Abstract
Aims
Healthcare systems have been rapidly restructured to meet COVID-19 demand. Clinicians are working to novel clinical guidelines, treating new patient cohorts and working in unfamiliar environments. Trauma and orthopaedics (T&O) has experienced cancellation of routine clinics and operating, with redistribution of the workload and human resources. To date, no studies have evaluated the mental health impact of these changes on the T&O workforce. We report the results of a novel survey on the impact of the pandemic on the mental health of our orthopaedic workforce and the contributory factors.
Methods
A 20-question survey-based cross-sectional study of orthopaedic team members was conducted during the COVID-19 pandemic. The primary objective was to identify the impact of the pandemic on mental health in the form of major depressive disorder (MDD) and general anxiety disorder (GAD). The survey incorporated the patient health questionnaire (PHQ-2), which is validated for screening of MDD, and the generalized anxiety disorder questionnaire (GAD-2), which is validated for screening of GAD.
Results
There were 62 respondents (18 females and 44 males). As compared to the general population, we noted a greater estimated prevalence of GAD (17.7% vs 5.9%, p = 0.0009297) and MDD (19.4% vs 3.3%, p = 0.0000007731). The prevalence of MDD symptoms was greatest among senior house officers (SHOs) (p = 0.02216). Female respondents scored higher for symptoms of MDD (p = 0.03583) and GAD (p = 0.0001086). Those identifying as ‘Black, African, Caribbean or Black British’ displayed a higher prevalence of GAD symptoms (p = 0.001575) and felt least supported at work (p = 0.001341).
Conclusion
Our study, in the first of its kind, shows a significant prevalence of GAD and MDD in the workforce. We found that SHOs, females and those of Black, African, Caribbean, or Black British origin were disproportionately affected. Action should be taken to help prevent adverse mental health outcomes for our colleagues during the pandemic.
Cite this article: Bone Joint Open 2020;1-6:316–325.
Keywords: mental health, depression, anxiety, orthopaedics, Covid 19, pandemic
Introduction
The COVID-19 pandemic has taken its toll on the wellbeing of patients across the world, with 4.5 million confirmed cases worldwide at the time of writing.1 Certainly, healthcare professionals are not immune to the physical or mental health impact of the pandemic. Research around COVID-19 focuses predominantly on physical health, but the mental health impact of this infection may be far wider reaching than expected and should not be neglected. Physicians are dealing with unprecedented demand for healthcare services that are struggling to cope, and this places a significant burden on their shoulders. During the pandemic orthopaedic surgeons have faced a reduction in routine workload, with widespread cancellation of elective operations and outpatient consultations, and an observed decline in acute trauma presentations. Instead, we have seen orthopaedic surgeons across the world re-assigned to duties which place them out of their area of expertise and beyond their comfort zone, such as covering emergency departments, intensive care units or medical COVID-19 wards. We therefore explore the impact of these changes on orthopaedic team members’ mental health during the COVID-19 pandemic.
To our knowledge, to date, there are no other studies that have investigated the mental health impact of the COVID-19 pandemic on the trauma and orthopaedic (T&O) workforce. However, studies have previously shown that poor mental health can result in reduced productivity, increase in sick leave and lower job satisfaction.2 Most importantly, there was a correlation with human errors which, in a surgical speciality, can be particularly concerning.3,4 Furthermore, studies have also shown a correlation between increasing physician burnout and patient dissatisfaction.5,6
The authors, therefore, hope to shed light on the impact of the pandemic on the mental health of our orthopaedic workforce and to explore the contributory factors. Through raising awareness of these issues, there is an opportunity to take action before there is a significant detriment to the workforce and our patients.
Methods
The authors conducted a survey-based cross-sectional study of orthopaedic team members across the UK during the COVID-19 pandemic. The survey was kept brief (20 questions) to promote completion.
The primary objective was to identify and characterise the impact of the pandemic on mental health in the form of major depressive disorder (MDD) and general anxiety disorder (GAD). We also aimed to identify other factors in the workplace that may have adversely impacted on mental health. Demographic data was collected including sex, age, clinical grade, and ethnicity to identify subgroups which were most affected.
The nine-question patient health questionnaire (PHQ-9) is a self-administered questionnaire validated for the assessment of major depressive disorder as per the diagnostic and statistical Manual of Mental Disorders 4 (DSM-IV) criteria in primary care settings. The first two questions, known as the PHQ-2 can be used for screening. PHQ-2 score greater than 2 has sensitivity of 82.9% and specificity of 90.0% for MDD.7
The seven-item generalized anxiety disorder questionnaire (GAD-7), is a self-administered questionnaire validated for the assessment of GAD. For screening, the first two items known as GAD-2 have been shown to have a sensitivity of 86% and specificity of 83% for GAD.8
The PHQ-2 and GAD-2 were included in the survey to estimate the prevalence of MDD and GAD in the responders.
