Abstract
Virtual encounters have experienced an exponential rise amid the current COVID-19 crisis. This abrupt change, seen in response to unprecedented medical and environmental challenges, has been forced upon the orthopaedic community. However, such changes to adopting virtual care and technology were already in the evolution forecast, albeit in an unpredictable timetable impeded by regulatory and financial barriers. This adoption is not meant to replace, but rather augment established, traditional models of care while ensuring patient/provider safety, especially during the pandemic. While our department, like those of other institutions, has performed virtual care for several years, it represented a small fraction of daily care. The pandemic required an accelerated and comprehensive approach to the new reality. Contemporary literature has already shown equivalent safety and patient satisfaction, as well as superior efficiency and reduced expenses with musculoskeletal virtual care (MSKVC) versus traditional models. Nevertheless, current literature detailing operational models of MSKVC is scarce. The current review describes our pre-pandemic MSKVC model and the shift to a MSKVC pandemic workflow that enumerates the conceptual workflow organization (patient triage, from timely care provision based on symptom acuity/severity to a continuum that includes future follow-up). Furthermore, specific setup requirements (both resource/personnel requirements such as hardware, software, and network connectivity requirements, and patient/provider characteristics respectively), and professional expectations are outlined. MSKVC has already become a pivotal element of musculoskeletal care, due to COVID-19, and these changes are confidently here to stay. Readiness to adapt and evolve will be required of individual musculoskeletal clinical teams as well as organizations, as established paradigms evolve.
Cite this article: Bone Joint Open 2020;1-6:272–280.
Keywords: Musculoskeletal Virtual Care, Virtual visits, Telehealth, Telemedicine, COVID-19, Beyond COVID-19, Triage
Introduction
Telemedicine, or the use of electronic information and communication technologies such as the internet to provide/support healthcare, has seen exponential growth over the past decade.1 Indeed, the telemedicine market was worth $30 billion in 2019 and is projected to grow 20% to 50% every year.2 Prior to the pandemic forcing a significant decrease in face-to-face clinical encounters, health professionals had been developing the opportunities and capabilities of telehealth services. Today, the remote provision of healthcare services has increased patient and provider safety. The global coronavirus 2019 (COVID-19) pandemic has forced increased interest and sudden adoption of this rapidly evolving field, specifically in the form of virtual clinical visits.3 The necessities of social distancing have forced a one-week transition from the traditional model of care (mainly face-to-face (F2F) encounters) to a predominantly virtual practice. Similar to many other institutions, prior to COVID-19, our department has performed virtual care for years, albeit this represented a small fraction of our practice. In response to the pandemic and public health recommendations for social distancing, there was a marked increase in telemedicine practices. Consequently, we have seen a transformation from a traditional model to a virtual model of care for the majority of non-acute orthopaedic patients. As such, adaptation to the COVID-19 crisis created a conversion to incorporating technology and virtual care that was a long-due necessity within the field of orthopaedics. The results of this crisis and this adaptation process will probably result in an evolution of how we practice.
One potential systematic algorithm to address adaptation and change in orthopaedics is the Observe-Orient-Decide-Act (O-O-D-A) loop, a model successfully adapted for use in numerous business4 and medical models.5–8 Applying such principles to the challenges currently faced by orthopaedic surgeons would initiate the following sequence: 1) An observation of persistent demand (especially postoperative care and established chronic disease management) for musculoskeletal care despite the challenges of social distancing and the longer-term barriers to patient access and increased time/resource utilization associated with in-office visits; 2) orientation of self and system regarding telemedicine as a viable tool to help overcome the aforementioned barriers; 3) a decision to establish workflows for virtual musculoskeletal care that are amenable to generalized implementation across orthopaedic surgery; and 4) action by applying such models while maintaining continuous testing for safety and efficacy, thereby bridging the dearth in literature. Simply stated, continuous evaluation through rational metrics is critical to avoid an adverse event.7,8
Of note, MSKVC is a modality of healthcare provision, rather than a distinct clinical service of its own accord.9 As such, MSKVC should be viewed as an integral clinical care delivery modality, rather than a separate complementary utility.10 An episode of care is a continuum of a number of methods.11 The current review describes a shift from a traditional model of musculoskeletal care (Figure 1) to include the MSKVC triaging platform to initiate the assignment to an episode of care management provision (Figure 2) ( Table I). In this paper, we outline the workflow organization (how the MSKVC model can be structured from triage-based on symptom acuity/severity to a continuum that extends to follow-up), set-up requirements (both resources and personnel necessary), and important encounter/billing considerations as experienced at an integrated healthcare system that provides MSKVC triage to a population of 4.5 million in North East Ohio. Furthermore, opportunities provided by the long-term implementation of such a system are outlined.
Fig. 1.
