Abstract
Background:
Coronavirus disease 2019 (COVID-19) has emerged as a global health threat. The South-Asian (SA) countries have witnessed both the initial brunt of the outbreak as well as the ongoing rise of cases. Their unique challenges in relation to mental health during the pandemic are worth exploring.
Materials and Methods:
A systematic review was conducted for all the original studies on the impact of COVID-19 and lockdown on psychological health/well-being in the SA countries of the World Psychiatric Association Zone 16. PubMed, Google Scholar, PSYCHINFO, EMBASE, and SCOPUS were searched till June 2020. Studies conducted in the age group of 18–60 years with a minimum sample size of 10, and statistically significant results were included.
Results:
Thirteen studies were included in the review. They showed increase prevalence in nonpsychotic depression, preanxiety, somatic concerns, alcohol-related disorders, and insomnia in the general population. Psychological symptoms correlated more with physical complaints of fatigue and pain in older adults and were directly related to social media use, misinformation, xenophobia, and social distancing. Frontline workers reported guilt, stigma, anxiety, and poor sleep quality, which were related to the lack of availability of adequate personal protective equipment, increased workload, and discrimination. One study validated the Coronavirus anxiety scale in the Indian population while another explored gaming as a double-edged sword during the lockdown in adolescents. Another study from Bangladesh explored psychosexual health during lockdown. Most studies were cross-sectional online surveys, used screening tools and had limited accessibility.
Conclusion:
The ongoing COVID-19 crisis and its impact serve as an important period for adequate mental healthcare, promotion, research, and holistic biopsychosocial management of psychiatric disorders, especially in vulnerable groups. Mental healthcare and research strategies during the pandemic and preparedness for postpandemic aftermath are advocated subsequently.
Keywords: Advocacy, coronavirus disease 2019, pandemic, psychosocial, review, South Asia, Zone 16 World Psychiatric Association
INTRODUCTION
The Coronavirus disease 2019 (COVID-19) has wreaked global havoc in the last 6 months. What started as a Public Health Emergency of International Concern, quickly escalated into a pandemic that took the world by its knees.[1] Outbreaks like this are far from just being a public health concern. They can have immense psychosocial offshoots that might far outlast the infection itself. Although less fatal than its earlier counterparts Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome, the human-to-human transmission has been exceptionally high for COVID-19, leading to its rapid spread across the world.[2] Vulnerable groups include the older adults, the socially impoverished (migrants, homeless, etc.), immunocompromised, those with preexisting cardio-pulmonary comorbidities and the gender minorities. They are susceptible to both the physiological as well as psychological effects of the outbreak. Even though each nation faces unique challenges against COVID-19, the common threads of psychosocial comorbidity connect them all. It has been well established by now that this outbreak has not only been causing high mortality but also large-scale psychological effects such as panic, health anxiety, loneliness, isolation, and fear of uncertainty. People with preexisting psychiatric conditions such as depression, schizophrenia, obsessive-compulsive disorders, and dementia have shown exacerbations due to multitude of factors that range from stress-diathesis, lack of access to mental healthcare resulting from lockdown and finally reduced compliance and poor supervision.[3,4] Unfortunately, in a frantic search for biological cure and vaccines against the virus, these issues are widely neglected, contributing to increased public health burden.
The importance of mental health during the COVID-19 pandemic has been stressed upon by various public health agencies like the World Health Organization (WHO) and the Centre for Disease Control and Prevention. According to Adhanom Ghebreyesus,[5] Director general, WHO, integrating mental health needs into public health response will form a vital tool against the ongoing pandemic. The emotional and psychological effects of the outbreak can range from biological factors like the neurotropic effects of SARS-CoV-2 (causative agent of COVID-19) and involvement of the limbic system, psychological factors of fear, discomfort, uncertainty, and addictions as well as socioeconomic issues of isolation, stigma, domestic violence, and loss of livelihoods. Especially the frontline workers, those affected and their families, those in isolation and the socioeconomically deprived population are thought to be at the highest risk for psychiatric comorbidities.[5] Adverse and distressing circumstances created by biological disasters have historically shown to increase disorders such as depression, posttraumatic stress disorder, generalized anxiety disorder (GAD), and substance use disorders. The impaired process of grieving associated with death, social stigma, prejudice, and discrimination with mass panic can complicate the management of infectious disease outbreaks that happened in the past with the SARS outbreak. Past studies indicated that besides the acute effect, the chronic sequelae of mental and behavioral disorders can also be prevalent that complicate the morbidities and quality of life in the postpandemic aftermath.[6,7]
Global studies have established by now that COVID-19 has been increasingly associated with neuropsychiatric manifestations such as delirium, anxiety, depressive disorders, insomnia, and increased self-harm. Besides, the incidence of cerebrovascular accidents and seizures have been reported due to the COVID-19 that can have added psychiatric associations.[8] Plethora of misinformation have added to societal stigma against the patients, their families and frontline health workers. The elderly, those staying alone or in isolation and the migrant workers have often been deprived of their basic living amenities making them doubly vulnerable to the health risks of the pandemics and its social effects. On the other side, those with pre-existing psychiatric conditions might be at increased risk for the infection due to lack of supervision and inadequate compliance to precautionary measures.[9] Most studies done till date are online surveys that have used non-specific tools to measure the overall psychological wellbeing, as the world awaits more systematic population-based work to understand the mental health risks that might help design interventions. Various assessment scales have also been used to gauge the psychological parameters specific to the COVID-19 pandemic such as the Coronavirus Anxiety Scale (CAS), Obsession with COVID19 Scale, Fear of COVID-19 Scale (FCV-19S) in Italian, Bangla, Russian and English versions, and the COVID Stress Scale which consists of five Likert subscales.[10-12] Data on the psychometric properties and widespread use of these scales are still limited though they offer promise in understanding the emotional consequences unique to the COVID-19 pandemic. In this context, mental health professionals can play an unique role in the wellbeing of the general public and bridging the gap in mental health care that becomes all the more apparent at times of crisis in public health infrastructures. Although a global crisis, COVID-19 has differentially affected certain sectors of the world. The South Asian Association for Regional Cooperation (SAARC) countries comprise 23.7% of the world population, and a major proportion of this section is of younger age, who are essentially the working class and hence the economically productive population. In contrast to the other countries in Asia and the west, the South Asian countries (including the SAARC) have a higher rate of COVID-19 infection in the young population, which obviously affects the financial parameters.[13] Zone 16 of the World Psychiatric Association (WPA) consists of these countries, namely India, Bangladesh, Pakistan, Sri Lanka, Nepal, Bhutan, Thailand, Indonesia, Malaysia, Philippines, and Singapore.[14] Interestingly, this group consists of nations such as Singapore, Indonesia, and Malaysia, which took the initial hit of the pandemic and are relatively stable at present, as well as the SAARC countries, which have rising cases presently with increased morbidities and fatalities. India, comprising one of the most major and diverse populations in the Zone 16 countries, has a case fatality rate lower than other areas of the world, but the growing number of cases and limited testing can easily overburden the public health infrastructure leading to trying conditions with respect to the psychosocial burden. Jean Gough, the United Nations Children's Fund (UNICEF) Regional Director for South Asia, recently mentioned that the COVID-19 pandemic, containment and prevention measures are complicated by the natural catastrophises of widespread floods, rains, landslides and locust swarms in South Asian countries that can cause significant social and environmental changes.[15] Added to that, is the mental health gap (mhGAP) that reaches up to 90 percent in low and middle income countries (LMIC), many of which are in South Asia.[16] The resources are predominantly dependent on grass root health workers and general physicians which bring in the question of adequate mental health risk communication and community awareness, concepts which become important during public health crises like COVID-19. Keeping this in the background, the authors attempted to review the psychological impact of the COVID-19 crisis and lockdown in the Zone 16 countries and consequently discuss the findings in light of a global picture and advocacy perspectives for mental well-being.