A question on previously seeking treatment for mental health conditions was included to explore if past experiences sensitised respondents to current stressors. Respondents were allowed to abstain from answering. Abstainers were treated as having not sought treatment previously.
A series of questions were constructed on potential stressors related to changes in the workplace due to COVID-19 assessed on a four-point Likert scale. These included: fear of contracting COVID-19; access to personal protective equipment; increase in workload pressure; uncertainty about the impact that COVID-19 might have on patient management; concern that redeployment might mean staff are less confident in their new roles; and concern about the impact changes might have on career and training progression.
We included a series of questions assessing the subjective thoughts in responders, assessing on a four-point Likert scale their ability to be open with their colleagues about current difficulties if they believed their mental health had impacted their behaviour in the workplace, if they had considered taking time off work due to mental health and if they felt supported in their workplace.
Finally, we also identified those who had sought wellbeing services during the pandemic and if this had any impact on their mental health. Respondents were allowed to abstain from answering. Abstainers were treated as having not sought support from wellbeing services.
The survey was distributed through multiple channels to reach as many doctors as possible, including email and social media. The NHS Research Ethics Committee decision tool excluded the need for ethics review. Participation was voluntary and all respondents gave consent for their data to be included for research purposes. The survey concluded with information signposting all respondents to wellbeing services.
Results
We received 62 response;, 44 (71.0%) were male and 18 (29.0%) were female. Further breakdown by demographics is shown in Table I.
Table I.
Breakdown of the demographics of survey respondents.
| Number of respondents | Percentage (%) | |
|---|---|---|
| Total number of respondents | 62 | 100 |
| Gender | ||
| Female | 18 | 29.0 |
| Male | 44 | 71.0 |
| Age (years) | ||
| 20 to 34 | 32 | 51.6 |
| 35 to 49 | 21 | 33.9 |
| 50 to 69 | 9 | 14.5 |
| Grade | ||
| Senior house officer (SHO) | 9 | 14.5 |
| Registrar | 33 | 53.2 |
| Fellow | 5 | 8.1 |
| Associate specialist | 7 | 11.3 |
| Consultant | 8 | 12.9 |
| Ethnicity | ||
| Asian | 26 | 41.9 |
| White | 23 | 37.1 |
| Black / African / Caribbean / Black British | 7 | 11.3 |
| Mixed / Multiple ethnic groups | 5 | 8.1 |
| Undisclosed | 1 | 1.6 |
We found that seven (11.3%) had previously sought treatment for a mental health condition, seven (11.3%) had accessed wellbeing services in the past, and seven (11.3%) had considered taking time off work as a result of their mental health during the pandemic.
Statistical analysis was performed between subgroups; sex, race, age, grade, those that had previously sought treatment for mental health conditions, and those that had accessed wellbeing services during the pandemic. Since, in no case were both groups’ data normal under the Shapiro-Wilkes test, the Mann-Whitney U test with continuity correction was used to compare subgroup responses to questions assessed on the Likert scale.
SHOs had a higher PHQ-2 score when compared to other doctors (p = 0.02216). There was no other significant difference in their response to the questions. Registrars had a lower GAD-2 score when compared to other doctors (p = 0.02059). There was no other significant difference in their response to the questions. Associate specialists had lower scores for concern about training than other grades (p = 0.01234).
Compared to males, females had higher scores in; PHQ-2 (p = 0.03583), GAD-2 (p = 0.0001086), concerns about contracting COVID-19 at work (p = 0.02235), concern about increased pressure in the workplace (p = 0.0006537), concerns about redeployment (p = 0.003701), felt less able to be open with colleagues about their mental health (p = 0.03573), and felt less supported in the workplace (p = 0.03382).
Those who previously sought treatment for a mental health condition scored higher on the PHQ-2 test (p = 0.04961) and were more concerned about training and career progression (p = 0.04266). Those who had previously accessed wellbeing services were more concerned about how COVID-19 affected the management of patients (p = 0.04215) and were more concerned about training and career progression (p = 0.02659).
Compared to other ethnicities, those that identified as 'Black/African/Caribbean/Black British' had higher GAD-2 scores (p = 0.001575) and felt less supported in the workplace (p = 0.001341). Those that identified as 'White' were less likely to think about taking time off sick for their mental health (p = 0.04946).
