Abstract
Background
Little is known about the contemporary mortality experience among adults with congenital heart disease (CHD). The objectives of this study were to assess the age at death, presence of cardiovascular comorbidities, and most common causes of death among adults with CHD in a contemporary cohort within the United States.
Methods and Results
Patients with CHD who had a healthcare encounter between 2008 and 2013 at 1 of 5 comprehensive CHD centers in North Carolina were identified by International Classification of Diseases, Ninth Revision (ICD‐9), code. Only patients who could be linked to a North Carolina death certificate between 2008 and 2016 and with age at death ≥20 years were included. Median age at death and underlying cause of death based on death certificate data were analyzed. The prevalence of acquired cardiovascular risk factors was determined from electronic medical record data. Among the 629 included patients, the median age at death was 64.2 years. Those with severe CHD (n=157, 25%), shunts (n=202, 32%), and valvular lesions (n=174, 28%) had a median age at death of 46.0, 65.0, and 73.3 years, respectively. Cardiovascular death was most common in adults with severe CHD (60%), with 40% of those deaths caused by CHD. Malignancy and ischemic heart disease were the most common causes of death in adults with nonsevere CHD. Hypertension and hyperlipidemia were common comorbidities among all CHD severity groups.
Conclusions
The most common underlying causes of death differed by lesion severity. Those with severe lesions most commonly died from underlying CHD, whereas those with nonsevere disease more commonly died from non‐CHD causes.
Keywords: aging, congenital heart disease, death
Subject Categories: Congenital Heart Disease, Mortality/Survival, Aging, Cardiovascular Disease
Nonstandard Abbreviations and Acronyms
- CHD
congenital heart disease
ICD ‐9
International Classification of Diseases, Ninth Revision
- IQR
interquartile range
- NC
North Carolina
Clinical Perspective
What Is New?
This is one of the largest and most contemporary analyses of the most common causes of death in adults with congenital heart disease (CHD) in the United States.
Patients with nonsevere CHD lived late into adulthood and most commonly died because of ischemic heart disease and malignancy.
Hypertension and hyperlipidemia were prevalent at high rates among those with nonsevere CHD.
Adults with severe CHD continue to die at a young age, most commonly because of their underlying congenital disease.
What Are the Clinical Implications?
Long‐term follow‐up for all adults with CHD is important, regardless of disease severity.
When following adult patients with nonsevere CHD longitudinally, special focus should be placed on acquired cardiovascular risk factor modification and age‐appropriate cancer screening.
Associated with improved pediatric surgical and perioperative outcomes, the population of patients living with congenital heart disease (CHD) is rapidly growing, with increasing numbers of patients surviving into late adulthood. 1 There are now an estimated 1.4 million adults and 1 million children living with CHD in the United States. 2 Although pediatric survival has improved, surgical strategies may not offer a cure for some forms of CHD; many patients are expected to experience sequelae of their original defect and possible additional interventions throughout their lifetime. Furthermore, despite significant advances, the mortality rate in adults with CHD remains higher than that of the general population. 3 , 4 A detailed understanding of long‐term complications and causes of mortality can be helpful in effectively caring for adults with CHD as they age. Prior studies that focused on defining the most common causes of death in adults with CHD have either used a historical cohort or been based outside of the United States. 3 , 4 , 5 , 6 , 7 , 8 , 9 The aims of the current study are to evaluate the age at death, presence of cardiovascular comorbidities, and the most common causes of death in a large, multicenter, contemporary cohort of adult patients with CHD within the United States.
METHODS
Because of the patient‐level identifiers collected for this study, requests to access the data set from qualified researchers trained in human subject confidentiality protocols may be sent to the Centers for Disease Control and Prevention National Center on Birth Defects and Developmental Disabilities.
