Abstract
Background.
Despite extensive research, symptom structure of posttraumatic stress disorder (PTSD) is highly debated. The network approach to psychopathology offers a novel method for understanding and conceptualizing PTSD. However, extant studies have mainly used small samples and self-report measures among sub-clinical populations, while also overlooking comorbid depressive symptoms.
Methods.
PTSD symptom network topology was estimated in a sample of 1489 treatment-seeking veteran patients based on a clinician-rated PTSD measure. Next, clinician-rated depressive symptoms were incorporated into the network to assess their influence on PTSD network structure. The PTSD-symptom network was then contrasted with the network of 306 trauma-exposed (TE) treatment-seeking patients not meeting full criteria for PTSD to assess corresponding network differences. Finally, a directed acyclic graph (DAG) was computed to estimate potential directionality among symptoms, including depressive symptoms and daily functioning.
Results.
The PTSD symptom network evidenced robust reliability. Flashbacks and getting emotionally upset by trauma reminders emerged as the most central nodes in the PTSD network, regardless of the inclusion of depressive symptoms. Distinct clustering emerged for PTSD and depressive symptoms within the comorbidity network. DAG analysis suggested a key triggering role for re-experiencing symptoms. Network topology in the PTSD sample was significantly distinct from that of the TE sample.
Conclusions.
Flashbacks and psychological reactions to trauma reminders, along with their strong connections to other re-experiencing symptoms, have a pivotal role in the clinical presentation of combat-related PTSD among veterans. Depressive and posttraumatic symptoms constitute two separate diagnostic entities, but with meaningful between-disorder connections, suggesting two mutually-influential systems.
Keywords: combat-related trauma, depressive symptoms, network analysis, Post-traumatic stress disorder, veterans
Posttraumatic stress disorder (PTSD) is a debilitating psychiatric disorder characterized by a prolonged and maladaptive response to traumatic events (American Psychiatric Association, 2013). It has a significant toll on both society and the individual and is associated with significant psychological dysfunction and health impairments (Stein et al., 1997; Kessler, 2000; Deykin et al., 2001; Westphal et al., 2011). While lifetime prevalence is estimated at 6% (Goldstein et al., 2016), for military veterans, a highly trauma-exposed population, prevalence rates are even higher, reaching 23% (Fulton et al., 2015), with increased severity and comorbidity rates (Tsai et al., 2015).
Despite extensive research, PTSD symptom structure is still highly debated (Hoge et al., 2016; McNally, 2016, 2017; Armour et al., 2017; McNally et al., 2017a), as reflected in the ongoing discussion surrounding its diagnosis following the publication of the Diagnostic and Statistical Manual of Mental Disorders-5 (DSM-5; Galatzer-Levy and Bryant, 2013; Hoge et al., 2014; Hoge et al., 2016), which presented marked differences in the diagnostic criteria of PTSD, (Hoge et al., 2014; Hoge et al., 2016) including, among others, a more restrictive definition of criterion A and marked changes in the number and nature of individual symptoms and symptom-clusters required for diagnosis (Armour et al., 2017). Importantly, this has led to lower PTSD prevalence rates compared with DSM-IV (Kilpatrick et al., 2013). Noticeable diagnostic differences also exist between DSM-5 and the International Classification of Diseases-11 (ICD-11; World Health Organization, 2018), which includes only six mandatory symptoms assumed to reflect core PTSD symptoms not shared by other disorders (Cloitre et al., 2013; Maercker et al., 2013; Mitchell et al., 2017). This difference has resulted, once more, in striking differences in PTSD rates (Hoge et al., 2014; Stein et al., 2014; Hansen et al., 2015; Friedman et al., 2016; Guina, 2016; Hoge et al., 2016; Wisco et al., 2016b; Mitchell et al., 2017), found to be 10%-to-30% lower according to ICD-11, compared to DSM-5, among trauma-exposed individuals (Hansen et al., 2015; Wisco et al., 2016b). While different treatments for PTSD are available, including psychotherapy and pharmacotherapy (Bradley et al., 2005; Sullivan and Neria, 2009; Steckler and Risbrough, 2012), research consistently shows that more than one-third of PTSD patients never fully remit, even if treated (Difede et al., 2014). As importantly noted in the guidelines of the National Institute for Health and Care Excellence (NICE) PTSD, treatment efficacy can only be achieved if the disorder is first accurately recognized (National Institue for Clinical Excellence, 2005; Spoont et al., 2015).
Recently, a novel network perspective on psychopathology has emerged, offering an alternative approach for understanding and conceptualizing symptomatology, which may be of use also in discerning the central and fundamental features of PTSD (McNally, 2016, 2017; Fried et al., 2017; Mitchell et al., 2017; Fried et al., 2018). According to the network perspective, psychopathology is not the result of underlying latent variables, but rather is the constitution of symptoms associated in dynamic and causal relations, interacting and possibly self-reinforcing each other (Borsboom et al., 2003; Cramer et al., 2010b; Borsboom and Cramer, 2013; Schmittmann et al., 2013; Boschloo et al., 2015; McNally et al., 2015; McNally, 2016, 2017; Fried et al., 2017). To use an example put forward by Birkeland and Heir (2017), in the aftermath of traumatic event, intrusive memories of the event might occur, leading to hyperarousal and sleep difficulties, which in turn lead to concentration deficiencies, which can be then looped back to the intrusive memories, creating feedback loops of symptoms that maintain each other. In the corresponding network structure, symptoms are represented by nodes, and the associations or connections between pairs of symptoms/nodes are represented by edges, establishing a specific disorder (Jones et al., 2017). The importance of each node within a specific network is quantified by measures of node centrality. As nodes are activated, their activation is transmitted to connected nodes, via the connecting edges, and an episode of a disorders unfolds (McNally et al., 2015). Thus, network findings can guide clinicians and researchers in measuring disorders and their symptoms, and eventually, in refining the nosology and classification of different psychopathologies. In PTSD, network analysis has been explicitly suggested as a vital tool for selection of diagnostic criteria, and for assessing its occurrence and severity (Phillips et al., 2018).
Extensive research implementing network models in PTSD among trauma-exposed adult populations, including several in veterans, has been conducted over the last several years, aiming to elucidate the symptom structure of PTSD (McNally et al., 2015; Knefel et al., 2016; Armour et al., 2017; Birkeland and Heir, 2017; Bryant et al., 2017; Haag et al., 2017; Mitchell et al., 2017; Spiller et al., 2017; Afzali et al., 2017a, 2017b; McNally et al., 2017a; Benfer et al., 2018; Epskamp et al., 2018; Fried et al., 2018; Greene et al., 2018; Moshier et al., 2018; Papini et al., 2018; Phillips et al., 2018; Ross et al., 2018; Sullivan et al., 2018; Vanzhula et al., 2018; von Stockert et al., 2018; Price et al., 2019). While some similarities in findings across studies exist, important disparities emerge (Birkeland and Heir, 2017, Phillips et al., 2018). For example, while amnesia is found to be the least central symptom in most PTSD network studies (McNally et al., 2015, Armour et al., 2017, Birkeland and Heir, 2017, Bryant et al., 2017, Mitchell et al., 2017, Spiller et al., 2017, Afzali et al., 2017a, McNally et al., 2017a, Benfer et al., 2018, Fried et al., 2018, Moshier et al., 2018, Papini et al., 2018, Phillips et al., 2018, Ross et al., 2018, Vanzhula et al., 2018, von Stockert et al., 2018), symptoms emerging as most central vary considerably across studies, including, among others, getting emotionally upset due to trauma reminders, hypervigilance, intrusive thoughts, concentration difficulties, nightmares, future foreshortening, negative trauma related emotions, detachment, loss of interest, emotional numbing, physical reactions to trauma reminders, and flashbacks (Phillips et al., 2018). Recently, it has been suggested that these mixed findings might be the result of corresponding differences in traumatic events, such as, for example, man-made trauma v. natural disasters, as this has been shown to affect PTSD presentation, and hence, network structure (Ross et al., 2018; Sullivan et al., 2018). Interestingly, when limiting past research to include only veteran samples, a more consistent result pattern emerges, demonstrating high centrality of getting emotionally upset by trauma reminders (Armour et al., 2017; Mitchell et al., 2017; Fried et al., 2018; Moshier et al., 2018; von Stockert et al., 2018). Other reasons implicated as responsible for observed inconsistencies across studies are differences in sample size, sample type (treatment-seeking, survey data), participants’ clinical status (PTSD, probable PTSD, subthreshold PTSD, trauma-exposed healthy participants), and the PTSD measure used for network construction (self-report, clinician-administered).
While extant network research in PTSD has advanced our knowledge in the field, important gaps still remain, which we aim to address in the present study. First, no study to date has used a sample comprised exclusively of treatment-seeking veterans with PTSD, while also basing analyses on clinician-rated measures only. Importantly, in clinical assessments, self-report measures do not allow for additional inquiries of ambiguous or vague answers (Trull et al., 2001), pose a risk for response biases, and are subjected to wording-effects (Moskowitz, 1986; Schwarz, 1999). In PTSD, self-reports can only result in a diagnosis of ‘probable’ PTSD (Wisco et al., 2016a), imperfectly capturing the examined pathology (McNally, 2016). Finally, while a recent study comparing PTSD network structures based on clinician-rated and patient-rated data reported similar network structures, results also showed that their global structure was not statistically identical and that networks also differed on node-clustering (Moshier et al., 2018). Indeed, most PTSD network studies have mentioned both using self-reports and non-clinical samples as limitations necessitating additional research (McNally et al., 2015; Knefel et al., 2016; Armour et al., 2017; Birkeland and Heir, 2017; Mitchell et al., 2017; Spiller et al., 2017; Afzali et al., 2017a, 2017b; Greene et al., 2018; Ross et al., 2018; Sullivan et al., 2018; Vanzhula et al., 2018; von Stockert et al., 2018).
Second, while sample size is crucial for establishing a reliable network structure, with robust estimation of edges and centrality metrics powered to detect even small coefficients (Epskamp et al., 2018; Epskamp and Fried, 2018; Fried et al., 2018), most studies used small sample sizes (McNally et al., 2015; Knefel et al., 2016; Armour et al., 2017; Birkeland and Heir, 2017; Haag et al., 2017; Spiller et al., 2017; Afzali et al., 2017a; McNally et al., 2017a; Epskamp et al., 2018; Greene et al., 2018; Ross et al., 2018; Vanzhula et al., 2018). For adequate power, sample size should be considerably larger than the number of parameters estimated in analyses, which given the number of variables in PTSD-related networks, tends to be relatively high (Spiller et al., 2017; Afzali et al., 2017a, 2017b; McNally et al., 2017a, Fried et al., 2018)1,†. To date, six studies used large samples of about 1000 participants (Bryant et al., 2017; Fried et al., 2018; Phillips et al., 2018; Sullivan et al., 2018; von Stockert et al., 2018; Price et al., 2019). Still, four assessed trauma-exposed participants with low-to-none rates of probable PTSD (Bryant et al., 2017; Sullivan et al., 2018; von Stockert et al., 2018; Price et al., 2019), the fifth pooled data from four datasets differing on country of origin, symptoms assessed, and assessment language and tools (Fried et al., 2018), and, as stated previously, all six studies assessed PTSD symptoms based on self-report measures only.
Finally, PTSD and depression symptoms frequently co-occur (Neria and Bromet, 2000; Lapierre et al., 2007; Au et al., 2013), with approximately 50% comorbidity rates between PTSD and major depressive disorder (MDD; Kessler et al., 1995; Elhai et al., 2008; Rytwinski et al., 2014; Flory and Yehuda, 2015). Compared to PTSD alone, patients with PTSD-MDD exhibit greater distress, higher suicide risk, and poorer treatment outcome (Blanchard et al., 1998; Oquendo et al., 2003; Green et al., 2006; Ramsawh et al., 2014; Flory and Yehuda, 2015), with co-morbid patients shown to be more likely to drop out from treatment, to be non-responders to prolonged exposure treatment, and to necessitate longer psychotherapy (Gillespie et al., 2002; Bryant et al., 2003; McDonagh et al., 2005; Stein et al., 2012). Thus, understanding the underlying structure of the PTSD-MDD comorbidity can enhance extant efforts to better assess and treat PTSD-MDD patients (Flory and Yehuda, 2015; Afzali et al., 2017b). Past research aiming to explore the PTSD-MDD comorbidity has mainly focused on shared features or similarities between disorders. For example, some have suggested that both disorders are high on a psychopathology-related diagnostic dimension of general distress, leading to increased comorbidity rates (i.e. the quadripartite model of psychopathology; Watson, 2009), while others have focused on more specific content-overlap between disorders (Elhai et al., 2008; Elhai et al., 2011). Research efforts undertaken to support these ideas have employed, among others, exploratory (Blanchard et al., 1998; Grant et al., 2008; Gros et al., 2010; Contractor et al., 2015; Price and van Stolk-Cooke, 2015) and confirmatory factor analytic approaches (Simms et al., 2002; Armour and Shevlin, 2010; Miller et al., 2010). However, an important limitation shared by all of these analyses is that they all assume symptoms to be independent constructs, related only via their corresponding factor, thereby missing important facets of the interplay between specific symptoms of different disorders (Afzali et al., 2017b; Price et al., 2019). Conversely, as described above, the network approach views symptoms as being in dynamic and causal associations, interacting and possibly self-reinforcing each other, hence tapping this important aspect. In line with this view, the network approach conceptualizes comorbidity as the overall constellation of symptom-level associations, including those that exist between symptoms of different disorders (Cramer et al., 2010a; Borsboom et al., 2011; Afzali et al., 2017b; Price et al., 2019). These between-disorder symptom associations are termed bridge nodes, and their importance is measured using centrality measures in a similar fashion to that used for within-disorder nodes. Thus, network analysis can be readily used to examine the role of more specific causes for high PTSD-MDD comorbidity rates such as between-disorder overlapping symptoms as sleep and concentration difficulties, which are part of both depression and PTSD (Spitzer et al., 2007; Cramer et al., 2010a; Afzali et al., 2017b). Importantly, the topic of overlapping symptoms gained renewed attention following the addition of Cluster D (i.e. Negative alterations in cognitions and mood associated with the traumatic event) to PTSD diagnosis per DSM-5 (American Psychiatric Association, 2013), which increased the number of potential overlapping symptoms between PTSD and depression (Mitchell et al., 2017; Price et al., 2019; but see O’Donnell et al. (2014) showing similar PTSD-MDD comorbidity rates based on DSM-IV and DSM-5). Still, while providing a novel approach to conceptualize and understand the PTSD-MDD comorbidity, to date, only four studies included depressive symptoms in their network analysis of PTSD. Yet, one measured lifetime occurrence, not current major depressive disorder (MDD) symptoms (Afzali et al., 2017b), and three used self-reported measures of PTSD and depression (Armour et al., 2017; Mitchell et al., 2017; Price et al., 2019).