Compared to those who scored less than 3 on the PHQ-2, those that scored 3 or more, had a higher GAD-2 score (p = 0.002548), scored that they were more concerned about workload pressures (p = 0.02454), felt that their behaviour had been impacted more (p = 0.0004031) and felt less supported in the workplace (p = 0.02683).
Compared to those who scored less than 3 on the GAD-2, those that scored 3 or more, had a higher PHQ-2 score (p = 0.006325), scored higher on concern about catching COVID-19 from the workplace (p = 0.03912), higher for concern about workload pressures (p = 0.0002035), felt that their behaviour had been impacted (p = 0.03554), and felt less supported in the workplace (p = 0.01234).
A two-sided exact binomial test found that the proportion of responders that scored 3 or more on GAD-2 (17.7%) was higher than the national prevalence of GAD (5.9%) (p = 0.0009297) and that the proportion of responders who scored 3 or more on the PHQ-2 (19.4%) was also higher than the national prevalence of MDD (3.3%) (p = 0.0000007731).9
A two proportion Z test was used to compare subgroup rates of scoring 3 or more on PHQ-2 or GAD-2. Females were more likely than males to score 3 or more on GAD-2 (p = 0.00161) and PHQ-2 (p = 0.004453). Those that had previously sought treatment for a mental health condition were more likely to score 3 or more on the PHQ-2 (p = 0.02934).
Multiple logistic regression was used to identify correlation between GAD-2/PHQ-2 scores and other Likert assessed questions. GAD-2 scores showed a positive correlation with scoring of workplace pressure (R2 = 0.2871 p = 0.000007186). PHQ-2 scores showed a positive correlation with the feeling that workplace behaviour had been impacted (R2 = 0.238 p = 0.000005783).
Discussion
There were 62 respondents to our survey, with over twice as many males than females taking part. Data from the British Orthopaedic Trainees Association currently estimates that 5% of the consultant body is female and approximately 25% of all newly appointed trainees are female. A two-sided exact binomial test showed that these figures were not significantly different to the response rate of our survey: none of the consultants were female (p = 0.2139) and 21.2% of the registrars were female (p = 0.6929).
Our data showed that the estimated likely prevalence of generalized anxiety disorder and major depressive disorder in our cohort was significantly greater than in the general population (p = 0.0009297 and p = 0.0000007731 respectively).
It is unclear from our survey whether this is a direct impact of the COVID-19 pandemic. Indeed, there may be other confounding factors not assessed in our survey, such as the general stressors of a surgical job, which may influence these results. However, a prevalence of GAD in our cohort that is almost three times greater than in the general population (17.7% vs 5.9%) and of MDD which is almost six times greater than in the general population (19.4% vs 3.3%) cannot be ignored regardless of the cause.
Senior House Officers (SHOs)
Our study found that symptoms of major depressive disorder were significantly more prevalent among SHOs, regardless of sex, as compared to all other grades of doctor (Figure 1). The SHO cohort, being the most junior grade of doctor within most orthopaedic departments, are likely to be the group placed under the most stress during the pandemic. As departments are restructured to meet the demand for COVID-19 patients, this cohort is likely to be re-allocated for roles beyond their usual practice. It is therefore unsurprising that those who recorded higher PHQ-2 scores were significantly more concerned about workload pressures. Those responsible for SHO rotas should be conscious of this and ensure that they are compliant with the 2016 junior doctors contract, which mandates appropriate rest periods and can thereby potentially prevent burnout. Although our survey did not demonstrate any correlation in the SHO cohort with regards to considering time off work for their mental health, excess workloads could contribute to deterioration in physical health and lead to a vicious cycle of rota gaps and overwork.10 A number of organisations, including the British Medical Association, have signposted a range of useful wellbeing resources to help junior doctors manage the impact of the pandemic on their physical and mental health.11
Fig. 1.
