Abstract
Background:
Osteochondral injuries of the elbow are limiting and affect the ability of pediatric and adolescent athletes to participate in sports.
Purpose:
To report short- and midterm outcomes on athletes undergoing microfracture or fragment fixation of osteochondral elbow lesions and evaluate the effects thereof on sporting activity.
Study Design:
Case series; Level of evidence, 4.
Methods:
This was a retrospective study analyzing patients who underwent surgical treatment via microfracture or fragment fixation for osteochondral elbow lesions. Patients were treated at a single institution by a single surgeon between 2012 and 2019. Diagnosis was confirmed with magnetic resonance imaging, and patients were indicated for surgery after having persistent symptoms despite trialing rest, immobilization, and/or activity restriction for at least 3 months. Demographic data including sports of choice were collected preoperatively. Imaging and intraoperative findings were documented, and any complications were noted. Range of motion (ROM) was compared pre- to postoperatively. Return-to-sport evaluation included the ability to play the preoperative sport of choice.
Results:
In total, 23 patients (25 elbows) were included with a mean follow-up of 23.5 months (range, 6-60.3 months) and a mean age of 13.8 years. Of 25 lesions, 20 (80%) were on the athlete’s dominant side. There was significant improvement from pre- to postoperative ROM, including extension (mean ± SD, 6.4° ± 5.3° to 0.04° ± 0.2°; P < .00001), flexion (129.2° ± 10.6° to 138.6° ± 4.4°; P = .00013), and arc of ROM (122.6° ± 13.2° to 138.6° ± 4.4°; P < .00001). Mean lesion size was 81.9 ± 59.3 mm2 (range, 15-225 mm2). All elbows demonstrated radiographic healing postoperatively. Mean time to release to sport was 4.48 ± 1.38 months (range, 2.5-8 months). Six (26.1%) patients changed or stopped their preoperative sporting activity, including 2 of 4 gymnasts and 4 of 11 baseball players.
Conclusion:
Arthroscopic technique with lesion debridement and microfracture or fixation appears safe and results in radiographic healing; however, with these techniques, there remains a high rate of inability to return to sport in patients involved in higher-demand upper extremity activity, such as baseball and gymnastics. Further treatment strategies, including cartilage restoration procedures, may be warranted in this population.
Keywords: elbow, osteochondral, osteochondritis dissecans, pediatric sports medicine, baseball/softball, gymnastics
Osteochondral lesions are among the injuries sustained by youth athletes who participate in high-volume and high-demand upper extremity sports. Osteochondral lesions or osteochondritis dissecans (OCD) lesions of the elbow cause pain that may limit activity and function in sport with decreased range of motion (ROM), particularly in athletes with repetitive overhead motion; the cause may be related to repetitive stresses or microtrauma across the radiocapitellar joint or tenuous vascular supply with microvascular disruption.8,12,21 Diagnosis of these lesions is confirmed on imaging, with frequent use of radiographs and magnetic resonance imaging (MRI), although ultrasound has been used as a screening method for further investigation.10,16,18,21,31 Lesions may be classified as stable or unstable. Stable lesions are defined by an open capitellar growth plate, localized flattening or radiolucency of subchondral bone on radiographs, absence of surrounding signal abnormality on T2-weighted MRI, and normal elbow ROM.24,25 However, unstable lesions are characterized by one of the following: closed capitellar growth plate, lesion fragmentation on plain radiographs, high signal intensity on T2-weighted MRI, or restricted ROM by ≥20° on examination.24,25
Osteochondral lesions of the elbow remain a difficult entity to treat, and variability in outcomes makes counseling patients and parents challenging. Stable lesions may undergo a trial of nonoperative management. Current literature demonstrates that early-stage lesions have a healing rate of 53% to 91% without surgery.17,19,20,24 Lack of compliance, cystlike lesions, and large lesion areas have been associated with inferior outcomes of nonoperative management.19,20 A recent study also showed that radial head enlargement in the affected arm and advanced skeletal age in the affected versus nonaffected elbow were predictive of later-stage capitellar OCD and therefore potentially poorer healing rates with nonoperative treatment.9 Although many lesions may be treated nonoperatively—particularly if the patient has open physes or a stable lesion—the later the stage, the lower the likelihood of successful nonoperative management.19,20,24 Unstable lesions have worse success with nonoperative treatment, only 9% to 11%, and are therefore most frequently treated with surgery.19,24 Surgical techniques include fragment fixation, microfracture, and cartilage restoration procedures.29
While osteochondral lesions of the knee have been more frequently studied, there is limited literature discussing return to sport at short- and midterm follow-up in patients with elbow OCD, particularly for patients treated with nonosteochondral grafting procedures such as lesion fixation and microfracture. The purpose of this study was to evaluate the short- and midterm clinical outcomes of arthroscopic osteochondral lesion treatment in a cohort of pediatric and adolescent patients and its effects on sporting activity, including return to sport and whether patients returned to their sport of choice.
Methods
This was a retrospective study of consecutively treated patients who underwent surgical treatment for osteochondral lesions of the elbow between 2012 and 2019 by a single surgeon (N.K.P.) at a single tertiary referral center. All patients had been referred to our institution after nonoperative treatment had failed, either guided by another clinician or initiated at our center. All included patients had confirmed osteochondral lesions of the elbow as diagnosed via MRI. Patients with concomitant ligamentous instability requiring reconstruction or repair, skeletal dysplasia, neuromuscular disorders, or <6 months of follow-up were excluded. This study was deemed exempt from institutional review board approval.
