurality, there were no refugees living in rural areas who had both CMC and the outcome, so we excluded this variable from the multivariable models. Prior to model fitting, all variables met required thresholds for collinearity tests. We did not include potential pathway variables, such as pregnancy complications.
We conducted several additional analyses. We examined the impact of having multiple CMCs (defined as having ≥2 of the conditions listed above), 1 CMC, and no CMCs, stratified by migrant status. We also examined the association between any CMC and the outcome among (1) long-term residents, immigrants living in Canada <5 years, and those living in Canada ≥5 years separately and (2) long-term residents, immigrants from Europe or North America, and those from other regions separately.
In sensitivity analyses, we estimated the relative risk of acute psychiatric health-care encounters in the perinatal period among women with CMC versus without CMC, stratified by migrant status, by (1) type of CMC (diabetes; thyroid disease; circulatory, respiratory, nervous system, musculoskeletal, and skin and subcutaneous tissue diseases; others) and (2) type of acute psychiatric health-care encounters such as psychotic, mood or anxiety, substance use, self-harm, and other. SAS Enterprise version 7.1 was used (SAS Institute Inc., Cary, North Carolina).
Results
There were 630,833 women with 858,004 singleton live births during the study period; 187,430 of these live births were to nonrefugee immigrants and 29,189 to refugees. Compared to long-term residents, immigrants and refugees were more likely to be multiparous and to live in low-income neighborhoods and those with indicators of high marginalization. They were less likely to live in rural areas or have a remote history of mental illness. Regardless of migration status, those with CMC were more likely than those without CMC to be multiparous, live in low-income neighborhoods and those with higher material deprivation and ethnic concentration, and have a remote history of mental illness (Table 1). In the cohort, 11.7% of long-term residents, 11.6% of nonrefugee immigrants, and 12.6% of refugees had a CMC. The distributions of specific CMCs differed by migrant status; rates of diabetes, thyroid disease, and circulatory and musculoskeletal diseases were somewhat higher in immigrants and refugees compared to long-term residents (Supplemental Table S2). None of the differences in rates of specific types of acute perinatal psychiatric health-care encounters by migrant status were clinically significant (see also Supplemental Table S2).
Table 1.
Baseline Characteristics by Migrant and CMC Category.
| Long-Term Residents | Immigrants | Refugees | ||||
|---|---|---|---|---|---|---|
| No CMC n = 566,333 |
CMC n = 75,052 |
No CMC n = 165,744 |
CMC n = 21,686 |
No CMC n = 25,519 |
CMC n = 3,670 |
|
| Median age (IQR) | 29 (26 to 33) | 30 (26 to 34) | 31 (27 to 34) | 32 (28 to 35) | 29 (26 to 33) | 31 (27 to 35) |
| Primiparousa | 26,5013 (46.8) | 33,356 (44.5) | 62,656 (33.4) | 6,778 (31.3) | 10,126 (39.7) | 1,123 (30.6) |
| Low-income statusb,c | 208,480 (37.1) | 28,919 (38.7) | 83,730 (50.6) | 11,376 (52.5) | 15,626 (61.3) | 2,345 (64.0) |
| Marginalizationd | ||||||
| Material deprivation | 206,547 (36.5) | 21,905 (39.2) | 94,842 (57.2) | 13,035 (60.1) | 17,099 (67.0) | 2,580 (70.3) |
| Residential instability | 219,905 (38.8) | 29,813 (39.7) | 66,461 (40.1) | 8,159 (37.6) | 12,291 (48.2) | 1,722 (46.9) |
| Dependency | 174,855 (30.9) | 23,665 (31.5) | 30,105 (18.2) | 3,708 (17.1) | 4,843 (19.0) | 644 (17.6) |
| Ethnic concentration | 240,462 (42.5) | 33,332 (44.4) | 145,124 (87.6) | 19,401 (89.5) | 22,314 (87.4) | 3,335 (90.9) |
| Rural/remote residencee | 55,126 (13.6) | 7,299 (13.1) | 1,470 (1.1) | 137 (0.8) | 73 (0.4) | 14 (0.5) |
| Remote history of mental illness | 293,971 (51.9) | 46,156 (61.5) | 50,341 (30.4) | 8,397 (38.7) | 10,150 (39.8) | 1,755 (47.8) |
Note. Reported as n (%) unless otherwise indicated. Boldface values indicate a standardized difference >0.10, with long-term residents with no CMC as referent. CMC = chronic medical condition; IQR = interquartile range.
a n = 17 missing.
b n = 4,571 missing.
c Proportion in bottom 2 income quintiles.
d Proportion in top 2 quintiles.
e n = 82 missing.
