Abstract
Objective
The Intular Scope™ (Medical Park, South Korea) (IS) is a video-lighted stylet that can be used for endotracheal intubation with excellent visualization by adding a camera to its end. We compared the efficacy of a direct laryngoscope (DL) with that of the IS based on hemodynamic changes, ease of intubation, and postoperative airway morbidities.
Methods
Seventy patients with expected normal airways were randomized for intubation using an IS (n = 35) or DL (n = 35). The primary outcome was the mean arterial pressure during intubation. The secondary outcomes were the time to intubation (TTI), percentage of glottic opening (POGO) score, and number of intubation attempts. The incidence and severity of bleeding, hoarseness, and sore throat after intubation were also recorded.
Results
Hemodynamic changes during intubation were not significantly different between the groups. The TTI was longer in the IS than DL group. The POGO score was higher in the IS than DL group. Hoarseness and sore throat were significantly less severe in the IS than DL group.
Conclusions
Using the IS did not significantly improve hemodynamics and resulted in a longer TTI. However, the IS was associated with less severe postoperative airway morbidities compared with the DL.
Keywords: Direct laryngoscope, hemodynamic change, Intular Scope™, endotracheal intubation, mean arterial pressure, time to intubation
Introduction
Direct laryngoscopy is the most common and conventional method of intubation performed in the operating room. However, direct laryngoscopic intubation is difficult in 4.5% to 7.5% of patients.1 A lighted stylet is frequently used for tracheal intubation in patients undergoing general anesthesia and as an alternative to a direct laryngoscope (DL) in patients with anticipated intubation difficulties.2 Indications for lighted stylet-assisted tracheal intubation include difficult intubation in patients with limited cervical spine immobility, jaw immobility, excessive bleeding or airway secretions, and facial anomalies.2 However, a lighted stylet has the following disadvantages: it does not provide direct visualization of the vocal cords during intubation, and the intubation conditions may be affected by the operating room lighting, patient’s skin color, or patient’s body habitus (especially obesity). Additionally, because lighted stylet-assisted tracheal intubation is a blind method, esophageal intubation and airway trauma may occur. The Intular Scope™ (Medical Park, South Korea) (IS) is a recently developed video-lighted stylet that overcomes these limitations. The IS provides excellent visualization of the larynx by the addition of a camera to its end.
During endotracheal intubation, the distension force exerted on supraglottic tissues by the traditional DL may be a major cause of hemodynamic responses such as hypertension and tachycardia.3,4 Thus, minimizing laryngeal stimulation or avoiding direct laryngoscopy may attenuate these sympathetic responses. Rhee et al.5 reported that a lighted stylet attenuated the hemodynamic responses that occurred during intubation. In the present study, we hypothesized that endotracheal intubation using an IS would more effectively attenuate the hemodynamic responses than endotracheal intubation using a DL. We compared a DL with an IS while performing intubation in patients with a normal airway in terms of hemodynamic changes during intubation, ease of intubation, time to intubation (TTI), and postoperative airway morbidities.
Patients and methods
This study was approved by the Institutional Review Board of Gil Medical Center in Incheon, South Korea (GDIRB 2018-291), and all patients provided written informed consent. The study involved patients aged 20 to 65 years with an American Society of Anesthesiologists physical status of 1 to 2 who were scheduled for elective surgery with orotracheal intubation. The patients were randomized for intubation using either an IS (IS group) or DL (DL group) by computer-generated random numbers (Figure 1). The exclusion criteria were a history of difficult airway; upper airway abnormalities such as airway inflammation, tumors, abscesses, foreign bodies, or known cervical spine injury; morbid obesity (body mass index of >30 kg/m2); performance of rapid sequence induction; uncontrolled systemic hypertension; and performance of an emergency operation.
Figure 1.
Patient flow diagram.
IS, Intular Scope; DL, direct laryngoscope.
The IS is a flexible fiberoptic device similar to a lighted stylet with a 38-cm-long shaft and a 5-mm outer diameter. Its distal angle can be flexibly modified before tracheal intubation, whereas it is stiff enough to maintain its shape (Figure 2(a) and (b)). Additionally, the device is considered an endoscope because image transmission occurs by a sensor of an image. An image of the upper airway is obtained through the lens of an endoscope, and the signal of the image is then displayed through a USB cable on the screen of a smart device such as a smartphone or tablet PC using an Android system (Figure 2(c)). The displayed image is considered beneficial when performing tracheal intubation, allowing the clinician to monitor the pharyngeal and laryngeal structures. Because a smartphone or tablet monitor is used together with this device, no additional light source or monitor system is required. The “Intular Scope” application, which is now freely available through Google Play, can be easily downloaded onto smart devices that use the Android system. Additionally, because the IS is a disposable device, it can reduce the risk of infection.
