Abstract
Aims
Robotic-assisted total knee arthroplasty (RA-TKA) has been introduced to provide accurate bone cuts and help achieve the target knee alignment, along with symmetric gap balancing. The purpose of this study was to determine if any early clinical benefits could be realized following TKA using robotic-assisted technology.
Methods
In all, 140 consecutive patients undergoing RA-TKA and 127 consecutive patients undergoing conventional TKA with minimum six-week follow-up were reviewed. Differences in visual analogue scores (VAS) for pain at rest and with activity, postoperative opiate usage, and length of stay (LOS) between the RA-TKA and conventional TKA groups were compared.
Results
Patients undergoing RA-TKA had lower average VAS pain scores at rest (p = 0.001) and with activity (p = 0.03) at two weeks following the index procedure. At the six-week interval, the RA-TKA group had lower VAS pain scores with rest (p = 0.03) and with activity (p = 0.02), and required 3.2 mg less morphine equivalents per day relative to the conventional group (p < 0.001). At six weeks, a significantly greater number of patients in the RA-TKA group were free of opioid use compared to the conventional TKA group; 70.7% vs 57.0% (p = 0.02). Patients in the RA-TKA group had a shorter LOS; 1.9 days versus 2.3 days (p < 0.001), and also had a greater percentage of patient discharged on postoperative day one; 41.3% vs 20.5% (p < 0.001).
Conclusion
Patients undergoing RA-TKA had lower pain levels at both rest and with activity, required less opioid medication, and had a shorter LOS.
Keywords: Robotic-assisted TKA, Postoperative pain, Postoperative opioid usage, Length of stay
Introduction
The demand for total knee arthroplasty (TKA) continues to increase, with over 3.5 million projected to be performed per year by 2030.1 With the increase in volume and demand, there are concerns over the available resources required to meet it. In an effort to preserve resources, there has been an impetus towards earlier discharge and return to function through perioperative patient optimization, multimodal analgesia, and rehabilitation protocols focused on optimizing postoperative recovery. Postoperative pain is a leading cause of increased length of stay, complications, and patient satisfaction.2
Robotic-assisted total knee arthroplasty (RA-TKA) has been introduced to provide accurate bone cuts, precise placement of total knee implants, and to help provide symmetrically balanced flexion and extension gaps.3-5 In addition, this technology theoretically minimizes the amount of bone resection and soft tissue damage, which are both thought to be significant pain generators.6 There have been very few studies demonstrating the early clinical benefits of RA-TKA compared to conventional TKA using manual instruments. The purpose of this study was to compare early postoperative pain, opioid usage, and length of stay (LOS) in patients undergoing RA-TKA versus conventional TKA with manual instrumentation.
Methods
This retrospective study included 268 consecutive patients with osteoarthritis (OA) of the knee undergoing primary TKA. Data from this study was abstracted from the institution’s established prospective total joint registry database. The study was approved through our Institutional Review Board (IRB). All cases were performed during the same time period, and using the same anaesthesia team, postoperative protocols, and surgical approach at the same institution from April 2017 to April 2018. Inclusion criteria consisted of patients with knee OA undergoing primary unilateral TKA, with a minimum of six-weeks postoperative follow-up. Exclusion criteria consisted of patients with a history of prior infection of the knee joint, and patients undergoing conversion of unicompartmental arthroplasty to a TKA. This was a consecutive series with patients undergoing RA-TKA on days the robotic system was available and jig-based manual instruments with cutting guides used when the robotic system was not available. In the RA-TKA group, there were 140 consecutive patients with an average age of 65.4 years (26 to 85). There were 127 consecutive patients undergoing conventional TKA using manual jig-based instruments with an average age of 66.6 years (36 to 91). There were no differences between the groups with respect to age, sex, and preoperative ASA scores, which is shown in Table I. Paired t-test was used for statistical analysis for difference in age, and Fisher’s exact test for sex, ASA score, and operative side. All surgical cases were performed by the same surgeon at the same institution. The same implant design was utilized in all patients (Triathlon PS TKA; Stryker, Mahwah, New Jersey, USA). In the RA-TKA group, intraoperative computer technology was utilized with a semi-active robotic system (Mako; Stryker). All patients were entered into a total joint programme preoperatively, where they were educated on risk, benefits, and expected postoperative course.
Table I.