MATERIALS AND METHODS
Search strategy
The search protocol followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines as per Moher et al.[17] The present study was performed by a comprehensive literature search of five electronic databases, namely PubMed, Google Scholar, PsychINFO, EMBASE, SCOPUS, and the last search was done on June 10, 2020. The search keywords for the present study were “COVID-19” OR “Coronavirus” OR “SARS-CoV-2” OR “COVID-19 pandemic” AND “mental health” OR “mental wellbeing” OR “psychiatry” OR “psychosocial” OR “psychiatric” OR “psychosexual” OR “sexual” OR “sexuality” OR “depression” OR “anxiety” OR “psychosis” OR “loneliness” OR “psychological problem,” used in varying permutations and combinations, along with extensive cross-referencing. The nine countries of Zone 16 were separately added as keywords to exclude studies from other countries as an initial filter. First, all titles and abstracts were screened for relevance to the study, and the full content of the relevant studies were reviewed.
Identification and selection of studies
Search results were evaluated twice through successive screenings with increasingly stringent criteria. The initial screen was conducted on article abstracts. An article was included if the abstract indicated as a peer-reviewed original research article, written in English, and used online survey and/or cross-sectional and/or longitudinal research study on the impact of COVID-19/SARS-CoV-2 pandemic on mental health or psychological or psychosexual well-being in the population of Zone 16 (South Asian [SA]) countries. Reviews, letters to editors, case reports, and commentaries were excluded. Intervention studies were also excluded. The initial screening of this study applied the following inclusion criteria: (1) sample sizes ≥10 participants, (2) studied prevalence/surveys of psychological or psychosocial problems in the WPA Zone 16 countries, (3) investigated prevalence/incidence of psychiatric disorders in general population/frontline workers/COVID-19 affected patients as a consequence of COVID-19 pandemic; (4) used study population of adults age-ranged between ≥18 years, and (5) reported significant statistical differences in the studied parameters. The exclusion criteria were selected as: (1) <10 patients; (2) intervention studies, (3) study with only children and adolescence, and (4) studies from other countries. General perspectives and viewpoint articles, even if related to data within the country, were also excluded.
Data extraction
DB and TSSR performed the initial searches and screened for duplicates. Other reviewers independently screened all unique search results for potential above-mentioned inclusions studied in the Systematic Review with extensive cross-referencing. The articles passing both reviewers' approval and cross-checked by other authors were finally considered for inclusion. Finally, data extraction was done by using a standardized data extraction sheet for extracted data from each study. The authors did not include stringent quality check measures as research in this area is still emerging and too strict inclusion was avoided. The data extraction form included: (1) author name, (2) year of publication, (3) study area, (4) age-groups of the participants, (5) the assessment tools and outcome measures (6) number of participants, and (7) grand mean cross-correlation matrices.
RESULTS
Selection of studies and characteristics of included studies
Figure 1 (PRISMA flowchart) depicts the process of study inclusion and selection for review. In total, 176 citations were obtained after the initial screening, which were on “COVID-19 and mental health.” After further screening for original articles based on the outcome of interest, 23 articles were read in full-text, and 10 were excluded based on the exclusion criteria mentioned earlier. Hence, eventually, 13 articles were included in the systematic review.
Figure 1.
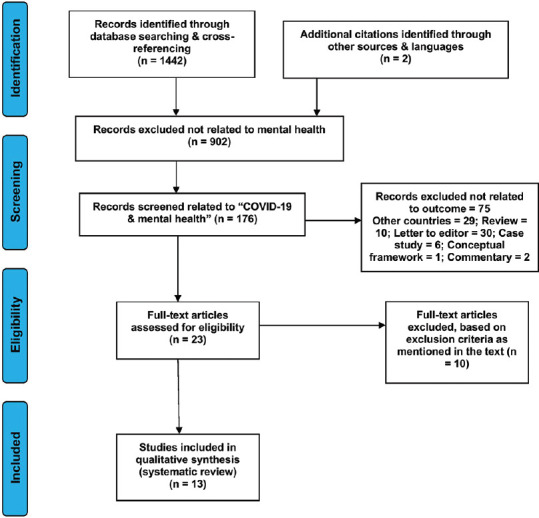
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flowchart for the systematic review
As the studies had used different tools and outcome measures related to the COVID-19, they will be briefly described based on their country of origin before moving into the discussion.
India
In the Indian context, Table 1 describes 10 studies on the psychosocial impact of COVID-19. These are briefly discussed as follows:
Table 1.
