Abstract
Introduction
The aim of this study is to report the 30 day COVID-19 related morbidity and mortality of patients assessed as SARS-CoV-2 negative who underwent emergency or urgent orthopaedic surgery in the NHS during the peak of the COVID-19 pandemic.
Method
A retrospective, single centre, observational cohort study of all patients undergoing surgery between 17 March 2020 and 3May 2020 was performed. Outcomes were stratified by British Orthopaedic Association COVID-19 Patient Risk Assessment Tool. Patients who were SARS-CoV-2 positive at the time of surgery were excluded.
Results
Overall, 96 patients assessed as negative for SARS-CoV-2 at the time of surgery underwent 100 emergency or urgent orthopaedic procedures during the study period. Within 30 days of surgery 9.4% of patients (n = 9) were found to be SARS-CoV-2 positive by nasopharyngeal swab. The overall 30 day mortality rate across the whole cohort of patients during this period was 3% (n = 3). Of those testing positive for SARS-CoV-2 66% (n = 6) developed significant COVID-19 related complications and there was a 33% 30-day mortality rate (n = 3). Overall, the 30-day mortality in patients classified as BOA low or medium risk (n = 69) was 0%, whereas in those classified as high or very high risk (n = 27) it was 11.1%.
Conclusion
Orthopaedic surgery in SARS-CoV-2 negative patients who transition to positive within 30 days of surgery carries a significant risk of morbidity and mortality. In lower risk groups, the overall risk of becoming SARS-CoV-2 positive, and subsequently developing a significant postoperative related complication, was low even during the peak of the pandemic. In addition to ensuring patients are SARS-CoV-2 negative at the time of surgery it is important that the risk of acquiring SARS-CoV-2 is minimized through their recovery.
Cite this article: Bone Joint Open 2020;1-8:474–480.
Keywords: OrthopaedicSurgery, Morbidity, Mortality, Patient Outcomes, COVID-19, SARS-CoV-2
Introduction
In December 2019 an outbreak of coronavirus disease 2019 (COVID-19) caused by a novel coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was recognized in Wuhan, China.1 Over the following 3 months the virus spread globally and on 11 March 2020 was declared a pandemic by the World Health Organization (WHO). In the UK, due to the increase in reported cases and the impending demand on NHS critical care pathways, all elective surgery in the NHS ceased on 15 April 2020.2 Emergency and urgent surgical cases continued as local resources allowed.
Emerging data on the outcomes of surgery in patients who are screened as SARS-CoV-2 positive in the seven days prior to surgery has reported a 30 day mortality rate of 21.2%, with 30 day mortality rates of up to 40% in those who develop respiratory complications.3,4 In particular, in adjusted analyses, male sex, age 70 years or greater, American Society of Anesthesiologists5 grade 3 or greater, major surgery and emergency surgery have been identified as presenting the highest risk of mortality.4
As the UK is now past the peak of COVID-19, the UK government has asked hospitals to attempt to return to elective surgery.6 This should be undertaken in hospitals using clinical pathways where patients are screened for COVID-19 prior to undertaking surgery and risk is reduced by operating on patients who are believed to be at lower risk of COVID-19 complications.7,8 However, as yet there is no published data on the outcome of patients who are believed to be COVID-19 negative following preoperative screening. This lack of data adversely affects shared decision making for patients and clinical teams, where the decision to undergo surgery depends on the balance between benefit and risk.9,10 If elective surgery is to be restarted, there is a critical need for short-term outcome data of patients who are believed to be COVID-19 negative at the time of surgery to help develop safe patient pathways and provide data to inform shared decision making for elective surgery when COVID-19 remains in circulation.
The aim of this study is to report the 30 day COVID-19 related morbidity and mortality of patients assessed as COVID-19 negative through screening who underwent emergency or urgent surgery in the NHS during the peak of the COVID-19 pandemic.
Methods
A retrospective, single centre, observational cohort study of all patients undergoing orthopaedic surgery under general or regional anaesthetic between 17 March 2020 and 3 May 2020 was performed. Outcomes were stratified by British Orthopaedic Association (BOA) COVID-19 Patient Risk Assessment Tool.7 Patients considered COVID-19 positive at the time of surgery, based on nasopharyngeal swab positive for SARS-CoV-2 viral RNA or symptoms suggestive of COVID-19 in the absence of a negative nasopharyngeal swab result at the time of surgery, were excluded from the analysis. The study was approved by the local audit committee.