In line with the above-mentioned gaps in knowledge, here we examined PTSD symptom structure in a sample of clinically-diagnosed, treatment-seeking Israel Defense Forces combat-exposed veterans. Our goal was to extend current knowledge in the following ways: (1) analyze PTSD symptom networks using data from structured clinician-administered interviews; (2) use a large sample (N = 1489); (3) re-estimate network structure when including clinician-rated depressive symptoms; (4) compare the PTSD network to that of trauma-exposed (TE) treatment-seeking combat veterans not meeting PTSD diagnostic criteria; and (5) explore potential directionality among symptoms including depressive symptoms and a daily functioning measure, as the DSM classification system specifically requires significant impairment in one or more areas of functioning for a PTSD diagnosis. Several hypotheses were made. First, due to lack of consensus in the literature on central symptoms, we hypothesized that re-experiencing symptoms would emerge as highly central based on findings of most network studies focusing on trauma-exposed veterans (Armour et al., 2017; Mitchell et al., 2017; Fried et al., 2018; Moshier et al., 2018; von Stockert et al., 2018). In line with numerous network studies across different traumatic populations, we also predicted low centrality for amnesia. Second, based on previous studies incorporating depressive symptoms in the network structure of military veterans (Armour et al., 2017; Mitchell et al., 2017), we hypothesized that while the introduction of depressive symptoms would result in several significant bridge nodes, this would have little effect on the PTSD symptom structure. Third, we hypothesized greater overall connectivity in the clinical PTSD group, compared with the trauma-exposed (TE) treatment-seeking patients not meeting full criteria for PTSD, which in accordance with the conceptualization of psychopathology per the network approach and with the only study to date that examined this possibility in veterans with PTSD compared with subthreshold PTSD (Phillips et al., 2018). Still, we would like to emphasize at this juncture that the current study is the first to employ a network analysis approach using a large sample comprised exclusively of treatment-seeking veterans with PTSD, while also basing analyses on clinician-rated measures only. Thus, present analyses should be regarded as partly exploratory in nature. Put differently, as previous research has implicated numerous factors (e.g. sample size, sample type, participants’ clinical status, trauma type, and the PTSD measure used for network construction) in results heterogeneity across studies, current hypotheses are in part extrapolations based on extant findings in the field.
Methods
Participants
Participants were 1795 male veterans seeking treatment from the Israel Defense Forces Unit for Treatment of Combat-Related PTSD (UTC-PTSD), an outpatient clinic specializing in assessing and treating combat-related PTSD. Upon contacting the clinic, veterans were first phone-screened to ascertain past exposure to a combat-related event. Veterans fulfilling this requirement were then invited for a formal clinical assessment by one of the clinic’s assessors, namely, psychiatrists, clinical psychologists, or social workers with 12 or more years of experience in PTSD diagnosis in veterans. Importantly, as assessors also completed the mandatory Israel Defense Forces service, they were familiar with the language, manners, behavioral norms, belief system, and rituals of Israeli military culture (Levi et al., 2016; Levi et al., 2017). Next, semi-structured diagnostic interviews based on DSM-IV-TR were administered as part of the routine admission process to the clinic. Interviews followed the UTC-PTSD assessment manual, developed within the UTC-PTSD, which comprises an anamnestic section to collect socio-demographic and personal background, as well as general medical information, and a diagnostic section using both clinician-rated measures (i.e. the clinician-administered PTSD Scale (CAPS-IV; Blake et al., 1995) and the Montgomery–Asberg Depression Rating Scale (MADRS; Montgomery and Asberg, 1979)) and self-report questionnaires (for full measures description see Measures below). Next, each patient’s assessment record was presented in the clinic’s staff meeting, and final decisions relating to diagnoses (and ensuing treatment course) were made (Levi et al., 2016). Veterans with active or past psychosis or current severe substance use disorder were not accepted for treatment at the clinic and were referred out to specialized clinics. Veterans with high levels of active suicidality, as indicated by concrete suicidal plans, were taken to a psychiatric emergency room for immediate intervention. Finally, veterans receiving psychotherapy or pharmacotherapy elsewhere were also excluded from the clinic’s care. The present study analyzed the assessment-data collected from 1795 male veterans that were admitted to the clinic’s care between 2006-to-2014. Of note, about 15% of patients were still part of the military, but only as reserve forces, during their assessment.
In total, of the 1795 treatment-seeking male veterans, 1489 met diagnostic criteria for PTSD while 306 did not (See Table 1 for demographic characteristics of the two groups), with all being exposed to combat-related traumatic events (i.e. DSM-IV criterion A). Specifically, these events included: (1) participating in direct combat, including incoming mortar and rocket attacks, while participating in one of Israel’s major wars (e.g. ‘Second Lebanon War’); (2) receiving incoming small fire-arms and/or experiencing detonations of improvised explosive devices (IEDs) while participating in one of Israel’s combat operations (e.g. ‘Operation Cast Led’); (3) routine security measures including clearing and searching operations while undergoing extensive Molotov cocktail and/or stone throwing attacks; and (4) personally knowing someone seriously injured or killed in one of the aforementioned wars or combat operations2. A clinical diagnosis of PTSD was established using CAPS-IV (Blake et al., 1995), based on the relatively lenient F1/I2 item rule (i.e. Frequency ⩾ 1, Intensity > 2; Blake et al., 1995). Accordingly, PTSD diagnosis necessitated endorsing at least one re-experiencing symptom, three avoidance symptoms, and two hyperarousal symptoms. For the purpose of the present study, those not meeting this requirement were regarded as trauma-exposed (TE) treatment-seeking patients not meeting full criteria for PTSD. Of note, of the 306 TE patients, exactly half (n = 153) met criteria for subthreshold PTSD, defined as fulfilling symptom-requirement of two out of the three symptom-clusters (Keane and Barlow, 2002; Phillips et al., 2018). The study was approved by the Israel Defense Forces Medical Corps Ethics Committee.
Table 1.
Demographic characteristics by group
| PTSD group |
TE group |
Statistics |
||||
|---|---|---|---|---|---|---|
| M | s.d. | M | s.d. | Statistic | p Value | |
| Age at assessment (years) | 36.13 | 13.95 | 34.99 | 12.78 | t = 1.318 | 0.19 |
| Age at event (years) | 23.97 | 5.58 | 24.79 | 5.93 | t = 2.265 | 0.02 |
| Education (years) | 12.49 | 1.90 | 12.76 | 2.30 | t = 2.173 | 0.03 |
| Family status (%) | χ2 = 0.61 | 0.89 | ||||
| Single | 47.75 | – | 47.38 | – | ||
| Married | 42.71 | – | 44.44 | – | ||
| Divorced | 9.27 | – | 7.85 | – | ||
| Widowed | 0.27 | – | 0.33 | – | ||
| Number of children (N) | 3.70 | 63.44 | 1.38 | 1.62 | t = 0.567 | 0.57 |
| Employed (%) | 59.10 | – | 69.28 | – | χ2 = 10.58 | <0.01 |
| Military occupation (%) | χ2 = 4.03 | 0.04 | ||||
| Combat soldiers | 85.02 | – | 89.44 | – | ||
| Specialist military personnel | 14.98 | – | 10.56 | – | ||
| Officers (%) | 7.46 | – | 11.51 | – | χ2 = 5.52 | 0.02 |
| Injured (%) | 12.89 | – | 9.80 | – | χ2 = 2.24 | 0.13 |
| Past Psychotherapy (%) | 56.22 | – | 28.95 | – | χ2 = 22.87 | <0.01 |
| Past pharmacotherapy (%) | 28.71 | – | 20.72 | – | χ2 = 8.08 | <0.01 |
PTSD, posttraumatic stress disorder; TE, trauma-exposed.
Measures
Clinician-rated PTSD symptoms
Severity of PTSD symptoms was measured using CAPS-IV (Blake et al., 1995), a 17-item structured interview used for diagnosing PTSD based on DSM-IV criteria, considered the gold standard in PTSD assessment. Each item/symptom is rated separately on frequency and intensity on a 0-to-4 scale, for an item total score of 0-to-8. Summed item scores yield an estimate of three symptom clusters (i.e. Cluster B, Re-experiencing; Cluster C, Avoidance, and Numbing; and Cluster D, Hyperarousal) and an overall PTSD severity score. The CAPS has excellent reliability, convergent and discriminant validity, diagnostic utility and sensitivity to clinical change in military veterans and other populations (Weathers et al., 2001; Pupo et al., 2011). Cronbach’s α in the current sample was 0.91.
Clinician-rated depressive symptoms
Clinician-evaluated levels of depressive symptoms were measured using the Montgomery–Asberg Depression Rating Scale (MADRS; Montgomery and Asberg, 1979), a 10-item questionnaire assessing core depressive symptoms during the past week, each rated on a 0-to-6 scale (no evidence to pervasive evidence). It has high inter-rater reliability, convergent validity, and similar rates of sensitivity to change compared to other measures of depression (Montgomery and Asberg, 1979; Khan et al., 2002; Khan et al., 2004). Cronbach’s α in the current sample was 0.90.
Functioning
Functioning in different life domains were assessed using the Psychotherapy Outcome Assessment and Monitoring System-Trauma Version (POAMS-TV) Assessment Questionnaire (Green et al., 2003). This self-report includes 10 items, each rated on a 0-to-5 scale (extreme distress/dissatisfaction to optimal functioning/satisfaction). A global functioning score is derived by averaging scores across items (Levi et al., 2016; Levi et al., 2017). The POAMS-TV has been shown to be reliable in other samples of Israel Defense Forces veterans (Svetlicky et al., 2010). Cronbach’s α in the current sample was 0.81.
Data analysis
Network analysis
Network models estimating the associations between symptoms are usually constructed using the Graphical Gaussian Model (GGM; Epskamp and Fried, 2016), through the R-package qgraph (Epskamp et al., 2012). Within the graphical network, each node depicts a symptom, and edges depict regularized partial correlations between two symptom nodes. Line thickness reflects association strength; blue and red edges represent positive and negative associations, respectively.
Here, as we had two different samples of participants (i.e. PTSD patients and TE participants) for which we constructed the same network structure based on the CAPS 17-symptomitems, we used the fused graphical lasso (FGL; Danaher et al., 2014). The FGL is a network estimation technique, which is an extension of the graphical lasso, that allows estimating several GGMs jointly, yielding a more accurate estimation of network structures than estimating each network individually using separate GGMs (Danaher et al., 2014; Costantini and Epskamp, 2017; Fried et al., 2018). Thus, we used FGL to plot the network structure for the PTSD and TE samples using the CAPS 17-symptom-items (CAPS-items and TE-CAPS-items networks, respectively). For the PTSD sample, we used GGM to plot the network structure incorporating both the CAPS 17-symptom-items and the MADRS depressive symptom-items (CAPS + MADRS-items network), as this network was conducted only for the PTSD sample.
Node centrality measures
Within-network symptoms importance was characterized using the one-step expected influence (EI) centrality measure indexing node strength (Robinaugh et al., 2016), as it takes into account negative as well as positive edges (Wang et al., 2018). It is considered the most reliable, stable and accurate measure of node centrality compared with other centrality measures, such as betweenness and closeness (Fried et al., 2018; Wang et al., 2018), which were recently deemed less suitable as measures of node importance in psychological networks (Bringmann et al., 2018; Hallquist et al., 2019).
EI analyses used the R-package bootnet (Epskamp et al., 2018) and included the one-step expected influence measure (Robinaugh et al., 2016), which reflects the summed weight of positive and negative edges with the neighboring nodes in the network (Heeren et al., 2018). Expected influence was computed for all networks. For the CAPS + MADRS-items network, EI was also computed for bridge nodes (nodes which have symptom-level connections with nodes of the other disorder), reflecting between-disorder symptom associations (Jones et al., 2019). For all measures, higher values of EI reflect greater node centrality (McNally, 2016; Bringmann et al., 2018; Fried et al., 2018; Hallquist et al., 2019).
Network robustness (accuracy and stability)
Network accuracy was computed using the R-package bootnet (Epskamp et al., 2018) employing a non-parametric bootstrap approach. We estimated edge weights accuracy at a 95% confidence intervals (CIs) by sampling the data 1000 times (with replacement), thereby generating a distribution of edge weights. Network stability was assessed using a bootstrap person-dropping procedure (Costenbader and Valente, 2003) providing a correlation stability (CS)-coefficient. While CS-coefficient ⩾0.25, and preferably ⩾0.50, reflects adequate network stability, those under 0.25 reflect insufficient network stability (Epskamp et al., 2018).