Patients with stable lesions on MRI underwent a course of rest, immobilization, and/or activity restriction for at least 3 months. If they had ongoing pain, these patients then underwent surgical intervention as outlined here. Patients with unstable lesions and/or loose bodies proceeded directly to surgical intervention.
Patients first underwent diagnostic elbow arthroscopy in the lateral decubitus position using a 2.7-mm 30° arthroscope. Any concomitant intra-articular pathology was addressed as encountered. Stable lesions underwent transarticular drilling using an 0.062-inch Kirschner wire. If loose and/or unstable osteochondral fragments were found to be viable, they were secured primarily using bioabsorbable fixation pins (SmartNails; ConMed Linvatec Biomaterials). Loose fragments found to be nonviable were removed. The donor site was then debrided in these cases, and the lesions underwent microfracture using chondral picks. In 2 cases, the microfracture was augmented with BioCartilage (Arthex). If visualization or instrumentation was difficult, a posterior mini-arthrotomy was made if indicated, which was used in all instances of fragment fixation.
Postoperatively, patients were discharged home and wore a posterior splint for 3 to 7 days. They were then transitioned to a hinged elbow brace with motion from 0° to 90° allowed. At 6 weeks postoperatively, patients were transitioned out of their brace and permitted full motion and nonweightbearing strengthening. At approximately 3 months postoperatively, if radiographs demonstrated progressive healing, patients were allowed to begin weightbearing strengthening and plyometric work. Healing was assessed on radiographs via resolution of preoperative lucency, sclerosis of the lesion, and return of articular contour. Return to sport was allowed when patients demonstrated pain-free symmetric strength and motion with radiographic healing. We recorded the type of sport to which patients returned as well as the number of months postoperatively at which they returned.
Demographic data collected included patient sex, age at the time of surgery, hand dominance, and preoperative preferred sports. Pre- and postoperative elbow ROM was measured clinically on the day of surgery and at time of final follow-up. Osteochondral lesion location and MRI findings, including osteochondral lesion size, were noted. Intraoperative findings were documented and retrieved from operative reports. Cartilage injury was recorded using the International Cartilage Repair Society classification system as well as the Outerbridge classification of chondral injury. The type of surgical management was included. The primary outcome was return to sporting activity, and secondary outcomes included ROM, radiographic healing, and complications. Data were analyzed and reported with descriptive statistics; unless otherwise noted, continuous data are expressed as mean and standard deviation with ranges where indicated. Comparisons were made of quantitative data utilizing 2-tailed t tests; for ROM, paired-sample t tests were used, whereas for other variables, independent-samples t tests were used. Level of statistical significance was set at alpha <.05.
Results
A total of 37 elbows underwent arthroscopic treatment during the study period. Six elbows had inadequate records and were excluded. After another 6 elbows with <6-month follow-up were excluded, 23 patients (25 elbows) were included and had a mean follow-up of 23.5 months (median, 19.6 months; range, 6-60.3 months). Of 25 elbows, 17 (68%) had a minimum follow-up of approximately 1 year, and 13 (52%) had at least 1.5 years of follow-up. Mean age at the time of surgery was 13.8 years (range, 11.3-17.0 years). Nineteen male and 4 female athletes (2 of whom had bilateral lesions) were involved in the following sports: baseball (9), tennis and baseball (1), baseball and water polo (1), gymnastics (4), basketball (3), lacrosse (1), golf (1), football and soccer (1), football (1), and swimming and water polo (1). Including patients who played baseball and another sport, 11 patients played baseball in some capacity (Table 1).
Table 1.
Patient Baseline Data and Sporting Informationa
| Patient Identifier | Age at Surgery, y | Physeal Status | Sex | Lesion Laterality | Final Follow-up, mo | Initial Sports of Choice | Change in Sport | RTS Clearance, mo |
|---|---|---|---|---|---|---|---|---|
| A | 12.6 | Open | F | L | 52.2 | Gymnastics | N | 4 |
| A | 13.2 | Closed | F | R | 45.1 | Gymnastics | N | 4 |
| B | 12 | Open | M | R | 7.9 | Football, soccer | N | 7 |
| C | 12.7 | Open | M | L | 60.3 | Basketball | N | 4 |
| D | 16.3 | Closed | M | R | 19.6 | Basketball | N | 5 |
| E | 15.8 | Closed | M | R | 42.5 | Baseball | N | 4 |
| F | 11.3 | Open | M | R | 6.0 | Baseball | N | 5 |
| G | 12.9 | Closed | M | L | 39.9 | Baseball | N | 2.5 |
| H | 14.1 | Open | M | R | 55.3 | Football | N | 6 |
| I | 11.4 | Open | M | R | 6.0 | Baseball | N | 3 |
| J | 15.9 | Open | M | R | 28.5 | Lacrosse | N | 4 |
| K | 14.8 | Open | M | R | 27.9 | Golf | N | 3 |
| L | 15.4 | Open | M | R | 8.2 | Basketball | N | 3 |
| M | 13.8 | Closed | M | R | 12.7 | Baseball | N (continued baseball but stopped pitching) | 5 |
| N | 12 | Open | F | L | 22.1 | Gymnastics | N | 5 |
| N | 12.1 | Open | F | R | 20.2 | Gymnastics | N | 3 |
| O | 15 | Closed | M | R | 10.0 | Baseball | N | 6 |
| P | 15.8 | Open | M | R | 7.1 | Swimming, water polo | N | 3 |
| Q | 13.5 | Open | M | R | 12.2 | Baseball | N | 5 |
| R | 12.5 | Open | M | R | 40.7 | Baseball, water polo | Stopped baseball, continued water polo | 5 |
| S | 14.1 | Closed | F | L | 12.4 | Gymnastics | Switched to lacrosse and water polo | 3 |
| T | 12.6 | Open | M | R | 10.3 | Baseball | Switched to basketball | 4.5 |
| U | 12.6 | Open | F | R | 23.3 | Gymnastics | Stopped sports | 4 |
| V | 17 | Closed | M | R | 11.9 | Baseball | Stopped sports | 8 |
| W | 14.6 | Closed | M | R | 6.0 | Baseball, tennis | Stopped baseball, continued tennis | 6 |
aThe highlighted rows indicate single patients with bilateral osteochondral lesions treated at different times. F, female; L, left; M, male; N, no change in sport of choice; R, right; RTS, return-to-sport.
