Abstract
Background
Myoglobin clearance in acute kidney injury requiring renal replacement therapy is important because myoglobin has direct renal toxic effects. Clinical data comparing different modalities of renal replacement therapy addressing myoglobin clearance are limited. This study aimed to compare two renal replacement modalities regarding myoglobin clearance.
Methods
In this prospective, randomized, single-blinded, single-center trial, 70 critically ill patients requiring renal replacement therapy were randomized 1:1 into an intervention arm using continuous veno-venous hemodialysis with high cutoff dialyzer and a control arm using continuous veno-venous hemodiafiltration postdilution with high-flux dialyzer. Regional citrate anticoagulation was used in both groups to maintain the extracorporeal circuit. The concentrations of myoglobin, urea, creatinine, β2-microglobulin, interleukin-6 and albumin were measured before and after the dialyzer at 1 h, 6 h, 12 h, 24 h and 48 h after initiating continuous renal replacement therapy.
Results
Thirty-three patients were allocated to the control arm (CVVHDF with high-flux dialyzer) and 35 patients to the intervention arm (CVVHD with high cutoff dialyzer). Myoglobin clearance, as a primary endpoint, was significantly better in the intervention arm than in the control arm throughout the whole study period. The clearance values for urea and creatinine were higher in the control arm. There was no measurable albumin clearance in both arms. The clearance data for β2-microglobulin and interleukin-6 were non-inferior in the intervention arm compared to those for the control arm. Dialyzer lifespan was 57.0 [38.0, 72.0] hours in the control arm and 70.0 [56.75, 72.0] hours in the intervention arm (p = 0.029).
Conclusions
Myoglobin clearance using continuous veno-venous hemodialysis with high cutoff dialyzer and regional citrate anticoagulation is better than that with continuous veno-venous hemodiafiltration with regional citrate anticoagulation.
Trial registration
German Clinical Trials Registry (DRKS00012407); date of registration 23/05/2017. https://www.drks.de/drks_web/navigate.do?navigationId=trial.HTML&TRIAL_ID=DRKS00012407.
Keywords: Myoglobin clearance, Rhabdomyolysis, Acute kidney injury, High cutoff dialyzer, Renal replacement therapy, EMiC2
Background
Acute kidney injury (AKI) is one of the leading organ dysfunctions in critically ill patients. According to the multinational acute kidney injury–epidemiologic prospective investigation (AKI-EPI) study, more than half of critical care patients suffer from AKI and this is associated with high mortality rates, particularly if renal replacement therapy (RRT) is required [1–3].
Several pathogenetic mechanisms are involved in the development of AKI in critically ill patients. Hemodynamic alterations or inflammation-related stress may trigger renal damage [4].
One precisely defined cause of AKI is rhabdomyolysis, characterized by damage of skeletal muscles and the leakage of muscle cell contents into the circulation, e.g., myoglobin and other proteins [5]. Up to 7–10% of AKI is attributed to rhabdomyolysis [6]. The reported incidence of AKI in patients with rhabdomyolysis is 13–46% [7], and RRT may be necessary in these patients.
Continuous renal replacement therapy (CRRT) may be favorable in these critical ill patients, since it enables gentle removal of solutes and control of fluid balance. However, it is not yet clear if continuous or intermittent hemodialysis would be the best regarding clinical outcome [8–10].
Current international guidelines recommend anticoagulation with citrate for CRRT, unless systemic anticoagulation is required for other indications or citrate use is contraindicated [11]. Regional citrate anticoagulation (RCA) is associated with less bleeding complications, longer lifespan of the dialyzer and lower incidence of heparin-induced thrombocytopenia (HIT) than systemic anticoagulation [12, 13].
Convection-based RRT techniques such as continuous veno-venous hemofiltration (CVVH) require higher extracorporeal circuit blood flow than diffusion-based ones, which is related to hemoconcentration at the dialyzer. Therefore, RCA during CVVH is hardly possible due to the high risk of citrate accumulation.
Continuous veno-venous hemodialysis (CVVHD) enables reducing citrate load [14], so that this mode using RCA is favorable in critically ill patients. One disadvantage of diffusive techniques is the poor clearance of molecules with middle molecular weight [15]. Continuous veno-venous hemodiafiltration (CVVHDF) is one opportunity to realize a low blood flow with consecutive lower citrate load and maintain middle molecule clearance.
Another solution for this problem could be the application of high cutoff (HCO) membranes with a pore size larger than 0.01 μm in CVVHD (CVVHD-HCO) [16]. It has already been shown that CVVHD using a high cutoff dialyzer is superior than that using a conventional high-flux dialyzer regarding the clearance of β2-microglobulin, a molecule with a middle molecular weight [17]. The application of HCO dialyzers in CVVHDF is not recommended, because it leads to albumin leakage, particularly with postdilution hemodiafiltration [18, 19].
Based on this finding, we have designed a prospective, randomized controlled trial to evaluate the myoglobin clearance with CVVHDF compared to that with CVVHD-HCO using RCA. Clearance of myoglobin is important due to its direct toxic effects. Clinical data comparing different modalities of CRRT addressing myoglobin clearance are lacking.
Methods
Study design
The present study is a prospective, randomized, single-blinded, single-center trial. It was approved by the local ethics committee, conducted in accordance with the German medical product law and registered at the German Clinical Trials Registry (DRKS00012407).
We enrolled patients from May 2017 to September 2018 in our 28-bed medical intensive care unit (ICU) at the University Hospital Leipzig. Informed consent was either given by the patients or their legal guardians. Allocation concealment and unrestricted randomization was carried out using sequentially numbered, opaque sealed envelopes as previously described [20]. In detail, a sheet of standard-sized paper marked with the treatment arm was folded to fit an envelope, with 35 each marked for treatment arms A and B. To prevent attempts to decipher the allocation sequence, one sheet of carbon paper was put on top of this paper and wrapped with aluminum foil. This was then inserted in an opaque envelope and sealed. The 70 sealed envelopes were then thoroughly mixed and marked with unique numbers, and then kept in a container [20]. For technical reasons, only patients were blinded to the treatment arm.
Patients
During the study period, 430 patients with acute renal failure and indication for RRT (based on the recommendations of the kidney disease, improving global outcomes (KDIGO)) [11] were admitted to the ICU and were screened for eligibility. Exclusion criteria were need for systemic anticoagulation for other reasons, high risk for citrate accumulation (e.g., liver failure), pregnancy and lactation, age < 18 years, rejection of renal replacement therapy, refusal to participate in the study, high risk to die during the first 48 h after admission and end-stage underlying disease.
We planned to show non-inferiority in myoglobin clearance as the primary end-point in the intervention arm compared to the control arm. Based on previous trials, a difference in myoglobin clearance of not more than 1.85 ml/min between the two treatment arms was considered to show non-inferiority of the intervention arm [17, 21]. Based on that, the inclusion of 66 patients was calculated to be required with a two-tailed power of 90% and p of < 0.05. Our study protocol allowed testing for superiority after demonstration of non-inferiority of the intervention arm [22].
