Abstract
Aims
The exact risk to patients undergoing surgery who develop COVID-19 is not yet fully known. This study aims to provide the current data to allow adequate consent regarding the risks of post-surgery COVID-19 infection and subsequent COVID-19-related mortality.
Methods
All orthopaedic trauma cases at the Wrightington Wigan and Leigh NHS Foundation Trust from ‘lockdown’ (23 March 2020) to date (15 June 2020) were collated and split into three groups. Adult ambulatory trauma surgeries (upper limb trauma, ankle fracture, tibial plateau fracture) and regional-specific referrals (periprosthetic hip fracture) were performed at a stand-alone elective site that accepted COVID-19-negative patients. Neck of femur fractures (NOFF) and all remaining non-NOFF (paediatric trauma, long bone injury) surgeries were performed at an acute site hospital (mixed green/blue site). Patients were swabbed for COVID-19 before surgery on both sites. Age, sex, nature of surgery, American Society of Anaesthesiologists (ASA) grade, associated comorbidity, length of stay, development of post-surgical COVID-19 infection, and post-surgical COVID-19-related deaths were collected.
Results
At the elective site, 225 patients underwent orthopaedic trauma surgery; two became COVID-19-positive (0.9%) in the immediate perioperative period, neither of which was fatal. At the acute site, 93 patients underwent non-NOFF trauma surgery, of whom six became COVID-19-positive (6.5%) and three died. A further 84 patients underwent NOFF surgery, seven becoming COVID-19 positive (8.3%) and five died.
Conclusion
At the elective site, the rate of COVID-19 infection following orthopaedic trauma surgery was low, at 0.9%. At the acute mixed site (typical district general hospital), for non-NOFF surgery there was a 6.5% incidence of post-surgical COVID-19 infection (seven-fold higher risk) with 50% COVID-19 mortality; for NOFF surgery, there was an 8.3% incidence of post-surgical COVID-19 infection, with 71% COVID-19 mortality. This is likely to have significance when planning a resumption of elective orthopaedic surgery and for consent to the patient.
Cite this article: Bone Joint Open 2020;1-9:556–561.
Keywords: COVID-19, Consent, Elective orthopaedic surgery
Introduction
Following the complete cessation of elective orthopaedic surgery in the UK in response to the national COVID-19 pandemic, now with a steady reduction in COVID-19 infection rates, attention has been drawn to planning for a potential gradual resumption of elective surgical activity. However, not only does this entail hospital process best planning and management, but it necessitates, in the current post-Montgomery era, ‘true’ informed patient consent. Current consent guideline documents, as of the time of writing this article, from the European Society of Sports Traumatology, Knee Surgery and Arthroscopy (ESSKA) and the British Association of Spine Surgeons (BASS),1,2 are somewhat nebulous, reporting some increased risk to the patient with surgery in the current COVID-19 climate. While this provides some information to the patient, it does not provide sufficient detail medico-legally for the patient to form a ‘true, balanced opinion’ and will, in all likelihood, provide an opportunity for litigious challenge should subsequent post-surgical fatal COVID-19 infection ensue. Would the patient really have agreed to surgery, at that particular time if they knew, for example, that post-surgical COVID-19 infection rates were 5%, with a 50% mortality, or would they have waited and deferred their surgery to a later date? The aim of this article is to provide accurate current data, both for the patient and the surgeon, regarding the risk of post-surgery COVID-19 infection and the risk of this causing subsequent COVID-19-related mortality, in light of the current COVID-19 national and hospital precautions.
Methods
Data from all orthopaedic trauma procedures performed at Wrightington Wigan and Leigh NHS Foundation Trust were prospectively collected from ‘lockdown’ (23 March 2020) to date (15 June 2020). We recorded patient age, sex, nature of surgery, American Society of Anaethesiologists (ASA) grade, associated medical comorbidity, length of hospital stay, development of post-surgical COVID-19 infection, and the number of post-surgical COVID-19-related deaths. The study was registered with our Foundation Trust’s audit department. Statistical analysis was performed using Stata (v15.1, StataCorp, College Station, Texas, USA). Statistical significance was set at p = 0.05.
