Abstract
Background:
The increased prevalence of psychiatric illness among patients with takotsubo cardiomyopathy (TC) has been previously described.
Objectives:
We sought to assess the effect of pre-existing psychiatric illness on clinical outcomes following the diagnosis of TC.
Methods:
Adults diagnosed with TC at Vanderbilt University Medical Center between 1999 and 2015 were included in the study. Medical records were retrospectively reviewed to identify any pre-existing mood, anxiety, or schizophrenia-spectrum illness before TC presentation. Multivariable logistic regression was used to test for independent association of pre-existing psychiatric illness with 30-day mortality and recurrent TC; Cox proportional hazard analysis was used to evaluate for association with long-term mortality.
Results:
Among 306 patients diagnosed with TC during the study period, 114 (37%) had a pre-existing psychiatric illness. In all, 43 (14%) and 88 (29%) patients died within 30 days of index diagnosis and as of last medical record review, respectively. Of the 269 who survived their index hospitalization, 19 (7%) had a confirmed recurrent episode of TC. In multivariable analyses, pre-existing psychiatric illness was not associated with increased 30-day (P = 0.320) or long-term (P = 0.621) mortality. Pre-existing psychiatric illness was associated with higher risk of recurrent TC (odds ratio = 7.44, 95% CI: 2.30–24.01, P < 0.001).
Conclusions:
Pre-existing psychiatric illness was associated with an increased risk of recurrent TC. No significant association was noted between pre-existing psychiatric illness and survival.
Keywords: Takotsubo, Stress cardiomyopathy, Psychiatric illness, Survival, Recurrence
INTRODUCTION
Takotsubo cardiomyopathy (TC), also known as stress cardiomyopathy, is commonly recognized as transient left ventricular dysfunction that may mimic acute coronary syndrome but is without angiographic evidence of obstructive coronary artery disease.1 TC has been increasingly associated with pre-existing psychiatric illness. Higher burden of pre-existing psychiatric comorbidity has been identified in patients with TC compared to healthy controls and patients with a history of myocardial infarction or chronic heart failure.2,3 Nevertheless, there is no strong consensus on the true spectrum of psychiatric illness in TC or the association of individual psychiatric diagnoses with this disorder. A number of studies have indicated that anxiety, but not mood disorders, may be associated with a higher risk of TC.4,5
Additionally, little remains known about any association of pre-existing psychiatric disease with clinical outcomes. We sought to assess the prognostic significance of pre-existing psychiatric illness for survival and recurrent cardiomyopathy after an index diagnosis of TC.
METHODS
Population and Study Design
After obtaining Institutional Review Board approval, we performed a retrospective observational study of all adult patients diagnosed with TC at Vanderbilt University Medical Center between 1999 and 2015. TC was defined using the following Mayo Clinic Criteria: transient abnormality in left ventricle wall motion beyond the perfusion territory of a single epicardial coronary artery, absence of obstructive coronary artery disease or angiographic evidence of acute plaque rupture, presence of new electrocardiographic abnormalities or elevation in cardiac bio-markers, and the absence of pheochromocytoma or myocarditis.1
Demographic and clinical data were collected by manual review of the electronic health record (EHR). Problematic alcohol use was defined as current consumption of more than 2 alcoholic drinks per day, self-report of current alcohol abuse, or a positive answer to a CAGE question at the time of index diagnosis. Overall burden of medical comorbidity was estimated using the Charlson comorbidity index.6 The clinical context for each TC case was reviewed to distinguish among physical, emotional, and unidentified stressors. The presence of chest pain, shortness of breath, and syncope/presyncope was recorded when present at the time of TC presentation. Pattern of wall motion abnormality was reviewed from echocardiography; midventricular, basal, and focal wall motion abnormality were defined as atypical variants of TC.