Figure 2.
Intular Scope. (a) Structure of the Intular Scope. The Intular Scope comprises (1) a distal lens with a camera, (2) a bendable shaft, (3) a connector to fix the endotracheal tube, (4) a handle to use after intubation, and (5) a cable to connect to a smart device. (b) Lens of the Intular Scope. The lens of the Intular Scope includes (1) a camera, (2) a flexible copper tube, and (3) a cover glass to prevent decomposure of the camera and copper tube. (c) The Intular Scope was bent at a 90° angle 6.5 cm from the distal end before intubation.
In the pre-anesthesia room, we assessed the patients’ Mallampati score, thyromental distance, upper incisor status (normal, absent, or loose), inter-incisor distance, and cervical spine mobility (normal, reduced, or fixed). None of the patients received premedication. In the operating room, we monitored the electrical activity of the heart, amount of oxygen in the body, and depth of sedation using an electrocardiogram, pulse oximeter, and bispectral index (BIS) monitor (BIS VISTA Monitor Revision 3.0; Aspect Medical Systems, Norwood, MA, USA), respectively. Noninvasive blood pressure measurements were obtained from the patients’ upper arm. Before anesthetic induction and intubation, 100% oxygen was administered via a face mask. In both groups, 10 µg/kg of alfentanil, 2 mg/kg of propofol, and 0.9 mg/kg of rocuronium were administered for anesthetic induction. Hemodynamic variables and the BIS were recorded before anesthetic induction (baseline), before intubation, and at 1, 2, 3, 4, and 5 minutes after intubation.
Train-of-four (TOF) measurements were performed every 15 s using the ToFscan (IDMED, Marseille, France). Intubation was performed with adequate neuromuscular blockade when obtaining a 0 response at the TOF approximately 2 minutes after rocuronium injection. The IS was preloaded with a tracheal tube (internal diameter, 7.5 mm for men and 7.0 mm for women) and bent at a 90° angle 6.5 cm from the distal end (Figure 2(c)). After inserting the IS into the posterior pharynx and identifying the epiglottis and glottic opening, the distal tip of the IS was advanced below the glottic aperture, and the tracheal tube was advanced until the cuff passed through the glottis. Tracheal intubation using a DL was conventionally performed with a Macintosh laryngoscope. Tracheal intubation was performed by two anesthesiologists (J.Y.L. and H.J.H.), who had >4 years of clinical experience and had performed at least 20 cases of intentional scope-assisted intubation, respectively.
The TTI was defined as the time from insertion of an IS or Macintosh laryngoscope into the oral cavity to withdrawal from the oral cavity after intubation. Endotracheal intubation was confirmed by the presence of an end-tidal carbon dioxide reading. An observer measured the TTI and hemodynamic data. Another investigator performed optimal external laryngeal manipulation if requested. The operator recorded the Cormack–Lehane glottis grade (C/L grade), percentage of glottic opening (POGO) score, and oropharyngeal bleeding. The intubation time in each group was limited to 90 s per trial. If the peripheral oxygen saturation was <90% or the intubation time was >90 s, the intubation trial was stopped and manual ventilation was performed for 1 minute. Failed intubation was defined as failure of intubation despite three consecutive intubation trials using the same equipment. For failed intubation, we employed alternative equipment not used in this study (e.g., fiberoptic bronchoscope or videolaryngoscope). Anesthesia was maintained with 2% sevoflurane and 100% oxygen for 5 minutes after intubation.
Postoperative pharyngeal complications, such as sore throat and hoarseness, were assessed in the post-anesthesia care unit and 1 day after surgery.
