Abstract
Background:
Information on diabetes-related excess medical expenditures for youth is important to understand the magnitude of financial burden and to plan the health care resources needed for managing diabetes. However, diabetes-related excess medical expenditures for youth covered by Medicaid program have not been investigated recently.
Objective:
To estimate excess diabetes-related medical expenditures among youth aged below 20 years enrolled in Medicaid programs in the United States.
Methods:
We analyzed data from 2008 to 2012 MarketScan multistate Medicaid database for 6502 youths with diagnosed diabetes and 6502 propensity score matched youths without diabetes, enrolled in fee-for-service payment plans. We stratified analysis by Medicaid eligibility criteria (poverty or disability). We used 2-part regression models to estimate diabetes-related excess medical expenditures, adjusted for age, sex, race/ethnicity, year of claims, depression status, asthma status, and interaction terms.
Results:
For poverty-based Medicaid enrollees, estimated annual diabetes-related total medical expenditure was $9046 per person [$3681 (no diabetes) vs. $12,727 (diabetes); P<0001], of which 41.7%, 34.0%, and 24.3% were accounted for by prescription drugs, outpatient, and inpatient care, respectively. For disability-based Medicaid enrollees, the estimated annual diabetes-related total medical expenditure was $9944 per person ($14,149 vs. $24,093; P<0001), of which 41.5% was accounted for by prescription drugs, 31.3% by inpatient, and 27.3% by outpatient care.
Conclusions:
The per capita annual diabetes-related medical expenditures in youth covered by publicly financed Medicaid programs are substantial, which is larger among those with disabilities than without disabilities. Identifying cost-effective ways of managing diabetes in this vulnerable segment of the youth population is needed.
Kew Words: costs, children, public, poverty-based, disability-based
Diabetes incidence and prevalence among youth in the United States have been increasing.1–3 From 2001 to 2009, diabetes prevalence among youth aged below 20 years increased from 1.82 to 2.22 per 1000.1,2 At the same time, youth accounted for a large and growing number of enrollees in public health programs, such as Medicaid and the Children’s Health Insurance Program (CHIP). The Medicaid is a publicly financed US federal and state program that offers health insurance to low income or medically needy children and adults with US citizenship or lawful permanent residents, whereas CHIP covers the uninsured children (below 19 y) from families who do not qualify for Medicaid because of higher income (www.medicaid.gov/index.html). In 2000, ∼24 million US chidren were ever covered by public insurance programs; by 2011, coverage nearly doubled to 43.5 million.4
Despite these increases in diabetes prevalence and public insurance coverage, the magnitude of financial burden of diabetes on public insurance programs such as Medicaid among youth has not been recently evaluated. In 2003, one study reported per capita annual excess medical costs of diabetes among persons aged below 18 years who were eligible for Medicaid based on poverty criteria.5 The estimates from this study could be biased due to a lack of adjusting for factors such as demographics and comorbidities that could potentially affect health expenditures. Another study, using the California Children’s Services program claims data, estimated per capita median medical cost for presumed type 1 children.6 Again the estimate was based on small sample and did not adjust for covariates. Further, we are not aware of studies that estimated diabetes-related expenditures among youth eligible for public health insurance by eligibility criteria (disability vs. nondisability).
Estimates on the health care expenditure among youth with public health insurance and its eligibility criteria are needed to understand the magnitude of the economic burden of diabetes and to plan the health care resources needed for managing diabetes in this population. The health care needs and associated cost for children with disability is likely to be greater than without the disability.7,8 Children with severe chronic condition enrolled in Medicaid with disability (recipient of supplemental security income) reported to have higher per capita medical expenditure than those eligible for other than disability.8
Here, we estimated diabetes-related excess expenditures separately for poverty-eligible and disability-eligible Medicaid enrollees. We also adjusted for demographic factors and comorbid conditions that could affect expenditures between person with and without diabetes. As for privately insured youth,9 we hypothesized that among youth covered by Medicaid the per capita annual medical expenditures would be higher among youth with diabetes than in youth without this condition. The co-occurrence of disability may require additional health care for diabetes management, hence we hypothesized that the medical expenditures associated with diabetes would be higher among youth enrolled based on disability than those based on poverty criteria.