Pre-existing mood, anxiety, or schizophrenia-spectrum illness and use of psychotropic medications, including antidepressants, antipsychotics, and anxiolytics, at the time of TC presentation were identified by expert review of EHR. For subjects with sufficient documentation of psychiatric history, pre-existing medical record diagnoses were manually reviewed per Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition criteria.7 Antidepressants were classified as selective serotonin reuptake inhibitors, serotonin-norepinephrine reuptake inhibitors, and other antidepressant agents including monoamine oxidase inhibitors, tricyclic antidepressants, bupropion, and mirtazapine. Antipsychotics included typical and atypical antipsychotic agents. Categorized anxiolytic agents included benzodiazepines and buspirone.
Duration of follow-up was calculated as the time between index discharge and last clinical encounter with a health care provider. Mortality was assessed by review of the EHR and Social Security Death Index as of January 14, 2016. The designated outcomes of the study were 30-day mortality following index diagnosis in addition to overall mortality and recurrent TC as of last medical record review.
Statistical Analysis
Statistical analyses were performed using Stata Statistical Software: Release 14 (College Station, TX).8 Descriptive statistics are expressed as median with interquartile ranges for continuous variables and frequencies (percentages) for categorical variables. Univariate analyses were performed using the Pearson chi-squared test and Wilcoxon rank sum test for categorical and continuous variables, respectively. Death and recurrence after index discharge are depicted using Kaplan-Meier plots. Multivariable logistic regression was used to test for independent association of pre-existing psychiatric illness with 30-day mortality and recurrent TC. Association between pre-existing psychiatric illness and long-term mortality following index discharge was assessed using a multivariable Cox proportional hazard model. Covariates included in the models were age, Charlson comorbidity index score, and mode of cardiomyopathy trigger. Results are expressed as odds ratios and hazard ratios with 95% CI. All tests were two-tailed and a P ≤ 0.05 was considered statistically significant.
RESULTS
A total of 306 patients were diagnosed with TC during the study period. Baseline demographic and clinical features are depicted in Table 1. Further, 114 (37%) patients had a pre-existing mood, anxiety, or schizophrenia-spectrum illness at the time of index TC diagnosis, accounting for a total 151 diagnoses (Figure 1). A summary of psychotropic medication use among patients with pre-existing psychiatric illness is provided in Table 2.
TABLE 1.
Baseline Demographic and Clinical Features
| N | No psychiatric illness (N = 192) | Pre-existing psychiatric illness (N = 114) | P value | |
|---|---|---|---|---|
| Age (y) | 306 | 69 (57–75) | 60 (51–69) | <0.001* |
| Female (%) | 306 | 149 (78%) | 92 (81%) | 0.522† |
| Race (% white) | 306 | 161 (84%) | 99 (87%) | 0.480† |
| Insurance (% Medicaid) | 304 | 16 (8%) | 12 (11%) | 0.513† |
| Education (% with college degree) | 249 | 38 (25%) | 24 (25%) | 0.917† |
| Ongoing tobacco use (%) | 299 | 30 (16%) | 46 (41%) | <0.001† |
| Problematic alcohol use (%) | 299 | 18 (10%) | 15 (13%) | 0.336† |
| Charlson comorbidity index | 302 | 1 (0–3) | 2 (1–3) | 0.099* |
| Chest pain at presentation (%) | 272 | 85 (50%) | 48 (47%) | 0.639† |
| Shortness of breath at presentation (%) | 275 | 78 (46%) | 49 (47%) | 0.809† |
| Syncope or presyncope at presentation (%) | 276 | 20 (12%) | 13 (13%) | 0.793† |
| Physical trigger (%) | 306 | 115 (60%) | 82 (72%) | 0.034† |
| Atypical variant (%) | 306 | 26 (14%) | 21 (18%) | 0.252† |
| Duration of hospitalization (d) | 306 | 6 (3–12) | 6 (3–10) | 0.955* |
| Duration of follow-up (y) | 277 | 0.1 (0–1.6) | 0.2 (0–1.8) | 0.594* |
Data are presented as median (IQR) for continuous variables and number (percentage) of patients for categorical variables. N represents the number of patients with non-missing values. IQR = interquartile range.
Wilcoxon rank sum test.