Network comparison
For network comparison analysis we first randomly sampled 306 PTSD patients from the original PTSD sample to ensure an even number of participants in the PTSD and TE samples. Next, a Network Comparison Test (NCT R-package; van Borkulo and Millner, 2016) was used to compare the CAPS-items and TE-CAPS-items networks. We used an omnibus test evaluating invariance of the network structure across groups, and also tested the differences in global strength between the networks, comparing the sum of absolute edge weight values.
Directed acyclic graph (DAG) analysis
The DAG is a Bayesian network approach that models a network in which edges are directed and noncircular. Thus, the DAG gives us information about both the strength and the direction of connections between symptoms, which are regarded as clues as to which associations between symptoms might be causally important, that is, which symptoms may play a causal role in creating other symptoms (Jones et al., 2018). Here, a Bayesian network analysis applying the R-package bnlearn (Scutari, 2010) was used to produce DAGs aiming to discern directionality among nodes from cross-sectional data (McNally, 2016). For the present study, we used the completed partially DAG (CPDAG) which accounts for some of the shortcomings of equivalent separate DAGs (Scutari and Denis, 2014). DAG analysis considered CAPS and MADRS single-items as well as the daily functioning total score.
See Supplemental Material for a more comprehensive description of data analyses including the original analytic code (R-scripts) and the underlying co-variance matrices of the different presented networks.
Results
Psychopathology measures
Mean scores of the PTSD sample were 81.77 (S.D. = 17.21) for the CAPS, 29.23 (S.D. = 10.825) for the MADRS, and 2.07 (S.D. = 0.74) for the POAMS-TV. In the trauma-exposed (TE) treatment-seeking patients not meeting full criteria for PTSD sample, mean scores were 33.95 (S.D. = 18.26), 25.31 (S.D. = 9.68), and 2.67 (S.D. = 0.76), respectively. Independent-samples t tests revealed significant group differences on all measures, all ps<0.0001. Of the PTSD group, 57% also met diagnostic criteria for MDD (i.e. a PTSD-MDD comorbidity), while only 32% of the TE sample met MDD criteria.
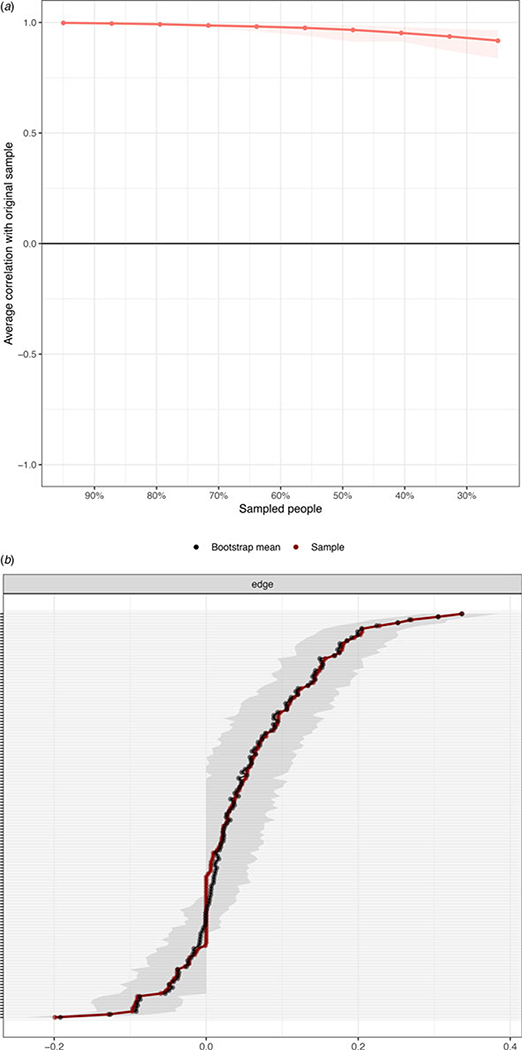
CAPS-items network
The CAPS-items network of the PTSD sample is depicted in Fig. 1a (for the TE-CAPS-items network see Fig. 1b and section below). The stability of the estimated network (CS-coefficient) was 0.75 for expected influence (Fig. 2a), reflecting a highly stable network. For edge-weight accuracy, see Fig. 2b.
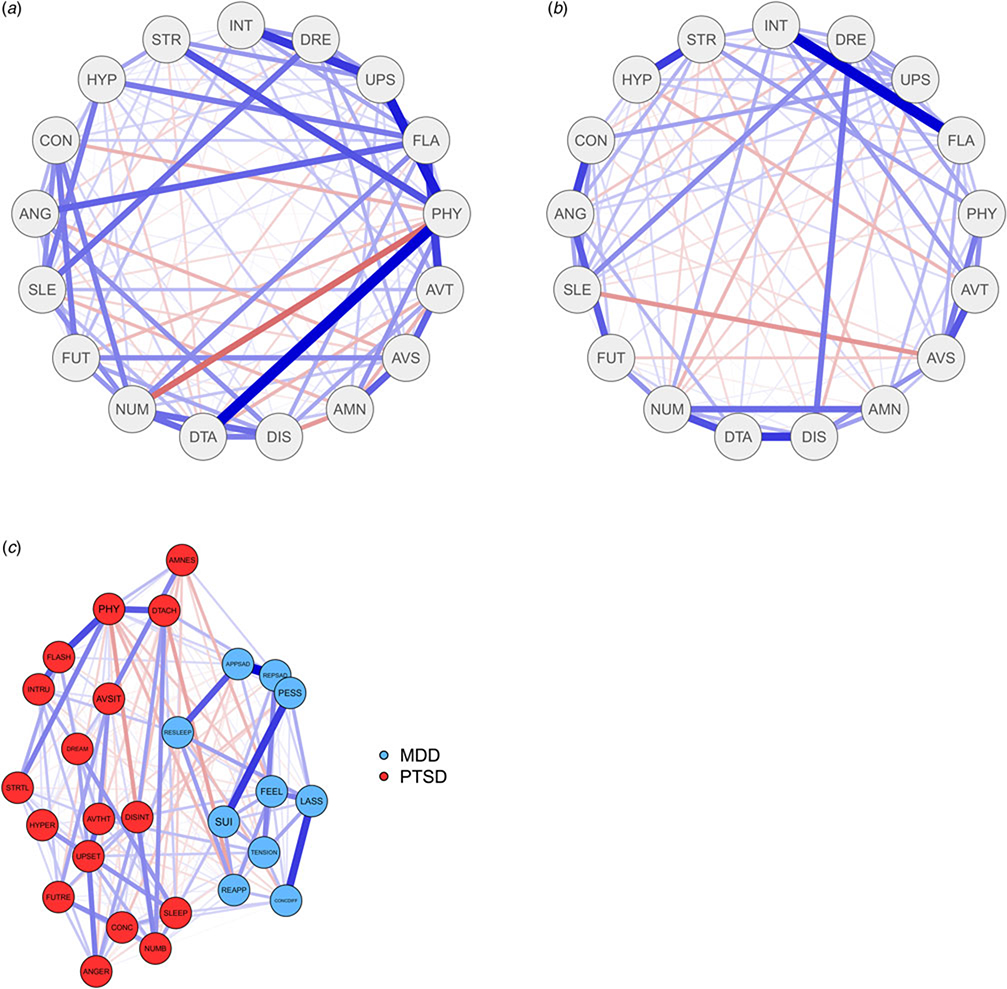
Fig. 1.
Symptom-items Networks. (a) The clinician-administered PTSD Scale (CAPS-IV) 17-symptom-items network among PTSD patients (CAPS-items network). Positive edges appear in blue and negative appear in red. The stronger and saturated edges represent stronger regularized partial correlations. The item label abbreviations for the CAPS are: AMN, amnesia; ANG, irritability; AVS, avoidance of situations; AVT, avoidance of thoughts; CON, concentration deficits; DIS, disinterest in activities; DRE, nightmares; DTA, detachment from others; FLA, flashbacks; FUT, foreshortened future; HYP, hypervigilance; INT, intrusions; NUM, emotional numbing; PHY, physiological reactivity; SLE, sleep disturbance; STR, startle response; and UPS, upset by reminders. (b) The clinician-administered PTSD Scale (CAPS-IV) 17-symptom-items network among treatment-seeking patients who did not meet full criteria for PTSD (TE-CAPS-items network). Positive edges appear in blue and negative appear in red. The stronger and saturated edges represent stronger regularized partial correlations. The item label abbreviations for the CAPS are the same. (c) The network of the clinician-administered PTSD Scale (CAPS-IV) 17-symptom-items combined with the 10-symptom-items of the clinician-rated Montgomery–Asberg Depression Rating Scale (MADRS) among PTSD patients. The items from the CAPS-IV are colored red and the items from the MADRS are colored blue (CAPS + MADRS-items network). Positive edges appear in blue and negative appear in red. The stronger and saturated edges represent stronger regularized partial correlations. The item label abbreviations for the CAPS (red circles) are: AMNES, amnesia; ANGER, irritability; AVSIT, avoidance of situations; AVTHT, avoidance of thoughts; CONC, concentration deficits; DISINT, disinterest in activities; DREAM, nightmares; DTACH, detachment from others; FLASH, flashbacks; FUTRE, foreshortened future; HYPER, hypervigilance; INTRU, intrusions; NUMB, emotional numbing; PHY, physiological reactivity; SLEEP, sleep disturbance; STRTL, startle response; and UPSET, upset by reminders. The item abbreviation labels for the MADRS (blue circles) are: APPSAD, apparent sadness; REPSAD, reported sadness; TENSION, Inner Tension; RESLEEP, reduced sleep; REAPP, reduced appetite; CONCDIFF, concentration difficulties, LASS, lassitude; FEEL, inability to feel; PESS, pessimistic thoughts; SUI, suicidal thoughts.
Fig. 2.
Network Robustness Measures (Accuracy and Stability). (a) Bootstrapped node expected influence of the clinician-administered PTSD Scale (CAPS-IV) 17-symptom-items network among PTSD patients. (b) Bootstrapped confidence intervals of all edge weights of the clinician-administered PTSD Scale (CAPS-IV) 17-symptom-items network among PTSD patients. The red line represents sample values, the black line represents bootstrap means, and the gray area is the bootstrapped CIs. Each horizontal line represents one edge of the network, ordered from the edge with the highest edge-weight to the edge with the lowest edge-weight.
The strongest edges were physiological reactivity by trauma reminders (B5)-to-feelings of detachment from others (C5); physiological reactivity by trauma reminders (B5)-to-getting emotionally upset by trauma reminders (B4); getting emotionally upset by trauma reminders (B4)-to-intrusive thoughts (B1); and flashbacks (B3)-to-avoidance of thoughts (C1).
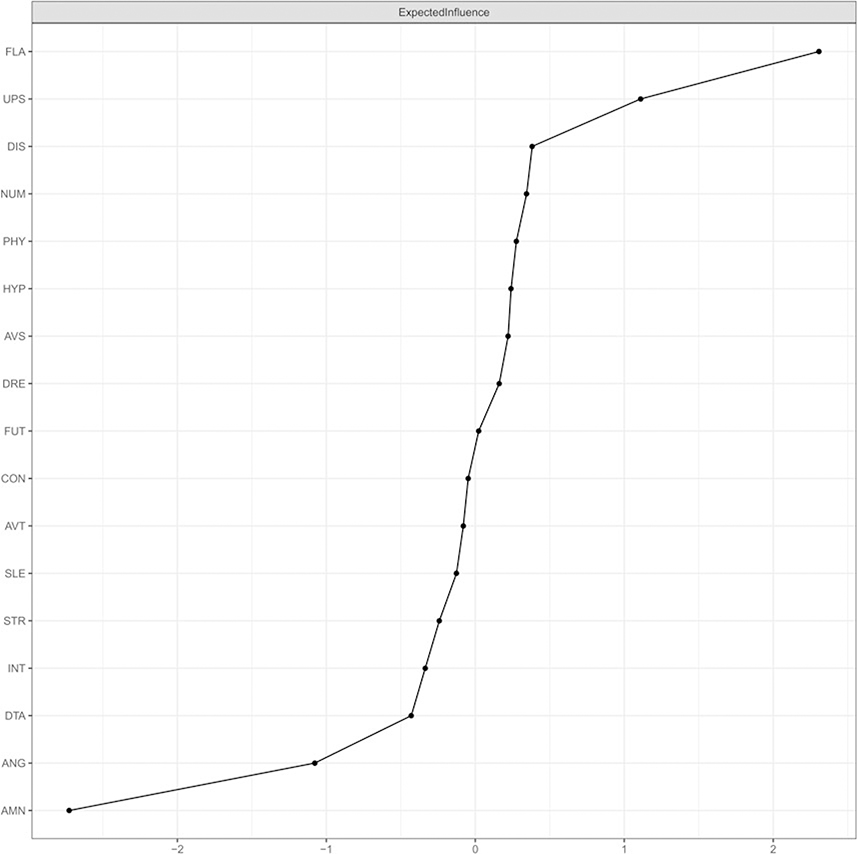
The standardized estimate of the expected influence centrality measure is depicted in Fig. 3. Flashbacks (B3) and getting emotionally upset by trauma reminders (B4) emerged as the most influential symptoms, with amnesia (C3) and irritability (D2) emerging as the least influential.
Fig. 3.
Network Centrality – Expected Influence. The expected influence measure for the clinician-administered PTSD Scale (CAPS-IV) 17-symptom-items network among PTSD patients.