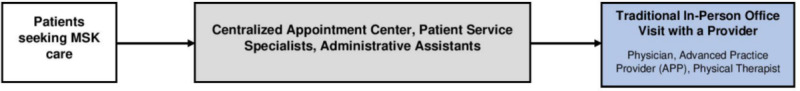
The traditional pathway for patient access to musculoskeletal care.
Fig. 2.
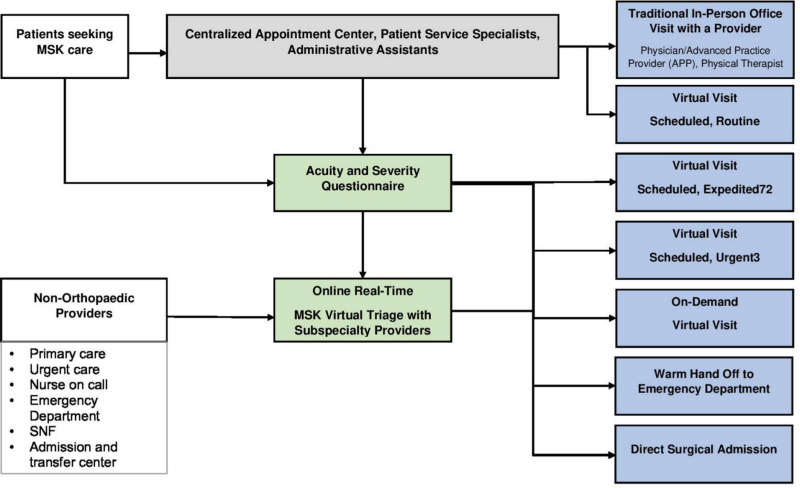
Integration of the virtual visits into patient access pathways.
Table I.
Elements of an ideal remote digital health virtual visit platform.
| Access management | Patient queue management system Appointment scheduling Automated appointment reminders |
| Technology communications integration | High resolution hosting and video conferencing Cloud based video hosting Secure messaging pre- and post-visit Electronic Health Record (EHR) integration Facility systems integration |
| Security | End-to-end Secure Sockets Layer (SSL) 128 to 256-bit Advanced Encryption Standard (AES) |
| Support | Reliable cloud-based technologies Technology support, call, and web Training and education |
The proposition of a universally applicable model
The COVID-19 pandemic was associated with an exponential rise in the utilization of MSKVC reaching 76% of daily patient encounters, compared to 0.4% during a similar time-period of 2019. The following model describes the MSKVC triage system established to accommodate the sudden rise in demand.
The conceptual workflow organization
Patients seeking musculoskeletal care are introduced by contacting the centralized appointment desk originating most from a provider referral, emergency department (ED), or urgent care consults. Patients are diverted to a virtual short questionnaire that can be administered electronically or via telephone (Table II). The questionnaire would assess the acuity, severity or urgency and a secondary questionnaire that includes basic patient demographics, pertinent comorbidities, and key elements would provide insight into the nature of the patients' complaints, including type, location, character, acuity, recent surgical history, and newly obtained imaging.4,12 An acuity and urgency-based stratification of patients would be conducted based on outcomes of the virtual musculoskeletal triage questionnaire, where patients with chronic conditions and established follow-up patients are offered routine virtual visits according to availability12 and geographical location. Conversely, derangements that are deemed to be acute, especially among patients with recent surgical history, are directed to a virtual musculoskeletal triage channel where a live interview with a musculoskeletal provider would guide down-stream disposition.13 Based on the results of the triaging questionnaire, coupled with providers’ assessment, patients would be referred to an urgency-appropriate disposition ranging from direct surgical admission, referral to the emergency department (ED) or orthopaedic acute care centre after direct notification, and provision of a plan-of-care, or requesting appropriate imaging. Alternatively, patients could be scheduled for an on-demand (immediate), urgent (same-day), expedited (within 72 hours), or routine virtual visit with the appropriate member of an orthopaedic clinical care team (Figure 2). Notably, virtual encounters have the potential to replace numerous episode-of-care interactions and, therefore, can be recurrently utilized along the patients' continuum of care (Figure 3). Significant benefits of telemedicine include access to care especially in geographically isolated areas, improving quality of delivery (privacy assurance, decreasing waiting time), and healthcare cost reduction through both convenience and increased time efficiency. The largest limitations include limited physical exam assessment capabilities, potential electronic glitches, and decreasing face-to-face time, although the latter point is currently preferred in the context of the COVID-19 pandemic.
Table II.
The Acuity and Severity questionnaire form directing downstream decision making the Musculoskeletal Virtual Care (MSKVS) triage model.
| |
| |
| |
| |
| 5. For shoulder: For elbow: For hand and wrist: For hip: For knee: For foot and ankle: |
Are you able to lift your arm above your head? Are you able to fully extend and bend your elbow? Are you able to fully grip objects with your hand? Are you able to bear weight on your hip? Are you able to fully extend and bend your knee? Are you able to walk 4 steps? Do you have pain on inside/outside of your ankle? Do you have pain on the inside outside of your foot? |
| |
| |
| |
Fig. 3.