Participants
The Nuffield Orthopaedic Centre (NOC) is a tertiary referral centre providing services for all orthopaedic specialties including treatment of sarcoma. Trauma, excluding peri-prosthetic and malignant pathological fractures who are treated at the NOC, are managed under the care of the Trauma Unit based at the John Radcliffe Hospital. The NOC stands on a separate site to other NHS hospitals. It also provides rheumatology, sports medicine, and clinical genetics services but does not have any general medical or respiratory wards. Following the WHO declaring COVID-19 a pandemic on 11 March 2020, all non-cancer elective activity stopped at our trust on 17 March 2020. During the study period we continued to run surgical lists for patients who required emergency or urgent orthopaedic surgery requiring general or spinal anaesthesia and these patients form our study group.
There were three routes of admission to the NOC for emergency or urgent orthopaedic surgical care: emergency admission, planned urgent admission or transfer from another centre or MDT admission via the tumour service, or bone infection service (Figure 1). Emergency admissions from the on-call emergency patient pathway had direct admission to the NOC. Planned admissions were patients, already on treatment pathways, who were admitted to the NOC for urgent surgery. Tumour service cases were discussed at MDT with this service continuing in line with national guidance following NHS guidelines. The local peak of COVID-19, as assessed by the number of inpatients at our trust, occurred during the first half of April 2020 (Figure 2).
Fig. 1.
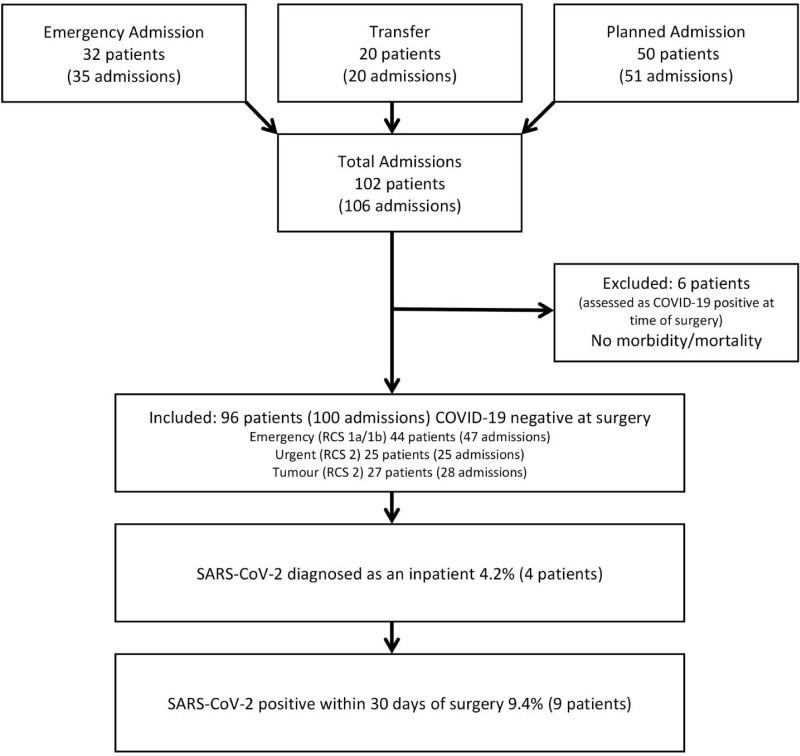
Study flow.
Fig. 2.
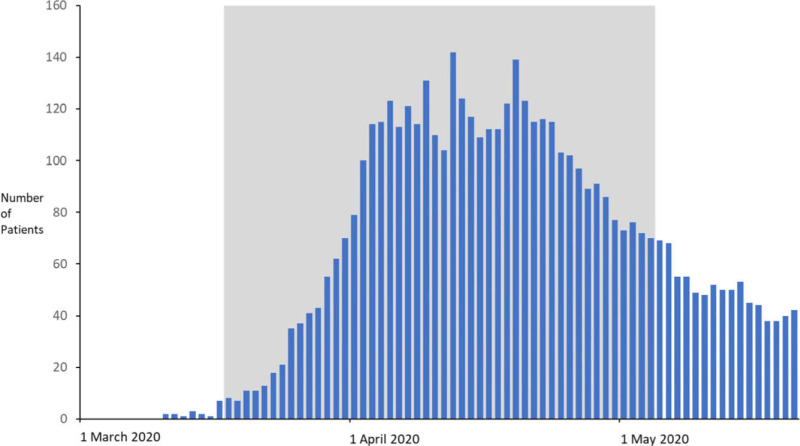
Local inpatient caseload across our trust during study period (grey).