The trust consists of two surgical orthopaedic sites. Wrightington Hospital is a 12-theatre, specialist elective orthopaedic institute, which provides an elective orthopaedic service to the North West of England and beyond. It performs around 3000 arthroplasties per year. Wigan Hospital is the acute site, comprising an accident and emergency (A&E) department, medical services, and an intensive care unit, and which provides the orthopaedic trauma services to the local population. Following the commencement of lockdown and the start of this study period, with the cessation of all elective orthopaedic surgery, there was a reconfiguration of the orthopaedic provision. All acute fractures initially continued to be seen at the A&E department on the Wigan site. The patients underwent nose/throat swab polymerase chain reaction (PCR) testing for the CoV-2 antigen. Adult ambulatory fracture cases (upper limb fracture, lower limb foot and ankle fracture, tibial plateau fracture), together with regional tertiary emergency referrals (periprosthetic fracture and complex upper limb trauma) that were COVID-19 negative, underwent their surgery at Wrightington. All hip fracture cases, long bone injuries requiring intramedullary nailing, and all paediatric trauma cases underwent their surgery at Wigan.
Wrightington also became the site for urgent soft-tissue breast surgery/cancer cases, which was also included in the data collection. Finally, we prospectively collected data for the number of ‘medical’ COVID-19 infections presenting to the Wigan site, and how many of these patients died of COVID-19 illness, to assess whether there was a difference between ‘surgical’ and ‘medical’ COVID-19 mortality rates.
Results
Tables I–VI provide the data results. At the elective stand-alone site (Wrightington), there were 225 orthopaedic trauma operations performed during the study period. Two patients became COVID-19-positive (0.9%) in the immediate perioperative period, neither of whom died. One patient died of a non-COVID-19-related cause. For the purely soft-tissue cases (urgent breast cases) also performed at Wrightington, 74 procedures were performed with no perioperative COVID-19 infections. At the acute site (Wigan), there were 84 neck of femur fracture (NOFF) cases. Seven of these (8.3%) became COVID-19-positive and five of these patients unfortunately died from COVID-19-related complications. There were an additional 13 patients (15.5%) who died of non-COVID-19-related causes. There were 93 non-NOFF orthopaedic cases performed on the Wigan site, of which six patients became COVID-19-positive (6.5%) and three died of COVID-19-related complications. There were an additional four patients (4.3%) who died of non-COVID-19-related causes. Table VI reports the number of complex trauma cases and periprosthetic fractures performed across the two sites. On the elective site, 10.2% of the trauma surgeries (23/225) were complex (intramedullary nailing, open reduction internal fixation pilon, tibial plateau, distal femur or proximal humerus), 4% (9/225) were for periprosthetic fracture of which two patients became COVID-19-positive postoperatively (22% of these cases), and there was one manipulation of a dislocated total hip arthroplasty (THA). At the acute site, 10.8% of the trauma surgeries were complex (10/93), of which one patient became COVID-19-positive postoperatively, and 3.2% (3/93) were for periprosthetic fracture (of which one patient became COVID-19-positive postoperatively). There were 13 manipulations of a dislocated THA (14.0% cases), of which three patients became COVID-19-positive postoperatively (23.1% of these cases).
Table I.
Patients at Wrightington stand-alone site undergoing orthopaedic trauma surgery.
| Wrightington (n = 225) | Sex | Age/years (range) | ASA grade | Length of stay/days (range) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Male | Female | LA | 1 | 2 | 3 | 4 | |||
| COVID-19-negative | 127 | 96 | 51 (16 to 89) |
38 | 73 | 85 | 27 | 0 | 0.9 (D/C to 21) |
| COVID-19-positive and survived | 0 | 2 | 79 (72 to 85) |
0 | 0 | 1 | 1 | 0 | 3 (2 to 4) |
| COVID-19-positive and died | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | _ |
ASA, American Society of Anaesthesiologists; LA, Local Anaesthetic; D/C, Day Case
Table VI.
Overview for case mix breakdown of patients at the elective and acute sites undergoing orthopaedic trauma surgery (non neck of femur fracture cases). Complex trauma is defined as intramedullary nailing, ORIF pilon fracture, tibial plateau, distal femur or proximal humerus.
| Wrightington (n = 225) | Number of cases | COVID-19-positive | COVID-19 death |
|---|---|---|---|
| Complex trauma | 23 | 0 | 0 |
| Periprosthetic fracture | 9 | 2 | 0 |
| MUA dislocated THA | 1 | 0 | 0 |
| Other | 192 | 0 | 0 |
| Wigan (n = 93) | |||
| Complex trauma | 10 | 1 | 0 |
| Periprosthetic fracture | 3 | 1 | 0 |
| MUA dislocated THA | 13 | 3 | 3 |
| Other | 67 | 1 | 0 |
MUA, manipulation under anaesthetic; THA, total hip arthroplasty.