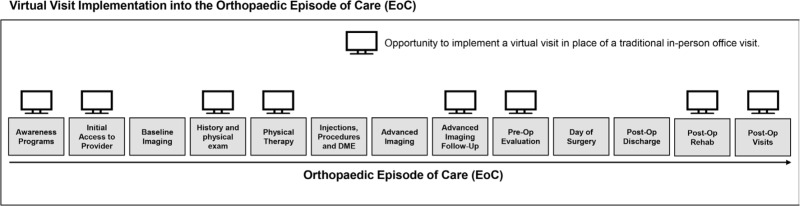
Multiple opportunities to implement a virtual visit in place of a traditional in-person office visit across the orthopaedic episode of care (EoC).
Patient selection and education
Equivalent safety and patient satisfaction after virtual and in-office/ED visits have been established in the literature.14,15 Selecting patients for continued virtual interaction without the need for an in-office presentation requires scrutiny. Patients requiring routine follow-up have constituted the main bulk of MSKVC consumers, virtual triaging will allow for expansion to encompass several non-acute conditions. In addition, virtual care may add value to care of patients with chronic painful conditions. This subset of patients is characterized by increased healthcare utilization, recurrent presentation to the ED and outpatient clinics, and high risk for "doctor shopping" and opioid medication use. Virtual follow-up of such patients may mitigate expenses while providing patients with the required provider consistency. Conversely, patients will require immediate in-person evaluation or care provision, as indicated by MSKVC triaging. Such patients typically have a history of significant trauma raising suspicion for acute injury or fracture, or patients within their postoperative course who report a sudden onset of swelling, significant pain, or concerning wound features, including dehiscence or purulent discharge.
Patients require appropriate orientation regarding the required tasks and expectations of the virtual visit. This can be communicated in a checklist format to ensure success of the virtual interaction.16,17 Certainly, adoption of mobile devices and technologies has helped accelerate demand and acceptance of digital healthcare services. Patient compliance and high education level are likely conducive to successful continuous virtual care, while failure or impatience might prompt providers to recommend in-office visits. Nevertheless, evidence suggesting such variation has not been conclusive.18–21 Measuring PROM and the business value of IT in healthcare will provide guidance on the efficiency and efficacy of these virtual care methods.7,21–24
The setup/resource requirements
Adequate setup is essential to maintain high-quality virtual healthcare delivery. Currently available mainstream video-streaming methods are generally sufficient for successful patient-provider interaction. Basic hardware requirements for virtual healthcare provision vary between patients and providers (Table III).25–27 Nevertheless, system requirements for patients encompass basic specifications present in most commercially available and current models of laptops and cell-phones.26 The basic business network connection has speeds of 50 to 100 megabits/sec (Mbps); however, minimum requirements to allow for smooth and clear video streaming is typically 5 Mbps of upload and 15 Mbps of download speeds which are considered commonplace.26,28 In brief, ideally, the provider should have the virtual visit on one screen with electronic medical record and imaging studies on another screen.
Table III.
Recommended specifications and room set-up for the patient-provider virtual encounter based on currently available mainstream technology.
| Item | Patient requirements* | Provider requirements | |
|---|---|---|---|
| System requirement | Display | A 720 p display is recommended. | A 720 p is acceptable; 1080 p is preferred. |
| Processor | A 3.4 GHz processor. | A 4.5GHz-capable multithread processor is preferred to allow for multitasking. | |
| Audio | High definition input/output, preferably with echo suppression. | ||
| Graphics | No need for a dedicated graphics processing unit. | A dedicated graphics processing unit is recommended. | |
| Connectivity | A minimum of 1-5Mbps upload/download speed. | A minimum of 5 to 15 upload/download speed. | |
| Cable management | Maintain < 12 feet of ethernet cable to prevent the loss of data packets. | ||
| Broadband traffic | Mitigate traffic during session. | ||
| Lighting | Adequate lighting directed to the patient/provider and away from the camera. | ||
| Audio recording precautions | Turn-off audio-activated and recording devices to prevent interference and for confidentiality purposes. Block sources of noise interference thorough closing windows and doors. A furnished room is more suited to mitigate echoing in the absence of soundproof walls. | ||
Present in most commercially available laptops and cell-phone devices.