Sixteen (64%) elbows had open physes on imaging at the time of surgical management. Of the 25 lesions, locations included the capitellum (22), trochlea (2), and radial head (1). All 23 patients were right-handed, and there were 20 of 25 (80%) dominant-sided lesions, including 10 of 11 in those playing baseball. The 2 patients with bilateral lesions were gymnasts. All cases were primary surgery.
There was significant improvement from pre- to postoperative ROM, including extension (6.4° ± 5.3° to 0.04° ± 0.2°; P < .00001), flexion (129.2° ± 10.6° to 138.6° ± 4.4°; P = .00013), and arc of ROM (122.6° ± 13.2° to 138.6° ± 4.4°; P < .00001) (Table 2).
Table 2.
Pre- and Postoperative Elbow ROMa
| Preoperative ROM, deg | Postoperative ROM, deg | |||||
|---|---|---|---|---|---|---|
| Patient Identifier | Extension | Flexion | Elbow Arc | Extension | Flexion | Elbow Arc |
| A | 0 | 140 | 140 | 0 | 140 | 140 |
| A | 10 | 120 | 110 | 0 | 140 | 140 |
| B | 0 | 140 | 140 | 0 | 120 | 120 |
| C | 5 | 140 | 135 | 0 | 140 | 140 |
| D | 5 | 140 | 135 | 0 | 140 | 140 |
| E | 0 | 120 | 120 | 0 | 135 | 135 |
| F | 0 | 100 | 100 | 0 | 140 | 140 |
| G | 0 | 140 | 140 | 0 | 140 | 140 |
| H | 5 | 135 | 130 | 0 | 140 | 140 |
| I | 10 | 130 | 120 | 0 | 140 | 140 |
| J | 10 | 130 | 120 | 0 | 140 | 140 |
| K | 5 | 130 | 125 | 0 | 140 | 140 |
| L | 10 | 130 | 120 | 0 | 140 | 140 |
| M | 20 | 110 | 90 | 1 | 140 | 139 |
| N | 10 | 130 | 120 | 0 | 140 | 140 |
| N | 5 | 130 | 125 | 0 | 140 | 140 |
| O | 10 | 130 | 120 | 0 | 140 | 140 |
| P | 10 | 130 | 120 | 0 | 140 | 140 |
| Q | 10 | 130 | 120 | 0 | 140 | 140 |
| R | 15 | 130 | 115 | 0 | 140 | 140 |
| S | 10 | 120 | 110 | 0 | 130 | 130 |
| T | 0 | 140 | 140 | 0 | 140 | 140 |
| U | 5 | 110 | 105 | 0 | 140 | 140 |
| V | 0 | 140 | 140 | 0 | 140 | 140 |
| W | 5 | 130 | 125 | 0 | 140 | 140 |
aElbow arc ROM is calculated as flexion minus extension. ROM, range of motion.
Mean intraoperative lesion area, as measured arthroscopically via its medial-to-lateral and superior-to-inferior dimensions (not including lesion depth), was 81.9 ± 59.3 mm2 (range, 15-225 mm2) (Table 3). Three patients underwent surgical fixation of the lesion; the remainder (22 elbows) underwent microfracture and removal of loose bodies. Two patients had microfracture augmented with BioCartilage. Four patients had a mini-arthrotomy, 3 of which were to assist with fragment fixation and 1 to facilitate use of BioCartilage. Mean tourniquet time was 40.8 ± 11.6 minutes (Table 4).
Table 3.