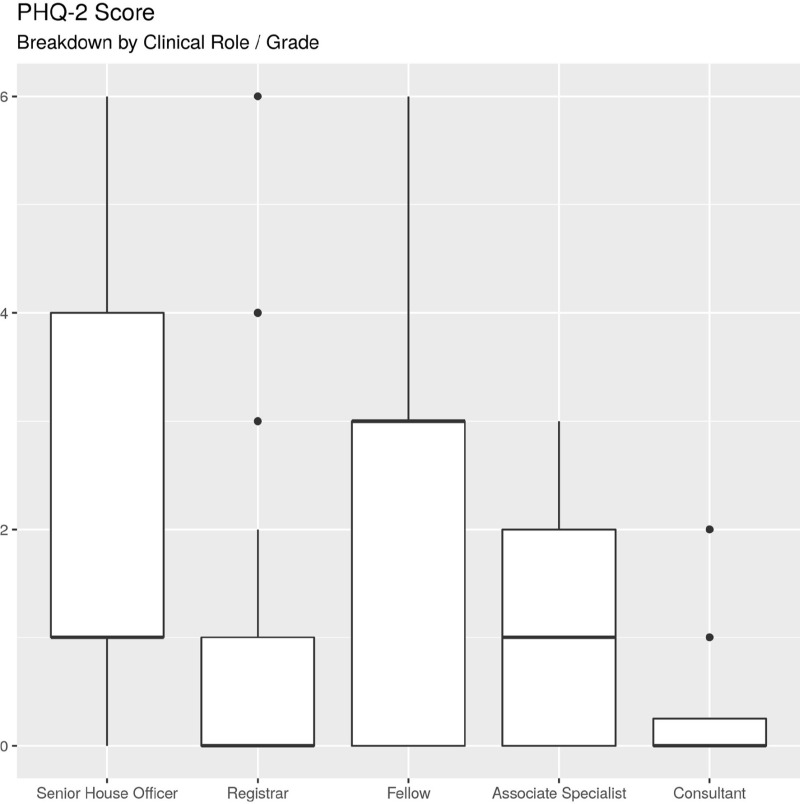
Boxplot showing PHQ-2 by grade, SHOs had a higher PHQ-2 score when compared to other doctors (p = 0.02216).
Registrars
We found that significantly fewer registrars displayed symptoms of anxiety as compared to all other grades of doctor (Figure 2). It is unclear from the data why this might be the case, particularly since the registrar cohort demonstrated a positive correlation between GAD-2 score and fear of contracting COVID-19 (R2 = 0.2835, p = 0.001426). It may be that registrars are relatively well protected in their job roles: they are not routinely in a senior decision-making role nor in many cases at the front-line of the COVID-19 pandemic.
Fig. 2.
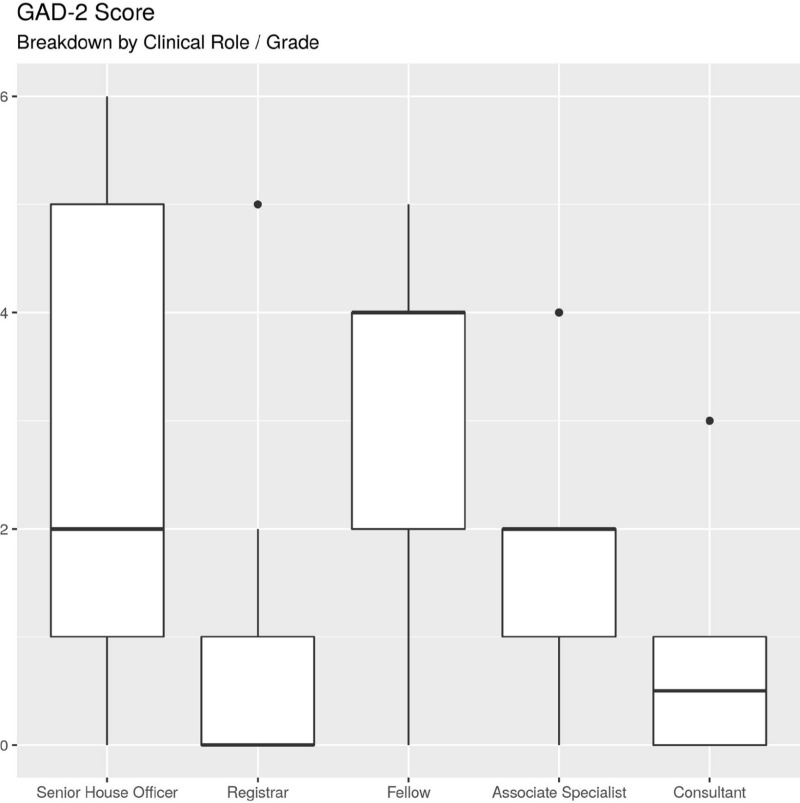
Boxplot of GAD-2 by grade. Registrars had a lower GAD-2 score when compared to other doctors (p = 0.02059).
Furthermore, changes to registrars’ daily rotas will in many cases have resulted in a reduction in overall workload. For example, some hospitals have implemented a ‘three days on and three days off’ rota pattern, incorporating a rest period of three days for every three days worked. This is a significant increase in rest days and provides ample time to recover from the stressors of the job. In addition, non-urgent clinics have been cancelled nationwide. Firstly, this reduces face-to-face patient contact and cuts the risk of contracting the COVID-19 infection and secondly, alleviates the associated administrative workload for registrars, such as preparing clinic notes, organizing investigations and signing off clinic letters. On-call commitments have also been altered in some instances, with the conversion of 24 hour non-resident on call shifts to shorter 12 hour resident on-call shifts. These changes may translate to lower levels of anxiety among this cohort of doctors.