In light of the COVID-19 pandemic, the Office for Civil Rights (OCR, the HIPAA-enforcement arm of the US Department of Health and Human Services) stated it will exercise “enforcement discretion” and not penalize noncompliance with regulatory requirements during the “good faith provision of telehealth” in the COVID-19 public health emergency.29 Nevertheless, the utilization of dedicated HIPAA compliant software specifically optimized for the purposes of virtual visits should be sought. HIPAA telemedicine guidelines detail that only authorized users should have access to electric patient health information (ePHI), and recommend a system of secure communication protecting ePHI integrity, and a system for monitoring ePHI communications to prevent accidental or malicious breaches.30 Such software would provide the patient status, waiting time, provider status, and a patient-friendly interface optimized for the nature of the visit. Furthermore, it would be at least dual encrypted for safety/privacy purposes and linked to an EMR for documentation.28
While the aforementioned requirements are generally regarded as mainstream, socioeconomic barriers may restrict the availability of such systems among certain patient populations. Rural areas, older populations (> 65 years), household income in the lowest quartile, education levels below a high school degree, and individuals with a disability status are more likely to lack internet connections, despite an arguable greater need for MSKVC.31 Therefore, regional healthcare centres may be provided with the necessary setup to act as MSKVC hubs for in-need populations. Indeed, published investigations highlight the value of virtually equipped healthcare centres that provide musculoskeletal care. Sinha et al15 investigated patient satisfaction, travel cost and time in paediatric fracture patients receiving real-time video consultation with an orthopaedic surgeon in a regional medical centre (n = 101) versus those presenting to an outpatient clinic at a tertiary hospital (n = 66). The authors highlighted similar satisfaction rates between both cohorts, with a total of 8/101 patients reporting a preference for conventional follow-up after receiving MSKVC at their regional health centre.
Personnel requirements
Ensuring minimal disruption of routine and optimizing the system to fit providers' preferences is crucial for mainstream adoption of virtual healthcare. The provision of virtual musculoskeletal healthcare will require various degrees of provider training in the efficient utilization of virtual systems.32 Specifically, the advent of virtual triaging may engender the need for a “MSK virtualist”; an orthopaedic specialist or advanced care provider who is well-versed at utilizing virtual systems and conducting virtual examinations to accurately stratify patients according to their acuity and urgency.
Telemedicine scheduling requirements can, at times, require a connected scheduling team and telehealth coordinator appropriately trained in video-conferencing platform use to facilitate scheduling, provide technical support, and educate patients regarding requisite downloads to a smartphone, tablet, or the computer and subsequent use. In the current triage model, the musculoskeletal triage system is operated by trained providers who alternated shifts to ensure continuous coverage. Patients who eventually required emergent in-person assessment were evaluated by the on-call resident and the supervising attending physician. Additional options for providing care included an 'on demand' or 'same day virtual visit', which provided near immediate sub-speciality evaluation. Of note, non-emergent virtual visits were incorporated into a half-day virtual/in-office alternating clinic schedule. This allowed for the most-efficient workflow and ensured responsible ancillary staff utilization. To further maximize time efficiency, clinic workload could be divided with graduated responsibility dependent on level/education of healthcare provider. Attending physicians and fellows are encouraged to receive new patients, while resident trainees and non-physician providers could provide supervised care for follow-up visits. While telehealth may be initially associated with decreased time efficiency due to lack of established guidelines and overall novelty, over time providers have become quickly acclimated to this new visit format.
The encounter
Patients and MSK care providers should be available online and on-time for MSKVC visits. Patients should check-in at least ten minutes before starting, and physicians should be notified via the online interface. It is important that the level of professionalism a patient would receive in the clinic is replicated within the virtual visit. To this end, a white coat/professional attire is recommended. Such professional attire is associated with high levels of patient satisfaction and increased patient scores rating physician knowledge, trustworthiness, care, and approachability.33 Patients are inviting us into their homes and often vice versa, so respect for the visualized environment is important to consider.
The chief complaint, history of present illness, current medications, allergies, and medical and surgical history should be obtained, as seen with typical in-office encounters. Under certain circumstances, patients may need to be accompanied by an aide such as a family member during the encounter whenever possible. Such measures would be contingent upon the patient's familiarity with the system, degree of education, compliance, and the nature of the disease. The patient's aide can help readjust the camera according to the provider instructions and if needed, help in conducting simple examination maneuvers according to the provider's direction. Notably, inability to perform a physical examination, as well as potentially compromised privacy in the presence of the patient’s aide, are hurdles that require further innovation.34 Baseline vitals such as heart rate/rhythm and BP can be obtained through telemedicine peripherals when available which include electronic stethoscopes and blood pressure cuffs, in addition to cell-phone based features that measure a multitude of vital signs.35 Patients can be individually queried for their own weight, although potential inter-reliability changes cannot be overlooked.
A major advantage conferred by MSKVC is the efficiency of the virtual encounter given the lack of travel, enabling providers and patients to make the most out of the interaction while affording synchronous electronic medical record documentation (Figure 4A, 4B). Notably, the additional time spent on electronic medical record documentation is associated with a significant diminution in the time dedicated to patient interaction,36 while virtual encounters highlights documentation as an integral part of the visit, especially given the electronic nature of the encounter.
Fig. 4.