Table II.
Patients at the mixed Wigan site undergoing non-NOFF trauma surgery.
| Wigan (n = 93) | Sex | Age/years (range) | ASA grade | Length of stay/days (range) | ||||
|---|---|---|---|---|---|---|---|---|
| Male | Female | 1 | 2 | 3 | 4 | |||
| COVID-19-negative | 46 | 41 | 46 (3 to 93) |
33 | 27 | 26 | 1 | 2.4 (D/C to 27) |
| COVID-19-positive and survived | 1 | 2 | 69 (51 to 85) |
0 | 0 | 3 | 0 | 13.3 (8 to 24) |
| COVID-19-positive and died | 0 | 3 | 85 (83 to 91) |
0 | 1 | 2 | 0 | 7.7 (2 to 17) |
NOFF, Neck of femur fracture; ASA, American Society of Anaesthesiologists; D/C, day case.
Table III.
Patients at the mixed Wigan site undergoing NOFF trauma surgery.
| Wigan (n = 84) | Sex | Age/years (range) | ASA grade | Length of stay/days (range) | ||||
|---|---|---|---|---|---|---|---|---|
| Male | Female | 1 | 2 | 3 | 4 | |||
| COVID-19-negative | 28 | 49 | 80 (44 to 99) |
0 | 12 | 52 | 13 | 9.8 (3 to 33) |
| COVID-19-positive and survived | 1 | 1 | 81 (73 to 88) |
0 | 0 | 2 | 0 | 15.5 (9 to 22) |
| COVID-19-positive and died | 3 | 2 | 86 (81 to 95) |
0 | 0 | 3 | 2 | 14.2 (4 to 34) |
ASA, American Society of Anaesthesiologists; NOFF, neck of femur fracture.
Table V.
Overview on patients at theWrightington and Wigan sites undergoing orthopaedic trauma surgery.
| Sex | Age/years (range) | ASA grade | Non-COVID-19 | COVID-19 | p-value* | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | LA | 1 | 2 | 3 | 4 | |||||
| Wrightington | 56% | 44% | 51 (16 to 89) |
38 | 73 | 86 | 28 | 0 | 223 | 2 | |
| Wigan non-NOFF | 51% | 49% | 48 (3 to 91) |
0 | 33 | 27 | 32 | 1 | 87 | 6 | 0.009 |
| Wigan NOFF | 38% | 62% | 81 (44 to 99) |
0 | 0 | 12 | 57 | 15 | 77 | 7 | 0.78 |
Fisher’s exact test.
ASA, American Society of Anaesthesiologists; NOFF, neck of femur fracture; LA, local anaesthetic.
From our data, the overall rate of post-surgical COVID-19 infection at the acute site (Wigan) was 7.3% (13/177), with a COVID-19 mortality rate of 62%. Analysis of the rate of ‘medical’ COVID-19 mortality at Wigan Hospital during the same period confirmed 529 medical cases of COVID-19 admitted to the hospital, of which 235 patients died (44% mortality). For the elective site (Wrightington), however, the rate of post-surgical COVID-19 infection was 0.7% (2/299), with a COVID-19 mortality rate of 0% (Tables I and IV).
Table IV.
Patients at the Wrightington stand-alone site undergoing urgent ‘elective’ soft-tissue breast surgery.
| Wrightington (n = 74) | Sex | Age/years (range) | ASA grade | Length of stay | ||||
|---|---|---|---|---|---|---|---|---|
| Male | Female | 1 | 2 | 3 | 4 | |||
| COVID-19-negative | 0 | 74 | 59.7 (39 to 83) |
13 | 54 | 7 | 0 | D/C |
| COVID-19-positive and survived | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| COVID-19-positive and died | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
ASA, American Society of Anaesthesiologists; D/C, day case.
We noted that all the COVID-19 infections occurred across both sites during the early study period, when the prevalence of COVID-19 infection in the community was at its peak, with no post-surgical COVID-19 infections occurring at either site during the last 18 days of study, despite 21% of the cases being performed during this time period.