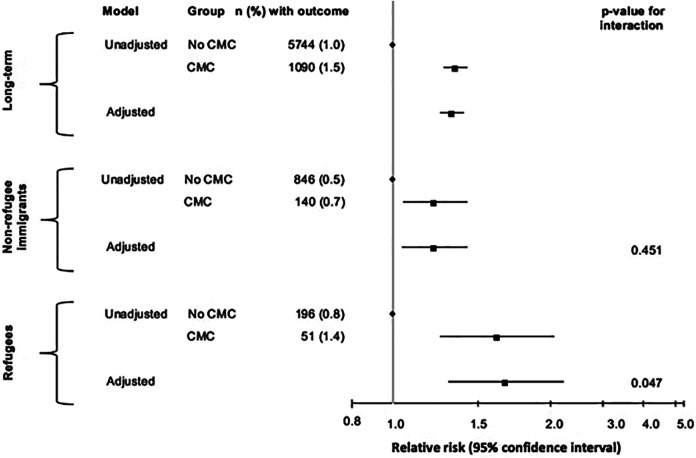
Figure 1 shows the relationship between CMC and acute perinatal psychiatric health-care encounters by migrant status. Women with CMC in each of the 3 groups were more likely than those without CMC to have the outcome. The relationship was stronger in refugees (1.4% vs. 0.8%; adjusted relative risk [aRR] = 1.87; 95% confidence interval [95% CI], 1.36 to 2.58) compared to long-term residents (1.5% vs. 1.0%; aRR = 1.39; 95% CI, 1.30 to 1.48; interaction P = 0.047). However, the strength of the relationship was no different in nonrefugee immigrants (0.7% vs. 0.5%; aRR = 1.26; 95% CI, 1.05 to 1.51) compared to long-term residents (interaction P = 0.45).
Figure 1.
Association between any CMC and the risk of any acute perinatal psychiatric health-care encounter by migrant status. Adjusted models control for age, parity, low neighborhood income, material deprivation, residential instability, dependency, ethnic concentration, and remote history of mental illness. We could not adjust for rurality due to small cell sizes. CMCs = chronic medical conditions.
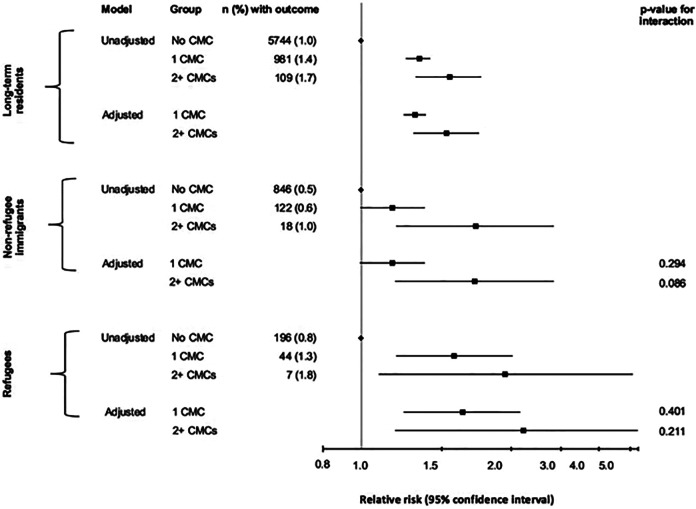
Figure 2 shows the relationship between multiple CMCs, 1 CMC, and none and acute perinatal psychiatric health-care encounters by migrant status. While there was a dose–response relationship in all groups, the impact of multiple CMCs on outcome risk was not significantly greater in refugees (aRR [vs. no CMC] = 2.56; 95% CI, 1.22 to 5.38; interaction P = 0.21) or nonrefugee immigrants (aRR = 1.93; 95% CI, 1.22 to 3.06; interaction P = 0.09) compared to long-term residents (aRR = 1.64; 95% CI, 1.36 to 1.98).