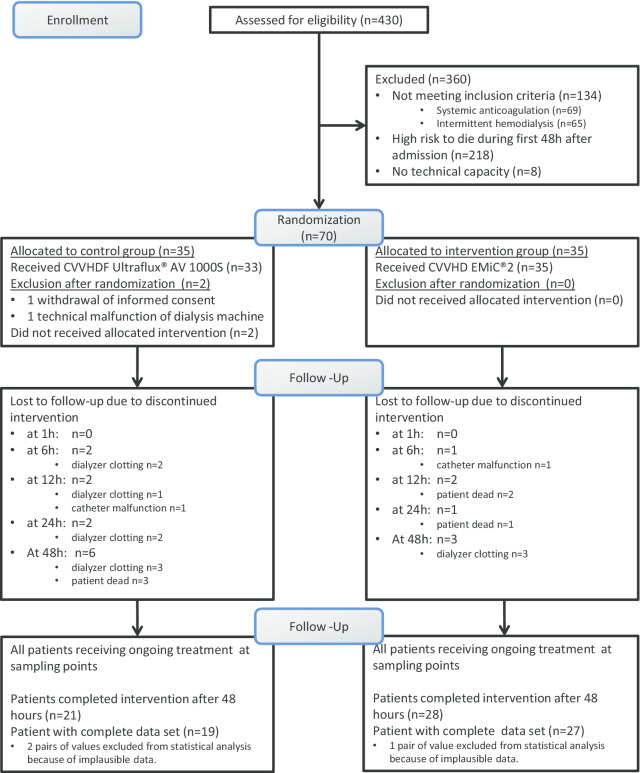
A total of 70 patients underwent randomization 1:1 into the intervention and control arms. We later excluded two patients, one due to withdrawal of informed consent and another patient because of technical malfunction of the dialysis machine. Three pairs of values were excluded from statistical analysis because of implausible data, presumably related to preanalytical errors. Recruitment flowchart is displayed in Fig. 1.
Fig. 1.
Recruitment flowchart. CVVHDF continuous veno-venous hemodiafiltration, CVVHD continuous veno-venous hemodialysis, AV1000S type of high-flux dialyzer, EMiC2 type of high cut-off dialyzer
Data collection
Demographic and clinical data were collected in all patients. Baseline criteria were recorded at time of initiating RRT (renal function, admission diagnosis, indication for renal replacement therapy, acute physiology and chronic health evaluation II (APACHE II), sequential organ failure assessment (SOFA), simplified acute physiology score II (SAPS II), mean arterial blood pressure, need for mechanical ventilation, need for vasopressor, sepsis, concomitant medication and pre-existing diseases). Laboratory and clinical data during the intervention were daily collected (urea, creatinine, sodium, potassium, chloride, phosphate, calcium, magnesium, hemoglobin, hematocrit, platelet count, white blood cell count, albumin, pH, bicarbonate, base excess, lactate, mean arterial pressure, heart rate and oxygen saturation).
Clinical follow-up data (ICU mortality, length of ICU stay, 28-day mortality and 90-day mortality) were extracted from patient records.
Treatment-related adverse events (AE) (hypocalcemia, alkalosis, citrate accumulation, catheter malfunction) and severe adverse events (SAE) (treatment associated life-threatening complication and death from any cause during intervention period) were monitored.
Procedure
A central venous access using a 13 French double-lumen high-flow catheter (Achim Schulz-Lauterbach VMP, Iserlohn, Germany) was placed. The control arm was managed with CVVHDF postdilution using the high-flux dialyzer Ultraflux AV1000S (Fresenius Medical Care, Bad Homburg, Germany), while the intervention arm was managed with CVVHD using the high cutoff dialyzer Ultraflux EMiC2 (Fresenius Medical Care, Bad Homburg, Germany). Both dialyzers have the same effective surface area (1.8 m2), consist of identical material (polysulfone) and exhibit a similar wall thickness (35 µm). The only difference between the applicated dialyzers is the pore size, which is 30 kilodaltons (kDa) for the high-flux and 45 kDa for the high cutoff dialyzer.
The dialysis machine used in both arms was multiFiltrate® (Fresenius Medical Care, Bad Homburg, Germany). A bicarbonate-buffered dialysate (CiCa® dialysate K4 or K2, Fresenius medical care, Bad Homburg, Germany) and replacement fluid (multiBic® K4 or K2, Fresenius medical care, Bad Homburg, Germany) were used. Anticoagulation of the extracorporeal circuit was maintained with regional citrate anticoagulation in both arms. Regional anticoagulation of the extracorporeal circuit was monitored by measuring ionized postfilter calcium and guided by citrate supply (citrate: 136 mmol/l). An ionized postfilter calcium of 0.20–0.29 mmol/l for CVVHDF and 0.25–0.34 mmol/l for CVVHD was targeted. At the start of treatment, citrate flow was set at 5.0 mmol citrate/l blood for CVVHDF and 4.0 mmol citrate/l blood for CVVHD. To keep systemic ionized calcium stable between 1.12 and 1.20 mmol/l, a calcium chloride solution (calcium: 83 mmol/l) was added to the extracorporeal circuit near the backflow to the patient. Both groups started with a flow of 1.7 mmol Ca2+/l dialysate.
The total turnover rate (TTR) (dialysate and replacement fluid) rate was calculated at 25 ml/kg ideal or adjusted body weight/h [23]. Ideal body weight was calculated using the Hamwi equation (for males: 48 kg for the first 152 cm + 1.1 kg for each additional cm; for females 45 kg for the first 152 cm + 0.9 kg for each additional cm). If the quotient of actual body weight divided by ideal body weight was more than 1.3 [24], the adjusted body weight was used for calculation of dialysate flow (for males: (actual body weight-ideal body weight) * 0.38 + ideal body weight; for females: (actual body weight-ideal body weight) * 0.32 + ideal body weight) [25].
The ratio of dialysate flow to replacement fluid in CVVHDF was 2:1, and blood flow (QB) was threefold of the dialysate flow in both arms as specified by the manufacturer. According to the statement of the manufacturer, the maximum dialyzer lifespan was limited to 72 h.
Endpoints and calculations
The concentrations of myoglobin (17,053 Dalton (Da), urea (60 Da), creatinine (113 Da), β2-microglobulin (11,800 Da), interleukin 6 (IL-6, 26,000 Da) and albumin (66,470 Da) were measured before (Cpre) and after (Cpost) the dialyzer 1, 6, 12, 24 and 48 h after initiating CRRT.
To avoid additional effect of hemoconcentration at the dialyzer, ultrafiltration was set at zero ten minutes before drawing samples for laboratory analysis.
Plasma flow in the extracorporeal circuit (Qppre) was calculated using blood flow (Qb) of extracorporeal circuit and patient's hematocrit level (hct) at the time of sampling:
The substance-specific plasma clearance (Clp) was calculated at the sampling time points:
The primary outcome parameter was plasma clearance of myoglobin after 1 h, 6 h, 12 h, 24 h and 48 h. Secondary outcome parameters were plasma clearances of urea, creatinine, β2-microglobulin, interleukin 6 and albumin at the same time points.
Equality of plasma clearance (Clp.corr.) in both study groups relating to different TTR was tested using the following formula:
In CVVHDF (control arm), a sampling port was available only before instead of after the replacement fluid flows into the extracorporeal circuit. Therefore, the postfilter solute concentration (Cpost) had to be corrected to account for replacement fluid flow.
