At the end of December 2019, a novel coronavirus (SARS-CoV-2) started to spread in the city of Wuhan, Hubei province in China, first described as novel coronavirus [1,2]. Meanwhile, the current COVID-19 pandemic has hit every country on the globe.
Health care systems have since varied significantly in their response to the immense challenges.
With an online survey targeting the worldwide medical community (emergency medical service, nurses, physicians, sonographers, technicians) we sought to discover experiences, fears, and successful strategies for the expected second wave.
The survey was open from April 24th, 2020 until June 24th, 2020. A total of 3,090 participants from 88 countries completed the survey, 49.4% were female, sample characteristics are presented in Table 1 . During the worst times of the pandemic in their country, 238 (7.7%) reported to have suffered from a collapse of the system.
Table 1.
Baseline characteristics of the participants and main results of the survey.
| Total | Collapse of the system | No collapse | P value | |
|---|---|---|---|---|
| Number of participants | 3090 | 238 | 2850 | |
| Country USA Germany India Austria Italy United Kingdom Others |
502 (16.2) 216 (7) 179 (5.8) 171 (5.5) 116 (3.8) 106 (3.4) 1800 (58) |
30 (12.6) 3 (1.3) 14 (5.9) 6 (2.5) 24 (10.1) 7 (2.9) 154 (64.7) |
472 (16.5) 213 (7.5) 165 (5.8) 165 (5.8) 92 (3.2) 99 (3.5) 1644 (57.7) |
0.74 |
| Male sex | 1565 (50.6) | 128 (53.8) | 1437 (50.4) | 0.32 |
| Age 18-35 36-45 46-60 >60 |
819 (24.5) 863 (27.8) 1035 (33.5) 373 (12.1) |
55 (23.1) 62 (26) 91 (38.3) 30 (12.6) |
763 (26.8) 800 (28) 944 (33.1) 343 (12) |
0.18 |
| Profession Sonographer Cardiologist Internist ICU doctor ER doctor General practitioner Other doctor |
643 (20.8) 577 (18.7) 382 (12.4) 242 (7.8) 129 (4.2) 165 (5.3) 557 (18) |
50 (21) 38 (16) 31 (13) 31 (13) 7 (2.9) 14 (5.9) 42 (17.7) |
593 (20.8) 538 (18.9) 351 (12.3) 211 (7.4) 122 (4.3) 151 (5.3) 515 (18.1) |
0.95 |
| Workplace Tertiary hospital Local hospital Private hospital Secondary care Primary care |
956 (30.9) 766 (24.8) 550 (17.8) 225 (7.3) 309 (10) |
85 (35.7) 49 (20.6) 40 (16.8) 16 (6.7) 27 (11.3) |
869 (30.5) 717 (25.2) 510 (17.9) 209 (7.3) 282 (9.9) |
0.27 |
| Have you personally been tested? Yes (pos) Yes (neg) No |
114 (3.7) 840 (27.2) 2134 (69.1) |
22 (9.2) 65 (27.3) 151 (63.4) |
92 (3.2) 775 (27.2) 1983 (69.6) |
0.006 |
| Do you know a colleague who tested positive? Yes No |
1888 (61.1) 1200 (38.8) |
185 (77.7) 53 (22.3) |
1703 (59.8) 1147 (40.2) |
<0.001 |
| Do you know a colleague who died from COVID-19? Yes No |
560 (18) 2528 (82) |
97 (40.8) 141 (59.2) |
463 (16.2) 2387 (83.8) |
<0.001 |
| Have you observed patients who were harmed by measures not by COVID19 Yes No |
1793 (58) 748 (24.2) |
152 (63.9) 47 (19.7) |
1640 (57.5) 701 (24.6) |
0.13 |
| What is your greatest fear during pandemic Falling ill/dying from COVID Financial losses Losing family member Pandemic cannot be controlled Negative impact on my career No fear |
414 (13.4) 394 (12.8) 1259 (40.7) 696 (22.5) 81 (2.6) 246 (8) |
35 (14.7) 22 (9.2) 97 (40.8) 57 (23.9) 11 (4.6) 16 (6.7) |
379 (13.3) 372 (13.1) 1161 (40.7) 638 (22.4) 70 (2.5) 230 (8.1) |
0.75 |
| Have you observed patients who tested negative but actually were positive No Few (1-5) Many (>5) |
1094 (35.4) 1108 (35.9) 886 (28.6) |
70 (29.4) 62 (26.1) 106 (44.5) |
1024 (35.9) 1046 (36.7) 780 (27.4) |
<0.001 |
The pandemic is having an impact on the life of all, but particularly on those in the first line of the defense, the health care professionals (HCP). In this global survey, a total of 92% of the participants reported to have fears related to the pandemic, most (41%) are afraid of losing a family member, 22.5% worry there might be no control over the pandemic, 13.4% are afraid to fall ill or die themselves, and 12.8% are afraid of private financial losses. Interestingly, there was no difference in fears between those countries where high incidence rates were reported and those where there were few COVID-19 cases.