Figure 2.
Impact of multiple CMCs, 1 CMC, versus no CMC on the risk of any acute perinatal psychiatric health-care encounter by migrant status. Adjusted models control for age, parity, low neighborhood income, material deprivation, residential instability, dependency, ethnic concentration, and remote history of mental illness. We could not adjust for rurality due to small cell sizes. CMCs = chronic medical conditions.
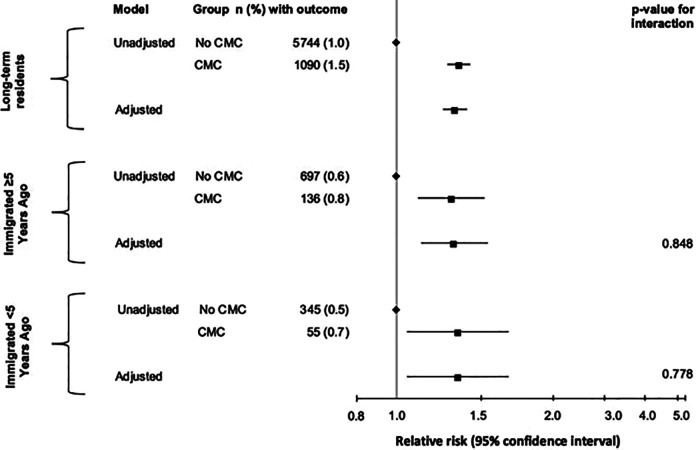
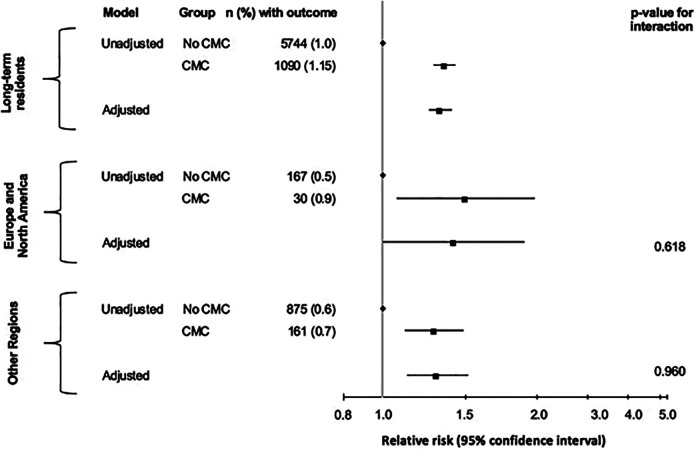
Figures 3 and 4 show the relationship between CMC and acute perinatal psychiatric health-care encounters by length of stay and region of origin. The relationship between CMC and the outcome among migrants living in Canada for ≥5 years (aRR = 1.38; 95% CI, 1.15 to 1.66; interaction P = 0.85) and <5 years (aRR = 1.41; 95% CI, 1.06 to 1.87; interaction P = 0.78) was no different than that among long-term residents (aRR = 1.39; 95% CI, 1.30 to 1.48). The association was no different in women migrating from Europe or North America (aRR = 1.50; 95% CI, 1.01 to 2.23; interaction P = 0.62) or elsewhere (aRR = 1.36; 95% CI, 1.15 to 1.62; interaction P = 0.96) compared to long-term residents (aRR = 1.39; 95% CI, 1.30 to 1.48).
Figure 3.
Impact of any CMC on the risk of any acute perinatal psychiatric health-care encounter by length of stay in Canada. Adjusted models control for age, parity, low neighborhood income, material deprivation, residential instability, dependency, ethnic concentration, and remote history of mental illness. We could not adjust for rurality due to small cell sizes. CMCs = chronic medical conditions.
Figure 4.
Impact of any CMC on the risk of any acute perinatal psychiatric health-care encounter by region of origin. Adjusted models control for age, parity, low neighborhood income, material deprivation, residential instability, dependency, ethnic concentration, and remote history of mental illness. We could not adjust for rurality due to small cell sizes. CMCs = chronic medical conditions.
