Abstract
Aims
This study aimed to identify patients receiving total hip arthroplasty (THA) for trauma during the peak of the COVID-19 pandemic in the UK and quantify the risks of contracting SARS-CoV-2 virus, the proportion of patients requiring treatment in an intensive care unit (ICU), and rate of complications including mortality.
Methods
All patients receiving a primary THA for trauma in four regional hospitals were identified for analysis during the period 1 March to 1 June 2020, which covered the current peak of the COVID-19 pandemic in the UK.
Results
Overall, one of 48 patients (2%) contracted COVID-19 during their admission. Although they required a protracted stay in hospital, they did not require ICU treatment. Two patients did require ICU support for medical problems but not relating to COVID-19. Complications were no greater than expected given the short follow-up. There were no mortalities.
Conclusion
There is a paucity of evidence to guide restarting elective joint arthroplasties following the COVID-19 pandemic. Although THAs for trauma are by no means a perfect surrogate, the results of this study show a low incidence of contracting COVID-19 virus during admission and no significant sequalae during this period.
Cite this article: Bone Joint Open 2020;1-7:438–442.
Keywords: COVID-19, Total hip arthroplasty, Fractured neck of femur
Introduction
The COVID-19 pandemic has profoundly affected the delivery of medical services across the globe. In an attempt to conserve resources, all elective operating in the UK was phased out between March and April 2020.1 As a result, many patients are now facing a longer waiting times for life-changing joint arthroplasty surgery, such as total hip arthroplasties (THAs).
Where emergency surgery has taken place during the COVID-19 incubation period, it is associated with a high risk of exposure to the SARS-CoV-2 virus. Among patients who contract it, pulmonary complications have been recorded in up to 50% of cases and the 30-day mortality may be as high as 24%.2,3
Restarting elective surgery will be a complex process, and research is required to guide policy decisions.4 The risks associated with planned orthopaedic surgery and specifically arthroplasty have not yet been established.5,6 Although no elective THAs were carried out in the UK during the pandemic, a small number were indicated for trauma patients with displaced intracapsular femoral neck fractures.5 This provides an opportunity to study early outcomes following hip arthroplasty surgery in the COVID-19 era, and offers insights into the challenges faced by resuming elective services following the pandemic.
The aim of this paper therefore was to quantify the risk to patients undergoing THA for neck of femur fractures during the peak of the COVID-19 pandemic. Primary outcome measures were inpatient death, admission to an intensive care unit (ICU), and positive SARS-CoV-2 test as an inpatient. Secondary outcome measures included length of stay and early complications, including periprosthetic fracture, dislocation, and infection.
Methods
Four hospitals within the Wessex region of the UK participated in this study, including the major trauma centre and three district general hospitals. Local departmental approval for the study was obtained. Patients were identified by surgeons at each hospital analyzing admission records, theatre databases, and postoperative x-rays. Patients were included if they underwent a primary THA for a displaced intracapsular neck of femur fracture during the period 1 March to 1 June 2020. This period corresponded with the most significant phase of the COVID-19 outbreak so far in this country (Figure 1).6 Patients undergoing THA for pathological or periprosthetic fractures were excluded. Details were gathered on patient demographics, time to surgery, and SARS-CoV-2 status taken from swabs on admission and throughout their inpatient stay.
Fig. 1.
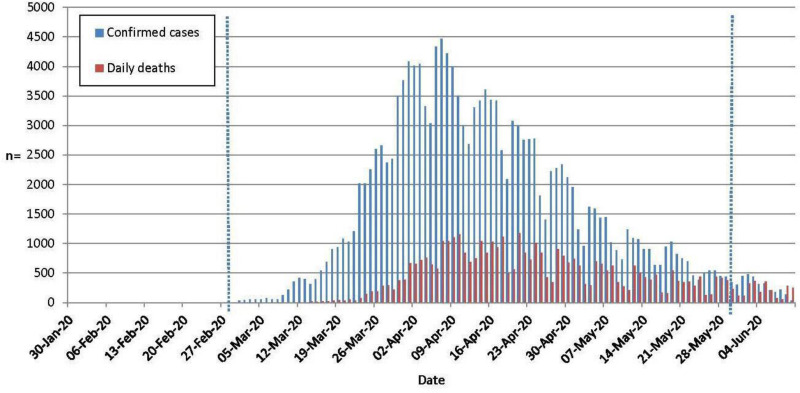
Confirmed SARS-CoV-2 cases and COVID-19-associated deaths.7 1 March to 1 June 2020 indicated.