METHODS
Data Source
We used data from the 2008 to 2012 MarketScan Medicaid multistate databases (Truven Health Analytics, Ann Arbor, MI). These data were from 10 to 12 unidentified US states, hence did not allow us to study by state. This database contains information on enrollees’ enrollment, demographics, and health care claims, including outpatient, inpatient, and pharmaceutical claims. Outpatient claims include services that occurred outside of an inpatient admission, such as visits to a physician’s office, patient’s home, or hospital outpatient facility, as well as laboratory testing. Inpatient claims include those associated with hospital admission, such as physician, surgeon, independent laboratories, and medication charges. Pharmaceutical claims include prescription drugs in outpatient settings, including diabetes supplies such as insulin pumps, pens, syringes, glucose monitors, and test strips. These claims are linkable using enrollees’ unique encrypted identifiers that allow estimating total medical expenditures at the patient level. Expenditures include reimbursed payments from the Medicaid or CHIP and from patients, but patient expenditures are nominal.10
Study Population
Figure 1 shows how we selected individuals for this study. We included youth aged below 20 years who were fully enrolled in Medicaid or CHIP for at least 1 year during 2008–2012. If the enrollees were fully enrolled in multiple years, we included data from the most recent years. We included multiple years of data to increase the sample size, allowing us to analyze data by subpopulations. We were unable to distinguish between Medicaid or CHIP coverage because of lack of information in the database; we henceforth use the term Medicaid to represent both programs.
FIGURE 1.
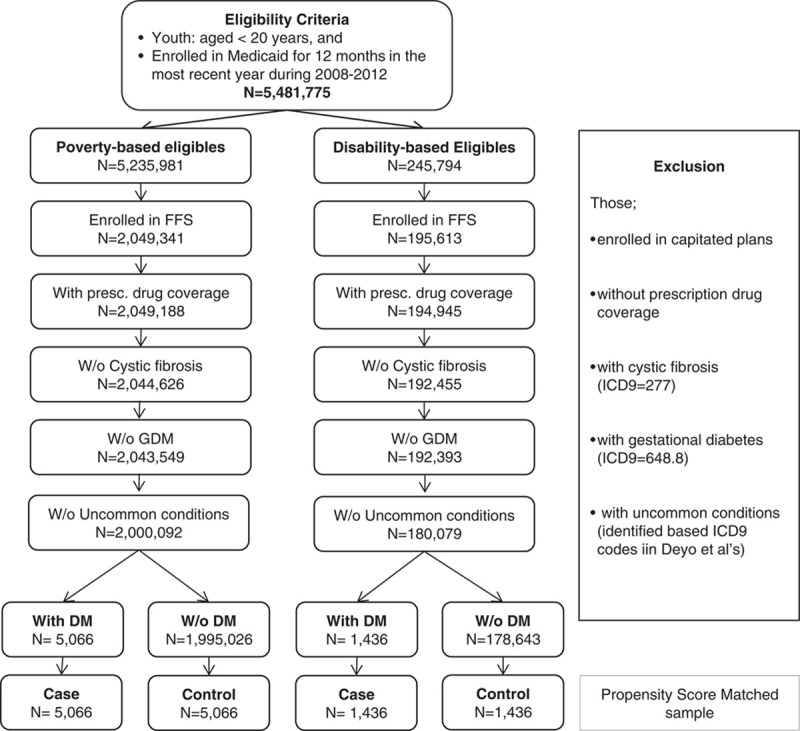
Sample selection. DM indicates diagnosed with diabetes mellitus; FFS, fee-for-service; GDM, gestational diabetes mellitus; ICD9, International Classification of Diseases, 9th Revision, Clinical Modification; W/o, without.