Data Source and Study Population
Data for this analysis were obtained from the North Carolina (NC) Congenital Heart Defect Surveillance Network database. This database is composed of patients with CHD, as identified by International Classification of Diseases, Ninth Revision (ICD‐9), code in the electronic medical record, who had a healthcare encounter between 2008 and 2013 at 1 of 5 comprehensive CHD centers or affiliated satellite clinics included in the NC Congenital Heart Defect Surveillance Network. Of the 60 059 patients included in this database, those who could be linked to an NC death certificate between 2008 and 2016 and were ≥20 years old at the time of death were included. Therefore, only those patients with CHD who died during the study period were analyzed in this study. For comparison, all other NC death certificates between 2008 and 2016 with age at death ≥20 years were also analyzed. Institutional Review Board approval was obtained at all of the participating NC sites. The requirement for informed consent was waived.
Study Definitions
CHD diagnoses were grouped by lesion severity for all analyses. The groupings of severe, shunt, and valve were predetermined by the Centers for Disease Control and Prevention Congenital Heart Defect Surveillance Network using a previously described method that categorizes CHD diagnostic codes into mutually exclusive hierarchical groups, similar to Marelli et al, integrating both hemodynamic severity and basic anatomical characteristics. 10 , 11 Diagnoses included in each group with corresponding ICD‐9 codes are shown in Table S1. The category of other included CHD ICD‐9 codes that could not be classified as severe, shunt, or valve. Patients with more than one lesion were classified by the lesion of highest severity (severe > shunt > valve > other). To ensure that only patients with CHD were included, the ICD‐9 code 745.5 (atrial septal defect [secundum] or patent foramen ovale) was not included in the analysis. Furthermore, as the other CHD category represents a highly heterogeneous group of diagnoses, it was excluded from the cause of death portion of the analysis.
Statistical Analysis
Baseline characteristics were summarized as medians (25th–75th percentiles) for continuous variables and percentages (frequencies) for categorical variables. Median age at death, with interquartile ranges (IQRs), was analyzed for the overall CHD cohort, as well as for each lesion severity group. P values for median age at death among patients with CHD versus all NC deaths was generated using a 2‐sided Wilcoxon rank‐sum test. P values for median age at death among CHD lesion severity groups versus other lesion severity groups were generated using the Kruskal‐Wallis test (overall), followed by pairwise comparisons with Wilcoxon rank‐sum test with Tukey adjustment for multiple comparisons.
The underlying cause of death, as reported on each NC death certificate, was categorized into descriptive groups by the study team. Descriptive groups were further categorized as cardiovascular death, noncardiovascular death, and CHD death (a subgroup of cardiovascular death). Crude mortality rates for all‐cause mortality, cardiovascular mortality, and CHD‐related mortality were calculated using the number of deaths during the study period (2008–2013) at age ≥20 years as the numerator and the NC Congenital Heart Defect Surveillance Network population age >20 years at study midpoint as the denominator. Crude mortality rates were presented per 1000 patients per year.
A proportionate mortality analysis comparing cardiovascular death versus noncardiovascular death and CHD death versus non‐CHD cardiovascular death was completed. For comparison, median age at death and underlying cause of death analyses were repeated using all other NC death certificates between 2008 and 2016 with age at death ≥20 years. To further understand the observed differences in age at death and causes of death, the prevalence of risk factors for acquired cardiovascular disease was analyzed for the overall cohort, as well as by lesion severity group, using electronic health record data. P values were obtained from the Fisher exact test. All analyses were performed using SAS v9.4 TS1M4 (SAS, Inc, Cary, NC).
RESULTS
Baseline Characteristics and Age at Death
Baseline characteristics are summarized in Table 1. Age at death is presented in Table 2. A total of 629 adult patients with CHD who died in NC during the study period were included (Figure 1). Of those included, 157 (25%) were characterized as having severe CHD, 202 (32%) were characterized as having a shunt lesion, and 174 (28%) were characterized as having a valvular lesion. A total of 96 patients (15%) could not be classified in the severe, shunt, or valve group. The median age at death for all patients with CHD was 64.2 years (IQR, 47.5–76.5 years). Those with severe CHD, shunts, and valvular lesions had a median age of death at 46.0 (IQR, 34.3–76.5), 65.0 (IQR, 51.8–75.1), and 73.3 (IQR, 56.4–81.5) years, respectively. Among all other adult NC death certificates during the study period, the median age at death was 76.5 (IQR, 63.6–86.0) years.