Demographic data comparing conventional versus robotic-assisted TKA.
| Characteristics | Category | Conventional (n = 127) | Robotic (n = 140) | p-value |
|---|---|---|---|---|
| Mean age (years) | 66.6 | 65.4 | 0.306* | |
| Sex (%) | Male | 38.6 | 38.5 | 1.0† |
| Female | 61.4 | 61.5 | 1.0† | |
| ASA score (%) | I | 0.0 | 1.4 | 0.499† |
| II | 48.8 | 55.7 | 0.272† | |
| III | 51.2 | 42.9% | 0.179† | |
| Operative side (%) | Right | 54.3 | 47.1 | 0.271† |
| Left | 45.7 | 52.9 | 0.271† |
Paired t-test.
Fisher’s exact test.
Patients undergoing RA-TKA underwent a preoperative CT scan to generate a 3D preoperative plan for component sizing and placement. Light-emitting diode trackers were placed on the femur and tibia, to be used with the semi-active robotic system to achieve the desired bone cuts and target limb alignment, along with symmetrically-balanced flexion and extension gaps. There were no intramedullary guides or cutting jigs utilized for the RA-TKA cases. For the manual jig-based cases, an intramedullary alignment guide was utilized for the distal femoral cut and an extramedullary guide for the tibial cut. A gap balancing technique was utilized using a ligamentous tensioning device with the extension gap balanced followed by balancing the flexion gap after release of the posterior cruciate ligament. The patella was resurfaced in both groups using a free-hand technique. All patients received the same anaesthesia protocol consisting of local adductor canal and posterior capsule blocks along with general anaesthesia.
Patient demographics were obtained along with American Society of Anesthesiologists (ASA) score. There was no statistical difference in demographics or preoperative clinic characteristics between the robotic-assisted and conventional TKA groups (Table I). Operative time and blood loss was recorded along with any intraoperative complications. Outcome measures utilized in this study included differences in LOS, visual analogue scores (VAS) for pain at rest and with activity, and postoperative opiate use in morphine equivalents between the robotic and conventional TKA groups. Patients were discharged based on standardized guidelines, which take into consideration the patient’s health, mental status, and ability to ambulate established by our institution’s Total Joint Committee. All patients in this study had a minimum of six-weeks postoperative follow-up. The average follow-up in the RA-TKA group was 7.3 weeks (standard deviation (SD) 1.6) and 7.2 weeks (SD 1.5) for the conventional TKA group. All statistical analyses were performed using Excel 2018 (Microsoft, Redmond, Washington, USA). The two-tailed student t-test was utilized to compare all normally distributed continuous variables. A Mann-Whitney U test was utilized for all non-normally distributed continuous variables. Statistical significance was set as a p-value < 0.05.
Results
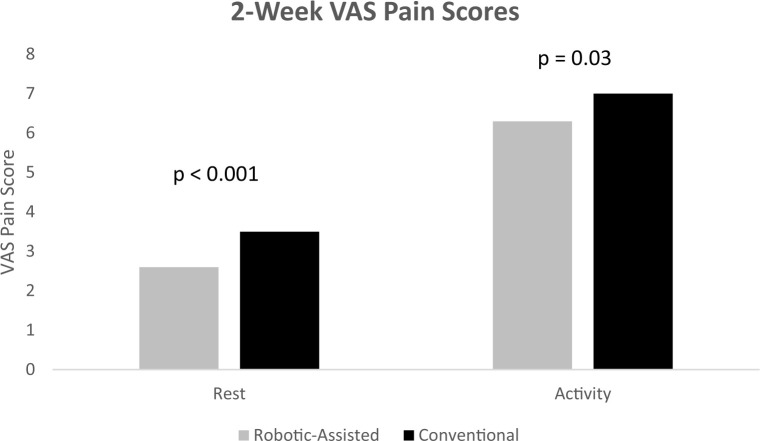
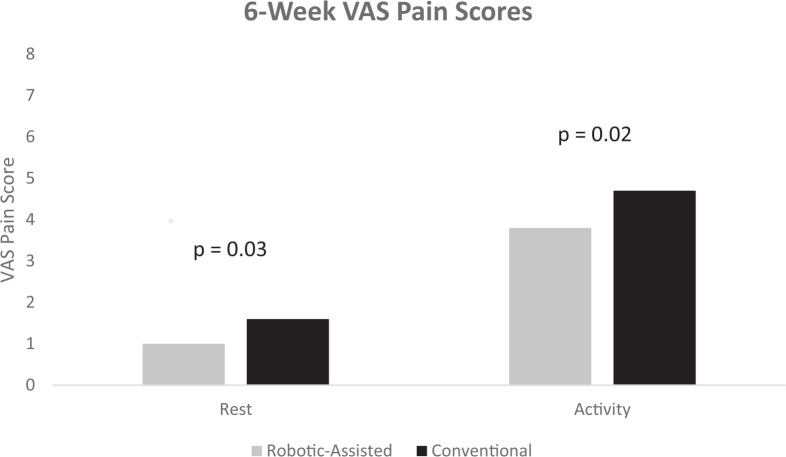
At two weeks postoperatively, patients undergoing RA-TKA had a significantly lower average VAS pain score at rest (2.6 vs 3.5 (p = 0.001)) and VAS pain score with activity (6.3 vs 7.0 (p = 0.03)) compared to the manual instrumentation group. At six-weeks postoperatively, patients undergoing RA-TKA also had significantly lower VAS pain scores at rest (1.0 vs 1.6 (p = 0.03)) and with activity (3.8 vs 4.7 (p = 0.02)) compared to the conventional TKA group. This data is summarized in Figures 1 and 2.