In sensitivity analyses by type of CMC (Supplemental Table S3), the relationship between circulatory disorders and any acute perinatal psychiatric health-care encounter was stronger in refugees (aRR = 2.13; 95% CI, 0.92 to 4.96) compared to long-term residents (aRR = 0.93; 95% CI, 0.70 to 1.23; interaction P = 0.03). Likewise, the relationship between nervous system disorders and the outcome was stronger in refugees (aRR = 2.79; 95% CI, 1.85 to 4.22) compared to long-term residents (aRR = 1.76; 95% CI, 1.60 to 1.93; interaction P = 0.04). Other interactions were nonsignificant. In sensitivity analyses by type of acute perinatal psychiatric health-care encounter (Supplemental Table S4), no interactions were statistically significant. For both analyses, several models could not be run due to small cell sizes.
Discussion
This is the first population-based study to examine the relationship between CMC and perinatal mental illness requiring acute hospital care by migrant status. We found refugees, nonrefugee immigrants, and long-term residents with CMC were all at elevated risk for an acute perinatal psychiatric health-care encounter versus those without CMC. The association was significantly stronger in refugees compared to long-term residents, with little heterogeneity according to the number of CMCs, length of stay, or region of origin. Overall, our findings suggest refugees with CMC may be at particularly high risk for acute perinatal psychiatric health-care encounters. Although the overall risk of the outcome was low, with 1.5% in long-term residents with CMC representing the highest incidence, these events represent serious mental illness, with significant potential negative consequences for mothers and children, that clinical practice should endeavor to prevent. Our findings therefore support the development of more responsive perinatal mental health-care for women with CMC and particularly refugees with CMC.
Our findings align with prior research showing increased risk of perinatal mental illness in women with CMC generally. A meta-analysis of 12 studies investigating this relationship found a pooled adjusted odds ratio of 1.43 (95% CI, 1.25 to 1.63),12 which is comparable to the aRR of 1.39 we found among long-term residents. None of the studies included in this meta-analysis looked at migrants separately or controlled for migrant status. Therefore, the impact of migrant status on the magnitude of the association could not be determined. In nonobstetric populations, a handful of studies have examined the impact of CMC on depression in refugees, showing a weak association.42,43 However, no comparison to this association in long-term residents has been made previously.
Our findings also speak to a broader body of literature examining the impact of length of stay and region of origin on health outcomes in immigrants. Previous work in nonobstetric populations has found that while immigrants tend be healthier than the Canadian-born population upon arrival, particularly in terms of lower CMC rates, their health converges with that of Canadian-born residents and in some cases become worse as length of stay increases.3,44 Research in obstetric populations has observed this trend for some perinatal outcomes, such as preterm birth, but not for postpartum depression, the risk of which is elevated regardless of length of stay.45 Likewise, research has found rates of CMC and adverse perinatal outcomes tend to be higher in migrant groups from certain world regions but not others.8,46,47 We expected the impact of CMC on perinatal mental illness risk to be greater in recent migrants (vs. nonrecent) as well as among those from outside of Europe and North America (vs. other regions) because of greater marginalization and barriers to accessing health-care in these groups.48,49 However, this was not the case. This lack of heterogeneity could be explained by our broad categorizations (<5 vs. ≥5 years, North America or Europe vs. all other regions), which may obscure variation within these categories. This constitutes an important limitation of our analysis.
Potential mechanisms for the association between CMC and perinatal mental illness include biological pathways (e.g., chronic inflammation)12 and psychosocial pathways (e.g., stress associated with managing a CMC).12 Psychosocial mechanisms relate to our finding of a stronger association between CMC and perinatal mental illness in refugees, as this group faces significant challenges related to marginalization and barriers to accessing health-care50 including racism from providers, challenges communicating with providers due to lack of interpretative services, and poor familiarity with the health-care system.51 Immigrants are less likely to be enrolled in comprehensive primary care models.15 These challenges may have debilitating consequences for mental health during an already stressful period in the life of a woman with CMC. However, this does not explain why the strength of the association between CMC and acute perinatal psychiatric health-care encounters was no different in nonrefugee immigrants compared to long-term residents. One explanation differentiating nonrefugee immigrants from refugees is that immigrants who can choose to migrate are often among the wealthier and healthier individuals from their region of origin45 and tend to have lower rates of both CMC and perinatal mental illness than refugees.7,44,46,52 Refugees, on the other hand, are forced to migrate due to adverse conditions in their home country and may have experienced significant trauma, which could manifest in high rates of posttraumatic stress disorder.53 It is possible, then, that the same mechanisms that buffer nonrefugee migrants against CMCs and acute psychiatric health-care encounters separately mitigate the relationship between the 2 variables.