The primary outcome variable was the mean arterial pressure (MAP) during intubation. The secondary outcomes were the TTI, POGO score, C/L grade, use of optimal external laryngeal manipulation, and number of intubation attempts. Based on a previous study,5 33 patients per group were required to detect a difference of 20 mmHg in the MAP change between the groups and to achieve an α-error of 0.05 and a β-error of 0.8. Therefore, we enrolled 35 patients per group to compensate for a 5% possible dropout rate. Statistical analyses were performed using IBM SPSS Statistics for Windows, Version 23.0 (IBM Corp., Armonk, NY, USA). Hemodynamic changes over time were compared between the groups using repeated-measures analysis of variance, and post-hoc comparisons were performed using Bonferroni’s test. The MAP and heart rate (HR) at each time point were compared using a t-test. Patients’ characteristics and induction profiles were compared using an unpaired t-test or the chi-square test. We used the Mann–Whitney U test to assess the TTI and POGO score. Statistical significance was set at P < 0.05.
Results
Seventy patients completed the study (IS group, n = 35; DL group, n = 35) (Figure 1). The patients’ age, sex, and weight did not differ between the groups. There were also no significant differences in the preoperative airway assessment (Table 1).
Table 1.
Patients’ characteristics and preoperative airway assessments.
| IS group (n = 35) | DL group (n = 35) | P value | |
|---|---|---|---|
| Sex, male/female | 14/21 | 13/22 | 0.626 |
| Age, years | 50 ± 11 | 49 ± 10 | 0.871 |
| Weight, kg | 65 ± 16 | 68 ± 14 | 0.426 |
| Height, cm | 163 ± 11 | 164 ± 9 | 0.686 |
| ASA PS, 1/2 | 15/20 | 18/17 | 0.632 |
| TMD, cm | 7.2 ± 0.8 | 7.1 ± 0.9 | 0.726 |
| Mouth opening, cm | 4.4 ± 0.4 | 4.5 ± 0.1 | 0.458 |
| ROM, normal/reduced | 31/4 | 33/2 | 0.673 |
| Upper incisors, absent/normal/loose | 1/24/10 | 0/28/7 | 0.399 |
| Mallampati class, 1/2/3/4 | 1/20/12/2 | 2/16/17/0 | 0.303 |
Values are presented as mean ± standard deviation or number of patients.
IS group, intubation using an Intular Scope; DL group, intubation using a direct laryngoscope; ASA PS, American Society of Anesthesiologists physical status; TMD, thyromental distance; ROM, range of motion of the cervical spine.
The patients’ intubation profiles are listed in Table 2. The TTI (median [interquartile range]) was significantly longer in the IS group than DL group (45 [26–64] vs. 34 [28–42] s, respectively; P < 0.001). The first-attempt failure rate was 17% in the IS group and 3% in the DL group, with no significant difference. One patient in the IS group underwent laryngoscope-assisted IS intubation after the second trial failed. The POGO score (median [interquartile range]) was 80% [70%–90%] in the IS group and 30% [20%–50%] in the DL group. No patients in either group developed desaturation events during anesthetic induction. Sore throat on the first postoperative day and hoarseness in the post-anesthesia care unit were significantly less severe in the IS group than DL group.
Table 2.
Intubation profiles.
| IS group | DL group | P value | |
|---|---|---|---|
| Time to intubation, s | 45 [26–64] | 34 [28–42] | <0.001 |
| First-attempt failure | 6 | 1 | 0.106 |
| Number of intubation attempts | 29/5/1 | 34/1/0 | 0.131 |
| POGO score, % | 80 [70–90] | 30 [20–50] | <0.001 |
| Cormack–Lehane grade, I/II/III/IV | 21/12/2/0 | 1/19/15/0 | <0.001 |
| OELM, no/yes | 5/30 | 18/17 | 0.002 |
| Bleeding, none/trace/moderate | 25/10/0 | 31/4/0 | 0.133 |
| Sore throat-PACU, none/mild/moderate/severe | 10/17/7/1 | 7/15/11/2 | 0.598 |
| Sore throat-POD 1, none/mild/moderate/severe | 24/10/1/0 | 14/14/6/1 | 0.049 |
| Hoarseness-PACU, none/mild/moderate/severe | 5/24/6/0 | 3/14/18/0 | 0.010 |
| Hoarseness-POD 1, none/mild/moderate/severe | 26/8/1/0 | 18/15/1/1 | 0.205 |
Values are presented as median [interquartile range] or number of patients.
IS group, intubation using an Intular Scope; DL group, intubation using a direct laryngoscope; POGO, percentage of glottic opening; OELM, optimal external laryngeal manipulation; PACU, post-anesthesia care unit; POD, postoperative day.