Details of study group
A total of 102 patients (106 admissions, 106 operations) underwent surgery during the study period (Figure 1). Two patients were admitted twice and each time underwent surgery; one case was a revision total knee arthroplasty that subsequently required debridement, antibiotics and implant retention (DAIR) the other case was excision of sarcoma with flap reconstruction that subsequently required debridement and antibiotics. One patient was admitted three times and underwent three operations; their primary procedure was excision of sarcoma that required revision surgery for incomplete margins followed by debridement and antibiotics.
Exclusions
Six patients, all emergency cases, were excluded from the analysis as at presentation they had symptoms suggestive of COVID-19 but results of their SARS-CoV-2 nasopharyngeal swab were not back at the time of surgery. Ultimately, all swabs returned a negative result and no morbidity or mortality was reported in this group.
Patient demographics and surgery details
Of the 96 patients (100 admissions, 100 operations) who were assessed as negative for COVID-19 at the time of surgery, there were an equal proportion of men and women, with a mean age of 63.2 years (SD 19.8) (Table I). BOA risk stratification classified 28% (n = 27) as High or Very High risk with 46% (n = 44) being ASA 3 or above (Table I). Overall, of the 100 operations, 47% of procedures (n = 47) were classified as emergency cases (19% (n = 19) Category 1a and 28% (n = 28) Category 1b) and 53% (n = 53) as urgent, Category 2, cases according to the Royal College of Surgeons Classification8 (Figure 1, Table II). In total, 70% of operations (n = 70) were conducted under general anaesthesia and 30% (n = 30) were under regional anaesthesia.
Table I.
Demographic details of included patients.
| Characteristic | Patients (n = 96) |
| Mean age, yrs (SD) | 63.2 (19.8) |
| Male, n (%) | 48 (50.0) |
| Mean BMI, kg/m2 (SD) | 27.8 (6.7) |
| ASA grade, n (%) | |
| 1 | 9 (9.4) |
| 2 | 43 (44.8) |
| 3 | 39 (40.6) |
| 4 | 5 (5.2) |
| BOA risk, n (%) | |
| Low | 32.3 (31) |
| Medium | 38 (39.6) |
| High | 20 (20.8) |
| Very High | 7 (7.3) |
ASA, American Society of Anaesthesiologists; BMI, body mass index; BOA, British Orthopaedic Association.
Table II.
Details of surgeries performed classified by Royal College of Surgeons (RCS) Prioritisation8.
| RCS category | n (%) | Indication | Procedure |
| 1a | 19 (19) | Prosthetic joint infection | DAIR (5) Single stage revision (2) |
| Dislocated prosthetic joint | Closed reduction (5) Open reduction (1) |
||
| Limb threatening infection | Debridement (4) | ||
| Native joint infection | Arthroscopic debridement (1) Open debridement (1) |
||
| 1b | 28 (28) | Periprosthetic fracture | Revision prosthesis (11) |
| Limb threatening infection | Debridement (4) | ||
| Haematoma | Exploration and washout (4) | ||
| Infected metalwork | Removal metal and debridement (3) | ||
| Prosthetic joint infection | DAIR (1) Single stage revision (2) |
||
| Other | Other (3) | ||
| 2 | 53 (53) | Bone or soft tissue tumour | MDT directed treatment (27) |
| Prosthetic joint infection | Second stage revision (5) | ||
| Aseptic loosening prosthesis | Single stage revision (3) Exploration of prosthesis (1) |
||
| Locked knee | Arthroscopic repair/resection (3) | ||
| Osteomyelitis | Debridement (2) | ||
| Completed deformity correction | Removal of frame (2) | ||
| Other | Other (10) |
DAIR, debridement, antibiotics, irrigation, and retention; MDT, multidisciplinary team.