See online Supplementary Figs S1 and S2 for significant tests between edge weights and nodes, respectively.
CAPS + MADRS-items network
CAPS and MADRS items formed two separate clusters within the co-morbidity network (Fig. 1c). Network stability remained high for expected influence (0.75; online Supplementary Fig. S3A) reflecting a highly stable network. For edge-weight accuracy, see online Supplementary Fig. S3B.
Within the PTSD cluster, same edges as in the CAPS-item network emerged as strongest. Within the depressive symptoms cluster, strongest edges were suicidality (Q10)-to-pessimistic thoughts (Q9); reported sadness (Q2)-to-apparent sadness (Q1); and lassitude (Q7)-to-concentration difficulties (Q6).
The standardized estimate of expected influence for the CAPS + MADRS-items network is depicted in online Supplementary Fig. S4. Getting emotionally upset by trauma reminders (B4) and flashbacks (B3) emerged once more as the two most influential PTSD symptoms in the network. Depressive symptoms of reported sadness (Q2), lassitude (Q7), and inner tension (Q3) also demonstrated high expected influence. As in the CAPS-item network, amnesia (C3) and irritability (D2) were found to be the lowest on EI. Reduced appetite (Q5) and detachment from others (C5) also demonstrated low EI.
See online Supplementary Figs S5 and S6 for significant tests between edge weights and nodes, respectively.
Considering only bridge-nodes (online Supplementary Fig. S7), results showed that the most influential bridge-nodes were (depression-related) reduced sleep (Q4), reported sadness (Q2), inner tension (Q3), (PTSD-related) disturbed sleep (D1), avoidance of thoughts (C1), and getting emotionally upset by trauma reminders (B4). Reduced appetite (Q5) and physiological reactions from trauma reminders (B5) were the least influential bridge-nodes.
TE-CAPS-items network (v. CAPS-items network)
The stability of the TE network showed a lower CS-coefficient of 0.52 compared with the PTSD-related networks (0.75 for both the CAPS-items and the CAPS + MADRS-items). However, this score is still above the recommended score of 0.5, reflecting a stable enough network (online Supplementary Fig. S8A). For edge-weight accuracy, online Supplementary Fig. S8B.
The strongest positive edges in the TE network were intrusive thoughts (B1)-to-flashbacks (B3); anhedonia (C4)-to-detachment from others (C5); irritability (D2)-to-concentration deficits (D3); and hypervigilance (D4)-to-startle response (D5).
The standardized estimate of the expected influence centrality measure is depicted in online Supplementary Fig. S9. Intrusive thoughts (B1), flashbacks (B3), irritability (D2), and nightmares (B2) were the strongest nodes, with the weakest being amnesia (C3), foreshortened future (C7), and disturbed sleep (D1).
See online Supplementary Figs S10 and S11 for significant tests between edge weights and nodes, respectively.
The two networks differed significantly on structure ( p = 0.0018) and global strength ( p = 0.0262). As seen in Fig. 1, the network structure of the PTSD sample (Fig. 1a) is more interconnected relative to the TE sample (Fig. 1b).
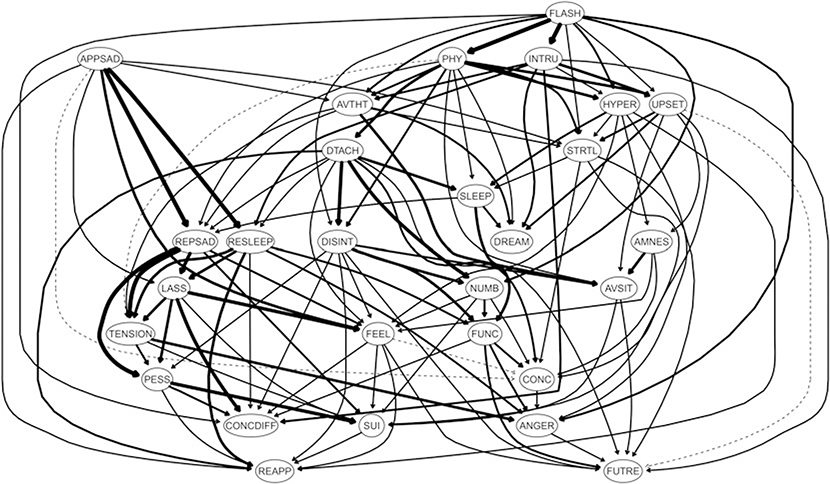
Directed acyclic graph (DAG) analysis
In the DAG analysis (Fig. 4), flashbacks (B3) emerged once more as the most pivotal network node. While not being triggered by any higher located nodes, it triggered nine other PTSD symptoms, with the strongest edges being with intrusive thoughts (B1) and physiological reactivity by trauma reminders (B5), with all three triggering getting emotionally upset by trauma reminders (B4), hypervigilance (D4), and avoiding trauma-related thoughts (C1). The most downstream PTSD symptoms (i.e. triggered nodes that trigger no other nodes) were nightmares (B2), irritability (D2) and foreshortened future (C7) with concentration difficulties (D3) being mostly triggered by other nodes.
Fig. 4.
Directed Acyclic Graph (DAG). Directed acyclic graph (DAG) of the clinician-administered PTSD Scale (CAPS-IV) 17-symptom-items (PTSD), the clinician-rated Montgomery–Asberg Depression Rating Scale (MADRS) 10-symptom-items (depression), and the psychotherapy outcome assessment and monitoring system-trauma version (POAMS-TV) total score reflecting overall functioning levels (functioning) among PTSD patients. Nodes represent symptoms and edges represent directed connections between symptoms. The item label abbreviations for the CAPS are: AMNES, amnesia; ANGER, irritability; AVSIT, avoidance of situations; AVTHT, avoidance of thoughts; CONC, concentration deficits; DISINT, disinterest in activities; DREAM, nightmares; DTACH, detachment from others; FLASH, flashbacks; FUTRE, foreshortened future; HYPER, hypervigilance; INTRU, intrusions; NUMB, emotional numbing; PHY, physiological reactivity; SLEEP, sleep disturbance; STRTL, startle response; and UPSET, upset by reminders. The item abbreviation labels for the MADRS are: APPSAD, apparent sadness; REPSAD, reported sadness; TENSION, Inner Tension; RESLEEP, reduced sleep; REAPP, reduced appetite; CONCDIFF, concentration difficulties, LASS, lassitude; FEEL, inability to feel; PESS, pessimistic thoughts; SUI, suicidal thoughts. The item abbreviation label for the POAMS-TV is FUNC.
Of note, PTSD and depressive symptoms, while showing some between-disorders edges in the DAG, were once more clustered separately from each other. Importantly, most of the existing between-disorders edges were PTSD-to-depressive symptoms edges, with almost none of the opposite direction. Daily functioning was directly influenced by several PTSD-related symptoms, including disturbed sleep (D1), anhedonia (C4), and numbness (C6), but only by one depressive symptom of reduced sleep (Q4). In turn, daily functioning showed a triggering effect on foreshortened future (C7), concentration difficulties (D3), and irritability (D2), all PTSD-related symptoms.
Discussion
This study examined PTSD network structure in treatment-seeking veterans with PTSD (n = 1489). To our knowledge, this is the largest single-sample PTSD network study, and the first to include participants meeting full diagnostic criteria for PTSD, while basing network structure exclusively on clinician-administered measures. Network structure was further assessed after introducing depressive symptoms, and again using a DAG analysis, including also depressive symptoms and a functioning measure, to better discern association directionality (McNally, 2016; McNally et al., 2017a).
Flashback and getting emotionally upset by trauma reminders emerged as the most central symptoms across all PTSD-related networks, highlighting their importance in the clinical presentation of PTSD among treatment-seeking veterans, echoing prior results in various populations (Spiller et al., 2017; Afzali et al., 2017a; Epskamp et al., 2018; Fried et al., 2018; Greene et al., 2018), including veterans (Armour et al., 2017; Mitchell et al., 2017; Fried et al., 2018; von Stockert et al., 2018), for which their clinical importance was specifically emphasized (Armour et al., 2017). Amnesia emerged as the least central symptom across all networks, reaffirming previous findings (Birkeland and Heir, 2017; Bryant et al., 2017; Mitchell et al., 2017; Spiller et al., 2017; Afzali et al., 2017a; McNally et al., 2017a; Fried et al., 2018; Moshier et al., 2018; Phillips et al., 2018; Ross et al., 2018; von Stockert et al., 2018), which have led some to question amnesia as a core PTSD symptom (Armour et al., 2017). Low centrality of amnesia is also in line with factor-analysis studies (Yufik and Simms, 2010; Armour et al., 2015; Forbes et al., 2015) and memory research demonstrating similarities in the clearness and vividness of traumatic and non-traumatic memories, with the former found to be more potent amongst PTSD patients compared with trauma-exposed-non-PTSD individuals (Porter and Birt, 2001; Megias et al., 2007; Ross et al., 2018).
The physiological reactivity by trauma reminders-to-getting emotionally upset by trauma reminders-to-intrusive thoughts edges (all re-experiencing symptoms), as well as three additional edges involving re-experiencing nodes ( physiological reactivity by trauma reminders-to-detachment, flashbacks-to-avoidance of thoughts, and physiological reactivity by trauma reminders-to-startle response) were found to be of the strongest in the network. The DAG analysis further underscored the importance of re-experiencing symptoms, as physiological reactivity by trauma reminders and intrusive thoughts emerged as additional influential nodes, with flashbacks found to drive both these symptoms, with all three driving getting emotionally upset by trauma reminders. These results are in line with previous networks studies emphasizing the importance of re-experiencing symptoms in PTSD (Knefel et al., 2016; Armour et al., 2017; Bryant et al., 2017) and with research using structural equation modeling reporting a positive association between trauma-exposure and re-experiencing symptoms severity in veterans (Miller et al., 2008). The importance of re-experiencing symptoms as maladaptive reactivity to trauma-reminders in the symptom structure of PTSD is also in accordance with early and more recent theoretical accounts of PTSD (Brewin and Holmes, 2003). For example, the stress response theory (Horowitz, 1976; Horowitz, 1986), one of the earliest theoretical formulations of PTSD, suggests that a failure in assimilating an overflow of new trauma-related information with prior knowledge results in persistent posttraumatic reactions, as trauma memories continuously break into consciousness (i.e. re-experiencing symptoms such as intrusions and flashbacks). As a defensive response, the individual employs avoidance of trauma reminders. Thus, trauma information continues to repeatedly intrude and be avoided, creating a re-experiencing and avoidance cycle (Horowitz, 1986). Interestingly, in addition to the importance of re-experiencing symptoms in the PTSD network structure, results of the DAG analysis further showed most avoidance symptoms (e.g. avoidance of thoughts, anhedonia, detachment) to be directly triggered mostly by re-experiencing symptoms (or by other avoidance symptoms connected to re-experiencing symptoms), echoing the suggestion of the stress response theory. A more recent theory, the dual representation theory of PTSD (Brewin et al., 1996; Brewin, 2001; Brewin et al., 2010), also assign importance to re-experiencing symptoms in PTSD. According to this theory, posttraumatic pathological responses, and especially uncontrollable re-experiencing symptoms, emerge when traumatic memories are dissociated and stored separately from ordinary memories. Specifically, trauma stimuli that receive insufficient processing to be stored as regular autobiographical memories in the ‘verbally accessible memory’ (VAM), are stored instead in the parallel operating, but separate, image-based ‘situationally accessibly memory’ (SAM) system. In the context of trauma reminders, these trauma-related memories give rise to uncontrollable intrusions and to maladaptive psychological and physiological responses (Brewin and Holmes, 2003). Another recent theory acknowledging the importance of re-experiencing symptoms in PTSD is Ehlers and Clark’s cognitive model (Ehlers and Clark, 2000). Per this model, a pathological reaction following a traumatic event unfolds when the processing of traumatic information produces a continuous current sense of threat. As in the dual process theory, a trauma-related memory that lacks elaboration, that is not given a complete context, and that is inadequately integrated into the autobiographical memory system results in a memory that is hard to retrieve intentionally, leading to re-experiencing symptoms. The model further suggests that retrieval of trauma-related information from the associative memory system is mainly cue-driven and unintentional, priming the individual to trauma-reminders and leading directly to re-experiencing symptoms in response to relevant cues (Brewin and Holmes, 2003). Importantly, in comparison to avoidance and hyperarousal symptoms, also implicated in other psychopathologies (Joiner et al., 1999; Chawla and Ostafin, 2007), re-experiencing symptoms are regarded as more unique features of PTSD, less overlapping with other disorders (Chemtob et al., 1988; Brewin and Holmes, 2003; Ehlers, 2015). Thus, in conjunction with previous findings and theories, current results could be interpreted as suggesting re-experiencing symptoms, and especially flashbacks and getting emotionally upset by trauma reminders, as potential treatment targets for veterans with PTSD. Still, as the present study is cross-sectional in nature, this possibility should be taken with cautious and rigorously explored in future studies (Fried and Cramer, 2017; Dablander and Hinne, 2018; Phillips et al., 2018).