Our findings suggest changes to health-care delivery for refugees with CMC may be necessary to reduce their risk of perinatal mental illness. To improve management of CMC in refugees, in addition to increasing access to primary care, health-care providers should be trained to provide services that are respectful of the needs of diverse groups of women.51 Embedding cultural sensitivity training for providers and interpreting services for patients in prenatal care could facilitate better care for refugees by reducing discrimination and communication barriers. Our findings also suggest universal screening for perinatal mental illness should be implemented for all women with CMC, while ensuring refugee women receive supportive resources to mitigate their perinatal mental illness risk. More efficient surveillance and responsive care could have a positive impact on mental health.
Strengths and Limitations
Our use of population-based data allowed inclusion of all women, regardless of language and other barriers to participation in research. We used validated algorithms to ensure accurate ascertainment of CMCs. However, our findings are only generalizable to migrants with permanent residency status and not to those ineligible for OHIP in the 2-year look back period. Those who immigrated recently had an incomplete look back period for some covariates such as remote history of mental illness; however, only 11% of nonrefugee migrants and 8% of refugees migrated within 3 years of conception. Nevertheless, this might explain the differences observed in the prevalence of remote history of mental illness between migrants and long-term residents. Despite the large cohort size, we were unable to control for rurality because there were no refugees in rural areas who had both CMC and the outcome. Due to small cell sizes, we were also unable to disaggregate regions of origin and length of stay into finer subgroups, which may have masked heterogeneity in health outcomes.8,46 Finally, we were unable to measure some important characteristics (education, language ability) since these variables were not available for nonimmigrants.
Conclusion
With an increasing number of pregnancies affected by a CMC and the elevated risk of perinatal mental illness these conditions incur, our analysis supports the need for universal screening of perinatal mental illness among women affected by CMC. Further, the migrant population in Canada is rapidly increasing and with that increase comes a growing need for perinatal health and mental health services that are tailored to their needs. Refugees with CMC, in particular, represent a vulnerable maternal population that could benefit from psychosocial assessments to determine the need for supportive resources.
Supplemental Material
Suppplement_material for Association Between Chronic Medical Conditions and Acute Perinatal Psychiatric Health-Care Encounters Among Migrants: A Population-Based Cohort Study by Anthony McKnight, Simone N. Vigod, Cindy-Lee Dennis, Susitha Wanigaratne and Hilary K. Brown in The Canadian Journal of Psychiatry
Acknowledgments
We gratefully acknowledge the Canadian Institutes of Health Research for their support of this study through their Project Grant program (376290). The funding agency had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Authors’ Note: This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The opinions, results and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred. Parts of this material are based on data and information compiled and provided by the Canadian Institute for Health Information (CIHI). However, the analyses, conclusions, opinions, and statements expressed herein are those of the author and not necessarily those of CIHI. Data used for this study were housed at ICES, an independent not-for-profit corporation. The data set used in this study is held securely in coded form at ICES. While the data sharing agreements that govern the data set prohibit making it publicly available, access may be granted to those who meet specified criteria for confidential access. External individuals must apply for access through ICES’ Data and Analytic Services (DAS), a division of ICES established to provide data and analytic services to “third party researchers.” The data set that approved third party researchers would be permitted to access would be adjusted to ensure the risk of reidentification of any underlying individuals is low. Information about the application process, including the DAS Data Request Form and the criteria for access, including, for example, confirmation of approval by a Research Ethics Board, is available at https://www.ices.on.ca/DAS/Submitting-your-request. For general information visit www.ices.on.ca/DAS or email das@ices.on.ca.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Simone N. Vigod declares royalties from Up to Date Inc. for chapters on depression and antidepressants in pregnancy.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Hilary K. Brown, PhD  https://orcid.org/0000-0002-8690-5841
https://orcid.org/0000-0002-8690-5841
Supplemental Material: Supplemental material for this article is available online.