Associate specialists
Our results showed that those at the associate specialist level were less concerned about career progression than any other grade of doctor during the pandemic (Figure 3). This is not unexpected given that, in general, associate specialists already work at the highest sub-consultant level. It is generally accepted that those working at this level are usually in long-term roles. The need for progression is, therefore, less than in the more junior SHO and registrar grades, where doctors will be required to meet predetermined Annual Review of Competency Progression (ARCP) outcomes. Statistical analysis confirms that those at SHO and registrar level were significantly more concerned about training progression than associate specialists (p = 0.005407). Interestingly, those that reported significant concerns about training progression correlated with having previously sought mental health treatment or having sought wellbeing services during the pandemic.
Fig. 3.
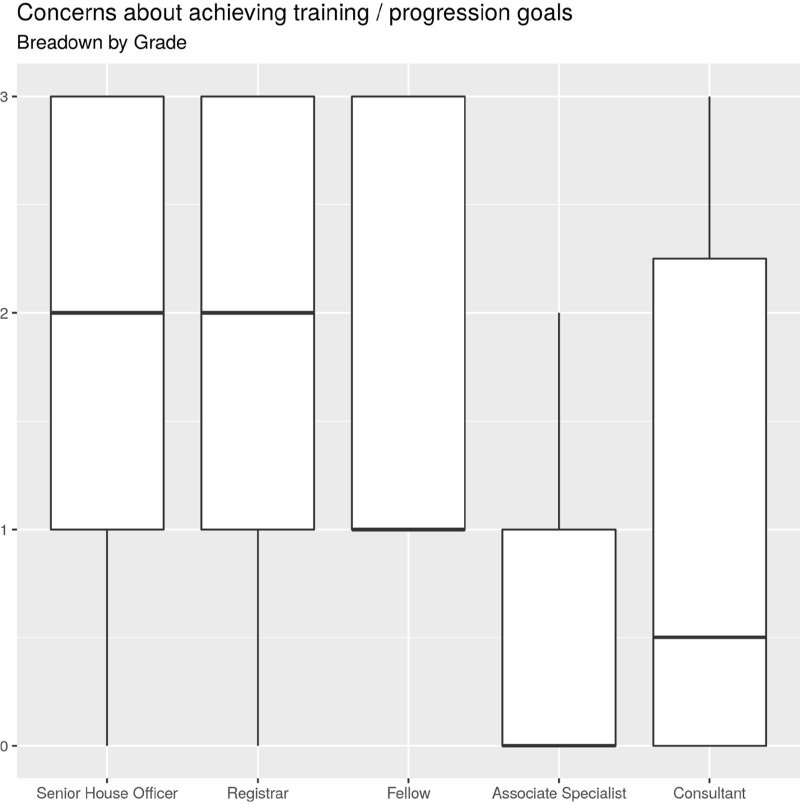
Boxplot of training by grade. Associate Specialists were significantly less concerned about the impact of COVID-19 training and career progression (p = 0.01234)
Sex
We identified that females scored significantly higher for symptoms of generalized anxiety disorder and major depressive disorder as compared to males (Figure 4). A systematic review by Remes et al12 found that in the general population, females were almost two times more likely to be affected by GAD than men and this was consistent across different countries and co-existing health conditions. In context, therefore, our results might not be unexpected but are certainly still concerning. Furthermore, women felt less able to be open with colleagues about their mental health (p = 0.03573) and felt less supported in the workplace (p = 0.03382). Unfortunately, discrimination and stigmatization among healthcare professionals still exists and this can obstruct the desire to seek mental health treatment.13,14
Fig. 4.