The comorbidity network revealed several important results. First, a distinct clustering of PTSD and depressive symptoms emerged, creating two discrete sub-networks. This differential clustering is in line with previous network research showing similar clustering when including depressive symptom as single nodes (Mitchell et al., 2017), and no change in the PTSD network structure after including depression as a single-node covariate (Armour et al., 2017). Second, same edges emerged as strongest in the CAPS-items network and within the PTSD cluster of the CAPS + MADRS-items network, suggesting minimal influence for the introduction of depression items on PTSD symptoms connectedness. Also, only slight changes in node centrality of PTSD symptoms within the co-morbid network were found, with flashbacks and getting emotionally upset by trauma reminders remaining the most central nodes, and amnesia and irritability the least central nodes. Finally, the DAG analysis yielded the same distinct clustering of PTSD and depressive symptoms. Together with findings of previous network studies, current results suggest that within-disorder (i.e. PTSD and depression) symptom connectivity is greater than between-disorder connections, even when co-occurrence of disorders is high. This suggestion is in accordance with previous research exploring the PTSD-MDD comorbidity using different analytic approaches, which supported the notion that while PTSD and MDD are highly correlated among traumatized individuals, they are also two distinct, independent and distinguishable constructs/responses to traumatic events (Blanchard et al., 1998; Grant et al., 2008; Gros et al., 2010; Post et al., 2011). Clinically, these findings might suggest that treatment of co-morbid PTSD-MDD should include components specifically addressing each pathology. Indeed, the above-cited research suggested to incorporate specific evidence-based treatment components for MDD into extant PTSD protocols to enhance treatment outcomes (Gros et al., 2010), as PTSD-MDD patients, compared to patients with PTSD alone, exhibit poorer treatment response following PTSD-focused treatment (Bernardy and Friedman, 2015), necessitating novel treatment strategies for PTSD-MDD (Flory and Yehuda, 2015).
Examining bridge nodes to explore between-disorders connections revealed that sleep difficulties per PTSD and depression emerged as major bridging nodes, replicating previous network studies (Mitchell et al., 2017; Afzali et al., 2017b). This fact is not surprising considering the high comorbidity rates of sleep disturbances with psychopathology in general, and more specifically with anxiety- and depression-related pathologies, with about 50–80% of psychiatric patients reporting sleep difficulties (Morin and Ware, 1996). Moreover, many DSM-based diagnoses, including PTSD and depression, entail sleep difficulties as one of their potential symptoms (American Psychiatric Association, 2000, 2013). Thus, the bridging role of sleep difficulties is in line with research considering overlapping symptoms as origins of high comorbidity in PTSD (Boschloo et al., 2015; Afzali et al., 2017b), supporting the notion that the PTSD-MDD comorbidity might reflect imprecisions in symptom classification into two discrete categorical diagnoses, suggesting a nosology artifact (Flory and Yehuda, 2015). However, avoidance of thoughts as well as getting emotionally upset by trauma reminders also emerged as a key bridge-nodes, replicating previous findings (Mitchell et al., 2017). Importantly, these symptoms are not overlapping symptoms, reflecting more unique pathways between PTSD and depression. Indeed, research has shown that removing overlapping symptoms from network analysis does not necessarily collapse the comorbidity networks (Afzali et al., 2017a, 2017b), and that overlapping symptoms cannot exclusive explain the PTSD-MDD association (Blanchard et al., 1998; Elhai et al., 2008; Elhai et al., 2011; Boschloo et al., 2015). Thus, the high centrality of non-overlapping bridge symptoms supports an alternative conceptualization of the PTSD-MDD comorbidity, namely, that this comorbidity is not a nosology artifact, but rather a distinct trauma-related phenotype, or even a subtype of PTSD, reflecting a fundamental dimension of risk for psychopathology following trauma exposure (Flory and Yehuda, 2015). On a more speculative note, current findings can be also viewed in light of research examining the temporal order of PTSD and MDD, in general and more specifically in combat-related PTSD, trying to ascertain whether pre-existing MDD is a risk factor for developing PTSD following trauma-exposure, whether MDD is a reaction to PTSD, considering PTSD as a risk factor for MDD, or whether there is a more complex, bi-directional relationship between PTSD and MDD, with shared risk factors and vulnerabilities (Stander et al., 2014; Angelakis and Nixon, 2015). While not addressing these options directly, due to the cross-sectional nature of our data, the differential clustering of PTSD and depressive symptoms in the CAPS + MADRS network, the results of the DAG analysis showing a similar differential clustering of PTSD and depressive symptoms, and the emergence of significant non-overlapping bridge symptoms, all allude to the conceptualization of the PTSD-MDD comorbidity as a trauma-related reaction comprised of mutual influential, yet distinct, symptom structures.
Addressing functioning in network analyses is important as the DSM classification system specifically requires significant impairment in functioning for a PTSD diagnosis (Ross et al., 2018). The DAG network revealed that functioning was directly triggered by the PTSD symptoms of disturbed sleep, anhedonia, and emotional numbness, and by one overlapping depressive symptom of reduced sleep. This is in line with research showing that sleep disturbances independently aggravate PTSD daytime symptoms, contributing to poorer functioning (DeViva et al., 2004; Germain et al., 2008), and that anhedonia and emotional numbness lead to deficient social activity and restriction of psychological resources in PTSD (Kashdan et al., 2006, 2007). Our results also align with the only network study that focused specifically on functional impairment in veterans with PTSD showing anhedonia to have the highest bridge centrality/EI measure (Ross et al., 2018). Thus, it seems that impaired functioning is directly influenced by depressive-like PTSD symptoms.
The network structure of the trauma-exposed (TE) treatment-seeking patients not meeting full criteria for PTSD was markedly less connected compared to the PTSD network, with different central edges and nodes, replicating a previous network study conducting similar analyses comparing US veterans with PTSD and subthreshold PTSD (Phillips et al., 2018). This aligns with the networks approach’s theoretical framing of psychopathology, namely, that a certain disorder will transpire when the required number of symptoms are activated for a sufficient duration, reaching the disorder’s ‘tipping point’ (van de Leemput et al., 2014; Hofmann et al., 2016; McNally, 2016, 2017). Still, this trauma-exposed population should not be taken lightly, especially among treatment-seeking veterans. Research has shown the detrimental effects of sub-threshold PTSD (Stein et al., 1997; Mylle and Maes, 2004; Jakupcak et al., 2007; Pietrzak et al., 2011; Mitchell et al., 2012; Schnurr, 2014; Jung et al., 2016), suggesting it as a risk condition at the prodromal phase of PTSD (Schnurr, 2014). Current results could assist therapists treating treatment-seeking trauma-exposed veterans with no ‘formal’ PTSD diagnosis by highlighting the need to address specific symptoms and connection between symptoms, which are different from those characterizing PTSD patients, aiming to weaken the corresponding network, and, potentially, halt the progression towards clinical PTSD.
While our findings corroborate previous research in PTSD, differences also emerged, potentially due to differences in various methodological features. This has been acknowledged by most network studies which have implicated potential differences in sample size, type (treatment-seeking, survey data), and status (clinical, probable, sub-threshold, trauma-exposed), and PTSD measures (self-report, clinician-administered) used for network construction (Armour et al., 2017; Birkeland and Heir, 2017; Bryant et al., 2017; Mitchell et al., 2017; Spiller et al., 2017; McNally et al., 2017a; Fried et al., 2018; Ross et al., 2018; Sullivan et al., 2018) in results heterogeneity. Gender may also contribute to observed differences (Mitchell et al., 2017), especially as we have explored an all-male sample. Finally, trauma type has been suggested as influencing PTSD expression/presentation (Norris et al., 2002a, 2002b; Chung and Breslau, 2008; Kelley et al., 2009; McNally, 2009), and, accordingly, network structure (Armour et al., 2017; Birkeland and Heir, 2017; Phillips et al., 2018; Ross et al., 2018; Sullivan et al., 2018; von Stockert et al., 2018). Indeed, comparing networks across three different traumatic events revealed corresponding differences in network structures (Benfer et al., 2018). Importantly, while seven studies explored veteran samples (Armour et al., 2017; Mitchell et al., 2017; Fried et al., 2018; Moshier et al., 2018; Phillips et al., 2018; Ross et al., 2018; von Stockert et al., 2018), trauma was restricted to being combat- or deployment-related only in three (Mitchell et al., 2017; Fried et al., 2018; Phillips et al., 2018), with results being mostly similar to the present study, namely, high centrality of getting emotionally upset by trauma reminders and low centrality for amnesia and irritability.
Limitations should be considered. First, data from this study is cross-sectional and as such cannot directly examine the temporal nature and directed influences of associations between symptoms (Fried and Cramer, 2017; Dablander and Hinne, 2018; Phillips et al., 2018). While trying to address this issue using the DAG analysis, which provides preliminary clues of directionality in cross-sectional data, DAG analysis has some strict assumptions curbing potential inferences (McNally et al., 2017a, 2017b). Primarily, for psychopathology network, including DAG, one must assume that no important variable has been omitted from the network (Jones et al., 2017). While attempting to address this by including depressive symptoms and a functioning measure, many other non-symptoms may play a causal role in PTSD, as well as in bridging PTSD and other disorders (Jones et al., 2017). These may include, among others, threat-related cognitive biases (Lazarov et al., 2018, 2019), neural abnormalities (O’Doherty et al., 2015; Koch et al., 2016), social functioning (Wilcox, 2010), and other factors which have been implicated in PTSD such as age (Konnert and Wong, 2015) and gender (Lehavot et al., 2018). Thus, future network-based research should include additional non-symptom nodes to enrich our understanding of PTSD (Jones et al., 2017). In addition, one must also assume that there are no feedback loops between symptoms, as in DAG activation flow is uni-directional. While thick edges (as those connecting re-experiencing symptoms; see Fig. 4) increase our confidence in directionality, future longitudinal studies could better assist in clarifying temporal sequences and potential causal relations between symptoms (Bringmann et al., 2013; Bryant et al., 2017; Greene et al., 2018). Second, the PTSD-related network structures were modeled using the CAPS 17-symptom-items, which are the same symptoms/items used to select/create the study groups (i.e. PTSD and TE samples). Importantly, when using covariance-based methods, this selection might bias the resultant covariance structure leading to spurious correlations, a bias known as Berkson’s bias (Cole et al., 2010; Berkson, 2014; Phillips et al., 2018; de Ron et al., 2019). Although there is currently not a clear best-practice guide for how to deal with this in network analysis in psychopathology-related research (Phillips et al., 2018), we wish to emphasize that selection per PTSD diagnosis was established based on the relatively lenient F1/I2 item rule (i.e. Frequency ⩾ 1, Intensity ⩾ 2), and not on a clinical significance cutoff score (Blake et al., 1995). Third, the present study used DSM-IV criteria in diagnosing PTSD and in constructing the different PTSD-related networks. Importantly, in DSM-5 three additional symptoms were added (for a total of 20 symptoms as opposed to the 17 symptoms in DSM-IV) with the addition of a forth symptom-cluster, following the division of the DSM-IV avoidance cluster into avoidance and negative alterations in cognitions and mood associated with the traumatic event (American Psychiatric Association, 2013; Hoge et al., 2014). Specifically, the negative alterations in cognitions and mood symptom-cluster introduces three ‘new’ depressive-like symptoms which were not included in DSM-IV, namely, negative feeling about oneself, others and the world (Symptom D2), self-blame (Symptom D3), and persistent negative emotional state (Symptom D4). Thus, constructing the PTSD-MDD comorbidity network using DSM-5 might have yielded different results. Still, as network analysis is data-driven, including depressive symptoms and a functioning measure provide vital information on symptom structure, partly covering the above-mentioned DSM-5 additional symptoms. Finally, although representing an important sub-population of patients, the sample’s homogeneity (i.e. male veterans with combat-related PTSD) impedes result-generalizability to other trauma-exposed populations.
Despite these limitations, the present study has several key strengths that outweigh its limitations and contribute to extant knowledge in the field. Results indicate a pivotal role for flashbacks and psychological reaction to trauma reminders, with strong connections to other re-experiencing symptoms, in the clinical presentation of combat-exposed veterans with PTSD. Depressive symptoms had little effect on the PTSD network structure, reflecting two separate diagnostic entities, but with meaningful between-disorder connections, suggesting independent yet mutually-influential systems.
Supplementary Material
Acknowledgments
Financial support. This work was supported by the National Institute of Mental Health T32-MH020004 (Amit Lazarov), T32-MH015144 (Benjamin Suarez-Jimenez), K01MH118428 (Benjamin Suarez-Jimenez), and R01MH105355 (Yuval Neria). The funding agency had no role in the study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Footnotes
Conflict of interest. None.
Supplementary material. The supplementary material for this article can be found at https://doi.org/10.1017/S0033291719002034.
Ethical standards. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Recently, however, some have questioned increasing sample size as means to ensure reduction in estimation errors and risk measures and, enhancement of specificity in network-based models (Epskamp and Fried, 2016; Kuismin and Sillanpaa, 2016; Williams and Rast, 2018).
Armed conflicts included Israel’s war of Independence; Operation Kadesh; the Six-Day War; War of Attrition; the Yom Kippur War; the 1982 and 2006 Lebanon Wars; Lebanon and West Bank routine security measures; the first and second Intifada (civilian uprising); and Operations Defensive Shield, Pillar of Defense, Cast Lead, and Protective Edge. Majority of veterans included in the present study participated in routine security measures in Lebanon and the 2006 Lebanon War
The notes appear after the main text.
The online version of this article has been updated since original publication. A notice detailing the changes has also been published.