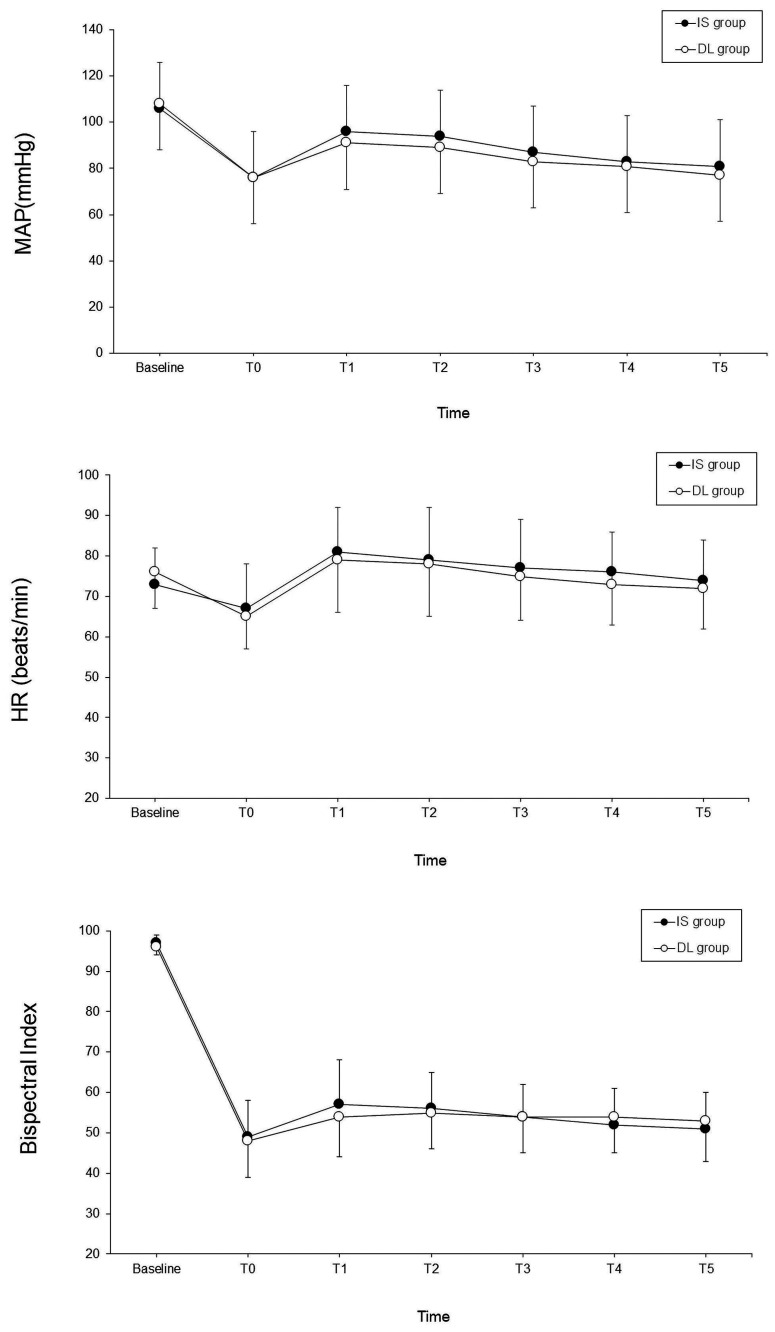
The hemodynamic changes during the operation are shown in Figure 3. There were no significant differences in the changes in the MAP, HR, or BIS over time between the groups during endotracheal intubation.
Figure 3.
Changes in MAP (upper), HR (middle), and bispectral index (lower) during intubation. There were no significant differences in the changes in the MAP, HR, and bispectral index over time between the groups during endotracheal intubation (P = 0.383, 0.253, and 0.387, respectively). Error bars represent the standard deviation. DL group (unfilled circle, ○): intubation with direct laryngoscope; IS group (filled circle, ●): intubation with Intular Scope. Baseline: pre-induction; T0: pre-intubation; T1, T2, T3, T4, and T5: 1, 2, 3, 4, and 5 minutes after intubation.
MAP, mean arterial pressure; HR, heart rate.
Discussion
This study demonstrated that although use of the IS produced hemodynamic responses similar to those of the DL during intubation, it prolonged the TTI. However, use of the IS resulted in less severe postoperative airway morbidities.