For this purpose, postfilter plasma flow (Qppost) was calculated subtracting filtration portion (FP; ml/min) from prefilter plasma flow (Qppre):
The solute-specific concentration at the end of the extracorporeal circuit (Cpost.corr.) was adjusted using the ratio of plasma flow pre- and postfilter (Qppost/Qppre):
Laboratory analysis
Laboratory analyses were performed using Cobas 8000 (Roche, Mannheim, Germany) according to the manufacturer´s instructions, immediately after sampling.
The following methods were used:
Urea: kinetic test with urease and glutamate dehydrogenase.
Creatinine: enzymatic method with creatinase.
β2-microglobulin: am c701 immunological test for turbidity.
Myoglobin: ElektroChemiLumineszenzImmunoAssay (ECLIA).
IL-6: ECLIA.
Human albumin: color test with bromocresol green.
Statistical analysis
We planned the trial as a non-inferiority trial keeping in mind to present the results in terms of superiority if the effect is large enough. Sample size was calculated cautiously for a non-inferiority study. We assumed a mean of 11.1 for the intervention arm and 7.4 for the control arm, with a standard deviation of 6.75 for myoglobin clearance from pilot data and a significance level α = 5%. The non-inferiority margin was chosen a sixth of standard deviation, which is 1.85 ml/min. The study was planned to show non-inferiority in values of myoglobin clearance with 90% power. A sample size of 66 was calculated using the software PASS 2008 for non-inferiority. Taking 5% dropouts into account, this results in a sample size N = 70. The study was not powered to show differences in the other substance specific clearances.
Continuous variables are given as mean with standard deviation or median with 25th and 75th quantile in square brackets based on test for normal distribution using the Shapiro–Wilk test. Categorical variables are displayed as n (%). Normally distributed variables were analyzed by the Student’s t test. Not normally distributed variables were assessed by the Mann–Whitney U test. Categorical variables were tested by Chi-square (two-sided), reported as frequencies and percentages. Measures of clearance are repeated measurements from the same patients and thus are correlated. Therefore, we fitted general linear models with repeated measurements. Differences between the arms were calculated at each time point with 95% confidence interval (CI). Marginal means were compared and the difference was calculated with 95% CI as effect measure. A test of non-inferiority was performed with these confidence intervals.
The Kaplan–Meier method was applied to calculate and depict the survival function of the dialyzer lifetime.
Statistical analysis was performed using IBM SPSS, versions 24 to 26 (Minneapolis, USA). R (R Core Team, Vienna) was applied for the generation of graphs. The significance level was defined 5% for two-tailed tests.
Results
Baseline criteria
Serum creatinine concentration was significantly higher in the control arm. There were no differences regarding other baseline variables between both study arms (Table 1).
Table 1.
Baseline characteristics of the study population
| Variable | Control arm CVVHDF, n = 33 | Intervention arm CVVHD-HCO, n = 35 | p value |
|---|---|---|---|
| Age, years | 67 [51,74.5] | 68 [57,74.0] | 0.626 |
| Males | 26 (78.8%) | 18 (51.4%) | 0.180 |
| Actual body weight, kg | 80 [72,100] | 80 [70,90] | 0.341 |
| Height, cm | 174.70 ± 10.58 | 170.83 ± 9.16 | 0.113 |
| BMI | 26 [24, 30] | 27 [24, 30] | 0.873 |
| APACHE II score | 29.27 ± 7.27 | 29.60 ± 8.11 | 0.861 |
| SOFA score | 9.15 ± 3.57 | 10.09 ± 3.88 | 0.305 |
| SAPS II score | 56.27 ± 14.29 | 57.43 ± 14.63 | 0.743 |
| Creatinine (µmol/l) | 240 [170,413] | 188 [129,266] | 0.031 |
| Urea (mmol/l) | 19.90 ± 8.80 | 19.14 ± 8.99 | 0.728 |
| urine output during first 24 h (ml) | 530 ± 752 | 518 ± 602 | 0.941 |
| Admission diagnosis | |||
| Sepsis | 9 (27.3%) | 11 (31.4%) | |
| Pneumonia | 3 (9.1%) | 3 (8.6%) | |
| ARDS | 3 (9.1%) | 4 (11.4%) | |
| AKI | 2 (6.1%) | 3 (8.6%) | |
| Hemorrhage | 4 (12.1%) | 1 (2.9%) | |
| Cardiac | 4 (12.1%) | 5 (14.3%) | |
| Rhabdomyolysis | 2 (6.1%) | 0 (0%) | |
| Pancreatitis | 1 (3.0%) | 2 (5.7%) | |
| Liver failure | 1 (3.0%) | 5 (14.3%) | |
| Other | 4 (12.1%) | 1 (2.9%) | |
| Systolic BP, mmHg | 108.33 ± 20.94 | 108.29 ± 20,04 | 0.992 |
| MAP mmHg | 70 [62,78.5] | 72 [63,80] | 0.961 |
| Mechanical ventilation | 24 (72.7%) | 33 (94.3%) | 0.16 |
| Vasopressor | 23 (69.7%) | 32 (91.4%) | 0.23 |
| Pre-existing diseases | |||
| Congestive heart failure NYHA IV | 6 (18.2%) | 8 (22.9%) | 0.634 |
| Pre-existing immunosuppression | 9 (27.3%) | 17 (48.6%) | 0.71 |
| Liver cirrhosis | 7 (21.2%) | 10 (28.6%) | 0.484 |
| History of malignancy | 7 (21.2%) | 11 (31.4%) | 0.34 |
| Chronic pulmonary disease | 3 (9.1%) | 8 (22.9%) | 0.123 |
| Indication for RRT | |||
| Metabolic acidosis | 5 (15.2%) | 12 (34.3%) | 0.069 |
| Pulmonary edema | 12 (36.4%) | 15 (42.9%) | 0.584 |
| Hyperpotassemia | 8 (24.2%) | 7 (20%) | 0.673 |
| Anuria (< 100 ml/d) | 26 (78.8%) | 25 (71.4%) | 0.484 |
| Uremia | 20 (60%) | 13 (37.1%) | 0.53 |
| Main reason for AKI | |||
| Septic | 13 (39.4%) | 19 (54.3%) | |
| Postrenal | 0 (0%) | 0 (0%) | |
| Cardiorenal | 4 (12.1%) | 5 (14.3%) | |
| Toxic | 3 (9.1%) | 0 (0%) | |
| Hypovolemia | 6 (18.2%) | 3 (8.6%) | |
| Rhabdomyolysis | 3 (9.1%) | 0 (0%) | |
| Hepatorenal | 2 (6.1%) | 5 (14.3%) | |
| Other | 2 (6.1%) | 3 (8.6%) |
Data presented as n (%), mean ± standard deviation or median [25th, 75th quantile]
BMI body mass index, APACHE II acute physiology and chronic health evaluation II, SOFA sequential organ failure assessment, SAPS II simplified acute physiology score II, ARDS Acute Respiratory Distress Syndrome, AKI acute kidney injury, BP blood pressure, MAP mean arterial blood pressure, RRT renal replacement therapy, CVVHDF continuous veno-venous hemodiafiltration, CVVHD-HCO continuous veno-venous hemodialysis using high cutoff filter
Blood flow effectively obtained in both treatment arms was equal (after 1 h: control arm: 86.4 ± 23 ml/min; intervention arm: 91.7 ± 18 ml/min; p = 0.3). TTR in the control arm was higher (after 1 h: control arm: 2116 ± 328 ml/h; intervention arm: 1821 ± 351 ml/h; p = 0.001). Data are displayed in an additional file (see Additional file 1).