References
- Afzali MH, Sunderland M, Batterham PJ, Carragher N, Calear A and Slade T (2017a) Network approach to the symptom-level association between alcohol use disorder and posttraumatic stress disorder. Social Psychiatry and Psychiatric Epidemiology 52, 329–339. [DOI] [PubMed] [Google Scholar]
- Afzali MH, Sunderland M, Teesson M, Carragher N, Mills K and Slade T (2017b) A network approach to the comorbidity between posttraumatic stress disorder and major depressive disorder: the role of overlapping symptoms. Journal of Affective Disorders 208, 490–496. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association (2000) Diagnostic and Statistical Manual of Mental Disorders, 4th Edn text revised. Washington, DC: American Psychiatric Publishing. [Google Scholar]
- American Psychiatric Association (2013) Diagnostic and Statistical Manual of Mental Disorders, 5th Edn Washington, DC: American Psychiatric Publishing. [Google Scholar]
- Angelakis S and Nixon RDV (2015) The comorbidity of PTSD and MDD: implications for clinical practice and future research. Behaviour Change 32, 1–25. [Google Scholar]
- Armour C and Shevlin M (2010) Testing the dimensionality of PTSD and the specificity of the dysphoria factor. Journal of Loss & Trauma 15, 11–27. [Google Scholar]
- Armour C, Tsai J, Durham TA, Charak R, Biehn TL, Elhai JD and Pietrzak RH (2015) Dimensional structure of DSM-5 posttraumatic stress symptoms: support for a hybrid anhedonia and externalizing behaviors model. Journal of Psychiatric Research 61, 106–113. [DOI] [PubMed] [Google Scholar]
- Armour C, Fried EI, Deserno MK, Tsai J and Pietrzak RH (2017) A network analysis of DSM-5 posttraumatic stress disorder symptoms and correlates in US military veterans. Journal of Anxiety Disorders 45, 49–59. [DOI] [PubMed] [Google Scholar]
- Au TM, Dickstein BD, Comer JS, Salters-Pedneault K and Litz BT (2013) Co-occurring posttraumatic stress and depression symptoms after sexual assault: a latent profile analysis. Journal of Affective Disorders 149, 209–216. [DOI] [PubMed] [Google Scholar]
- Benfer N, Bardeen JR, Cero I, Kramer LB, Whiteman SE, Rogers TA, Silverstein MW and Weathers FW (2018) Network models of post-traumatic stress symptoms across trauma types. Journal of Anxiety Disorders 58, 70–77. [DOI] [PubMed] [Google Scholar]
- Berkson J (2014) Limitations of the application of fourfold table analysis to hospital data. International Journal of Epidemiology 43, 511–515. [DOI] [PubMed] [Google Scholar]
- Bernardy NC and Friedman MJ (2015) Psychopharmacological strategies in the management of posttraumatic stress disorder (PTSD): what have we learned? Current Psychiatry Reports 17, 20. [DOI] [PubMed] [Google Scholar]
- Birkeland MS and Heir T (2017) Making connections: exploring the centrality of posttraumatic stress symptoms and covariates after a terrorist attack. European Journal of Psychotraumatology 8, 75–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS and Keane TM (1995) The development of a clinician-administered PTSD scale. Journal of Traumatic Stress 8, 75–90. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Buckley TC, Hickling EJ and Taylor AE (1998) Posttraumatic stress disorder and comorbid major depression: is the correlation an illusion? Journal of Anxiety Disorders 12, 21–37. [DOI] [PubMed] [Google Scholar]
- Borsboom D and Cramer AOJ (2013) Network analysis: an integrative approach to the structure of psychopathology. Annual Review of Clinical Psychology 9, 91–121. [DOI] [PubMed] [Google Scholar]
- Borsboom D, Mellenbergh GJ and van Heerden J (2003) The theoretical status of latent variables. Psychological Review 110, 203–219. [DOI] [PubMed] [Google Scholar]
- Borsboom D, Epskamp S, Kievit RA, Cramer AOJ and Schmittmann VD (2011) Transdiagnostic networks: commentary on Nolen-Hoeksema and Watkins (2011). Perspectives on Psychological Science 6, 610–614. [DOI] [PubMed] [Google Scholar]
- Boschloo L, van Borkulo CD, Rhemtulla M, Keyes KM, Borsboom D and Schoevers RA (2015) The network structure of symptoms of the diagnostic and statistical manual of mental disorders. Plos One 10, e0137621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley R, Greene J, Russ E, Dutra L and Westen D (2005) A multidimensional meta-analysis of psychotherapy for PTSD. The American Journal of Psychiatry 162, 214–227. [DOI] [PubMed] [Google Scholar]
- Brewin CR (2001) A cognitive neuroscience account of posttraumatic stress disorder and its treatment. Behaviour Research and Therapy 39, 373–393. [DOI] [PubMed] [Google Scholar]
- Brewin CR and Holmes EA (2003) Psychological theories of posttraumatic stress disorder. Clinical Psychology Review 23, 339–376. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Dalgleish T and Joseph S (1996) A dual representation theory of posttraumatic stress disorder. Psychological Review 103, 670–686. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Gregory JD, Lipton M and Burgess N (2010) Intrusive images in psychological disorders: characteristics, neural mechanisms, and treatment implications. Psychological Review 117, 210–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bringmann LF, Vissers N, Wichers M, Geschwind N, Kuppens P, Peeters F, Borsboom D and Tuerlinckx F (2013) A network approach to psychopathology: new insights into clinical longitudinal data. Plos One 8, e60188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bringmann LF, Elmer T, Epskamp S, Krause RW, Schoch D, Wichers M, Wigman J and Snippe E (2018) What do centrality measures measure in psychological networks? Preprint downloaded from ResearchGate. doi: 10.13140/RG.2.2.25024.58884. [DOI] [PubMed] [Google Scholar]
- Bryant RA, Moulds ML, Guthrie RM, Dang ST and Nixon RDV (2003) Imaginal exposure alone and imaginal exposure with cognitive restructuring in treatment of posttraumatic stress disorder. Journal of Consulting and Clinical Psychology 71, 706–712. [DOI] [PubMed] [Google Scholar]
- Bryant RA, Creamer M, O’Donnell M, Forbes D, McFarlane AC, Silove D and Hadzi-Pavlovic D (2017) Acute and chronic posttraumatic stress symptoms in the emergence of posttraumatic stress disorder: a network analysis. JAMA Psychiatry 74, 135–142. [DOI] [PubMed] [Google Scholar]
- Chawla N and Ostafin B (2007) Experiential avoidance as a functional dimensional approach to psychopathology: an empirical review. Journal of Clinical Psychology 63, 871–890. [DOI] [PubMed] [Google Scholar]
- Chemtob CM, Roitblat HL, Hamada RS, Carlson JG and Twentyman CT (1988) A cognitive action theory of post-traumatic stress disorder. Journal of Anxiety Disorders 2, 253–275. [Google Scholar]
- Chung H and Breslau N (2008) The latent structure of post-traumatic stress disorder: tests of invariance by gender and trauma type. Psychological Medicine 38, 563–573. [DOI] [PubMed] [Google Scholar]
- Cloitre M, Garvert DW, Brewin CR, Bryant RA and Maercker A (2013) Evidence for proposed ICD-11 PTSD and complex PTSD: a latent profile analysis. European Journal of Psychotraumatology 4, 20706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole SR, Platt RW, Schisterman EF, Chu HT, Westreich D, Richardson D and Poole C (2010) Illustrating bias due to conditioning on a collider. International Journal of Epidemiology 39, 417–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Contractor AA, Elhai JD, Fine TH, Tamburrino MB, Cohen G, Shirley E, Chan PK, Liberzon I, Galea S and Calabrese JR (2015) Latent profile analyses of posttraumatic stress disorder, depression and generalized anxiety disorder symptoms in trauma-exposed soldiers. Journal of Psychiatric Research 68, 19–26. [DOI] [PubMed] [Google Scholar]
- Costantini G and Epskamp S (2017) EstimateGroupNetwork: Perform the joint graphical lasso and selects tuning parameters. R package version 0.1.2. https://cran.r-project.org/web/packages/EstimateGroupNetwork/index.html. [Google Scholar]
- Costenbader E and Valente TW (2003) The stability of centrality measures when networks are sampled. Social Networks 25, 283–307. [Google Scholar]
- Cramer AOJ, Waldorp LJ, van der Maas HLJ and Borsboom D (2010a) Comorbidity: a network perspective. Behavioral and Brain Sciences 33, 137–150. [DOI] [PubMed] [Google Scholar]
- Cramer AOJ, Waldorp LJ, van der Maas HLJ and Borsboom D (2010b) Complex realities require complex theories: refining and extending the network approach to mental disorders. Behavioral and Brain Sciences 33, 178–193. [Google Scholar]
- Dablander F and Hinne M (2018) Centrality measures as a proxy for causal influence? A cautionary tale. Preprint downloaded from PsyArXiv. 10.31234/osf.io/nue4z. [DOI] [Google Scholar]
- Danaher P, Wang P and Witten DM (2014) The joint graphical lasso for inverse covariance estimation across multiple classes. Journal of the Royal Statistical Society Series B-Statistical Methodology 76, 373–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Ron J, Fried EI and Epskamp S (2019) Psychological Networks in Clinical Populations: A tutorial on the consequences of Berkson’s Bias. Preprint downloaded from PsyArXiv. 10.31234/osf.io/5t8zw. [DOI] [PubMed] [Google Scholar]
- DeViva JC, Zayfert C and Mellman TA (2004) Factors associated with insomnia among civilians seeking treatment for PTSD: an exploratory study. Behavioral Sleep Medicine 2, 162–176. [DOI] [PubMed] [Google Scholar]
- Deykin EY, Keane TM, Kaloupek D, Fincke G, Rothendler J, Siegfried M and Creamer K (2001) Posttraumatic stress disorder and the use of health services. Psychosomatic Medicine 63, 835–841. [DOI] [PubMed] [Google Scholar]
- Difede J, Olden M and Cukor J (2014) Evidence-based treatment of post-traumatic stress disorder. Annual Review of Medicine 65, 319–332. [DOI] [PubMed] [Google Scholar]
- Ehlers A (2015) Intrusive reexperiencing in posttraumatic stress disorder: memory processes and their implications for therapy. Clinical Perspectives on Autobiographical Memory 12, 109–132. [Google Scholar]
- Ehlers A and Clark DM (2000) A cognitive model of posttraumatic stress disorder. Psychiatria Hungarica 15, 319–345. [DOI] [PubMed] [Google Scholar]
- Elhai JD, Grubaugh AL, Kashdan TB and Frueh BC (2008) Empirical examination of a proposed refinement to DSM-IV posttraumatic stress disorder symptom criteria using the National Comorbidity Survey Replication data. Journal of Clinical Psychiatry 69, 597–602. [DOI] [PubMed] [Google Scholar]
- Elhai JD, Carvalho LDF, Miguel FK, Palmieri PA, Primi R and Frueh BC (2011) Testing whether posttraumatic stress disorder and major depressive disorder are similar or unique constructs. Journal of Anxiety Disorders 25, 404–410. [DOI] [PubMed] [Google Scholar]
- Epskamp S and Fried EI (2016) A primer on estimating regularized psychological networks. Retrieved from http://arxiv.org/abs/1607.01367. [Google Scholar]
- Epskamp S and Fried EI (2018) A tutorial on regularized partial correlation networks. Psychological Methods 23, 617–634. [DOI] [PubMed] [Google Scholar]
- Epskamp S, Cramer AOJ, Waldorp LJ, Schmittmann VD and Borsboom D (2012) Qgraph: network visualizations of relationships in psychometric data. Journal of Statistical Software 48, 1–18. [Google Scholar]
- Epskamp S, Borsboom D and Fried EI (2018) Estimating psychological networks and their accuracy: a tutorial paper. Behavior Research Methods 50, 195–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flory JD and Yehuda R (2015) Comorbidity between post-traumatic stress disorder and major depressive disorder: alternative explanations and treatment considerations. Dialogues in Clinical Neuroscience 17, 141–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes D, Lockwood E, Elhai JD, Creamer M, Bryant R, McFarlane A, Silove D, Miller MW, Nickerson A and O’Donnell M (2015) An evaluation of the DSM-5 factor structure for posttraumatic stress disorder in survivors of traumatic injury. Journal of Anxiety Disorders 29, 43–51. [DOI] [PubMed] [Google Scholar]
- Fried EI and Cramer AOJ (2017) Moving forward: challenges and directions for psychopathological network theory and methodology. Perspectives on Psychological Science 12, 999–1020. [DOI] [PubMed] [Google Scholar]
- Fried EI, van Borkulo CD, Cramer AOJ, Boschloo L, Schoevers RA and Borsboom D (2017) Mental disorders as networks of problems: a review of recent insights. Social Psychiatry and Psychiatric Epidemiology 52, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried EI, Eidhof MB, Palic S, Costantini G, Huisman-van Dijk HM, Bockting CLH, Engelhard I, Armour C, Nielsen ABS and Karstoft KI (2018) Replicability and generalizability of posttraumatic stress disorder (PTSD) networks: a cross-cultural multisite study of PTSD symptoms in four trauma patient samples. Clinical Psychological Science 6, 335–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman MJ, Kilpatrick DG, Schnurr PP and Weathers FW (2016) Correcting misconceptions about the diagnostic criteria for posttraumatic stress disorder in DSM-5. JAMA Psychiatry 73, 753–754. [DOI] [PubMed] [Google Scholar]
- Fulton JJ, Calhoun PS, Wagner HR, Schry AR, Hair LP, Feeling N, Elbogen E and Beckham JC (2015) The prevalence of posttraumatic stress disorder in operation enduring freedom/operation Iraqi freedom (OEF/OIF) veterans: a meta-analysis. Journal of Anxiety Disorders 31, 98–107. [DOI] [PubMed] [Google Scholar]
- Galatzer-Levy IR and Bryant RA (2013) 636120 ways to have posttraumatic stress disorder. Perspectives on Psychological Science 8, 651–662. [DOI] [PubMed] [Google Scholar]