MRI and Intraoperative Findingsa
| Patient Identifier | Lesion Location | Non-OCD MRI findings | Intraoperative findings | OCD Lesion Area, mm2 | ICRS Stage |
|---|---|---|---|---|---|
| A | Capitellumb | None | Loose bodies | 100 | IV |
| A | Capitellum | None | Loose body | 81 | IV |
| B | Capitellum | None | Unstable | 144 | III |
| C | Trochlea | Cubitus varus | Outerbridge 4 trochlea, no loose body | 35 | III |
| D | Capitellum | None | Unstable | 150 | III |
| E | Capitellum | Loose bodies | Loose body | 64 | IV |
| F | Capitellum | Loose body | Loose body | 64 | IV |
| G | Capitellum | Loose body, UCL strain | Loose body, healed capitellar lesion, Outerbridge 1 and 2 in RC and UH joints | 150 | IV |
| H | Capitellum | Loose body | Loose bodies, synovitis, Outerbridge 2 UH and radial head | 15 | IV |
| I | Capitellum | Effusion | Stable, Outerbridge 1-2 changes in capitellum with cartilage softening and fissuring, no other loose bodies | 60 | II |
| J | Radial head | None | Stable, no loose body, scattered Outerbridge 1-2 changes in capitellum | 100 | III |
| K | Capitellum | None | Stable, Outerbridge 3-4 changes in capitellum | 56 | III |
| L | Capitellum | None | Loose body, stable ligamentous examination | 40 | IV |
| M | Capitellum | Subchondral cyst radial head | Multiple loose bodies, stable, Outerbridge 3-4 capitellum, Outerbridge 1-2 radial head | 50 | IV |
| N | Capitellum | Synovitis | Loose body in joint, synovitis | 35 | IV |
| N | Capitellum | Loose body, medial epicondylitis | Loose body in joint, synovitis | 35 | IV |
| O | Capitellum | Loose body, synovitis | Loose body in joint, synovitis | 35 | IV |
| P | Capitellum | Loose body, chondral wear radial head | Loose bodies × 2, Outerbridge 2 changes in radial head and UH joint | 225 | IV |
| Q | Capitellum | Medial epicondyle apophysitis, signal in anterior band of UCL, ulnar neuritis, triceps tendinopathy | Loose bodies × 2, Outerbridge 2 changes in UH joint, synovitis | 150 | IV |
| R | Capitellum | Synovitis | Loose body | 64 | IV |
| S | Capitellum | UCL strain | Loose body, Outerbridge 2 UH joint | 60 | IV |
| T | Capitellum | None | Loose body, Outerbridge 1-2 changes in UH and radial head, synovitis | 50 | IV |
| U | Capitellum | None | Unstable, Outerbridge 2 changes in radial head, synovitis | 225 | III |
| V | Trochlea | UCL strain, signal around ulnar nerve | Outerbridge 3-4 changes in trochlear, synovitis | 25 | III |
| W | Capitellum | Loose body | Loose body, synovitis | 35 | IV |
aICRS, International Cartilage Repair Society; MRI, magnetic resonance imaging; OCD, osteochondritis dissecans; RC, radiocapitellar; UCL, ulnar collateral ligament; UH, ulnohumeral.
bPatient/elbow ultimately underwent revision surgery with osteochondral transfer system with allograft.
Table 4.
Surgical Procedures Performeda
| Patient Identifier | Lesion Location | Lesion Fixation | Microfracture | Chondroplasty | BioCartilage | Mini-arthrotomy | Tourniquet time, min |
|---|---|---|---|---|---|---|---|
| A | Capitellum b | — | ** | ** | — | — | 42 |
| A | Capitellum | — | ** | ** | — | — | 55 |
| B | Capitellum | ** | — | ** | — | ** | 48 |
| C | Trochlea | — | ** | ** | — | — | 42 |
| D | Capitellum | ** | — | ** | — | ** | 67 |
| E | Capitellum | — | ** | ** | — | — | 51 |
| F | Capitellum | — | ** | ** | — | — | 49 |
| G | Capitellum | — | ** | ** | — | — | 28 |
| H | Capitellum | — | ** | ** | — | — | 44 |
| I | Capitellum | — | ** | ** | — | — | 26 |
| J | Radial head | — | ** | ** | — | — | 28 |
| K | Capitellum | — | ** | ** | — | — | 32 |
| L | Capitellum | — | ** | ** | — | — | 28 |
| M | Capitellum | — | ** | ** | ** | ** | 60 |
| N | Capitellum | — | ** | ** | — | — | 23 |
| N | Capitellum | — | ** | ** | — | — | 32 |
| O | Capitellum | — | ** | ** | — | — | 35 |
| P | Capitellum | — | ** | ** | — | — | 38 |
| Q | Capitellum | — | ** | ** | ** | — | 60 |
| R | Capitellum | — | ** | ** | — | — | 39 |
| S | Capitellum | — | ** | ** | — | — | 39 |
| T | Capitellum | — | ** | ** | — | — | 46 |
| U | Capitellum | ** | — | ** | — | ** | 42 |
| V | Trochlea | — | ** | ** | — | — | 35 |
| W | Capitellum | — | ** | ** | — | — | 32 |
aTwo asterisks indicate Yes, procedure performed. A dash indicates No, procedure not performed.
bPatient/elbow ultimately underwent revision surgery with osteochondral transfer system with allograft.
All 25 (100%) elbows demonstrated radiographic healing on postoperative imaging before return to sport (Figures 1 and 2). Mean time to clearance for return to sport for the cohort was 4.48 ± 1.38 months (range, 2.5-8 months) postoperatively.
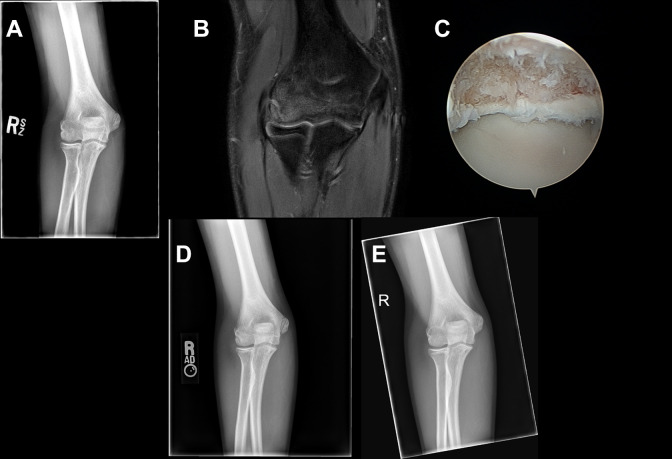
Figure 1.