Figure 1.
Robotic-assisted TKA demonstrates decreased VAS pain scores at two weeks postoperatively compared to conventional TKA.
Figure 2.
Robotic-assisted TKA also demonstrates decreased VAS pain scores at six weeks postoperatively compared to conventional TKA.
Patients in the RA-TKA and conventional groups had similar opioid usage rates at two weeks (30.2 morphine equivalents vs 27.4 morphine equivalents); however, at six weeks postoperatively the RA-TKA group had a significantly lower opioid usage rate (4.5 morphine equivalents versus 7.7 morphine equivalents) for the conventional TKA group (p < 0.001). Furthermore, at the six-week postoperative period, a significantly higher percentage of patients in the RA-TKA group (70.7% (99/140)), were free of opioid use compared to 57.0% (73/127) of patients in the conventional TKA group (p = 0.02).
Patients in the RA-TKA group had a shorter LOS compared to the conventional TKA group (1.9 days vs 2.3 days (p < 0.001)). The RA-TKA group had a significantly greater percentage of patients discharged on postoperative day one compared to the conventional TKA group (41.3% vs 20.5% (p < 0.001)). This data is summarized in Table II with statistical analysis performed using paired t-test. The mean operative time for the RA group was 95 minutes versus 87 minutes for the manual conventional TKA group. There were no differences in overall complications between the two groups, with two prosthetic joint infections in the robotic-assisted group and one in the manual TKA group.
Table II.
Postoperative results comparing outcomes of conventional versus robotic-assisted TKA.
| Outcome | Conventional (n = 127) | Robotic (n = 140) | p-value* |
|---|---|---|---|
| Estimated blood loss (ml) | 74.1 | 70.3 | 0.374 |
| Length of stay (days) | 2.3 | 1.9 | < 0.001 |
| Discharge postoperative day one (%) | 20.5 | 41.3 | < 0.001 |
| Morphine eq at two weeks | 27.4 | 30.2 | 0.369 |
| Morphine eq at six weeks | 7.7 | 4.5 | < 0.001 |
| Opioid free at six weeks (%) | 57.0 | 70.7 | 0.020 |
eq; equivalent.
Paired t-test.
Discussion
In this retrospective cohort study, there were no differences in baseline characteristics between the patients who underwent TKA using robotic-assisted or manual instrumentation with respect to age, sex, and ASA score. Our results demonstrate that patients who underwent RA-TKA had significantly lower VAS pain scores at rest and with activity at both the two- and six-week time periods, significantly lower opioid use at six weeks, significantly greater likelihood of being free of opioid use at six weeks, and shorter LOS compared to patients undergoing conventional TKA. Minimizing early postoperative pain after TKA is important to improve short-term outcomes with respect to opioid consumption, range of motion, achieving the desired rehabilitation goals, and improving patient satisfaction.
Although TKA has been considered one of the most successful procedures in orthopaedics with excellent survivorship, postoperative patient satisfaction rates remain unexpectedly lower than anticipated.7-9 Several studies have demonstrated that pain after TKA significantly contributes to a lower satisfaction score postoperatively, while some have even shown that pain is the most important prognostic indicator of dissatisfaction after TKA.10 Our results demonstrate that RA-TKA leads to significantly decreased postoperative pain in addition to decreased opioid consumption and are similar to those previously published studies. Our results corroborate the findings of Kayani et al.11 They compared 40 patients undergoing RA-TKA with 40 patients undergoing conventional jig-based TKA in a prospective cohort study, and found that patients in the RA-TKA group had reduced pain scores and decreased opioid consumption in the short-term.