We identified Medicaid enrollees as poverty-based or disability-based, using the basis of eligibility codes in the enrollment file. Youth coded blind or disabled were categorized as eligible based on disability; and those coded as living in foster care, youth of unemployed adults or families with an income level below the poverty threshold were categorized as eligible based on poverty (or nondisability).11
We excluded enrollees: (i) not fully enrolled (ie, below 12 mo) in the calendar year to estimate the full annual cost; (ii) in capitated health plans, because their insurance claims often reflect only encounters with health care providers rather than actual charges12; (iii) without prescription drug coverage, because we could not estimate the total medical expenditures without knowing those for prescription drugs; (iv) diagnosed with cystic fibrosis (ICD9=277), because it is associated with secondary diabetes; (iv) diagnosed with gestational diabetes (ICD9=648.8); (v) diagnosed with medical conditions uncommon in youth, including myocardial infarction, congestive heart failure, peripheral vascular disease, cerebrovascular disease, Down syndrome, rheumatic disease, peptic ulcer, liver diseases, hemiplegia, lymphoma, tumor, and acquired immune deficiency syndrome,13 because of the small number of occurrences prevented us from getting accurate estimates of their effects on the medical expenditures. However, we retained in the study population enrollees with common conditions, such as asthma (ICD9=493) and major depression (ICD9=296.2 or 296.3) (Fig. 1).
We identified youth with diabetes if they had ≥2 outpatient claims, at least 30 days apart, or at least 1 inpatient admission in which diabetes was a primary or secondary diagnosis (ICD9 codes: 250, 357.2, 362.0, 362.0-362.02). All had to have at least 1 diabetes prescription drug claim [therapeutic class codes (TCC) of 172, 173, and 174 based on the American Hospital Formulary Service Classification Compilation therapeutic class].9 The requirement for at least 2 outpatient claims is the conventional way of defining diabetes using claims data,9,14 as it excludes youth who were misdiagnosed as having diabetes at the first encounter and were later determined not to have diabetes. Following these criteria, we identified 6502 youth with diagnosed diabetes: 5066 poverty-based and 1436 disability-based.
After we identified youth with diagnosed diabetes, we matched each case with 1 control using a propensity score matching method. We estimated propensity score for cases of diabetes using a Probit model controlling for age, sex, race/ethnicity, major depression, asthma, and claim year. Next, for each case we matched 1 control (1:1) without diagnosed diabetes using the nearest neighbor algorithm.15 The case control matched sample for our analyses included 10,132 poverty-based and 2872 disability-based youth (Fig. 1).
Among youth identified with diabetes, we identified those with insulin-treated diabetes mellitus if they had at least 1 prescription for insulin (TCC, 172) and with noninsulin-treated diabetes mellitus if they had at least 1 oral hypoglycemic drug prescription (TCC, 173, 174). Using the ICD9 codes in outpatient and inpatient claims, we defined cases of diabetes ketoacidosis (DKA) (ICD9 codes 250.1x) and hypoglycemia (ICD9 codes 250.8, 251.0, 251.1, and 251.2). Diabetes-related medical expenditures are higher among those with insulin-treated diabetes mellitus than those with noninsulin-treated diabetes mellitus and those with DKA and hypoglycemia than without these complications.9,16
Statistical Analysis
The main outcome of interest includes the per capita total medical expenditure, which comprised of sum of outpatient, inpatient, and prescription drug expenditures.
We used χ2 statistics to test the differences in the proportion of sample characteristics. We used the Student t test to compare the means of health services utilization between persons with and without diabetes. We also compared excess diabetes-related health services use between categories of demographic groups (age, sex, and race/ethnicity). For this, we estimated each service use separately using negative binomial regression, controlling for age, sex, race/ethnicity, major depression status, asthma status, year of claims, and diabetes status. We also included statistically significant (ie, P<0.05) interaction terms between diabetes and age group, sex, and race/ethnicity.
For estimating diabetes-related excess medical expenditures for each component of total medical expenditure, we used a 2-part model. For the first part, we used a generalized linear regression model with logit link and binomial distribution to estimate the probability that an individual had a positive expenditure. For the second part, we used a generalized linear regression model with log link and gamma distribution to estimate medical expenditures for those who had positive expenditure.17 This accounted for a large proportion of youth with no medical expenditures, and the positive skew of expenditures among those who used services. In both models, we included covariates as used in our analyses for service use.