Indian studies showing impact of coronavirus disease 2019 on mental health
| Authors (year) | Place of the study | n (number of subjects) | Methods | Outcome and tools |
|---|---|---|---|---|
| Varshney et al., 2020 (FEEL-COVID survey) | Department of Psychiatry, ILBS, New Delhi, India | 653 | Cross sectional survey and IES-R method | Psychological impact/life eventsbased on IES-R score |
| Khanna et al., 2020 | LV Prasad Eye Institute, LV Prasad Marg, Hyderabad, Telangana, India | 2,355 | Online survey | Depression at mild, moderate and severe levels of severity |
| Chandu et al., 2020 | Sibar Institute of Dental Sciences, Guntur, Andhra Pradesh, India | 307 | Questionnaire-based survey as per Likert scale | COVID-19 Anxiety Scale and its psychometric properties |
| Narasimha et al., 2020 | NIMHANS, Hosur Road, Bengaluru, India | 96 | Hospital-based observational study | Alcohol withdrawal syndrome with seizures, delirium tremens and hallucinations |
| Roy et al., 2020 | King George’s Medical University, Lucknow, Uttar Pradesh, India | 662 | Cross-sectional, and observational study | Knowledge, attitude, practices and perceived anxiety related to COVID-19 |
| Balhara et al., 2020 | National Drug Dependence Treatment Center, All India Institute of Medical Sciences, New Delhi, India | 393 | Cross-sectional study | PHQ-9, GAD-7, DSM-IV (to assess depression) and IGDSF-9 for gaming behavior during lockdown |
| Balhara et al., 2020 | National Drug Dependence Treatment Center, All India Institute of Medical Sciences, New Delhi, India | 73 | Hospital-based observational study | Psychological distress, alcohol consumption and alcohol withdrawal symptoms |
| Grover et al., 2020 | Department of Psychiatry, Postgraduate Institute of Medical Education and Research, Chandigarh, India | 1685 | Multicenter online survey | PHQ-9, GAD-7, WEMWS for anxiety, depression, stress, sleep and other associated psychological parameters |
| Chakraborty and Chatterjee, 2020 | Departments of Psychiatry and Anatomy, College of Medicine and JNM Hospital, Nadia, West Bengal, India | 507 | Online survey | Self-designed questionnaire for assessing worry about infection, distress, anxiety and sleep disorders |
| Chatterjee et al., 2020 | Department of Psychiatry, Diamond Harbour Medical College, Diamond Harbour, West Bengal, India | 152 | Cross-sectional online survey | Knowledge, attitude, behaviour of doctors; DASS-21 for psychiatric morbidities |
IES-R – Impact of Events Scale-Revised; PHQ – Patient Health Questionnaire; GAD – Generalized Anxiety Disorder; IGDSF – Internet Gaming Disorder Short Form; WEMWS – WarwickEdinburgh Mental Well-being Scale; DASS-21 – Depression Anxiety Stress Scale-21; ILBS – Institute of Liver and Biliary Science; NIMHANS – National Institute of Mental Health and Neurosciences; COVID-19 – Coronavirus disease 2019; DSM-IV – Diagnostic and Statistical Manual-IV
Varshney et al.[18] studied the psychological impact of COVID-19 and recruited 1106 subjects in a cross-sectional study from 64 cities in India. The mean age of the participants was 41.82 ± 13.85 years and 22% of participants were health-care professionals. One-third of participants had a significant psychological impact based on the Impact of Event-revised (IES-R) score. Higher psychological impact was found in the younger group, females and those with comorbid physical illness, especially liver disease. Regarding psychological impact, most of the participants had minimal (66.8%) or mild (15%) severity (IES-R score 24–32) of impact. Few participants reported moderate (5.5%) (IES-R score 33–36) to severe (12.7%) symptoms (IES-R score >36). The need for tailored mental health interventions were stressed on by the authors.
Khanna et al.[19] conducted an online survey on the psychological impact of COVID-19 between two groups of respondents, namely Practicing Ophthalmologists and trainees Ophthalmologists. The survey included 2,355 participants with mean age of 42.5 ± 12.05 years. Of these, 56.7% were male, 20.2% were still not in practice, 15.5% were single. Nearly half (52.8%) of the participants felt that training or professional work was impaired due to COVID-19, while 37% encountered difficulties to meet living expenses. The mean Patient Health Questionnaire-9 (PHQ-9) score was 3.98 ± 4.65. One-third (32.6%) of the participants had depressive symptoms, mostly of mild (21.4%) severity, followed by moderate (6.9%) and severe (4.3%) symptoms. Subsequent analysis revealed that the significant predictors of depression were age (younger age), gender, marital status, practicing status, type of service, concerns about the profession, and inability to incur expenses.
Chandu et al.[20] attempted to validate COVID-19-related anxiety scale (CAS) and they studied 307 subjects. According to their study, CAS determined a two-component structure such as: “fear of social interaction” and “illness anxiety.” The final scale with seven items showed good internal consistency and reliability (Cronbach's alpha = 0.736) along with moderately negative correlation (Pearson's r = −0.417) with self-rated mental health. Interestingly, the results found significantly higher anxiety scores in the lower educational qualification group. The authors stressed that CAS is a rapid, valid, and reliable test, which might be a useful tool to assess the psychological impact of the pandemic in the Indian population.
Narasimha et al.[21] investigated hospital-based 96 middle-aged participants with an average 46.0 ± 9.0 years and male patients were found suffering from severe alcohol withdrawal syndrome during the lockdown period. Delirium tremens, with or without seizures, was the most common presentation (80%), followed by withdrawal seizures (17%) and withdrawal hallucinosis (12%). Three-fourth (76%) belonged to below the poverty level. All subjects reported heavy alcohol use as per standard use on a daily basis. Majority (95%) subjects reported COVID-19-related lockdown cause for the sudden cessation of alcohol use. This was one of the first Indian studies to explore substance abuse complications as a result of the sudden national lockdown.
Roy et al.[22] assessed the knowledge, attitude, anxiety experience, and perceived mental healthcare need among 662 adult subjects in India during COVID-19. The online survey was questionnaire-based and used non-probability snowball sampling technique. A moderate level of knowledge about the COVID-19 infection and the least knowledge about prevention were reported. The subjects showed higher levels of anxiety and 80% were preoccupied with the thoughts of COVID-19. The overuse of gloves and sanitizers was reported in 72%. The study indicated sleep difficulties (12.5%), paranoia about acquiring COVID-19 infection (37.8%) and distress related to social media (36.4%) as the common distressing factors. Perceived mental healthcare need was reported by >80% of the sample, which again advocated the need for enhanced psychosocial care during the pandemic.
Balhara et al.[23] conducted a cross-sectional study to know about the gaming behavior of 393 college students during the lockdown period. This study was carried out through social media contact, namely E-mail and WhatsApp messenger using PHQ-9, GAD-7, Diagnostic and Statistical Manual-IV (to assess depression), and Internet Gaming Disorder Short form-9. About half (50.8%) of the participants reported an increase in gaming behavior during the lockdown period. Further analysis indicated that hours of gaming per day increased due to the stress of examination and the participants' belief that gaming helps in stress management. Social isolation and lack of family activities were added factors. The authors suggested “gaming” as a two-edged sword during the lockdown period.
In another study, Balhara et al.[24] studied 73 males with alcohol use disorder of 8.66 ± 6.2 years. Although sale was restricted during the lockdown, 20% of subjects continued procuring alcohol. Two-third (62.5%) of the participants obtained alcohol at higher prices from illicit sources. In addition, about one-fifth of these patients, were at risk of consuming adulterated alcohol. A small proportion (6.6%) participants reported experience of alcohol withdrawal during the starting of lockdown. Only one subject experienced withdrawal seizures. Majority of the subjects could not access health-care facilities to manage their withdrawals. The exacerbated psychosocial effects of alcohol use due to the pandemic situation were once again highlighted in this study.