Table 1.
Baseline Characteristics
| Characteristic | Adults (N=629) |
|---|---|
| Sex | |
| Men | 344 (54.7) |
| Women | 285 (45.3) |
| Lesion severity group | |
| Severe | 157 (25.0) |
| Shunt | 202 (32.1) |
| Valve | 174 (27.7) |
| Other* | 96 (15.3) |
Data are given as number (percentage).
Congenital heart disease diagnosis code not classified as severe, shunt, or valve.
Table 2.
Age at Death
| Variable | Age at Death, Median (IQR), y | P Value (vs All NC)* | P Value (vs Other Lesion Severity Groups) † |
|---|---|---|---|
| All NC death certificates | 76.5 (63.6–86.0) | … | … |
| All CHD cohort | 64.2 (47.5–76.5) | <0.0001 | <0.001 (Overall) |
| Severe CHD | 46.0 (34.3–63.0) | <0.0001 | <0.001 (Severe vs shunt) |
| Shunt CHD | 65.0 (51.8–75.1) | <0.0001 | 0.003 (Shunt vs valve) |
| Valve CHD | 73.3 (56.4–81.5) | <0.0001 | <0.001 (Valve vs severe) |
| Other CHD | 69.9 (59.7–79.6) | <0.0001 | … ‡ |
CHD indicates congenital heart disease; IQR, interquartile range; and NC, North Carolina.
Two‐sided Wilcoxon rank‐sum test.
Kruskal‐Wallis test (overall) and Wilcoxon rank‐sum test (pairwise, with Tukey adjustment for multiple comparisons).
Other CHD group not included in pairwise tests with CHD severity groups because of high heterogeneity among included diagnosis codes.
Figure 1.
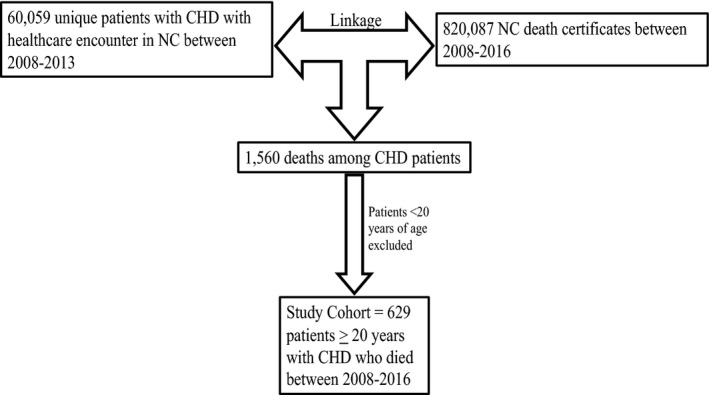
Derivation of patient cohort. CHD indicates congenital heart disease; and NC, North Carolina.
Underlying Cause of Death
The all‐cause mortality rate among all patients with CHD was 11.6 per 1000 patients per year. The cardiovascular and CHD‐specific mortality rates were 4.9 and 1.5 per 1000 patients per year, respectively. The most common causes of death by group are presented in Figure 2. The most common causes of death among all adults with CHD in the death cohort were malignancy (14%), CHD (14%), ischemic heart disease (11%), infection (8%), and lung disease (7%). The most common causes of death among those with severe CHD, shunts, and valvular CHD were CHD (41%), ischemic heart disease (15%), and cancer (17%), respectively. Malignancy was either the most common or the second most common cause of death in all CHD groups. Ischemic heart disease was either the most common or the second most common cause of death in all groups, except among those with severe CHD. Among all other adult deaths in NC in this same time period, the most common causes were malignancy (22%), ischemic heart disease (13%), and chronic neurologic disease (dementia) (10%).
Figure 2.