For each cost component, we predicted annual medical expenditures for youth with and without diabetes. The predicted mean differences provided the mean excess diabetes-related medical expenditure. We also predicted the annual excess diabetes-related medical expenditures for youth by age, sex, and racial and ethnic groups to understand if excess diabetes-related expenditures vary across these groups. We used the t test with unequal variance to examine differences in predicted expenditures.
We used 1000 nonparametric bootstrap replications to calculate SEs for predicted excess expenditures. All expenditures were adjusted to 2012US$ using the medical care part of consumer price index for all urban consumers (www.bls.gov/cpi/tables.htm).
RESULTS
Characteristics of Study Population
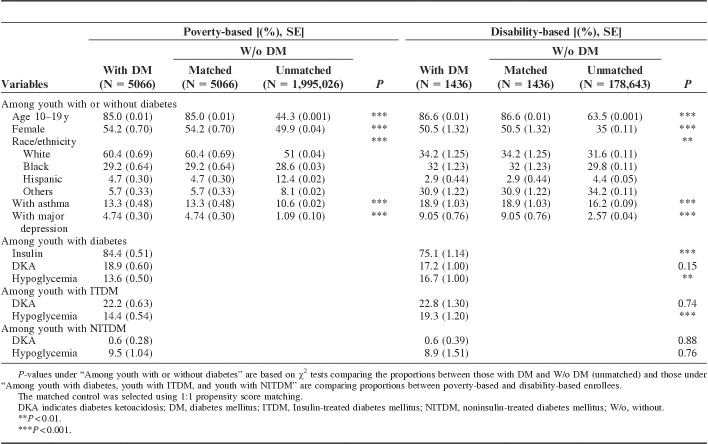
Youth with diabetes were more likely to be older (aged, 10–19 y), female, and white or black, and to have asthma, as compared with youth without diabetes (unmatched) (Table 1). The majority of youth with diabetes were on insulin treatment, with a larger proportion among poverty-based enrollees than among disability-based enrollees. The proportion of youth with at least 1 claim for DKA was similar regardless of eligibility; hypoglycemia claims were more common among disability-based enrollees.
TABLE 1.
Sample Characteristics by Medicaid Eligibility and Diabetes Status
Health Services Use
As compared with youth without diabetes, those with diabetes had higher health services use. For example, the mean number of inpatient admissions among enrollees with diabetes was 4.8 times higher among poverty-based enrollees and 3.1 times higher among disability-based enrollees. Similarly, as compared with poverty-based enrollees, disability-based enrollees had higher health services use (Table 2).
TABLE 2.
Health Care Services Use (Percentage Using and Annual Mean and Median) by Medicaid Eligibility and Diabetes Status, 2008–2012
Among poverty-based enrollees, youth aged 10–19 years had fewer diabetes-related outpatient visits but more emergency room (ER) visits, inpatient admissions, and longer hospital stays and number of therapeutic classes of prescription than those aged below 10 years (Appendix 1). Females had more diabetes-related outpatient visits, emergency room visits, inpatient admissions, and number of therapeutic classes of prescription drugs, and longer inpatient stays than males. Compared with whites, blacks had a higher number of days of admissions but lower outpatient visits, ER visits, days of prescription filled, and number of therapeutic classes of prescription. Hispanics had a lower number of diabetes-related excess services use as compared with whites.
APPENDIX 1.
Negative Binomial Regression Estimates of Per Capita Annual Diabetes-related Excess Health Services Use by Demographic Group and Medicaid Eligibility Criteria
Among disability-based enrollees, the diabetes-related excess services use were higher in the 10–19-year-old group than the below 10-year-old group (Appendix 1). Females had more diabetes-related ER visits, inpatient admissions, days of prescriptions filled, and therapeutic classes of prescriptions filled but lower outpatient visits, and shorter hospital stays than males. Compared with whites, blacks, and Hispanic had lower diabetes-related health services use, except for length of hospital stay for blacks.