However, not only the psychological burden is high for HCP. When comparing those with a collapse of the system and those without, 9% vs. 3% (p=0.006) of the participants tested positive themselves, 78% vs. 60% (p<0.001) know a colleague who tested positive, and 41% vs. 16% (p<0.001) know a colleague who died from COVID-19.
At this time, most countries are preparing for or are already experiencing the second wave. Therefore, it is essential to learn the lessons from those who went through an extreme first wave. This survey confirms the unreliability of a negative COVID-19 test. A total of 64% of the participants reported of personal experience with false-negative tests, 44% of those from countries hit hard by the pandemic reported to have seen more than five patients with an initially negative test who turned positive during their stay at the hospital. A negative test must not be considered a safe rule-out of COVID-19 if clinical suspicion is high.
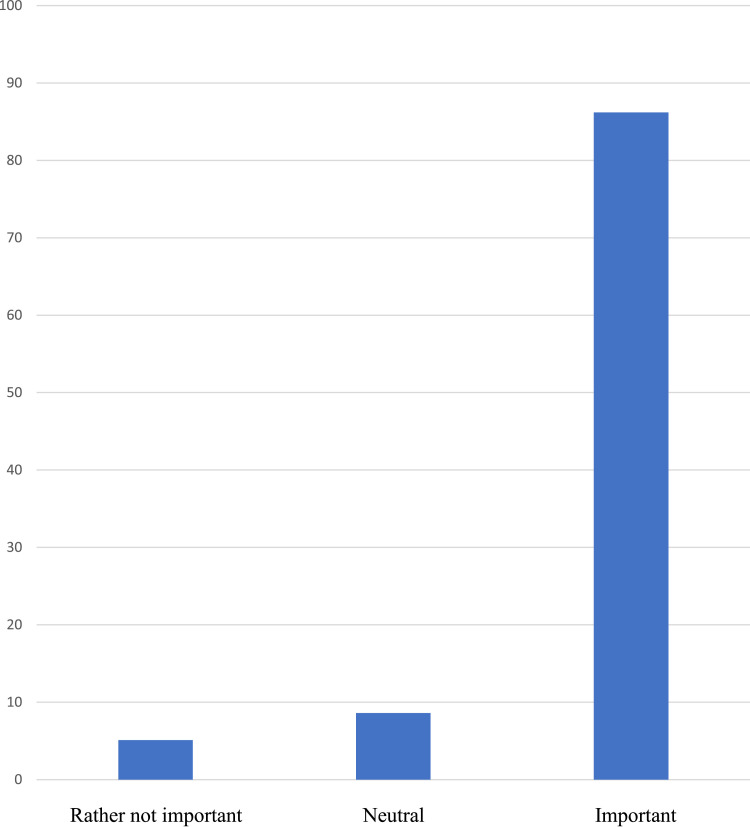
The pandemic of a hazardous and highly contagious virus is a medical disaster. The medical community is the group which is directly in contact with COVID-19. Therefore, their firsthand experience and opinion should have a loud voice in policy making and public health discussions: A total of 86% reported that they consider social distancing important to tackle the pandemic (Fig. 1 ). At the same time, 58% reported that they have seen patients who had a serious health hazard not due to COVID-19 but due to the lockdowns. During reduction of service or lockdowns, concepts must be implemented to ensure the medical service for those with chronic and acute diseases other than COVID-19.
Fig. 1.
Answer to the question “how important do you consider social distancing?”. A total of 159 (5.1%) participants chose “rather not important”, 267 (8.6%) were undecided, and 2664 (86.2%) answered “important” or “very important”.
Declaration of Competing Interest
All authors have read and approved submission of the manuscript and have no conflict of interest to disclose.
References
- 1.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Viruses CSGotICoTo The species severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 2020;5(4):536–544. doi: 10.1038/s41564-020-0695-z. [DOI] [PMC free article] [PubMed] [Google Scholar]