Assessment of COVID-19 status
On admission, all patients were screened for signs and symptoms of COVID-19 using standardized screening questions (recent high temperature, new or worse than usual continuous cough, breathing difficulties, coryzal/flu symptoms, systemic upset, recent travel, recent contact with suspected or confirmed COVID-19, and, from April 2020, anosmia). In addition, a set of clinical observations was performed by the admitting nurse. Between 17 March and 27 April 2020, a nasopharyngeal swab for SARS-CoV-2 was taken, when screening questions were positive, or clinical observations deviated from normal values. From 28 April onwards, all patients admitted to the NOC were swab tested. For planned admissions from home and transfers from outside centres, screening questions and nasopharyngeal swabs, where indicated, were performed prior to transfer with patients not transferred to our centre until the result was known. While an inpatient, nasopharyngeal swabs for SARS-CoV-2 viral RNA were performed if patients developed new signs or symptoms of COVID-19. Nasopharyngeal swabs for SARS-CoV-2 were performed on discharge if the patient was to be discharged to a community hospital or nursing home.
All patients were followed after discharge via their electronic record for patients in region, and telephone call for patients out of region, up to 30 days from surgery establishing whether they were tested for SARS-CoV-2 outside the NOC, were readmitted to hospital, developed COVID-19 related complications or died.
Decision to proceed with surgery
Patients were prioritized using the Royal College of Surgeons Priority guidelines.8 The final decision to proceed with surgery was made as a shared decision between the patient and the treating consultant. In emergency cases, by definition, it was felt that surgery should be performed with little, or in some cases, no delay. In these cases, the final results of the COVID-19 screening process may not have been available at the time of surgery, but the need to proceed with surgery took precedence. We are not aware of any patients who had clinical symptoms suggestive of COVID-19 infection, but if this scenario occurred it was proposed that surgery was deferred until symptoms had resolved, regardless of the test results for SARS-CoV-2 viral RNA.
Outcomes
The primary outcome was 30-day mortality following surgery. Secondary outcomes included COVID-19 related morbidity including pneumonia, acute respiratory distress syndrome (ARDS), or unexpected postoperative ventilation. Where patients were diagnosed as COVID-19 positive within the 30 day postoperative period we extended the period of follow-up to establish their final outcome. Data were retrieved from our electronic patient records (Cerner Millennium, Missouri, USA) with mortality data retrieved from the NHS spine.
Results
COVID-19 status post-surgery
Of the 96 patients who were assessed as COVID-19 negative at the time of surgery 32% (31 patients) developed signs or symptoms of COVID-19 as an inpatient and had a nasopharyngeal swab for SARS-CoV-2 performed prior to discharge. Overall 4.2% (4 patients) were confirmed as SARS-CoV-2 positive prior to discharge (Figure 1). Following discharge, a further 11.5% (11 patients) developed signs or symptoms of COVID-19 within 30 days of discharge. Of the 92 patients who on discharge were SARS-CoV-2 negative, five (5.2%) were confirmed as SARS-CoV-2 positive by nasopharyngeal swab with 30 days of operation (Figure 1). Overall 9.4% (nine patients) of patients were confirmed as SARS-CoV-2 by nasopharyngeal swab within 30 days of surgery [Table III]. The demographics of patients who remained SARS-CoV-2 negative at 30 days and those who did not are listed in Table III. Of those patients who had general anaesthesia 10.3% (n = 7) tested positive for SARS-CoV-2 within 30 days of surgery compared to 7.1% (n = 2) in those who had regional anaesthesia.
Table III.
Demographic details of included patients based on COVID-19 status at 30 days postoperation stratified by COVID-19 morbidity and mortality.
| Variable | COVID-19 negative (n = 87) | COVID-19 positive (n = 9) | COVID-19 positive, no morbidity/mortality (n = 3) | COVID-19 positive, with morbidity (n = 6) | COVID-19 positive, with mortality (n = 3) |
| Mean age, yrs (range) | 61.72 (17 to 91) | 77.11 (59 to 88) | 75.67 (67 to 80) | 77.83 (59 to 88) | 81.67 (70 to 88) |
| Mean BMI, kg/m2 (range) | 27.85 (16.78 to 60) | 26.35 (19.26 to 33.63) | 23.56 (19.26 to 29.3) | 27.75 (20.96 to 33.63) | 28.26 (22.07 to 32.5) |
| Male, % | 52.9 | 22.2 | 33.3 | 16.7 | 0 |
| ASA 3 or greater, % | 44.8 | 55.6 | 33.3 | 66.7 | 100 |
| BOA High or Very High, % | 27.6 | 55.6 | 33.3 | 66.7 | 100 |
ASA, American Society of Anaesthesiologists; BMI, body mass index; BOA, British Orthopaedic Association.