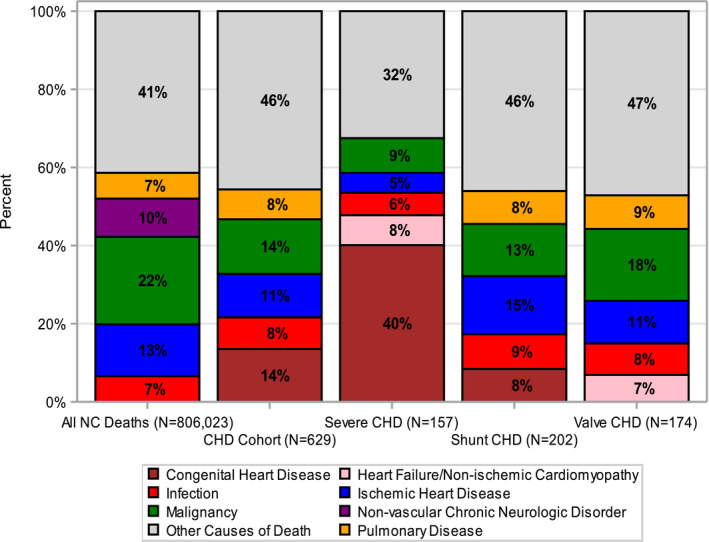
Top 5 most common causes of death. “Other” represents a compilation of all other causes of death not included in the top 5. CHD indicates congenital heart disease; and NC, North Carolina.
The proportion of deaths attributable to cardiovascular disease versus all other causes is summarized in Figure 3. The proportion of deaths attributable to CHD versus non‐CHD cardiovascular disease is presented in Figure 4. Among all adults with CHD, 43% died from any cardiovascular cause, with 33% of those deaths attributable to CHD. In those with severe CHD, most deaths were attributable to a cardiovascular cause (60%), with 68% of the cardiovascular deaths attributable to CHD. Among those with shunts and valvular CHD, 42% and 34% of deaths were attributable to any cardiovascular cause, respectively, with a minority of those cardiovascular deaths attributable to CHD (21% and 8%, respectively). When analyzing all NC death certificates during the study period, 27% of the deaths were attributable to any cardiovascular cause, with 0.1% of those cardiovascular deaths attributable to CHD.
Figure 3.
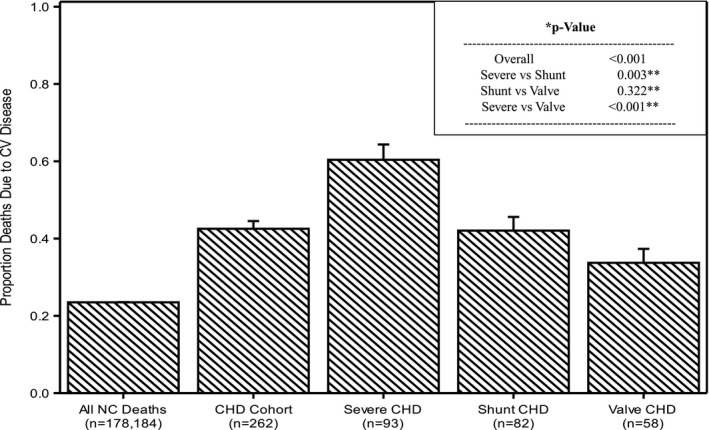
Deaths attributable to cardiovascular disease vs all other causes among all patients in North Carolina (NC) and those with congenital heart disease (CHD). The CHD group is further divided by lesion severity into severe CHD, shunt CHD, and valve CHD. *P values obtained from the Fisher exact test. **The Tukey adjustment for multiple comparisons was applied. CV indicates cardiovascular.
Figure 4.
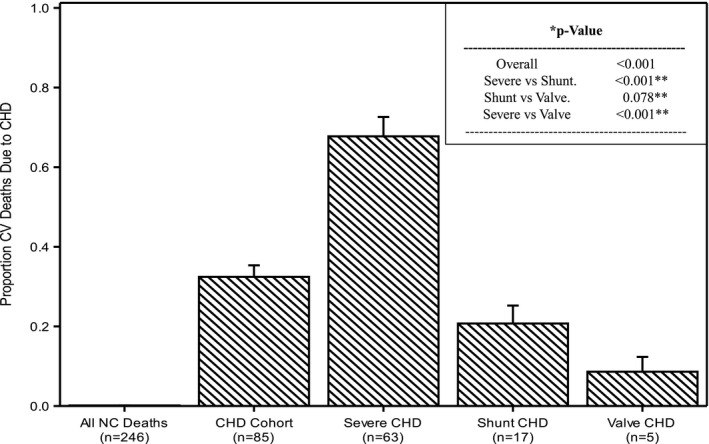
Deaths attributable to congenital heart disease (CHD) vs noncongenital cardiovascular disease among all patients in North Carolina (NC) and those with CHD. The CHD group is further divided by lesion severity into severe CHD, shunt CHD, and valve CHD. *P values obtained from the Fisher exact test. **The Tukey adjustment for multiple comparisons was applied. CV indicates cardiovascular.