Estimated Excess Medical Expenditures From Diabetes
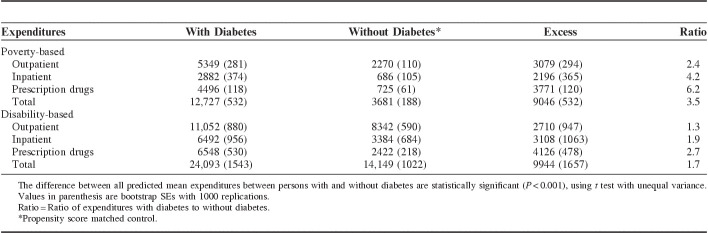
Among poverty-based enrollees, youth with diabetes had 3.5 times as much of the estimated annual per capita medical expenditure of those without diabetes ($12,727 vs. $3681, an excess of $9046; P<0001) (Table 3). Amount spent on individual components of health care services by youth with diabetes ranged from 2.4 to 6.2 times as much as that for those without diabetes. Prescription drugs accounted for the largest proportion of excess expenditure (41.7%), followed by outpatient care (34.0%), and inpatient care (24.3%).
TABLE 3.
Estimated Per Capita Annual Medical Expenditures (at 2012$) by Medicaid Eligibility and Diabetes Status, 2008–2012
Among disability-based enrollees, estimated annual per capita total medical expenditure for those with diabetes was 1.7 times as much as among those without diabetes ($24,093 vs. $14,149, an excess of $9944; P<0.001) (Table 3). Medical expenditures for individual components of health care services ranged from 1.3 to 2.7 times as much for youth with diabetes as for those without diabetes. Prescription drugs accounted for the largest proportion (41.5%), of excess medical expenditure from diabetes, followed by inpatient care (31.3%), and outpatient care (27.3%) (Table 3).
Excess diabetes-related medical expenditure for disability-based enrollees was 1.1 times as much as that for poverty-based enrollees, mainly due to higher inpatient care expenditures (Table 3).
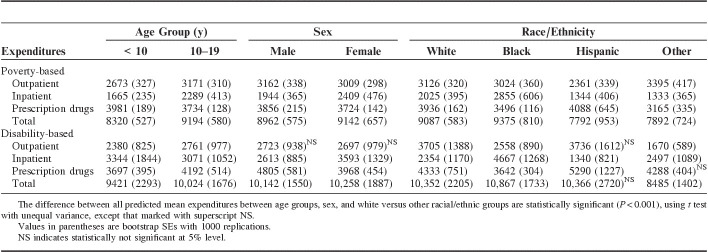
Among poverty-based enrollees, annual per capita diabetes-related medical expenditure was higher in the 10–19-year-old age group than in the below 10-year-old age group, although this varied by type of care: youth aged below 10 years spent more on prescription drugs, but less on inpatient care and outpatient care than those aged 10–19 years (Table 4). Among disability-based enrollees also the annual per capita diabetes-related medical expenditure was higher in the 10–19-year-age group than in the below 10-year-old age group, mainly attributed to higher expenditures on prescription drugs and outpatient care. The per capita excess diabetes-related medical expenditures were slightly higher among females as compared with males for poverty-based enrollees by $180, mainly attributed to excess expenditure on inpatient care. Among disability-based enrollees, female spent more on inpatient care but less on prescription drugs compared with males. By race/ethnicity, the per capita excess expenditures were higher among blacks, followed by whites, other race/ethnicity, and Hispanics among poverty-based enrollees. Among disability-based enrollees the medical expenditures were lower among whites than blacks but higher than other race/ethnicity. For example, compared with whites, diabetes-related medical expenditures among blacks were $288 higher (P<0.001) among poverty-based enrollees and $515 higher (P<0.001) among disability-based enrollees (Table 4).
TABLE 4.