RA-TKA provides intraoperative flexibility with the ability to balance flexion and extension gaps with bony resection and manipulation of the tibial and femoral component position. By placing the tibial component in one to three degrees of varus, in cases of preoperative varus deformity, the medial gap space can be balanced without performing any additional soft tissue releases following the basic exposure. We believe this helps contribute to decreased postoperative pain. Khlopas et al12 demonstrated in a cadaveric study that bony resection of the tibia in RA-TKA did not require subluxation, which causes significant ligamentous stretching and subsequently can lead to increased postoperative pain. Not requiring tibial subluxation during tibial bony resection in the RA-TKA cohort may explain the decreased short-term postoperative pain levels compared to conventional TKA. In addition, Siebert et al13 demonstrated reduced postoperative soft tissue swelling in a retrospective study of 70 patients undergoing robotic-arm assisted to a matched historic cohort of 50 conventional TKAs. The reduced inflammatory response in robotic-arm assisted TKA likely explains the decrease in pain associated with robotic-assisted surgery.
Postoperative pain after TKA is controlled, in most patients, through the use of prescription opioid medication. While Americans comprise 5% of the world’s population, they consume 80% of the total opioids prescribed.14 As a consequence, there has been an increase in opioid dependence and an increase in opioid-related deaths. There has been an increasing focus in the USA to limit opioid consumption. Our results have demonstrated a significant decrease in opioid consumption at the six-week period in patients undergoing RA-TKA compared to those with manual jig-based instruments. The decrease in opioid consumption in the RA-TKA group may be related to less bony trauma, since there is no intramedullary guide or drill hole at the distal femur and less soft tissue trauma. Decreased opioid consumption may help decrease the risk of opioid dependency.
Our results demonstrate that patients in the RA-TKA group had a shorter LOS with a significantly greater percentage of patients discharged on postoperative day one. These results are similar to those in the literature. Kayani et al11 also compared LOS between 40 patients in a RA-TKA group to 40 patients undergoing conventional jig-based TKA, and demonstrated a significantly shorter length of stay (77 hours vs 105 hours, respectively). Although clinically, 1.9 versus 2.3 days may not seem significant, the cost-savings to the hospital is relevant. According to a study by Barad et al,15 the cost-saving of discharge on postoperative day one versus postoperative day two is $1,216.
There are several limitations of this study that must be considered when interpreting these findings. This was a retrospective review and not a prospective randomized study. However, this was a consecutive series with patients allocated to the robotic or conventional TKA groups in order of appearance, and based on the availability of robotic instrumentation. However, this study design may allow for the inadvertent introduction of selection bias but there were no differences between the two groups with respect to age, sex, and ASA scores. The results of this study are only short-term, evaluating pain scores, opioid consumption, and LOS; there was no long-term follow-up to determine if the benefits of RA-TKA continue to surpass those performed using manual jig-based instruments. This study also did not include any radiological findings given the short-term focus of this study.
RA-TKA provides intraoperative information for the surgeon to achieve the target alignment and symmetrically-balanced gaps. RA-TKA is associated with decreased pain levels at rest and with activity at two and six weeks postoperatively. Patients demonstrated significantly decreased opioid consumption at six weeks postoperatively, in addition to a significantly great number being free of opioid use at six weeks. There were no differences in postoperative ROM, WOMAC knee and function scores, KSS knee and function scores, or complications between the RA-TKA and conventional TKA groups. The short-term results of robotic-assisted surgery compared to the use of manual jig-based instruments in patients undergoing primary TKA appear promising, but longer follow-up is needed to determine the true efficacy of this innovative technology.
Footnotes
Author contributions: S. J. Bhimani: Wrote the manuscript, Performed the statistical analysis, Created the tables and figures, Conceived the study, Designed the study.
R. Bhimani: Collected the data, Analyzed the data, Assisted with the creation of tables and figures.
A. Smith: Collected the data, Analyzed the data.
C. Eccles: Collected the data, Analyzed the data.
L. Smith: Coordinated the study, Collected the data, Formatted and submitted the manuscript.
A. Malkani: Conceived the study, Designed the study, Wrote the manuscript.
Funding statement: Although none of the authors has received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this article, benefits have been or will be received but will be directed solely to a research fund, foundation, educational institution, or other non- profit organization with which one or more of the authors are associated.