Prevalence of Risk Factors for Acquired Cardiovascular Disease
The prevalence of acquired cardiovascular risk factors in our study population is presented in Table 3. Most patients with CHD had hypertension (63.1%). Hypertension was more common among those with shunt and valve lesions (63.9% and 74.7%, respectively) than in those with severe CHD (47.1%). Nearly half of all patients with CHD had hyperlipidemia (48.5%). Hyperlipidemia was also more common among those with shunt and valve lesions (49% and 64.4%, respectively) than in those with severe CHD (35.0%). Diabetes mellitus and chronic kidney disease were both seen in around one third of patients with CHD, both among all included patients and when analyzed by CHD severity group.
Table 3.
Risk Factors for Acquired Cardiovascular Disease
| Characteristic | Severe (N=157) | Shunt (N=202) | Valve (N=174) | P Value* |
|---|---|---|---|---|
| Hypertension | 74 (47.1) | 129 (63.9) | 130 (74.7) | <0.001 |
| Diabetes mellitus | 36 (22.9) | 68 (33.7) | 70 (40.2) | 0.003 |
| Chronic kidney disease | 56 (35.7) | 74 (36.6) | 58 (33.3) | 0.804 |
| Hyperlipidemia | 55 (35.0) | 99 (49.0) | 112 (64.4) | <0.001 |
Values presented are counts (percentages) for categorical variables.
P values obtained from the Fisher exact test.
Discussion
In this analysis, we identified several notable findings. First, among patients with nonsevere CHD, the age at death was approaching, but still younger than, that of the general population. Second, the most common causes of death differed by lesion severity, with CHD being the most common cause of death only among those with severe disease. Third, patients with severe CHD more commonly died from CHD and any cardiovascular disease than those with nonsevere disease. Finally, among those with nonsevere CHD, ischemic heart disease and malignancy were the most common causes of death.
The current study showed that, with the exception of those with severe CHD, the median age at death was approaching, but still younger than, that seen in the general population. Patients with severe CHD continue to die at a comparatively young age, whereas those with nonsevere CHD frequently live into late adulthood. Given that our analysis excluded patients who died during childhood (before the age of 20 years), these results suggest that patients with nonsevere CHD who survive childhood have excellent long‐term survival. This finding highlights the improving management of long‐term sequelae of mild and moderate CHD during adulthood. Conversely, those with severe disease continue to experience early mortality compared with the general population, even when the sickest children who do not survive to adulthood are excluded from analysis.
The most common causes of death seen in adults with CHD differed by the severity of the underlying congenital lesion. Historical studies demonstrated that complications of CHD, specifically heart failure and arrhythmias, were the most common causes of death among all patients with CHD. 3 , 4 , 5 , 7 , 8 , 9 In our analysis, however, CHD was the most commonly reported underlying cause of death only among those with severe CHD, whereas those with nonsevere disease most commonly died due to non‐CHD causes.
Malignancy was 1 of the 2 most common causes of death among patients with nonsevere CHD, and was the most common cause of death in the general population. It has previously been suggested that adults with CHD are at risk for malignancy because of cumulative exposure to ionizing radiation from cardiac procedures over the course of their lifetime. 12 Our analysis further underscores the importance of close monitoring for the development of malignancy with vigilant age‐appropriate cancer screening in adults with CHD.