Discussion
When a resumption of elective orthopaedic surgery occurs, it is imperative to give some quantification to any potential increased patient risk of post-surgical COVID-19 infection in order to satisfy ‘modern’ consent. The authors are aware of only one clinical paper to date that attempts to quantify this risk, from the Galeazzi Institute, Milan, Italy,3 which reported, just at the time of Italian lockdown, that 2.5% of all of their admissions for elective orthopaedic surgery subsequently became symptomatic and COVID-19-positive in the immediate perioperative period. Further reports have suggested that patients who developed COVID-19 in this early postoperative period show around a 20% mortality rate,4,5 with patients of ASA grade 3 or 4 particularly vulnerable (odds ratio (OR) of 2.35).5,6 Other reports have identified other risk factors including age > 70 years (OR 2.30), male sex (OR 1.75), comorbidity, being immunocompromised, and obesity.6-8
In this paper, we have attempted to collate the risk to patients of developing the COVID-19 infection from hospital admission and surgical procedure and then how many cases result in a specifically COVID-19-related death. Results from our study have shown that on an elective site, with current COVID-19 screening practices (COVID-19-negative on admission), in the current climate, the rate of subsequent COVID-19 infection following orthopaedic surgery is very low, at 0.9%. Furthermore, for those patients undergoing purely soft-tissue, day-case surgery (urgent breast surgery), the rate of subsequent COVID-19 infection was 0%. While this subgroup of patients arguably had higher risk factors (some patients had cancer), these data would be relevant to orthopaedic surgeons undertaking elective soft-tissue and arthroscopic surgery. No patient in either of these groups died from COVID-19-related infection.
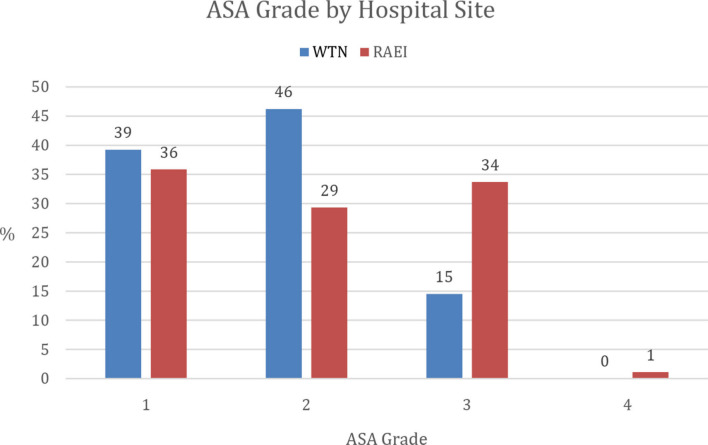
We note that on the acute site (typical district general hospital), those patients undergoing non-NOFF orthopaedic trauma surgical procedures had a 6.5% incidence of subsequent COVID-19 infection (seven times higher risk than the elective site), with a 50% COVID-19 mortality rate, which was significantly higher when compared with the elective site (Fisher’s exact test; p = 0.009). Subanalysis of this group found no significant difference in the known risk factors of age and sex when compared with the group of patients undergoing trauma surgery on the elective site. While the median ASA for both of these groups was also identical (ASA 2), the distributions were significantly different (two-sample Mann-Whitney test p = 0.025), with the elective site having a higher proportion of ASA 2 patients (46% vs 29%) and a lower proportion of ASA 3 patients (15% vs 34%) (Figure 1). When surgical case mix across the two sites was compared (Table VI), there was no significant difference between numbers of complex trauma (10.2% vs 10.8%; elective to acute sites) and periprosthetic fracture cases (4% vs 3.2%; elective to acute sites). It is concerning to note, however, that there was such a high number of post-surgical COVID-19 infections at the acute site from a minor surgical procedure such as manipulation of dislocated THA (3/13), which suggests that COVID-19 risk is a complex interaction, and that medical comorbidity, being immunocompromised, and age may have a stronger overall COVID-19 risk than complexity of surgery. The authors acknowledge further work needs to be performed on this.
Fig. 1.
Depicting percentage distribution of patients undergoing orthopaedic trauma surgery across the two sites as determined by American Society of Anaesthesiologists (ASA) grade. WTN, Wrightington elective site; RAEI , Wigan site.