Pearson chi-squared test.
FIGURE 1.
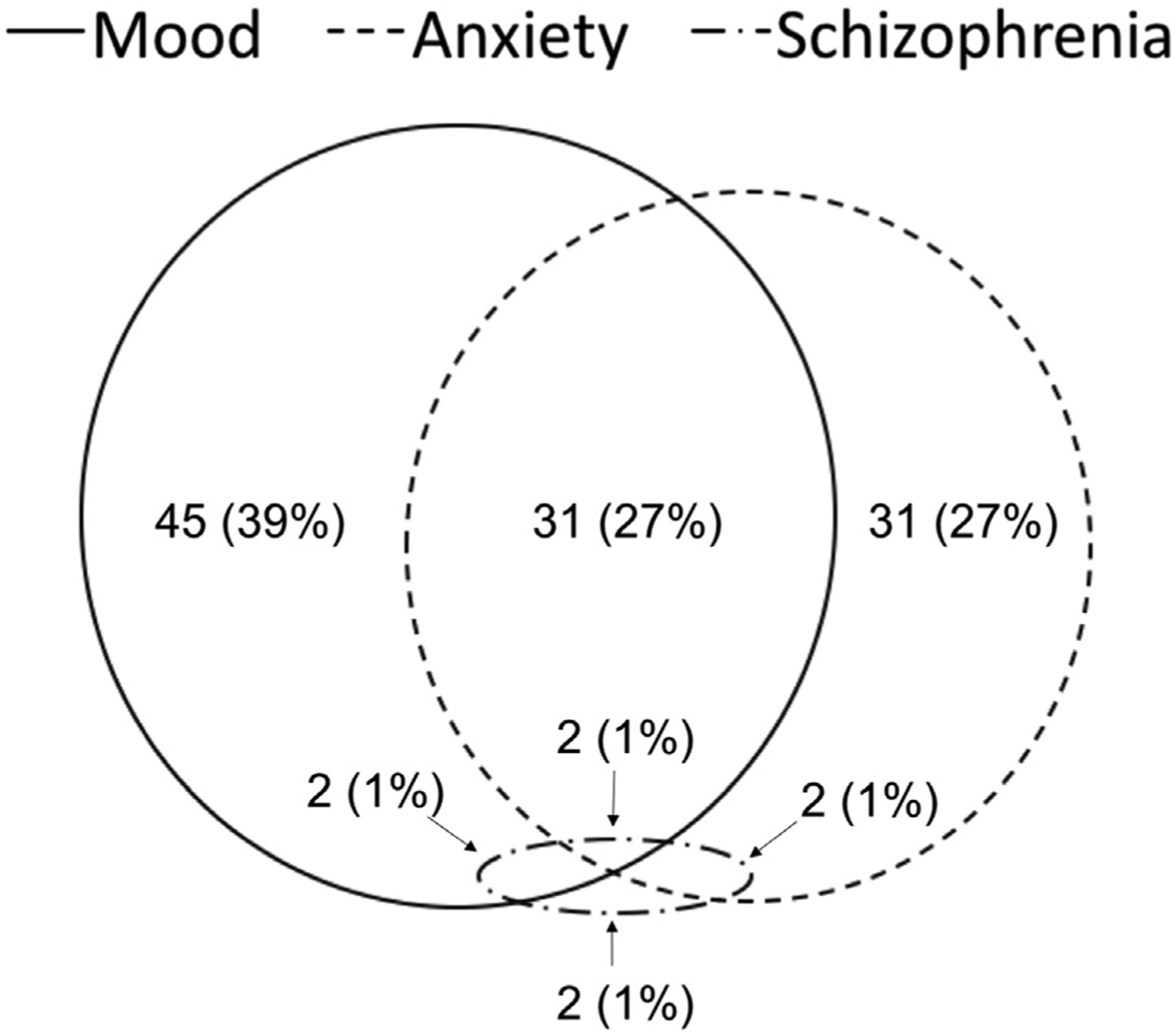
Spectrum of Psychiatric Illness in Takotsubo Cardiomyopathy. A Total of 114 Patients Accounted for a total of 151 Mood, Anxiety, and Schizophrenia-Spectrum Diagnoses.