ICMJE COI statement: A. Malkani reports that Stryker Orthopedics acted as the funding agency for the research. Funding was provided to Louisville Orthopedic Research & Education Foundation, where Dr. Malkani is an officer. Dr Malkani also reports consultancy, payment for lectures (including service on speakers’ bureaus), and royalties, all from Stryker Orthopedics, but unrelated to this article.
Ethical review statement: This study received full approval from our local Institutional Review Board.
References
- 1.Kurtz SM, Lau E, Ong K, et al. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009;467(10):2606–2612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang S, Huang Q, Xie J, et al. Factors influencing postoperative length of stay in an enhanced recovery after surgery program for primary total knee arthroplasty. J Orthop Surg Res. 2018;13(1):29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shalhoub S, Moschetti WE, Dabuzhsky L, et al. Laxity profiles in the native and replaced knee-application to robotic-assisted gap-balancing total knee arthroplasty. J Arthroplasty. 2018;33(9):3043–3048. [DOI] [PubMed] [Google Scholar]
- 4.Song E-K, Seon J-K, Yim J-H, Netravali NA, Bargar WL. Robotic-Assisted TKA reduces postoperative alignment outliers and improves gap balance compared to conventional TKA. Clin Orthop Relat Res. 2013;471(1):118–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mullaji A, Shetty GM. Computer-Assisted TKA: greater precision, doubtful clinical efficacy: opposes. Orthopedics. 2009;32(9):pii: orthosupersite.com/view.asp?rID=42846. [DOI] [PubMed] [Google Scholar]
- 6.Sultan AA, Piuzzi N, Khlopas A, et al. Utilization of robotic-arm assisted total knee arthroplasty for soft tissue protection. Expert Rev Med Devices. 2017;14(12):925–927. [DOI] [PubMed] [Google Scholar]
- 7.Deakin AH, Smith MA, Wallace DT, Smith EJ, Sarungi M. Fulfilment of preoperative expectations and postoperative patient satisfaction after total knee replacement. A prospective analysis of 200 patients. Knee. 2019;26(6):1403–1412. [DOI] [PubMed] [Google Scholar]
- 8.Bierke S, Häner M, Karpinski K, Hees T, Petersen W. Midterm effect of mental factors on pain, function, and patient satisfaction 5 years after uncomplicated total knee arthroplasty. J Arthroplasty. 2020;35(1):105–111. [DOI] [PubMed] [Google Scholar]
- 9.Galea VP, Rojanasopondist P, Connelly JW, et al. Changes in patient satisfaction following total joint arthroplasty. J Arthroplasty. 2020;35(1):32–38. [DOI] [PubMed] [Google Scholar]
- 10.Scott CEH, Howie CR, MacDonald D, Biant LC. Predicting dissatisfaction following total knee replacement: a prospective study of 1217 patients. J Bone Joint Surg Br. 2010;92-B(9):1253–1258. [DOI] [PubMed] [Google Scholar]
- 11.Kayani B, Konan S, Tahmassebi J, Pietrzak JRT, Haddad FS. Robotic-arm assisted total knee arthroplasty is associated with improved early functional recovery and reduced time to hospital discharge compared with conventional jig-based total knee arthroplasty: a prospective cohort study. Bone Joint J. 2018;100-B(7):930–937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khlopas A, Chughtai M, Hampp EL, et al. Robotic-arm assisted total knee arthroplasty demonstrated soft tissue protection. Surg Technol Int. 2017;30:441–446. [PubMed] [Google Scholar]
- 13.Siebert W, Mai S, Kober R, Heeckt PF. Technique and first clinical results of robot-assisted total knee replacement. Knee. 2002;9(3):173–180. [DOI] [PubMed] [Google Scholar]
- 14.Halawi MJ, Lieberman JR. Battling the opioid epidemic: lessons learned and management strategies. Arthroplast Today. 2019;5(1):2–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barad SJ, Howell SM, Tom J. Is a shortened length of stay and increased rate of discharge to home associated with a low readmission rate and cost-effectiveness after primary total knee arthroplasty? Arthroplast Today. 2018;4(1):107–112. [DOI] [PMC free article] [PubMed] [Google Scholar]