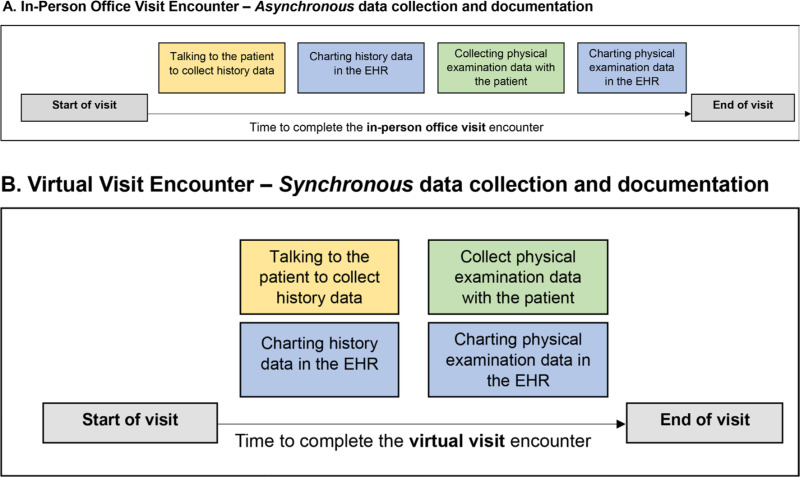
The time to complete an in-person office visit encounter (A) is dependent upon asynchronous collection and documentation of history and physical examination data in the electronic health record (EHR). Virtual visit encounters (B) allow for synchronous collection and documentation of history and physical examination data in the electronic health record (EHR), resulting in a shorter overall time to complete the entire encounter.
Billing
Medicare restrictions to virtual video visits have been a notorious detractor to widespread acceptance of MSKVC. Specifically, the law governing part B narrowed Medicare coverage of virtual visits to a mere 20% of its beneficiaries residing in rural areas.10 However, more recently, The Coronavirus Preparedness and Response Supplemental Appropriations Act has removed significant barriers to billing for telehealth encounters by allowing physicians and other health care professionals to bill Medicare fee-for-service during the COVID-19 health emergency.37,38 The marked flourishing of the telehealth sector highlights a much-needed reform in the billing process to reflect the provided service. Further billing reform regulations governing virtual healthcare provision is mandated to facilitate the routine use of MSKVC.
The value of going virtual beyond COVID-19
The potential for improved efficiency using a MSKVC triage model should be viewed in the context of that afforded by traditional musculoskeletal emergent care provision systems.6–8 Anderson et al39 retrospectively compared the waiting time, visit duration, and time to evaluation by an orthopaedic specialist among 12,722 patients presenting to dedicated musculoskeletal urgent care centres (MSKUC) versus the traditional ED in the USA. The authors described shorter waiting times (MSKUC: 17 minutes vs ED: 46 minutes; p < 0.05), visit durations (MSKUC: 43 minutes vs ED: 156 minutes; p < 0.05), and time to evaluation by an orthopaedic specialist (MSKUC: 1.2 days vs ED: 3.4 days; p < 0.05) when dedicated musculoskeletal urgent care centres were utilized. Nevertheless, the proposed virtual model holds potential in achieving several fold diminutions in the waiting time and time to evaluation by orthopaedic specialists compared to that currently afforded by urgent musculoskeletal care centres. Furthermore, improved efficiency would reflect on the pre-existing models of in-person care (ED and urgent care centres) via load mitigation and provide an initial impression and management plan, thereby enhancing efficiency.40–42 Such benefits are not provided at the expense of patient safety, as Rademacher et al43 outlined similar safety and efficacy between a matched cohort study of 1,933 patients receiving in-person screening versus 1,497 patients receiving tele-screening in the ED. Similarly, Mackenzie et al13 described the experience of the Edinburgh Trauma Triage Clinic by comparing outcomes of simple fractures of the radial head, little finger, and fifth metacarpal pre- and post-implementation of a consultant-led virtual triage unit. The authors confirmed previous findings, highlighting similar to better patient-reported outcomes among the virtually triaged cohort. Furthermore, mean cost per patient exhibited a four-fold decreased with the implementation of the virtual triage system.
The US healthcare system is transitioning to a value-based model, with emphasis on quality of healthcare provision, patient satisfaction, and outcomes.44,45 The Comprehensive Care for Joint Arthroplasty (CJR) is a national mandatory bundled-payment model for hip and knee arthroplasty that has been implemented in several metropolitan areas, with further expansion plans.46 Such a model provides compensation for joint arthroplasty based on net expenses incurred during a hospitalization episode followed by a 90-day post-discharge period. Therefore, the prospect of cost mitigation through virtual follow-up among low-risk patients for postoperative complications can drive further generalization of virtual care. Moreover, the stratification of high-risk patients according to personalized follow-up requirements can diminish unnecessary costs incurred by visits that could be safely virtualized. Buvik et al47 conducted an economic evaluation of remote orthopaedic consultations based on a randomized controlled trial of 559 consultations in 389 patients (video-assisted: n = 199 patients; standard outpatient consultation: n = 190 patients). The authors demonstrated that virtual orthopaedic and outpatient consults demonstrated similar gains in quality-adjusted life years (QALYs) despite diminished costs (an average of $75.30 lower) among the virtual consult cohort, as long as the number of patients receiving the service exceeded 151 annually. These findings conform to future US healthcare policies of expanding the healthcare provision net and decreasing costs while maintaining high levels of quality.