COVID-19-related complications and mortality
The overall mortality across the whole cohort assessed as negative for COVID-19 at the time of surgery was 3%. Of the nine patients confirmed as SARS-CoV-2 positive following surgery, 67% (six patients) developed a postoperation complication, all viral pneumonia, that was attributable to COVID-19. In patients confirmed as SARS-CoV-2 positive following surgery, the 30-day mortality was 33% (three patients). The COVID-19 related mortality and morbidity stratified by BOA COVID-19 Patient Risk Assessment is listed in Table IV. Of those seven patients who tested positive for SARS-CoV-2 and who had general anaesthetic, the COVID-19 related morbidity (including those who ultimately died), was 71.4% (n = 5) and mortality, all due to viral pneumonia, 42.9% (n = 3) compared to a COVID-19 related morbidity of 50% (n = 1) and mortality of 0% in those two patients who tested positive for SAS-CoV-2 and who underwent regional anaesthetic.
Table IV.
COVID-19 mortality and morbidity by British Orthopaedic Association (BOA) COVID-19 Patient Risk Assessment.
| BOA risk | COVID-19 morbidity, n (%) (n = 6) | COVID-19 mortality, n (%) (n = 3) |
| Low (n = 31) | 0 (0) | 0 (0) |
| Medium (n = 38) | 2 (5.3) | 0 (0) |
| High (n = 20) | 2 (10.0) | 2 (10) |
| Very High (n = 7) | 2 (28.6) | 1 (14.3) |
BOA, British Orthopaedic Association.
All mortalities were female, aged 70 years or older, ASA 3 and assessed as high or very high risk using the BOA Risk Categorization. One patient underwent surgery for a high grade leiomyosarcoma, one for a Vancouver B211 periprosthetic hip fracture and one a single stage revision hip arthroplasty for infection. All patients were swabbed negative for SARS-CoV-2 following surgery at our institution before testing positive for SARS-CoV-2 at day 11, day 22 and day 24 respectively. One patient died as an inpatient and two patients had been discharged, both to a community hospital. Following a positive swab for SARS-CoV-2, death occurred at 14 days, 3 days and 15 days respectively.
Discussion
In a cohort of 96 patients assessed as negative for COVID-19 at the time of surgery who underwent 100 emergency or urgent orthopaedic procedures during the COVID-19 pandemic 9.4% (nine patients) were found to be SARS-CoV-2 positive by nasopharyngeal swab by 30 days after operation. The overall 30-day mortality rate across the whole cohort of patients during this period was 3%. Of those testing positive for SARS-CoV-2 66% (six patients) developed significant COVID-19 related complications and there was a 33% (three patients) 30 day mortality rate. The COVID-19 related morbidity and mortality was 2.9% and 0% respectively in British Orthopaedic Association COVID-19 Patient Risk Assessment low and medium risk patients and 14.8% and 11.1% in high and very high risk patients.
The emerging data indicate that SARS-CoV-2 infection at the time of surgery is associated with a high mortality.3,4 Furthermore, there is some data that infection during the postoperative period, (within 30 days of surgery) carries a similar risk of mortality, with rates of up to 25% reported.4 Our data have confirmed that while overall the mortality across our cohort was low, in those that were diagnosed as SARS-CoV-2 positive within 30 days of surgery it was 33%. The relevance of this is that when considering the risk versus benefit of operative intervention, in addition to considering a patient’s SARS-CoV-2 status at base line, it also important to consider a patients risk of acquiring symptomatic SARS-COV-2 during their postoperative recovery, as this may also present a significant risk to life.