Grover et al.[25] evaluated the psychological impact of lockdown due to COVID-19 pandemic in 1685 people to assess the prevalence of depression, anxiety, perceived stress, well-being, and sleep. It was a online survey conducted with the Survey Monkey platform, the survey link being circulated using WhatsApp. In this study, PHQ-9, GAD-7, WarwickEdinburgh Mental Well-being Scale were used to assess the various parameters. About two-fifth (38.2%) of the participants had anxiety and 10.5% of the participants had depressive disorder. Among the participants, about 40.5% had either anxiety or depression. Moderate stress and poor well-being were found in 74.1% and 71.7% respectively. Overall two-fifths were experiencing common mental disorders during the COVID-19 situation. This was the first study by the Indian Psychiatric Society (IPS) to assess the psychological impact of the outbreak.
Chakraborty and Chatterjee[26] in a regional survey evaluated 507 subjects with a mean age of 33.9 ± 8.27 years in West Bengal, India. The 38-item self-designed questionnaire was circulated through WhatsApp. 71.8% and 24.7% showed increased worries and depressive symptoms during the pandemic. About half (52.1%) of the participants were preoccupied with the idea of contracting COVID-19 and 21.1% wanted testing irrespective of symptoms. About 69.6% were worried of financial loss during the period of lockdown. Slightly less than one-third (30.8%) of the participants perceived health anxiety to be significantly increased and feared that it might not normalize even post lockdown. This study especially showed the importance of uncertainty and panic as factors influencing psychological health.
Chatterjee et al.[27] cross-sectionally assessed the knowledge, attitude, and behavior (KAB) of 152 doctors regarding the pandemic and the influence of depression, anxiety, and stress. KAB of the participants was obtained through semi-structured proforma, and psychiatric morbidity was measured by the Depression, Anxiety, and Stress Scale-21 (DASS-21). Among the participants, 34.9%, 39.5%, and 32.9% were depressed, anxious, and stressed, respectively. Significant predictors of psychological burden were job in the health sector, duty hours, lack of protective measures, and altruistic coping. Stigma and discrimination against the frontline workers were identified as important factors contributing to their stress.
Pakistan
Balkhi et al.[28] [Table 2] studied behavioral changes during COVID-19 pandemic situation among 400 participants in Karachi. It was an online survey through a structured self-administered questionnaire. Majority of participants were aged <35 years, with equal male: female ratio. Everyday fear related to COVID-19 was seen in 62.5%. Participants manifested fear when they visited outdoor (88.8%), were concerned about family's health (94.5%), and felt lack of confidence related to the precautionary measures (71%). Home was not considered to be safe by most. Majority (82.8%) subjects reported panic due to fake news in social media. A small proportion (14.8%) of subjects had pretended to be sick for avoiding the workplace/educational institute. In addition, 86.5% of participants had restricted their physical contact with people, 74.5% avoided health-care facilities, 84.5% postponed social engagement and 87% showed obsessive washing of hands.
Table 2.
Study in Pakistan showing impact of coronavirus disease 2019 on mental health
| Authors (year) | Place of the study | n (number of subjects) | Methods | Outcome and tools |
|---|---|---|---|---|
| Balkhi et al., 2020 | Jinnah Sindh Medical University, Karachi, Pakistan | 400 | Descriptive and cross-sectional online survey | Behavioural reactions to pandemic: fear, distress, anxiety, attitudes to social media; self-designed questionnaire |
Multicenter studies [Table 3]
Table 3.
Multicenter studies on impact of coronavirus disease 2019 on mental health
| Authors (year) | Place of the study | n (number of subjects) | Methods | Outcome and tools |
|---|---|---|---|---|
| Arafat et al., 2020 | Department of Psychiatry, Enam Medical College and Hospital, Dhaka, Bangladesh | 120 | Multicenter cross-sectional and cross-national online survey | Sexual behavior for pre, during and post-COVID-19 lockdown; Self-designed questionnaire (Google form) |
| Chew et al., 2020 | Division of Neurology, Department of Medicine, National University Health System, Singapore and The Department of Neurology, Yashoda Hospital, Secunderabad, India and other departments | 480 (India)+426 (Singapore)=906 | Multicentre cross-sectional online survey | DASS-21 and the IES-R for psychological problems viz. depression, anxiety, stress, and posttraumatic stress disorder |
DASS-21 – Depression Anxiety Stress Scales-21; IES-R – Impact of Events Scale-Revised; COVID-19 – Coronavirus disease 2019
The Multicenter studies included in the review are summarized in Table 3. Arafat et al.[29] performed a multicenter online survey to study the effects of lockdown on the sexual life of the participants from three South-East Asian countries (India, Nepal, and Bangladesh). This research was conducted through Google form in the English language among 120 participants. The average age of the participants was 35.42 ± 5.73 years and majority were in the 30–39 years age group. Three-fourth (77.5%) of the participants were male and most subjects had a postgraduate degree. Majority of participants engaged in sexual activity with their partner once to five times a week before (76%) and during lockdown (72%), while 10% showed an increase in sexual interactions during the lockdown period.
Chew et al.[30] investigated the relationship between psychological outcomes and physical symptoms among 906 health-care workers in five major COVID-19 hospitals of India and Singapore. DASS-21 and IES-R were used besides evaluation of demographics factors and medical history. The age range was 25–35 years and about 50.2% were single. The subjects reported common physical symptoms such as headache (31.9%), throat pain (33.6%), anxiety (26.7%), lethargy (26.6%), and insomnia (21.0%). A small proportion (5.3%) had moderate-to-severe depression, 8.7% had moderate-to-extremely severe anxiety, 2.2% had moderate-to-extremely severe stress, while 3.8% had moderate-to-severe levels of psychological distress. Older subjects had more correlation between physical symptoms in the preceding month and depressive symptoms as well as posttraumatic stress. Linear regression indicated that the presence of physical symptoms was related to higher mean scores in the IES-R, DASS Anxiety, Stress and Depression subscales.