Conclusion
MSKVC is projected to experience an exponential rise in demand during and beyond the COVID-19 crisis. Applicable MSKVC will require integration of patient triaging into the proposed workflow. Such workflow dictates the continuous efficient interaction between various healthcare providers and patients in a virtual setting utilizing up-to-par physical setups and safe communication platforms. The value provided by MSKVC in both cost mitigation improving accessibility and equivalent safety, and patient satisfaction compared to its traditional outpatient counterparts, will drive the generalization of MSKVC in the field of orthopaedic surgery.
Footnotes
Author contributions: D. King: Drafted of manuscript, Collected and interpreted the data, Critically revised the draft, Designed the figures.
A. K. Emara: Drafted the manuscript, Collected and interpreted the data, Critically revised the draft, Designed the figures and tables.
M. K. Ng: Drafted the manuscript, Critically revised the draft, Collected the data.
P. J. Evans: Study conception and design, Critically revised the draft.
K. Estes: Study conception and design, Collected the data, Critically revised the draft.
K. P. Spindler: Study conception and design, Collected the data; Critically revised the draft, Suprevised the work.
T. Mroz: Study conception, Collected and interpreted the data, Supervised the work.
B. M. Patterson: Designed the study, Collected the data, Drafted the manuscript, Critically revised the draft.
V. E. Krebs: Acquired the data, Study conception, Critically revised the draft.
S. Pinney: Acquired and interpreted the data, Critically revised the draft.
N. S. Piuzzi: Study conception and design, Acquired, analyzed, and interpreted the data, Critically revised the draft.
J. L. Schaffer: Study conception and design, Acquired, analyzed, and interpreted the data, Critically revised the draft, Supervised the work.
Funding statement: No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
ICMJE COI statement: P. J. Evans reports being a paid presenter/speaker from Acumed, a board or committee member for the American Association for Hand Surgery and the American Society for Surgery of the Hand, a paid consultant and presenter/speaker from Axogen, IP royalties and being a paid presenter/speaker from Biomet, and IP royalties from Extremity Medical, Hely Weber and Innomed, stock/stock options from Lineage Medical, Nutek and Tenex, all of which are unrelated to this article.
V. E. Krebs reports being on the editorial or governing body of the Journal of Arthroplasty, IP royalties and being a paid presenter/speaker for Stryker, and being a paid consultant for Stryker Orthopaedics, all of which are unrelated to this article.
T. Mroz reports being a board or committee member for the Cervical Spine Research Society and the North American Spine Society, being on the editorial or governing board for SpineLine (Editor) and Global Spine Journal (Deputy Editor), having stock/stock options in PearlDiver, and IP royalties from Stryker, all of which are unrelated to this article.
B. M. Patterson reports being a board or committee member of the Orthopaedics Trauma Association, which is unrelated to this article.
S. Pinney reports being a board or committee member of the Codman Group, on the editorial and governing board of Foot and Ankle International, Foot and Ankle Orthoapedics, the Journal of Bone and Joint Surgery (American), and Techniques in Foot and Ankle Surgery, publishing royalties, financial or material support from FootEducation, and stock/stock options in LifeCycle Health, all of which are unrelated to this article.
N. S. Piuzzi reports being a board or committee member of ISCT and the Orthopaedic Research Society, on the editorial or governing board of the Journal of Hip Surgery and the Journal of Knee Surgery, and research support from RegenLab and Zimmer, all of which are unrelated to this article.
J. L. Schaffer reports being a paid consultant for MyDoc and Orthogenics, a paid consultant and stock/stock options from Compliant Innovations, stock/stock options from iBalance Medical and SnappSkin, and publishing royalties, financial or material support from Elsevier, all of which are unrelated to this article.
K. P. Spindler reports being a board or committee member for AAOS and the American Orthopaedic Society for Sports Medicine, a paid consultant for Cytori-Scientific Advisory Board, Flexion and Mitek, and research support from DJ Orthopaedics and National Institutes of Health (NIAMS and NICHD), all of which are unrelated to this article.