- Germain A, Buysse DJ and Nofzinger E (2008) Sleep-specific mechanisms underlying posttraumatic stress disorder: integrative review and neurobiological hypotheses. Sleep Medicine Reviews 12, 185–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillespie K, Duffy M, Hackmann A and Clark DM (2002) Community-based cognitive therapy in the treatment of post-traumatic stress disorder following the omagh bomb. Behavior Research and Therapy 40, 345–357. [DOI] [PubMed] [Google Scholar]
- Goldstein RB, Smith SM, Chou SP, Saha TD, Jung J, Zhang HT, Pickering RP, Ruan WJ, Huang BJ and Grant BF (2016) The epidemiology of DSM-5 posttraumatic stress disorder in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions-III. Social Psychiatry and Psychiatric Epidemiology 51, 1137–1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant DM, Beck JG, Marques L, Palyo SA and Clapp JD (2008) The structure of distress following trauma: posttraumatic stress disorder, major depressive disorder, and generalized anxiety disorder. Journal of Abnormal Psychology 117, 662–672. [DOI] [PubMed] [Google Scholar]
- Green JL, Lowry JL and Kopta SM (2003) College students versus counseling center clients: what are the differences? Journal of College Student Psychotherapy 17, 25–37. [Google Scholar]
- Green BL, Krupnick JL, Chung J, Siddique J, Krause ED, Revicki D, Frank L and Miranda J (2006) Impact of PTSD comorbidity on one-year outcomes in a depression trial. Journal of Clinical Psychology 62, 815–835. [DOI] [PubMed] [Google Scholar]
- Greene T, Gelkopf M, Epskamp S and Fried E (2018) Dynamic networks of PTSD symptoms during conflict. Psychological Medicine 48, 2409–2417. [DOI] [PubMed] [Google Scholar]
- Gros DF, Simms LJ and Acierno R (2010) Specificity of posttraumatic stress disorder symptoms an investigation of comorbidity between posttraumatic stress disorder symptoms and depression in treatment-seeking veterans. Journal of Nervous and Mental Disease 198, 885–890. [DOI] [PubMed] [Google Scholar]
- Guina J (2016) Changes to the definition of posttraumatic stress disorder in the DSM-5. JAMA Psychiatry 73, 1201–1202. [DOI] [PubMed] [Google Scholar]
- Haag C, Robinaugh DJ, Ehlers A and Kleim B (2017) Understanding the emergence of chronic posttraumatic stress disorder through acute stress symptom networks. JAMA Psychiatry 74, 649–650. [DOI] [PubMed] [Google Scholar]
- Hallquist M, Wright AG and Molenaar PCM (2019) Problems with centrality measures in psychopathology symptom networks: Why network psychometrics cannot escape psychometric theory. Preprint downloaded from PsyArXiv. 10.31234/osf.io/pg4mf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen M, Hyland P, Armour C, Shevlin M and Elklit A (2015) Less is more? Assessing the validity of the ICD-11 model of PTSD across multiple trauma samples. European Journal of Psychotraumatology 6, 28766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heeren A, Jones PJ and McNally RJ (2018) Mapping network connectivity among symptoms of social anxiety and comorbid depression in people with social anxiety disorder. Journal of Affective Disorders 228, 75–82. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Curtiss J and McNally RJ (2016) A complex network perspective on clinical science. Perspectives on Psychological Science 11, 597–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoge CW, Riviere LA, Wilk JE, Herrell RK and Weathers FW (2014) The prevalence of post-traumatic stress disorder (PTSD) in US combat soldiers: a head-to-head comparison of DSM-5 versus DSM-IV-TR symptom criteria with the PTSD checklist. The Lancet. Psychiatry 1, 269–277. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Yehuda R, Castro CA, McFarlane AC, Vermetten E, Jetly R, Koenen KC, Greenberg N, Shalev AY, Rauch SAM, Marmar CR and Rothbaum BO (2016) Unintended consequences of changing the definition of posttraumatic stress disorder in DSM-5 critique and call for action. JAMA Psychiatry 73, 750–752. [DOI] [PubMed] [Google Scholar]
- Horowitz MJ (1976) Stress Response Syndromes. New York: Aronson. [Google Scholar]
- Horowitz MJ (1986) Stress Response Syndromes. Northvale, NJ: Jason Aronson. [Google Scholar]
- Jakupcak M, Conybeare D, Phelps L, Hunt S, Holmes HA, Felker B, Klevens M and McFall ME (2007) Anger, hostility, and aggression among Iraq and Afghanistan war veterans reporting PTSD and subthreshold PTSD. Journal of Traumatic Stress 20, 945–954. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Steer RA, Beck AT, Schmidt NB, Rudd MD and Catanzaro SJ (1999) Physiological hyperarousal: construct validity of a central aspect of the tripartite model of depression and anxiety. Journal of Abnormal Psychology 108, 290–298. [DOI] [PubMed] [Google Scholar]
- Jones PJ, Heeren A and McNally RJ (2017) Commentary: a network theory of mental disorders. Frontiers in Psychology 8, 1305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones PJ, Mair P, Riemann BC, Mugno BL and McNally RJ (2018) A network perspective on comorbid depression in adolescents with obsessive-compulsive disorder. Journal of Anxiety Disorders 53, 1–8. [DOI] [PubMed] [Google Scholar]
- Jones PJ, Ma R and McNally RJ (2019) Bridge centrality: a network approach to understanding comorbidity. Multivariate Behavioral Research 1–15. [DOI] [PubMed] [Google Scholar]
- Jung WH, Chang KJ and Kim NH (2016) Disrupted topological organization in the whole-brain functional network of trauma-exposed firefighters: a preliminary study. Psychiatry Research-Neuroimaging 250, 15–23. [DOI] [PubMed] [Google Scholar]
- Kashdan TB, Elhai JD and Frueh BC (2006) Anhedonia and emotional numbing in combat veterans with PTSD. Behaviour Research and Therapy 44, 457–467. [DOI] [PubMed] [Google Scholar]
- Kashdan TB, Elhai JD and Frueh BC (2007) Anhedonia, emotional numbing, and symptom overreporting in male veterans with PTSD. Personality and Individual Differences 43, 725–735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keane TM and Barlow DH (2002) Posttraumatic stress disorder In Barlow DH (ed.), Anxiety and Its Disorders: The Nature and Treatment of Anxiety and Panic. New York, NY: Guilford Press, pp. 418–453. [Google Scholar]
- Kelley LP, Weathers FW, McDevitt-Murphy ME, Eakin DE and Flood AM (2009) A comparison of PTSD symptom patterns in three types of civilian trauma. Journal of Traumatic Stress 22, 227–235. [DOI] [PubMed] [Google Scholar]
- Kessler RC (2000) Posttraumatic stress disorder: the burden to the individual and to society. The Journal of Clinical Psychiatry 61, 4–12. [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M and Nelson CB (1995) Posttraumatic-Stress-Disorder in the national comorbidity survey. Archives of General Psychiatry 52, 1048–1060. [DOI] [PubMed] [Google Scholar]
- Khan A, Khan SR, Shankles EB and Polissar NL (2002) Relative sensitivity of the Montgomery-Asberg Depression Rating Scale, the Hamilton Depression rating scale and the Clinical Global Impressions rating scale in antidepressant clinical trials. International Clinical Psychopharmacology 17, 281–285. [DOI] [PubMed] [Google Scholar]
- Khan A, Brodhead AE and Kolts RL (2004) Relative sensitivity of the Montgomery-Asberg depression rating scale, the Hamilton depression rating scale and the Clinical Global Impressions rating scale in antidepressant clinicatrials: a replication analysis. International Clinical Psychopharmacology 19, 157–160. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM and Friedman MJ (2013) National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. Journal of Traumatic Stress 26, 537–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knefel M, Tran US and Lueger-Schuster B (2016) The association of post-traumatic stress disorder, complex posttraumatic stress disorder, and borderline personality disorder from a network analytical perspective. Journal of Anxiety Disorders 43, 70–78. [DOI] [PubMed] [Google Scholar]
- Koch SBJ, van Zuiden M, Nawijn L, Frijling JL, Veltman DJ and Olff M (2016) Aberrant resting-state brain activity in posttraumatic stress disorder: a meta-analysis and systematic review. Depression and Anxiety 33, 592–605. [DOI] [PubMed] [Google Scholar]
- Konnert C and Wong M (2015) Age differences in PTSD among Canadian veterans: age and health as predictors of PTSD severity. International Psychogeriatrics 27, 297–304. [DOI] [PubMed] [Google Scholar]
- Kuismin M and Sillanpaa MJ (2016) Use of Wishart prior and simple extensions for sparse precision matrix estimation. Plos One 11, e0148171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lapierre CB, Schwegler AE and LaBauve BJ (2007) Posttraumatic stress and depression symptoms in soldiers returning from combat operations in Iraq and Afghanistan. Journal of Traumatic Stress 20, 933–943. [DOI] [PubMed] [Google Scholar]
- Lazarov A, Suarez-Jimenez B, Abend R, Naim R, Shvil E, Helpman L, Zhu X, Papini S, Duroski A, Rom R, Schneier FR, Pine DS, Bar-Haim Y and Neria Y (2018) Bias-contingent attention bias modification and attention control training in treatment of PTSD: a randomized control trial. Psychological Medicine 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarov A, Suarez-Jimenez B, Tamman A, Falzon L, Zhu X, Edmondson DE and Neria Y (2019) Attention to threat in posttraumatic stress disorder as indexed by eye-tracking indices: a systematic review. Psychological Medicine 49, 705–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehavot K, Katon JG, Chen JA, Fortney JC and Simpson TL (2018) Post-traumatic stress disorder by gender and veteran Status. American Journal of Preventive Medicine 54, e1–e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levi O, Bar-Haim Y, Kreiss Y and Fruchter E (2016) Cognitive-Behavioural therapy and psychodynamic psychotherapy in the treatment of combat-related post-traumatic stress disorder: a comparative effectiveness study. Clinical Psychology & Psychotherapy 23, 298–307. [DOI] [PubMed] [Google Scholar]
- Levi O, Shoval-Zuckerman Y, Fruchter E, Bibi A, Bar-Haim Y and Wald I (2017) Benefits of a Psychodynamic Group Therapy (PGT) model for treating veterans With PTSD. Journal of Clinical Psychology 73, 1247–1258. [DOI] [PubMed] [Google Scholar]
- Maercker A, Brewin CR, Bryant RA, Cloitre M, Reed GM, van Ommeren M, Humayun A, Jones LM, Kagee A, Llosa AE, Rousseau C, Somasundaram DJ, Souza R, Suzuki Y, Weissbecker I, Wessely SC, First MB and Saxena S (2013) Proposals for mental disorders specifically associated with stress in the International Classification of Diseases-11. Lancet 381, 1683–1685. [DOI] [PubMed] [Google Scholar]
- McDonagh A, Friedman M, McHugo G, Ford J, Sengupta A, Mueser K, Carney-Demment C, Fournier D, Schnurr PP and Descamps M (2005) Randomized trial of cognitive-behavioral therapy for posttraumatic stress disorder in adult female survivors of childhood abuse. Journal of Consulting and Clinical Psychology 73, 515–524. [DOI] [PubMed] [Google Scholar]
- McNally RJ (2009) Can we fix PTSD in DSM-V? Depression and Anxiety 26, 597–600. [DOI] [PubMed] [Google Scholar]
- McNally RJ (2016) Can network analysis transform psychopathology? Behaviour Research and Therapy 86, 95–104. [DOI] [PubMed] [Google Scholar]
- McNally RJ (2017) Networks and nosology in posttraumatic stress disorder. JAMA Psychiatry 74, 124–125. [DOI] [PubMed] [Google Scholar]
- McNally RJ, Robinaugh DJ, Wu GWY, Wang L, Deserno MK and Borsboom D (2015) Mental disorders as causal systems: a network approach to posttraumatic stress disorder. Clinical Psychological Science 3, 836–849. [Google Scholar]
- McNally RJ, Heeren A and Robinaugh DJ (2017a) A Bayesian network analysis of posttraumatic stress disorder symptoms in adults reporting childhood sexual abuse. European Journal of Psychotraumatology 8, 341276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNally RJ, Mair P, Mugno BL and Riemann BC (2017b) Co-morbid obsessive-compulsive disorder and depression: a Bayesian network approach. Psychological Medicine 47, 1204–1214. [DOI] [PubMed] [Google Scholar]
- Megias JL, Ryan E, Vaquero JMM and Frese B (2007) Comparisons of traumatic and positive memories in people with and without PTSD profile. Applied Cognitive Psychology 21, 117–130. [Google Scholar]
- Miller MW, Wolf EJ, Martin E, Kaloupek DG and Keane TM (2008) Structural equation modeling of associations among combat exposure, PTSD symptom factors, and global assessment of functioning. Journal of Rehabilitation Research and Development 45, 359–369. [DOI] [PubMed] [Google Scholar]
- Miller MW, Wolf EJ, Harrington KM, Brown TA, Kaloupek DG and Keane TM (2010) An evaluation of competing models for the structure of PTSD symptoms using external measures of comorbidity. Journal of Traumatic Stress 23, 631–638. [DOI] [PubMed] [Google Scholar]
- Mitchell KS, Mazzeo SE, Schlesinger MR, Brewerton TD and Smith BN (2012) Comorbidity of partial and subthreshold ptsd among men and women with eating disorders in the national comorbidity survey-replication study. International Journal of Eating Disorders 45, 307–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell KS, Wolf EJ, Bovin MJ, Lee LO, Green JD, Rosen RC, Keane TM and Marx BP (2017) Network models of DSM-5 posttraumatic stress disorder: implications for ICD-11. Journal of Abnormal Psychology 126, 355–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montgomery SA and Asberg M (1979) A new depression scale designed to be sensitive to change. The British Journal of Psychiatry 134, 382–389. [DOI] [PubMed] [Google Scholar]