Patients and implants
In all, 48 patients met the inclusion criteria and underwent a primary THA for displaced intracapsular neck of femur fracture during the study period. The mean age was 73 years (56 to 90); 34 (71%) were female, and 14 (29%) were male. The median time from admission to surgery was two days (interquartile range (IQR) 4). A variety of prostheses were used (Figure 2); the majority of patients (32/48, 67%) received a hybrid THA (CPT/Exeter Hip system).
Fig. 2.
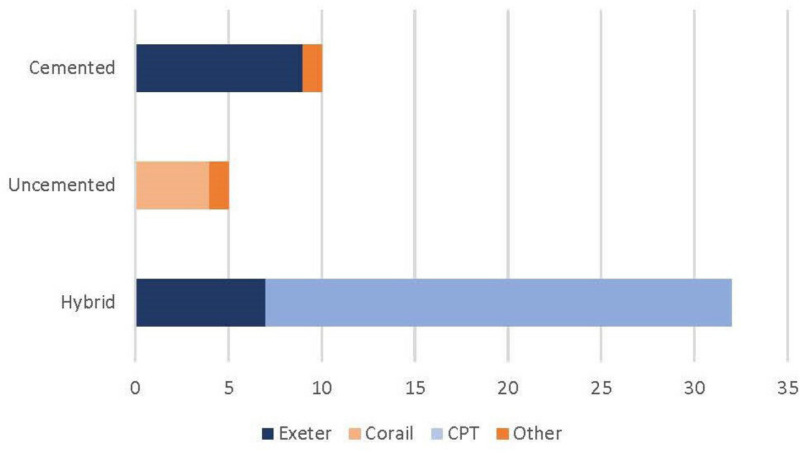
Total hip arthroplasty prostheses used in this cohort.
Outcomes
All the sites in this study had different ways of recording outcomes so these were gathered manually and collated. Primary outcome measures (30-day mortality, admission to ICU, and positive COVID-19 test) were confirmed using a combination of hospital notes, laboratory records, and discharge summaries. Length of stay was calculated using data routinely submitted to the National Hip Fracture Database and compared against discharge summaries. Complications were recorded from discharge summaries and postoperative clinic letters (where available). Radiographs were independently reviewed for all patients to check the prosthesis.
Results
Primary outcome measures
There were no inpatient deaths in this cohort of patients. Two patients (2/48, 4%) required admission to ICU postoperatively (Figure 3), but not for complications related to COVID-19.
Fig. 3.
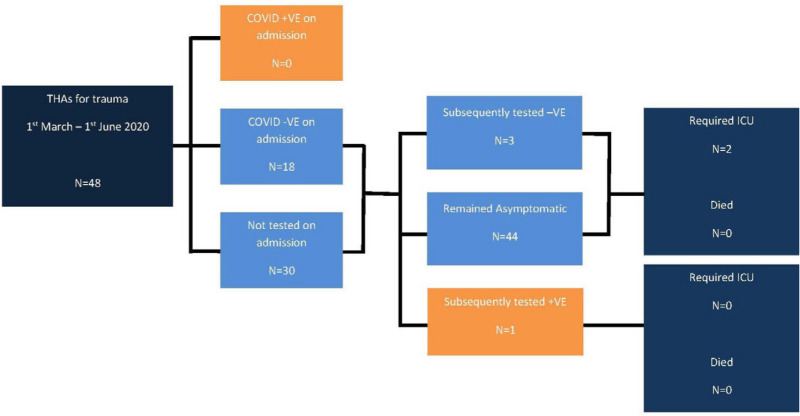
COVID-19 status, intensive care unit requirements, and death.
Overall, 18 patients (18/48, 38%) were tested on admission for COVID-19: all were negative. The time taken for test results to be available varied considerably between trusts (median 1.5 days, IQR 2.5). Four patients (4/48, 8%) developed either a new persistent cough or pyrexia postoperatively and were tested for COVID-19: three (3/4, 75%) had previously been tested and one patient was not. Only one patient (1/48, 2%) tested positive for COVID-19, which was on day 20 of their stay; they had not been tested upon admission to hospital. They did not require ICU support but did remain an inpatient for a further 29 days.