Primary endpoint
The 95% confidence intervals for the difference of myoglobin clearance were at the pre-specified margin − 1.85 for non-inferiority at all time points. Indeed, these confidence intervals are right from zero indicating a significant advantage of the intervention versus control arm (Fig. 2). This is reflected by a significant comparison of the marginal means (p < 0.0005, Table 2) too. Myoglobin clearance was higher in the intervention arm than in the control arm at every time point (Fig. 3).
Fig. 2.

Non-inferiority of myoglobin clearance. The mean arm differences with 95% confidence intervals at 1, 6, 12, 24, 48 h. The null hypothesis Δ = 0 (no arm difference) was tested against the alternative hypothesis Δ > −1.85 ml/min (margin of non inferiority), depicted by the dashed red line
Table 2.
Substance specific clearances (ml/min) (primary and secondary endpoints)
| End-points | Time after starting treatment | n | Control arm CVVHDF† | Intervention arm CVVHD-HCO† | Mean difference‡ | p value# |
|---|---|---|---|---|---|---|
| Myoglobin | 1 h | 66 | 3.7 [2.3, 4.7] | 12.3 [10.1, 14.4] | 5.5 (4.0–7.0) | < 0.0005 |
| 6 h | 65 | 3.4 [1.6, 3.9] | 10 [8.3, 12.7] | |||
| 12 h | 62 | 2.3 [1.5, 4] | 8.3 [6.7, 10.7] | |||
| 24 h | 57 | 1.9 [0.2, 3.1] | 8.2 [6.8, 10.3] | |||
| 48 h | 48 | 2.1 [0.1, 5.5] | 6.9 [5.1, 8.8] | |||
| Urea | 1 h | 66 | 28.7 [25.6, 33.2] | 24.8 [20.9, 28.7] | − 5.3 (− 8.4− (− 2.3)) | 0.001 |
| 6 h | 65 | 29.6 [25, 31.4] | 25.1 [22.8, 28.3] | |||
| 12 h | 62 | 28.8 [25.2, 32.9] | 26.1 [19.8, 28.8] | |||
| 24 h | 57 | 28.6 [25.8, 32.4] | 26.7 [20.9, 29.7] | |||
| 48 h | 48 | 31 [26.2, 32.8] | 23 [20.4, 30.9] | |||
| Creatinine | 1 h | 66 | 31.4 [27.6, 35.9] | 28.5 [24.7, 34.1] | 4.2 (0.8–7.6) | 0.015 |
| 6 h | 65 | 31.7 [27.2, 34.5] | 29.5 [25.3, 34.9] | |||
| 12 h | 62 | 31.1 [27.8, 34.8] | 29.5 [22.5, 33] | |||
| 24 h | 58 | 31.5 [28, 37.1] | 30.4 [24.6, 35.9] | |||
| 48 h | 48 | 32,9 [27.5, 36.5] | 25.7 [23.7, 34.7] | |||
| β2− Microglobulin | 1 h | 66 | 21.1 [18, 23.8] | 24.5 [19.2, 28.1] | 4.4 (2.2–6.6) | < 0.0005 |
| 6 h | 65 | 19 [17.1, 22.4] | 24.1 [21,1, 26.6] | |||
| 12 h | 62 | 7.8 [4.5, 10.9] | 22.7 [18.2, 24.5] | |||
| 24 h | 57 | 16.4 [15.5, 19.4] | 22.1 [19.2, 25.8] | |||
| 48 h | 48 | 18 [15.5, 20.4] | 21.4 [16.9, 23.7] | |||
| Interleukin− 6 | 1 h | 66 | 0.2 [− 0.9, 1.2] | 5 [2.4, 5.9] | 1.4 (− 0.3–3.1) | 0.107 |
| 6 h | 65 | 0.3 [− 1, 2.5] | 2.5 [1, 3.5] | |||
| 12 h | 62 | 1.2 [0, 3.7] | 1.8 [0.6, 3.4] | |||
| 24 h | 57 | − 0.6 [− 1.3, 1.5] | 1.6 [0.4, 3] | |||
| 48 h | 48 | 0.7 [− 1.1, 4.2] | 1.3 [0, 2.3] | |||
| Albumin | 1 h | 66 | − 3.4 [− 4.2, − 1.1] | − 1.2 [− 2.6, 0.3] | − 1.1 (− 2.7–0.5) | 0,170 |
| 6 h | 65 | − 2.1 [− 3.5, 0.3] | − 1.4 [− 3, − 0.2] | |||
| 12 h | 62 | − 1.4 [− 2.9, 1.7] | − 1.7 [− 3.1, − 0.1] | |||
| 24 h | 57 | − 2.3 [− 4.5, − 0.8] | − 1.6 [− 3.2, − 07] | |||
| 48 h | 48 | − 1.7 [− 5.7, 1.2] | − 2.4 [− 5, − 0.8] |
Data presented as † median [25th, 75th quantile], ‡ Estimated difference of marginal means (95% confidence interval)
ml/min milliliters per minute, CVVHDF continuous veno-venous hemodiafiltration, CVVHD-HCO continuous veno-venous hemodialysis using high cutoff filter
#p value from comparison of marginal means
Fig. 3.

Myoglobin clearance at different time points. Graphical analysis in grouped boxplots. ml/min milliliters per minute, RRT renal replacement therapy, CVVHDF continuous veno-venous hemodiafiltration, CVVHD continuous veno-venous hemodialysis
The mean arm differences Δ with 95% confidence intervals at 1, 6 12, 24 and 48 h. The null hypothesis Δ = 0 (no arm difference) was tested against the alternative hypothesis Δ > − 1.85 ml/min (margin of non-inferiority), depicted by the dashed red line.
Graphical analysis in grouped boxplots. ml/min milliliters per minute, RRT renal replacement therapy, CVVHDF continuous veno-venous hemodiafiltration, CVVHD continuous veno-venous hemodialysis,
Secondary endpoints
The clearance values for urea and creatinine were higher in the control arm than in the intervention arm. After accounting for the higher TTR in the control arm, clearance values were equal in both arms (Clp.corr.) and displayed in an additional file (see Additional file 2).
The clearance for β2-microglobulin was better in intervention group. Although no significant difference in IL-6 and albumin clearance could be observed concerning marginal means, IL-6-clearance was higher after 1, 6 and 24 h and albumin clearance after 1 h in the intervention arm (see Additional file 3).
Dialyzer lifespan
Dialyzer lifespan was reported as Kaplan–Meier plot. Six patients were excluded from this analysis because treatment was terminated prematurely for other reasons. Median dialyzer lifespan was 57.0 [38.0, 72.0] hours in the control arm and 70.0 [56.75, 72.0] hours in the intervention arm. This difference was statistically significant (log-rank (Mantel-Cox), p = 0.029, Fig. 4).
Fig. 4.