There are very few studies to date that report the results of surgery performed in patients screened and considered COVID-19 negative prior to surgery. The focus of other studies has been on the outcomes of patients who are COVID-19 positive at the time of surgery where mortality rates of 21% have been previously reported.3,4 In our study we identified a transition rate from SARS-CoV-2 negative to positive following surgery of 9.4% within 30 days, with around half of cases being detected as an inpatient and half as a outpatient. This data is consistent with data reported by the COVIDSurg collaborative, where over half of inpatient COVID-19 diagnosis were postoperative.4 While our hospital does not have any general medical wards, nor ICU, during the study period our hospital provided rehabilitation for trauma patients as well as looked after patients with hip fractures presenting a risk of patient to patient transmission. In addition healthcare workers present a risk, both as an inpatient and outpatient and it is known that the incidence of SARS-CoV-2 in healthcare workers shadows the patient population that they treat and in around a third of cases it is asymptomatic.12 This highlights that healthcare acquired SARS-CoV-2 presents a risk to patients and that, in addition to ensuring that patients do not have SARS-CoV-2 at the time of surgery, specific attention should be placed on the postoperative pathway to include minimizing inpatient stay, minimizing healthcare contacts, and recommending isolation in the immediate postoperative period.
Patients who transitioned from SARS-CoV-2 negative to positive during the study period had a mean age that was 15 years older than those who remained negative and had more medical comorbidities, as assessed by ASA and BOA Risk Assessment. Death from SARS-CoV-2 pneumonia occurred in the oldest (mean age 82 years) and most frail in the cohort, with all being ASA grade 3 or greater and assessed as high or very high risk using the BOA assessment. While increasing age and comorbidity infer an increased risk of mortality following both surgery and infection with SARS-CoV-2, the relationship between surgery and SARS-CoV-2 with respect to the impact on mortality has yet to be fully defined. Nonetheless, despite our small numbers, our study has highlighted that in addition to being more likely to acquire COVID-19 following surgery, older, more comorbid patients are more likely to have COVID-19 associated morbidity and mortality. Therefore, there should be specific consideration to the potential additional risk when considering urgent or elective surgery in this population. While the numbers were too small to permit meaningful statistical analysis anaesthetic strategy may also have an impact outcomes following surgery with patients receiving general anaesthesia having around a 50% higher incidence of SARS-CoV-2 and COVID-19 related morbidity at 30 days with all deaths occurring in the general anaesthesia group. Due the potential for confounders further data are required to confirm these findings.
There are some methodological issues that must be addressed in interpreting the results. The study represents a small cohort of patients and the results might not be generalizable to the wider population. However at present there are very few, if any, reports of orthopaedic surgery performed in patients who are COVID-19 negative prior to surgery. This study offers an important early view of the potential level of risk associated with orthopaedic surgery in this group of patients. Within the study group, screening for COVID-19 negative status was performed with a history and examination with a throat and nose swab test reserved for those who were symptomatic, for the majority of the cohort. Towards the end of the study period all admissions were tested. Therefore it is possible that some of the patients in the cohort were screened with a false negative result, either due to their asymptomatic state or failure of the test to identify them. This would mean that they were presumed COVID-19 negative because they were asymptomatic and underwent surgery, despite actually being COVID-19 positive. Testing of all patients, as currently happens in elective ‘green pathways’, may have reduced the number of false-negative cases but would not have completely excluded them.
Despite the relatively small number of cases in this study, the results offer some insight into the outcome of patients who are screened COVID-19 negative at the time of surgery. It is useful to see that in the early postoperation period, very few patients developed COVID-19-related complications. Our hospital is a specialist orthopaedic unit which does not admit patients for treatment of respiratory diseases and has no intensive care unit and as such, at the time of the study, may have been regarded as a low risk for transmission of SARS-CoV-2 within the hospital. Despite this, 4.2% of patients were SARS-CoV-2 positive on discharge. The risk may be higher for orthopaedic patients treated alongside elderly patients with medical comorbidities, respiratory disease, or Covid-19. This early evidence suggests that when planning a “safe” pathway, not only should we confirm COVID-19 negative status preoperatively, but it is also critical to establish a safe environment for patients during their recovery in hospital and rehabilitation post-discharge. This pathway should include minimizing inpatient stay and recommending isolation in the immediate postoperative period, with this combined approach potentially reducing the risk of contracting COVID infection.13
This study reports outcome in emergency and urgent orthopaedic cases, where there is a clear necessity to perform surgery. However, these observations also raise important questions when considering the reintroduction of primary elective orthopaedic surgery where the decision to undergo surgery is discretionary and balanced around risk and benefit. The emerging data suggest that for patients in the highest risk groups of a poor outcome, if they contract COVID-19, the increased level of risk may make the decision of proceeding with surgery more challenging and should be fully discussed as part of a shared decision making process. This re-emphasises the requirement to develop safe pre- and postoperative pathways.