Secondary outcome measures
The median time from surgery to discharge was five days (2 to 47). The median length of hospital stay for all patients was seven days (IQR 4) (Table I).
Table I.
Time from admission to surgery, surgery to discharge, admission to test result, and total length of stay.
| Variable | Median (days) | Range (days) |
|---|---|---|
| Admission to operation | 2 | 0 to 9 |
| Operation to discharge | 5 | 2 to 47 |
| Length of stay | 7 | 3 to 49 |
| Admission COVID-19 test result | 1.5 | 0 to 7 |
In the short study period, there were no periprosthetic fractures or prosthesis-related infections. One patient suffered a dislocation of their THA following discharge from hospital; this was successfully manipulated under general anaesthesia and did not require additional procedures during this period. Postoperative medical complications (non-COVID-19-related) were recorded in ten (28%) patients (see Table II).
Table II.
Postoperative complications following total hip arthroplasty for intracapsular femoral neck fractures.
| Variable | Number (%) |
|---|---|
| Inpatient mortality | 0 (0) |
| ICU admission | 2 (4.2) |
| COVID-19 infection | 1 (2.1) |
| Periprosthetic fracture | 0 (0) |
| Prosthetic joint infection | 0 (0) |
| Dislocation | 1 (2.1) |
| Blood transfusion | 4 (8.3) |
| Other complications | |
| AKI | 2 (4.2) |
| Electrolyte imbalances | 2 (4.2) |
| HAP | 1 (2.1) |
| Delirium | 1 (2.1) |
ICU, intensive care unit; AKI, acute kidney injury; HAP, hospital-acquired pneumonia.
Discussion
Principal findings
This study presents early data concerning outcomes of 48 patients undergoing THA for femoral neck fracture in four UK hospitals during the height of the current COVID-19 pandemic in the UK.
During our study period no patients have yet died of any cause. Two patients did require between 24 to 48 hours in the ICU but not for COVID-19-related medical problems. Only one patient (2%) was proven to contract COVID-19 during their admission; they spent seven weeks in hospital but did not require ICU treatment. Other complications included one dislocation (2%), one hospital acquired pneumonia (2%), anaemia requiring ≥ 1 unit blood transfusion (4/48; 8%), and acute kidney injury or electrolyte imbalance (4/48; 8% combined). The median length of stay was seven days.
Interpretation
Demographically speaking, our patients were older than the average patient receiving an elective THA (73 vs 70 years).8 THAs performed for trauma are associated with higher complication rates generally (9% vs 4%) and specifically higher 30-day mortality (0.15% to 0.3% vs 1.4%).9–12 While we might not have anticipated any deaths given the small number of patients, the proportion of patients requiring ICU was about half that cited in one study (4% vs 7%).13 Our median length of stay was just seven days compared 15 days reported elsewhere.14 Given this, outcomes are similar to what might have been expected for a representative period prior to the COVID-19 crisis.15
In keeping with policy across all four hospitals, patients who were symptomatic on admission or at any point during their hospital stay were swabbed for the SARS-CoV-2 virus wherever possible. In the early stages of the pandemic (March to mid-April), very few patients in our study were tested, reflecting the low number of tests available nationally. A higher number of tests were carried out from mid-April to May, bringing the total number to 18 (38%) with four patients (8%) tested subsequently. This does not allow for patients who may have been asymptomatic, those who obtained a false negative test result, or who took independent tests elsewhere and so may be an underestimation of the true figure.
Implications for clinicians and policymakers
This study shows that it is possible to maintain a safe THA service for trauma even during this (or subsequent) peak(s) of the COVID-19 crisis. In April, the British Orthopaedic Association (BOA) cautioned surgeons to consider hip hemiarthoplasty in patients who might otherwise have met National Institute for Health and Care Excellence (NICE) standards for THA to facilitate early surgery and prompt discharge.15 The relative merits of hemiarthroplasty versus THA for trauma was a point of discussion prior to the COVID-19 pandemic and remains so.16 While this study does not directly address that issue, the results do not support a widespread policy of avoiding THAs in eligible patients where resources are available.