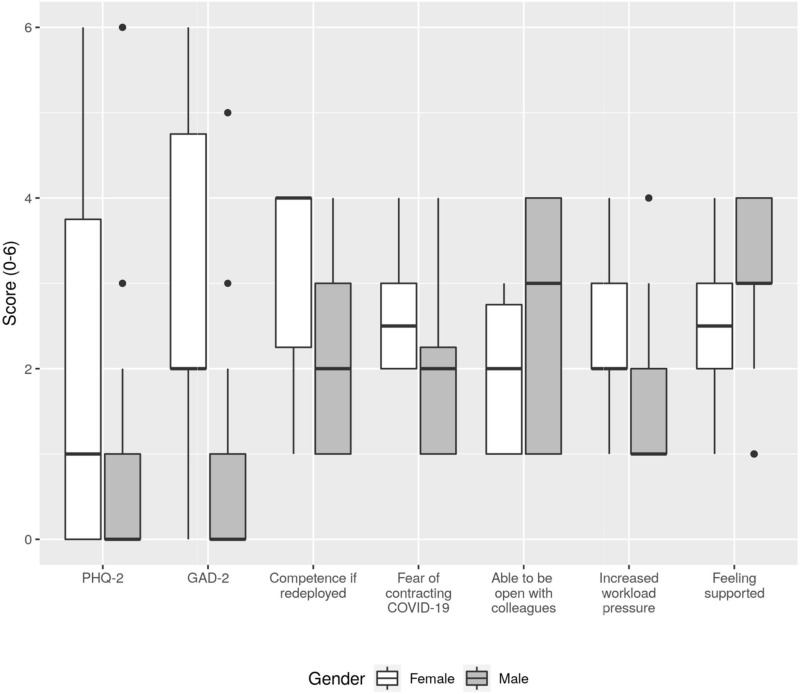
Boxplot showing questions in which males’ and females' scores were significantly different. Males had lower PHQ-2 (p = 0.03583) and GAD-2 (p = 0.0001086) scores, females were more concerned about contracting COVID-19 at work (p = 0.02235), more concerned about increased pressure in the workplace (p = 0.0006537) and more concerned about redeployment (p = 0.003701). Females felt less able to be open with colleagues about their mental health (p = 0.03573) and felt less supported in the workplace lower (p = 0.03382).
Ethnicity
We found that those who had identified as ‘Black/African/Caribbean/Black British’ had higher prevalence of anxiety symptoms than the rest of the cohort (Figure 5). A recent survey of doctors conducted by the Royal College of Physicians (RCP) found that 76% of all that identified as BAME (Black, Asian and minority ethnic) were either concerned or very concerned for their health during the pandemic. This may be the driving force behind the higher incidence of anxiety we observed. Our survey did demonstrate correlation in this cohort with feeling less supported in the workplace (p = 0.001341), however, we were unable to demonstrate a correlation with concerns specifically about contracting COVID-19 in the workplace (p = 0.4529).
Fig. 5.
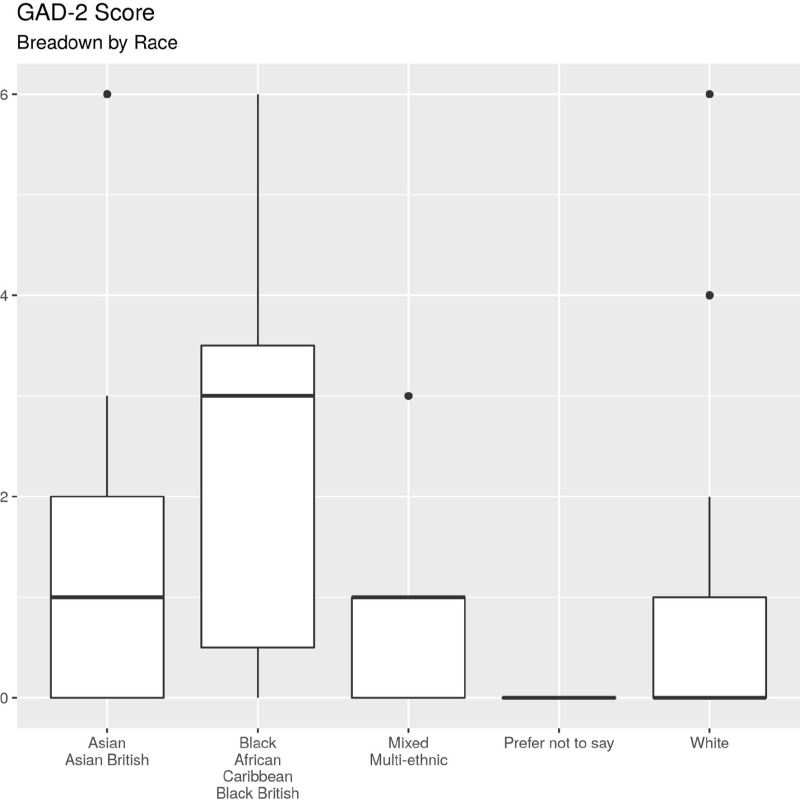
Boxplots of GAD-2 by race. Compared to other races those that identified as 'Black/African/Caribbean/Black British' had higher GAD-2 scores (p = 0.001575)
Generalized anxiety disorder (GAD)
We found a significant correlation between those respondents who felt they were experiencing increased workload pressure and the prevalence of anxiety symptoms. Significant correlation was also seen between those respondents who showed evidence of GAD and those who felt that their workplace behaviour had been adversely affected during the time of the pandemic. A meta-analysis of eleven papers performed in 2006 showed that those experiencing high demands at work with reduced decision latitude (control over a person's own role or tasks) is a risk factor for a number of common mental health disorders. It follows that those clinicians who are put under more pressure at work, for example, due to an increase in workload or change in the work environment are likely to experience symptoms of anxiety. During the pandemic, significant top-down changes to the workplace have been enforced in many areas of the NHS and it is possible that this is a driving force behind the results of our study.15
Major depressive disorder (MDD)
We noted that those that had previously sought mental health treatment had a greater incidence of depressive symptoms. Kupfer et al16 showed that following an index episode of major depressive disorder at least 50% will go on to have at least one further episode. Furthermore, it has also been shown that the mean duration of an episode of major depressive disorder is 16 weeks with severe role impairment in almost 60% of cases.17 MDD in the trauma and orthopaedic speciality could therefore create a significant burden on workforce planning when services are already struggling.