The hemodynamic changes associated with tracheal intubation have been well studied. Intubation and airway manipulation by direct laryngoscopy can cause sympathetic stimulation, resulting in hypertension and dysrhythmias. Factors contributing to these hemodynamic changes include the force used during laryngoscopy and the duration and number of intubation attempts. Distension of supraglottic tissues by direct laryngoscopy may be a major cause of these responses.4 Therefore, avoiding direct laryngoscopy may attenuate these sympathetic responses. Several studies have investigated the possibility that light wand intubation may prevent sympathetic stimulation. Hirabayashi et al.6 found no significant maximal changes in the HR or MAP during tracheal intubation. Friedman et al.7 and Knight et al.8 also found no significant hemodynamic differences during intubation. In special cases, however, some studies have shown that the use of a light wand attenuated the hemodynamic response in patients with hypertension9 or a high Mallampati score.5 In the present study, intubation was performed in patients with normal airways, and there were no hemodynamic differences between the IS and DL groups during intubation. This result might be attributed to the IS group having a longer intubation time than the DL group. This long intubation time may counterweigh the expected effect by avoiding the use of a DL. Additionally, hemodynamic changes during airway intubation are more likely to be caused by tracheal stimulation by intubation itself than by laryngeal traction by direct laryngoscopy.10
An adequate laryngeal view is essential for endotracheal intubation. The POGO score or C/L grade is used to evaluate the laryngeal view. During endotracheal intubation, the POGO score or C/L grade is reported very differently depending on the intubation device or patient’s characteristics. In a manikin study by Choi et al.,11 high POGO scores were obtained using the Pentax, C-MAC, and GlideScope (81.7% ± 18.3%, 65.4% ± 25.0%, and 72.9% ± 20.8%, respectively). In a study of obese patients by Yumul et al.,12 the POGO scores using the Video-MAC, GlideScope, and McGrath were also very high (84% ± 20%, 87% ± 16%, and 91% ± 11%, respectively). In other manikin and clinical studies, a video laryngoscope provided a good laryngeal view or high POGO score.13,14 In the present study, the IS had a mean POGO score of 75% ± 23%, similar to other videolaryngoscopes.
In this study, the TTI was longer in the IS group than DL group, probably because the IS group had a higher first-attempt failure rate than the DL group. Earlier studies have shown that a lighted stylet has no time advantage over a DL.6,15 In contrast to our results, Hung et al.16 reported that the TTI was significantly shorter when using a lighted stylet (the Trachlight) than when using a laryngoscope. In this study, the main reason for the longer TTI was difficulty in finding and entering the midline of the upper airway when inserting the IS. An Ovassapian airway or Berman airway, which is used for oral fiberoptic intubation, can be used to help guide the IS to the midline of the airway and thus overcome this limitation. Additionally, if difficult intubation is anticipated or intubation fails, direct laryngoscopy-assisted IS intubation may be helpful.
Comparison of postoperative airway morbidities between the two groups showed that sore throat on the first postoperative day and hoarseness in the recovery room immediately after surgery were significantly less severe in the IS group than DL group. These results are consistent with the results of previous reports. Friedman et al.7 showed that a lighted stylet was associated with a significantly lower incidence and severity of sore throat, hoarseness, and dysphagia than was a DL. Hung et al.16 found that fewer patients developed sore throats in the lighted stylet group than in the DL group.
Our study has several limitations. First, our study only involved patients with normal airways. The IS, similar to the lighted stylet, will be useful mainly in patients with limited cervical motion, limited mouth opening, or a difficult airway. Therefore, further studies involving patients with these difficult airway problems are required. Second, the experienced anesthesiologists were not blinded to the use of an IS or DL. Therefore, an observer effect might have occurred during the performance of intubation and affected the hemodynamic responses.13 Third, because we only compared the IS and DL, further studies comparing the IS with other lighted stylets or videolaryngoscopes might produce different results.
In conclusion, use of the IS did not provide significant improvements in hemodynamics and resulted in a longer intubation procedure. However, the IS was associated with less severe postoperative airway morbidities compared with the DL.
Footnotes
Declaration of conflicting interest: The authors declare that there is no conflict of interest.
Funding: This research was supported by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: GDIRB 2019-291).