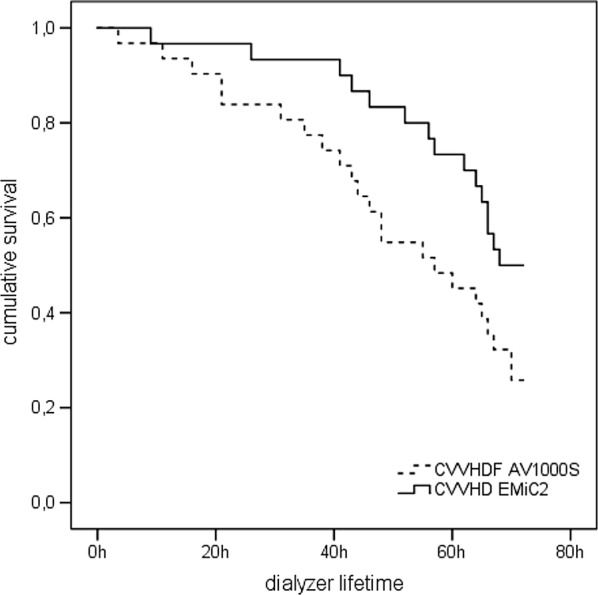
Kaplan–Meier plot for dialyzer lifespan. CVVHDF continuous veno-venous hemodiafiltration, CVVHD continuous veno-venous hemodialysis, AV1000S type of high-flux dialyzer, EMiC2 type of high cut-off dialyzer
Safety endpoints
ICU mortality was higher in the intervention arm than in the control arm. There were no differences in hospital, 28- and 90-day mortality. Adverse events and severe adverse events did not differ between the groups (Table 3).
Table 3.
Safety endpoints
| Variable | Control arm CVVHDF, n = 33 | Intervention arm CVVHD-HCO, n = 35 | p value |
|---|---|---|---|
| Clinical outcome | |||
| ICU length of stay (days) | 11 (5.21) | 13 (7.27) | 0.543 |
| ICU mortality | 10 (30.3%) | 22 (62.9%) | 0.007 |
| Hospital mortality | 18 (54.5%) | 24 (68.6%) | 0.234 |
| Mortality day 28 | 15 (45.5%) | 21 (60%) | 0.23 |
| Mortality day 90 | 21 (65.6%) | 25 (73.5%) | 0.485 |
| Adverse events | 0.205 | ||
| Hypocalcemia | 1 (3%) | 6 (17.1%) | |
| Metabolic alkalosis | 1 (3%) | 0 (0%) | |
| Citrate accumulation | 0 (0%) | 0 (0%) | |
| Catheter malfunction | 1 (3.3%) | 1 (2.9%) | |
| Severe adverse events | 0.265 | ||
| Treatment-associated life-threatening complication | 0 (0%) | 0 (0%) | |
| Dead of any cause during intervention | 2 (6.1%) | 5 (14.3%) |
Data presented as n (%). median [25th, 75th quantile]
ICU intensive care unit, CVVHDF continuous veno-venous hemodiafiltration, CVVHD-HCO continuous veno-venous hemodialysis using high cutoff filter
Discussion
The present study demonstrated that plasma myoglobin clearance in patients with AKI requiring RRT is significantly higher using CVVHD with a high cutoff dialyzer compared to that of CVVHDF with a high-flux dialyzer.
In contrast to recent clinical trials which evaluated the clearance of β2-microglobulin with HCO membranes [17, 26–29], we investigated myoglobin as primary endpoint. High myoglobin levels are associated with AKI and higher mortality rates [6, 7]. Therefore, myoglobin clearance represents a more relevant clinical issue in AKI than the clearance of β2-microglobulin. Serum myoglobin is the best parameter to indicate rhabdomyolysis and can provide the best prediction for AKI in these cases [30, 31]. One retrospective analysis showed that 68.9% of elderly people with rhabdomyolysis developed AKI [32].
Fast elimination of myoglobin is essential due to its direct toxic renal effects [33]. Myoglobin is endocytosed by tubular cells and oxidized, resulting in radical oxygen species that alter DNA and protein function. It activates an inflammatory response in the kidney and mediates vasoconstriction, which perpetuate renal damage. Myoglobin is also filtered by the glomerulus and precipitates in the renal tubules, particularly in combination with the Tamm–Horsfall proteins, forming tubular casts, which consequently result in acute tubular obstruction [5, 33].
Because working kidneys are able to remove more myoglobin than any extracorporeal system [34], the first therapeutic choice is prevention of myoglobinuric AKI and maintain diuresis with adequate fluid resuscitation [35, 36]. RRT might be necessary in patients in whom fluid resuscitation cannot prevent AKI. Clinical data addressing extracorporeal removal of myoglobin are lacking, and it is not yet clear if that prevents AKI, influences the duration of oliguria/anuria or reduces mortality.
Hemofiltration is recommended to eliminate myoglobin in patients with myoglobinuric AKI who need RRT [21]. Due to the hemoconcentration along the dialyzer, CVVH requires higher blood flow than CVVHD. Thus, CVVH with RCA and the required higher blood flow would imply higher citrate load. Systemic anticoagulation increases the risk of bleeding complications, particularly after traumatic rhabdomyolysis, and it may also be associated with HIT [12, 13]. Therefore, CVVHD with RCA using HCO dialyzer could be one possible solution to this problem. Another possibility to reduce citrate load and ensure myoglobin clearance is the combination of hemofiltration and hemodialysis (CVVHDF).
Effective elimination of myoglobin by CVVHDF in rhabdomyolysis was first reported by Mikkelsen and Toft [37]. Albert et al. showed a decline of myoglobin levels using HCO dialyzer [38]. This result was in accordance with another case series involving 18 patients with rhabdomyolysis who underwent longer treatment (6–10 h) with HCO hemodialysis [39]. The effectiveness of HCO dialyzers to eliminate myoglobin was confirmed in another case series with sustained low efficiency daily dialysis (SLEDD) and CVVHD [40]. The cutoff values for the HCO dialyzers used in these studies were similar to the HCO dialyzer in our study, although the effective membrane surface area differed [38–40].
A good clearance of β2-microglobulin was demonstrated in chronic dialysis patients using dialyzers with increased pore size [26, 27]. Recent studies have also confirmed a good clearance for middle molecules in CVVHD with RCA and HCO dialyzers in critically ill patients [17, 28].
Better clearance of β2-microglobulin in the intervention arm in this study is in line with the results of others [17, 28, 41]. Contrary to these findings, another small cohort (n = 10), which compared the β2-microglobulin clearance between CVVHDF using high-flux and HCO dialyzers, showed no difference in both study arms, although the dialysis dose was much higher in the CVVHDF arm (36 ± 4 ml/kg/h) than in the CVVHD arm (21 ± 6 ml/kg/h) [29].
High levels of β2-microglobulin were observed in patients with end-stage renal disease and might be presumed to be a prognostic parameter in chronic dialysis patients [42, 43]. However, the prognostic role of β2-microglobulin in acute kidney injury and critical care medicine and whether if effective clearance of this molecule could be associated with survival advantage is not elucidated.
Initial albumin loss during CVVH using HCO dialyzers was reported in an older study [19]. That is why we used the HCO dialyzers only in CVVHD. With the exception of the sample after 1 h we did not observe differences in albumin clearance in both study groups, which is similar to the findings of recent studies [16, 17, 41].