TABLE 2.
Psychotropic Use Among 114 Patients With Pre-existing Psychiatric Illness
| Pharmacologic agent | Subjects (%) |
|---|---|
| Antidepressants | |
| SSRI | 46 (43%) |
| SNRI | 15 (14%) |
| Other | 17 (16%) |
| Antipsychotics | |
| Typical | 1 (1%) |
| Atypical | 14 (13%) |
| Anxiolytics | |
| Benzodiazepine | 46 (43%) |
| Buspirone | 3 (3%) |
SNRI = serotonin-norepinephrine reuptake inhibitor; SSRI = selective serotonin reuptake inhibitor.
In all, 43 (14%) and 88 (29%) patients died within 30 days of index diagnosis and as of last medical record review, respectively. Of the 269 patients who survived the index hospitalization, 19 (7%) had a confirmed recurrent episode of TC at a time interval ranging between 29 days and 15 years following initial diagnosis. Overall risk of TC recurrence was 5.8% per patient-year. Of the 19 patients with recurrent TC, 15 (79%) had pre-existing psychiatric illness (5 patients with mood-spectrum and anxiety-spectrum illness, respectively, in addition to 5 patients with concomitant mood-anxiety disorders). Risk of TC recurrence among patients without pre-existing psychiatric illness was 1.9% per patient-year compared to 11.4% per patient-year in patients with psychiatric comorbidity. Comparison of mortality and recurrent TC based on pre-existing psychiatric illness is provided in Figure 2.
FIGURE 2.
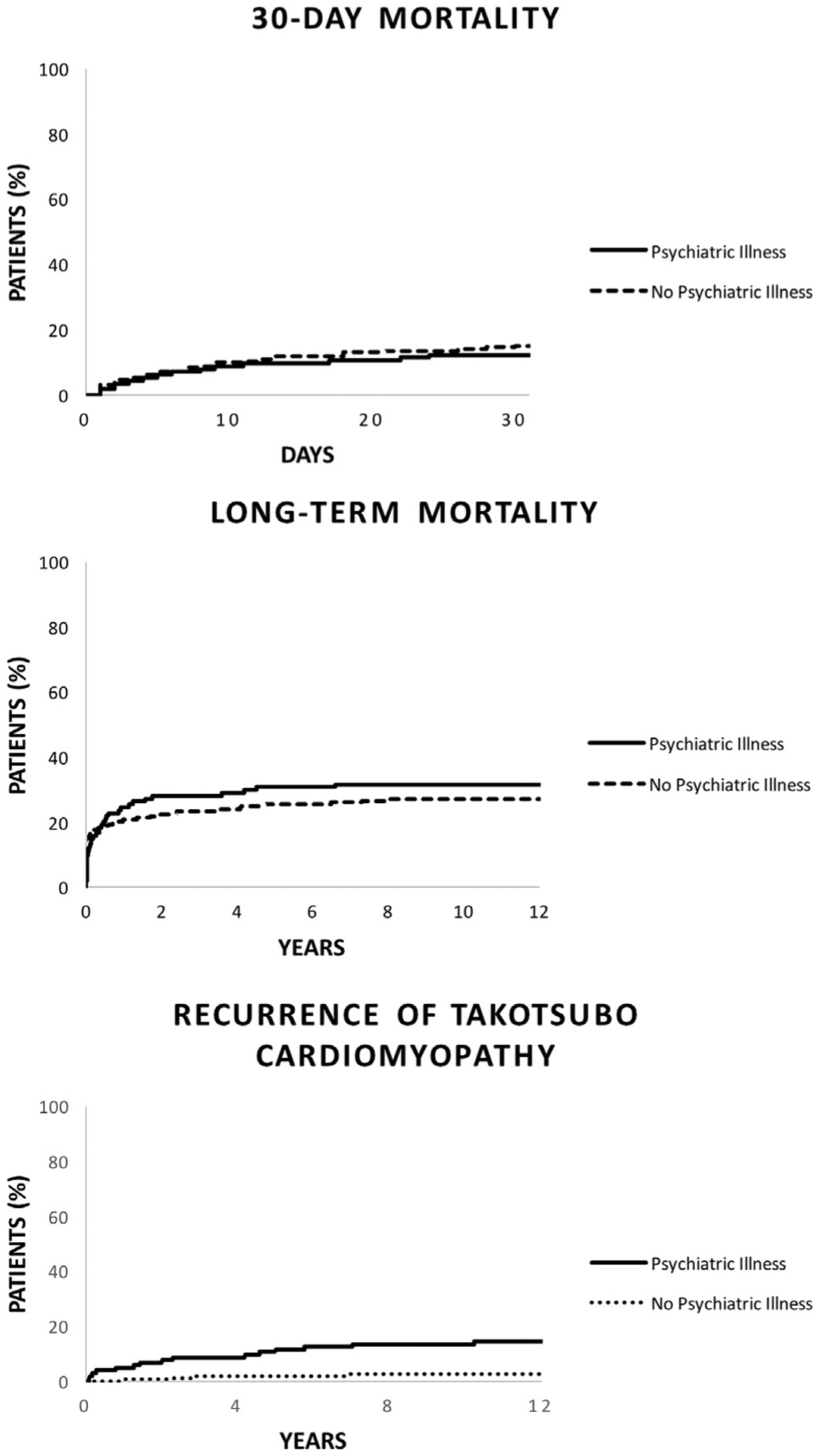
Kaplan-Meier Survival and Temporal Distribution of Recurrence in Patients Following Takotsubo Cardiomyopathy. Long-term Mortality Represents Cumulative Mortality from Index Diagnosis to the Date of Last Medical Record Review.