ORCID iDs: Ho Jin Hur https://orcid.org/0000-0003-2380-3538
Hyun Jeong Kwak https://orcid.org/0000-0003-4432-8510
References
- 1.Shiga T, Wajima Z, Inoue T, et al. Predicting difficult intubation in apparently normal patients: a meta-analysis of bedside screening test performance . Anesthesiology 2005; 103: 429.–. [DOI] [PubMed] [Google Scholar]
- 2.Davis L, Cook-Sather SD, Schreiner MS. Lighted stylet tracheal intubation: a review. Anesth Analg 2000; 90: 745–756. [DOI] [PubMed] [Google Scholar]
- 3.Forbes AM, Dally FG. Acute hypertension during induction of anaesthesia and endotracheal intubation in normotensive man. Br J Anaesth 1970; 42: 618–624. [DOI] [PubMed] [Google Scholar]
- 4.Thomson IR. The haemodynamic response to intubation: a perspective. Can J Anaesth 1989; 36: 367–369. [DOI] [PubMed] [Google Scholar]
- 5.Rhee KY, Lee JR, Kim J, et al. A comparison of lighted stylet (Surch-Lite) and direct laryngoscopic intubation in patients with high Mallampati scores. Anesth Analg 2009; 108: 1215–1219. [DOI] [PubMed] [Google Scholar]
- 6.Hirabayashi Y, Hiruta M, Kawakami T, et al. Effects of lightwand (Trachlight) compared with direct laryngoscopy on circulatory responses to tracheal intubation. Br J Anaesth 1998; 81: 253–255. [DOI] [PubMed] [Google Scholar]
- 7.Friedman PG, Rosenberg MK, Lebenbom-Mansour M. A comparison of light wand and suspension laryngoscopic intubation techniques in outpatients. Anesth Analg 1997; 85: 578–582. [DOI] [PubMed] [Google Scholar]
- 8.Knight RG, Castro T, Rastrelli AJ, et al. Arterial blood pressure and heart rate response to lighted stylet or direct laryngoscopy for endotracheal intubation. Anesthesiology 1988; 69: 269–272. [DOI] [PubMed] [Google Scholar]
- 9.Kihara S, Brimacombe J, Yaguchi Y, et al. Hemodynamic responses among three tracheal intubation devices in normotensive and hypertensive patients. Anesth Analg 2003; 96: 890–895. [DOI] [PubMed] [Google Scholar]
- 10.Takahashi S, Mizutani T, Miyabe M, et al. Hemodynamic responses to tracheal intubation with laryngoscope versus lightwand intubating device (Trachlight) in adults with normal airway. Anesth Analg 2002; 95: 480–484. [DOI] [PubMed] [Google Scholar]
- 11.Choi HY, Oh YM, Kang GH, et al. A randomized comparison simulating face to face endotracheal intubation of Pentax airway scope, C-MAC video laryngoscope, Glidescope video laryngoscope, and Macintosh laryngoscope. Biomed Res Int 2015; 2015: 961782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yumul R, Elvir-Lazo OL, White PF, et al. Comparison of three video laryngoscopy devices to direct laryngoscopy for intubating obese patients: a randomized controlled trial. J Clin Anesth 2016; 31: 71–77. [DOI] [PubMed] [Google Scholar]
- 13.Kim JE, Kwak HJ, Jung WS, et al. A comparison between McGrath MAC videolaryngoscopy and Macintosh laryngoscopy in children. Acta Anaesthesiol Scand 2018; 62: 312–318. [DOI] [PubMed] [Google Scholar]
- 14.Kim KN, Jeong MA, Oh YN, et al. Efficacy of Pentax airway scope versus Macintosh laryngoscope when used by novice personnel: a prospective randomized controlled study. J Int Med Res 2018; 46: 258–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ellis DG, Jakymec A, Kaplan RM, et al. Guided orotracheal intubation in the operating room using a lighted stylet: a comparison with direct laryngoscopic technique. Anesthesiology 1986; 64: 823–826. [DOI] [PubMed] [Google Scholar]
- 16.Hung OR, Pytka S, Morris I, et al. Clinical trial of a new lightwand device (Trachlight) to intubate the trachea. Anesthesiology 1995; 83: 509–514. [DOI] [PubMed] [Google Scholar]
- 17.Holden JD. Hawthorne effects and research into professional practice. J Eval Clin Pract 2001; 7: 65–70. [DOI] [PubMed] [Google Scholar]