(A) Preoperative anteroposterior radiograph and (B) selected T2 coronal magnetic resonance image of a 14-year-old male (patient H) with a right capitellar osteochondral lesion who underwent arthroscopic loose body removal and microfracture. (C) Arthroscopic image demonstrates the osteochondral defect prior to microfracture. (D) Three-month and (E) 6-month postoperative anteroposterior radiographs show ossification of bone within the region of microfracture with healing, including resolution of lucency, sclerosis, and restoration of articular contour. Evidence of healing is present 3 months postoperatively.
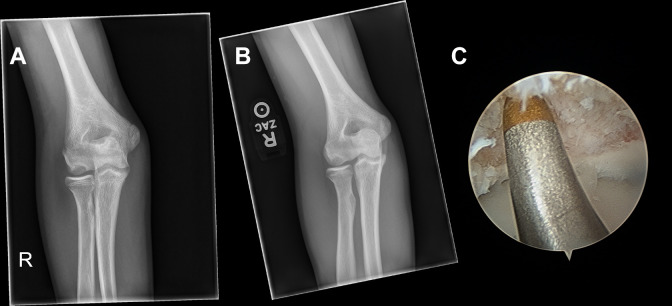
Figure 2.
(A) Preoperative and (B) 3-month postoperative anteroposterior radiographs of a right elbow in a 13-year-old male pitcher (patient Q) with a capitellar osteochondral defect. In the 3-month postoperative radiograph, there is evidence of early ossification and restoration of the articular contour. (C) Arthroscopic image demonstrates the patient’s capitellar osteochondral defect that is undergoing microfracture with the microfracture awl.
One elbow (4%) underwent revision surgery involving the osteochondral transfer system using allograft (OATS). This patient (patient A) underwent a primary procedure of arthroscopic loose body removal, chondroplasty, and microfracture. At 3 months postoperatively, radiographs showed restoration of the contour of the articular surface with increased sclerosis indicative of healing. The patient then returned to prior high-impact gymnastics activity and, after an acute injury during gymnastics, had increased pain. Radiographs and an MRI scan demonstrated a new, more anteriorly based unstable osteochondral defect in the capitellum with a loose body (Figure 3). She ultimately returned to her full activities and gymnastics after recovering from that procedure without complication. No other postoperative complications were noted in any patients.
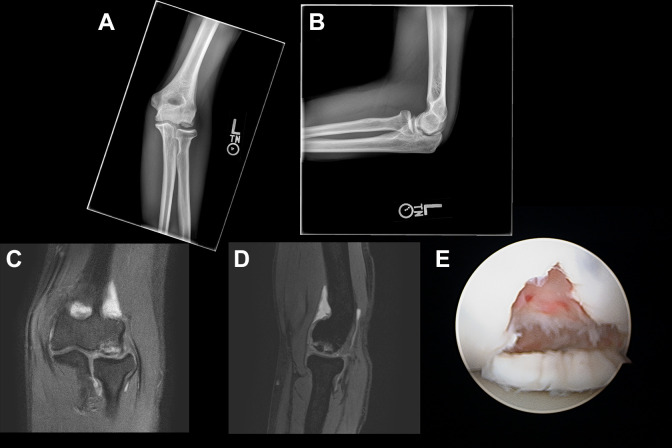
Figure 3.
(A) Anteroposterior and (B) lateral radiographs of the left elbow of a 16-year-old female gymnast (patient A) who sustained a repeat injury from continued gymnastics 2 years after arthroscopy, chondroplasty, microfracture, and loose body removal and required an OATS procedure. After the index procedure, there was restoration of the articular contour and sclerosis indicative of radiographic healing 3 months postoperatively. These radiographs are from just before the OATS procedure and illustrate the new large capitellar osteochondral defect that did not resolve with nonoperative management. Selected T2 (C) coronal and (D) sagittal magnetic resonance images of the left elbow. Imaging was obtained before the OATS procedure and demonstrates an unstable osteochondral fragment. (E) Arthroscopic image shows the large capitellar osteochondral defect after repeat injury. After the OATS procedure, the patient had clinical and radiographic healing and was able to return to full activities, including gymnastics. OATS, osteochondral transfer system with allograft.
Of 23 patients, 6 (26.1%; 6 elbows) changed sports (3) or ceased a sporting activity (3) during follow-up, including 2 gymnasts and 4 baseball players (Table 1). Between those who stopped or changed sports and those who returned to sport, there was no significant difference in age of patient, lesion size, or pre- or postoperative ROM. One patient who stopped gymnastics had undergone lesion fixation of the capitellum; the remainder who stopped or changed sports underwent microfracture. One patient who stopped baseball had a trochlear lesion, with Outerbridge 3-4 changes noted arthroscopically. The other 4 had capitellar lesions.
Of the 6 patients not returning to prior activities, 3 had open physes (50%); on the contrary, for those returning to original sport, 13 of 19 elbows had open physes (68.4%). Two of 3 (66.7%) patients undergoing fixation returned to sports, while 17 of 22 (77.3%) undergoing microfracture returned to sport. No difference existed between the groups in terms of lesion size (return to sport, 83.6 ± 56.1 mm2; change or no return to sport, 76.5 ± 74.2 mm2). Mean postoperative time to clearance to return to sporting activities did not significantly differ between those who returned to their primary sport and those who switched (4.29 ± 1.24 months and 5.08 ± 1.74 months, respectively).