Recommendations
Preserving mental health and wellbeing during the pandemic is not a straightforward task and these issues are not unique to the trauma and orthopaedic workforce. Sanatarone et al18 recommend that to preserve the mental health and resilience of the workforce during the COVID-19 pandemic, a hierarchy of needs should be considered. They suggest the primary need is protecting physical wellbeing and the secondary need is supporting psychological wellbeing. We therefore outline below some recommendations which may assist with psychological wellbeing.
Communication
At times when there are rapid changes to the day-to-day running of the department, clear communication between management and juniors is essential. Regular meetings are difficult due to social distancing measures; however, videoconferencing tools can facilitate departmental meetings with all grades of doctor. Our study showed that those at SHO grade were disproportionately affected by symptoms of MDD and so the inclusion of juniors in such discussions may improve the perception of their decision latitude and translate to better mental health outcomes.
Rest
In usual times, healthcare professionals could find relief in knowing that they have access to leisure and social activities that help them unwind. The current pandemic, however, restricts those very activities which provide solace for individuals. Facilitation of adequate rest days therefore is likely to contribute to better recovery from the stressors of the job. Given that many elective activities are cancelled, the extra availability of human resources may be able to facilitate such changes more easily.
Support
During the pandemic direct social interaction is often limited to our work colleagues, however, over half our respondents felt unable to speak to colleagues about their mental health and one third felt unsupported at work. Research by the ‘Time to Change’ campaign, revealed that when asked, over 78% of respondents would tell colleagues they are ‘fine’, even if they are indeed struggling with a mental health problem.19 The campaign urges people to ‘Ask Twice’ to really understand underlying mental health issues. Awareness of this simple intervention may prompt those who feel unsupported to engage in conversation about their mental wellbeing. Furthermore, many organisations such as the British Medical Association have made online wellbeing resources available and these should be regularly signposted by departmental leads11.
Limitations
There is likely to have been a selection bias of our cohort. Since the survey was optional, it is possible that those who participated have a personal interest in mental health related disorders and therefore the data may be skewed in their favour. Due to the stigmatisation of mental illness there may also be a response bias with survey takers not wishing to fully disclose their mental health difficulties despite the survey being entirely anonymous.
It should be noted that the prevalence of these disorders in our cohort are estimates since the GAD-2 and PHQ-2 tools are screening tools used to prompt further diagnostic evaluation to confirm the diagnosis.
The overall number of respondents to our survey are likely to be in the region of 1% of the trauma and orthopaedic workforce and therefore may not effectively provide a cross-sectional analysis of the topic. Repeat studies that can draw on a larger cohort are likely to add more power to the outcomes, especially for subgroups which were underrepresented.
Conclusion
Our study, in the first of its kind, shows a significant incidence in symptoms of generalized anxiety and major depressive disorders in the trauma and orthopaedic workforce during the COVID-19 pandemic. We found that SHOs, females and those of Black, African, Caribbean, or Black British origin were disproportionately affected. The estimated prevalence of major depressive disorder was significantly higher in those who had previously sought treatment for mental health disorders. We believe that mental health issues are likely underreported among trauma and orthopaedics colleagues. Though it may not seem that the mental health of this subgroup of doctors would be directly affected by the COVID-19 pandemic, our study shows that it is, in fact, a significant issue. Action should be promptly taken, and awareness raised, to help prevent adverse mental health outcomes for our colleagues during these challenging circumstances.