In multivariable logistic regression and Cox proportional hazard analysis, pre-existing psychiatric illness was not associated with increased 30-day (odds ratio = 0.69; 95% CI: 0.33–1.44; P = 0.320) or long-term (odds ratio = 0.89; 95% CI: 0.56–1.41; P = 0.621) mortality. In a similar analysis controlling for age, Charlson comorbidity index scores, and mode of cardiomyopathy trigger, pre-existing psychiatric illness was associated with higher risk of recurrent TC (odds ratio = 7.44; 95% CI: 2.30–24.01; P ≤ 0.001) (Table 3).
TABLE 3.
Adjusted Odds Ratios for 30-d Mortality and Cardiomyopathy Recurrence in Addition to Hazard Ratios for Long-Term Mortality Following Takotsubo Cardiomyopathy
| Characteristics | OR | 95% CI | P value |
|---|---|---|---|
| 30-d mortality | |||
| Age (y) | 1.00 | 0.98–1.03 | 0.604 |
| Charlson comorbidity index (CCI) | 1.21 | 1.05–1.40 | 0.010 |
| Physical stress as takotsubo trigger | 7.55 | 2.21–25.71 | <0.001 |
| Pre-existing psychiatric illness | 0.69 | 0.33–1.44 | 0.320 |
| HR | 95% CI | P value | |
| Long-term mortality | |||
| Age (y) | 0.99 | 0.97–1.01 | 0.186 |
| Charlson comorbidity index (CCI) | 1.14 | 1.02–1.26 | 0.016 |
| Physical stress as takotsubo trigger | 1.59 | 0.76–3.32 | 0.213 |
| Pre-existing psychiatric illness | 0.89 | 0.56–1.41 | 0.621 |
| OR | 95% CI | P value | |
| Recurrent takotsubo cardiomyopathy | |||
| Age (y) | 1.00 | 0.96–1.04 | 0.897 |
| Charlson comorbidity index (CCI) | 1.01 | 0.76–1.34 | 0.968 |
| Physical stress as takotsubo trigger | 0.51 | 0.18–1.42 | 0.196 |
| Pre-existing psychiatric illness | 7.44 | 2.30–24.01 | < 0.001 |
HR = hazard ratio; OR = odds ratio.