References
- 1. O’Hara M, Wisner K, Asher N. Perinatal mental illness: definition, description and aetiology. Best Pract Res Clin Obstet Gynaecol. 2014;28(1):3–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Meltzer-Brody S, Stuebe A. The long-term psychiatric and medical prognosis of perinatal mental illness. Best Pract Res Clin Obstet Gynaecol. 2014;28(1):49–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Vang ZM, Sigouin J, Flenon A, Gagnon A. Are immigrants healthier than native-born Canadians? A systematic review of the healthy immigrant effect in Canada. Ethn Health. 2017;22(3):209–241. [DOI] [PubMed] [Google Scholar]
- 4. Collns CH, Zimmerman C, Howard LM. Refugee, asylum seeker, immigrant women and postnatal depression: rates and risk factors. Arch Womens Ment Health. 2011;14(1):3–11. [DOI] [PubMed] [Google Scholar]
- 5. Falah-Hassani K, Shiri R, Vigod S, Dennis CL. Prevalence of postpartum depression among immigrant women: a systematic review and meta-analysis. J Psychiatr Res. 2015;70:67–82. [DOI] [PubMed] [Google Scholar]
- 6. Stewart DE, Gagnon A, Saucier JF, Wahoush O, Dougherty G. Postpartum depression symptoms in newcomers. Can J Psychiatry. 2008;53(2):121–124. [DOI] [PubMed] [Google Scholar]
- 7. Anderson FM, Hatch SL, Comacchio C, Howard LM. Prevalence and risk of mental disorders in the perinatal period among migrant women: a systematic review and meta-analysis. Arch Womens Ment Health. 2017;20(3):449–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Vigod SN, Bagadia AJ, Hussain-Shamsy N, et al. Postpartum mental health of immigrant mothers by region of origin, time since immigration, and refugee status: a population-based study. Arch Womens Ment Health. 2017;20(3):439–447. [DOI] [PubMed] [Google Scholar]
- 9. Immigration Refugees & Citizenship Canada. Facts & figures 2017: immigration overview—permanent residents. Annual IRCC updates. Canada—permanent residents by province or territory and category. Ottawa (ON); 2017. [accessed 2019 Dec 22]. https://open.canada.ca/data/en/dataset/082f05ba-e333-4132-ba42-72828d95200b [Google Scholar]
- 10. Statistics Canada. Immigration and ehnocultural diversity: Key results from the 2016 census. Ottawa (ON); 2017. [accessed 2019 Dec 22] https://www150.statcan.gc.ca/n1/daily-quotidien/171025/dq171025b-eng.htm [Google Scholar]
- 11. Chui T. Immigrant women Women in Canada: A gender-based statistical report. Ottawa (ON: ): Statistics Canada; 2011. [Google Scholar]
- 12. Brown HK, Qazilbash A, Rahim N, Dennis CL, Vigod SN. Chronic medical conditions and peripartum mental illness: a systematic review and meta-analysis. Am J Epidemiol. 2018;187(9):2060–2068. [DOI] [PubMed] [Google Scholar]
- 13. Kersten I, Lange AE, Haas JP, et al. Chronic diseases in pregnant women: Prevalence and birth outcomes based on the SNiP-study. BMC Pregnancy Childbirth. 2014:14:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Statistics Canada. Births, estimates, by province and territory. Ottawa (ON); 2014. [accessed 2019 Dec 22] http://www.statcan.gc.ca/tables-tableaux/sum-som/l01/cst01/demo04a-eng.htm [Google Scholar]
- 15. Batsta R, Pottie KC, Dahrouge S, et al. Impact of health care reform on enrolment of immigrants in primary care in Ontario, Canada. Fam Pract. 2019;36(4):445–451. [DOI] [PubMed] [Google Scholar]
- 16. Sunderland A, Findlay LC. Perceived Need for Mental Health Care in Canada: Results from the 2012 Canadian Community Health Survey-Mental Health. Health Rep. 2013;24(9):3–9. [PubMed] [Google Scholar]
- 17. Government of Ontario. Apply for OHIP and get a health card. Toronto (ON); 2019. [accessed 2019 Jul 22]https://www.ontario.ca/page/apply-ohip-and-get-health-card#section-2 [Google Scholar]
- 18. Hux JE, Ivis F, Flintoft V, Bica A. Diabetes in Ontario determination of prevalence and incidence using a validated administrative data algorithm. Diabetes Care. 2002;25(3):512–516. [DOI] [PubMed] [Google Scholar]
- 19. Frot L, Vestergaard P, Mosekilde L. Hyperthyroidism and risk of atrial fibrillation or flutter. Arch Intern Med. 2004;164(15):1675. [DOI] [PubMed] [Google Scholar]