- Morin CM and Ware JC (1996) Sleep and psychopathology. Applied & Preventive Psychology 5, 211–224. [Google Scholar]
- Moshier SJ, Bovin MJ, Gay NG, Wisco BE, Mitchell KS, Lee DJ, Sloan DM, Weathers FW, Schnurr PP, Keane TM and Marx BP (2018) Examination of posttraumatic stress disorder symptom networks using clinician-rated and patient-rated data. Journal of Abnormal Psychology 127, 541–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moskowitz DS (1986) Comparison of self-reports, reports by knowledgeable informants, and behavioral observation data. Journal of Personality 54, 294–317. [Google Scholar]
- Mylle J and Maes M (2004) Partial posttraumatic stress disorder revisited. Journal of Affective Disorders 78, 37–48. [DOI] [PubMed] [Google Scholar]
- National Institute for Clinical Excellence (2005) Post-traumatic Stress Disorder: The Management of PTSD in Adults and Children in Primary and Secondary Care. London, UK: National Institute for Clinical Excellence (NICE). [Google Scholar]
- Neria Y and Bromet EJ (2000) Comorbidity of PTSD and depression: linked or separate incidence. Biological Psychiatry 48, 878–880. [DOI] [PubMed] [Google Scholar]
- Norris FH, Friedman MJ and Watson PJ (2002a) 60000 disaster victims speak: part II. Summary and implications of the disaster mental health research. Psychiatry-Interpersonal and Biological Processes 65, 240–260. [DOI] [PubMed] [Google Scholar]
- Norris FH, Friedman MJ, Watson PJ, Byrne CM, Diaz E and Kaniasty K (2002b) 60000 disaster victims speak: part I. An empirical review of the empirical literature, 1981–2001. Psychiatry 65, 207–239. [DOI] [PubMed] [Google Scholar]
- O’Doherty DCM, Chitty KM, Saddiqui S, Bennett MR and Lagopoulos J (2015) A systematic review and meta-analysis of magnetic resonance imaging measurement of structural volumes in posttraumatic stress disorder. Psychiatry Research-Neuroimaging 232, 1–33. [DOI] [PubMed] [Google Scholar]
- O’Donnell ML, Alkemade N, Nickerson A, Creamer M, McFarlane AC, Silove D, Bryant RA and Forbes D (2014) Impact of the diagnostic changes to post-traumatic stress disorder for DSM-5 and the proposed changes to ICD-11. British Journal of Psychiatry 205, 230–235. [DOI] [PubMed] [Google Scholar]
- Oquendo MA, Friend JM, Halberstam B, Brodsky BS, Burke AK, Grunebaum MF, Malone KM and Mann JJ (2003) Association of comorbid posttraumatic stress disorder and major depression with greater risk for suicidal behavior. American Journal of Psychiatry 160, 580–582. [DOI] [PubMed] [Google Scholar]
- Papini S, Rubin M, Telch MJ, Smits JAJ and Hien DA (2018) Pretreatment PTSD symptom network metrics predict the strength of the relationship between node change and network change during treatment. Preprint downloaded from ResearchGate. doi: 10.1002/jts.22379. [DOI] [PubMed] [Google Scholar]
- Phillips RD, Wilson SM, Sun DL, VA Mid-Atlantic MIRECC Workgroup and Morey R (2018) Posttraumatic stress disorder symptom network analysis in U.S. Military veterans: examining the impact of combat exposure. Frontiers in Psychiatry 9, 608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrzak RH, Goldstein RB, Southwick SM and Grant BF (2011) Prevalence and axis I comorbidity of full and partial posttraumatic stress disorder in the United States: results from wave 2 of the national epidemiologic survey on alcohol and related conditions. Journal of Anxiety Disorders 25, 456–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porter S and Birt AR (2001) Is traumatic memory special? A comparison of traumatic memory characteristics with memory for other emotional life experiences. Applied Cognitive Psychology 15, S101–S117. [Google Scholar]
- Post LM, Zoellner LA, Youngstrom E and Feeny NC (2011) Understanding the relationship between co-occurring PTSD and MDD: symptom severity and affect. Journal of Anxiety Disorders 25, 1123–1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price M and van Stolk-Cooke K (2015) Examination of the interrelations between the factors of PTSD, major depression, and generalized anxiety disorder in a heterogeneous trauma-exposed sample using DSM 5 criteria. Journal of Affective Disorders 186, 149–155. [DOI] [PubMed] [Google Scholar]
- Price M, Legrand AC, Brier ZMF and Hebert-Dufresne L (2019) The symptoms at the center: examining the comorbidity of posttraumatic stress disorder, generalized anxiety disorder, and depression with network analysis. Journal of Psychiatric Research 109, 52–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pupo MC, Jorge MR, Schoedl AF, Bressan RA, Andreoli SB, Mello MF and Mari JD (2011) The accuracy of the clinician-administered PTSD scale (CAPS) to identify PTSD cases in victims of urban violence. Psychiatry Research 185, 157–160. [DOI] [PubMed] [Google Scholar]
- Ramsawh HJ, Fullerton CS, Mash HB, Ng TH, Kessler RC, Stein MB and Ursano RJ (2014) Risk for suicidal behaviors associated with PTSD, depression, and their comorbidity in the U.S. Army. Journal of Affective Disorders 161, 116–122. [DOI] [PubMed] [Google Scholar]
- Robinaugh DJ, Millner AJ and McNally RJ (2016) Identifying highly influential nodes in the complicated grief network. Journal of Abnormal Psychology 125, 747–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross J, Murphy D and Armour C (2018) A network analysis of DSM-5 post-traumatic stress disorder and functional impairment in UK treatment-seeking veterans. Journal of Anxiety Disorders 57, 7–15. [DOI] [PubMed] [Google Scholar]
- Rytwinski NK, Avena JS, Echiverri-Cohen AM, Zoellner LA and Feeny NC (2014) The relationships between posttraumatic stress disorder severity, depression severity and physical health. Journal of Health Psychology 19, 509–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmittmann VD, Cramer AOJ, Waldorp LJ, Epskamp S, Kievit RA and Borsboom D (2013) Deconstructing the construct: a network perspective on psychological phenomena. New Ideas in Psychology 31, 43–53. [Google Scholar]
- Schnurr PP (2014) A guide to the literature on partial PTSD. PTSD Research Quarterly 25, 1–3. [Google Scholar]
- Schwarz N (1999) Self-reports – How the questions shape the answers. American Psychologist 54, 93–105. [Google Scholar]
- Scutari M (2010) Learning Bayesian networks with the bnlearn R package. Journal of Statistical Software 35, 1–22.21603108 [Google Scholar]
- Scutari M and Denis JB (2014) Bayesian Networks: With Examples in R. New York: Chapman and Hall/CRC. [Google Scholar]
- Simms LJ, Watson D and Doebbeling BN (2002) Confirmatory factor analyses of posttraumatic stress symptoms in deployed and nondeployed veterans of the gulf War. Journal of Abnormal Psychology 111, 637–647. [DOI] [PubMed] [Google Scholar]
- Spiller TR, Schick M, Schnyder U, Bryant RA, Nickerson A and Morina N (2017) Symptoms of posttraumatic stress disorder in a clinical sample of refugees: a network analysis. European Journal of Psychotraumatology 8, 1318032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, First MB and Wakefield JC (2007) Saving PTSD from itself in DSM-V. Journal of Anxiety Disorders 21, 233–241. [DOI] [PubMed] [Google Scholar]
- Spoont MR, Williams JW, Kehle-Forbes S, Nieuwsma JA, Mann-Wrobel MC and Gross R (2015) Does this patient have posttraumatic stress disorder? Rational clinical examination systematic review. JAMA 314, 501–510. [DOI] [PubMed] [Google Scholar]
- Stander VA, Thomsen CJ and Highfill-McRoy RM (2014) Etiology of depression comorbidity in combat-related PTSD: a review of the literature. Clinical Psychology Review 34, 87–98. [DOI] [PubMed] [Google Scholar]
- Steckler T and Risbrough V (2012) Pharmacological treatment of PTSD-established and new approaches. Neuropharmacology 62, 617–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein MB, Walker JR, Hazen AL and Forde DR (1997) Full and partial post-traumatic stress disorder: findings from a community survey. American Journal of Psychiatry 154, 1114–1119. [DOI] [PubMed] [Google Scholar]
- Stein NR, Dickstein BD, Schuster J, Litz BT and Resick PA (2012) Trajectories of response to treatment for posttraumatic stress disorder. Behavior Therapy 43, 790–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein DJ, McLaughlin KA, Koenen KC, Atwoli L, Friedman MJ, Hill ED, Maercker A, Petukhova M, Shahly V, van Ommeren M, Alonso J, Borges G, de Girolamo G, de Jonge P, Demyttenaere K, Florescu S, Karam EG, Kawakami N, Matschinger H, Okoliyski M, Posada-Villa J, Scott KM, Viana MC and Kessler RC (2014) DSM-5 and ICD-11 definitions of posttraumatic stress disorder: investigating “narrow” and “broad” approaches. Depression and Anxiety 31, 494–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan GM and Neria Y (2009) Pharmacotherapy of PTSD: current Status and controversies. Psychiatric Annals 39, 342–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan CP, Smith AJ, Lewis M and Jones RT (2018) Network analysis of PTSD symptoms following mass violence. Psychological Trauma-Theory Research Practice and Policy 10, 58–66. [DOI] [PubMed] [Google Scholar]
- Svetlicky V, Solomon Z, Benbenishty R, Levi O and Lubin G (2010) Combat exposure, posttraumatic stress symptoms and risk-taking behavior in veterans of the Second Lebanon War. Israel Journal of Psychiatry and Related Sciences 47, 276–283. [PubMed] [Google Scholar]
- Trull TJ, Widiger TA and Burr R (2001) A structured interview for the assessment of the five-factor model of personality: facet-level relations to the axis II personality disorders. Journal of Personality 69, 175–198. [DOI] [PubMed] [Google Scholar]
- Tsai J, Harpaz-Rotem I, Armour C, Southwick SM, Krystal JH and Pietrzak RH (2015) Dimensional structure of DSM-5 posttraumatic stress disorder symptoms: results from the national health and resilience in veterans study. Journal of Clinical Psychiatry 76, 546–553. [DOI] [PubMed] [Google Scholar]
- van Borkulo CD and Millner SE (2016) Network Comparison Test: Statistical comparison of two networks based on three invariance measures. R package version 2.0.1. https://cran.r-project.org/web/packages/NetworkComparisonTest/index.html. [Google Scholar]
- van de Leemput IA, Wichers M, Cramer AOJ, Borsboom D, Tuerlinckx F, Kuppens P, van Nes EH, Viechtbauer W, Giltay EJ, Aggen SH, Derom C, Jacobs N, Kendler KS, van der Maas HLJ, Neale MC, Peeters F, Thiery E, Zachar P and Scheffer M (2014) Critical slowing down as early warning for the onset and termination of depression. Proceedings of the National Academy of Sciences of the United States of America 111, 87–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanzhula IA, Calebs B, Fewell L and Levinson CA (2018) Illness pathways between eating disorder and post‐traumatic stress disorder symptoms: understanding comorbidity with network analysis. European Eating Disorders Review 27, 147–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Stockert SHH, Fried EI, Armour C and Pietrzak RH (2018) Evaluating the stability of DSM-5 PTSD symptom network structure in a national sample of US military veterans. Journal of Affective Disorders 229, 63–68. [DOI] [PubMed] [Google Scholar]
- Wang SB, Jones PJ, Dreier M, Elliott H and Grilo CM (2018) Core psychopathology of treatment-seeking patients with binge-eating disorder: a network analysis investigation. Psychological Medicine 49, 1923–1928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D (2009) Differentiating the mood and anxiety disorders: a quadripartite model. Annual Review of Clinical Psychology 5, 221–247. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Keane TM and Davidson JRT (2001) Clinician-administered PTSD scale: a review of the first ten years of research. Depression and Anxiety 13, 132–156. [DOI] [PubMed] [Google Scholar]
- Westphal M, Olfson M, Gameroff MJ, Wickramaratne P, Pilowsky DJ, Neugebauer R, Lantigua R, Shea S and Neria Y (2011) Functional impairment in adults with past posttraumatic stress disorder: findings from primary care. Depression and Anxiety 28, 686–695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilcox S (2010) Social relationships and PTSD symptomatology in combat veterans. Psychological Trauma-Theory Research Practice and Policy 2, 175–182. [Google Scholar]
- Williams DR and Rast P (2018) Back to the basics: rethinking partial correlation network methodology. British Journal of Mathematical and Statistical Psychology 1–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wisco BE, Marx BP, Miller MW, Wolf EJ, Mota NP, Krystal JH, Southwick SM and Pietrzak RH (2016a) Probable posttraumatic stress disorder in the US veteran population according to DSM-5: results from the national health and resilience in veterans study. Journal of Clinical Psychiatry 77, 1503–1510. [DOI] [PubMed] [Google Scholar]
- Wisco BE, Miller MW, Wolf EJ, Kilpatrick D, Resnick HS, Badour CL, Marx BP, Keane TM, Rosen RC and Friedman MJ (2016b) The impact of proposed changes to ICD-11 on estimates of PTSD prevalence and comorbidity. Psychiatry Research 240, 226–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2018) International statistical classification of diseases and related health problems (11th Revision). Retrieved from https://icd.who.int/browse11/l-m/en. [Google Scholar]
- Yufik T and Simms LJ (2010) A meta-analytic investigation of the structure of posttraumatic stress disorder symptoms. Journal of Abnormal Psychology 119, 764–776. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.