HCO dialyzers show a greater clearance for inflammatory cytokines than conventional high-flux membranes [16, 44, 45]. Interleukin-6 clearance in our study was superior in the intervention arm after 1, 6 and 24 h, but showed no difference at the remaining time points compared to the control arm. Possible reasons could be the higher molecular weight of Il-6 compared to that of myoglobin and the so-called membrane fouling by protein adsorption and polarization within the membranes over time [16]. This observation was in accordance with the findings of another study on 30 patients comparing HCO and high-flux dialyzers in CVVHD with RCA [46]. In that study, the HCO arm showed a higher clearance of IL-6 and interleukin 10 and decreasing clearance values during the study period [46]. Recent findings strengthen the hypothesis that the clearance for molecules with higher molecular weight decreases over time according to the specific molecular weight [28]. Experimental data support the results of lower clearance rates at a molecular weight greater than 30 kDa and the time dependent influence on middle molecule clearance [47]. The higher albumin clearance after 1 h in CVVHD-HCO group supports this assumption.
Higher TTR had to be realized in the control arm to maintain calcium homeostasis. This accounted for higher clearance values for urea and creatinine in this group. However, no clearance differences of these two small molecules could be detected after correcting for TTR. We therefore conclude that CVVHD using HCO dialyzers is not inferior than CVVHDF using high-flux dialyzers regarding urea and creatinine clearance.
The observed shorter dialyzer lifespan in our control arm in comparison with our intervention arm may be related to hemoconcentration at the dialyzer during CVVHDF, which may contribute to clot formation [48]. This effect could be enhanced by the postdilution modality. Another reason might be the more error-prone management of CVVHDF with RCA, related to different dialysis and replacement fluids. Older studies comparing CVVHDF with RCA versus systemic anticoagulation with heparin showed no advantage regarding dialyzer survival using RCA [49, 50]. This seems to be a specific problem using CVVHDF with RCA. Contrary to these older studies, newer studies, although using CVVHDF, showed longer dialyzer survival using RCA similar to the findings of other trials using other modes of CRRT with RCA [12, 13].
The high observed mortality in both treatment arms is in line with results of other studies considering the disease severity of investigated patient population [51].
Limitations
There are certain limitations to our trial. Firstly, it is a monocentric, single-blinded trial, conducted at a medical ICU. A double-blind design was impossible, because the extracorporeal circuit differs between the two study arms.
Secondly, we analyzed the performance of two different renal replacement methods concerning solute specific clearances in critical care patients who suffered AKI for different reasons. It is not possible to conclude that the choice of procedure effects mortality or renal outcome. Thirdly, we cannot provide any recommendation when RRT should be started to remove myoglobin. Finally, the primary endpoint consists of 5 repeated measurements. However, we believe that using the marginal mean for comparison of the arms is a good choice, which also addresses the problem of multiple tests sufficiently.
Conclusion
In summary, this study demonstrates that myoglobin can be cleared using CVVHD-HCO with regional citrate anticoagulation in AKI in critical ill patients in a medical ICU.
This study provides a solid background to generate hypotheses and design large clinical trials with hard clinical end points. Further studies are needed to show non-inferiority of CVVHD-HCO compared to CVVH with systemic anticoagulation, especially in cases of severe rhabdomyolysis.
In our opinion, CVVHD using high cutoff dialyzers with RCA could be beneficial in patients suffering from AKI and high myoglobin values, particularly in conditions with high risk of bleeding.
Supplementary information
Additional file 2. Substance specific clearances (ml/min) after 1h and adjustment for TTR.
Additional file 3. Substance specific clearances (ml/min) at different time points.
Acknowledgements
We thank Peter Appelt, Carsten Bayer, Antonia Borrmann, Martin Grimm, Dirk Hasenclever, Kevin Kunz, Konstanze Lichtenberger, Laura Oehler, Alexander Peschka, Frank Seidel, Sebastian Sewerin, Clemens Stehl, Jasmin Tischer, Manuel Viehmann, Henning Weidhase and the ICUs staff for their support.
Abbreviations
- AKI
Acute kidney injury
- RRT
Renal replacement therapy
- CRRT
Continuous renal replacement therapy
- RCA
Regional citrate anticoagulation
- HIT
Heparin-induced thrombocytopenia
- CVVH
Continuous veno-venous hemofiltration
- CVVHD
Continuous veno-venous hemodialysis
- CVVHDF
Continuous veno-venous hemodiafiltration
- HCO
High cutoff
- KDIGO
Kidney disease, improving global outcomes
- ICU
Intensive care unit
- kDa
Kilodaltons
- TTR
Total turnover rate (dialysate and substituent)
- QB
Blood flow
- Il-6
Interleukin-6
- Cpre
Concentration before the dialyzer
- Cpost
Concentration after the dialyzer
- Cpost.corr
Corrected concentration after the dialyzer
- Qppre
Prefilter plasma flow
- Hct
Hematocrit level
- Clp
Substance-specific plasma clearance
- Clp.corr.
Corrected plasma clearance
- Qppost
Postfilter plasma flow
- FP
Filtration portion
- ECLIA
ElektroChemiLumineszenzImmunoAssay
- CI
Confidence interval
- SLEDD
Sustained low efficiency daily dialysis
Authors’ contributions
LW, JF and SP were involved in conceptualization. LW, JF and EH helped in data curation. LW, JF and MM contributed to formal analysis. LW and JF were involved in funding acquisition. LW, JF and EH helped in investigation. LW, JF and MM contributed to methodology. LW and JF were involved in project administration. LW and TK helped in resources. TK and SP contributed to supervision. SP was involved in validation. JF and MM helped in visualization. JF contributed to writing—original draft. LW, JF, MM, EH, TK and SP were involved in writing—review and editing. All authors read and approved the final manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL. Lorenz Weidhase received funding from Fresenius Medical Care Deutschland GmbH (Else-Kröner-Straße 1, D-61352 Bad Homburg, Germany). The remaining authors have disclosed that they do not have any conflicts of interest.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
The study was approved by the local ethics committee (ethical committee at the medical faculty, Leipzig university, 480/19-ek), conducted in accordance with the German medical product law and registered at the German Clinical Trials Registry (DRKS00012407). Informed consent was either given by the patients or their legal guardians.
Consent for publication
Not applicable.
Competing interests
None.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Lorenz Weidhase and Jonathan de Fallois have contributed equally to this work
Supplementary information
Supplementary information accompanies this paper at 10.1186/s13054-020-03366-8.