Among patients with nonsevere CHD, ischemic heart disease was also 1 of the 2 most common causes of death in all groups. Similarly, ischemic heart disease was the second most common cause of death in the general population. Although there has been disagreement in the literature about the importance of coronary artery disease in patients with CHD, a more recent analysis demonstrated that as the life expectancy of patients with CHD increased over time, the most common cause of death in patients with noncyanotic CHD shifted from CHD‐related complications to ischemic heart disease. 7 , 13 In a more contemporary cohort, our analysis again demonstrates that acquired heart disease is an important cause of death in patients with nonsevere CHD.
To better understand why ischemic heart disease has emerged as an important cause of death in patients with nonsevere CHD, the prevalence of risk factors for acquired cardiovascular disease among patients with CHD was assessed. This analysis demonstrated that hypertension and hyperlipidemia were prevalent at high rates among those with nonsevere CHD. Patients with severe CHD had lower rates of these risk factors, likely because an earlier age at death precluded the development of these age‐related conditions. Prior studies have demonstrated that patients with CHD frequently do not receive medical therapy for management of acquired modifiable cardiovascular risk factors. 14 These results suggest the importance of acquired cardiovascular disease risk factor management in adult patients with CHD, particularly those with nonsevere disease, a practice that has the potential to be overlooked because of the complexity of patients' cardiac history.
Limitations
Because CHD and cause of death diagnoses were based on electronic health record and death certificate data, the accuracy of these diagnoses was dependent on physician documentation. The end points of this study were not adjudicated, and clinical information surrounding the death event was not available. Therefore, in some cases in which general diagnoses, such as heart failure and respiratory failure, were used, it was difficult to determine whether the cause of death could have been related to CHD. In addition, in this descriptive analysis, the cardiovascular comorbidities of CHD, such as pulmonary hypertension, arrhythmias, and thrombosis, which may have directly contributed to death caused by CHD, were not evaluated as covariates. Because only NC death certificates were linked, patients who died outside of NC were not included. However, on the basis of 2017 US Census Bureau data showing the rate of migration out of NC to be ≈3% per year, it is unlikely that this significantly affected our results. Because only patients with CHD with a healthcare encounter at a tertiary care center within NC during the study period were included, the results may not be generalizable to all patients with CHD. Finally, because patients were not followed up longitudinally, a survival analysis, which would be a more rigorous way to assess age at death, was not possible.
Conclusions
With the exception of those with severe disease, patients with CHD frequently live into late adulthood, placing them at risk for mortality related to both acquired cardiovascular and noncardiovascular disease. Patients with severe CHD remain at risk for early mortality, primarily related to their underlying congenital heart condition. Those with severe CHD are significantly more likely to die from CHD and any cardiovascular cause than those with nonsevere disease. These results highlight the importance of close long‐term follow‐up for all adults with CHD, with a focus on age‐appropriate cancer screening and acquired risk factor modification in those with nonsevere CHD. Further advances in the long‐term prevention of CHD‐related mortality in patients with severe CHD are still needed.
Sources of Funding
Support for the creation of the North Carolina Congenital Heart Defect Surveillance Network database and statistical analysis was provided by Centers for Disease Control and Prevention grant 5 NU50DD004933‐03‐00.
Disclosures
Dr Goldstein is supported by the National Institutes of Health training grant T‐32‐HL069749‐15. Dr Krasuski is a principal investigator and consultant for Actelion Pharmaceuticals, is a study investigator for Edwards Life Sciences, is an unpaid member of the Scientific Advisory Board for Ventripoint, and has received travel funding from Medtronic and Cryolife. The remaining authors have no disclosures to report.
Supporting information
Table S1
(J Am Heart Assoc. 2020;9:e016400 DOI: 10.1161/JAHA.119.016400.)
For Sources of Funding and Disclosures, see page 7.