- 20. Tu K, Campbell NR, Chen ZL, et al. Accuracy of administrative databases in identifying patients with hypertension. Open Med J. 2007;1(1):e18–E26. [PMC free article] [PubMed] [Google Scholar]
- 21. Austin PC, Daly PA, Tu JV. A multicenter study of the coding accuracy of hospital discharge administrative data for patients admitted to cardiac care units in Ontario. Am Heart J. 2002;144(2):290–296. [DOI] [PubMed] [Google Scholar]
- 22. Schultz SE, Rothwell DM, Chen Z, Tu K. Identifying cases of congestive heart failure from administrative data: a validation study using primary care patient records. Chronic Dis Inj Can. 2013;33(3):160–166. [PubMed] [Google Scholar]
- 23. Atzema CL, Austin PC, Miller E, Chong AS, Yun L, Dorian P. A population-based description of atrial fibrillation in the emergency department, 2002 to 2010. Ann Emerg Med. 2013;62(6):570–577.e7. [DOI] [PubMed] [Google Scholar]
- 24. Tu K, Wang M, Young J, et al. Validity of administrative data for identifying patients who have had a stroke or transient ischemic attack using EMRALD as a reference standard. Can J Cardiol. 2013;29(11):1388–1394. [DOI] [PubMed] [Google Scholar]
- 25. Gershon AS, Wang C, Guan J, Vasilevska-Ristovska J, Cicutto L, To T. Identifying patients with physician-diagnosed asthma in health administrative databases. Can Respir J. 2009;16(6):183–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Widdifield J, Ivers NM, Young J, et al. Development and validation of an administrative data algorithm to estimate the disease burden and epidemiology of multiple sclerosis in Ontario, Canada. Mult Scler. 2015;21(8):1045–1054. [DOI] [PubMed] [Google Scholar]
- 27. Tu K, Wang M, Jaakkimainen RL, et al. Assessing the validity of using administrative data to identify patients with epilepsy. Epilepsia. 2014;55(2):335–343. [DOI] [PubMed] [Google Scholar]
- 28. Van Walraven C, Colman I. Migraineurs were reliably identified using administrative data. J Clin Epidmiol. 2016;71:68–75. [DOI] [PubMed] [Google Scholar]
- 29. Cadarette SM, Jaglal SB, Raman-Wilms L, Beaton DE, Paterson JM. Osteoporosis quality indicators using healthcare utilization data. Osteoporos Int. 2011;22(5):1335–1342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Widdifield J, Bombardier C, Bernatsky S, et al. An administrative data validation study of the accuracy of algorithms for identifying rheumatoid arthritis: the influence of the reference standard on algorithm performance. BMC Musculoskelet Disord. 2014;15(1):216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Bernatsky S, Joseph L, Pineau CA, et al. A population-based assessment of systemic lupus erythematosus incidence and prevalence results and implications of using administrative data for epidemiological studies. Rheumatology (Oxford). 2007;46(12):1814–1818. [DOI] [PubMed] [Google Scholar]
- 32. Fleet JL, Dixon SN, Shariff SZ, et al. Detecting chronic kidney disease in population-based administrative databases using an algorithm of hospital encounter and physician claim codes. BMC Nephrol. 2013;14(1):81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Benchimol EI, Guttmann A, Mack DR, et al. Validation of international algorithms to identify adults with inflammatory bowel disease in health administrative data from Ontario, Canada. J Clin Epidemiol. 2014;67(8):887–896. [DOI] [PubMed] [Google Scholar]
- 34. Vigod S, Sultana A, Fung K, Hussain-Shamsy N, Dennis CL. A population-based study of postpartum mental health service use by immigrant women in Ontario, Canada. Can J Psychiatry. 2016;61(11):705–713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Wanigaratne S, Shakya Y, Gagnon AJ, et al. Refugee maternal and perinatal health in Ontario, Canada: a retrospective population-based study. BMJ Open. 2018;8(4):e018979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Muldoon L, Rayner J, Dahrouge S. Patient poverty and workload in primary care: study of prescription drug benefit recipients in community health centres. Can Fam Physician. 2013;59(4):384–390. [PMC free article] [PubMed] [Google Scholar]