References
- 1.Hoste EAJ, Bagshaw SM, Bellomo R, Cely CM, Colman R, Cruz DN, et al. Epidemiology of acute kidney injury in critically ill patients: the multinational AKI-EPI study. Intensive Care Med. 2015;41:1411–1423. doi: 10.1007/s00134-015-3934-7. [DOI] [PubMed] [Google Scholar]
- 2.Uchino S, Kellum JA, Bellomo R, Doig GS, Morimatsu H, Morgera S, et al. Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA. 2005;294:813–818. doi: 10.1001/jama.294.7.813. [DOI] [PubMed] [Google Scholar]
- 3.Levy EM, Viscoli CM, Horwitz RI. The effect of acute renal failure on mortality. A cohort analysis. JAMA. 1996;275:1489–1494. doi: 10.1159/000489082. [DOI] [PubMed] [Google Scholar]
- 4.Bellomo R, Kellum JA, Ronco C. Acute kidney injury. Lancet (London, England) 2012;380:756–766. doi: 10.1016/S0140-6736(11)61454-2. [DOI] [PubMed] [Google Scholar]
- 5.Bosch X, Poch E, Grau JM. Rhabdomyolysis and acute kidney injury. N Engl J Med. 2009;361:62–72. doi: 10.1056/NEJMra0801327. [DOI] [PubMed] [Google Scholar]
- 6.Bagley WH, Yang H, Shah KH. Rhabdomyolysis. Intern Emerg Med. 2007;2:210–218. doi: 10.1007/s11739-007-0060-8. [DOI] [PubMed] [Google Scholar]
- 7.Melli G, Chaudhry V, Cornblath DR. Rhabdomyolysis. Medicine (Baltimore) 2005;84:377–385. doi: 10.1097/01.md.0000188565.48918.41. [DOI] [PubMed] [Google Scholar]
- 8.Truche AS, Darmon M, Bailly S, Clec’h C, Dupuis C, Misset B, et al. Continuous renal replacement therapy versus intermittent hemodialysis in intensive care patients: impact on mortality and renal recovery. Intensive Care Med. 2016;42:1408–1417. doi: 10.1007/s00134-016-4404-6. [DOI] [PubMed] [Google Scholar]
- 9.Zhang L, Yang J, Eastwood GM, Zhu G, Tanaka A, Bellomo R. Extended daily dialysis versus continuous renal replacement therapy for acute kidney injury: a meta-analysis. Am J Kidney Dis. 2015;66:322–330. doi: 10.1053/j.ajkd.2015.02.328. [DOI] [PubMed] [Google Scholar]
- 10.Bagshaw SM, Berthiaume LR, Delaney A, Bellomo R. Continuous versus intermittent renal replacement therapy for critically ill patients with acute kidney injury: a meta-analysis. Crit Care Med. 2008;36:610–617. doi: 10.1097/01.CCM.0B013E3181611F552. [DOI] [PubMed] [Google Scholar]
- 11.KDIGO Clinical practice guideline for acute kidney injury (AKI) Kidney Int Suppl. 2012;2:4. doi: 10.1038/kisup.2012.4. [DOI] [Google Scholar]
- 12.Bai M, Zhou M, He L, Ma F, Li Y, Yu Y, et al. Citrate versus heparin anticoagulation for continuous renal replacement therapy: an updated meta-analysis of RCTs. Intensive Care Med. 2015;41:2098–2110. doi: 10.1007/s00134-015-4099-0. [DOI] [PubMed] [Google Scholar]
- 13.Liu C, Mao Z, Kang H, Hu J, Zhou F. Regional citrate versus heparin anticoagulation for continuous renal replacement therapy in critically ill patients: a meta-analysis with trial sequential analysis of randomized controlled trials. Crit Care. 2016;20:1–13. doi: 10.1186/S13054-016-1299-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morgera S, Scholle C, Voss G, Haase M, Vargas-Hein O, Krausch D, et al. Metabolic complications during regional citrate anticoagulation in continuous venovenous hemodialysis: Single-center experience. Nephron Clin Pract. 2004;97:131–136. doi: 10.1159/000079171. [DOI] [PubMed] [Google Scholar]
- 15.Ricci Z, Ronco C, Bachetoni A, D’amico G, Rossi S, Alessandri E, et al. Solute removal during continuous renal replacement therapy in critically ill patients: convection versus diffusion. Crit Care. 2006;10:1–7. doi: 10.1186/cc4903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Villa G, Zaragoza JJ, Sharma A, Neri M, De Gaudio AR, Ronco C. Cytokine removal with high cut-off membrane: review of literature. Blood Purif. 2014;38:167–173. doi: 10.1159/000369155. [DOI] [PubMed] [Google Scholar]
- 17.Weidhase L, Haussig E, Haussig S, Kaiser T, de Fallois J, Petros S. Middle molecule clearance with high cut-off dialyzer versus high-flux dialyzer using continuous veno-venous hemodialysis with regional citrate anticoagulation: a prospective randomized controlled trial. PLoS ONE. 2019;14:e0215823. doi: 10.1371/journal.pone.0215823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Masakane I, Sakurai K. Current approaches to middle molecule removal: room for innovation. Nephrol Dial Transplant. 2018;33:iii12–21. doi: 10.1093/ndt/gfy224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morgera S, Slowinski T, Melzer C, Sobottke V, Vargas-Hein O, Volk T, et al. Renal replacement therapy with high-cutoff hemofilters: impact of convection and diffusion on cytokine clearances and protein status. Am J Kidney Dis. 2004;43:444–453. doi: 10.1053/j.ajkd.2003.11.006. [DOI] [PubMed] [Google Scholar]
- 20.Doig GS, Simpson F. Randomization and allocation concealment: a practical guide for researchers. J Crit Care. 2005;20:187–191. doi: 10.1016/j.jcrc.2005.04.005. [DOI] [PubMed] [Google Scholar]
- 21.Amyot SL, Leblanc M, Thibeault Y, Geadah D, Cardinal J. Myoglobin clearance and removal during continuous venovenous hemofiltration. Intensive Care Med. 1999;25:1169–1172. doi: 10.1007/s001340051031. [DOI] [PubMed] [Google Scholar]
- 22.Wellek S, Blettner M. Establishing equivalence or non-inferiority in clinical trials: part 20 of a series on evaluation of scientific publications. Dtsch Arztebl Int. 2012;109:674–679. doi: 10.3238/arztebl.2012.0674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fayad AI, Buamscha DG, Ciapponi A. Intensity of continuous renal replacement therapy for acute kidney injury. Cochrane Database Syst Rev. 2016 doi: 10.1002/14651858.CD010613.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Glynn CC, Greene GW, Winkler MF, Albina JE. Predictive versus measured energy expenditure using limits-of-agreement analysis in hospitalized, obese patients. JPEN J Parenter Enteral Nutr. 1999;23:147–154. doi: 10.1177/0148607199023003147. [DOI] [PubMed] [Google Scholar]
- 25.Krenitsky J. adjusted body weight, pro: evidence to support the use of adjusted body weight in calculating calorie requirements. Nutr Clin Pract. 2005;20:468–473. doi: 10.1177/0115426505020004468. [DOI] [PubMed] [Google Scholar]
- 26.Locatelli F, Martin-Malo A, Hannedouche T, Loureiro A, Papadimitriou M, Wizemann V, et al. Effect of membrane permeability on survival of hemodialysis patients. J Am Soc Nephrol. 2009;20:645–654. doi: 10.1681/ASN.2008060590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pellicano R, Polkinghorne KR, Kerr PG. Reduction in β2-microglobulin with super-flux versus high-flux dialysis membranes: results of a 6-week, randomized, double-blind, crossover trial. Am J Kidney Dis. 2008;52:93–101. doi: 10.1053/j.ajkd.2008.02.296. [DOI] [PubMed] [Google Scholar]