REFERENCES
- 1. Khairy P, Ionescu‐Ittu R, Mackie AS, Abrahamowicz M, Pilote L, Marelli AJ. Changing mortality in congenital heart disease. J Am Coll Cardiol. 2010;56:1149–1157. [DOI] [PubMed] [Google Scholar]
- 2. Gilboa SM, Devine OJ, Kucik JE, Oster ME, Riehle‐Colarusso T, Nembhard WN, Xu P, Correa A, Jenkins K, Marelli AJ. Congenital heart defects in the United States: estimating the magnitude of the affected population in 2010. Circulation. 2016;134:101–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Diller GP, Kempny A, Alonso‐Gonzalez R, Swan L, Uebing A, Li W, Babu‐Narayan S, Wort SJ, Dimopoulos K, Gatzoulis MA. Survival prospects and circumstances of death in contemporary adult congenital heart disease patients under follow‐up at a large tertiary centre. Circulation. 2015;132:2118–2125. [DOI] [PubMed] [Google Scholar]
- 4. Oechslin EN, Harrison DA, Connelly MS, Webb GD, Siu SC. Mode of death in adults with congenital heart disease. Am J Cardiol. 2000;86:1111–1116. [DOI] [PubMed] [Google Scholar]
- 5. Engelings CC, Helm PC, Abdul‐Khaliq H, Asfour B, Bauer UM, Baumgartner H, Kececioglu D, Korten MA, Diller GP, Tutarel O. Cause of death in adults with congenital heart disease—an analysis of the German National Register for Congenital Heart Defects. Int J Cardiol. 2016;211:31–36. [DOI] [PubMed] [Google Scholar]
- 6. Raissadati A, Nieminen H, Haukka J, Sairanen H, Jokinen E. Late causes of death after pediatric cardiac surgery: a 60‐year population‐based study. J Am Coll Cardiol. 2016;68:487–498. [DOI] [PubMed] [Google Scholar]
- 7. Pillutla P, Shetty KD, Foster E. Mortality associated with adult congenital heart disease: trends in the US population from 1979 to 2005. Am Heart J. 2009;158:874–879. [DOI] [PubMed] [Google Scholar]
- 8. Zomer AC, Vaartjes I, Uiterwaal CS, van der Velde ET, van den Merkhof LF, Baur LH, Ansink TJ, Cozijnsen L, Pieper PG, Meijboom FJ, et al. Circumstances of death in adult congenital heart disease. Int J Cardiol. 2012;154:168–172. [DOI] [PubMed] [Google Scholar]
- 9. Oliver JM, Gallego P, Gonzalez AE, Garcia‐Hamilton D, Avila P, Alonso A, Ruiz‐Cantador J, Peinado R, Yotti R, Fernandez‐Aviles F. Impact of age and sex on survival and causes of death in adults with congenital heart disease. Int J Cardiol. 2017;245:119–124. [DOI] [PubMed] [Google Scholar]
- 10. Glidewell J, Book W, Raskind‐Hood C, Hogue C, Dunn JE, Gurvitz M, Ozonoff A, McGarry C, Van Zutphen A, Lui G, et al. Population‐based surveillance of congenital heart defects among adolescents and adults: surveillance methodology. Birth Defects Res. 2018;110:1395–1403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Marelli AJ, Ionescu‐Ittu R, Mackie AS, Guo L, Dendukuri N, Kaouache M. Lifetime prevalence of congenital heart disease in the general population from 2000 to 2010. Circulation. 2014;130:749–756. [DOI] [PubMed] [Google Scholar]
- 12. Cohen S, Liu A, Gurvitz M, Guo L, Therrien J, Laprise C, Kaufman JS, Abrahamowicz M, Marelli AJ. Exposure to low‐dose ionizing radiation from cardiac procedures and malignancy risk in adults with congenital heart disease. Circulation. 2018;137:1334–1345. [DOI] [PubMed] [Google Scholar]
- 13. Giamberti A, Lo Rito M, Conforti E, Varrica A, Carminati M, Frigiola A, Menicanti L, Chessa M. Acquired coronary artery disease in adult patients with congenital heart disease: a true or a false problem? J Cardiovasc Med (Hagerstown). 2017;18:605–609. [DOI] [PubMed] [Google Scholar]
- 14. Bauer UMM, Korten MA, Diller GP, Helm P, Baumgartner H, Ewert P, Tutarel O. Cardiovascular risk factors in adults with congenital heart defects—recognised but not treated? An analysis of the German National Register for Congenital Heart Defects. Int J Cardiol. 2019;277:79–84. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1