DISCUSSION
The primary findings of this study are that pre-existing psychiatric illness (particularly mood and anxiety-spectrum) in TC is common, is not associated with short-term or long-term survival, but does predict increased risk of TC recurrence.
There are scant data on predictors of recurrent TC, and, to our knowledge, this is the first study identifying the prognostic significance of pre-existing psychiatric illness. Although this finding requires confirmation in larger scale or prospective studies, it suggests that pre-existing psychiatric illness may be useful to stratify patients in regard to the risk of TC recurrence. Given an estimated 10% risk of cardiogenic shock and 4% risk of inpatient death with each presentation of TC,2 proper risk stratification may lead to more individualized prognostication and guide research into potential interventions aimed at reducing long-term morbidity and mortality in this patient population.
The appropriate management of psychiatric illness in TC is unclear. Insufficient statistical power precluded the study of an association between psychotropic use and TC recurrence. We chose to summarize the use of some common psychotropic agents among our patient population for descriptive purposes. Overall, there is no evidence to suggest that psychiatric illness in TC should be managed any differently than in the absence of this disorder. However, there are multiple reports of psychotropic agent withdrawal or overdose in addition to electroconvulsive therapy triggering TC in patients with psychiatric illness.9–11 Careful management of psychotropic medications and understanding that cardiomyopathy may be triggered by electroconvulsive therapy is likely appropriate in the care of patients with ongoing psychiatric illness and a history of TC.
In addition to assessing the prognostic significance of psychiatric illness in TC, we attempted to evaluate potential demographic and clinical differences based on pre-existing psychiatric pathology. In univariate analyses, no significant difference was noted among the most common presenting symptoms of TC. Patients with pre-existing psychiatric illness were on average younger at the time of TC diagnosis, used tobacco in higher rates, and were more likely to present with TC triggered by a physical stressor. Younger age at index diagnosis of TC among patients with psychiatric illness could further support the association of psychiatric pathology with increased risk of TC. Relatively increased proportion of cases triggered by physical stressors may also support an inherent predisposition of patients with psychiatric illness toward TC even in the absence of acute emotional stressors.
Despite an increasing number of studies evaluating psychiatric illness in TC, overall knowledge and clinical application remains limited.12,13 The relative rarity of TC poses a significant challenge to most research endeavors and is a large reason why several distinct mood, anxiety, and schizophrenia-spectrum diagnoses are often grouped together. In a number of relatively smaller studies, only anxiety-spectrum disorders were associated with increased risk of TC.4,5 Larger-scale studies may help to better differentiate the association of different psychiatric illnesses with the occurrence of TC in addition to long-term prognosis. Regarding long-term management of psychiatric illness in patients with a history of TC, there is a great need for prospective studies that evaluate the role of pharmacological or behavioral therapy in potentially reducing the risk of recurrent cardiomyopathy.
Study Limitations
This study should be interpreted in the context of its limitations. The retrospective cohort design only allows for identification of association and cannot infer causation. Moreover, the size of our cohort limits statistical power to detect associations and constrains the number of covariates included in the multivariable analyses. Ongoing tobacco use, although associated with pre-existing psychiatric illness in univariate analyses, was not included in the multivariable analyses for recurrence or survival. This study is likely underpowered to detect a smaller association between psychiatric illness and long-term survival. Insufficient statistical power also limits the ability to analyze different psychiatric illnesses individually. There are potential biases related to follow-up duration, limitations of the EHR and Social Security Death Index in defining the cause of death, and incomplete ascertainment of pre-existing psychiatric illnesses or use of psychotropic medications at index diagnosis. In particular, most psychiatric diagnoses were obtained from review of medical history listings, and appropriate confirmation of Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition criteria was not feasible for all patients. We acknowledge that this may have led to the underdiagnosis or misdiagnosis of psychiatric illness in the cohort.