Estimated Per Capita Excess Annual Medical Expenditures (at 2012$) Related to Diabetes by Medicaid Eligibility and Demographics, 2008–2012
DISCUSSION
Consistent with previous studies9,16,18 and as hypothesized, we found that, regardless of eligibility criteria, estimated per capita medical expenditure was higher for youth with diabetes than without it. Higher medical expenditures were mainly due to excess health services use. Part of the excess expenditure could be attributable to the occurrence of severe acute complications of diabetes, such as DKA or hypoglycemia. These complications are very costly,16 but potentially preventable. Also as hypothesized, regardless of diabetes status, our study showed that disability-based enrollees experience higher excess mean expenditures than poverty-based enrollees. These excess expenditures were mainly attributable to higher expenditure on inpatient care, attributed to higher number of inpatient admissions, and longer average length of stay.
Our finding that a large proportion of per capita excess total medical expenditures accounted for by prescription drugs was consistent with those of studies among privately insured youth with diabetes,9 a small cohort of youth with type 1 diabetes at the Texas Children’s Hospital19 and among Swedish youth aged 14 years or below.18 Using data from presumed type 1 diabetes children enrolled in California Children’s Services program, Lee et al6 also found that diabetes-related expenditure on prescription drugs (insulin and supplies) was higher than outpatient care cost (outpatient clinic and emergency department visits), which is consistent with our results. The higher expenditure on prescription drugs in our study was mainly due to insulin use, which is costlier than oral medications. In addition to the insulin itself, these patients incur expenses on medical devices that are integral to diabetes management, such as insulin pumps, pens, syringes, glucose monitors and test strips, and glucagon, in the case of severe hypoglycemia.18 Lee et al6 estimated that the annual median cost for glucose monitoring supplies was over half of the cost incurred for insulin.
Among poverty-based enrollees, per capita diabetes-related medical expenditures were higher for older than younger individuals, and for females than for males, mainly attributed to higher expenditures on inpatient care resulting from longer stays and more admissions. Our results of higher cost for female than male mainly attributed to inpatient expenditure is consistent with Lee et al’s results.6 Programs aimed at reducing the number of hospitalizations in these groups may reduce costs associated with diabetes.
Our study showed that per capita diabetes-related medical expenditures among whites were lower than among blacks but higher than among other racial and ethnic groups, regardless disability status. The higher excess total expenditure among blacks than in whites was primary driven by the higher excess expenditure on inpatient care. However, whites incurred higher excess expenditures on prescription medications and outpatient care. This could be because white youth have a higher prevalence of type 1 diabetes than youth of minority groups,2 therefore, they are more likely to be on insulin treatment. A previous study of privately insured youth reported higher medical expenditures for youth on insulin as compared with those on oral agents.9
We previously estimated the excess diabetes-related medical expenditure among youth with private health insurance to be $8889 (at 2012US$).9 Excess medical expenditure among Medicaid-enrolled or CHIP-enrolled youth from our current study, compared with expenditure for youth with private health insurance, was higher by $377 (4%) for poverty-based and by $1297 (14%) for disability-based enrollees. However, the factors causing diabetes-related expenditure to be higher among publicly than privately insured youth remain unclear. A part of this discrepancy could be associated with higher out-of-pocket expenditures among persons with private health insurance than in persons with Medicaid coverage.
Another potential reason may be that youth covered by public insurance experience costly health services use, for example, for acute diabetes complications. Rewers et al20 reported that at the onset of diabetes, the prevalence of DKA was higher among youth of low-income households. Consistent with this, the occurrence of DKA or hypoglycemia in youth with diabetes who were treated with insulin in the current study was higher than that observed among privately insured youth in our previous study.16 The higher occurrence of DKA among youth under Medicaid coverage could also be associated with low continuity of primary care.21 Another reason to explain the expenditure discrepancy between privately and publicly insured youth could be that the study of privately insured youth was based on data from 2007,9 whereas our present study used data from 2008 to 2012. Previous studies comparing medical expenditures for other conditions such as sickle cell disease, autism spectrum disorder between Medicaid and private insurance have found inconsistent patterns depending on the diseases examined,22–24 suggesting that excess medical expenditure for public over private insurance coverage could be driven by benefits covered. Further research, using data from the same years and the same methods, could more accurately compare differences in costs between privately and publicly insured youth with diabetes.