References
- 1. Williams AM, Bhatti UF, Alam HB, Nikolian VC. The role of telemedicine in postoperative care. Mhealth. 2018;4:11–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Adler-Milstein J, Kvedar J, Bates DW. Telehealth among US hospitals: several factors, including state reimbursement and licensure policies, influence adoption. Health Aff. 2014;33(2):207–215. [DOI] [PubMed] [Google Scholar]
- 3. Hollander JE, Carr BG. Virtually perfect? telemedicine for Covid-19. N Engl J Med. 2020;382(18):1679–1681. [DOI] [PubMed] [Google Scholar]
- 4. Bazin AA. Boyd’s OODA loop and the infantry company commander. Infantry Mag. 2005;94:17–19. [Google Scholar]
- 5. Haddad P, Schaffer JL, Wickramasinghe N. Evaluating business value of it in healthcare: three clinical practices from Australia and the US. Stud Health Technol Inform. 2015;216:183–187. [PubMed] [Google Scholar]
- 6. Schaffer JL, Haddad P, Wickramasinghe N. Measuring user satisfaction with clinical information systems: what really matters? Stud Health Technol Inform. 2017;245:1311. [PubMed] [Google Scholar]
- 7. Schaffer JL, Rasmussen PA, Faiman MR. The emergence of distance health technologies. J Arthroplasty. 2018;33(8):2345–2351. [DOI] [PubMed] [Google Scholar]
- 8. Schaffer JL, Zembo MM, Hamilton JJ, Isenman AW. Managing the academic orthopaedic practice as a business. Instr Course Lect. 2006;55:663–673. [PubMed] [Google Scholar]
- 9. Haukipuro K, Ohinmaa A, Winblad I, Linden T, Vuolio S. The feasibility of telemedicine for orthopaedic outpatient clinics--a randomized controlled trial. J Telemed Telecare. 2000;6(4):193–198. [DOI] [PubMed] [Google Scholar]
- 10. Wongworawat MD, Capistrant G, Stephenson JM. The opportunity Awaits to lead orthopaedic telehealth innovation: AOA critical issues. J Bone Joint Surg Am. 2017;99(17):e93. [DOI] [PubMed] [Google Scholar]
- 11. Lamberts H, Hofmans-Okkes I. Episode of care: A core concept in family practice. In: Journal of Family Practice . Vol. 1996;42:161–167. [PubMed] [Google Scholar]
- 12. Ferdinandus S, Smith LK, Pandit H, Stone MH. Setting up an arthroplasty care practitioner-led virtual clinic for follow-up of orthopaedic patients. Br J Nurs. 2019;28(20):1326–1330. [DOI] [PubMed] [Google Scholar]
- 13. Mackenzie SP, Carter TH, Jefferies JG, et al. Discharged but not dissatisfied: outcomes and satisfaction of patients discharged from the Edinburgh trauma triage clinic. Bone Joint J. 2018;100-B(7):959–965. [DOI] [PubMed] [Google Scholar]
- 14. Heinzelmann PJ, Williams CM, Lugn NE, Kvedar JC. Clinical outcomes associated with telemedicine/telehealth. Telemed J E Health. 2005;11(3):329–347. [DOI] [PubMed] [Google Scholar]
- 15. Sinha N, Cornell M, Wheatley B, Munley N, Seeley M. Looking Through a Different Lens. JAAOS Glob . Res. Rev. 2019;3:e100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Galey S, Cantrell WA, Magnuson JA, et al. Predicting the need for surgical intervention prior to first encounter for individuals with shoulder complaints: a unique approach. JSES International. 2020;4(1):207–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Vega JF, Strnad GJ, Bena J, Spindler KP. Predicting the need for surgical intervention prior to first encounter for individuals with knee complaints: a novel approach. Orthop J Sports Med. 2019;7:232596711985948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Baldwin L-M, Fischer MA, Powell J, et al. Virtual educational outreach intervention in primary care based on the principles of academic detailing. J Contin Educ Health Prof. 2018;38(4):269–275. Available at: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Conde JG, De S, Hall RW, et al. Telehealth innovations in health education and training. Telemed J E Health. 2010;16(1):103–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Pathipati AS, Azad TD, Jethwani K. Telemedical education: training digital natives in telemedicine. J Med Internet Res. 2016;18(7):e193–e193 10.2196/jmir.5534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Schaffer JL, Plona S, Omori S, Miller H, Harris CM. The consult is real, the visit is virtual. J Healthc Inf Manag. 2002;16(3):30–34. [PubMed] [Google Scholar]
- 22. Harris CM, Burns J, Gregorich T, et al. Managing technology in a complex healthcare delivery system. J Healthc Inf Manag. 2003;17(2):37–41. [PubMed] [Google Scholar]
- 23. Rao SP, Jayant NS, Stachura ME, Astapova E, Pearson-Shaver A. Delivering diagnostic quality video over mobile wireless networks for telemedicine. Int J Telemed Appl. 2009;2009:406753–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wickramasinghe N, Bali RK, Gibbons MC, Choi JHJ, Schaffer JL. A systematic approach: optimization of healthcare operations with knowledge management. J Healthc Inf Manag. 2009;23(3):44–50. [PubMed] [Google Scholar]
- 25. Jin Z, Chen Y. Telemedicine in the cloud era: prospects and challenges. IEEE Pervasive Comput.. 2015;14(1):54–61. [Google Scholar]
- 26. Kornak J. System Requirements for Delivery of Telemedicine Services. In: Telemanagement of Inflammatory Bowel Disease . Springer International Publishing. 2016:117–151. [Google Scholar]
- 27. Patricoski C, Ferguson AS. Selecting a digital camera for telemedicine. Telemed J E Health. 2009;15(5):465–475. [DOI] [PubMed] [Google Scholar]
- 28. Anon What are the basic technical requirements for telehealth?.