In conclusion, this study establishes that orthopaedic surgery in COVID-19 negative patients carries significant risks in those patients who become COVID-19 positive after their surgery, particularly in the known high risk groups where 30-day mortality exceeds 30%. In lower risk groups, the overall risk of becoming COVID-19 positive and subsequently developing a significant postoperation COVID-19 related complication is much lower. Further research is required to define how elective surgical pathways can be optimized and more clearly establish the risks of developing COVID-19 related comorbidity after surgery.
Acknowledgements
COVID-19 NOC surgical team
Rasheed Afinowi-Luitz FRCS, Consultant Orthopaedic Surgeon,
Bessam Ahmed FRCS (Trauma & Orthopaedics), Orthopaedic Fellow,
Khalid Al-Dadah FRCS (Trauma & Orthopaedics), Orthopaedic Fellow,
Simon Aquilina MD MRCS MSc, Orthopaedic Trainee,
Karen Barker MSc PhD FCSP, Clinical Director Trauma & Orthopaedics,
Oxford University Hospitals NHS Foundation Trust
Nicholas Beresford-Cleary MBChB BEng FRCS (Trauma & Orthopaedics), Orthopaedic Fellow,
Halimatou Bourdanne MD Orthopaedic Trainee,
Nicholas Bottomley FRCS, Consultant Orthopaedic Surgeon,
Harriet A Branford White MBChB MRCS DPhil (Oxon) FRCS (Trauma & Orthopaedics)
Rick Brown FRCS, Consultant Orthopaedic Surgeon,
Bedansh Chaudary FRCS, Consultant Orthopaedic Surgeon,
Thomas Cosker FRCS, Consultant Orthopaedic Surgeon,
Paul Critchley FRCS, Consultant Plastic Surgeon,
Abd-Allah El Ashmawy MCh Orth PhD FRCS (Trauma & Orthopaedics), Orthopaedic Fellow,
Jamie Ferguson FRCS, Consultant Orthopaedic Surgeon,
Anton Fries FRCS, Consultant Plastic Surgeon,
Max Gibbons FRCS, Consultant Orthopaedic Surgeon,
Siôn Glyn-Jones FRCS, Consultant Orthopaedic Surgeon,
Sean Grannum FRCS, Consultant Orthopaedic Surgeon,
Peter Hambly FRCA, Consultant Anaesthetist,
Daniel J Howgate MBChB BSc (Hons) FRCS (Trauma & Orthopaedics) Orthopaedic Trainee,
William Jackson FRCS, Consultant Orthopaedic Surgeon,
Johann A Jeevaratnam FRCS (Plastic Surgery), Plastics Fellow,
Ryan L Kerstein FRCS (Plastic Surgery), Plastics Fellow,
Jennifer C E Lane MA MEd MRCS Orthopaedic Trainee,
Constantinos Loizou FRCS, Consultant Orthopaedic Surgeon,
Daniel Markeson MBBS MD (Res) FRCS(Plastic Surgery), Plastics Fellow,
Martin McNally FRCS, Consultant Orthopaedic Surgeon,
Ross L Muir, BMBCh MSc FRCS (Orthopaedics & Trauma), Orthopaedic Fellow,
Richard W Myatt BMedSci BMBS Orthopaedic Trainee,
Andreas Naparus MBBS, Plastics Fellow,
Simon Newman FRCS, Consultant Orthopaedic Surgeon,
Colin Ng MD FRCS (Trauma & Orthopaedics), Orthopaedic Trainee,
Tasos Panagiotou FRCS(Trauma & Orthopaedics), Orthopaedic Fellow,
Alex Ramsden FRCS, Consultant Plastic Surgeon,
Raja Bhaskara RajasekaranMS DNB FNB, Orthopaedic Fellow,
Claire Sethu, BM MRCS, Plastics Fellow,
Bob Sharp FRCS, Consultant Orthopaedic Surgeon,
Ather Siddiqui, FRCS (Orthoapedics & Trauma), Orthopaedic Fellow,
David Stubbs FRCS, Consultant Orthopaedic Surgeon,
Tom Stevenson MBBS MRCS PhD, Orthopaedic Trainee,
Adrian Taylor FRCS, Consultant Orthopaedic Surgeon,
Chrishan Thakar FRCS, Consultant Orthopaedic Surgeon,
Kenneth M Vaz MD, Orthopaedic Fellow,
Duncan Whitwell FRCS, Consultant Orthopaedic Surgeon,
Nuffield Orthopaedic Centre
Footnotes
Author contributions: A. Price: Involved in the surgery and documentation of the primary data, Analyzed and interpreted the data, Drafted and critically reviewed the manuscript.