CONCLUSIONS
In this single institution cohort, pre-existing psychiatric illness was associated with an increased risk of recurrent TC. No significant association was noted between pre-existing psychiatric illness and survival. The prognostic significance of specific psychiatric disorders in TC and their appropriate management is unclear. There is a great need for larger scale and prospective studies that evaluate prognostic indicators and long-term management strategies in patients with comorbid psychiatric illness and TC.
FUNDING RESOURCES
The project was supported by AHA 13FTF16810038, CTSA Award no. UL1TR000445 from the National Center for Advancing Translational Sciences. No relationship with industry exists.
Footnotes
Disclosures: Vanderbilt Translational and Clinical Cardiovascular Research Center (V-TRACC). The Vanderbilt System for EHR-based Research in Cardiovascular Health (V-SERCH).
References
- 1.Prasad A, Lerman A, Rihal CS: Apical ballooning syndrome (Tako-Tsubo or stress cardiomyopathy): a mimic of acute myocardial infarction. Am Heart J 2008; 155(3): 408–417 [DOI] [PubMed] [Google Scholar]
- 2.Templin C, Ghadri JR, Diekmann J, et al. : Clinical features and outcomes of takotsubo (stress) cardiomyopathy. N Engl J Med 2015; 373(10):929–938 [DOI] [PubMed] [Google Scholar]
- 3.El-sayed AM, Brinjikji W, Salka S: Demographic and comorbid predictors of stress (takotsubo) cardiomyopathy. Am J Cardiol 2012; 110(9):1368–1372 [DOI] [PubMed] [Google Scholar]
- 4.Salmoirago-Blotcher E, Rosman L, Wittstein IS, et al. : Psychiatric history, post-discharge distress, and personality characteristics among incident female cases of takotsubo cardiomyopathy: a case-control study. Heart Lung. 2016; 45(6):503–509 [DOI] [PubMed] [Google Scholar]
- 5.Goh AC, Wong S, Zaroff JG, Shafaee N, Lundstrom RJ: Comparing anxiety and depression in patients with takotsubo stress cardiomyopathy to those with acute coronary syndrome. J Cardiopulm Rehabil Prev 2016; 36(2): 106–111 [DOI] [PubMed] [Google Scholar]
- 6.Charlson ME, Pompei P, Ales KL, Mackenzie CR: A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40(5):373–383 [DOI] [PubMed] [Google Scholar]
- 7.American Psychiatric Press Inc. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition Text Revised: American Psychiatric Association; Washington DC, 2000 [Google Scholar]
- 8.StataCorp: Stata Statistical Software: Release 14. College Station, TX: StataCorp LP; 2015 [Google Scholar]
- 9.Marabotti C, Venturini E, Marabotti A, Pingitore A: Delayed multifocal recurrent stress-induced cardiomyopathy after antidepressants withdrawal. Heart Lung 2014; 43(3): 225–230 [DOI] [PubMed] [Google Scholar]
- 10.Christoph M, Ebner B, Stolte D, et al. : Broken heart syndrome: tako tsubo cardiomyopathy associated with an overdose of the serotonin-norepinephrine reuptake inhibitor venlafaxine. Eur Neuropsychopharmacol 2010; 20(8): 594–597 [DOI] [PubMed] [Google Scholar]
- 11.Narayanan A, Russell MD, Sundararaman S, Shankar KK, Artman B: Takotsubo cardiomyopathy following electroconvulsive therapy: an increasingly recognised phenomenon. BMJ Case Rep 2014. [pii: bcr2014206816] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Compare A, Grossi E, Bigi R, et al. : Stress-induced cardiomyopathy and psychological wellbeing 1 year after an acute event. J Clin Psychol Med Settings 2014; 21(1): 81–91 [DOI] [PubMed] [Google Scholar]
- 13.Dias A, Franco E, Figueredo VM, Hebert K, Quevedo HC: Occurrence of takotsubo cardiomyopathy and use of antidepressants. Int J Cardiol 2014; 174(2):433–436 [DOI] [PubMed] [Google Scholar]


