We have read “Thorley J. Gut feelings. Lancet Gastroenterol Hepatol 2016; 1:14.”
In our opinion, the hypothesis made by the author in the article may lead to a misunderstanding, i.e., the function of serotonin secreted from argentaffin in intestines is different from that in the brain.
Depression and anxiety are caused by a change or decrease in the levels of serotonin found at nerve endings in some regions of the brain (1, 2). Of the total serotonin in our body, 90% is synthesized by the argentaffin cells in the gastrointestinal tract (GIT). Notably, only about 1%–2% of the total amount of serotonin in the body is produced by serotonergic neurons in the brain (1, 2).
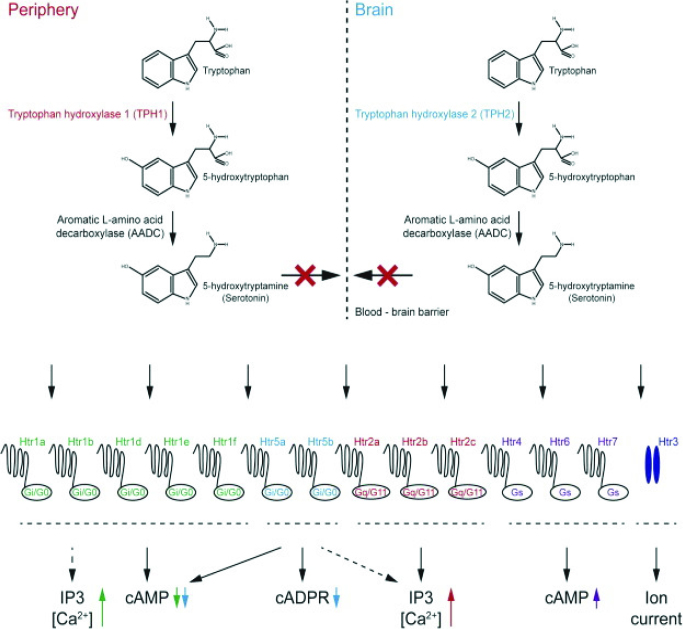
Serotonin is synthesized in different regions of the body. It acts as a neurotransmitter in the brain and as an intracellular signaling molecule and auto or paracrine factor in the periphery (1, 2). The serotonin synthesized in the argentaffin cells in intestines regulates functions such as excretion in the GIT (Figure 1). This serotonin cannot reach the brain since it cannot cross the “blood-brain barrier”; therefore, the serotonin acting as a hormone in the periphery is not relevant to the emotional status (Figure 2). Briefly, two major pools of serotonin can be distinguished: the brain serotonin, synthesized mainly in the brainstem, and the peripheral serotonin (2, 3). The brain cells synthesize their own serotonin from an amino acid called “tryptophan,” taken as a part of the diet. The amount of serotonin in these neurons can be controlled for the treatment of depression and anxiety disorders (4). Serotonin has been known for nearly 70 years. It was isolated from the serum for the first time in 1948. Soon after in 1951, enteramine was isolated and characterized from the gut enterochromaffin cells (argentaffin cells) (1). However, to date, no “serotonin” preparation that can be taken via the oral route has been developed.
Figure 1.
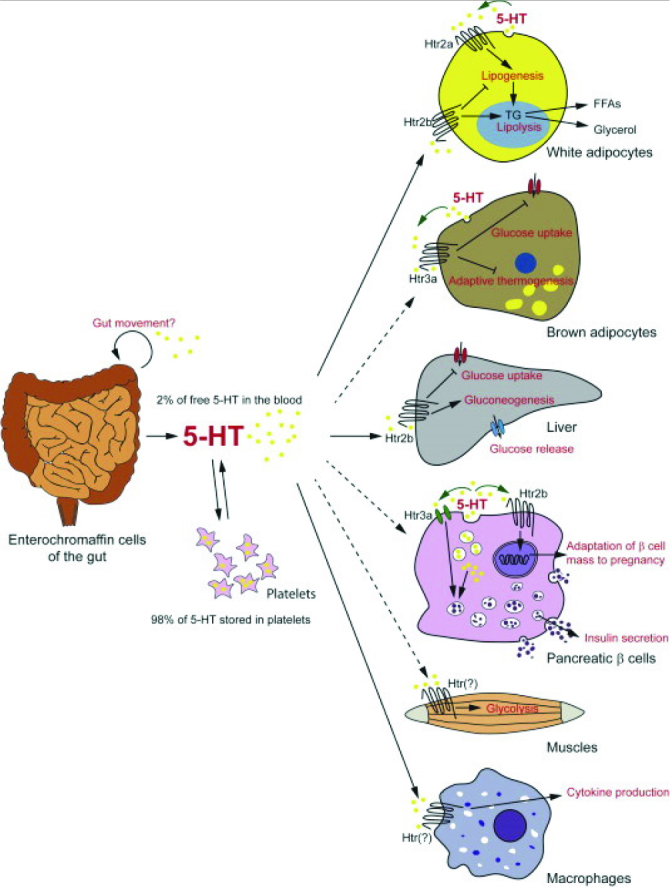
The serotonin synthesized in the argentaffin cells in intestines regulates functions, such as excretion, in the GIT. Furhermore, the serotonin acts as a hormone in the periphery (2).