A. D. Shearman: Involved in the surgery and documentation of the primary data, Completed the data collection, Analyzed and interpreted the data, Drafted and critically reviewed the manuscript.
T. W. Hamilton: Involved in the surgery and documentation of the primary data, Analyzed and interpreted the data, Drafted and critically reviewed the manuscript.
A. Alvand: Involved in the surgery and documentation of the primary data, Analyzed and interpreted the data, Drafted and critically reviewed the manuscript.
B. Kendrick: Involved in the surgery and documentation of the primary data, Analyzed and interpreted the data, Drafted and critically revised the manuscript.
Funding statement: No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Zhu H, Wei L, Niu P. The novel coronavirus outbreak in Wuhan, China. Glob Health Res Policy. 2020;5:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Iacobucci G. Covid-19: all non-urgent elective surgery is suspended for at least three months in England. BMJ. 2020;368:m1106. [DOI] [PubMed] [Google Scholar]
- 3. Lei S, Jiang F, Su W, et al. . Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine. 2020;100331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. COVIDSurg Collaborative Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020;396(10243):27–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Saklad M. Grading of patients for surgical procedures. Anesthesiology. 1941;2(3):281–284. [Google Scholar]
- 6. Stevens SS, Pritchard A. Second phase of NHS repsonse to COVID-19. NHS. 2020. https://www.england.nhs.uk/coronavirus/publication/second-phase-of-nhs-response-to-covid-19-letter-from-simon-stevens-and-amanda-pritchard/ (date last accessed 27 July 2020).
- 7. No authors listed Re-starting non-urgent trauma and orthopaeedic care: Summary guidance. British Orthopaedic Association. 2020. https://www.boa.ac.uk/uploads/assets/9383a53f-36d8-4782-8fe264c691b39b15/BOA-Guidance-for-restart-full-doc-final2-v11.pdf (date last accessed 27 July 2020).
- 8. No authors listed Clinical Guide to Surgical Prioritisation during the Coronavirus Pandemic.. Royal College of Surgeons. 2020. https://www.rcseng.ac.uk/-/media/files/rcs/coronavirus/surgical-prioritisation-under-covid19-26-june.pdf (date last accessed 27 July 2020).
- 9. Dieppe P, Lim K, Lohmander S. Who should have knee joint replacement surgery for osteoarthritis? Int J Rheum Dis. 2011;14(2):175–180. [DOI] [PubMed] [Google Scholar]
- 10. Oussedik S, Zagra L, Shin GY, et al. . Reinstating elective orthopaedic surgery in the age of COVID-19. Bone Joint J. 2020;102-B(7):807–810. [DOI] [PubMed] [Google Scholar]
- 11. Brady OH, Garbuz DS, Masri BA, Duncan CP. Classification of the hip. Orthop Clin North Am. 1999;30(2):215–220. [DOI] [PubMed] [Google Scholar]
- 12. Treibel TA, Manisty C, Burton M, et al. . COVID-19: PCR screening of asymptomatic health-care workers at London Hospital. Lancet. 2020;395(10237):1608–1610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lazizi M, Marusza CJ, Sexton SA, Middleton RG. Orthopaedic surgery in a time of COVID-19. Bone Joint Open. 2020;1(6):229–235. [DOI] [PMC free article] [PubMed] [Google Scholar]


