Abstract
The ongoing coronavirus disease-2019 (COVID-19) pandemic has been the focus of health care workers as it has affected millions of people and cost hundreds of thousands of lives around the world. As hospitals struggle to identify and care for those afflicted with COVID-19, it is easy to overlook endemic diseases that potentially worsen or mimic the pulmonary manifestations or may coinfect those with COVID-19. In this case report, we present the case of a 48-year-old Hispanic female who was admitted with respiratory distress from an acute COVID-19 infection but was also found to have acute pulmonary coccidioidomycosis infection and was treated successfully.
Keywords: COVID-19, coccidioidomycosis, valley fever, coccidioides, acute cocci, cocci COVID
Background
Coccidioides immitis is a well-known endemic fungus to the San Joaquin Valley region of California as well as Mexico and South America.1 Commonly referred to as “Valley Fever” in San Joaquin Valley, it typically manifests as a pulmonary infection with radiological appearance similar to coronavirus disease-2019 (COVID-19) or community-acquired pneumonia.2 Over the past decade, a dramatic increase in the incidence of coccidioidomycosis has been observed, particularly in endemic areas.3
The pandemic of COVID-19 is resulting in alarmingly high number of patients presenting with acute respiratory distress to the emergency rooms all over the country including in the city of Bakersfield, California, where coccidioidomycosis is an endemic infection for its visitors and residents. Because coccidioidomycosis can also mimic those symptoms of the SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) virus,2 serological testing for Coccidioides immitis were also performed on those presenting with respiratory distress. In this article, we present the first documented case of coinfection with SARS-CoV-2 as indicated with a positive reverse transcriptase-polymerase chain reaction and Coccidioides immitis as documented by positive immunoglobulin Ig M antibodies and complement fixation.
Patient Presentation
Our patient is a 48-year-old Hispanic female with a past medical history significant for systolic heart failure who presented to the emergency department on July 1, 2020, with complaints of shortness of breath. She was exposed to COVID-19 from her son. While in the emergency room, the patient had tested positive for COVID-19 and was discharged home on azithromycin as she was in respiratory distress.
Three days later, she returned with progressively worsening symptoms including headache, cough, and shortness of breath. While in the emergency room, the patient was in respiratory distress with a fever of 38.2 °C, a respiratory rate of 20 breaths per minute, and SpO2 of 93% requiring 3 L of O2 through nasal cannula. Chest X-ray taken on July 4, 2020, demonstrated decreased lung volumes with increased interstitial markings bilaterally (Figure 1), in addition to a follow-up computed axial tomography scan of the chest that showed no evidence of pulmonary embolus but possible right lower lobe atypical pneumonia (Figure 2).
Figure 1.
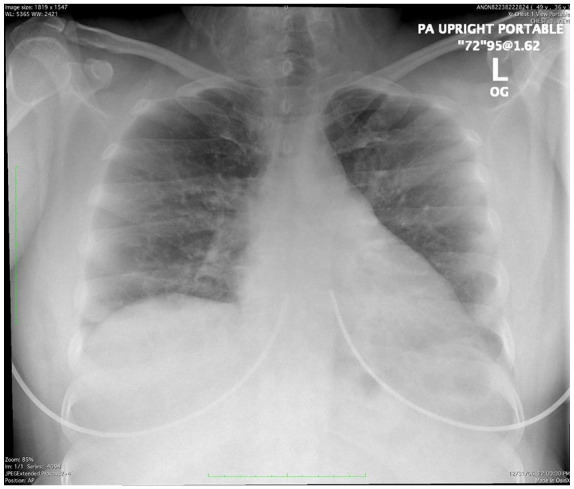
Chest radiograph from admission, July 4, 2020, showed decreased lung volumes and increased interstitial markings.
Figure 2.
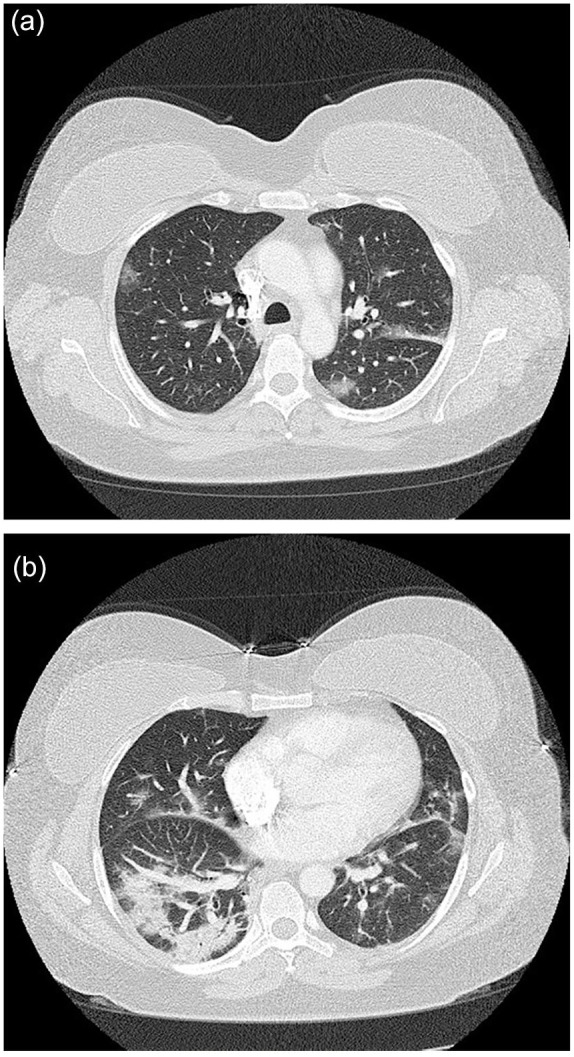
The computed axial tomography scan of the patient taken at the emergency department, July 4, 2020, indicated no evidence of pulmonary embolism (a). Atypical pneumonia was noted in the right lower lobe (b).