The risk for NOFF surgery and subsequent COVID-19 infection on an acute site was unfortunately even higher at 8.3%, which reflects both an increase in the group risk factors of age, ASA, and comorbidity, and the fact that these patients were in hospital for a longer period. The COVID-19 mortality rate for this group was also higher at 71%.
Kader et al9 estimated the theoretical risk of a COVID-19 death following elective orthopaedic surgery to be roughly one in 7,000. However, in calculating this estimation, these authors did not account for the risk of nosocomial COVID-19 infection and used the case fatality rate of 20.5% as documented by Lei et al5 who reports only on a series of 34 patients undergoing elective surgical procedures. Our data for orthopaedic trauma surgery from the acute hospital site demonstrate that overall COVID-19 surgical fatality rates may be much higher. However, from an elective site, the risk of COVID-19 surgical infection and mortality may be much lower. This illustrates the difficulties in estimating the theoretical risk of COVID-19 death with elective surgery when counselling patients.
Analysis of the post-surgical COVID-19 mortality figures against general medical COVID-19 mortality rates for the acute site hospital during the same three-month period confirmed a lower medical COVID-19 mortality rate, at 44%, when compared with the post-surgical COVID-19 mortality rate (62%). This may suggest that there is a role of either the surgical procedure or the general anaesthetic in increasing the risk to the surgical patient.8
Of the patients who died from COVID-19 following orthopaedic surgery during the study period (2.0%; 8/402), there were no deaths following local anaesthetic procedures or in those patients with ASA grade 1. Of the total deaths, 88% were in ASA grade 3 or 4 (Tables I–IV), which concurs with the evidence from others.3-8
Of particular note was that there were no post-surgical COVID-19 infections in any of the groups at either site for the last 18 days of the data, despite this accounting for 21% of our data. Review of the Government Public Health England figures confirms the peak infection rate for the North West region to have been mid-April, with the death rate at the beginning of May running at around 63% of peak and gradually reducing such that, by the end of our study period (mid-June), it was 24% of peak.10 This may suggest that the prevalence level of COVID-19 in the community is a factor in increasing the risk to the surgical patient. This could have significant implications again for elective surgery if there is a ‘second peak’ of community COVID-19 infections, and highlights the importance of proper screening processes and green pathways as described by the British Orthopaedic Association (BOA).11
This study has a number of limitations. First, we acknowledge that this paper provides data early within the timeline of the coronavirus pandemic and that not all areas reach statistical significance. Secondly, while patients undergoing surgery on the elective site were tested preoperatively for COVID-19, the staff, in particular the orthopaedic surgical staff, were not tested routinely for COVID-19 unless they became symptomatic. As, during the study period, they worked across both sites, they could potentially have become unwitting asymptomatic carriers. It is known that asymptomatic carriers have similar viral loads in their upper respiratory tract to those of symptomatic patients, and can therefore spread COVID-19 with similar virulence, so there is an argument for the regular testing of hospital medical staff working across such sites to confirm their negative status rather than rely just on presence of symptoms (fever, cough, anosmia) in order to maintain safety.12 Nonetheless, the very low rate of COVID-19 contraction on the elective site with orthopaedic surgery (0.9%) and with soft-tissue surgery (0%) indicated that, practically, this risk may be very low. Thirdly, we acknowledge that only relying only on positive swabs postoperatively to count COVID-19-positive cases postoperatively is a methodological flaw.
Furthermore, we only have results of postoperative COVID-19 contraction if patients became sufficiently symptomatic to necessitate a re-attendance at our A&E department or developed symptoms while in hospital. We acknowledge that some patients potentially may have subsequently either contracted COVID-19 and re-attended another A&E department, or contracted mild COVID-19 but not presented to hospital. If this were the case, then potentially the COVID-19 post-surgical infection rate may be actually higher than our data suggest (albeit the mortality rate would then be lower).
In conclusion, therefore, these results provide data both for patient COVID-19 consent and evidence to suggest that the use of an elective site, with established green pathways, can significantly reduce the risk of subsequent COVID-19 infection after surgery when compared with acute sites. This has immense implications for the NHS when planning any resumption of elective orthopaedic surgical activity. We hope these data will inform the commencement of elective surgery and strengthen the green pathway strategy as described by the BOA. These recommendations should be considered along with other existing recommendations, including keeping hospital visitations to a minimum. Regular screening of staff members, while potentially having implications on workforce planning and operational capacity, should be deemed good medical practice and is to be recommended.