This study has several limitations. First, the MarketScan multistate Medicaid database covered data from only about one fifth of the unidentified states in the country. We were, therefore, unable to examine the impact of state-specific eligibility criteria on the health services use and medical expenditures.24 Second, our sample population represents only those enrolled in fee-for-service plans; therefore, results may not apply to enrollees in capitated plans or managed care programs. Hence, our results may not be generalizable to the entire US youth population. Third, because of data limitation we could not estimate the costs by diabetes type, separating for those enrolled in CHIP and regular Medicaid enrollees, and could not include several nondiabetes-related comorbidities. Whether or not the inclusion of those enrolled in CHIP results in bias estimates for general Medicaid enrollees is not clear and needs further investigation. Fourth, the type of diabetes9,25 the severity of illness; duration of diabetes; place of residence16; and household income may affect the comparability of estimated costs. Finally, as in previous studies, we grouped those with only 1 outpatient visit indicating diabetes as nondiabetic to increase the positive predictive value.14 If some of those with only 1 outpatient diabetes visit indeed had diabetes, our estimated diabetes-related excess expenditure would be biased although the direction of the biases is not clear.
Our study showed that the per capita annual diabetes-related medical expenditures in youth covered by Medicaid or CHIP programs were substantial, expenditures were higher among those eligible based on disability than nondisability. This highlights the need for identifying effective ways of managing diabetes and its complications in this population. As Medicaid coverage and diabetes prevalence among youth continue to increase, our estimates may be used to evaluate the potential financial burden of diabetes on publicly funded Medicaid programs, to project health care resources needed for managing diabetes in youth, and to help guide the design and implementation of diabetes intervention programs aimed at improving care and reducing costs.
ACKNOWLEDGMENTS
The authors thank Tony Pearson-Clarke, the Health Writer-Editor and Karen R. Siegel, Orise Fellow at the Centers for Disease Control and Prevention, Atlanta for their editorial contributions.
Footnotes
The earlier version of the abstract was presented (oral) at American Diabetes Association’s 73rd Scientific Sessions, June 21–25, 2013 in Chicago, IL.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the US Centers for Disease Control and Prevention.
The authors declare no conflict of interest.
REFERENCES
- 1.Liese AD, D’Agostino RB, Jr, Hamman RF, et al. The burden of diabetes mellitus among US youth: prevalence estimates from the SEARCH for Diabetes in Youth Study. Pediatrics. 2006;118:1510–1518. [DOI] [PubMed] [Google Scholar]
- 2.Pettitt DJ, Talton J, Dabelea D, et al. Prevalence of diabetes in US youth in 2009: the SEARCH for diabetes in youth study. Diabetes Care. 2014;37:402–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vehik K, Dabelea D. The changing epidemiology of type 1 diabetes: why is it going through the roof? Diabetes Metab Res Rev. 2011;27:3–13. [DOI] [PubMed] [Google Scholar]
- 4.Department of Health and Human Services. Connecting kids to coverage: steady growth and new innovation. 2011 Chipra annual report. Available at: https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Childrens-Health-Insurance-Program-CHIP/Downloads/chip-annual-report-2011.pdf. Accessed January 23, 2017.
- 5.Cohen M. An overview of Medicaid enrollees with diabetes in 2003. Kaiser Commission on Medicaid and the Insured, October 2007. 2007.
- 6.Lee JM, Sundaram V, Sanders L, et al. Health care utilization and costs of publicly-insured children with diabetes in California. J Pediatr. 2015;167:449–454. e446. [DOI] [PubMed] [Google Scholar]
- 7.Kancherla V, Amendah DD, Grosse SD, et al. Medical expenditures attributable to cerebral palsy and intellectual disability among Medicaid-enrolled children. Res Dev Disabil. 2012;33:832–840. [DOI] [PubMed] [Google Scholar]
- 8.Burwell BCW, Drabek J. MEDSTAT Group. Chidren with severe chronic conditions on Medicaid. Prepared for office of disability, aging and long-term care policy office of the Assistant Secretary for Planning and Evaluation US Department of Health and Human Services Contract #HHS-100-92-0013. 1997. Available at: https://aspe.hhs.gov/sites/default/files/pdf/72876/children.pdf. Accessed January 23, 2017.