DISCUSSION
The reviewed studies mainly show an increase in the prevalence of nonpsychotic depression, anxiety, fear, somatization, insomnia, and alcohol abuse disorders. All the surveys were online except two, which studied a hospital-based sample.[21,24] This is pragmatic considering the travel restriction during the lockdown. However, multiple studies have stated this as a limitation as only people who were conversant in English could attend to online questionnaires and technologically savvy were accessed.[18,19,22,23] Few studies have also used socioculturally relevant surveys, translated in local languages.[25,27,30] The results resonate with large-scale surveys done in other countries, which bore significant burden of COVID-19. Huang and Zhao collected data from 7236 participants in China and reported increased prevalence of generalized anxiety (35.1%), depressive symptoms (20.1%), and sleep anxiety in the general population.[31] The health-care workers (HCWs) had the worst sleep quality and decreased total sleep time. Health-related anxiety and guilt were marked in them. A recent study involving 1563 health professionals found that nearly half reported depression, whereas 44.7% and 36.1% reported anxiety and sleep disturbances, respectively.[32] Two studies from India and one multicenter study assessed physicians for psychological complaints (present in one-third) and reported the anxiety symptoms to be directly correlated with increased duty hours, lack of shift rotations, societal stigma, and inadequate medical protective equipment.[19,27,30] This is in contrast with the physician stress factors in China and the United Kingdom (U.K.), which were increased witness to death and dying, increased risk of exposure and self-blame, as well as the guilt of spreading the infection to the family members.[33,34,35] Liu et al.[36] explored the qualitative perspectives from doctors and nurses in Hubei, China and stated the crucial role of social support, peer counseling and self-management strategies for psychological resilience. Although similar recommendations along with community awareness have been suggested in various of the reviewed studies, the “voices” of the HCW are yet to be heard and explored in SA countries, which is particularly important considering the increasing cases and burdened public health infrastructure. Worsening in preexisting psychiatric disorders has been reported in studies across countries, especially those affected with psychotic, affective, and cognitive disorders. Suicide risk related to socioeconomic crunches have been reported from the United States (U.S.) and Italy.[37,38,39] Such studies are probably warranted in the SA countries as they pass through the early stages of pandemic, especially with a high mental illness load and increased mhGAP. Some of the reviewed studies showed the increased correlation of social media exposure with psychological issues, especially sleep deprivation, increase in alcohol withdrawal after the sudden lockdown in India, increased gaming behavior that was inversely related to physical activity in students, and finally, impaired psychosexual psychosexual health.[21,22,23,24,27,29] The last study was, however, criticized due to the ethical considerations and standardization of the online surveys by multiple other authors. The study from Pakistan pointed out the importance of social distancing as it disrupted rituals, gatherings and was associated with increased social media consumption and enhanced fear as well as anxiety about the infection. Fear related to the infection, avoidance of workplace, and nonspecific panic arising from uncertainty were found to be common in the studies across the Zone 16 countries.[19,22,25,26] Only one study validated the Coronavirus anxiety scale (CAS) in India.[20] Although studies are emerging in this regard, the widespread use of these scales for data collection without appropriate testing of their psychometric properties have raised concerns in research.[40] It is also important to understand that all these studies are cross-sectional, have used screening tools like PHQ-9, GAD-7, etc., which do not necessarily help in the categorical diagnosis of disorders and have inherent limitations of using online surveys. Many of the surveys are conducted using google forms/WhatsApp, which have been criticized for poor reporting of response rates, nonverification of response sources, appropriate approvals, and standardization.[41] Furthermore, these studies on the general population miss the acute behavioral effects of the COVID-19 that might possibly elucidate the neurobiological interactions between the virus and the brain. Altered mental status and behavioral changes have been mentioned to be acute effects of the virus, and a putative link between those affected with COVID-19 and long-term psychiatric comorbidities might merit further research.[8] Nevertheless, even with these caveats, the reviewed studies portray various aspects of the psychological impact of the outbreak on the general population in the Zone 16 countries that can address interventions and policies for mental healthcare.
Advocacy principles for mental health during coronavirus disease 2019
Psychosocial healthcare
Since the time WHO called for a global mental health action related to COVID-19, various National mental health associations like the IPS, the Pakistan Psychiatric Society, Bangladesh Association of Psychiatrists, Singapore Psychiatric Association and even the SAARC Psychiatric Federation (SRF) have sprung into action for promoting psychosocial health and care under the adverse circumstances. Keeping in mind that the LMIC of South Asia can have unique considerations like accessibility to health care, limitation of resources increased population and viral case burden, difficulties in multi-sectoral coordination, outdated legislations in relation to pandemics with poor provision for mental healthcare and finally increased stigma, the estimated psychiatric comorbidities during a biological disaster like COVID-19 tend to get amplified. The IPS, in its official statement, stressed on the paramount importance of assessing the psychological needs of the general population during the pandemic, especially those affected and the frontline workers. Along with the National Institute of Mental Health and Neurosciences (NIMHANS), the IPS brought out the “Mental Health Challenges during COVID-19 pandemic: Guidance for psychiatrists,”[42] which borrows from the comprehensive guidelines for mental healthcare in psychiatric and general hospital settings, released earlier by NIMHANS.[43] The document holistically deals with “safe practices” to minimize the psychological and physiological risks of HCWs, the allied professionals, patients, and their families. It covers telepsychiatry, psychopharmacology, and brain stimulation practices during COVID-19, also catering to special populations like children and adolescents, older adults, perinatal groups, and rehabilitation settings. Various published commentaries from Pakistan, Bangladesh, Thailand, and Singapore also stress on psychological preparedness for the pandemic and warn about the upcoming rise in psychiatric morbidities in the near future.[44,45,46,47]
The role of mental health professionals can be vital in this regard, namely in education, training, encouraging mental health-promoting behaviors, cross-specialty integration, facilitating problems solving approaches, empowering patients and allied professionals, and finally enabling self-care strategies for resilience.[48] Prepared in lines of the Zika outbreak, a community-based psychosocial toolkit was proposed by Banerjee and Nair[49] that target socio-culturally sensitive interventions at different levels to integrate various stakeholders for public awareness, participation, and mental health-care delivery. The role of media integrating it with psychological care for the public has been stressed upon by the authors. Involving the general physicians, nurses, and primary care workers, as well as qualified practitioners of alternative medicine, are essential for service delivery in the community as many SA countries have an inadequate psychiatrist-patient ratio. Based on this, the Primary Care first (PCP) and Collaborative Care model had been suggested by Türközer and Öngür,[50] which integrate physical and behavioral care during the outbreak. Certain suggested areas of tertiary-primary collaboration are listed in [Box 1]. Mental health education can help Information-Education-Communication activities for the public to fight health-related misinformation, stigma and improve the Knowledge-Attitude-Practice gap of the masses. This serves for mental health advocacy and awareness that also help in early detection of cases, psychoeducation, better compliance and suicide prevention. Harnessing technology both for care and training need standard guidelines and prescriptive patterns. It can be a boon during restrictive conditions of an infectious disease outbreak like COVID-19, but at the same time, limited accessibility and poor Internet connectivity in various areas are the real challenges. NIMHANS, in collaboration with the Tele-medicine Society of India and the IPS recently released the tele-mental health guidelines (telepsychiatry, tele-psychotherapy and tele-psychiatric social work) that are first of its kind, are relevant to the current situation and can serve as a model for other countries.[51] The implementation is, however, fraught with its usual challenges and will serve as a test for time. Above all, suitable legislations are necessary to enable these measures updating the existing Pandemic Acts to suit the present needs and those of any such futuristic crises. Keeping in mind the myriads of challenges involved related to psychosocial needs during the pandemic spanning over dealing with psychiatric disorders to the mental health care needs of the general public and finally education, training and research, Figure 2 and Table 4 summarize the various aspects of mental health services during the pandemic, involving cross-country collaboration and coordination.