Discussion
In an era of early sports specialization and increasing youth sporting activity, the frequency with which providers encounter osteochondral lesions of the elbow will increase. Matsuura et al16 analyzed 1275 youth baseball players 6 to 11 years of age with screening ultrasound 1 year after playing baseball, and those with abnormal findings went on to radiographic evaluation. Capitellar OCD had an incidence of 1.8% within a 1-year period, with a significantly greater risk in patients aged 10 to 11 years. In a slightly older group and similar evaluation, Kida et al12 found capitellar OCD at an incidence of 3.4% in >2433 adolescent competitive baseball players.
Prior studies on capitellar osteochondral lesions suggest reasonable healing rates with nonoperative management if detected at an early stage of symptom duration.17,19,20 In this cohort, patients were recommended surgical management owing to persistent pain despite nonoperative care or if they had large unstable lesions on imaging. Our patients included 25 elbows with 22 capitellar lesions, 2 trochlear lesions, and 1 radial head lesion.
In the present study, surgical techniques were limited to either lesion fixation or lesion debridement and microfracture. Fragment fixation was performed on 3 capitellar lesions. Microfracture has been suggested for patients with lesions <1 cm in diameter, although studies have reported a variety of surgical techniques for similar lesion sizes.6,29 In 2006, Brownlow et al4 utilized arthroscopic debridement and loose body removal of OCD lesions in the capitellum, and in that cohort of 29 patients, 81% were able to continue their sport of choice. This percentage is higher than that of our cohort, in which 73.9% of patients returned to their preferred sport. One possibility for this difference in return to sport is the mean age of patients, which was higher in the cohort studied by Brownlow et al (22 years) as compared with the present study (13.8 years).4 Those of older age may have stronger commitments or obligations to their sport of choice. However, other studies have reported higher return to sports.22,27 A meta-analysis published in 2016 found a 71% rate of return to prior sport for the 10 studies including debridement and marrow stimulation and a 64% rate for the 6 studies in which surgical fragment fixation was performed.29 The rate of return to play in our arthroscopic debridement and microfracture group (77.3%) is slightly higher than that of an 81-elbow series published by Bexkens et al3 (62%). In patients with more advanced lesions, it has been shown that the return-to-sport rate may be lower among patients undergoing arthroscopic treatment.23,26
Patients were unable to return to sport because of pain and/or surgical counseling to avoid high-demand and high-impact activities. In total, 36.4% (4/11) of those playing baseball and 50% (2/4) of those partaking in gymnastics did not return to their respective preinjury sporting activity. This is consistent with previous data showing lower percentages of return to sport among these populations.5,26 Gymnasts and baseball players experience significant loading across the radiocapitellar joint. The compression and shear forces during the late cocking and early acceleration phases of throwing primarily load an elbow flexion range between 30° and 90°, while gymnasts tend to load their elbow more in extension. These specific loading patterns can lead to differences in capitellar lesion location.11 The repetitive stresses seen in these 2 sports are perhaps greater than those of the other sporting activities included in this cohort and may explain their worse outcomes. Moreover, while baseball players tend to place more stress on their dominant side, gymnasts may bear more similar loads in each arm. In the present cohort, 10 of 11 baseball players had their dominant/throwing side affected, and the 2 patients with bilateral lesions were gymnasts.
Prior evidence suggests that of the common surgical procedures performed for osteochondral lesions of the elbow, OATS has the highest return to preinjury level of sporting activity.7,29 However, OATS is often reserved for large, unstable, and uncontained OCD lesions and revision cases.1 Given the poor return to sporting activity in the gymnasts and baseball players in the present cohort independent of lesion size, we suggest that OATS or other cartilage restoration procedures be strongly considered in these higher-demand adolescent athletes with seemingly worse return to play. Another cohort study reported a lower return to preinjury sporting activity with arthroscopic debridement, drilling, and chondroplasty.26 Two separate meta-analyses noted a 94% rate of return to primary sport among patients who underwent OATS.14,29 Therefore, for those patients with a strong desire to return to preinjury sport or for those with higher upper extremity demands, cartilage restoration may be better suited.
Another variable that may affect the return-to-sport rate is the status of the physes. A higher percentage of patients returning to sport had open physes (68.4%) as compared with those unable to return (50%). This is in line with prior data suggesting that patients with open physes or those who are younger have better outcomes with operative and nonoperative management.3,9,15,19,20
We observed significant improvements in ROM in flexion, extension, and arc of elbow motion in this cohort, without difference with respect to surgical technique or sporting activities. Prior authors have also demonstrated improvements in flexion and/or extension ROM.3,26,30 Bexkens et al3 found significant improvements in flexion (134° to 139°; P < .001) and extension (8° to 3° deficit; P < .001) ROM after microfracture and debridement for capitellar OCD. There were no postoperative complications noted aside from the 1 patient who later underwent OATS. The techniques of arthroscopic debridement and loose body removal, microfracture, and chondroplasty and fragment fixation therefore appear safe in this patient cohort. It is interesting that despite the inability to continue with sporting, all patients in this study demonstrated radiographic healing on follow-up with the arthroscopic techniques used. Radiographs, however, have been shown to have poorer sensitivity than MRI or even computed tomography imaging when detecting osteochondral lesions.13,28 Although computed tomography has been used to evaluate healing, it does not appear to correlate with outcome measures.2 As such, the radiographic healing evident in all the patients in the present study may not be of high utility in counseling patients and parents on functional recovery. In high-demand athletes such as gymnasts and baseball players, it may be worthwhile to obtain postoperative MRI to evaluate for incomplete healing that is difficult to detect on radiographs, particularly if the athletes are returning to sport.