Due to the patient’s progressive respiratory symptoms and hypoxemia, she was admitted to the hospital and started on ceftriaxone, azithromycin, and dexamethasone 6 mg intravenous (IV) daily. Based off of her history of systolic heart failure, furosemide 40 mg bid was initiated intravenously early to achieve significant diuresis. With the patient’s clinical presentation and symptoms, she was also deemed appropriate for remdesivir 200 mg on day 1, followed by 100 mg IV daily for 4 days, and convalescent plasma.4 An echocardiogram was ordered as well for evaluation of her heart function.
As coccidioidomycosis is of continual concern in Bakersfield, a serology testing was dispatched on date of admission and returned July 4, 2020, as preliminary IgM positive indicating an acute infection that was confirmed through IgM and IgG immunodiffusion assays with a complement fixation of 1:2. Subsequently, fluconazole 400 mg daily was administered in addition to her current medication regimen for COVID-19. Her echocardiogram also demonstrated an ejection fraction of 50% to 55%.
Our patient experienced rapid resolution of her symptoms during the course of her hospitalization and 5-day course of remdesivir. Her hypoxemia rapidly resolved as well and she was able to be rapidly weaned off supplemental oxygen. She was subsequently discharged home on July 10, 2020, with oral fluconazole and dexamethasone.
Discussion
The patient presented above was exposed to and subsequently infected with the SARS-CoV-2 virus. Despite conservative home treatments as instructed through her initial emergency room encounter, the patient continued to have worsening symptoms until she was admitted on July 4, 2020, with acute hypoxic respiratory distress due to bilateral COVID-19 pneumonia.
Following current guidelines, she was deemed a candidate for remdesivir treatment as well as convalescent plasma.4,5 The patient was also initiated on antibiotics, as well as dexamethasone. Given her history of systolic heart failure, high-dose diuretics were initiated immediately on admission. Coccidioidomycosis was given strong consideration as a differential diagnosis for the patient’s bilateral pneumonia given the high prevalence rate endemic to Bakersfield, California, and similar clinical presentation.
On the regimen initiated, our patient made significant clinical improvement almost immediately after admission. The rapid serology screening for coccidioidomycosis returned with IgM positive suggesting an acute infection and fluconazole was initiated with the presumptive diagnosis of coccidioidomycosis infection with COVID-19, and was subsequently confirmed with a complement fixation of 1:2. The initiation of fluconazole was also important since the administration of steroids can worsen a coccidioidomycosis infection in an untreated individual.6
With the appropriate management of COVID-19 along with treatment of the endemic coccidioidomycosis, the patient showed rapid improvement and was discharged home in stable condition.
Conclusion
COVID-19, given its rapid spread and its destructive effect on the pulmonary system, is currently on the brink of overwhelming our health care system and needs to be aggressively screened for, triaged, and treated. However, endemic diseases like Coccidioides immitis that can mimic the clinical manifestations of COVID-19 can easily be overlooked or mistaken as being part of the COVID-19 pandemic. Our patient demonstrated that coccidioidomycosis can acutely coinfect those afflicted with COVID-19 requiring management for both pathogens to ensure appropriate recovery. In the time of COVID, it is important not to overlook endemic diseases like coccidioidomycosis that can synergistically play an active and potentially devastating role in a patient’s clinical outcome.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics Approval: Our institution does not require ethical approval for reporting individual cases series.
Informed Consent: Verbal informed consent was obtained from the patient for their anonymized information to be published in this article.
References
- 1. Kollath DR, Miller KJ, Barker BM. The mysterious desert dwellers: Coccidioides immitis and Coccidioides posadasii, causative fungal agents of coccidioidomycosis. Virulence. 2019;10:222-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bayer AS. Fungal pneumonias; pulmonary coccidioidal syndromes (part I). Primary and progressive primary coccidioidal pneumonias—diagnostic, therapeutic, and prognostic considerations. Chest. 1981;79:575-583. [DOI] [PubMed] [Google Scholar]
- 3. Centers for Disease Control and Prevention. Increase in reported coccidioidomycosis—United States, 1998-2011. MMWR Morb Mortal Wkly Rep. 2013;62:217-221. [PMC free article] [PubMed] [Google Scholar]
- 4. Duan K, Liu B, Li C, et al. Effectiveness of convalescent plasma therapy in severe COVID-19 patients. Proc Natl Acad Sci U S A. 2020;117:9490-9496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wang Y, Zhang D, Du G, et al. Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial. Lancet. 2020;395:1569-1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rutala PJ, Smith JW. Coccidioidomycosis in potentially compromised hosts: the effect of immunosuppressive therapy in dissemination. Am J Med Sci. 1978;275:283-295. [DOI] [PubMed] [Google Scholar]