Novel measures to facilitate timely discharge following surgery meant that our combined length of stay was markedly lower than national figures prior to the COVID-19 crisis.12 This demonstrates that is it possible to discharge these patients promptly and safely and we believe that patients’ time in hospital should be kept to a minimum as we emerge from this crisis. Clinicians may choose to consider a patient’s postoperative home support structure when selecting candidates for elective surgery.
Although it might be desirable to confine planned surgery to “clean sites”, the low infection rate observed in this study shows that it is possible to deliver arthroplasty surgery in hospitals which also treat patients with COVID-19 providing appropriate precautions are followed. These include rigorous hand hygiene, use of personal protective equipment (PPE), minimizing staff in theatres, enhanced cleaning protocols, ‘red and green’ zones within the hospital, and availability of side rooms. Demanding that patients self-isolate preoperatively and routine swab testing of staff and patients might further reduce the risk.
No elective joint arthroplasty surgery has taken place in the UK during the COVID-19 pandemic and so the risks are as yet unknown. Although our results are encouraging, we would advise caution when generalizing outcomes of elective hip arthroplasties from those performed for trauma. Surgical management for fractured femoral necks is invariably indicated even in the sickest patients. On the other hand, a hip arthroplasty – even for severe osteoarthritis – remains a quality of life decision and there are other measures such as weight loss, physiotherapy, walking aids, analgesia, and therapeutic joint injections, which may alleviate symptoms with considerably lower risk to the patient. Surgeons should think very carefully about how this information is explained to the patient when it comes to the surgical consent process.17
Unanswered questions and future research
The risk to patients is only one factor in a complex decision-making process regarding resumption of services following the pandemic. Specifically, we do not comment upon risk to staff, logistical or financial considerations, which are all worthy subjects of further research.
Rightly, it is anticipated that there will be a great deal of interest in outcomes of the first cohort of patients to receive planed prosthetic joints in the post-COVID-19 era.
Strengths and weaknesses
There are inherent weaknesses in reporting such a small cohort of patients and larger collaborations are required nationally and internationally to answer some of the questions raised here.
The follow-up was necessarily short, which will lead to an underestimation of complications such as dislocation (median time to readmission 40 days) or infection, where only 14% occur within the first three months.7,18 Other patient characteristics such as American Society of Anaesthesiologists (ASA) score and body mass index – which are also predictors of outcomes – were not recorded.13
Despite these weaknesses, we believe this to be the largest published cohort of joint arthroplasties performed during the peak of the COVID-19 pandemic. Having identified this cohort, we are in a position to follow them up over the lifespan of the patient and the prosthesis and observe any change reflected in the revision rate (currently 4.1% of THAs for trauma).12
Conclusion
This is an evolving situation limited by the paucity of evidence available and our understanding of the COVID-19 disease. It appears possible to perform THAs for trauma with only modest risk of contracting COVID-19 or experiencing serious sequalae of the disease. The results of this study do not support the guidance issued by the BOA to use hemiarthroplasties when a surgeon feels a patient would be better served by a THA.
Caution should be applied in generalizing the results of this study to elective arthroplasty. The possibility of contracting COVID-19 in hospital cannot be completely eliminated but we believe with careful patient selection, appropriate counselling, and strict protocols in place, elective services should be able to restart in the near future.
Take home message
- It is possible to deliver safe care to patients requiring a THA for trauma.
- The risk of contracting COVID-19 in hospital cannot be eliminated and is associated with extended length of stay.
Footnotes
Author contributions: A. C. S. Stoneham: Designed and ran the study, Wrote the manuscript, Liaised with the authors, Managed the submission process.
M. Apostolides: Co-designed the study, Performed the statistical analysis, Wrote the results section.
P. M. Bennett: Collected the data, Managed the references, Co-wrote first draft of the manuscript.
R. Hillier-Smith: Collected the data, Co-wrote second draft of the manuscript.
A. J. Witek: Collected the data, Co-wrote subsequent drafts of the manuscript.
H. Goodier: Collected the data, Co-wrote subsequent drafts of the manuscript.
R. Asp: Collected the data, co-wrote subsequent drafts of the manuscript.
Adam C. S. Stoneham is both lead and senior author
Funding statement: No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
ICMJE COI statement: The authors have no financial or competing interests to disclose.