- 28.Siebeck M, Dimski T, Brandenburger T, Slowinski T, Kindgen-Milles D. Super high-flux continuous venovenous hemodialysis using regional citrate anticoagulation: long-term stability of middle molecule clearance. Ther Apher Dial. 2018;22:355–364. doi: 10.1111/1744-9987.12656. [DOI] [PubMed] [Google Scholar]
- 29.Balgobin S, Morena M, Brunot V, Besnard N, Daubin D, Platon L, et al. Continuous veno-venous high cut-off hemodialysis compared to continuous veno-venous hemodiafiltration in intensive care unit acute kidney injury patients. Blood Purif. 2018;46:248–256. doi: 10.1159/000489082. [DOI] [PubMed] [Google Scholar]
- 30.El-Abdellati E, Eyselbergs M, Sirimsi H, van Hoof V, Wouters K, Verbrugghe W, et al. An observational study on rhabdomyolysis in the intensive care unit. Exploring its risk factors and main complication: acute kidney injury. Ann Intensive Care. 2013;3:1–8. doi: 10.1186/2110-5820-3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chavez LO, Leon M, Einav S, Varon J. Beyond muscle destruction: a systematic review of rhabdomyolysis for clinical practice. Crit Care. 2016;20:135. doi: 10.1186/s13054-016-1314-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wongrakpanich S, Kallis C, Prasad P, Rangaswami J, Rosenzweig A. The study of rhabdomyolysis in the elderly: an epidemiological study and single center experience. Aging Dis. 2018;9:1–7. doi: 10.14336/AD.2017.0304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Panizo N, Rubio-Navarro A, Amaro-Villalobos JM, Egido J, Moreno JA. Molecular mechanisms and novel therapeutic approaches to rhabdomyolysis-induced acute kidney injury. Kidney Blood Press Res. 2015;40:520–532. doi: 10.1159/000368528. [DOI] [PubMed] [Google Scholar]
- 34.Shigemoto T, Rinka H, Matsuo Y, Kaji A, Tsukioka K, Ukai T, et al. Blood purification for crush syndrome. Ren Fail. 1997;19:711–719. doi: 10.3109/08860229709109037. [DOI] [PubMed] [Google Scholar]
- 35.Sever MS, Vanholder R. RDRTF of ISN work group on recommendations for the management of crush victims in mass disasters. Recommendation for the management of crush victims in mass disasters. Nephrol Dial Transplant. 2012;27:i1–67. doi: 10.1093/ndt/gfs156. [DOI] [PubMed] [Google Scholar]
- 36.Scharman EJ, Troutman WG. Prevention of kidney injury following rhabdomyolysis: a systematic review. Ann Pharmacother. 2013;47:90–105. doi: 10.1345/aph.1R215. [DOI] [PubMed] [Google Scholar]
- 37.Mikkelsen TS, Toft P. Prognostic value, kinetics and effect of CVVHDF on serum of the myoglobin and creatine kinase in critically ill patients with rhabdomyolysis. Acta Anaesthesiol Scand. 2005;49:859–864. doi: 10.1111/j.1399-6576.2005.00577.x. [DOI] [PubMed] [Google Scholar]
- 38.Albert C, Haase M, Bellomo R, Mertens PR. High cut-off and high-flux membrane haemodialysis in a patient with rhabdomyolysis-associated acute kidney injury. Crit Care Resusc. 2012;14:159–162. [PubMed] [Google Scholar]
- 39.Premru V, Kovač J, Buturović-Ponikvar J, Ponikvar R. Some kinetic considerations in high cut-off hemodiafiltration for acute myoglobinuric renal failure. Ther Apher Dial. 2013;17:396–401. doi: 10.1111/1744-9987.12085. [DOI] [PubMed] [Google Scholar]
- 40.Heyne N, Guthoff M, Krieger J, Haap M, Häring H-U. High cut-off renal replacement therapy for removal of myoglobin in severe rhabdomyolysis and acute kidney injury: a case series. Nephron Clin Pract. 2012;121:c159–c164. doi: 10.1159/000343564. [DOI] [PubMed] [Google Scholar]
- 41.Schmidt JJ, Hafer C, Clajus C, Hadem J, Beutel G, Schmidt BMW, et al. New high-cutoff dialyzer allows improved middle molecule clearance without an increase in albumin loss: a clinical crossover comparison in extended dialysis. Blood Purif. 2012;34:246–252. doi: 10.1159/000342631. [DOI] [PubMed] [Google Scholar]
- 42.Roumelioti ME, Nolin T, Unruh ML, Argyropoulos C. Revisiting the middle molecule hypothesis of uremic toxicity: a systematic review of beta 2 microglobulin population kinetics and large scale modeling of hemodialysis trials in silico. PLoS ONE. 2016;11:e0153157. doi: 10.1371/journal.pone.0153157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Liabeuf S, Lenglet A, Desjardins L, Neirynck N, Glorieux G, Lemke H-D, et al. Plasma beta-2 microglobulin is associated with cardiovascular disease in uremic patients. Kidney Int. 2012;82:1297–1303. doi: 10.1038/ki.2012.301. [DOI] [PubMed] [Google Scholar]
- 44.Naka T, Haase M, Bellomo R. “Super high-flux” or “high cut-off” hemofiltration and hemodialysis. Contrib Nephrol. 2010;166:181–189. doi: 10.1159/000314871. [DOI] [PubMed] [Google Scholar]
- 45.Morgera S, Haase M, Kuss T, Vargas-Hein O, Zuckermann-Becker H, Melzer C, et al. Pilot study on the effects of high cutoff hemofiltration on the need for norepinephrine in septic patients with acute renal failure. Crit Care Med. 2006;34:2099–2104. doi: 10.1097/01.CCM.0000229147.50592.F9. [DOI] [PubMed] [Google Scholar]
- 46.Eichhorn T, Hartmann J, Harm S, Linsberger I, König F, Valicek G, et al. Clearance of selected plasma cytokines with continuous veno-venous hemodialysis using ultraflux EMiC2 versus ultraflux AV1000S. Blood Purif. 2017;44:260–266. doi: 10.1159/000478965. [DOI] [PubMed] [Google Scholar]
- 47.Hofmann CL, Fissell WH. Middle-molecule clearance at 20 and 35 ml/kg/h in continuous venovenous hemodiafiltration. Blood Purif. 2010;29:259–263. doi: 10.1159/000266483. [DOI] [PubMed] [Google Scholar]
- 48.Hemodiafiltration RC. Technical and clinical issues. Blood Purif. 2015;40:2–11. doi: 10.1159/000437403. [DOI] [PubMed] [Google Scholar]
- 49.Gabutti L, Marone C, Colucci G, Duchini F, Schönholzer C. Citrate anticoagulation in continuous venovenous hemodiafiltration: a metabolic challenge. Intensive Care Med. 2002;28:1419–1425. doi: 10.1007/s00134-002-1443-y. [DOI] [PubMed] [Google Scholar]
- 50.Brain MJ, Roodenburg OS, Adams N, McCracken P, Hockings L, Musgrave S, et al. Randomised trial of software algorithm driven regional citrate anticoagulation versus heparin in continuous renal replacement therapy: the Filter Life in Renal Replacement Therapy pilot trial. Crit Care Resusc. 2014;16:131–137. [PubMed] [Google Scholar]
- 51.Wang H, Kang X, Shi Y, Bai Z, Lv J, Sun J, et al. SOFA score is superior to APACHE-II score in predicting the prognosis of critically ill patients with acute kidney injury undergoing continuous renal replacement therapy. Ren Fail. 2020;42:638–645. doi: 10.1080/0886022X.2020.1788581. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 2. Substance specific clearances (ml/min) after 1h and adjustment for TTR.
Additional file 3. Substance specific clearances (ml/min) at different time points.
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.