Figure 2.
Two major pools of serotonin can be distinguished: the brain serotonin, synthesized in the brainstem, and the peripheral serotonin (2).
The best example to show that intestinal serotonin cannot be associated with depression is “carcinoid tumor” disease. In this disease, the amount of serotonin secreted by the intestinal argentaffin cells (IAC) substantially increases. If the point of view that “serotonin secreted from intestines makes you happy” is held, then the patients with carcinoid tumors who secrete excessive serotonin should be the happiest people in the world (5). In fact, the mental state of patients with this tumor is not good. Patients experience diarrhea, flushing, abdominal pain, and palpitations due to excessively increased intestinal serotonin and its metabolites(5, 6). Another popular myth about serotonin is that eating a banana makes a person happy, as it contains serotonin. The serotonin contained in a banana cannot cross blood-brain barrier either (6). It should be noted that psychiatric and neurological diseases do not develop because of a single cause, and gut microbiota may only be one of them.
In conclusion, the insights regarding serotonin secreted from the IAC should not be applied to that sectreted from the brain. If our immune and digestive systems are strong, and we are in good intestinal health, we feel happy and vigorous. This applies to all organs. For example, brain functions of a person with impaired hepatic and renal functions would be adversely affected.
Footnotes
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – A.B., İ.T.U.; Design – A.B.; Supervision - İ.T.U.; Resource – A.B., H.E.; Data Collection and/or Processing – H.E., M.U.; Analysis and/or Interpretation – A.B.; Literature Search – H.E., M.U.; Writing – H.E., M.U.; Critical Reviews – A.B., İ.T.U.
Conflict of Interest: The authors have no conflict of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Lv J, Liu F. The Role of Serotonin beyond the Central Nervous System during Embryogenesis. Front Cell Neurosci. 2017;11:74. doi: 10.3389/fnpit.2017.00400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.El-Merahbi R, Löffler M, Mayer A, Sumara G. The roles of peripheral serotonin in metabolic homeostasis. FEBS letters. 2015;589:1728–34. doi: 10.1016/j.febslet.2015.05.054. [DOI] [PubMed] [Google Scholar]
- 3.Gershon MD, Tack J. The serotonin signaling system: from basic understanding to drug development for functional GI disorders. Gastroenterology. 2007;132:397–414. doi: 10.1053/j.gastro.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 4.Molliver ME. Serotonergic neuronal systems: what their anatomic organization tells us about function. J Clin Psychopharmacol. 1987;7:3S–23S. doi: 10.1097/00004714-198712001-00002. [DOI] [PubMed] [Google Scholar]
- 5.Basuroy R, Srirajaskanthan R, Ramage JK. Neuroendocrine Tumors. Gastroenterol Clin North Am. 2016;45:487–507. doi: 10.1016/j.gtc.2016.04.007. [DOI] [PubMed] [Google Scholar]
- 6.Garcıa-Hernandez J, Mohmaduvesh M, Davies P, Toumpanakis C, Goodhand JR, Caplin M, Skuse D. PTU-163 Depression and carcinoid syndrome: is there any relationship? A cross-sectional study. Gut. 2012;61(Suppl 2):A252. [Google Scholar]
- 7.Young SN. How to increase serotonin in the human brain without drugs. J Psychiatry Neurosci. 2007;32:394–9. [PMC free article] [PubMed] [Google Scholar]