The retrospective nature of this study limits its interpretation. Based on the heterogeneity in treatment and the lack of a control group in the present study, the data should be interpreted with some caution. The present study utilized arthroscopic surgical treatments, including debridement and microfracture or fragment fixation. The duration of follow-up was short- or midterm; therefore, return to original sport may have occurred at a later time than what the study follow-up period captured. Longer follow-up may provide further information on recurrence of symptoms. The cohort evaluated is of small sample size; as such, comparisons between those who stopped or changed sports and those who were able to return are limited in interpretation, particularly given the smaller numbers in the former group. As this was a single-surgeon, single-institution study, outcomes are subject to that surgeon’s technique and recommendations for the assigned surgical procedures. Patient-reported outcome measures were not administered in the present study and would be important to follow to discern at which point patients note improvement postoperatively. We evaluated return to sport but are unable to comment on the performance metrics of these pediatric patients in our cohort. Radiographs were used to evaluate postoperative healing on imaging, which are less revealing than computed tomography or MRI; however, in the practice of the senior surgeon, use of postoperative advanced imaging is not routine. Ultimately, this study adds to the literature on short- and midterm outcomes and return to sport in patients with osteochondral lesions in the elbow treated with noncartilage restoration techniques.
Conclusion
Osteochondral lesions of the elbow pose a treatment challenge, and the incidence of such lesions may be rising with increased demands on youth athletes. Arthroscopic technique with lesion debridement and microfracture or fixation appears safe and results in radiographic healing; however, there remains a high rate of inability to return to sport in patients involved in higher-demand upper extremity activity, such as baseball and gymnastics. Further treatment strategies in these patients, including cartilage restoration procedures, may be warranted.
Footnotes
Final revision submitted May 6, 2020; accepted June 6, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: N.K.P. has received consulting fees from OrthoPediatrics and educational support from Evolution Surgical. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Institutional review board exemption was granted from UCSF Benioff Children’s Hospital Oakland (No. 161122).
References
- 1. Bae DS, Ingall EM, Miller PE, Eisenberg K. Early results of single-plug autologous osteochondral grafting for osteochondritis dissecans of the capitellum in adolescents. J Pediatr Orthop. 2020;40(2):78–85. [DOI] [PubMed] [Google Scholar]
- 2. Bexkens R, van Bergen CJA, van den Bekerom MPJ, Kerkhoffs GMMJ, Eygendaal D. Decreased defect size and partial restoration of subchondral bone on computed tomography after arthroscopic debridement and microfracture for osteochondritis dissecans of the capitellum. Am J Sports Med. 2018;46(12):2954–2959. [DOI] [PubMed] [Google Scholar]
- 3. Bexkens R, van den Ende KIM, Ogink PT, van Bergen CJA, van den Bekerom MPJ, Eygendaal D. Clinical outcome after arthroscopic debridement and microfracture for osteochondritis dissecans of the capitellum. Am J Sports Med. 2017;45(10):2312–2318. [DOI] [PubMed] [Google Scholar]
- 4. Brownlow HC, O’Connor-Read LM, Perko M. Arthroscopic treatment of osteochondritis dissecans of the capitellum. Knee Surg Sports Traumatol Arthrosc. 2006;14(2):198–202. [DOI] [PubMed] [Google Scholar]
- 5. Byrd JWT, Jones KS. Arthroscopic surgery for isolated capitellar osteochondritis dissecans in adolescent baseball players: minimum three-year follow-up. Am J Sports Med. 2002;30(4):474–478. [DOI] [PubMed] [Google Scholar]
- 6. Camp CL, Dines JS, Degen RM, Sinatro AL, Altchek DW. Arthroscopic microfracture for osteochondritis dissecans lesions of the capitellum. Arthrosc Tech. 2016;5(3):e477–e481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cheng C, Milewski MD, Nepple JJ, Reuman HS, Nissen CW. Predictive role of symptom duration before the initial clinical presentation of adolescents with capitellar osteochondritis dissecans on preoperative and postoperative measures: a systematic review. Orthop J Sports Med. 2019;7(2):2325967118825059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Churchill RW, Munoz J, Ahmad CS. Osteochondritis dissecans of the elbow. Curr Rev Musculoskelet Med. 2016;9(2):232–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Funakoshi T, Furushima K, Miyamoto A, Kusano H, Horiuchi Y, Itoh Y. Predictors of unsuccessful nonoperative management of capitellar osteochondritis dissecans. Am J Sports Med. 2019;47(11):2691–2698. [DOI] [PubMed] [Google Scholar]
- 10. Iwame T, Matsuura T, Suzue N, Sairyo K. Cumulative incidence of osteochondritis dissecans of the capitellum in child and adolescent baseball players. Orthop J Sports Med. 2016;4(7)(suppl 4):2325967116S00111. [Google Scholar]