Box 1.
Suggested areas of primary care collaboration in mental health during pandemics
| Using technology for supervision and training in identification and treatment of psychiatric disorders |
| Involving general physicians, nurses, lay health workers and counselors |
| Community programs for mental health awareness |
| Local management of stable patients to reduce risk of infection |
| Shared resources: Case worker based approach |
| Liaising with media for mental health promotion and stigma reduction |
| Improving knowledge and beliefs related to pandemic |
| Emergency triage planning at district levels: adequate referrals |
| Consultation-based care at tertiary centers |
| Adequate screening for depression, anxiety and substance use disorders in the community |
| Target vulnerable groups for interventions |
| Telephonic counseling and support for frontline workers |
| Multidisciplinary collaboration: Mental health professionals as advocates |
Figure 2.
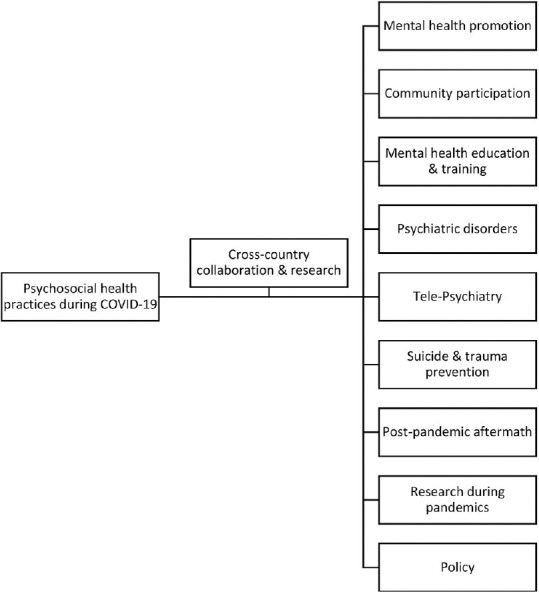
Mental and psychosocial health practices during the Coronavirus disease 2019 pandemic
Table 4.
Attributes of various mental health practices during the pandemic
| Mental healthcare practice | Attributes |
|---|---|
| Mental health promotion | Improve KAP |
| Fight misinformation | |
| Community awareness | |
| Community participation | Integration of care: GPs, AYUSH, primary HCWs, etc. |
| Tele-training and guidance | |
| Community screening for SMD and CMD | |
| Mental health education and training | IEC activities |
| Liaison with media/popular figures | |
| Anti-stigma interventions | |
| Prevention of domestic violence, child and elder abuse | |
| Dealing with psychiatric disorders | Tele-medicine (online platforms, mobile apps, telephonic consultations) |
| Medication availability | |
| District mental health teams | |
| Coordination of referrals | |
| Prompt management of psychiatric emergencies | |
| Decreased institutionalization | |
| Tele-psychiatry | Standardization of guidelines/prescribing patterns |
| Legislations | |
| Tele-psychotherapy | |
| Enabling access for the older adults/minorities | |
| Suicide and trauma prevention | Gatekeeper training |
| Suicide prevention community programs | |
| Target vulnerable groups | |
| Post-pandemic aftermath | Digitalization of care and research |
| Preparedness | |
| Resource allocation | |
| Cross-specialty coordination | |
| Epidemiological data to address policies | |
| Research during pandemics | Ethics |
| Validation of new tools specific to COVID-19 | |
| Standardization of online surveys | |
| Focus on: Neurobiology, acute and long-term neuropsychiatric effects, lived experiences, vulnerable groups, population-based psychiatric risk estimates for various disorders | |
| Sharing research | |
| Socio-cultural sensitivity | |
| Policy | Enabling the above practices |
| Budget and resource allocation | |
| Including mental health in legislations (pandemic acts) | |
| National guidelines for safe practice |
KAP – Knowledge attitude and practice; GP – General physicians; AYUSH – Ayurveda, Yoga, Unani, Sidda and Homeopathy; HCW – Health care workers; SMD – Severe mental disorders; CMD – Common mental disorders; IEC – Information Education and Communication; COVID-19 – Coronavirus disease 2019
Research in mental health during pandemics Implications
The effects of coronaviruses on human central nervous system are a well-known fact. It is worthwhile to explore the psychological, social and neuroscientific underpinnings of COVID-19 and systematic research might help shape interventions and policies. The landmark paper in Lancet on multidisciplinary research priorities in mental health science during the COVID-19 pandemic emphasizes on organized and high quality immediate priorities and long-term research strategies.[52] Research-driven management will be better suited to address the psychosocial and neuropsychiatric effects of the pandemic and shape guidelines for future. Holmes et al.[52] further raises several important areas of global research on “mental health and COVID-19” effect of the outbreak on self-harm and suicide, generation of chronic trauma, impact of social distancing and prolonged lockdown, vulnerabilities of the special groups, harmful effects of repetitive media exposure and misinformation, and finally compliance strategies for mental healthcare. Some of the studies reviewed in this article attempt to answer these questions, though cross-sectionally. Population-based risk estimates, lived experiences of the frontline groups and patients, ethnographic work with the minorities, and community-based heterogeneous mixed-method studies might offer better perspectives. The emerging novel tools specific to COVID-19 such as CAS, FCS, etc., offer promise but need be better understood in terms of psychometric properties and the cross-country validation will help add value to their use.[10]
The SAARC countries have numerous ethnocultural and racial variations, and research needs to be sensitive to them. Digital-driven research and standardization of online surveys will be a norm of the post-COVID era, and psychiatric research needs to be prepared for it.[50] At the same time, ethics is a vital aspect and there needs to be a fine balance between scientific enthusiasm and the principles of benevolence. This is specially applicable for populations with impaired capacity for consent like older adults with cognitive impairment, severe mental disorders, and minors.[53] The ultimate goal of scientific research is the greater good, but definitely not at the cost of undermining the autonomy and rights of the general population, who are already in the clutches of a pandemic.