- 29. Anon Key changes made to telehealth guidelines to boost COVID-19 care | American Medical association.
- 30. Anon Telemedicine security and HIPAA.
- 31. Scavo C. The digital divide and E-Government in the United States. Int. J. eGovernance Networks. 2013;1:45–68. [Google Scholar]
- 32. Higgins CA, Conrath DW, Dunn E V, Toronto O. Provider Acceptance of Telemedicine Systems in Remote Areas of Ontario.. 1984.. [PubMed]
- 33. Petrilli CM, Saint S, Jennings JJ, et al. Understanding patient preference for physician attire: a cross-sectional observational study of 10 academic medical centres in the USA. BMJ Open. 2018;8(5):e021239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Dixon RF, Stahl JE. Virtual visits in a general medicine practice: a pilot study. Telemed J E Health. 2008;14(6):525–530. [DOI] [PubMed] [Google Scholar]
- 35. Weinstein RS, Krupinski EA, Doarn CR. Clinical examination component of telemedicine, telehealth, mHealth, and connected health medical practices. Med Clin North Am. 2018;102(3):533–544. [DOI] [PubMed] [Google Scholar]
- 36. Scott DJ, Labro E, Penrose CT, et al. The impact of electronic medical record implementation on labor cost and productivity at an outpatient orthopaedic clinic. J Bone Joint Surg Am. 2018;100(18):1549–1556. [DOI] [PubMed] [Google Scholar]
- 37. 116th Congress H.R.6074 - Coronavirus Preparedness and Response Supplemental Appropriations Act, 2020. 2020. https://www.congress.gov/bill/116th-congress/house-bill/6074/text?q=%7B%22search%22%3A%5B%22Coronavirus+Preparedness+and+Response+Supplemental+Appropriations+Act%22%5D%7D&r=1&s=1 (date last accessed 4/10/2020).
- 38. Supplemental R, Act A, Year BF, et al. Cbo estimate for H. R. 6074, the coronavirus preparedness and response supplemental Appropriations act, 2020, as posted on March 4, 2020 CBO estimate for H. R. 6074, the coronavirus preparedness and response supplemental Appropriations act. 2020;2021(2020):1–2. [Google Scholar]
- 39. Anderson TJ, Althausen PL. The role of dedicated musculoskeletal urgent care centers in reducing cost and improving access to orthopaedic care. J Orthop Trauma. 2016;30(Suppl 5):S3–S6. [DOI] [PubMed] [Google Scholar]
- 40. Murphy C, Mullen E, Hogan K, O’toole ronan, Teeling SP. Streamlining an existing hip fracture patient pathway in an acute tertiary adult Irish hospital to improve patient experience and outcomes. Int J Qual Heal Care. 2019;31(Supplement_1):45–51. 10.1093/intqhc/mzz093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Sander B, Elliot-Gibson V, Beaton DE, Bogoch ER, Maetzel A. A coordinator program in post-fracture osteoporosis management improves outcomes and saves costs. J Bone Joint Surg Am. 2008;90(6):1197–1205. [DOI] [PubMed] [Google Scholar]
- 42. Walters S, Khan T, Ong T, Sahota O. Fracture liaison services: improving outcomes for patients with osteoporosis. Clin Interv Aging. 2017;12:117–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Rademacher NJ, Cole G, Psoter KJ, et al. Use of telemedicine to screen patients in the emergency department: matched cohort study evaluating efficiency and patient safety of telemedicine. J. Med. Internet Res. 2019;21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Goldman AH, Kates S. Pay-For-Performance in Orthopedics: how we got here and where we are going. Curr Rev Musculoskelet Med. 2017;10(2):212–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Virk SS, Phillips FM, Khan SN. Bundled payment reimbursement for anterior and posterior approaches for cervical spondylotic myelopathy: an analysis of private payer and Medicare databases. J Neurosurg Spine. 2018;28(3):244–251. [DOI] [PubMed] [Google Scholar]
- 46. Barnett ML, Wilcock A, McWilliams JM, et al. Two-Year evaluation of mandatory bundled payments for joint replacement. N Engl J Med. 2019;380(3):252–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Buvik A, Bergmo TS, Bugge E, et al. Cost-Effectiveness of telemedicine in remote orthopedic consultations: randomized controlled trial. J Med Internet Res. 2019;21(2):e11330–e11330. [DOI] [PMC free article] [PubMed] [Google Scholar]