Take home message
- Post-surgical COVID-19 risk appears to be much lower on an elective ‘stand-alone’ site than a mixed acute site.
- Rate of post-surgical COVID-19 infection at an elective ‘stand alone’ site following surgery, with current COVID precautions, particularly for day case or ASA 1 and 2 cases is very low.
Acknowledgements
The authors would like to thank the Trust Audit Department for their help and work in providing the data for analysis.
Footnotes
Author contributions: T. M. Clough: Wrote, edited, and proofread the manuscript.
N. Shah: Edited the manuscript.
H. Divecha: Helped to edit manuscript, Carried out statistical analysis.
S. Talwalkar: Edited the manuscript.
Funding statement: No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
ICMJE COI statement: T. M. Clough reports consultancy agreements with Wright MedicaL Arthrex, and OrthoSolutions, which are unrelated to this article. S. Talwalkar reports that the organisation may be reimbursed for the journal fees by the trust.
Ethical review statement: The study was registered with the Wrightington Wigan and Leigh NHS Foundation Trust.
References
- 1. No authors listed COVID-19 - ESSKA Guidelines and Recommendations for Resuming Elective Surgery. European Society of Sports Traumatology, Knee Surgery & Arthroscopy (ESSKA). 2020. https://cdn.ymaws.com/www.esska.org/resource/resmgr/covid-19/COVID-guidelines-Q&A.pdf (date last accessed 30 June 2020).
- 2. No authors listed Information for patients undergoing surgery during the coronavirus pandemic. BASS consent SARS-CoV-2. British Association of Spine Surgeons (BASS). 2020. https://spinesurgeons.ac.uk/resources/Documents/Member%20News/200514-BASS-ConsentCOVID.pdf (date last accessed 30 June 2020).
- 3. Zagra L, Faraldi M, Pregliasco F, Vinci A, Lombardi G, et al. Changes of clinical activities in an orthopaedic institute in North Italy during the spread of COVID-19 pandemic: a seven-week observational analysis. Int Orthop. 2020;44(8):1591–1598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. D’Apolito R, Faraldi M, Ottaiano I, Zagra L. Disruption of Arthroplasty Practice in an Orthopedic Center in Northern Italy During the Coronavirus Disease 2019 Pandemic. J Arthroplasty. 2020;35(7S):S6–S9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lei S, Jiang F, Su W, et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine. 2020;21:100331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. COVIDSurg Collaborative Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020;396(10243):27–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. No authors listed Coronavirus Disease 2019 (COVID-19): People with Certain Medical Conditions. Centers for Disease Control and Prevention (CDC). 2020. https;//www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/groups-at-higher-risk.html (date last accessed 29 June 2020).
- 8. Oussedik S, Zagra L, Shin GY, D’Apolito R, Haddad FS. Re-instating elective orthopaedic surgery in the age of COVID-19. Bone Joint J. 2020;102-B(7):807–810. [DOI] [PubMed] [Google Scholar]
- 9. Kader N, Clement ND, Patel VR, Caplan N, Banaszkiewicz P, Kader D. The theoretical mortality risk of an asymptomatic patient with a negative SARS-CoV-2 test developing COVID-19 following elective orthopaedic surgery. Bone Joint J. 2020;102-B(9):1256–1260. [DOI] [PubMed] [Google Scholar]
- 10. No authors listed Coronavirus (COVID-19) in the UK. Gov.UK. 2020. https://coronavirus.data.gov.uk/#category=regions&map=rate&area=e12000002 (date last accessed 29 June 2020).
- 11. No authors listed Re-starting non-urgent trauma and orthopaedic care: full guidance. British Orthopaedic Association (BOA). 2020. https://www.boa.ac.uk/uploads/assets/9383a53f-36d8-4782-8fe264c691b39b15/BOA-Guidance-for-restart-full-doc-final2-v11.pdf (date last accessed 15 July 2020).
- 12. Mueller M, Boettner F, Karczewski D, et al. Dealing with the COVID-19 pandemic in orthopaedics: experiences and procedure in Germany. Bone Joint Open. 2020;1(6):309–315. [DOI] [PMC free article] [PubMed] [Google Scholar]