Ethical review statement: This is a retrospective cohort study analyzing data routinely collected for the purposes of audit and research. Upon advice, we did not attempt to seek ethical approval.
References
- 1. Lacobuci G. Covid-19: all non-urgent elective surgery is suspended for at least three months in England. BMJ 2020; 368:m1106 2020. [DOI] [PubMed] [Google Scholar]
- 2. Collaborative C. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Santorelli G, Sheldon T, West J, Cartwright C, Wright J. COVID-19 in-patient hospital mortality by ethnicity. Wellcome Open Research. 2020;5(86):86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. No authors listed Recovery of surgical services during and after COVID-19. 2020. https://www.rcseng.ac.uk/coronavirus/recovery-of-surgical-services/ (date last accessed 15 July 2020).
- 5. No authors listed Hip fracture: management. Clinical guideline [CG124]; 2011. 2011. https://www.nice.org.uk/guidance/cg124 (date last accessed 15 July 2020).
- 6. No authors listed Coronavirus (COVID-19) in the UK. 2020. https://coronavirus.data.gov.uk/ (date last accessed 15 July 2020).
- 7. Gausden EB, Parhar HS, Popper JE, Sculco PK, Rush BNM. Risk factors for early dislocation following primary elective total hip arthroplasty. J Arthroplasty. 2018;33(5):1567–1571. [DOI] [PubMed] [Google Scholar]
- 8. Chidambaram R, Cobb A. Change in the age distribution of patients undergoing primary hip and knee replacements over 13 years-an increase in the number of younger men having hip surgery. Orthopaedic Proceedings, 2009:152. [Google Scholar]
- 9. Lim JW, Ng GS, Jenkins RC, et al. Total hip replacement for neck of femur fracture: comparing outcomes with matched elective cohort. Injury. 2016;47(10):2144–2148. [DOI] [PubMed] [Google Scholar]
- 10. Partridge T, Jameson S, Baker P, et al. Ten-Year trends in medical complications following 540,623 primary total hip replacements from a national database. J Bone Joint Surg Am. 2018;100(5):360–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Parvizi J, Johnson BG, Rowland C, Ereth MH, Lewallen DG. Thirty-day mortality after elective total hip arthroplasty. J Bone Joint Surg Am. 2001;83(10):1524–1528. [DOI] [PubMed] [Google Scholar]
- 12. Stafford GH, Charman SC, Borroff MJ, Newell C, Tucker JK. Total hip replacement for the treatment of acute femoral neck fractures: results from the National joint registry of England and Wales at 3-5 years after surgery. The Annals of The Royal College of Surgeons of England. 2012;94(3):193–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kamath AF, Gutsche JT, Kornfield ZN, et al. Prospective study of unplanned admission to the intensive care unit after total hip arthroplasty. J Arthroplasty. 2013;28(8):1345–1348. [DOI] [PubMed] [Google Scholar]
- 14. Richards T, Glendenning A, Benson D, Alexander S, Thati S. The independent patient factors that affect length of stay following hip fractures. The Annals of The Royal College of Surgeons of England. 2018;100(7):556–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. British Orthopaedic Association Management of patients with urgent orthopaedic conditions and trauma during the coronavirus pandemic. 2020. http://www.bapras.org.uk/docs/default-source/covid-19-docs/final-boast-doc-badged.pdf?sfvrsn=2 (date last accessed 15 July 2020).
- 16. Viswanath A, Malik A, Chan W, Klasan A, Walton NP. Treatment of displaced intracapsular fractures of the femoral neck with total hip arthroplasty or hemiarthroplasty: a single-centre review of 2,721 patients. Bone Joint J. 2020;102(6):693–698. [DOI] [PubMed] [Google Scholar]
- 17. Leigh B. Consent in the Post-COVID-19 era. https://www.boa.ac.uk/policy-engagement/journal-of-trauma-orthopaedics/journal-of-trauma-orthopaedics-and-coronavirus/consent-in-the-post-covid-19-era.html (date last accessed accessed 3 June 2020).
- 18. Lenguerrand E, Whitehouse MR, Beswick AD, et al. Risk factors associated with revision for prosthetic joint infection after hip replacement: a prospective observational cohort study. Lancet Infect Dis. 2018;18(9):1004–1014. [DOI] [PMC free article] [PubMed] [Google Scholar]