- 37. Matheson FI. Ontario Agency for Health Protection and Promotion (Public Health Ontario). 2011 Ontario marginalization index: user guide. Toronto (ON): St. Michael's Hospital; 2017. [Google Scholar]
- 38. Kralj B. Measuring “rurality” for purposes of health-care planning: an empirical measure for Ontario. Ontario Med Rev. 2000;67(9):33–52. [Google Scholar]
- 39. Austin PC. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun Stat Simul Comput. 2009;38(6):1228–1234. [Google Scholar]
- 40. Zou G. A Modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. [DOI] [PubMed] [Google Scholar]
- 41. Hanley JA, Negassa A, Edwardes MD, Forrester JE. Statistical analysis of correlated data using generalized estimating equations: an orientation. Am J Epidemiol. 2003;157(4):364–375. [DOI] [PubMed] [Google Scholar]
- 42. Gammouh OS, Al-Smadi AM, Tawalbeh LI, et al. Peer reviewed: chronic diseases, lack of medications, and depression among Syrian refugees in Jordan, 2013–2014. Prev Chronic Dis. 2015:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Orega AN, Feldman JM, Canino G, Steinman K, Alegría M. Co-occurrence of mental and physical illness in US Latinos. Soc Psychiatry Psych Epidemiol. 2006;41(12):927–934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Betancourt MT, Roberts KC. Chronic disease patterns for immigrants to Canada: a recent data analysis. Health Pol Res Bull. 2010;(17):22–23. [Google Scholar]
- 45. Urquia ML, O’Campo PJ, Heaman MI. Revisiting the immigrant paradox in reproductive health: the roles of duration of residence and ethnicity. Soc Sci Med. 2012;74(10):1610–1621. [DOI] [PubMed] [Google Scholar]
- 46. Creatore MI, Moineddin R, Booth G, et al. Age- and sex-related prevalence of diabetes mellitus among immigrants to Ontario, Canada. CMAJ. 2010;182(8):781–789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Chiu M, Austin PC, Manuel DG, Tu JV. Comparison of cardiovascular risk profiles among ethnic groups using population health surveys between 1996 and 2007. CMAJ. 2010;182(8):E301–E310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Durbin A, Moineddin R, Lin E, Steele LS, Glazier RH. Examining the relationship between neighbourhood deprivation and mental health service use of immigrants in Ontario, Canada: a cross-sectional study. BMJ Open. 2015;5(3):e006690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Sanmartin C, Ross N. Experiencing difficulties accessing first-contact health services in Canada: Canadians without regular doctors and recent immigrants have difficulties accessing first-contact healthcare services. Reports of difficulties in accessing care vary by age, sex and region. Healthc Policy. 2006;1(2):103–119. [PMC free article] [PubMed] [Google Scholar]
- 50. Heaman M, Bayrampour H, Kingston D, et al. Migrant women’s utilization of prenatal care: a systematic review. Matern Child Health J. 2013;17(5):816–836. [DOI] [PubMed] [Google Scholar]
- 51. Small R, Roth C, Raval M, et al. Immigrant and non-immigrant women’s experiences of maternity care: a systematic and comparative review of studies in five countries. BMC Pregnancy Childbirth. 2014;14(1):152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Anderson KK, Cheng J, Susser E, McKenzie KJ, Kurdyak P. Incidence of psychotic disorders among first-generation immigrants and refugees in Ontario. CMAJ. 2015; 187(9):E279–E286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Fazel M, Wheeler J, Danesh J. Prevalence of serious mental disorder in 7000 refugees resettled in western countries: a systematic review. Lancet. 2005;365(9467):1309–1314. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Suppplement_material for Association Between Chronic Medical Conditions and Acute Perinatal Psychiatric Health-Care Encounters Among Migrants: A Population-Based Cohort Study by Anthony McKnight, Simone N. Vigod, Cindy-Lee Dennis, Susitha Wanigaratne and Hilary K. Brown in The Canadian Journal of Psychiatry