- 9.Shrestha SS, Zhang P, Albright A, et al. Medical expenditures associated with diabetes among privately insured US youth in 2007. Diabetes Care. 2011;34:1097–1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Medicare and Medicaid Services. Cost sharing out of pocket costs. Available at: www.medicaid.gov/medicaid-chip-program-information/by-topics/cost-sharing/cost-sharing-out-of-pocket-costs.html. Accessed January 23, 2017.
- 11.Guh S, Grosse SD, McAlister S, et al. Health care expenditures for Medicaid-covered males with haemophilia in the United States, 2008. Haemophilia. 2012;18:276–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Truven Health Analytics. MarketScan Research Databases: Commercial Claims and Encounters Medicare Supplemental Data, 2011 Edition User Guide. Ann Arbor, MI: Truven Health Analytics; 2012. [Google Scholar]
- 13.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. [DOI] [PubMed] [Google Scholar]
- 14.Hebert PL, Geiss LS, Tierney EF, et al. Identifying persons with diabetes using Medicare claims data. Am J Med Qual. 1999;14:270–277. [DOI] [PubMed] [Google Scholar]
- 15.Durden ED, Alemayehu B, Bouchard JR, et al. Direct health care costs of patients with type 2 diabetes within a privately insured employed population, 2000 and 2005. J Occup Environ Med. 2009;51:1460–1465. [DOI] [PubMed] [Google Scholar]
- 16.Shrestha SS, Zhang P, Barker L, et al. Medical expenditures associated with diabetes acute complications in privately insured US youth. Diabetes Care. 2010;33:2617–2622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Manning WG, Mullahy J. Estimating log models: to transform or not to transform? J Health Econ. 2001;20:461–494. [DOI] [PubMed] [Google Scholar]
- 18.Wirehn AB, Andersson A, Ostgren CJ, et al. Age-specific direct healthcare costs attributable to diabetes in a Swedish population: a register-based analysis. Diabet Med. 2008;25:732–737. [DOI] [PubMed] [Google Scholar]
- 19.Ying AK, Lairson DR, Giardino AP, et al. Predictors of direct costs of diabetes care in pediatric patients with type 1 diabetes. Pediatr Diabetes. 2011;12:177–182. [DOI] [PubMed] [Google Scholar]
- 20.Rewers A, Klingensmith G, Davis C, et al. Presence of diabetic ketoacidosis at diagnosis of diabetes mellitus in youth: the Search for Diabetes in Youth Study. Pediatrics. 2008;121:e1258–e1266. [DOI] [PubMed] [Google Scholar]
- 21.Christakis DA, Feudtner C, Pihoker C, et al. Continuity and quality of care for children with diabetes who are covered by Medicaid. Ambul Pediatr. 2001;1:99–103. [DOI] [PubMed] [Google Scholar]
- 22.Wang L, Mandell DS, Lawer L, et al. Healthcare service use and costs for autism spectrum disorder: a comparison between Medicaid and private insurance. J Autism Dev Disord. 2013;43:1057–1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ku L, Broaddus M. Public and private health insurance: stacking up the costs. Health Aff. 2008;27:w318–w327. [DOI] [PubMed] [Google Scholar]
- 24.Mvundura M, Amendah D, Kavanagh PL, et al. Health care utilization and expenditures for privately and publicly insured children with sickle cell disease in the United States. Pediatr Blood Cancer. 2009;53:642–646. [DOI] [PubMed] [Google Scholar]
- 25.Dall TM, Mann SE, Zhang Y, et al. Distinguishing the economic costs associated with type 1 and type 2 diabetes. Popul Health Manag. 2009;12:103–110. [DOI] [PubMed] [Google Scholar]