CONCLUSION
COVID-19 has created rippling psychosocial effects globally, and the South Asian countries face unique challenges to deal with the same as discussed above. The WPA in its official position statement has highlighted the role of psychiatrists, protection of the mentally ill, and improvising on the quality on psychiatric care and research.[54] The present review shows an increased prevalence of depression, anxiety, sleep, and alcohol use disorders in the general population as an impact of COVID-19 and lockdown, with the symptoms being related to social isolation, misinformation, social media exposure, fear of infection, and uncertainty. Xenophobia and stigma are other related factors. Mental healthcare and research strategies during the pandemic and preparedness for post-pandemic aftermath are advocated subsequently. It is imperative to mention that recent Indian studies have been published on the state of mental health services in various training centers and sleep quality during the COVID-19 lockdown.[55,56] They were outside the timeline for the review, but nevertheless holds promise in subsequent analysis and research. The validity of mental health assessment tools specific to COVID-19 and ethical concerns for online surveys are vital areas for consideration. Lessons learnt from this pandemic might help shape interventions and legislations in the near future. “Tremendous interconnectedness” at local and global levels has been recommended to fight the pandemic.[57] In that context, the available research forms the anchor and calls for more systematic exploration and multi-disciplinary care in areas of mental health during the ongoing crisis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.World Health Organization. Coronavirus Disease (COVID-19): Situation Report, 165. World Health Organization: 2020. [Google Scholar]
- 2.Singhal T. A review of coronavirus disease-2019 (COVID-19) Indian J Pediat. 2020;87:1–6. doi: 10.1007/s12098-020-03263-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Torales J, O'Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. 2020;66:317–20. doi: 10.1177/0020764020915212. [DOI] [PubMed] [Google Scholar]
- 4.Duan L, Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatry. 2020;7:300–2. doi: 10.1016/S2215-0366(20)30073-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Adhanom Ghebreyesus T. Addressing mental health needs: An integral part of COVID-19 response. World Psychiatry. 2020;19:129–30. doi: 10.1002/wps.20768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu P, Fang Y, Guan Z, Fan B, Kong J, Yao Z, et al. The psychological impact of the SARS epidemic on hospital employees in China: Exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry. 2009;54:302–11. doi: 10.1177/070674370905400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li W, Yang Y, Ng CH, Zhang L, Zhang Q, Cheung T, et al. Global imperative to combat stigma associated with the coronavirus disease 2019 pandemic. Psychol Med. 2020;1-2 doi: 10.1017/S0033291720001993. Published online first on May 26, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Troyer EA, Kohn JN, Hong S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain Behav Immunity. 2020;87:34–9. doi: 10.1016/j.bbi.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hao F, Tan W, Jiang L, Zhang L, Zhao X, Zou Y, et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav Immunity. 2020;87:100–6. doi: 10.1016/j.bbi.2020.04.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ransing R, Ramalho R, Orsolini L, Adiukwu F, Gonzalez-Diaz JM, Larnaout A, et al. Can COVID-19 related mental health issues be measured? Assessment options for mental health professionals. Brain Behav Immunity. 2020;88:32. doi: 10.1016/j.bbi.2020.05.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee SA. How much “Thinking” about COVID-19 is clinically dysfunctional? Brain Behav Immun. 2020;87:97–8. doi: 10.1016/j.bbi.2020.04.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Taylor S, Landry C, Paluszek M, Fergus TA, McKay D, Asmundson GJ. Development and initial validation of the COVID stress scales. J Anxiety Disord. 2020;72:102232. doi: 10.1016/j.janxdis.2020.102232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sultana F, Reza HM. Are SAARC countries prepared to combat COVID-19 to save young, working-age population? AIMS Public Health. 2020;7:440. doi: 10.3934/publichealth.2020036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Psychiatric Association. [Last accessed on 2020 June 25]. Available from: https://wwwwpanetorg/copy-of-member-societies .
- 15.UNICEF South Asia. [Last accessed on 2020 Jun 25]. Available from: https://wwwuniceforg/rosa/press-releases/millions-children-affected-devastating-flooding-southasia-many-more-risk-covid-19 .
- 16.Patel V, Maj M, Flisher AJ, De Silva MJ, Koschorke M, Prince M. WPA Zonal and Member Society Representatives, Tempier R, Riba M, Sanchez M, Campodonico FD. Reducing the treatment gap for mental disorders: A WPA survey. World Psychiatry. 2010;9:169–76. doi: 10.1002/j.2051-5545.2010.tb00305.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement [published correction appears] Int J Surg. 2010;8:658. [Google Scholar]
- 18.Varshney M, Parel JT, Raizada N, Sarin SK. Initial psychological impact of COVID-19 and its correlates in Indian Community: An online (FEEL-COVID) survey. PLoS One. 2020;15:e0233874. doi: 10.1371/journal.pone.0233874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Khanna RC, Honavar SG, Metla AL, Bhattacharya A, Maulik PK. Psychological impact of COVID-19 on ophthalmologists-in-training and practising ophthalmologists in India. Indian J Ophthalmol. 2020;68:994–8. doi: 10.4103/ijo.IJO_1458_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chandu VC, Pachava S, Vadapalli V, Marella Y. Development and Initial Validation of the COVID-19 Anxiety Scale. Indian J Public Health. 2020;64:S201–S204. doi: 10.4103/ijph.IJPH_492_20. [DOI] [PubMed] [Google Scholar]
- 21.Narasimha VL, Shukla L, Mukherjee D, Menon J, Huddar S, Panda UK, et al. Complicated alcohol withdrawal-an unintended consequence of COVID-19 lockdown. Alcohol Alcohol. 2020;55:350–3. doi: 10.1093/alcalc/agaa042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Roy D, Tripathy S, Kar SK, Sharma N, Verma SK, Kaushal V. Study of knowledge, attitude, anxiety perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian J Psychiatr. 2020;51:102083. doi: 10.1016/j.ajp.2020.102083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Balhara YP, Kattula D, Singh S, Chukkali S, Bhargava R. Impact of lockdown following COVID-19 on the gaming behavior of college students. Indian J Public Health. 2020;64:S172–6. doi: 10.4103/ijph.IJPH_465_20. [DOI] [PubMed] [Google Scholar]