Footnotes
Author contributions: A. Thakrar: Conceptualization, Wrote the manuscript.
A. Raheem: Creation of survey and statistical analysis.
K. Chui: Formulation of survey methods.
E. Karam: Distribution of survey, Edited the manuscript.
L. Wickramarachchi: Distribution of survey, Edited the manuscript.
K. Chin: Senior editor and supervisor.
Funding statement: No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Twitter: Follow A. Thakrar @DrAmitThakrar
References
- 1. COVID-19 Map [Internet] Johns Hopkins Coronavirus Resource Center. 2020. https://coronavirus.jhu.edu/map.html (date last accessed 21 May 2020).
- 2. Anagnostopoulos F, Liolios E, Persefonis G, et al. Physician burnout and patient satisfaction with consultation in primary health care settings: evidence of relationships from a one-with-many design. J Clin Psychol Med Settings. 2012;19(4):401–410. [DOI] [PubMed] [Google Scholar]
- 3. Dewa CS, Loong D, Bonato S, Thanh NX, Jacobs P. How does burnout affect physician productivity? A systematic literature review. BMC Health Serv Res. 2014;14:325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Fahrenkopf AM, Sectish TC, Barger LK, et al. Rates of medication errors among depressed and burnt out residents: prospective cohort study. BMJ. 2008;336(7642):488–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lu DW, Dresden S, McCloskey C, Branzetti J, Gisondi MA. Impact of burnout on self-reported patient care among emergency physicians. West J Emerg Med. 2015;16(7):996–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Shanafelt TD, Mungo M, Schmitgen J, et al. Longitudinal study evaluating the association between physician burnout and changes in professional work effort. Mayo Clin Proc. 2016;91(4):422–431. [DOI] [PubMed] [Google Scholar]
- 7. Arroll B, Goodyear-Smith F, Crengle S, et al. Validation of PHQ-2 and PHQ-9 to screen for major depression in the primary care population. Ann Fam Med. 2010;8(4):348–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Skapinakis P. The 2-item generalized anxiety disorder scale had high sensitivity and specificity for detecting GAD in primary care. Evid Based Med. 2007;12(5):149. [DOI] [PubMed] [Google Scholar]
- 9. Stansfeld S, Clark C, Bebbington P, et al. Chapter 2: Common mental disorders : McManus S, Bebbington P, Jenkins R, Brugha T., Mental health and wellbeing in England: adult psychiatric morbidity survey 2014. Leeds: NHS Digital, 2016. [Google Scholar]
- 10. Terms and conditions contracts [Internet] nhsemployers.org. 2020. https://www.nhsemployers.org/pay-pensions-and-reward/medical-staff/doctors-and-dentists-in-training/terms-and-conditions-contracts (date last accessed 21 May 2020).
- 11. Looking after yourself - COVID-19: your wellbeing - BMA [Internet] The British Medical Association. 2020. https://www.bma.org.uk/advice-and-support/covid-19/your-health/covid-19-your-wellbeing/looking-after-yourself (date last accessed 21 May 2020).
- 12. Remes O, Brayne C, van der Linde R, Lafortune L. A systematic review of reviews on the prevalence of anxiety disorders in adult populations. Brain Behav. 2016;6(7):e00497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Zheng W. Mental health and a novel coronavirus (2019-nCoV) in China. J Affect Disord. 2020;269(269):201–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bianchi EF, Bhattacharyya MR, Meakin R. Exploring senior doctors' beliefs and attitudes regarding mental illness within the medical profession: a qualitative study. BMJ Open. 2016;6(9):e012598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Stansfeld S, Candy B. Psychosocial work environment and mental health—a meta-analytic review. Scand J Work Environ Health. 2006;32(6):443–462. [DOI] [PubMed] [Google Scholar]
- 16. Kupfer DJ. Long-Term treatment of depression. J Clin Psychiatry. 1991;52 Suppl(52 Suppl):28–34. [PubMed] [Google Scholar]
- 17. Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: results from the National comorbidity survey replication (NCS-R). JAMA. 2003;289(23):3095–3105. Jun 18;. [DOI] [PubMed] [Google Scholar]
- 18. Santarone K, McKenney M, Elkbuli A. Preserving mental health and resilience in frontline healthcare workers during COVID-19. Am J Emerg Med. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ask twice, people urged, as new research shows three quarters of Brits would say they are ‘fine’ even if struggling with a mental health problem [Internet] Time To Change. 2020. https://www.time-to-change.org.uk/news/ask-twice-people-urged-new-research-shows-three-quarters-brits-would-say-they-are-‘fine’-even (date last accessed 8 June 2020).