- 11. Kajiyama S, Muroi S, Sugaya H, et al. Osteochondritis dissecans of the humeral capitellum in young athletes: comparison between baseball players and gymnasts. Orthop J Sports Med. 2017;5(3):23259 67117692513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kida Y, Morihara T, Kotoura Y, et al. Prevalence and clinical characteristics of osteochondritis dissecans of the humeral capitellum among adolescent baseball players. Am J Sports Med. 2014;42(8):1963–1971. [DOI] [PubMed] [Google Scholar]
- 13. Kijowski R, De Smet AA. Radiography of the elbow for evaluation of patients with osteochondritis dissecans of the capitellum. Skeletal Radiol. 2005;34(5):266–271. [DOI] [PubMed] [Google Scholar]
- 14. Kirsch JM, Thomas JR, Khan M, Townsend WA, Lawton JN, Bedi A. Return to play after osteochondral autograft transplantation of the capitellum: a systematic review. Arthroscopy. 2017;33(7):1412–1420.e1. [DOI] [PubMed] [Google Scholar]
- 15. Logli AL, Bernard CD, O’Driscoll SW, et al. Osteochondritis dissecans lesions of the capitellum in overhead athletes: a review of current evidence and proposed treatment algorithm. Curr Rev Musculoskelet Med. 2019;12(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Matsuura T, Iwame T, Suzue N, et al. Cumulative incidence of osteochondritis dissecans of the capitellum in preadolescent baseball players. Arthroscopy. 2019;35(1):60–66. [DOI] [PubMed] [Google Scholar]
- 17. Matsuura T, Kashiwaguchi S, Iwase T, Takeda Y, Yasui N. Conservative treatment for osteochondrosis of the humeral capitellum. Am J Sports Med. 2008;36(5):868–872. [DOI] [PubMed] [Google Scholar]
- 18. Matsuura T, Suzue N, Iwame T, Nishio S, Sairyo K. Prevalence of osteochondritis dissecans of the capitellum in young baseball players: results based on ultrasonographic findings. Orthop J Sports Med. 2014;2(8):2325967114545298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mihara K, Tsutsui H, Nishinaka N, Yamaguchi K. Nonoperative treatment for osteochondritis dissecans of the capitellum. Am J Sports Med. 2009;37(2):298–304. [DOI] [PubMed] [Google Scholar]
- 20. Niu EL, Tepolt FA, Bae DS, Lebrun DG, Kocher MS. Nonoperative management of stable pediatric osteochondritis dissecans of the capitellum: predictors of treatment success. J Shoulder Elbow Surg. 2018;27(11):2030–2037. [DOI] [PubMed] [Google Scholar]
- 21. Otoshi K, Kikuchi S, Kato K, et al. Age-specific prevalence and clinical characteristics of humeral medial epicondyle apophysitis and osteochondritis dissecans: ultrasonographic assessment of 4249 players. Orthop J Sports Med. 2017;5(5):2325967117707703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rahusen FTG, Brinkman J-M, Eygendaal D. Results of arthroscopic debridement for osteochondritis dissecans of the elbow. Br J Sports Med. 2006;40(12):966–969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Schoch B, Wolf BR. Osteochondritis dissecans of the capitellum: minimum 1-year follow-up after arthroscopic debridement. Arthroscopy. 2010;26(11):1469–1473. [DOI] [PubMed] [Google Scholar]
- 24. Takahara M, Mura N, Sasaki J, Harada M, Ogino T. Classification, treatment, and outcome of osteochondritis dissecans of the humeral capitellum. J Bone Joint Surg Am. 2007;89(6):1205–1214. [DOI] [PubMed] [Google Scholar]
- 25. Takeda H, Watarai K, Matsushita T, Saito T, Terashima Y. A surgical treatment for unstable osteochondritis dissecans lesions of the humeral capitellum in adolescent baseball players. Am J Sports Med. 2002;30(5):713–717. [DOI] [PubMed] [Google Scholar]
- 26. Tis JE, Edmonds EW, Bastrom T, Chambers HG. Short-term results of arthroscopic treatment of osteochondritis dissecans in skeletally immature patients. J Pediatr Orthop. 2012;32(3):226–231. [DOI] [PubMed] [Google Scholar]
- 27. Uchida S, Utsunomiya H, Taketa T, et al. Arthroscopic fragment fixation using hydroxyapatite/poly-L-lactate acid thread pins for treating elbow osteochondritis dissecans. Am J Sports Med. 2015;43(5):1057–1065. [DOI] [PubMed] [Google Scholar]
- 28. van den Ende KIM, Keijsers R, van den Bekerom MPJ, Eygendaal D. Imaging and classification of osteochondritis dissecans of the capitellum: x-ray, magnetic resonance imaging or computed tomography? Shoulder Elbow. 2019;11(2):129–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Westermann RW, Hancock KJ, Buckwalter JA, Kopp B, Glass N, Wolf BR. Return to sport after operative management of osteochondritis dissecans of the capitellum: a systematic review and meta-analysis. Orthop J Sports Med. 2016;4(6):2325967116654651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wulf CA, Stone RM, Giveans MR, Lervick GN. Magnetic resonance imaging after arthroscopic microfracture of capitellar osteochondritis dissecans. Am J Sports Med. 2012;40(11):2549–2556. [DOI] [PubMed] [Google Scholar]
- 31. Yang T-H, Lee Y-Y, Huang C-C, et al. Effectiveness of ultrasonography screening and risk factor analysis of capitellar osteochondritis dissecans in adolescent baseball players. J Shoulder Elbow Surg. 2018;27(11):2038–2044. [DOI] [PubMed] [Google Scholar]