- 24.Balhara YP, Singh S, Narang P. Effect of lockdown following COVID-19 pandemic on alcohol use and help-seeking behavior: Observations and insights from a sample of alcohol use disorder patients under treatment from a tertiary care center. Psychiatry Clin Neurosci. 2020;74:440–1. doi: 10.1111/pcn.13075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Grover S, Sahoo S, Mehra A, Avasthi A, Tripathi A, Subramanyan A, et al. Psychological impact of COVID19 lockdown: An online survey from India. Indian J Psychiatry. 2020;62:354. doi: 10.4103/psychiatry.IndianJPsychiatry_427_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chakraborty K, Chatterjee M. Psychological impact of COVID19 pandemic on general population in West Bengal: A cross-sectional study. Indian J Psychiatry. 2020;62:266–72. doi: 10.4103/psychiatry.IndianJPsychiatry_276_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chatterjee SS, Bhattacharyya R, Bhattacharyya S, Gupta S, Das S, Banerjee BB. Attitude, practice, behavior, and mental health impact of COVID-19 on doctors. Indian J Psychiatry. 2020;62:257–65. doi: 10.4103/psychiatry.IndianJPsychiatry_333_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Balkhi F, Nasir A, Zehra A, Riaz R. Psychological and Behavioral Response to the Coronavirus (COVID-19) Pandemic. Cureus. 2020;12:e7923. doi: 10.7759/cureus.7923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Arafat SM, Alradie-Mohamed A, Kar SK, Sharma P, Kabir R. Does COVID-19 pandemic affect sexual behaviour? A cross-sectional, cross-national online survey. Psychiatry Res. 2020;289:113050. doi: 10.1016/j.psychres.2020.113050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chew NW, Lee GK, Tan BY, Jing M, Goh Y, Ngiam NJ. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. 2020;1591:30523–7. doi: 10.1016/j.bbi.2020.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Res. 2020;288:112954. doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liu S, Yang L, Zhang C, Xiang YT, Liu Z, Hu S, et al. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e17–8. doi: 10.1016/S2215-0366(20)30077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lin K, Yang BX, Luo D, Liu Q, Ma S, Huang R, et al. The mental health effects of COVID-19 on health care providers in China. Am J Psychiatry. 2020;177:635–6. doi: 10.1176/appi.ajp.2020.20040374. [DOI] [PubMed] [Google Scholar]
- 34.Galbraith N, Boyda D, McFeeters D, Hassan T. The mental health of doctors during the COVID-19 pandemic. BJ Psych Bull. 2020:1–4. doi: 10.1192/bjb.2020.44. Published online on April 28th 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li W, Yang Y, Liu ZH, Zhao YJ, Zhang Q, Zhang L, et al. Progression of mental health services during the COVID-19 outbreak in China. Int J Biol Sci. 2020;16:1732–8. doi: 10.7150/ijbs.45120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liu Q, Luo D, Haase JE, Guo Q, Wang XQ, Liu S, et al. The experiences of health-care providers during the COVID-19 crisis in China: A qualitative study. Lancet Glob Health. 2020;8:e790–e798. doi: 10.1016/S2214-109X(20)30204-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Amerio A, Bianchi D, Santi F, Costantini L, Odone A, Signorelli C, et al. Covid-19 pandemic impact on mental health: A web-based cross-sectional survey on a sample of Italian general practitioners. Acta Biomed. 2020;91:83–8. doi: 10.23750/abm.v91i2.9619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McIntyre RS, Lee Y. Preventing suicide in the context of the COVID -19 pandemic. World Psychiatry. 2020;19:250–1. doi: 10.1002/wps.20767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sharma R, Tikka SK. COVID-19 Online Surveys Need to Follow Standards and Guidelines: Comment on” Does COVID-19 Pandemic Affect Sexual Behaviour A Cross-Sectional, Cross-National Online Survey” and” Binge Watching Behavior During COVID 19 Pandemic: A Cross-Sectional, Cross-National Online Survey”. Psychiatry research. 2020 Aug 1;290:113173. doi: 10.1016/j.psychres.2020.113173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sharma R, Tikka SK. COVID-19 online surveys need to follow standards and guidelines: Comment on “Does COVID-19 pandemic affect sexual behaviour? A cross-sectional, cross-national online survey” and “Binge watching behavior during COVID 19 pandemic: A cross-sectional, cross-national online survey”. Psychiatry Res. 2020;290:113173. doi: 10.1016/j.psychres.2020.113173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Indian Psychiatric Society. [Last accessed on 2020 Jul 25]. Available from: https://indianpsychiatricsocietyorg/ips-nimhans-ebook/May 2020 .
- 43.National Institute of Mental Health and Neurosciences. [Last accessed on 2020 Jul 25]. Available from: https://nimhansacin/wp-content/uploads/2020/04/Mental Health Issues COVID-19 NIMHANSpdf April 2020 .
- 44.Mukhtar S. Mental health and emotional impact of COVID-19: Applying Health Belief Model for medical staff to general public of Pakistan. Brain Behav Immun. 2020;87:28–9. doi: 10.1016/j.bbi.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Monjur MR. Covid19 COVID-19 and suicides: The urban poor in Bangladesh. Australian New Zealand J Psychiatry. 2020 Jun;19:0004867420937769. doi: 10.1177/0004867420937769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Srichannil C. The COVID-19 pandemic and Thailand: A psychologist's viewpoint. Psychol Trauma. 2020;12:485. doi: 10.1037/tra0000808. [DOI] [PubMed] [Google Scholar]
- 47.Ho CS, Chee CY, Ho RC. Mental health strategies to combat the psychological impact of COVID-19 beyond paranoia and panic. Ann Acad Med Singap. 2020;49:155–60. [PubMed] [Google Scholar]
- 48.Banerjee D. The COVID-19 outbreak: Crucial role the psychiatrists can play. Asian J Psychiatr. 2020;50:102014. doi: 10.1016/j.ajp.2020.102014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Banerjee D, Nair VS. Handling the COVID-19 pandemic: Proposing a community based toolkit for psycho-social management and preparedness. Asian J Psychiatry. 2020;51:102152. doi: 10.1016/j.ajp.2020.102152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Türközer HB, Öngür D. A projection for psychiatry in the post-COVID-19 era: Potential trends, challenges, and directions. Mol Psychiatry. 202:1–6. doi: 10.1038/s41380-020-0841-2. Published online July 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Indian Psychiatric Society. [Last accessed on 2020 Jul 25]. Available from: https://indianpsychiatricsociety org/e-book-telepsychiatry-operational-guidelines-2020/June 2020 .
- 52.Holmes EA, O'Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry. 2020;7:547–60. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Townsend E, Nielsen E, Allister R, Cassidy SA. Key ethical questions for research during the COVID-19 pandemic. Lancet Psychiatry. 2020;7:381–3. doi: 10.1016/S2215-0366(20)30150-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.World Psychiatric Association. [ First accessed on 2020 Jul 30]. Available from: https://wwwwpanetorg/position-statements/COVID-19 2020 .
- 55.Grover S, Mehra A, Sahoo S, Avasthi A, Tripathi A, D'Souza A, et al. State of mental health services in various training centers in India during the lockdown and COVID-19 pandemic. Indian J Psychiatry. 2020;62:363. doi: 10.4103/psychiatry.IndianJPsychiatry_567_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gupta R, Grover S, Basu A, Krishnan V, Tripathi A, Subramanyam A, et al. Changes in sleep pattern and sleep quality during COVID-19 lockdown. Indian J Psychiatry. 2020;62:370. doi: 10.4103/psychiatry.IndianJPsychiatry_523_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Unützer J, Kimmel RJ, Snowden M. Psychiatry in the age of COVID-19. World Psychiatry. 2020;19:130. doi: 10.1002/wps.20766. [DOI] [PMC free article] [PubMed] [Google Scholar]


